Key Points
Question
What differences between 3-dimensional and 2-dimensional endoscopy are important in endoscopic ear surgery?
Findings
In this cohort study including 16 inexperienced and experienced surgeons, surgical assessment revealed similar operating times for both techniques with a slight advantage for the 3-dimensional technique when used by inexperienced surgeons. Surgeons indicated a preference for the 3-dimensional technique, even though a higher incidence of eye strain was observed; recordings of eye movements suggest the need for dedicated training in 3-dimensional endoscopy, even for experienced surgeons.
Meanings
Three-dimensional endoscopy appears to be suitable for endoscopic ear surgery, especially for inexperienced surgeons whose mental model of the intervention has still to be consolidated; the application of 3-dimensional endoscopy in clinical routines and for educational purposes may be feasible and beneficial.
Abstract
Importance
Endoscopic ear surgery (EES) is an emerging technique to treat middle ear diseases; however, the interventions are performed in 2-dimensional (2D) endoscopic views, which do not provide depth perception. Recent technical developments now allow the application of 3-dimensional (3D) endoscopy in EES.
Objective
To investigate the usability, advantages, and disadvantages of 3D vs 2D endoscopy in EES under standardized conditions.
Design, Setting, and Participants
This cohort study conducted at a tertiary academic medical center in Bern, Switzerland, included 16 residents and consultants of the Department of Otorhinolaryngology, Head & Neck Surgery, Inselspital, Bern.
Interventions
Each participant performed selected steps of a type I tympanoplasty and stapedotomy in 3D and 2D views in a cadaveric model using a randomized, Latin-square crossover design.
Main Outcomes and Measures
Time taken to perform the EES, number of attempts, and accidental damage during the dissections were compared between 3D and 2D endoscopy. Eye tracking was performed throughout the interventions. Cognitive load and subjective feedback were measured by standardized questionnaires.
Results
Of the 16 surgeons included in the study (11 inexperienced residents; 5 experienced consultants), 8 were women (50%); mean age was 36 years (range, 27-57 years). Assessment of surgical time revealed similar operating times for both techniques (181 seconds in 2D vs 174 seconds in 3D). A total of 64 surgical interventions were performed. Most surgeons preferred the 3D technique (10 for 3D vs 6 for 2D), even though a higher incidence of eye strain, measured on a 7-point Likert scale, was observed (3D, 2.19 points vs 2D, 1.44 points; mean difference , 0.74; 95% CI, 0.29-1.20; r = 0.67). Eye movement assessment revealed a higher duration of fixation for consultants in 2D (0.79 seconds) compared with 3D endoscopy (0.54 seconds), indicating a less-efficient application of previously acquired experiences using the new technique. Residents (mean [SD], 49.02 [16.4]) had a significantly higher workload than consultants (mean [SD], 27.21 [12.20]), independent of the used technique or task.
Conclusions and Relevance
Three-dimensional endoscopy is suitable for EES, especially for inexperienced surgeons whose mental model of the intervention has yet to be consolidated. The application of 3D endoscopy in clinical routines and for educational purposes may be feasible and beneficial.
This cohort study compares the use of 3-dimensional vs 2-dimensional endoscopes by surgeons performing endoscopic ear surgery.
Introduction
Endoscopic ear surgery (EES) is gaining popularity among ear surgeons because it permits minimally invasive and functional surgery. Advantages of the endoscopic technique include (1) panoramic views of middle ear anatomy,1 especially of the retrotympanum and hypotympanum2,3,4; (2) enhanced magnification of very small anatomic structures, such as, a malformed stapes5; (3) the possibility to use angled endoscopes6; (4) preservation of healthy mastoid and middle ear mucosa7; and (5) possible shorter operating times.8 However, the endoscopic technique has its inherent challenges: (1) because it is a 1-handed technique, the learning curve is deemed to be slower and management of bleeding may be challenging,9 (2) the narrow space available in the external auditory canal (EAC) limits the movements of surgical instruments, (3) disease inside the mastoid may not be addressed, and (4) until recently, high-definition camera systems were exclusively 2-dimensional (2D).
However, recent technical developments now permit 3-dimensional (3D) endoscopy based on 2-lens camera systems and passive polarizing glasses worn by the surgeon, providing stereoscopic depth perception, which may improve visibility and spatial acuity in the operating field. The applicability of 3D endoscopy in EES has recently been reported in a case series.10
To our knowledge, no comparative studies have been performed in EES to investigate surgical performance in 3D vs 2D endoscopy. Using a randomized, Latin-square crossover study design, we aimed to assess the usability, advantages, and disadvantages of 3D vs 2D endoscopy in EES. In addition, we looked into the association between the additional information provided by 3D endoscopy and eye movement patterns. It has been shown that eye movement analysis (duration and number of fixations, blink rates) is able to distinguish between different tasks, different levels of expertise, and different contexts.11,12 Therefore, we aimed to determine differences in gaze behavior to offer additional insights into the utility and advantages of 3D vs 2D endoscopy.
