Key Points
Question
The evolving demographics, care patterns, and outcomes in the modern cardiac intensive care unit (CICU) are incompletely characterized.
Findings
In this study of 3049 consecutive admissions in the Critical Care Cardiology Trials Network (CCCTN), an investigator-initiated network of North American tertiary CICUs, while ACS and heart failure were the most common admission diagnoses, the range of acute cardiac conditions was diverse. The most common indications for CICU admission were respiratory insufficiency and shock; resource use was high, and the outcome was poor for many indications.
Meaning
The CCCTN provides a multicenter characterization of contemporary CICU care and could be used as a platform for observational studies and randomized clinical trials.
Abstract
Importance
Single-center and claims-based studies have described substantial changes in the landscape of care in the cardiac intensive care unit (CICU). Professional societies have recommended research to guide evidence-based CICU redesigns.
Objective
To characterize patients admitted to contemporary, advanced CICUs.
Design, Setting, and Participants
This study established the Critical Care Cardiology Trials Network (CCCTN), an investigator-initiated multicenter network of 16 advanced, tertiary CICUs in the United States and Canada. For 2 months in each CICU, data for consecutive admissions were submitted to the central data coordinating center (TIMI Study Group). The data were collected and analyzed between September 2017 and 2018.
Main Outcomes and Measures
Demographics, diagnoses, management, and outcomes.
Results
Of 3049 participants, 1132 (37.1%) were women, 797 (31.4%) were individuals of color, and the median age was 65 years (25th and 75th percentiles, 55-75 years). Between September 2017 and September 2018, 3310 admissions were included, among which 2557 (77.3%) were for primary cardiac problems, 337 (10.2%) for postprocedural care, 253 (7.7%) for mixed general and cardiac problems, and 163 (4.9%) for overflow from general medical ICUs. When restricted to the initial 2 months of medical CICU admissions for each site, the primary analysis population included 3049 admissions with a high burden of noncardiovascular comorbidities. The top 2 CICU admission diagnoses were acute coronary syndrome (969 [31.8%]) and heart failure (567 [18.6%]); however, the proportion of acute coronary syndrome was highly variable across centers (15%-57%). The primary indications for CICU care included respiratory insufficiency (814 [26.7%]), shock (643 [21.1%]), unstable arrhythmia (521 [17.1%]), and cardiac arrest (265 [8.7%]). Advanced CICU therapies or monitoring were required for 1776 patients (58.2%), including intravenous vasoactive medications (1105 [36.2%]), invasive hemodynamic monitoring (938 [30.8%]), and mechanical ventilation (652 [21.4%]). The overall CICU mortality rate was 8.3% (95% CI, 7.3%-9.3%). The CICU indications that were associated with the highest mortality rates were cardiac arrest (101 [38.1%]), cardiogenic shock (140 [30.6%]), and the need for renal replacement therapy (51 [34.5%]). Notably, patients admitted solely for postprocedural observation or frequent monitoring had a mortality rate of 0.2% to 0.4%.
Conclusions and Relevance
In a contemporary network of tertiary care CICUs, respiratory failure and shock predominated indications for admission and carried a poor prognosis. While patterns of practice varied considerably between centers, a substantial, low-risk population was identified. Multicenter collaborative networks, such as the CCCTN, could be used to help redesign cardiac critical care and to test new therapeutic strategies.
This study characterizes patients admitted to US cardiac intensive care units within the Critical Care Cardiology Trials Network.
Introduction
Coronary care units originated in the 1960s with the goal of rapidly resuscitating patients with dysrhythmias complicating acute myocardial infarction (MI), but have evolved into cardiac intensive care units (CICUs) that deliver comprehensive critical care for patients with cardiovascular diseases.1 A series of important single-center and small multicenter studies have described substantial changes in the landscape of care in terms of diagnoses, acuity, comorbidity, and the need for noncardiac ICU therapies in the CICUs in the United States.2,3,4,5,6 In addition, a nationwide study using Medicare administrative data demonstrated an increase in the proportion of noncardiac primary diagnoses in contemporary US CICUs, reflecting an increase in chronic cardiovascular conditions complicated by noncardiac acute illnesses triaged to CICUs (eg, severe cardiomyopathy with sepsis).6 In light of such changes, expert groups from international professional societies have identified a need for CICUs to adapt to this transformation of cardiac critical care and called for additional research to quantitatively characterize the demographics, diagnoses, therapies, technology, and outcomes in contemporary CICUs to aid in directing such redesigns.1,7,8 Additionally, experts have identified gaps in the evidence guiding the organization of CICUs as well as the management of the highly morbid conditions encountered in these units.1,9,10 Despite the substantial resource consumption and heightened risk of many conditions requiring CICU care, to our knowledge, there are few high-quality prospective studies and randomized clinical trials to guide practice in this environment.
