Abstract
Objective:
Family caregivers are the default caring personnel for terminal cancer patients. The characteristics, demographics, distribution, psychological burden, and socioeconomic standards differ between high- and low-income countries. We aimed to assess those factors and their direct reflection on both the patient and the caregiver.
Patients and Methods:
This is a comparative cross-sectional study for terminal cancer patients in the palliative care unit between the United Kingdom (UK) as a high-income community and Egypt as a low-income community. We assessed the different characteristics, demographics, living place, the degree of relevance, and the availability of caregivers.
Results:
We have recruited 216 patients from the UK and 117 patients from Egypt. Informal caregivers were available in 74.5% and 92.3% for these patients with a mean age of 71.5 (standard deviation [SD] 16) years and 50.9 (SD 15.18) years, respectively. There has been a statistically significant difference between the two countries’ caregivers in being married, family, and living in the same household (P < 0.0001).
Conclusion:
Low-income countries are more common to have an informal caregiver who is a family member of different degree of relevance. Caregivers in low-income settings tend to be younger, of the female gender, married, and living in the same household than in high-income ones.
Keywords: Cancer, caregivers, developing countries, income, palliative care, socioeconomic
INTRODUCTION
The modern palliative care movement started in higher-income countries where palliative care models were developed to meet the needs of patients and their families. Although the principles of palliative care are the same, the ideal palliative care models in lower-income countries may be different from that in higher-income ones due to many variables related to culture and resources. Among the factors that need to be considered when developing suitable palliative care models in lower-income settings are the availability of informal caregivers and the degree to which they are involved in the care of palliative care patients.
The prevalence of chronic illness in the world comes with evident fact, that one may be a caregiver to one of his family members at least once during his lifetime. Cancer is of no exception, thanks to the improvement of survival rates and the increasing dependence on outpatient settings to manage some cancer patients on chemo- or radiotherapy protocols. That's in addition to the shortages of health-care resources and personnel. All these factors make the family caregiver a cornerstone of the long-term program of managing cancer patients. However, who cares about those caregivers.
A strong positive relationship between the country income and the survival rate of certain cancers does exist.[1] Given that the proportion of cancer cases in developing countries is increasing and that two-thirds of cancer deaths in the world occur in these countries, a global call to action for improving cancer care in the developing countries is becoming essential.
This study aimed to identify the characteristics and availability of caregivers of terminally ill cancer patients presenting to the palliative care unit of a cancer center in a developing country like Egypt and compare them with those of a developed high-income country with a different culture like the United Kingdom (UK).
PATIENTS AND METHODS
This is a cross-sectional study which included all patients presenting to the palliative care unit at both Kasr Al-Ainy Centre of Clinical Oncology, Faculty of Medicine, Cairo University, Egypt, and the palliative care unit at Chelsea and Westminster Hospital, London, UK, during the period between May 2012 and November 2012.
Variables assessed for patients were as follows: age, gender, marital status, and primary cancer. Caregivers were assessed regarding their number, age, sex, relation to the patient, and living with the patient or not. The caregiver was defined as the person who conducted or coordinated the majority of the patient's home care needs.
Sample size calculation
Estimating availability of caregivers in high-income versus low-income country is 75% and 90%, respectively, and a minimum of 100 patients in each arm is needed to be able to reject the null hypothesis that the incidence between the two settings is equal with probability (power) 0.80. The Type I error probability associated with this test of this null hypothesis is 0.05.
Statistical methods
Statistical analyses of the data were conducted using small Stata 12.1 software for Windows (StataCorp LP, College Station, TX, USA). A comparison between the two cohorts was done using the Student's t-test for continuous data and Chi-square test for categorical data.
RESULTS
This study included informal caregivers for 216 patients with advanced cancer from a higher-income setting in the UK and 117 patients from a lower-income setting in Egypt who were seen by the palliative care team in either site. The most common cancers in the UK group were lung (19%), colon (11.5%), and pancreas (7.9%) cancer and in the Egypt group, breast (28.2%) and bladder (8.5%) cancer. There was a difference in the demographic characteristics of patients between Egypt and the UK [Table 1]. Patients in Egypt were significantly younger than patients in the UK (mean age = 50.9 [standard deviation (SD) =15.18] years and 71.5 [SD = 16] years, respectively; P < 0.0001) and were more likely to be married (83.8% vs. 50.3%, respectively; P < 0.0001).