Methods
Study Setup and Participants
All senior surgeons and residents of the Otorhinolaryngology, Head and Neck Surgery Department at Inselspital, University Hospital Bern, Bern, Switzerland, were invited to participate in this study. The only restriction was normal visual acuity or vision corrected by contact lenses. Glasses were not permitted because of simultaneous eye tracking. Demographic characteristics were assessed, including the participants’ prior endoscopic experience. The institutional review board (Kantonale Ethikkomission Bern) granted approval for the study. All participants signed an informed consent form; no financial compensation was provided.
A within-subjects Latin-square design was used: the participants were consecutively taught to perform predefined surgical steps of a relatively easy task (type I tympanoplasty) and an advanced task (stapedotomy) in 2D and in 3D view in each intervention. We used a Latin square13 to counterbalance the order of interventions (tympanoplasty, stapedotomy) and techniques (2D, 3D endoscopy), resulting in 4 different experimental sequences, each administered to 4 of the participants (eTable 1 in the Supplement).
Specimen Preparation
First, the cadaveric specimen (right ear of a Thiel-fixed, whole head preparation) was positioned and a tympanomeatal flap, including detachment of the eardrum from the handle of the malleus, was prepared according to a previously published dissection manual.14 A slight enlargement of the EAC and curettage of the scutum were performed consecutively to allow unhindered access to the stapes. The chorda tympani was resected to guarantee standardized conditions for all participants in case of accidental transection. The incudostapedial joint was disarticulated and the stapes suprastructure was removed using a diode laser (FOX laser, A.R.C. Laser GmbH), followed by a laser platinotomy.
Dissection Tasks
Participants performed the surgical steps on the same cadaveric specimen using 4-mm diameter, 18-cm length 2D and 3D endoscopes (Karl Storz SE & Co KG). Standard otologic tools were used. Before the measurements were taken, the participants were instructed on the handling of the endoscopes and had time to explore the middle ear.
For the tympanoplasty task, the participants were asked to place the tympanomeatal flap on the anterior wall of the EAC and an artificial membrane (Biodesign; Cook Medical) using the underlay technique. Thereafter, the tympanomeatal flap was brought back on the membrane and into its final position. The task was considered successfully completed if the membrane was positioned on the handle of the malleus and completely covered the superior quadrants of the eardrum.
The stapedotomy task consisted of the positioning of a piston prosthesis (0.5 × 4.5 mm) (Heinz Kurz GmbH Medizintechnik) on the long process of the incus and inside the platinotomy. No crimping was performed to facilitate removal of the prosthesis.
Perioperative Measurements
For both tasks, the time taken for completion and the number of attempts required were measured. During the tympanoplasty task, 2 graders, blinded to the study hypothesis, assessed the number of involuntary contacts with the ossicular chain. In addition, we measured the participants’ cognitive workload after each trial using the NASA Task Load Index.15 The questionnaire consisted of 6 subscales (mental demand, physical demand, temporal demand, performance, effort, and frustration), each scale ranging from 0 to 100.16,17,18,19
While performing the tasks, the surgeons’ eye movements during the task were recorded with a head-mounted eye-tracking device (SensoMotoric Instruments) (Figure 1). The applied eye-tracker has a gaze position accuracy of 0.5° and a frame rate of 60 Hz and was calibrated before each task with a 3-point calibration method. For computation of fixation durations (mean duration of fixations per task) and blink rates (blinks per minute), we used BeGaze Analysis software, version 3.7 (SensoMotoric Instruments).
Figure 1. Experimental Setup.
Illustration of the eye tracking glasses and endoscopic setup for 3-dimensional (A) and 2-dimensional (B) endoscopy.
Postoperative Assessment
Immediately on completion of all 4 dissection trials, participants completed computer-based questionnaires.20 They were asked to rate the 3D endoscope and the 2D endoscope separately based on a 7- or 5-point Likert scale with regard to the usability,21 naturalness,21 perceived discomfort,21 depth perception,22 and image quality22 of the techniques (eTable 2 in the Supplement). Participants also made a direct comparison of the 2 endoscopes with regard to 9 aspects (Table 1).
Table 1. Participant Assessment of the 2 Endoscopic Techniques (N = 16).
| Question | Participants in favor of 3D | Participants in favor of 2D |
|---|---|---|
| If you had the choice, with which endoscopic technique would you perform future interventions? | 13 | 3 |
| Which technique offers the better depth perception? | 13 | 3 |
| Which technique offers the better views of middle ear anatomy? | 13 | 3 |
| Overall, with which technique were the tasks easier? | 11 | 5 |
| Which endoscope was easier to handle? | 5 | 11 |
| Overall, which technique did you prefer? | 10 | 6 |
| Which technique offered the better image quality? | 9 | 7 |
| Overall, in which technique were the tasks more comfortable? | 9 | 7 |
Abbreviations: 2D, 2-dimensional; 3D, 3-dimensional.
