This crossover randomized clinical trial assesses whether participants completing the American College of Surgeons Bleeding Control Basic training with Combat Application Tourniquets can effectively apply bleeding control principles using other tourniquet types.
Key Points
Question
How effective is the Bleeding Control Basic course at training participants to use commercial tourniquets other than the type taught in the course and to improvise a tourniquet?
Findings
In this crossover randomized clinical trial, 102 participants were evaluated on application of 5 different tourniquets sequentially. Compared with the tourniquet taught in the course, participants were significantly less likely to correctly apply any 1 of the 3 commercial tourniquets or improvise a tourniquet.
Meaning
The Bleeding Control Basic principles for correct Combat Application Tourniquet application are not fully translatable to other commercial or improvised tourniquet types.
Abstract
Importance
More than 500 000 laypeople in the United States have been trained in hemorrhage control, including tourniquet application, under the Stop the Bleed campaign. However, it is unclear whether after hemorrhage control training participants become proficient in a specific type of tourniquet or can also use other tourniquets effectively.
Objective
To assess whether participants completing the American College of Surgeons Bleeding Control Basic (B-Con) training with Combat Application Tourniquets (CATs) can effectively apply bleeding control principles using other tourniquet types (commercial and improvised).
Design, Setting, and Participants
This nonblinded, crossover, sequential randomized clinical trial with internal control assessed a volunteer sample of laypeople who attended a B-Con course at Gillette Stadium and the Longwood Medical Area in Boston, Massachusetts, for correct application of each of 5 different tourniquet types immediately after B-Con training from April 4, 2018, to October 9, 2018. The order of application varied for each participant using randomly generated permutated blocks.
Interventions
Full B-Con course, including cognitive and skill sessions, that taught bleeding care, wound pressure and packing, and CAT application.
Main Outcomes and Measures
Correct tourniquet application (applied pressure of ≥250 mm Hg with a 2-minute time cap) in a simulated scenario for 3 commercial tourniquets (Special Operation Forces Tactical Tourniquet, Stretch-Wrap-and-Tuck Tourniquet, and Rapid Application Tourniquet System) and improvised tourniquet compared with correct CAT application as an internal control using 4 pairwise Bonferroni-corrected comparisons with the McNemar test.
Results
A total of 102 participants (50 [49.0%] male; median [interquartile range] age, 37.5 [27.0-53.0] years) were included in the study. Participants correctly applied the CAT at a significantly higher rate (92.2%) than all other commercial tourniquet types (Special Operation Forces Tactical Tourniquet, 68.6%; Stretch-Wrap-and-Tuck Tourniquet, 11.8%; Rapid Application Tourniquet System, 11.8%) and the improvised tourniquet (32.4%) (P < .001 for each pairwise comparison). When comparing tourniquets applied correctly, all tourniquet types had higher estimated blood loss, had longer application time, and applied less pressure than the CAT.
Conclusions and Relevance
The B-Con principles for correct CAT application are not fully translatable to other commercial or improvised tourniquet types. This study demonstrates a disconnect between the B-Con course and tourniquet designs available for bystander first aid, potentially stemming from the lack of consensus guidelines. These results suggest that current B-Con trainees may not be prepared to care for bleeding patients as tourniquet design evolves.
Trial Registration
ClinicalTrials.gov identifier: NCT03538379
Introduction
Prehospital bleeding control interventions within the US military have decreased preventable deaths from exsanguinating extremity hemorrhage by 67%, with an estimated 1000 to 2000 lives saved.1,2,3 The Stop the Bleed campaign was introduced to the public in 2015, with a focus on translating these interventions to the civilian sector to support the National Trauma Action Plan to achieve zero preventable deaths after injury. As an element of the Stop the Bleed campaign, the American College of Surgeons’ Bleeding Control Basic (B-Con) course was implemented. B-Con is the most widely adopted standardized course for civilians, with 525 000 graduates to date.4,5
Many different types of tourniquets are commercially available, and there is little consensus regarding specific tourniquet design for civilian use.6,7 Therefore, as hemorrhage control readiness training and public placement of hemorrhage control kits are implemented in the civilian arena, various types of tourniquets are being placed in these bleeding control kits, ranging from windlass-based to elastic-based products (Figure 1).8,9,10 The Combat Application Tourniquet (CAT), a windlass-based tourniquet, was initially chosen by the military after simulation and real-world testing demonstrated its efficacy at stopping bleeding.11,12,13 Citing this evidence, B-Con in its current form teaches the application of the CAT for extremity hemorrhage control.7,14 The B-Con course informs participants that other commercial tourniquets exist, with the presumption that the course teaches the underlying principle of tourniquet application and course participants will be able to apply other tourniquet types in an emergency.5,6,14 In addition, the Hartford consensus states that when a commercial tourniquet is not available, an improvised tourniquet can be fashioned and applied, whereas the B-Con course does not specifically address the issue.6,7 However, it is unknown whether teaching CAT application sufficiently trains laypeople in the use of other commonly available tourniquets or an improvised tourniquet to effectively control hemorrhage. It is important to determine whether the current teaching standards are resilient to future variations in tourniquet design.
