Abstract
Objective:
The objective of this study was to examine shared and unique risk factors for incident depression and diabetes mellitus in a national longitudinal population-based survey.
Methods:
Canadian National Population Health Survey (NPHS) longitudinal study was used. A subsample of the initial NPHS sample (n = 4845), free of depression or diabetes mellitus at baseline was tracked over a 10-year period. Univariate and multivariate modified Poisson regression models were used to estimate the relative risk (RR). Stratified analyses by sex were conducted to measure its moderating role. The goodness-of-fit of the various models was tested.
Results:
The cumulative incidence rate of major depressive disorder and incident diabetes mellitus at 10-year follow-up were 4.1% and 10.1% respectively. Hypertension, daily smoking, physical inactivity and being overweight or obese were shared risk factors for major depressive episode and diabetes mellitus. Being female, family stress, traumatic events, having any chronic disease or heart disease were uniquely associated with depression while increasing age and ethnicity (non-white) were unique risk factors for diabetes mellitus. Also, underweight, family stress, chronic disease, and heart disease were risk factors for major depressive disorder in both sexes. Six risk factors, age, ethnicity (non-white), high blood pressure, daily smoking, physical inactivity, and body mass index were associated with incident diabetes mellitus in both sexes.
Conclusion:
We found common risk behaviors/conditions not specific to either diabetes mellitus or depression. These risks have also been implicated in the development of a variety of chronic diseases. These findings underline the importance of public health prevention programs targeting generic risk behaviors.
Keywords: cohort study, diabetes, implications for prevention, major depressive disorder, risk factors, sex differences
Introduction
The relationship between depression and diabetes is of interest to healthcare providers because both conditions contribute significantly to the global burden of disease. Depression is a major public health problem and its prevalence and incidence increasing globally as reported by the Global Burden of Disease Study 2010 and other studies.1–3 The increasing burden of depression has a huge financial impact on many national healthcare systems as they struggle to meet needs.4,5 It is a common and often recurrent mental disorder with known risk factors that have been documented in the literature. These include body mass index (BMI),6 female gender, younger adults, having a chronic disease,7 family or maternal stress,8,9 child abuse and adverse childhood experience,10,11 smoking,7,12 and physical inactivity.13 Although there is a U-shaped relationship between BMI and depression,6 its relationship with diabetes mellitus is positive.14–16
Diabetes mellitus is a complex disease that continues to increase in many countries including Canada. It is estimated that 90% of diabetes mellitus cases among Canadian adults are type 2 whereas 10% constitute type 1 and gestational diabetes mellitus.17 According to the most recent data, an estimated 2.3 million (7.3%) of Canadians aged ⩾12 years live with a diabetes mellitus diagnosis in 2017.17 Recent reports by the International Diabetes Federation suggest that in 2017 about 425 million people globally were living with diabetes mellitus and this number is expected to increase to 642 million by the year 2040.18 This means 1 in 11 adults had diabetes mellitus as of 2017. The World Health Organization (WHO) estimated diabetes mellitus to be the seventh leading cause of death in 2016.19 The commonly reported risk factors of diabetes mellitus include rapid increases in overweight, obesity, physical inactivity, sedentary lifestyles, and dietary factors, such as high fat intake.14 Other risk factors include smoking, age, abdominal obesity, high blood pressure or hypertension, urban residence, and family history of diabetes mellitus.20 The Global Burden of Disease Study 2016 reports that depression and diabetes mellitus accounted for 34 million and 57 million all-age disability adjusted life-years (DALYs), respectively.21
Aside from known traditional risk factors for the two conditions, others suggest depression and diabetes mellitus are closely linked.22,23 Ducat et al.24 reported that mental health problems often co-occur in people with diabetes mellitus. In addition, depression is twice as common in people with diabetes mellitus as in the general population, and is associated with poorer outcomes.25 Three meta-analyses collectively report that individuals with depressive symptoms had a 37–60% greater risk of incident diabetes mellitus compared with those without depressive symptoms.26–28 In addition, Chireh et al.29 found a 33% increased risk of depression in patients with diabetes mellitus in their recent review of longitudinal studies. Other studies suggest a reciprocal or bidirectional relationship between these diseases.25,27,28
Several interpretations seek to disentangle the link between depression and diabetes mellitus. Some are of the view that the psychological trauma associated with a chronic disease diagnosis predisposes patients to depression and at the same time depression in patients with diabetes mellitus is associated with poor self-care behaviors.25,30 Katon et al.31 report that depressed people are more likely to have a high BMI, poor diet, be physically inactive, and smoke daily, all of which are known risk factors for diabetes.
There is evidence that depression and diabetes mellitus are linked. What is not well understood are the mechanisms linking depression and diabetes mellitus although no doubt behavioral and biological factors may both contribute. Depression and diabetes mellitus share common biological origins, particularly overactivation of innate immunity leading to a cytokine-mediated inflammatory response, and potentially through dysregulation of the hypothalamic–pituitary–adrenal axis. During an individual’s life course, these pathways can lead to insulin resistance, cardiovascular disease, depression, increased risk of diabetes mellitus, and increased mortality.32
Although both cross-sectional and longitudinal studies have consistently reported the risk factors for depression and diabetes mellitus separately, few have investigated the two disorders together and literature is scarce regarding shared disease risk factors for depression and diabetes mellitus at a national population level. There is a need to conduct well-characterized longitudinal cohort analyses to determine whether shared origins of depression and diabetes mellitus exist and that these shared origins could provide joint avenues for public health prevention strategies for both conditions.32
This study aims to: (1) explore shared and unique risk factors for incident depression and diabetes mellitus in the same population over a 10-year follow-up period; (2) assess sex differences in sex-specific shared or unique risk factors for depression and diabetes mellitus. What this study adds new is the concurrent assessment of shared disease risk factors over a 10-year follow-up period among middle age and older national population survey sample.