Statistical Analysis
We used an analysis of variance (general linear model for repeated measures) to examine differences in the dependent variables assessed during surgery (time required, cognitive workload, fixation duration, blink rate). Endoscopic technique (3D and 2D) and task (tympanoplasty and stapedotomy) were used as within-subject variables and medical experience (residents vs consultants) was used as a between-subject variable. A square-root transformation of the indices was considered where appropriate. The values for the involuntary contacts with the ossicular chain and the number of attempts were right-skewed (skewness >1.10), indicating that distributions were not normal.23 Because transformation did not strongly decrease skewness (>0.95), we used nonparametric Wilcoxon signed rank tests for paired samples to compare these values between the 2 techniques. The ratings of the 2 endoscopic techniques were analyzed with t tests for paired data, and binomial tests were used to examine the direct comparisons. Variables are described in terms of mean (SD) values unless otherwise noted. Effect size metrics, including Cohen d, were used to describe the magnitude of the difference between compared groups and, where appropriate, 95% CIs were used to describe the precision of the effect size metric. The Cohen test suggested that d = 0.2 be considered a small effect size; 0.5, a medium effect size; and 0.8, a large effect size.24 P < .05 was deemed statistically significant. All computations were executed in R, version 3.5 (R Foundation for Statistical Computing).25
Results
Participants
A total of 64 surgical interventions in 2D and 3D views performed by 16 participants were analyzed. The mean age of the participants was 36 years (range, 25-57); 8 were women (50%). All participants were assigned as either residents (n = 11) or consultants (n = 5) according to their clinical function. Regarding prior experience in endoscopic surgery, including functional endoscopic sinus surgery, there was a large difference between the groups with a median experience of 0 procedures (range, 0-40) in the residents group and 300 procedures (range, 200-5000) in the consultants group.
Personal Preference
The subjective feedback provided by participants at the end of all surgical tasks revealed a significant difference in 2 ratings (eTable 1 in the Supplement). Measured on a 7-point Likert scale, visual discomfort was perceived to be higher for 3D endoscopy (2.19 points) compared with 2D endoscopy (1.44 points) (mean difference, 0.74; 95% CI, 0.29-1.20; r = 0.67), and depth perception was rated higher when using the 3D compared with the 2D technique (mean difference, 1.62; 95% CI, 0.49-2.76; r = 0.62). Direct comparison revealed a preference of the participants for the 3D endoscope, with 13 participants selecting 3D for use in future procedures vs 3 participants favoring 2D and, overall, 10 participants favoring 3D and 6 favoring 2D (Table 1).
Surgical Assessment
The order of trials had no significant association with the time required for the tasks, indicating a successful application of the Latin-square design. Results showed that the time required for the trials differed between the 2 surgical tasks, as well as between the 2 experience levels. The tympanoplasty took longer to complete than the stapedotomy task, independent of the function or the endoscopic technique (mean [SD] difference, 85.31 [23.98] seconds; 95% CI, 37.96-132.67 seconds; r = 0.59). Assessment of surgical time revealed similar operating times for both techniques (181 seconds in 2D vs 174 seconds in 3D). Moreover, residents needed more time to complete the tasks than the consultants (Table 2). These observations were independent of the task or the technique used (total mean [SD] difference, 83.35 [31.83] seconds; 95% CI, 17.25-149.44 seconds; r = 0.59), which was confirmed by Kendall τ = 0.245. We observed a tendency toward faster execution of the surgical tasks using 3D endoscopy in the residents group (mean [SD] for tympanoplasty: 256 [128] seconds in 3D vs 264 [106] seconds in 2D; stapedotomy: mean, 129 [73] seconds in 3D vs 167 [154] seconds in 3D); in contrast, consultants took longer to perform the same interventions in 3D compared with 2D (mean [SD] for tympanoplasty: 147 [55] seconds in 3D vs 120 [21] seconds in 2D; stapedotomy: 123 [124] seconds in 3D vs 92 [59] seconds in 3D) (Table 2) (mean [SD] difference, –52.64 [63.46] seconds; 95% CI, –183.32 to 78.05 seconds; r = 0.22).
Table 2. Time Required to Complete Procedure as a Function of Task and Experience.
| Procedure | 2-Dimensional | 3-Dimensional | ||||
|---|---|---|---|---|---|---|
| Mean (SD) Difference, s | Difference (95% CI) | Mean (SD) Difference, s | Difference (95% CI) | |||
| Resident (n = 22) | Consultant (n = 10) | Resident (n = 22) | Consultant (n = 10) | |||
| Tympanoplasty (n = 32) | 264 (106) | 120 (21) | 144 (46.3 to 242.3) | 256 (128) | 147 (55) | 109 (−12.7 to 229.7) |
| Stapedotomy (n = 32) | 167 (154) | 92 (59) | 75 (−69.8 to 219.9) | 129 (73) | 123 (124) | 6 (−92.6 to 103.7) |
| Total (n = 64) | 216 (138) | 106 (44) | 110 (1.6 to 217.7) | 192 (121) | 135 (91) | 57 (−23.4 to 137.4) |
Analysis of the number of attempts required to fulfill the assignments and the number of involuntary contacts with the ossicular chain revealed no meaningful differences between the 2 techniques. The median difference for the number of involuntary contacts was -0.50 (95% CI, -1.50 to 0.99).