Therefore, we established an investigator-initiated, multicenter network focused on cardiac critical care to (1) quantitatively characterize cardiac critical care in contemporary advanced CICUs and (2) develop an infrastructure for nested, pragmatic, clinical trials in critical care cardiology. This inaugural registry of the network aimed to determine the demographics, diagnoses, and outcomes for patients who were triaged to receive cardiac critical care.
Methods
Registry Design and Data Collection
The Critical Care Cardiology Trials Network (CCCTN) is a voluntary, collaborative research network of advanced (American Heart Association level 11) CICUs in the United States and Canada (eTable in the Supplement). Scientific oversight of the CCCTN is conducted by its academic executive and steering committees. The CCCTN is coordinated by the TIMI Study Group of Brigham and Women's Hospital (Boston, Massachusetts).
In this first CCCTN project, each participating center contributed data for all consecutive medical CICU admissions for 2 months. To focus on medical CICU admissions, the primary analysis cohort excluded general medical ICU overflow and admissions solely for postoperative management after cardiac surgery.
Additional details of the inception of the CCCTN and methods are included in the eMethods in the Supplement. Clinical data were collected through a comprehensive standardized clinical review of each patient rather than abstraction from administrative or claims data. Race/ethnicity was according to self-report. All site personnel were trained by the CCCTN Coordinating Center and data captured via the CCCTN registry electronic case report form with remote monitoring of data quality by the TIMI Study Group.
The sequential organ failure assessment (SOFA) score, which ranges from 0 to 24, was developed to predict ICU mortality using arterial oxygenation, supplemental oxygen, mechanical ventilatory status, platelet cell counts, Glasgow Coma Scale score, total bilirubin level, mean arterial pressure, vasopressor use, and renal function.11 In the derivation cohort, a medicosurgical unit, a score of more than 11 was associated with an 80% mortality rate. For this analysis, the maximal SOFA score within 24 hours of CICU admission was calculated for each patient by the local investigator using the raw clinical data and the published SOFA algorithm.4
The CCCTN Registry protocol and waiver of informed consent were reviewed and approved by the institutional review board or ethics committee at Brigham and Women’s Hospital and at each of the participating centers. Consent was waived because of the minimal risk associated with registry enrollment (no personal identifying health information was collected in the registry database) and the importance of collecting data for all consecutive patients to accurately assess the patient population.
Participating Centers
Sixteen enrolling CICUs contributed to this initial campaign of the CCCTN registry (eTable in the Supplement). Participating CICUs were largely based at academic medical centers with cardiologist-led, ICU-based (“closed”) physician staffing (16 [100%]). Most centers were self-described as urban (13 [81.3%]), with only 1 (6.3%) rural in location, and ranged in size from 400 to 1400 hospital beds. The individual CICUs ranged in size from 8 to 28 beds. With 1 exception (6.3%), all centers involved cardiovascular medicine trainees on the CICU team.
Statistical Analyses
The analyses in this study were descriptive. For categorical variables, we reported counts and percentages with absolute 95% confidence intervals when relevant. For continuous variables, we reported the median along with the 25th and 75th percentiles unless otherwise specified. All analyses were conducted using Stata, version 13.1 (StataCorp), or SAS, version 9.4 (SAS Institute).
Results
Population
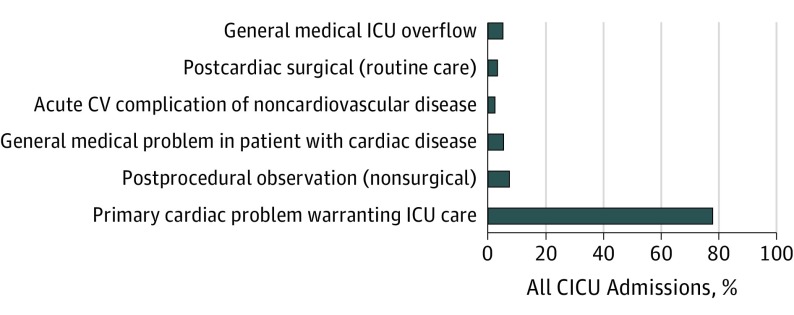
Between September 2017 and September 2018, 3310 admissions entered the CCCTN Registry. Although most CICU admissions were for acute primary cardiovascular problems (2557 [77.3%]), 253 (7.7%) were for mixed general and cardiovascular problems, 163 (4.9%) of admissions were for overflow from general medical ICUs, and the remainder were for periprocedural care (Figure 1). The primary analysis population comprised 3049 patients. Of this cohort, 1427 patients (46.9%) presented to the emergency department of participating sites and were directly admitted to the CICU, 1112 (36.5%) were directly transferred to the CICU from another hospital, and the remainder were transferred from other inpatient units.