Figure 1. Types of Commercial Tourniquets Assessed.
The Combat Application Tourniquet (A) and Special Operations Forces Tactical Tourniquet (B) are windlass tourniquets, whereas the Stretch-Wrap-and-Tuck Tourniquet (C) and Rapid Application Tourniquet System (D) are elastic tourniquets. The Stretch-Wrap-and-Tuck Tourniquet comes with instructions for application printed on the tourniquet.
In this context, we evaluated laypeople immediately after completing the standard B-Con course on their ability to correctly apply each of 4 different commercially available tourniquets and to devise an improvised tourniquet. The primary outcome was correct application of each tourniquet type compared with the CAT. Secondary outcomes included the pressure applied by the tourniquet, time to tourniquet application, estimated blood loss (EBL) if the tourniquet was applied correctly, and understanding of how to apply the tourniquet.
Methods
Study Design
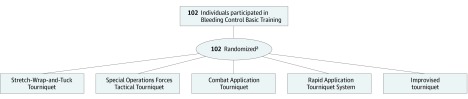
This was a nonblinded, crossover, sequential, intention-to-treat randomized clinical trial with internal control that involved application by all participants of each of 5 different tourniquet types in a randomized sequence; the study can be considered an extension of a crossover study (Figure 2). The trial protocol can be found in Supplement 1. The study followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline.15 Partners Institutional Review Board approved the study. Verbal consent was obtained from all participants before enrollment. All data were deidentified.
Figure 2. CONSORT Flow Diagram.
aParticipants applied each of the 5 tourniquets in a randomized sequence.
Participants
Participants included adults without formal medical training who completed B-Con training in the Longwood Medical Area or at Gillette Stadium in Boston, Massachusetts, from April 4, 2018, to October 9, 2018. All B-Con trainees older than 18 years were eligible for inclusion with no prespecified exclusion criteria. Participants were recruited immediately before the beginning of the course that they attended after being provided an overview of the study by the lead investigator (J.C.M.). Participation in the study was not a requirement of taking the B-Con course. Participants completed questionnaires after consenting to participate and before B-Con training to obtain demographic information, including age, sex, educational level, and self-report of prior first-aid training with or without prior hemorrhage control training. In addition, these questionnaires queried participants on domains related to resilience-associated traits and perceived actions that the participant would take if presented with a bleeding person. The present study focuses on the primary aim; therefore, the remaining questionnaire results will be presented in the future. Those with prior training were not excluded from the study because all participants were formally trained in hemorrhage control just before testing; thus, minimal differences between the previously trained and untrained groups were hypothesized a priori.
Interventions
All participants completed B-Con, which includes a didactic and hands-on component. The didactic component outlines initial actions to take when approaching a bleeding person, when and how to pack and apply pressure to a wound, and when and how to apply a CAT. Although B-Con guidelines allow for other windlass-based tourniquets to be substituted into the training at the discretion of the instructor, the CAT application is depicted in the B-Con PowerPoint (Microsoft) and was used in all training sessions for this study.6,14
After completing B-Con, participants were individually assessed by study investigators (J.C.M., Z.G.H., J.P.H.-E., E.d.J., M.A.C., and E.G.), all of whom were trained B-Con instructors, in a separate room on their ability to correctly apply each of 4 common commercial tourniquets (CAT, Special Operation Forces Tactical Tourniquet [SOFT-T], Stretch-Wrap-and-Tuck Tourniquet [SWAT-T], and Rapid Application Tourniquet System [RATS]) and improvise a tourniquet (Figure 2). The CAT and SOFT-T are both windlass-based tourniquets, whereas the SWAT-T and RATS are elastic-based tourniquets. These tourniquets are described in further detail in the eMethods in Supplement 2). For the improvised tourniquet, participants were given an assortment of materials, including a 6-ft length of gauze, a shoestring, a leather belt, and a 12-in polyvinyl chloride plastic or heavy wooden rod. Participants were blinded to what tourniquets they would be applying other than the CAT until the moment of each test.