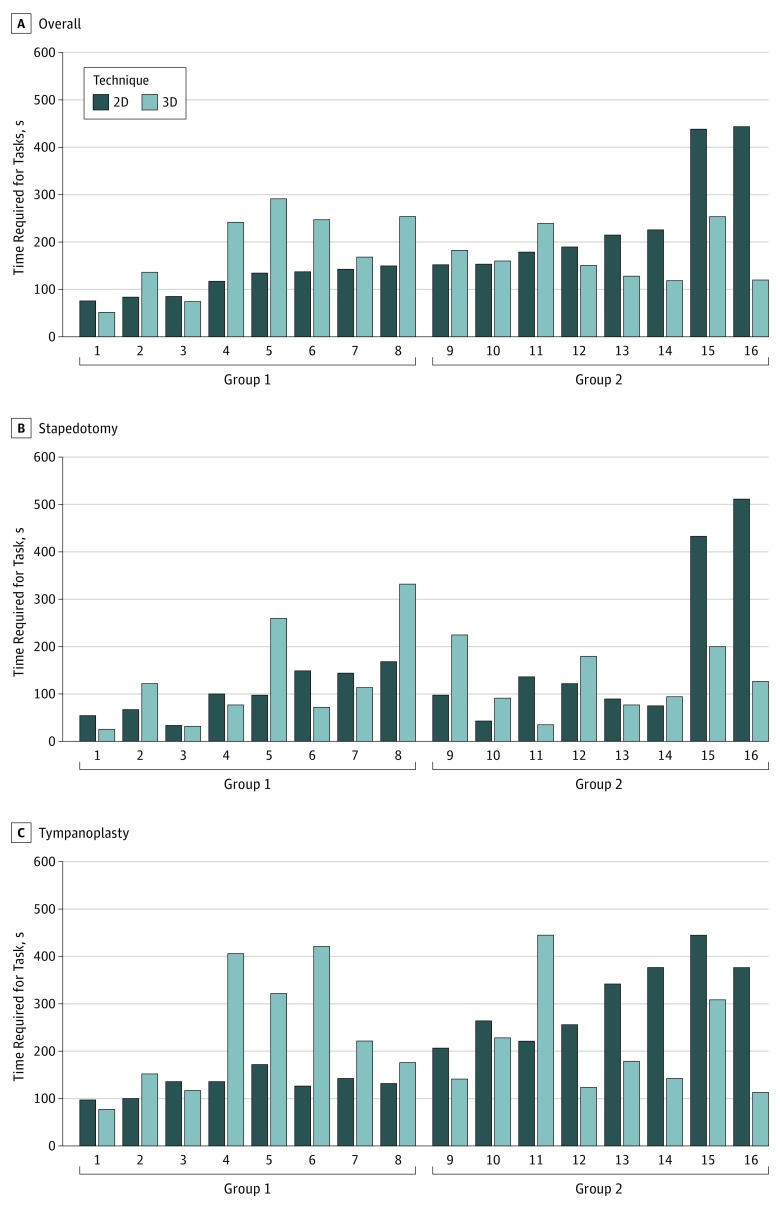
Surgical speed in the standard 2D technique is another indicator of expertise. By calculating a 3D/2D ratio, it would be possible to draw conclusions on the utility of the 3D technique, especially in surgeons not previously trained in it. Therefore, we investigated the association between the endoscopic technique and the time required to fulfill the tasks by dividing the participants by median split into 2 groups according to the mean time required for both tasks in the 2D technique: group 1 (<150 seconds) and group 2 (≥150 seconds). Subsequently, to analyze the outcome of prior experience with the 2D technique (faster surgical time), we compared the 3D/2D time ratio of these groups using a Welch t test. The ratio of 3D/2D completion time was significantly higher in group 1 (mean, 1.52) compared with group 2 (mean, 0.79; t12.31 = 3.07; 95% CI, 0.21-1.24; r = 0.659) (Figure 2).
Figure 2. Surgical Completion Times for All 16 Surgeons.
Mean time for both tasks (A), stapedotomy (B), and type I tympanoplasty (C) by group 1 (time required, <150 seconds) and group 2 (time required, ≥150 seconds). 2D indicates 2-dimensional; 3D, 3-dimensional.
Cognitive Load
Assessment of cognitive load after each task revealed a lower cognitive load with increasing experience. Residents (mean [SD], 49.02 [16.40] points) had a higher workload than consultants (mean [SD], 27.21 [12.20] points), independent of the technique used or the task (mean change, 21.81; 95% CI, 7.52-36.10).