Figure 1. Category of Primary Reason for Admission to the Cardiac Intensive Care Unit (CICU) in the Overall Cohort.
Analysis includes all CICU admissions for 2 months. CV indicates cardiovascular; ICU, intensive care unit.
The baseline characteristics of the primary analysis cohort are reported in the Table. The median age was 65 years (25th and 75th percentiles, 55 and 75 years, respectively). More than a third of the patients (1177 [38.6%]) admitted to the CICU were 70 years or older and 438 (14.4%) were at least age 80 years. Women composed 37.1% of the population. Patients admitted to the CICU commonly had significant chronic cardiac and noncardiac comorbid conditions. The most common chronic cardiac conditions included ischemic heart disease (1267 [41.6%]), and heart failure (1103 [36.2%]), of which most was due to reduced ejection fraction. Noncardiac comorbidities included diabetes (1062 [34.8%]), chronic kidney disease (736 [24.1%]), chronic pulmonary disease (432 [14.2%]), and active malignancy (202 [6.6%]). Overall, the global severity of illness as assessed by SOFA score was low, with a median SOFA score of 3 (25th and 75th percentiles, 1 and 6, respectively) with substantial variation across CICUs (median SOFA range by site, 2-5).
Table. Baseline Characteristicsa.
| Characteristic | Primary Analysis Population (N = 3049) |
|---|---|
| Demographics | |
| Age, years (median [25th, 75th]) | 65 (55, 75) |
| Female | 1132 (37.1) |
| Individuals of color, No. (%) | 797 (31.4) |
| BMIb (median [25th, 75th]) | 28.0 (24.1, 32.9) |
| General Medical Problems and Risk Factors | |
| Smoking status | |
| Current | 572 (19.0) |
| Ex-smoker | 1106 (36.7) |
| Unknown | 254 (8.4) |
| Hypertension | 1997 (65.5) |
| Diabetes | 1062 (34.8) |
| Chronic kidney disease | 736 (24.1) |
| Dialysis-dependent (% of total) | 170 (5.6) |
| Significant pulmonary disease | 432 (14.2) |
| Significant liver disease | 97 (3.2) |
| Significant dementia | 55 (1.8) |
| Active cancer | 202 (6.6) |
| Cardiovascular History | |
| Coronary artery disease | 1267 (41.6) |
| Cerebrovascular disease | 300 (9.8) |
| Peripheral artery disease | 288 (9.4) |
| Heart failure | 1103 (36.2) |
| HFrEF (EF, <40%) (% of total) | 677 (22.2) |
| Heart transplant | 45 (1.5) |
| Atrial fibrillation | 712 (23.4) |
| Ventricular arrhythmia | 183 (6.0) |
| Severe valvular disease | 427 (14.0) |
| Pulmonary hypertension | 125 (4.1) |
| Congenital heart disease | 57 (1.9) |
Abbreviations: BMI, body mass index; EF, ejection fraction; HFrEF, heart failure with reduced ejection fraction.
All data are reported as number (percentage) unless otherwise specified. Past noncardiovascular medical conditions were captured as “significant” based on the clinical judgment of the local investigators.
Calculated as weight in kilograms divided by height in meters squared.
Admission Diagnoses and ICU Indications
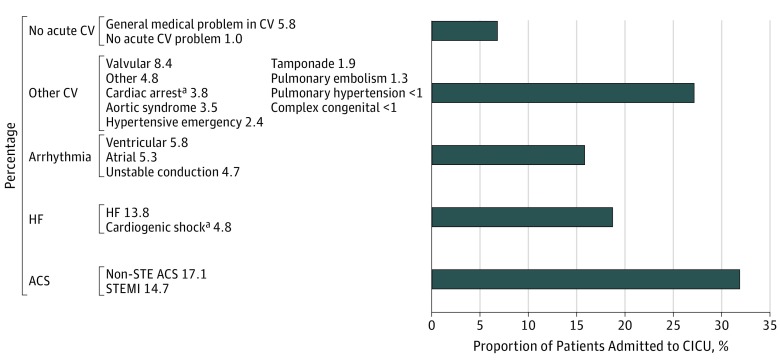
The primary cardiac problems leading to CICU admission were diverse (Figure 2). Among primary acute cardiac problems, the 2 most common primary reasons for cardiac CICU admission were acute coronary syndrome (ACS) (969 [31.8%]) and heart failure (567 [18.6%]). Only 448 ACS admisions (46.3%) were for ST-segment elevation MI, accounting for only 14.7% of all CICU admissions. Only 420 admissions (44.3% of all ACS admissions) had an ICU indication other than a perceived need for monitoring. Moreover, the proportion of CICU admissions that were for ACS was highly variable across centers (15%-57%; eFigure 1 in the Supplement). When secondary diagnoses of unstable angina or MI, inclusive of type 2 MI, were included, the proportion of admissions that involved unstable coronary ischemic syndromes increased to 35.3%. Similarly, the proportion of admissions that included heart failure more than doubled to 41.3% when secondary diagnoses were included.