Each participant applied all 5 tourniquets to a HapMed trainer, a high-fidelity mannequin that simulates a traumatic lower-extremity amputation with ongoing hemorrhage. The HapMed measures the pressure applied by the tourniquet in millimeters of mercury and calculates an EBL. In addition, it provides real-time feedback when bleeding is ongoing using red lights on the end of the leg, which decrease in intensity as bleeding slows and are completely off once bleeding stops (ie, when sufficient pressure is applied). Participants were told that the lights represent ongoing blood loss, but no other feedback was given to participants during the tourniquet testing phase. For the improvised tourniquet, participants were told that they could use any of or all the available components. The order of application varied for each participant using randomly generated permutated blocks. There was less than a minute washout time between application of different tourniquet types.
Outcomes
Primary Outcome
Correct tourniquet application was defined a priori as (1) adequate pressure from the tourniquet (>250 mm Hg), (2) correct anatomical placement (minimum of 2 inches proximal to the wound), and (3) time to application less than 2 minutes. Participants were given 2 minutes to apply each tourniquet based on the results of the Public Access and Tourniquet Training Study trial, which showed that the 90th percentile time for correct application was 117 seconds.16 Participants could also inform the instructor of completion any time before the 2 minutes, and the timer would be stopped regardless of whether the tourniquet was correctly applied. The same criteria for correct application was used for all tourniquet types.
Secondary Outcomes
Secondary outcomes included the mean pressure applied by each tourniquet, the time to tourniquet application for those tourniquets applied in less than 2 minutes, EBL, and understanding of how to apply the tourniquet. During the testing phase, the instructor assessed whether the participant understood the mechanism for correct application of each of the different tourniquets using a general set of criteria specific to each tourniquet type (eMethods in Supplement 2).
Statistical Analysis
For the primary outcome of correct tourniquet application, 4 pairwise comparisons of each tourniquet type with the CAT as the internal control were performed using the McNemar test to account for the within-participant correlation of application of different tourniquet types from the same participant. For the secondary outcomes, the normality of the data was assessed, and appropriate univariate paired statistical measures were used to compare the pressure applied, EBL if applied correctly, and time to tourniquet application. Multiple logistic regression was a priori planned to assess whether age, sex, educational level, prior training, and order of test in the randomization sequence correlated with correct tourniquet application for the different devices. However, there were few outcomes to power the models for multiple tourniquet types, resulting in models with wide CIs that may result in inappropriate inferences (eTable 1 in Supplement 2).
Sample size was calculated based on the primary outcome of correct tourniquet application with 80% power and Bonferroni correction for 4 pairwise McNemar test comparisons setting the 2-sided α at .0125 and with a hypothesized correlation of 0.1 between repeated measures for the same participant. The smallest hypothesized difference for which the study was initially powered to detect was between the CAT and SOFT-T, with hypothesized correct application rates of 80% for CAT and 40% for SOFT-T, yielding a sample size of 34 people. Additional individuals were recruited to power the secondary outcome assessing demographic indicators of correct application using logistic regression. Stata statistical software, version 15.1 (StataCorp) was used for all statistical calculations.
Results
Participants
A total of 102 people (50 [49.0%] male; median [interquartile range] age, 37.5 [27.0-53.0] years) participated in the study (Table 1). There were no losses or exclusions from the study. Participants in the sample had higher educational levels than national figures, with 67 (65.7%) having a bachelor or more-advanced degree. Thirty-five (34.3%) self-reported prior first-aid training, and 25 (24.5%) reported prior first-aid plus hemorrhage-control training. The median time since prior hemorrhage-control training was 6.5 years (interquartile range, 2.0-20.0 years). Nineteen participants (18.6%) reported having prior training in how to use a tourniquet.