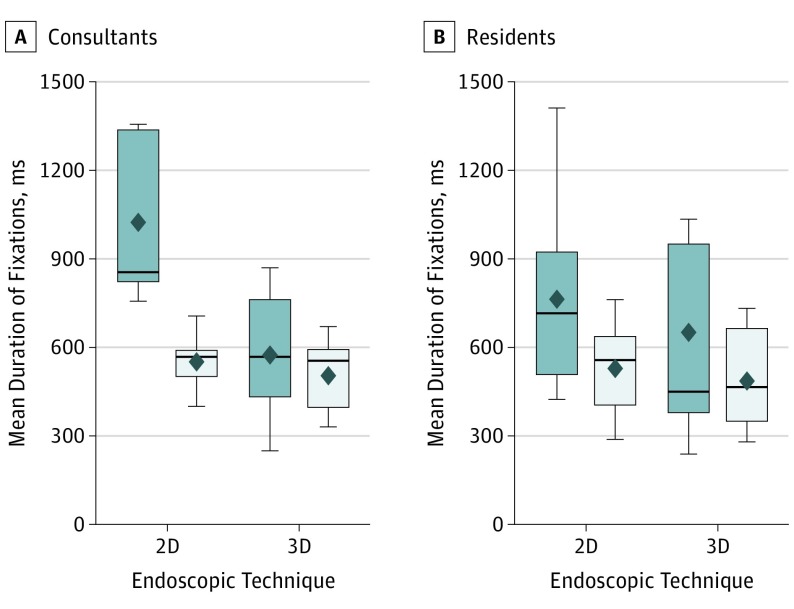
Intraoperative Analysis of Eye Movements
Mean duration of fixation differed between residents and consultants (Figure 3). Residents had longer fixation duration in the stapedotomy task than in the tympanoplasty task (eTable 3 in the Supplement), independent of the endoscopic technique used (mean change, -0.24 seconds; 95% CI, -0.36 to -0.12 seconds). Consultants also had higher mean fixation duration for the stapes task than the tympanoplasty task; however, this difference increased when using the 2D endoscope (eTable 3 in the Supplement) (mean change, 0.34 seconds; 95% CI, 0.0-0.70 seconds). While the fixation duration between the tasks differed marginally between residents and consultants in 3D endoscopy (0.07 seconds), it increased when consultants used the 2D endoscope (0.47 seconds) (Figure 3).
Figure 3. Eye Movement Analysis.
Duration of eye fixation specified per position, task, and endoscope used by consultants (A) and residents (B). The box represents 50% of procedures, the line indicates the median value, and the point indicates the mean value. The top and bottom borders of the box mark the 75th and 25th percentiles, respectively. The whiskers above and below the box mark the 90th and 10th percentiles. 2D indicates 2-dimensional; 3D, 3-dimensional.
Furthermore, blink rate was higher in 3D endoscopy (mean [SD], 9.10 [8.45]) than in 2D endoscopy (mean [SD], 6.68 [5.40]), independent of the task completed or participants’ medical experience (mean [SD] change, 2.42 [1.02]; 95% CI, 0.26-4.57; r = 0.49).
Discussion
Surgical Considerations
This study investigated, in a randomized, Latin-square crossover design, the use of 3D vs 2D endoscopy in EES. Under standardized and controlled laboratory conditions, the study participants performed a type I tympanoplasty, which is an easy or beginners’ operation, and the placement of a stapes prosthesis during stapedotomy, which is an advanced surgical task. Moreover, the tympanoplasty task requires less depth perception because the surgical steps are performed in almost the same plane, whereas, the placement of the stapes prosthesis requires good depth perception. The main surgical outcome in terms of operating time revealed shorter surgical times with growing experience, confirming a realistic experimental setup.
Comparing results from functional endoscopic sinus surgery, a 2017 study observed a significantly shorter time in 3D compared with 2D endoscopy on a surgical simulator. Moreover, beginners reported a preference for 3D compared with experts.26 Another study identified the 3D system to be useful in clinical practice.27 Similar results have been reported for laparoscopic surgery.28,29 We observed a tendency toward faster execution of the surgical tasks using 3D endoscopy in the residents group; in contrast, consultants took longer to perform the same interventions in 3D endoscopy. Whether these differences would represent a clinically significant outcome during procedures in the operating room is difficult to assess because this study was conducted under standardized conditions in a model. The 3D/2D ratios between the fast and slow group in 2D (Figure 2) showed differences with regard to surgical speed. A possible explanation for this finding might be because surgical speed in the standard 2D technique is another measure of expertise; therefore, the decreased 3D/2D ratio for the slower surgeons in 2D may indicate an increased utility of 3D endoscopy for inexperienced surgeons. The increased utility of 3D endoscopy for inexperienced surgeons can be related to the strategies developed by the experienced surgeons to overcome the limited depth perception in the 2D technique and, therefore, the measurable benefit from the additionally provided information in 3D would be lower. In contrast, inexperienced surgeons do not rely on previously acquired skills and may easily benefit from the additionally offered information in the 3D view.
Cognitive Load
The subjective assessment of mental workload was comparable between 2D and 3D endoscopy, indicating no disadvantage for either technique in this setting. Previous research using the same subjective measurement for cognitive load but applied to laparoscopic tasks showed variable outcomes. Gómez-Gómez et al30 and Smith et al31 found a decrease in cognitive load for the 3D technique, suggesting a benefit for surgeons’ cognitive capacity using 3D technology. However, Wilhelm et al19 observed no difference between 2D and 3D setups. Taken together, there is no reason to assume that 3D endoscopy affects the surgeon’s cognitive capacity in any negative way.