Method
Data sources
The Canadian longitudinal National Population Health Survey (NPHS) is used. It is a nationally representative longitudinal community study (n = 17,276) started in 1994–1995 with participants followed until 2010–2011. It has the ability to establish a temporal relationship between predictor variables and incident depression and diabetes mellitus. It was conducted by Statistics Canada with the sole purpose of collecting longitudinal information on the health of the Canadian population. A multistage stratification method was used to select respondents whilst taking into consideration the geographic and socioeconomic characteristics and clustering of the population. Interviewers had face-to-face interviews with respondents at baseline and after which respondents were re-interviewed every second year by telephone. Our study used six cycles (to 2004–2005) for this analysis. We excluded respondents who were less than 45 years of age. The NPHS longitudinal study initial sample had 17,726 participants (ages 12 years and over) and after follow-up to cycle 9 had an overall response rate of 69.7%.33 Our analysis stopped at cycle 6 in order to limit loss to follow up issues. We recorded a lower response rate after cycle 6 and the age restriction of our sample affected loss to follow up, with significant losses to follow up recorded after cycle 6 probably due to death. The NPHS ethics review process was approved by Statistics Canada and all respondents to the original survey provided informed consent. A detailed description of the survey is available elsewhere.34,35
Study sample
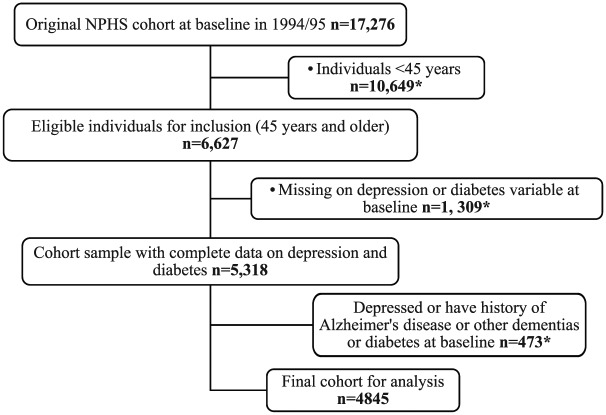
Our study was limited to 4,845 participants who were free of depression and diabetes mellitus at baseline and aged ⩾45 years. They were followed to 2004/2005. Five exclusion criteria were used at baseline. These include: (1) those who were depressed at baseline (1994–1995); (2) participants who self-reported positively to having a doctor diagnosis of diabetes mellitus at or before baseline; (3) reported a history of Alzheimer’s disease or other dementias; (4) had missing values on diabetes mellitus at baseline or at follow up; and (5) had missing values on depression at baseline or at follow up. Incident cases of depression and diabetes mellitus were the focus of this study. Figure 1 shows a detailed description of the selection criteria used to generate the study cohort. At cycle 6, 56.6% of depression sample respondents and 62.7% of diabetes mellitus sample respondents remained in the study.
Figure 1.
Restriction criteria employed to obtain the subsample of National Population Health Survey (NPHS) cohort in this study.
*Excluded from the analysis.
Measures
Depression
Major depressive episode (MDE) over the past 12 months was assessed using the Composite International Diagnostic Interview Short Form (CIDI-SF), an internationally recognized depression diagnostic questionnaire which was keyed to major depression criteria in the Diagnostic and Statistical Manual of Mental Disorders 3rd edition (DSM-III-R).36 Participant’s symptoms were assessed in the past year prior to the interview. In the NPHS study, MDE was defined by a cut-point of 90% predictive probability for the CIDI-SF.
Diabetes
Diabetes mellitus incidence was assessed based on a self-report of diagnosis by a doctor or health professional through to cycle 6.
Predictors/covariates
A wide variety of lifestyle, behavioral, sociodemographic, and physiological predictors or covariates were assessed at baseline (1994–1995). The variables included in this analysis were: sex, age (45–54, 55–64, ⩾65 years), household annual income (<$15,000, $15,000–$29,999, $30,000–$49,999, $50,000–$79,999, ⩾$80,000), self-reported BMI (underweight < 18.5 kg/m2, normal weight 18.5–24.9 kg/m2, overweight 25–29.9 kg/m2, and obese > 30 kg/m2 ), type of smoker (‘occasional/former/never smoked’ and ‘daily smoker’), ethnicity (‘Caucasian/white’ and ‘all other ethnicities/nonwhite’), family stress index (‘some stress/stress overload/yes’ and ‘no stress/no’), traumatic life events (‘less than three traumatic life events/three or more traumatic life events/yes’ and ‘no traumatic life events/no’), high blood pressure (‘yes’ and ‘no’), chronic disease (‘yes’ and ‘no’), heart disease (‘yes’ and ‘no’). Hypertension, heart disease, and chronic disease were assessed at baseline through doctor or health professional diagnoses of any of the conditions. The survey reported both heart disease and chronic disease separately. We used the term ‘sex’ here rather than gender as the NPHS survey questionnaire asked respondent whether they were male or female.
Statistical analysis
This secondary analysis of the NPHS, longitudinal 1994 dataset was done using Statistics Canada confidential microdata files (Master data files) that are accessible through Research Data Centers only (https://crdcn.org). The modified Poisson regression was used to estimate the relative risk (RR) because of its ability to consistently and effectively estimate RR with a robust error variance in prospective studies.37 Univariate modified Poisson regression was conducted to assess the unadjusted relationship between shared or unique risk factors of both depression and diabetes mellitus and the new onset of both conditions. Unadjusted measures could not be reported in the stratified analysis because most variables did not meet the minimum required number of cases in a cell necessary for vetting. All included predictor variables recorded an unadjusted p < 0.20 at the univariate analysis stage and were maintained for subsequent analyses in multivariate Poisson regression. At the multivariate analysis stage, a modified Poisson regression was used to assess the association between shared or unique risk factors and the incidence of depression or diabetes mellitus during the follow up.
In total, three modified Poisson regression models were fitted: (1) associations between shared or unique risk factors and the onset of depression and/or diabetes mellitus; (2) characteristics associated with incident major depressive disorder during the 10-year follow up by sex; and (3) characteristics associated with incident diabetes mellitus during the 10-year follow up by sex. Sex differences were assessed because it was reported as a significant risk factor for both depression and diabetes mellitus in the univariate analysis. The goodness of fit for the various models was tested. We reported unadjusted and adjusted RR and 95% confidence intervals at a significance level of p < 0.05. STATA version 14 was used for the statistical analysis.38
Results
Study demographic characteristics
The majority of our subsample of adults free of depression and diabetes mellitus aged ⩾45 years at baseline were women (56.8%), fell within the age group of 55–64 years (40.8%), had less than secondary graduation education (43%), were married or in common law relationships (60%), were white (96.5%), 29.8% had a household income of $15,000–$29,999, and 56.5% were overweight or obese. Table 1 below lists the demographic characteristics of study subjects at baseline.