Table 1. Participant Demographic Characteristics.
| Characteristic | Findinga |
|---|---|
| Age, median (IQR), y | 37.5 (27.0-53.0) |
| Male sex | 50 (49.0) |
| Educational level | |
| High school or some college | 35 (34.3) |
| Bachelor or more advanced degree | 67 (65.7) |
| Prior first aid training onlyb | 35 (34.3) |
| Prior first aid and hemorrhage control trainingb | 25 (24.5) |
| No. of years since completing hemorrhage-control training, median (IQR) | 6.5 (2.0-20.0) |
| Prior experience with tourniquets | 19 (18.6) |
Abbreviation: IQR, interquartile range.
Data are presented as number (percentage) of participants unless otherwise indicated.
One missing data point in first aid.
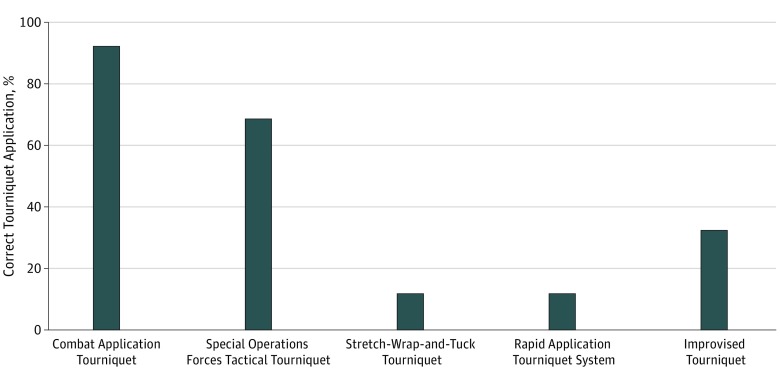
Comparison of Tourniquet Application Rates
The CAT was correctly applied at a significantly higher rate (94 [92.2%]; 95% CI, 85.1%-96.6%) than all other tourniquet types (P < .001 for each pairwise comparison) (Figure 3). The windlass-based SOFT-T had the second highest rate of correct application (70 [68.6%]; 95% CI, 58.7%-77.5%) followed by the improvised tourniquet (33 [32.4%]; 95% CI, 23.4%-42.3%), the SWAT-T (12 [11.8%]; 95% CI, 6.2%-19.6%), and the RATS (12 [11.8%]; 95% CI, 6.2%-19.6%). All incorrect applications were attributable to inadequate pressure applied by the tourniquet at the time when the participants stated that they were finished or at the conclusion of 2 minutes. No tourniquets were placed at the incorrect anatomical position. Participants ran out of time to apply the tourniquet 4 times for the SOFT-T, 20 times for the SWAT, 29 times for the RATS, and 59 times for the improvised tourniquet. No participant ran out of time while applying the CAT.
Figure 3. Proportions of Correct Tourniquet Application for Different Tourniquet Types.
For fashioning an improvised tourniquet, participants used 1 or more of the following available materials: leather belt, 37 (36.3%); gauze, 49 (48.0%); shoelace, 60 (58.8%); and a windlass, 80 (78.4%). During the first session of 10 participants, a 12-in-long heavy-duty polyvinyl chloride pipe was available as the windlass. This device broke in 7 instances secondary to the torque applied when used as a windlass (eFigure in Supplement 2). In all subsequent sessions, a 12-in heavy wooden rod was used. A windlass was used with the belt in 24 cases, and in 11 (45.8%) of these cases, the tension from the windlass caused the belt to break at the buckle or the strap (eFigure in Supplement 2). Among the 22 participants who did not use a windlass, 1 (4.6%) was able to correctly apply an improvised tourniquet.