Eye Movements
Fixation duration answers the question of how long the eyes and therefore the attention of the surgeon stay still and focused on a specific area of the surgical field.32 In our study, this focus differed between residents and consultants, which is consistent with previous research reporting longer fixation durations for experienced surgeons.33,34,35,36 These observations are interpreted under the information reduction hypothesis, which assumes that experts limit the processing of information that is not task relevant. Therefore, expert surgeons have longer fixation periods on the relevant area of interest as learned with growing experience.37 Also, the overall fixation duration was longer during the stapedotomy task, which is presumably because of the different kind of surgical task, which is consistent with previous results.33
In the present study, the 3D technique was associated with shorter fixation duration in the consultants’ eye movements, whereas it only marginally affected the residents’ gaze. These results indicate a hindered efficiency of the target-focused strategy in well-known tasks for the 3D technique. One likely explanation for this phenomenon could be the increase in information provided in the 3D view. Perceiving more depth detail in the 3D view, consultants might be distracted and less able to count on their mental model of the task. The decrease in fixation duration could suggest that, even though the consultants’ surgical performance did not appear to be hindered in 3D endoscopy, the technique requires the development of a new gaze strategy. We believe that this observation indicates the necessity for a dedicated learning curve, even for well-trained surgeons, when adopting a new surgical technique.
Blink rate has often been associated with mental workload, indicating lower blink rates for higher workloads.38 However, compared with the subjective assessment in the present study, the patterns diverge. Thus, it seems more plausible that the difference in blink rate was associated with the medium’s effect. In several cases, blink rate has been associated with eye strain and visual discomfort, especially for 3D displays.39,40 This outcome is also consistent with the participants’ personal rating, which states that more visual discomfort was perceived with 3D than 2D endoscopy. In our experience, this represents the only limitation to the application of 3D endoscopy in EES.
Personal Preference of Surgeons
In total, 10 of 16 participants in the present study preferred the 3D over the 2D technique. Thirteen participants would adopt the 3D technique in their future practice if they could choose. We observed that residents favored the 3D technique overall (8:3 in favor of 3D). These subjective perceptions indicate that 3D endoscopy will likely play an important part in the development of future surgical techniques.
Limitations
This study has limitations. Because the procedure was performed on a cadaveric model, the results may not be directly applicable to real surgery. Although we used 4-mm diameter, 18-cm length endoscopes for both techniques, the shape of the endoscopes is not similar for 2D and 3D endoscopy (Figure 1).
Conclusions
The surgical assessment revealed similar operating times for both 2D and 3D techniques. Most surgeons expressed a preference for the 3D technique, even though a higher incidence of eye strain was observed. Eye movement assessment revealed a decreased fixation duration for 3D endoscopy in experienced surgeons, indicating a less-efficient application of previous experiences. Therefore, 3D endoscopy may be especially suitable for EES, for inexperienced surgeons whose mental model of the intervention has yet to be consolidated. The application of 3D endoscopy in clinical routines and for educational purposes appears to be feasible and to offer advantages.
eTable 1. Counterbalanced Design of Trial Order by Latin Square
eTable 2. Postoperative Questionnaires Answered by Participants for Both Endoscopic Techniques
eTable 3. Mean and Standard Deviation for Fixation Duration in Milliseconds
References
- 1.Anschuetz L, Huwendiek S, Stricker D, Yacoub A, Wimmer W, Caversaccio M. Assessment of middle ear anatomy teaching methodologies using microscopy versus endoscopy: a randomized comparative study [published online November 14, 2018]. Anat Sci Educ. doi: 10.1002/ase.1837 [DOI] [PubMed] [Google Scholar]