Table 1.
Summary of characteristics of both populations of patients and their caregivers
| UK, n (%) | Egypt, n (%) | p | |
|---|---|---|---|
| Total patients | 216 | 117 | |
| Median age | 71.5 (20 - 100) | 50.9 (5-80) | <0.001 |
| Male/Female | 101/115 (1:1.13) | 55/62 (1:1.12) | |
| Marital status | 74 (34.2) | 98 (83.7) | <0.001 |
| Active treatment | 67 (31) | 37 (31.6) | |
| Hospice | 20 (9.3) | 0 | |
| Caregiver available | 161 (74.5) | 108 (92.3) | |
| No caregiver | 55 | 9 | <0.001 |
| Caregiver living with | 103 | 108 | <0.001 |
| Caregiver gender, M/F | 59/99 | 33/75 | |
| Caregiver relation* | |||
| Spouse | 66 (41) | 33 (30.5) | |
| 1st degree | 79 (49) | 84 (77.8) | |
| Non-Family | 13 (8) | 0 |
* Some patients have more than one caregiver
An informal caregiver was available in 92.3% of the cases from Egypt compared to 74.5% of the cases from the UK (P < 0.0001), with a mean age of 38.7 (SD = 13.9) years and 59.2 (SD = 16) years, all Egyptian informal caregivers were family members, meanwhile 8% of UK caregivers were nonfamily, and 9.3% of the UK cancer patients had paid care in a hospice, such facilities are rarely available in developing countries. In the Egyptian setting, 100% of informal caregivers were living with the patient compared to 64.6% in the UK setting (P < 0.0001). In total, 92% of Egyptian palliative care patients with cancer had an informal caregiver living with them. In comparison, 64.6% of palliative care patients with cancer from the UK had an informal caregiver living with them (P < 0.001). Table 2 shows the types of caregivers distributed in relation to the age of the cared patient. The Egyptian elderly patients were commonly cared by their offspring (65.7%), meanwhile the UK cancer patients were commonly cared by either offspring (33.9%), or spouse (26%), and in 27% of occasions there was no available caregiver for the UK cohort.
Table 2.
Types of caregivers distributed in relation to age of the cared patient
| Type of the caregiver | Patients ≤60 | Patients >60 | ||
|---|---|---|---|---|
| UK, n (%) total=53 | Egypt, n (%) total=82 | UK, n (%) total=163 | Egypt, n (%) total=35 | |
| Spouse | 21 (37%) | 26 (31.7) | 42 (26) | 7 (20) |
| Offspring | 2 (5.5%) | 27 (32.9) | 52 (33.9) | 23 (65.7) |
| Parent | 7 (9%) | 12 (14.6) | 1 (0.6) | 0 |
| Siblings | 8 (14.8%) | 10 (12.1) | 14 (9) | 3 (8.5) |
| others | 4 (7.5%) | 0 | 12 (7.4) | 0 |
| No caregiver available | 12 (22.2%) | 7 (8.5) | 41 (27) | 2 (5.7) |
DISCUSSION
With advanced medical care facilities, medical technologies, and aggressive treatments, cancer became more as a chronic illness with higher life expectancy.[2] Caregivers for terminal cancer patients are considered one of the most important rings of palliative care chain and quality of life enhancement[3] family caregiver are considered the default caregiver once a diagnosis of a terminal cancer is made, but many of them are not well-oriented to their role in the plan of management, emotional support, symptom relief, complication interval, and finally, the end-of-life place and preparation for “dying at home.”[4]
In 2010, a meta-analysis put some highlights on characteristics of caregivers among 29 studies that assessed interventions targeting family caregivers of cancer patients, but only one-third of these randomized controlled trials included advanced stage cancer patients.[5] Female gender and Caucasian race predominate 64% and 84%, respectively, with a mean age of 55 years. The interventions provided to caregivers were psychoeducational, skills training, and/or therapeutic counseling.
Communication between health-care providers, patients, and specifically caregivers has a key role in improving the quality of life for both patients and caregivers as they may suffer from psychological, social, financial, and mental health deterioration during the period of palliative therapy, such as lack of knowledge, loneliness, depression, anxiety, and sleep disorders.[6,7,8]
Many interventional programs have been offered for handling this point such as CSNAT,[7] CCP,[3] the booklet intervention,[9] CONNECT,[10] and interdisciplinary palliative care intervention[11] which proved their effectiveness in improving different aspects of caregivers life, psychologically, mentally, and socially.