Secondary Outcomes Relating to Tourniquet Type
The CAT exerted the most pressure of all tourniquet types (mean [SD], 390.0 [108.1] mm Hg) followed by the SOFT-T (mean [SD], 309.6 [158.2] mm Hg), improvised tourniquet (mean [SD], 160.9 [166.8] mm Hg), SWAT-T (mean [SD], 109.7 [130.1] mm Hg), and RATS (mean [SD], 92.4 [113.9] mm Hg) (Table 2). When the tourniquet was applied in less than 2 minutes, the CAT was applied faster than any other tourniquet, with the greatest mean difference present between the CAT and the improvised tourniquet (mean [SD] difference, 42.0 [25.6] seconds). When the tourniquet was applied correctly CAT was associated with a significantly lower mean (SD) EBL (232.3 [92.5] mL) compared with all other tourniquet types (SOFT-T: 287.1 [142.1] mL; SWAT: 311.4 [182.6] mL; RATS: 363.3 [170.2] mL; and improvised tourniquet: 552.9 [204.6] mL; P < .001 for each pairwise comparison).
Table 2. Comparison Between CAT and Other Tourniquet Types for Pressure Applied, Time to Application, Estimated Blood Loss, and Understanding of Mechanism.
| Tourniquet Type | Pressure, mean (SD), mm Hg | P Value | Time, mean (SD), sa | P Value | Estimated Blood Loss, mean (SD),b | P Value | Understood Mechanism, No. (%) | P Value |
|---|---|---|---|---|---|---|---|---|
| CAT | 390.0 (108.1) | NA | 36.3 (15.4) | NA | 232.3 (92.5) | NA | 99 (97.1) | NA |
| SOFT-T | 309.6 (158.2) | <.001 | 49.9 (24.3) | <.001 | 287.1 (142.1) | <.001 | 91 (89.9) | .04 |
| SWAT-T | 109.7 (130.1) | <.001 | 68.6 (28.8) | <.001 | 311.4 (182.6) | <.001 | 56 (54.9) | <.001 |
| RATS | 92.4 (113.9) | <.001 | 67.6 (28.0) | <.001 | 363.3 (170.2) | <.001 | 46 (45.1) | <.001 |
| Improvised | 160.9 (166.8) | <.001 | 77.0 (20.9) | <.001 | 552.9 (204.6) | <.001 | 71 (69.6) | <.001 |
Abbreviations: CAT, Combat Application Tourniquet; NA, not applicable; RATS, Rapid Application Tourniquet System; SOFT-T, Special Operations Forces Tactical Tourniquet, SWAT-T, Stretch-Wrap-and-Tuck tourniquet.
Time presented only for those cases that took less than the 2-minute cutoff.
Estimated blood loss presented only for those cases in which the tourniquet was correctly applied.
A total of 99 participants (97.1%) subjectively understood the mechanism for how to apply the CAT, followed by 91 (89.9%) for the SOFT-T, 56 (54.9%) for the SWAT-T, 46 (45.1%) for the RATS, and 71 (69.6%) for the improvised tourniquet (Table 2). As a nonprespecified exploratory analysis, instances in which the participant was judged as demonstrating understanding of the mechanism for application for each tourniquet were assessed. In these cases, 93 (93.4%) correctly applied the CAT, 69 (75.8%) correctly applied the SOFT-T, 10 (17.9%) correctly applied the SWAT, 10 (19.6%) correctly applied the RATS, and 32 (45.1%) correctly fashioned and applied an improvised tourniquet.
Discussion
This study demonstrates that the training principles for bleeding control with CAT application are not fully translatable to other commercial tourniquets or to improvised tourniquets. Specifically, we found significantly lower rates of correct tourniquet application when applying 3 different commercial tourniquets and an improvised tourniquet compared with the CAT. Furthermore, among the tourniquets applied correctly, the CAT applied more pressure, was applied faster, and had a lower EBL than all other tourniquet types.