- 2.Bonali M, Anschuetz L, Fermi M, et al. The variants of the retro- and hypotympanum: an endoscopic anatomical study. Eur Arch Otorhinolaryngol. 2017;274(5):2141-2148. doi: 10.1007/s00405-017-4492-0 [DOI] [PubMed] [Google Scholar]
- 3.Anschuetz L, Alicandri-Ciufelli M, Bonali M, et al. Novel surgical and radiologic classification of the subtympanic sinus: implications for endoscopic ear surgery [published online July 1, 2018]. Otolaryngol Head Neck Surg. 2018;194599818787180. doi: 10.1177/0194599818787180 [DOI] [PubMed] [Google Scholar]
- 4.Alicandri-Ciufelli M, Fermi M, Bonali M, et al. Facial sinus endoscopic evaluation, radiologic assessment, and classification. Laryngoscope. 2018;128(10):2397-2402. doi: 10.1002/lary.27135 [DOI] [PubMed] [Google Scholar]
- 5.Marchioni D, Soloperto D, Villari D, et al. Stapes malformations: the contribute of the endoscopy for diagnosis and surgery. Eur Arch Otorhinolaryngol. 2016;273(7):1723-1729. doi: 10.1007/s00405-015-3743-1 [DOI] [PubMed] [Google Scholar]
- 6.Bennett ML, Zhang D, Labadie RF, Noble JH. Comparison of middle ear visualization with endoscopy and microscopy. Otol Neurotol. 2016;37(4):362-366. [DOI] [PubMed] [Google Scholar]
- 7.Presutti L, Anschuetz L, Rubini A, et al. The impact of the transcanal endoscopic approach and mastoid preservation on recurrence of primary acquired attic cholesteatoma. Otol Neurotol. 2018;39(4):445-450. [DOI] [PubMed] [Google Scholar]
- 8.Kaya I, Sezgin B, Sergin D, et al. Endoscopic versus microscopic type 1 tympanoplasty in the same patients: a prospective randomized controlled trial. Eur Arch Otorhinolaryngol. 2017;274(9):3343-3349. doi: 10.1007/s00405-017-4661-1 [DOI] [PubMed] [Google Scholar]
- 9.Anschuetz L, Bonali M, Guarino P, et al. Management of bleeding in exclusive endoscopic ear surgery: pilot clinical experience. Otolaryngol Head Neck Surg. 2017;157(4):700-706. doi: 10.1177/0194599817726982 [DOI] [PubMed] [Google Scholar]
- 10.Bernardeschi D, Lahlou G, De Seta D, Russo FY, Mosnier I, Sterkers O. 3D endoscopic ear surgery: a clinical pilot study. Eur Arch Otorhinolaryngol. 2018;275(2):379-384. doi: 10.1007/s00405-017-4839-6 [DOI] [PubMed] [Google Scholar]
- 11.Ashraf H, Sodergren MH, Merali N, Mylonas G, Singh H, Darzi A. Eye-tracking technology in medical education: A systematic review. Med Teach. 2018;40(1):62-69. doi: 10.1080/0142159X.2017.1391373 [DOI] [PubMed] [Google Scholar]
- 12.Hermens F, Flin R, Ahmed I. Eye movements in surgery: a literature review. J Eye Mov Res. 2013;6(4):1-11. doi: 10.16910/jemr.6.4.4 [DOI] [Google Scholar]
- 13.Bradley J. Complete counterbalancing of immediate sequential effects in a Latin square design. J Am Stat Assoc. 1958;53(282):525-528. doi: 10.1080/01621459.1958.10501456 [DOI] [Google Scholar]
- 14.Anschuetz L, Presutti L, Marchioni D, et al. Discovering middle ear anatomy by transcanal endoscopic ear surgery: a dissection manual [published online January 11, 2018]. J Vis Exp. 2018;(131). doi: 10.3791/56390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hart SG, Staveland LE. Development of NASA-TLX (Task Load Index). Adv Psychol. 1988;52:139-183. doi: 10.1016/S0166-4115(08)62386-9 [DOI] [Google Scholar]
- 16.Dias RD, Ngo-Howard MC, Boskovski MT, Zenati MA, Yule SJ. Systematic review of measurement tools to assess surgeons’ intraoperative cognitive workload. Br J Surg. 2018;105(5):491-501. doi: 10.1002/bjs.10795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yurko YY, Scerbo MW, Prabhu AS, Acker CE, Stefanidis D. Higher mental workload is associated with poorer laparoscopic performance as measured by the NASA-TLX tool. Simul Healthc. 2010;5(5):267-271. doi: 10.1097/SIH.0b013e3181e3f329 [DOI] [PubMed] [Google Scholar]
- 18.Zheng B, Cassera MA, Martinec DV, Spaun GO, Swanström LL. Measuring mental workload during the performance of advanced laparoscopic tasks. Surg Endosc. 2010;24(1):45-50. doi: 10.1007/s00464-009-0522-3 [DOI] [PubMed] [Google Scholar]
- 19.Wilhelm D, Reiser S, Kohn N, et al. Comparative evaluation of HD 2D/3D laparoscopic monitors and benchmarking to a theoretically ideal 3D pseudodisplay: even well-experienced laparoscopists perform better with 3D. Surg Endosc. 2014;28(8):2387-2397. doi: 10.1007/s00464-014-3487-9 [DOI] [PubMed] [Google Scholar]
- 20.Qualtrics. http://www.qualtrics.com. Accessed April 1, 2018.
- 21.International Telecommunication Union (ITU) Radio Communication Sector . Recommendation ITU-R BT.500-11. Methodology for the subjective assessment of the quality of television pictures. https://www.itu.int/dms_pubrec/itu-r/rec/bt/R-REC-BT.500-11-200206-S!!PDF-E.pdf. Accessed June 12, 2019.