Table 1.
Baseline demographic characteristics of respondents (aged ⩾45) covered in the 1994/95 cycle.
| Characteristics | Frequency | Percentage (%) |
|---|---|---|
| Sex | ||
| Male | 2095 | 43.2 |
| Female | 2750 | 56.8 |
| Total | 4845 | 100 |
| Age categories, years | ||
| 45–54 | 896 | 18.5 |
| 55–64 | 1976 | 40.8 |
| 65 and above | 1973 | 40.7 |
| Total | 4845 | 100 |
| Educational level | ||
| Post-secondary graduation | 1205 | 24.9 |
| Some post-secondary education | 955 | 19.7 |
| Secondary graduation | 602 | 12.4 |
| Less than secondary graduation | 2083 | 43.0 |
| Total | 4845 | 100 |
| Marital Status | ||
| Married/common law | 2909 | 60.0 |
| Divorced/separate/widowed | 1547 | 31.9 |
| Never married/single | 389 | 8.0 |
| Total | 4845 | 100 |
| Race/ethnicity | ||
| White | 4673 | 96.5 |
| Nonwhite | 172 | 3.6 |
| Total | 4845 | 100 |
| Household income, CAD | ||
| <$15,000 | 1118 | 23.1 |
| $15,000–$29,999 | 1444 | 29.8 |
| $30,000–$49,999 | 1121 | 23.1 |
| $50,000–$79,999 | 762 | 15.7 |
| ⩾$80,000 | 400 | 8.3 |
| Total | 4845 | 100 |
| Self-reported body mass index | ||
| Normal weight | 1985 | 41.0 |
| Underweight | 122 | 2.5 |
| Overweight | 1995 | 41.2 |
| Obese | 743 | 15.3 |
| Total | 4845 | 100 |
Characteristics associated with incident depression and diabetes mellitus (multivariate analysis)
Four shared disease risk factors for incident depression and diabetes mellitus were found: (1) high blood pressure or hypertension, (2) being a smoker, (3) physical inactivity, and (4) self-reported BMI. Compared with nonhypertensive participants, those who were hypertensive were 1.34 times (95% CI = 0.87–2.07) and 1.62 times (95% CI = 1.28–2.06) more likely to report incident depression and diabetes mellitus, respectively. Daily smoking was significantly associated with the risk of depression (RR = 1.72, 95% CI = 1.16–2.56) and diabetes mellitus (RR = 1.36, 95% CI = 1.04–1.77). Respectively, physically inactive participants were 1.24 times (95% CI = 0.85–1.80) and 1.24 times (95% CI = 0.99–1.56) more likely to develop depression and diabetes mellitus. We found a U-shaped relationship between self-reported BMI and depression and a direct positive relationship between BMI and diabetes mellitus. Underweight participants were 3.34 times at risk for depression (95% CI = 1.40–7.97) whereas obese persons were 1.01 times (95% CI = 0.61–1.69) more likely to report depression. Overweight or obese survey participants had 1.81 and 3.24 times (p < 0.001) higher risk of reporting diabetes mellitus, respectively, compared with the normal weight respondents.
We found five unique disease risk factors for incident depression: (1) being female, (2) family stress, (3) traumatic life events, (4) presence of one or more chronic diseases, and (5) heart diseases. We found that women were 2.13 times (95% CI = 1.40–3.24) at risk of developing depression compared with men. Respondents with family stressors such as activity overload, financial difficulties and problems with relationships in their day-to-day encounters were 1.48 times (95% CI = 1.02–2.15) at risk of developing depression. Participants with any history of traumatic experiences during childhood, adolescence, or adulthood had a 46% (95% CI = 1.00–2.13) increased risk of having depression. Those with chronic health conditions were 2.47 times (95% CI = 1.47–4.15) at a higher risk of depression. Having a heart disease was also a significant unique risk factor for depression (RR = 2.21, 95% CI = 1.47–4.15).
This study recorded only two unique disease risk factors for incident diabetes mellitus. The risk of diabetes mellitus increased with age. Participants aged 55–64 years and those ⩾65 years were 1.66 times (95% CI = 1.22–2.28) and 1.63 times (95% CI = 1.16–2.29) more likely to develop diabetes mellitus, respectively. Participants indicating they were ‘nonwhite’ were almost twice as likely to report diabetes mellitus compared with those reporting themselves as ‘white’ (RR = 1.73, 95% CI = 1.09–2.75).
Overall, this study did not find shared protective factors for both conditions. However, increasing age was a significant protective factor for depression (p = 0.018), whereas increasing income was a significant protective factor for diabetes mellitus (p = 0.037). Table 2 represents the final multivariate modified Poisson regression model for incident depression and diabetes mellitus among those aged 45 years and over after adjusting for covariates and/or predictor variables.
Table 2.
Adjusted shared and unique risk factors for depression and diabetes mellitus during the 10-year follow up (cycle 6).