Figure 2. Primary Reason for Admission to the Cardiac Intensive Care Unit (CICU).
Analysis includes CICU admissions (N = 3049) from the primary analysis cohort, which excludes general medical intensive care unit overflow and admissions solely for postoperative management after cardiac surgery. Cardiogenic shock and cardiac arrest denote cases in which the etiology is not already captured by a primary causea (eg, acute coronary syndrome [ACS] leading to cardiogenic shock is captured as ACS and ventricular arrhythmia causing cardiac arrest is captured as VT/VF). CV indicates cardiovascular; HF, heart failure; STEMI, ST-elevation myocardial infarction.
An assessment of CICU use by primary cardiac diagnosis according to the proportion of total CICU patient-days (13 923 days) was also conducted (eFigure 2 in the Supplement). The proportion of CICU days allocated for patients with a primary diagnosis of ACS was 23.6%, reflecting a relatively short duration of CICU stay despite contributing to a higher proportion of admissions. In contrast, heart failure (including cardiogenic shock) as a primary diagnosis represented 567 admissions (18.6%) but accounted for 32.9% of the total CICU patient-days.
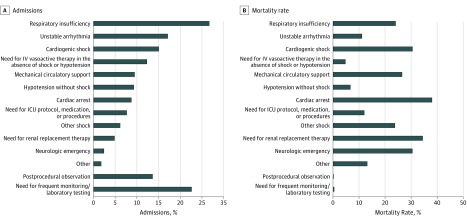
The indications for ICU-level care are presented in Figure 3A. The 2 leading indications were respiratory insufficiency (814 [26.7%]) and shock (643 [21.1%]), with mixed and noncardiogenic shock accounting for nearly a third of these cases. Cardiac arrest was reported as an indication for 265 CICU admissions (8.7%). Notably, 689 patients (22.6%) admitted to participating CICUs were triaged to be admitted to the CICU solely for the perceived need for monitoring, ICU-level nursing care, or frequent laboratory testing, and an additional 414 patients (13.6%) were transferred to the CICU for postprocedural monitoring in the absence of any other ICU indication. The median SOFA score for these patients was 2 (range, 1-3), compared with 5 (range, 2-8) in patients with an ICU indication beyond monitoring.
Figure 3. Frequency of Indication for Cardiac Intensive Care Unit (CICU) Admission and CICU Mortality by ICU Indications.
A, Represents percentage of admissions according to intensive care unit (ICU) indication. B, The CICU mortality rate represents the proportion of patients with the relevant indication who died while in the CICU. For both panels, the only mutually exclusive categories for indication were postprocedural observation and the need for frequent monitoring or laboratory testing (N = 3049). IV indicates intravenous.