- 22.Loertscher ML, Weibel D, Spiegel S, et al. As film goes byte: the change from analog to digital film perception. Psychol Aesthetics Creativity Arts. 2016;10(4):458-471. doi: 10.1037/aca0000082 [DOI] [Google Scholar]
- 23.Lienert GA, Raatz U. Test Construction and Test Analysis. 6th ed. Weinheim, Germany: Psychologie Verlags Union; 1998. [Google Scholar]
- 24.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. London, England: Routledge; 1988. [Google Scholar]
- 25.R Core Team . (2014). R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. http://www.R-project.org/. Accessed February 27, 2018.
- 26.Rampinelli V, Doglietto F, Mattavelli D, et al. Two-dimensional high definition versus three-dimensional endoscopy in endonasal skull base surgery: a comparative preclinical study. World Neurosurg. 2017;105:223-231. doi: 10.1016/j.wneu.2017.05.130 [DOI] [PubMed] [Google Scholar]
- 27.Albrecht T, Baumann I, Plinkert PK, Simon C, Sertel S. Three-dimensional endoscopic visualization in functional endoscopic sinus surgery. Eur Arch Otorhinolaryngol. 2016;273(11):3753-3758. doi: 10.1007/s00405-016-4040-3 [DOI] [PubMed] [Google Scholar]
- 28.Alaraimi B, El Bakbak W, Sarker S, et al. A randomized prospective study comparing acquisition of laparoscopic skills in three-dimensional (3D) vs. two-dimensional (2D) laparoscopy. World J Surg. 2014;38(11):2746-2752. doi: 10.1007/s00268-014-2674-0 [DOI] [PubMed] [Google Scholar]
- 29.Matsunaga R, Nishizawa Y, Saito N, Kobayashi A, Ohdaira T, Ito M. Quantitative evaluation of 3D imaging in laparoscopic surgery. Surg Today. 2017;47(4):440-444. doi: 10.1007/s00595-016-1428-z [DOI] [PubMed] [Google Scholar]
- 30.Gómez-Gómez E, Carrasco-Valiente J, Valero-Rosa J, et al. Impact of 3D vision on mental workload and laparoscopic performance in inexperienced subjects. Actas Urol Esp. 2015;39(4):229-235. [DOI] [PubMed] [Google Scholar]
- 31.Smith R, Schwab K, Day A, et al. Effect of passive polarizing three-dimensional displays on surgical performance for experienced laparoscopic surgeons. Br J Surg. 2014;101(11):1453-1459. doi: 10.1002/bjs.9601 [DOI] [PubMed] [Google Scholar]
- 32.Holmqvist K, Nyström M, Andersson R, et al. Eye Tracking: A Comprehensive Guide to Methods and Measures. New York, NY: Oxford University Press; 2011. [Google Scholar]
- 33.Eivazi S, Hafez A, Fuhl W, et al. Optimal eye movement strategies: a comparison of neurosurgeons gaze patterns when using a surgical microscope. Acta Neurochir (Wien). 2017;159(6):959-966. doi: 10.1007/s00701-017-3185-1 [DOI] [PubMed] [Google Scholar]
- 34.Wilson MR, McGrath JS, Vine SJ, Brewer J, Defriend D, Masters RSW. Perceptual impairment and psychomotor control in virtual laparoscopic surgery. Surg Endosc. 2011;25(7):2268-2274. doi: 10.1007/s00464-010-1546-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khan RSA, Tien G, Atkins MS, Zheng B, Panton ONM, Meneghetti AT. Analysis of eye gaze: do novice surgeons look at the same location as expert surgeons during a laparoscopic operation? Surg Endosc. 2012;26(12):3536-3540. doi: 10.1007/s00464-012-2400-7 [DOI] [PubMed] [Google Scholar]
- 36.Richstone L, Schwartz MJ, Seideman C, Cadeddu J, Marshall S, Kavoussi LR. Eye metrics as an objective assessment of surgical skill. Ann Surg. 2010;252(1):177-182. doi: 10.1097/SLA.0b013e3181e464fb [DOI] [PubMed] [Google Scholar]
- 37.Haider H, Frensch PA. Eye movement during skill acquisition: more evidence for the information-reduction hypothesis. J Exp Psychol Learn Mem Cogn. 1999;25(1):172-190. doi: 10.1037/0278-7393.25.1.172 [DOI] [Google Scholar]
- 38.Brookings JB, Wilson GF, Swain CR. Psychophysiological responses to changes in workload during simulated air traffic control. Biol Psychol. 1996;42(3):361-377. doi: 10.1016/0301-0511(95)05167-8 [DOI] [PubMed] [Google Scholar]
- 39.Cho S-H, Kang H-B. An assessment of visual discomfort caused by motion-in-depth in stereoscopic 3D video. Proc Br Mach Vis Conf. 2011:1-10. [Google Scholar]
- 40.Lee EC, Heo H, Park KR. The comparative measurements of eyestrain caused by 2D and 3D displays. IEEE Trans Consum Electron. 2010;56(3):1677-1683. doi: 10.1109/TCE.2010.5606312 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Counterbalanced Design of Trial Order by Latin Square
eTable 2. Postoperative Questionnaires Answered by Participants for Both Endoscopic Techniques
eTable 3. Mean and Standard Deviation for Fixation Duration in Milliseconds