| Depression n = 2743 |
Diabetes n = 3040 |
|||
|---|---|---|---|---|
| Characteristics | RR, 95% CI | p value | RR, 95% CI | p value |
| Sex | ||||
| Male | Reference | Reference | ||
| Female | 2.13 (1.40–3.24) | <0.001 | N/A | N/A |
| Age categories, years | ||||
| 45–54 | Reference | Reference | ||
| 55–64 | 0.65 (0.43–0.98) | 0.040 | 1.66 (1.22–2.28) | 0.002 |
| ⩾65 above | 0.43 (0.24–0.78) | 0.005 | 1.63 (1.16–2.29) | 0.005 |
| Household income, CAD | ||||
| <$15,000 | Reference | Reference | ||
| $15,000–$29,999 | N/A | N/A | 0.83 (0.63–1.09) | 0.188 |
| $30,000–$49,999 | N/A | N/A | 0.62 (0.45–0.85) | 0.003 |
| $50,000–$79,999 | N/A | N/A | 0.66 (0.46–0.94) | 0.023 |
| ⩾$80,000 | N/A | N/A | 0.76 (0.50–1.16) | 0.204 |
| Ethnic background | ||||
| White | Reference | Reference | ||
| Nonwhite | N/A | N/A | 1.73 (1.09–2.75) | 0.021 |
| High blood pressure | ||||
| No | Reference | Reference | ||
| Yes | 1.34 (0.87–2.07) | 0.183 | 1.62 (1.28–2.06) | <0.001 |
| Type of smoker | ||||
| Abstainer/never smoke | Reference | Reference | ||
| Daily smoker | 1.72 (1.16–2.56) | 0.007 | 1.36 (1.04–1.77) | 0.022 |
| Physical activity | ||||
| Active | Reference | Reference | ||
| Inactive | 1.24 (0.85–1.80) | 0.275 | 1.24 (0.99–1.56) | 0.066 |
| Self-reported BMI | ||||
| Normal weight | Reference | Reference | ||
| Underweight | 3.34 (1.40–7.97) | 0.007 | 0.39 (0.06–2.72) | 0.345 |
| Overweight | 0.94 (0.63–1.42) | 0.772 | 1.81 (1.36–2.40) | <0.001 |
| Obese | 1.01 (0.61–1.69) | 0.960 | 3.24 (2.39–4.41) | <0.001 |
| Family stress | ||||
| No | Reference | Reference | ||
| Yes | 1.48 (1.02–2.15) | 0.049 | N/A | N/A |
| Traumatic events | ||||
| No | Reference | Reference | ||
| Yes | 1.46 (1.00–2.13) | 0.001 | N/A | N/A |
| Chronic disease | ||||
| Without | Reference | Reference | ||
| With | 2.47 (1.47–4.15) | 0.001 | N/A | N/A |
| Heart disease | ||||
| No | Reference | Reference | ||
| Yes | 2.21 (1.33–3.69) | 0.002 | N/A | N/A |
Notes: Bold RR represents shared risk factors for both depression and diabetes mellitus.
BMI, body mass index; CI, confidence interval; RR, relative risk.
Sex differences in characteristics associated with incident depression
Different regression models were run for men and women. Four shared sex-specific risk factors for depression such as underweight, having family stress, one or more chronic diseases, and heart disease were found for both men and women although there are differences in the strength of those relationships. Underweight men were 9.09 times (95% CI = 1.95–42.5) more likely to report depression, in contrast, women were 2.92 times (95% CI = 1.09–7.84) more likely to develop depression. Men who experience family stress had a 1.82 times (95% CI = 0.85–3.90) increased risk of depression whereas women were 1.47 times (95% CI = 0.96–2.27) more likely. On the other hand, women with chronic diseases were more likely to report depression (RR = 2.45, 95% CI = 1.33–4.51) compared with men (RR = 2.14, 95% CI = 0.78–5.89). For participants with heart diseases, men were 3.29 times (95% CI = 1.34–8.07) more likely to report depression, in contrast, women were 1.94 times (95% CI = 1.02–3.69) as likely to develop depression.
Women reported two unique sex-specific risk factors for depression. Hypertensive women were 1.61 times (95% CI = 1.00–2.62) more at risk of depression. In addition, female daily smokers were more at risk of depression compared with non-smokers (RR = 1.82, 95% CI = 1.16–2.86). We, however, found that increasing age was an insignificant shared protective factor for depression among men (p = 0.251) and a significant protective factor among women (p = 0.003). Although women did not report any unique protective factor for depression, income was a unique significant protective factor for depression among men (p < 0.001). Table 3 presents shared and unique risk or protective factors for depression by sex differences.
Table 3.
Adjusted risk factors for incident major depressive disorder during the 10-year follow up stratified by sex.
| Men n = 1136 |
Women n = 1607 |
|||
|---|---|---|---|---|
| Characteristics | RR, 95% CI | p value | RR, 95% CI | p value |
| Age categories, years | ||||
| 45–54 | Reference | Reference | ||
| 55–64 | 0.53 (0.23–1.21) | 0.130 | 0.62 (0.38–0.99) | 0.048 |
| ⩾65 | 0.46 (0.15–1.39) | 0.170 | 0.33 (0.17–0.62) | 0.001 |
| Household income, CAD | ||||
| <$15,000 | Reference | Reference | ||
| $15,000–$29,999 | 0.38 (0.16–0.94) | 0.037 | N/A | N/A |
| $30,000–$49,999 | 0.26(0.089–0.76) | 0.013 | N/A | N/A |
| $50,000–$79,999 | 0.34 (0.13–0.90) | 0.030 | N/A | N/A |
| ⩾$80,000 | 0.21(0.006–0.45) | <0.001 | N/A | N/A |
| High blood pressure | ||||
| No | Reference | Reference | ||
| Yes | N/A | N/A | 1.61 (1.00–2.62) | 0.052 |
| Type of smoker | ||||
| Abstainer/never smoke | Reference | Reference | ||
| Daily smoker | N/A | N/A | 1.82 (1.16–2.86) | 0.010 |
| Self-reported BMI | ||||
| Normal weight | Reference | Reference | ||
| Underweight | 9.09 (1.95–42.5) | 0.005 | 2.92 (1.09–7.84) | 0.033 |
| Overweight | 1.61 (0.66–3.91) | 0.294 | 0.84 (0.52–1.35) | 0.471 |
| Obese | 1.35 (0.43–4.22) | 0.601 | 0.96 (0.54–1.71) | 0.888 |
| Family stress | ||||
| No | Reference | Reference | ||
| Yes | 1.82 (0.85–3.90) | 0.124 | 1.47 (0.96–2.27) | 0.079 |
| Chronic disease | ||||
| Without | Reference | Reference | ||
| With | 2.14 (0.78–5.89) | 0.141 | 2.45 (1.33–4.51) | 0.004 |
| Heart disease | ||||
| No | Reference | Reference | ||
| Yes | 3.29 (1.34–8.07) | 0.009 | 1.94 (1.02–3.69) | 0.044 |
Notes: Bold RR represents shared risk factors of depression by men and women.
BMI, body mass index; CI, confidence interval; RR, relative risk.