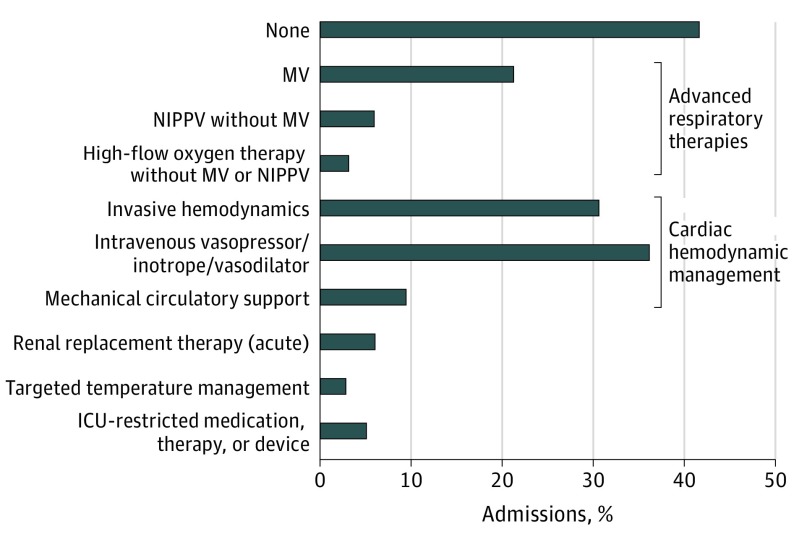
ICU Therapies
The proportion of patients treated with common advanced ICU-based monitoring or therapies is shown in Figure 4. Cardiac ICU care included an intravenous vasopressor, inotrope, or vasodilator for 1105 (36.2%) and advanced therapies 933 (30.6%), including invasive mechanical ventilation for 652 (21.4% with a range from 5.4% to 37.3% across CICUs). Mechanical circulatory support ranging from intra-aortic balloon pump (Impella, version CP/RP/5.0; Abiomed), right and left tandem heart peripheral ventricular assist devices, and extracorporeal membrane oxygenation was used in 289 patients (9.5%) in the overall population, including 207 patients with shock (30.7% of shock cases). While central venous access and arterial pressure monitoring were common, pulmonary artery catheters were used for 334 patients (11.0%), with high variability across sites (0.5%-33.5%). The proportion of patients treated without advanced ICU therapies or invasive monitoring was 41.8% overall and varied substantially between centers (interhospital range, 14%-62%; eFigure 3 in the Supplement).
Figure 4. Acute Intensive Care Therapies and Monitoring.
Invasive hemodynamics refers to central venous or arterial monitoring, with pulmonary artery (PA) catheters (11%) representing a subset of central venous cannulation. ICU indicates intensive care unit; MV, mechanical ventilation; NIPPV, noninvasive positive pressure ventilation.
CICU and Hospital Outcomes
The median length of ICU stay was 2.2 days (25th and 75th percentiles, 1.1 and 4.5, respectively) in the primary analysis population, 2.1 days (1.1-4.2) in survivors, and 3.5 (1.3-9.3) among those who died in the CICU. The median duration of CICU stay for patients not requiring advanced ICU therapies or invasive monitoring was 1.5 (25th and 75th percentile, 0.9 and 2.7, respectively) days, contrasting with 3.0 (25th and 75th percentile, 1.5 and 6.0, respectively) days among patients who required advanced ICU therapies/invasive monitoring.
The overall CICU mortality rate was 8.3% (95% CI, 7.3%-9.3%), with substantial variation by site (range, 4.0%-19.7%), primary diagnosis (eFigure 4 in the Supplement), and CICU indication (Figure 3B). Stratified by primary admission diagnosis, the highest mortality rate was in patients with cardiac arrest at 45.3%. In addition to cardiac arrest, the indications for CICU-level care that carried the highest mortality rates were shock (cardiogenic, 30.6%; other, 23.8%), the need for renal replacement therapy (34.5%), neurologic emergencies (30.6%), respiratory failure (24.1%), or use of mechanical circulatory support (26.6%; Figure 3B). Patients triaged to be admitted to the CICU solely for postprocedural observation or frequent laboratory testing or monitoring (more than one-third of patients) had very low rates of CICU mortality at 0.2% to 0.4%.
Among those who survived after being transferred out of the CICU (2056), 1572 (76.5%) were ultimately discharged home (51.6% of the overall of CICU admissions) and 360 (17.5%) were ultimately transferred to a rehabilitation hospital or extended care facility. Only 80 patients (2.6% of overall CICU admissions) died before hospital discharge after transferring out of the CICU, and 41 (1.3%) were referred to hospice care (eFigure 5 in the Supplement). As such, the overall in-hospital mortality rate was 10.9%.
Discussion
In this large, multicenter, prospective study of a well-characterized cohort of consecutive admissions to advanced CICUs, the primary reasons for triage to the CICU were broad and heterogeneous across centers, as were the advanced CICU therapies used in treatment. Despite the emergence of respiratory failure and shock as prevalent and high-risk indications for CICU care, a sizable cohort of patients was admitted to CICUs only for close monitoring. Our findings provide new evidence in 3 areas that affect the evolution of cardiac critical care: (1) the shift in CICU demographics toward a greater diversity of clinical conditions, (2) the potential for further refinement of triage to the CICU in light of favorable outcomes among a substantial subcohort of patients admitted for observation or monitoring, and (3) the complexity of advanced CICU care required for most patients admitted to contemporary CICUs.