A prior study16 demonstrated B-Con’s effectiveness at teaching laypeople correct application of the CAT tourniquet; 88% correctly applied the CAT immediately after training with skill degradation by 3 to 9 months, resulting in 55% of individuals correctly applying the CAT. This initial success rate immediately after training is similar to this study’s rate of 92%. The CAT, however, is not the only tourniquet device being deployed for layperson use in bleeding-control kits. Because no studies, to our knowledge, have compared the different devices in the civilian population after training, no definitive guidelines exist for which tourniquets should be made available to civilians.17,18 Large institutions have placed the SWAT-T in their bleeding-control kits with the only associated training being a short video.9,19 This lack of consensus for the type of tourniquet to equip extends to first responders, with examples of some police departments carrying the SWAT-T, whereas others carry the SOFT-T tourniquet.8,20 Furthermore, the inferiority of the application rate for the other tourniquet types would likely be even greater if participants were not tested immediately after training.16
The rate of correct application for the improvised tourniquet of 32% was consistent with prior simulation literature but higher than real-world data.21,22,23,24 This study finding should be viewed in the context that participants were provided the optimum materials for fashioning a tourniquet. When improvised tourniquets were the primary option for US soldiers before 2004, the US Department of Defense recommended that soldiers be provisioned a 6-in rod to act as a windlass to avoid the significant loss of time needed to locate an appropriate windlass and the high break rate of non–purpose-built devices.11 Controlled nonstressed simulation work with trained personnel fashioning improvised tourniquets demonstrated that, without a windlass, 79 of 80 tests (99%) failed to stop bleeding, whereas with a windlass, trained personnel failed to stop arterial flow in 25 of 80 tests (31%).22 Similar simulation work has shown rates of correct improvised tourniquet application of 10% to 40% when applied by trained personnel.24 Kragh et al25 also found that materials potentially used for windlasses in the simulation setting break at a higher rate of 20% to 53%. In the real world, improvised tourniquets have similar high failure rates, with the preeminent example coming from the Boston Marathon bombing during which 27 extremity tourniquets were placed, all improvised and all deemed ineffective on postevent review.21
The study findings have significant implications for the sustainability and implementation goals of the Stop the Bleed campaign. In the short term, consensus recommendations should focus on deploying a singular tourniquet design for which the largest portion of the lay population has been trained (at present, CAT). Potentially training participants in more than 1 type of tourniquet could also be beneficial. Both these strategies, however, represent temporary solutions because it is likely that tourniquet design will change over time. In the long term, tourniquets must evolve from the current designs, which require prior training, and transition to devices that are as intuitive as they are effective. Any proposals that advocate for laypeople to attempt to fashion an improvised tourniquet should be tempered by the study findings and the prior literature that the materials break, especially the windlass and belt, in a significant proportion of cases. This recommendation is further strengthened based on the effectiveness of immediately applying and maintaining pressure to the wound, an action delayed by attempting to find materials to fashion an improvised tourniquet.
Future studies should continue to investigate whether tourniquets manufactured for military use are optimally designed such that a layperson without training could use the device. Bleeding control kits and tourniquet design should follow the example of automated external defibrillators and the process of continuous quality improvement and testing that has resulted in easy-to-use and effective devices for layperson use.26,27 Other studies that would be beneficial to future implementation would be to continue to investigate the number of potential lives saved nationally from immediate responders controlling hemorrhage at the scene.
To support the National Trauma Research Plan’s primary aim of zero preventable trauma deaths, it is essential to identify implementation gaps in prehospital civilian hemorrhage control. Although prior studies7,16 have demonstrated varying efficacy of various educational interventions, different tourniquet types affect curricula effectiveness. Although the CAT was the most successful in this study, when new tourniquets come to market, this study raises the concern that those being trained today will not know how to use new devices. A short-term stop-gap measure would be for future curricula to incorporate various types of tourniquets, whereas a more long-term solution would be identification of universal equipment standards disseminated through a regulatory body and intuitive tourniquet design that does not require prior training.
Limitations
These data must be interpreted within the context of the study design. This study did not test and thus should not be interpreted to mean that these other tourniquet devices, when applied by individuals with device-specific training, are not effective. Participants were tested sequentially on each tourniquet type, which may have resulted in incremental learning. We attempted to mitigate this effect by randomization of the order of application, which allowed the participants to be their own internal controls and removed differences that arise from demographic differences among individuals (eTable 2 in Supplement 2). Testing via simulation rather than in a real-world scenario limits the generalizability to how precisely a layperson would act if presented with a bleeding person. We did, however, use a high-fidelity mannequin that provides real-time feedback to the participant to include active bleeding. There may be selection bias because we tested only volunteers, although we hypothesize that this would likely bias toward the null hypothesis in this study. There may be issues with generalizability of the study to all laypersons nationally, but given that the study population was highly educated, this would likely bias toward the null. Also, the planned logistic regression model to assess the various demographic variables was unstable; thus, individual demographic factors could not validly be assessed.