Sex differences in characteristics associated with incident diabetes mellitus
Six characteristics, age, race or ethnicity, hypertension, smoking status, physical inactivity, and self-reported BMI, were found to be shared sex-specific risk factors of diabetes mellitus among men and women. However, there were differences in the strength of the association between the sexes. Senior women (⩾65 years) were 2.72 times (95% CI = 1.54–4.79) more likely to report diabetes mellitus compared with 1.44 times (95% CI = 0.92–2.28) for senior men (⩾65 years). Female ‘nonwhites’ were also at a greater risk of diabetes mellitus (RR = 1.91, 95% CI = 1.02–3.58). Hypertensive men were 1.71 times (95% CI = 1.18–2.47) at a greater risk of diabetes mellitus compared with hypertensive women 1.59 times (95% CI = 1.17–2.16). Male daily smokers (RR = 1.49, 95% CI = 1.03–2.15) were significantly more at risk of incident diabetes mellitus compared with female daily smokers (RR = 1.30, 95% CI = 0.89–1.90). Men who were physically inactive had a 32% (95% CI = 0.93–1.87) increased risk of developing diabetes mellitus compared with physically inactive women 19% (95% CI = 0.93–1.87). Obese male survey respondents were at 3.73 times (95% CI = 2.24–6.18) greater risk of diabetes mellitus compared with obese female respondents at 3.09 times (95% CI = 2.09–4.58) greater risk.
We found heart disease to be a unique sex-specific risk factor for incident diabetes mellitus among women only. Women with heart disease were 1.66 times (95% CI = 1.08–2.56) at risk of incident diabetes mellitus compared with women without heart disease. However, this risk factor was not found to be present among men. The data analyzed did not reveal any sex-specific protective factors for diabetes mellitus in this survey sample (see Table 4).
Table 4.
Adjusted risk factors for diabetes mellitus incidence during the 10-year follow up stratified by sex.
| Men n = 1253 |
Women n = 1787 |
|||
|---|---|---|---|---|
| Characteristics | RR, 95% CI | p value | RR, 95% CI | p value |
| Age categories, years | ||||
| 45–54 | Reference | Reference | ||
| 55–64 | 1.25 (0.84–1.87) | 0.270 | 2.72 (1.57–4.73) | <0.001 |
| ⩾65 | 1.44 (0.92–2.28) | 0.110 | 2.72 (1.54–4.79) | 0.001 |
| Ethnic Background | ||||
| White | Reference | Reference | ||
| Nonwhite | 1.59 (0.80–3.17) | 0.185 | 1.91 (1.02–3.58) | 0.044 |
| High blood pressure | ||||
| No | Reference | Reference | ||
| Yes | 1.71 (1.18–2.47) | 0.005 | 1.59 (1.17–2.16) | 0.003 |
| Type of smoker | ||||
| Abstainer/never smoke | Reference | Reference | ||
| Daily smoker | 1.49 (1.03–2.15) | 0.036 | 1.30 (0.89–1.90) | 0.179 |
| Physical activity | ||||
| Active | Reference | Reference | ||
| Inactive | 1.32 (0.93–1.87) | 0.119 | 1.19 (0.88–1.61) | 0.270 |
| Self-reported BMI | ||||
| Normal weight | Reference | Reference | ||
| Underweight | 0.33 (1.33–8.33) | <0.001 | 0.53 (0.08–3.66) | 0.521 |
| Overweight | 1.73 (1.08–2.79) | 0.023 | 1.77 (1.23–2.55) | 0.002 |
| Obese | 3.73 (2.24–6.18) | <0.001 | 3.09 (2.09–4.58) | <0.001 |
| Heart disease | ||||
| No | Reference | Reference | ||
| Yes | N/A | 1.66 (1.08–2.56) | 0.021 | |
Note: Bold RR represents shared risk factors of diabetes mellitus by men and women.
BMI, body mass index; CI, confidence interval; RR, relative risk.
Discussion
We found that the cumulative incidence of depression and diabetes mellitus during the 10-year follow-up period were 4.1% and 10.1%, respectively. Our cumulative incidence of diabetes mellitus is higher than the 3.5% reported in a cohort study in Spain39 but lower than the 11.2% reported in a population-based longitudinal study in Singapore.16 In addition, the cumulative incidence of major depressive disorder we reported is much lower than the 12.1% cumulative incidence previously reported in a 16-year Canadian longitudinal study.7 However, these differences may be due to differences in age restrictions in our study sample and follow-up periods.
Foremost, we found four shared disease risk factors for both depression and diabetes mellitus. Those survey participants who were (1) hypertensive, (2) daily smokers, (3) physically inactive, and (4) overweight or obese had a higher risk of developing either depression or diabetes mellitus. These findings are in keeping with earlier results that reported risk factors for depression and diabetes mellitus separately.6,7,12–14,16,20,31
Second, we found that being female, family stress, traumatic life events, the presence of one or more chronic diseases and heart disease were the four risk factors that were uniquely associated with incident depression. Our findings are consistent with previous research.7–11
Third, we found that increasing age and being nonwhite were the only unique disease risk factors for diabetes mellitus. After age 55 years the risk of developing diabetes mellitus was almost twice as likely compared with those below 55. This finding is similar to that reported in earlier studies.20,39 Whites had a lower incidence of diabetes mellitus compared with nonwhites, which is similar to a previous study in the United States where a high prevalence of diabetes mellitus was found among non-Hispanic blacks and those of Mexican origin who had the highest prevalence rates.40 Our finding highlights the disproportionate ethnic burden of diabetes mellitus prevalence or incidence in Canada and requires the development of comprehensive policies and programs to help in the early prevention, diagnosis, and treatment of diabetes mellitus and its complications.
Surprisingly, we did not find shared protective factors for depression and diabetes mellitus. Each disease had different protective factors. Whereas increasing age was a significant protective factor for depression, income (higher income) was the only protective factor for diabetes mellitus. A possible explanation of the age–depression inverse relationship could be that older adults have become more self-accepting and may see depression as a normal part of aging. Similarly, it could also imply that wealthy Canadians are more likely to have access to fresh, healthy foods and programs that promote physical activity compared with poorer ones.