Shifting CICU Demographics
Our findings add to the growing body of evidence that characterizes an ongoing shift in the patient demographics and clinical entities treated in the CICU toward a broader array of cardiovascular conditions with a significant overlay of noncardiac organ dysfunction. Overall, the proportion of patients with a primary diagnosis of ACS in the CCCTN Registry was approximately 32%; remarkably, fewer than half of these patients had an ST-elevation MI and 539 (60%) were admitted for routine care post-MI in the absence of cardiac arrest, respiratory insufficiency, or shock. Concurrent with a decline in the proportion of admissions for ACS compared with historical patterns,2,12 the burden of heart failure on CICU resources has increased. Despite ranking less than ACS in its contribution to the number of admissions, heart failure, including cardiogenic shock, represented a disproportionate amount of total CICU time at 33% of ICU patient-days. Moreover, 1259 patients (41.3%) had heart failure as a part of their presenting syndrome when considering the primary and secondary diagnoses. This prominence is consistent with the increasing prevalence of heart failure in the US population.13 However, the most striking finding regarding the distribution of primary diagnoses is its heterogeneity. More than half of CICU admissions were neither for ACS nor heart failure, an observation that reinforces the importance of a broad base of knowledge and skills in general cardiovascular medicine and critical care medicine for the clinicians leading care in this environment.1,8,14
CICU Resource Use
Although the proportion of CICU admissions for ACS, particularly for ST-elevation MI, has declined, most patients with ACS admitted to CICUs were triaged to receive ICU-level care solely for monitoring. In light of the low mortality rate in this cohort, it is possible that triage to a lower level of care may be appropriate, reinforcing findings from other observational studies that suggest an additional opportunity for improved CICU admission-triage criteria for these patients.15 Moreover, considering the spectrum of patients in this multicenter collaborative, we found that more than one-third of all patients were admitted for postprocedural observation or postprocedural monitoring and approximately 1273 (40%) ultimately required no specific advanced ICU therapy or invasive monitoring. Notably, these patients had a very low CICU mortality rate of 0.2% to 0.4%. These findings, along with the variability between centers (eFigure 4 in the Supplement), suggest a potential for more alignment of hospital resources with patient care needs and patient safety, which includes avoiding the risks of being in a CICU environment.
However, while the observation of a very low mortality risk in a significant subcohort of patients suggests that they may be cared for in lower-intensity settings, it is possible that the favorable outcomes were achieved as a result of CICU care, including nursing staffing ratios and expertise, and would not be reproducible if triaged to other environments. We regard this aspect of our findings as providing a starting point for additional research and that a conclusion of an “overuse” of CICUs is premature. Controlled prospective studies of alternative triage strategies may be warranted.
Advanced Care in the CICU
In contrast to this lower-risk subcohort, the remaining roughly two-thirds of patients admitted to the CICU with indications other than the perceived need for monitoring were complex, with extracardiac organ dysfunction or shock, frequent use of advance CICU therapies, and poor short-term outcomes. Respiratory insufficiency was the most common CICU indication, with 814 predominantly cardiovascular patients (27%) requiring positive pressure ventilation. Indications associated with a greater need for advanced CICU therapies also were associated with high CICU mortality rates. For example, the mortality rate exceeded 20% in patients with cardiac arrest (101 [38%]), cardiogenic shock (140 [31%]), respiratory failure (196 [24%]), and renal replacement therapy (51 [35%]).
These data underscore the merit of proposals for advanced training and skills in those principally responsible for patients admitted to CICUs. While leadership of the CICU was guided historically by research interests and expertise in acute reperfusion therapy, based on observations from the CCCTN registry, the current training of practitioners with a career focus on cardiac critical care should include expertise in acute heart failure management, management of mechanical support, post–cardiac arrest care, electrical storm, and the ability to integrate significant noninvasive cardiovascular imaging data into acute clinical decision-making. These core cardiology skills ought be further complemented with expertise in managing acute respiratory failure16 and renal replacement therapy as well as preventive measures for patient safety, such as avoiding ventilator-associated pneumonia and central line-associated bloodstream infections, and the management of delirium. Two studies surveying the organization and staffing of CICUs in the United States have documented low rates of staffing in CICUs by cardiologists with critical care skills. In the first of these studies, fewer than half of CICUs had routine involvement of a physician with critical care skills.17 In the second, conducted among 612 centers from the American Heart Association Mission: Lifeline and American College of Cardiology ACTION Registry Get With the Guidelines hospitals,18 only 14.7% had dual-boarded critical care cardiologists practicing in the CICU.