Conclusions
The B-Con principles for correct CAT application are not fully translatable to other commercial or improvised tourniquet types. This study demonstrates a disconnect between the B-Con course and tourniquet designs available for bystander first aid, potentially stemming from the lack of consensus guidelines. These results suggest that current B-Con trainees may not be prepared to administer bleeding care as tourniquet design evolves.
Trial Protocol
eMethods. Description of Tourniquets
eTable 1. Multiple Logistic Regression Output Assessing Demographic Predictors for Correct Tourniquet Application
eTable 2. Result of Sequence Randomization
eFigure. Pictures of Broken PVC Pipe and Leather Belt
Data Sharing Statement
References
- 1.Kelly JF, Ritenour AE, McLaughlin DF, et al. Injury severity and causes of death from Operation Iraqi Freedom and Operation Enduring Freedom: 2003-2004 versus 2006. J Trauma. 2008;64(2)(suppl):S21-S26. doi: 10.1097/TA.0b013e318160b9fb [DOI] [PubMed] [Google Scholar]
- 2.Eastridge BJ, Mabry RL, Seguin P, et al. Death on the battlefield (2001-2011): implications for the future of combat casualty care. J Trauma Acute Care Surg. 2012;73(6)(suppl 5):S431-S437. doi: 10.1097/TA.0b013e3182755dcc [DOI] [PubMed] [Google Scholar]
- 3.Kragh JF Jr, Walters TJ, Baer DG, et al. Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann Surg. 2009;249(1):1-7. doi: 10.1097/SLA.0b013e31818842ba [DOI] [PubMed] [Google Scholar]
- 4.Jacobs L. Paper presented at: National Academies of Medicine, Department of Defense “Stop the Bleed” National Forum; October 17, 2018; Washington, DC. [Google Scholar]
- 5.BleedingControl.org. About us. http://www.bleedingcontrol.org/about-bc. Accessed July 17, 2017.
- 6.Jacobs LM, McSwain N, Rotondo M, et al. ; Joint Committee to Create a National Policy to Enhance Survivability from Mass Casualty Shooting Events . Improving survival from active shooter events: the Hartford Consensus. Bull Am Coll Surg. 2013;98(6):14-16. [PubMed] [Google Scholar]
- 7.Goolsby C, Jacobs L, Hunt RC, et al. ; Stop the Bleed Education Consortium . Stop the Bleed Education Consortium: education program content and delivery recommendations. J Trauma Acute Care Surg. 2018;84(1):205-210. doi: 10.1097/TA.0000000000001732 [DOI] [PubMed] [Google Scholar]
- 8.Talamo L. First Chance trauma kits save lives on the front lines. Shreveport Times. September 8, 2017. https://www.shreveporttimes.com/story/news/2017/09/08/first-chance-trauma-kits-save-lives-front-lines/633941001/. Accessed January 3, 2018.
- 9.Sidwell RA, Spilman SK, Huntsman RS, Pelaez CA. Efficient hemorrhage control skills training for healthcare employees. J Am Coll Surg. 2018;226(2):160-164. doi: 10.1016/j.jamcollsurg.2017.11.003 [DOI] [PubMed] [Google Scholar]
- 10.Chaudhary MA, McCarty J, Shah S, et al. Building community resilience: a scalable model for hemorrhage-control training at a mass gathering site, using the RE-AIM framework. Surgery. 2018;165(4):795-801. doi: 10.1016/j.surg.2018.10.001 [DOI] [PubMed] [Google Scholar]
- 11.Walters TJ, Mabry RL. Issues related to the use of tourniquets on the battlefield. Mil Med. 2005;170(9):770-775. doi: 10.7205/MILMED.170.9.770 [DOI] [PubMed] [Google Scholar]
- 12.Rasmussen TE, Kellermann AL. Wartime lessons—shaping a national trauma action plan. N Engl J Med. 2016;375(17):1612-1615. doi: 10.1056/NEJMp1607636 [DOI] [PubMed] [Google Scholar]
- 13.Kragh JF Jr, Walters TJ, Baer DG, et al. Practical use of emergency tourniquets to stop bleeding in major limb trauma. J Trauma. 2008;64(2)(suppl):S38-S49. doi: 10.1097/TA.0b013e31816086b1 [DOI] [PubMed] [Google Scholar]
- 14.American College of Surgeons. Bleeding Control (B-Con) Basic. 2017. https://www.jaxsmp.com/wp-content/uploads/2017/02/Bleeding-Control-Basic-Instructor-Presentation-Notes-PPT.pdf. Accessed January 2, 2019.