We found a U-shaped relationship between BMI and depression, this is in keeping with an earlier report.6 In contrast, the relationship between diabetes mellitus and BMI (overweight or obesity) was positive. Those overweight or obese were at a higher risk of diabetes mellitus. Similar findings have been reported in other studies including Chinese and Singaporean longitudinal studies.14–16
In sex-stratified analyses, we found four shared sex-specific risk factors for depression between men and women. Being underweight, having family stress, having a chronic disease, and heart disease were all shared risk factors for depression in both sexes. This is similar to findings reported in the literature.6–9
Two unique sex-specific risk factors for incident major depressive disorder were for women. Women that were hypertensive and smoke daily were at a significantly increased risk of depression. This was not true of men. These findings give credence to the existence of significant sex differences in the risk factors for the major depressive disorder in Canada which have also been reported in previous research.41–43 However, an Italian study found no association between smoking and the incidence of depression among either men or women, perhaps reflecting cultural differences in cigarette smoking patterns.44
For the incidence of diabetes mellitus, shared sex-specific risk factors were present for both men and women. Increasing age, being nonwhite, high blood pressure, smoking status, physical inactivity, and BMI were shared risk factors. Heart disease was, however, the only unique risk factor significantly associated with diabetes mellitus among women only and not for men. This finding possibly highlights the sex differences in heart disease treatment and management in Canada. There is, therefore, the need to improve detection, treatment, and management of heart diseases among women and also encourage them to adopt healthy lifestyles.
Our finding that self-reported BMI (overweight or obesity) was a strong risk factor for incident diabetes mellitus in both sexes has been reported elsewhere.45,46 We also found high blood pressure or hypertension was positively associated with incident diabetes mellitus in both men and women, which is somewhat at variance with an earlier study that found high blood pressure was associated with diabetes mellitus in men.46
We also found that physical inactivity was an insignificant risk factor for diabetes mellitus in both sexes. This is at variance to findings reported by the MONICA Augsburg Cohort Study, which found physical inactivity during leisure time to be significantly associated with (80%) increased risk of diabetes mellitus incidence in women.46 This results shows the minimal differences in physical inactivity between men and woman in Canada although women are more likely to be physical inactive than men.
We found that nonwhite women but not men were at a statistically significant higher risk of incident diabetes mellitus compared with their white counterparts. This is consistent with earlier results including the Atherosclerosis Risk in Communities (ARIC) study where the greatest disparity in diabetes mellitus incidence was found between nonwhite and white individuals.47–49 Previous studies also suggest that sex-specific risk factors are more likely to contribute to greater risk in diabetes mellitus incidence among nonwhite women than white men.49,50
Increasing age was an independent risk factor for diabetes mellitus in both men and women. However, the effect was more prominent in women than men and confirms an earlier study in the literature.46 In summary, our results show that although risk factors for diabetes mellitus were not generally different between men and women, their respective effects on diabetes mellitus incidence were more pronounced in women compared with men.
Strengths and weaknesses
The major strength of this study is the use of a nationally representative relatively large longitudinal population-based professionally conducted survey with a 10-year follow-up period to measure the shared disease risk factors for depression and diabetes mellitus incidence. The survey also examined sex disparities in the risk factors for depression and diabetes mellitus in the same population.
However, this study has limitations. In the ⩾45 years age group studied, there was a significant attrition. The attrition rate during the follow-up period was relatively high and could underestimate the cumulative incidence of depression and diabetes mellitus owing to attrition bias. In addition, some other potential risk factors such as childhood maltreatment particularly for depression were not assessed in the NPHS study.
In addition, the NPHS study was restricted to only residents in the 10 provinces of Canada. Residents in the three northern territories predominantly occupied by indigenous Canadians were excluded and this could possibly explain the large sample size of the white ethnicity compared with other ethnicities. This is also a major weakness of the study as this could result in selection bias.
Furthermore, the age of our dataset is a major limitation of this study. We described risk factors for depression and diabetes mellitus as of 14 years ago. There is the likelihood that a number of societal changes have occurred over this period. Factors such as changes in diagnostic criteria for depression, lifestyle or behavioral factors, and health seeking behaviors might have changed over the years.
This study did not include other important risk factors for diabetes mellitus such as waist-to-hip circumference, cholesterol level, and low-density lipoprotein cholesterol level. This is because data on these risk factors were not collected in the NPHS study. This may have biased the results in the direction of the reported risk factors compared with those that were not reported. Overall, the above limitations may have skewed the results resulting in under-reporting of the two chronic conditions.
Conclusion
This study has demonstrated that hypertension, daily smoking, physical inactivity, and overweight or obesity are shared disease risk factors for both depression and diabetes mellitus. The findings have also demonstrated the effect of sex differences in both of these diseases. Our stratified analyses have shown that being underweight, having family stress, having a chronic disease and heart disease are all shared sex-specific risk factors for major depressive disorder in both sexes. On the other hand, increasing age, being nonwhite, high blood pressure, daily smoking, physical inactivity, and overweight or obesity were shared sex-specific risk factors associated with an increased risk of incident diabetes mellitus in both men and women. From a prevention point of view, the results of this study strengthened the importance of public health prevention programs targeting general risk behaviors that are not specific to a particular disease but in fact are implicated in the genesis of a range of chronic diseases. The scientific and clinical relevance of these findings is that the shared disease risk factors found in this study are for important chronic conditions that are on the rise globally including Canada and that effective and early public health primary prevention strategies are essential. Sex differences should be taken into consideration in rolling out such prevention strategies. In addition, future research should concentrate on and adopt population-based primary prevention intervention studies to reduce the prevalence of modifiable risk factors for depression and diabetes mellitus.
Supplemental Material
Supplemental material, STROBE_checklist_cohort_Chireh1 for Shared and unique risk factors for depression and diabetes mellitus in a longitudinal study, implications for prevention: an analysis of a longitudinal population sample aged ⩾45 years by Batholomew Chireh and Carl D’Arcy in Therapeutic Advances in Endocrinology and Metabolism
Acknowledgments
The first author (BC) received a scholarship from the University of Saskatchewan School of Public Health Scholarship program. We thank the Saskatchewan Research Data Centre (SKY) and the Canadian Research Data Centre Network (CRDCN) for granting us access to their confidential data.