However, the variability between centers also highlights that one size does not fit all and that there is likely not a CICU triage or staffing model that is appropriate for every hospital and CICU. Rather, it may be advisable for individual institutions to critically evaluate their current CICU patient population, demographics, and outcomes to identify potential areas for increased efficiency and the optimization of triage, as well as to determine ideal staffing models.
Future Research in Cardiac Critical Care
Our report adds to previous studies demonstrating the evolving landscape of cardiac critical care2,3,4,5,6 and is responsive to calls for additional research to fill important gaps in the evidence base.1,7,8,9,10 To our knowledge, this report represents the first effort of a multicenter collaborative of advanced CICUs with the goal to design and execute observational studies and clinical trials that will advance cardiac critical care. These data from the CCCTN Registry add to the existing body of evidence through an acquisition of patient-level data across multiple institutions, with each patient individually reviewed by a clinical team to ensure the high-fidelity capture of diagnoses, resource use, and outcomes. We found that even across centers that are generally similar in their CICU structure, academic affiliation, and capabilities, there was significant variability in their patient populations and the therapies that were used. These observations highlight the advantage of the multicenter perspective in the collection of observational data and the testing of specific interventions in the CICU. The registry also demonstrates the power of such a collaboration, with more than 3000 admissions in 2 months, and the potential to accrue substantial numbers with shock, cardiac arrest, and multisystem organ dysfunction to enroll in clinical trials of new approaches to treating patients with these conditions.
Limitations
We did not specifically capture symptoms, such as persistent chest pain, as unique indications for CICU admission. The in-hospital mortality rate in the registry was 10.9%. However, the in-hospital mortality rate predicted by the median SOFA score was lower (range, 1%-5%)11,19 than observed. It is possible that the SOFA score was underestimated in this population or that while associated with outcome, SOFA is poorly calibrated for a contemporary CICU population.
Conclusions
In a network of academic, tertiary CICUs, respiratory failure and shock are currently the predominant indications for CICU admission, with patients with heart failure with an increased need for resources in the CICU. Patterns of practice varied substantially across centers and revealed potential areas for quality improvement. Multicenter collaborative networks, such as the CCCTN, could be used to inform the redesign of cardiac critical care and launch pragmatic registry-based randomized clinical trials to test new strategies and devices.
eMethods.
eTable. CCCTN Vanguard Enrolling Site Characteristics
eFigure 1. Variability in the proportion of admissions due to acute coronary syndromes
eFigure 2. Proportion of Total ICU Days by Primary Admission Diagnosis
eFigure 3. Proportion of admissions managed in the CICU without any advanced ICU therapies or invasive monitoring
eFigure 4. CICU Mortality Rate by Primary Admission Diagnosis
eFigure 5. CICU and hospital disposition
References
- 1.Morrow DA, Fang JC, Fintel DJ, et al. ; American Heart Association Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation, Council on Clinical Cardiology, Council on Cardiovascular Nursing, and Council on Quality of Care and Outcomes Research . Evolution of critical care cardiology: transformation of the cardiovascular intensive care unit and the emerging need for new medical staffing and training models: a scientific statement from the American Heart Association. Circulation. 2012;126(11):1408-1428. doi: 10.1161/CIR.0b013e31826890b0 [DOI] [PubMed] [Google Scholar]
- 2.Katz JN, Shah BR, Volz EM, et al. . Evolution of the coronary care unit: clinical characteristics and temporal trends in healthcare delivery and outcomes. Crit Care Med. 2010;38(2):375-381. doi: 10.1097/CCM.0b013e3181cb0a63 [DOI] [PubMed] [Google Scholar]
- 3.Ratcliffe JA, Wilson E, Islam S, et al. . Mortality in the coronary care unit. Coron Artery Dis. 2014;25(1):60-65. doi: 10.1097/MCA.0000000000000043 [DOI] [PubMed] [Google Scholar]
- 4.Holland EM, Moss TJ. Acute noncardiovascular illness in the cardiac intensive care unit. J Am Coll Cardiol. 2017;69(16):1999-2007. doi: 10.1016/j.jacc.2017.02.033 [DOI] [PubMed] [Google Scholar]