- 15.Schulz KF, Altman DG, Moher D, Group C; CONSORT Group . CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010;152(11):726-732. doi: 10.7326/0003-4819-152-11-201006010-00232 [DOI] [PubMed] [Google Scholar]
- 16.Goralnick E, Chaudhary MA, McCarty JC, et al. Effectiveness of instructional interventions for hemorrhage control readiness for laypersons in the public access and tourniquet training study (PATTS): a randomized clinical trial. JAMA Surg. 2018;153(9):791-799. doi: 10.1001/jamasurg.2018.1099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ross EM, Mapp JG, Redman TT, Brown DJ, Kharod CU, Wampler DA. The tourniquet gap: a pilot study of the intuitive placement of three tourniquet types by laypersons. J Emerg Med. 2018;54(3):307-314. doi: 10.1016/j.jemermed.2017.09.011 [DOI] [PubMed] [Google Scholar]
- 18.Glick CPTY, Furer MAJA, Glassberg COLE, Sharon R, Ankory MAJR. Comparison of two tourniquets on a mid-thigh model: the Israeli silicone stretch and wrap tourniquet vs. the combat application tourniquet. Mil Med. 2018;183(suppl_1):157-161. doi: 10.1093/milmed/usx169 [DOI] [PubMed] [Google Scholar]
- 19.Hegvik JR, Spilman SK, Olson SD, Gilchrist CA, Sidwell RA Effective hospital-wide education in hemorrhage control. J Am Coll Surg 2017;224(5):796-799, e791. [DOI] [PubMed]
- 20.Police in NYS To Be Equipped With Belt Trauma Kits. January 2, 2019. https://www.wxxinews.org/post/police-nys-be-equipped-belt-trauma-kits. Accessed January 10, 2019.
- 21.King DR, Larentzakis A, Ramly EP, Boston Trauma C; Boston Trauma Collaborative . Tourniquet use at the Boston Marathon bombing: lost in translation. J Trauma Acute Care Surg. 2015;78(3):594-599. doi: 10.1097/TA.0000000000000561 [DOI] [PubMed] [Google Scholar]
- 22.Altamirano MP, Kragh JF Jr, Aden JK III, Dubick MA. Role of the windlass in improvised tourniquet use on a manikin hemorrhage model. J Spec Oper Med. 2015;15(2):42-46. [DOI] [PubMed] [Google Scholar]
- 23.Levy MJ, Goolsby C, Eastman AL. Improvised vs commercial tourniquets. JAMA. 2017;318(6):575. doi: 10.1001/jama.2017.8589 [DOI] [PubMed] [Google Scholar]
- 24.Lyles WE III, Kragh JF Jr, Aden JK III, Dubick MA. Testing tourniquet use in a manikin model: two improvised techniques. J Spec Oper Med. 2015;15(4):21-26. [DOI] [PubMed] [Google Scholar]
- 25.Kragh JF Jr, Wallum TE, Aden JK III, Dubick MA, Baer DG. Which improvised tourniquet windlasses work well and which ones won’t? Wilderness Environ Med. 2015;26(3):401-405. doi: 10.1016/j.wem.2014.12.028 [DOI] [PubMed] [Google Scholar]
- 26.Caffrey SL, Willoughby PJ, Pepe PE, Becker LB. Public use of automated external defibrillators. N Engl J Med. 2002;347(16):1242-1247. doi: 10.1056/NEJMoa020932 [DOI] [PubMed] [Google Scholar]
- 27.Mosesso VN Jr, Shapiro AH, Stein K, Burkett K, Wang H. Effects of AED device features on performance by untrained laypersons. Resuscitation. 2009;80(11):1285-1289. doi: 10.1016/j.resuscitation.2009.07.016 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eMethods. Description of Tourniquets
eTable 1. Multiple Logistic Regression Output Assessing Demographic Predictors for Correct Tourniquet Application
eTable 2. Result of Sequence Randomization
eFigure. Pictures of Broken PVC Pipe and Leather Belt
Data Sharing Statement