Footnotes
Authors’ note: Authors BC and CD designed and conceptualized the work. Author BC analyzed the study results and drafted the various versions of the manuscript which were revised and edited by CD. Both authors reviewed and approved the final manuscript.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The first author is a PhD candidate in the University of Saskatchewan School of Public Health and is funded by the school’s scholarship program. The funder had no influence over the conduct and drafting of this manuscript.
Conflict of interest statement: The authors declare that there is no conflict of interest.
Ethical approval: Ethical approval was not required for this study because it was a secondary analysis of a national health survey already conducted by Statistics Canada. Written informed consent was obtained from all respondents, as well as ethics review approval for the original study before it started. The approval number of the original data could not be obtained because it was a confidential national health survey conducted by Statistics Canada and managed by the Social Sciences and Humanities Research Council (SSHRC). Data used for this cohort study analysis are not publicly available but can be accessed using Statistics Canada confidential microdata files (Master data files) through a Research Data Centre only (https://crdcn.org). A written proposal was sent to Statistics Canada for access to the data which was subsequently vetted and approved by the Social Sciences and Humanities Research Council (SSHRC) with approval number (Application Id: 928488). The analysis presented in this paper was conducted at the Saskatchewan Research Data Centre, which is part of the Canadian Research Data Centre Network (CRDCN). The services and activities provided by the Saskatchewan Research Data Centre are made possible by the financial or in-kind support of the Social Sciences and Humanities Research Council (SSHRC), the Canadian Institute of Health Research (CIHR), the Canadian Foundation for Innovation (CFI), Statistics Canada, and University of Saskatchewan. The views expressed in this paper do not necessarily represent the CRDCN’s or that of its partners’.
ORCID iD: Batholomew Chireh:  https://orcid.org/0000-0002-1803-2890
https://orcid.org/0000-0002-1803-2890
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Batholomew Chireh, School of Public Health, University of Saskatchewan, 104 Clinic Place, Saskatoon, SK, S7N 2Z4, Canada.
Carl D’Arcy, School of Public Health and Department of Psychiatry, University of Saskatchewan, Saskatoon, SK, Canada.
References
- 1. Ferrari AJ, Charlson FJ, Norman RE, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med 2013; 10: e1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fu TS, Lee CS, Gunnell D., et al. Changing trends in the prevalence of common mental disorders in Taiwan: a 20-year repeated cross-sectional survey. Lancet 2013; 381: 235–241. [DOI] [PubMed] [Google Scholar]
- 3. Smith RP, Larkin GL, Southwick SM. Trends in U.S. emergency department visits for anxiety-related mental health conditions, 1992–2001. J Clin Psych 2008; 69: 286–294. [DOI] [PubMed] [Google Scholar]
- 4. Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet 2012; 380: 2197–223. [DOI] [PubMed] [Google Scholar]
- 5. Crystal S, Sambamoorthi U, Walkup JT, et al. Diagnosis and treatment of depression in the elderly medicare population: predictors, disparities, and trends. J Am Geriatr Soc 2003; 51: 1718–1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. de Wit Leonore M, van Straten A, van Herten M, et al. Depression and body mass index, a u-shaped association. BMC Public Health 2009; 9: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Meng X, D’Arcy C. The projected effect of risk factor reduction on major depression incidence: a 16-year longitudinal Canadian cohort of the national population health survey. J Affect Dis 2014; 158: 56–61. [DOI] [PubMed] [Google Scholar]
- 8. Walder DJ, Faraone SV, Glatt SJ, et al. Genetic liability, prenatal health, stress and family environment: risk factors in the Harvard adolescent family high risk for schizophrenia study. Schizophr Res 2014; 157: 142–148. [DOI] [PubMed] [Google Scholar]
- 9. Walder DJ, Laplante DP, Sousa-Pires A, et al. Prenatal maternal stress predicts autism traits in 6½ year-old children: project ice storm. Psych Res 2014; 219: 353–360. [DOI] [PubMed] [Google Scholar]
- 10. Colman I, Murray J, Abbott RA, et al. Outcomes of conduct problems in adolescence: 40 year follow-up of national cohort. BMJ 2009; 338: 2981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kessler RC, Amminger GP, Aguilar-Gaxiola S, et al. Age of onset of mental disorders: a review of recent literature. Curr Opin Psych 2007; 20: 359–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. He Q, Yang L, Shi S, et al. Smoking and major depressive disorder in Chinese women. PLoS One 2014; 9: e106287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Meng X, D’Arcy C. The projected effect of increasing physical activity on reducing the prevalence of common mental disorders among Canadian men and women: a national population-based community study. Prev Med 2013; 56: 59–63. [DOI] [PubMed] [Google Scholar]
- 14. Hu FB, Manson JE, Stampfer MJ, et al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med 2001; 345: 790–797. [DOI] [PubMed] [Google Scholar]
- 15. Wang C, Li JX, Xue HF, et al. Type 2 diabetes mellitus incidence in Chinese: contributions of overweight and obesity. Diab Res Clin Pr 2015; 107: 424–432. [DOI] [PubMed] [Google Scholar]
- 16. Man REK, Charumathi S, Gan ATL, et al. Cumulative incidence and risk factors of prediabetes and type 2 diabetes in a Singaporean Malay cohort. Diab Res Clin Pract 2017; 127:163–171. [DOI] [PubMed] [Google Scholar]
- 17. Public Health Agency of Canada (PHAC). Fast facts about diabetes: Data compiled from the 2011 survey on living with chronic diseases in Canada, https://www.canada.ca/en/public-health/services/chronic-diseases/reports-publications/diabetes/fast-facts-about-diabetes-2011.html (2011, accessed 2 July 2019).
- 18. International Diabetes Federation. IDF Diabetes Atlas: 8th ed, http://www.diabetesatlas.org/resources/2017-atlas.html (2017, accessed 28 July 2018).
- 19. World Health Organization. Diabetes, https://www.who.int/news-room/fact-sheets/detail/diabetes (2016, accessed 28 July 2018).