- 5.Watson RA, Bohula EA, Gilliland TC, Sanchez PA, Berg DD, Morrow DA. Prospective registry of cardiac critical illness in a modern tertiary care cardiac intensive care unit [published online July 1, 2018]. Eur Heart J Acute Cardiovasc Care. [DOI] [PubMed] [Google Scholar]
- 6.Sinha SS, Sjoding MW, Sukul D, et al. . Changes in primary non-cardiac diagnoses over time among elderly cardiac intensive care unit patients in the United States. Circ Cardiovasc Qual Outcomes. 2017;10(8):e003616. doi: 10.1161/CIRCOUTCOMES.117.003616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wong GC, van Diepen S, Ainsworth C, et al. ; CCS Post Cardiac Arrest Guidelines Committee . Canadian Cardiovascular Society/Canadian Cardiovascular Critical Care Society/Canadian Association of Interventional Cardiology position Statement on the optimal care of the postarrest patient. Can J Cardiol. 2017;33(1):1-16. doi: 10.1016/j.cjca.2016.10.021 [DOI] [PubMed] [Google Scholar]
- 8.Bonnefoy-Cudraz E, Bueno H, Casella G, et al. . Editor’s choice—acute cardiovascular care association position paper on intensive cardiovascular care units: an update on their definition, structure, organisation and function. Eur Heart J Acute Cardiovasc Care. 2018;7(1):80-95. doi: 10.1177/2048872617724269 [DOI] [PubMed] [Google Scholar]
- 9.van Diepen S, Granger CB, Jacka M, Gilchrist IC, Morrow DA, Katz JN. The unmet need for addressing cardiac issues in intensive care research. Crit Care Med. 2015;43(1):128-134. doi: 10.1097/CCM.0000000000000609 [DOI] [PubMed] [Google Scholar]
- 10.Katz JN, Minder M, Olenchock B, et al. . The genesis, maturation, and future of critical care cardiology. J Am Coll Cardiol. 2016;68(1):67-79. doi: 10.1016/j.jacc.2016.04.036 [DOI] [PubMed] [Google Scholar]
- 11.Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286(14):1754-1758. doi: 10.1001/jama.286.14.1754 [DOI] [PubMed] [Google Scholar]
- 12.Killip T III, Kimball JT. Treatment of myocardial infarction in a coronary care unit: a two year experience with 250 patients. Am J Cardiol. 1967;20(4):457-464. doi: 10.1016/0002-9149(67)90023-9 [DOI] [PubMed] [Google Scholar]
- 13.Benjamin EJ, Virani SS, Callaway CW, et al. ; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e67-e492. doi: 10.1161/CIR.0000000000000558 [DOI] [PubMed] [Google Scholar]
- 14.O’Gara PT, Adams JE III, Drazner MH, et al. . COCATS 4 Task Force 13: training in critical care cardiology. J Am Coll Cardiol. 2015;65(17):1877-1886. doi: 10.1016/j.jacc.2015.03.027 [DOI] [PubMed] [Google Scholar]
- 15.van Diepen S, Tran DT, Ezekowitz JA, et al. . The high cost of critical care unit over-utilization for patients with NSTE ACS. Am Heart J. 2018;202:84-88. doi: 10.1016/j.ahj.2018.05.003 [DOI] [PubMed] [Google Scholar]
- 16.Alviar CL, Miller PE, McAreavey D, et al. ; ACC Critical Care Cardiology Working Group . Positive pressure ventilation in the cardiac intensive care unit. J Am Coll Cardiol. 2018;72(13):1532-1553. doi: 10.1016/j.jacc.2018.06.074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O’Malley RG, Olenchock B, Bohula-May E, et al. . Organization and staffing practices in US cardiac intensive care units: a survey on behalf of the American Heart Association Writing Group on the Evolution of Critical Care Cardiology. Eur Heart J Acute Cardiovasc Care. 2013;2(1):3-8. doi: 10.1177/2048872612472063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van Diepen S, Fordyce CB, Wegermann ZK, et al. . Organizational structure, staffing, resources, and educational initiatives in cardiac intensive care units in the United States: an American Heart Association Acute Cardiac Care Committee and American College of Cardiology Critical care Cardiology Working Group cross sectional survey. Circ Cardiovasc Qual Outcomes. 2017;10(8):e003864. doi: 10.1161/CIRCOUTCOMES.117.003864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vincent JL, de Mendonça A, Cantraine F, et al. . Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998;26(11):1793-1800. doi: 10.1097/00003246-199811000-00016 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods.
eTable. CCCTN Vanguard Enrolling Site Characteristics
eFigure 1. Variability in the proportion of admissions due to acute coronary syndromes
eFigure 2. Proportion of Total ICU Days by Primary Admission Diagnosis
eFigure 3. Proportion of admissions managed in the CICU without any advanced ICU therapies or invasive monitoring
eFigure 4. CICU Mortality Rate by Primary Admission Diagnosis
eFigure 5. CICU and hospital disposition