- 20. Seung JH, Hae JK, Dae JK, et al. Incidence and predictors of type 2 diabetes among Koreans: a 12-year follow up of the Korean genome and epidemiology study. Diab Res Clin Pr 2017; 123: 173–180. [DOI] [PubMed] [Google Scholar]
- 21. GBD 2016. DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet 2017; 390:1260–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Talbot F, Nouwen F. A review of the relationship between depression and diabetes in adults: is there a link? Diab Care 2000; 23:1556–1562. [DOI] [PubMed] [Google Scholar]
- 23. Carnethon MR, Kinder LS, Fair JM, et al. Symptoms of depression as a risk factor for incident diabetes: findings from the national health and nutrition examination epidemiologic follow-up study, 1971–1992. Am J Epidemiol 2003; 158: 416–423. [DOI] [PubMed] [Google Scholar]
- 24. Ducat L, Philipson LH, Anderson BJ. The mental health comorbidities of diabetes. JAMA 2014; 312: 691–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Anderson RJ, Freedland KE, Clouse RE, et al. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diab Care 2001; 24:1069–1078. [DOI] [PubMed] [Google Scholar]
- 26. Knol MJ, Twisk JWR, Beekman ATF, et al. Depression as a risk factor for the onset of type 2 diabetes mellitus. A meta-analysis. Diabetol 2006; 49: 837–845. [DOI] [PubMed] [Google Scholar]
- 27. Mezuk B, Eaton WW, Albrecht S, et al. Depression and type 2 diabetes over the lifespan a meta-analysis. Diab Care 2008; 31: 2383–2390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rotella F, Mannucci E. Depression as a risk factor for diabetes: a meta-analysis of longitudinal studies. J Clin Psych 2013; 74: 32–38. [DOI] [PubMed] [Google Scholar]
- 29. Chireh B, Li M, D’Arcy C. Diabetes increases the risk of depression: a systematic review, meta-analysis and estimates of population attributable fractions based on prospective studies. Prev Med Rep 2019; 14: 100822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Katon WJ, Russo JE, Heckbert SR, et al. The relationship between changes in depression symptoms and changes in health risk behaviors in patients with diabetes. Int J Geriatr Psych 2010; 25: 466–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Katon WJ, Lin EH, Russo J, et al. Cardiac risk factors in patients with diabetes mellitus and major depression. J Gen Intern Med 2004; 19: 1192–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Moulton DC, Pickup CJ, Khalida I. The link between depression and diabetes: the search for shared mechanisms. Lancet Diab Endocrinol 2015; 3: 461–471. [DOI] [PubMed] [Google Scholar]
- 33. Statistics Canada. National population health survey – household component longitudinal(NPHS), http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3225&Item_Id=1824&lang=en (2012, accessed 25 July 2018).
- 34. Swain L, Catlin G, Beaudet MP. The national population health survey – its longitudinal nature. Health Rep 1999; 10: 69–82. [PubMed] [Google Scholar]
- 35. Tambay JL, Catlin G. Sample design of the national population health survey. Health Rep 1995; 7: 29–38. [PubMed] [Google Scholar]
- 36. Kessler RC, Andrews G, Mroczek D, et al. The world health organization composite international diagnostic interview short-form (CIDI-SF). Int J Methods Psychiatr Res 1998; 7: 171–185. [Google Scholar]
- 37. Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004; 159: 702–706. [DOI] [PubMed] [Google Scholar]
- 38. StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP, 2014. [Google Scholar]
- 39. Gil-Montalbán E, Martín-Ríos MD, Ortiz-Marrón H, et al. Incidencia de diabetes tipo 2 y factores asociados en la población adulta de la Comunidad de Madrid. Cohorte PREDIMERC. Rev Clin Esp 2015; 215: 495–502. [DOI] [PubMed] [Google Scholar]
- 40. Cowie CC, Rust KF, Ford ES, et al. Full accounting of diabetes and pre-diabetes in the US population in 1988–1994 and 2005–2006. Diab Care 2009; 32: 287–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Piccinelli M, Wilkinson G. Gender differences in depression. Critical review. Br J Psych 2000; 177: 486–492. [DOI] [PubMed] [Google Scholar]
- 42. Meng X, Brunet A, Turecki G, et al. Risk factor modifications and depression incidence: a 4-year longitudinal Canadian cohort of the montreal catchment area study. BMJ Open 2017; 7: e015156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kim SM, Jung JW, Park IW, et al. Gender differences in relations of smoking status, depression, and suicidality in Korea: findings from the Korea national health and nutrition examination survey 2008–2012. Psych Investig 2016; 13: 239–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Forlani C, Morri MAM, Ferrari B, et al. Prevalence and gender differences in late-life depression: a population-based study. Am J Geriatr Psych 2014; 22: 370–380. [DOI] [PubMed] [Google Scholar]
- 45. Njolstad I, Arnesen E, Lund-Larsen PG. Sex differences in risk factors of clinical diabetes mellitus in a general population: a 12-year follow-up of the Finnmark Study. AM J Epidemiol 1998; 147: 49–58. [DOI] [PubMed] [Google Scholar]
- 46. Meisinger C, Thorand B, Schneider A, et al. Sex differences in risk factors for incident type 2 diabetes mellitus: the MONICA Augsburg cohort study. Arch Intern Med 2002; 162: 82–89. [DOI] [PubMed] [Google Scholar]
- 47. Brancati FL, Kao WH, Folsom AR, et al. Incident type 2 diabetes mellitus in African American and white adults: the atherosclerosis risk in communities study. JAMA 2000; 283: 2253–2259. [DOI] [PubMed] [Google Scholar]
- 48. Chatterjee R, Brancati FL, Shafi T, et al. Non-traditional risk factors are important contributors to the racial disparity in diabetes risk: the atherosclerosis risk in communities study. J Gen Intern Med 2014; 29: 290–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Michael PB, Kiarri K, April PC, et al. Association of modifiable risk factors in young adulthood with racial disparity in incident type 2 diabetes during middle adulthood. JAMA 2017; 318: 2457–2465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Carnethon MR, Palaniappan LP, Burchfiel CM, et al. Serum insulin, obesity, and the incidence of type 2 diabetes in black and white adults: the atherosclerosis risk in communities study: 1987–1998. Diab Care 2002; 25: 1358–1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, STROBE_checklist_cohort_Chireh1 for Shared and unique risk factors for depression and diabetes mellitus in a longitudinal study, implications for prevention: an analysis of a longitudinal population sample aged ⩾45 years by Batholomew Chireh and Carl D’Arcy in Therapeutic Advances in Endocrinology and Metabolism