Caregivers have different characteristics and distributions worldwide. Based on seven studies[8,10,12,13,14,15,16] conducted in different communities along with this one, they are mainly showing a high female to male ratio as outlined in Figure 1, the mean age is lesser in developing countries as shown in Figure 2, and most of the caregivers are partner/spouse as shown in Figure 3 ranging from 41% to 61% of the whole caregivers numbers.
Figure 1.
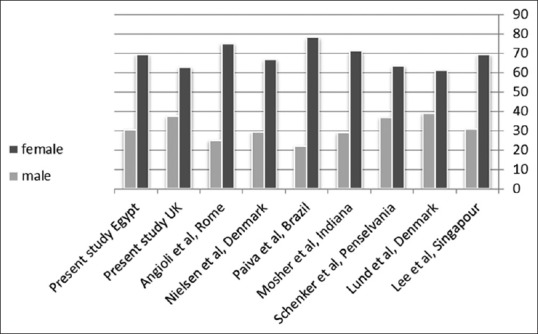
The high female: Male ratio among caregivers is evident worldwide
Figure 2.
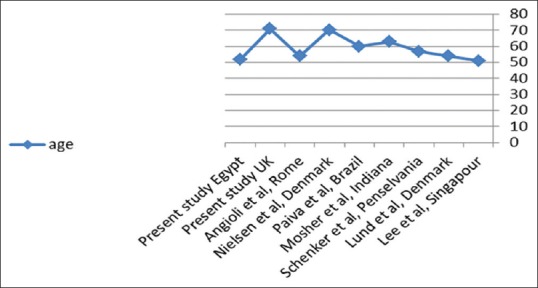
The mean age of caregivers across different studies along with the current one
Figure 3.
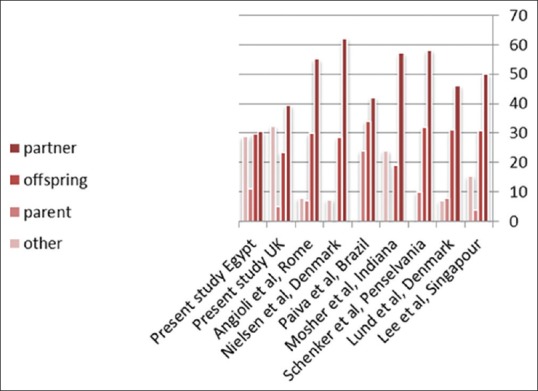
Diagram summarizes results from different studies on the type of caregivers that is in most cases the partner
In lower-income countries, it is expected that the caregiver is almost always a family member. However, a significant percentage of caregivers may be nonfamily in high-income countries, for example, in the present study, this percent was 8% in the UK cohort not to mention a significant portion living in a hospice. When comparing the pros and cons of family versus nonfamily caregivers, many points of conflict are raised: the family caregiver is ill-prepared, the costs of specialized caring facilities or personnel, cultural norms, and negative social and psychological impact. For instance, Lkhoyaali et al.[17] surveyed 150 family caregivers of elderly cancer patients in Morocco, a country that is not different from Egypt regarding culture and society norms and socioeconomic standards. They have found that family caregivers become less social, spouses develop more fatigue and insomnia, and female partners, in particular, suffer more due to more depression. This is in accordance with several other studies conducted in higher-income societies.[18,19] However, this study pointed out that the cultural norms in such societies disgrace and dishonor the act of putting a parent in a hospice or nursing facility. Another conflicting point is the distance of the caregiver. Is it favorable that caregiver being lived in the same household with the patient or not? Caring for a cancer patient consumes 8.3 h/day,[20] sure this time is cut from work hours of caregiver with negative financial impact.
CONCLUSION
The results of this study suggest that there are significant differences between higher-income and lower-income settings regarding the availability and characteristics of informal caregivers for palliative care patients with cancer. The palliative care models developed in higher-income countries may not be “universally” suitable for lower-income countries. Future research is essential to develop palliative care delivery models suitable for the culture and resources in Egypt and other lower-income settings. In lower-setting, the caregiver tends to be an ill-prepared family member that in most occasions lives with the patient.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Farmer P, Frenk J, Knaul FM, Shulman LN, Alleyne G, Armstrong L, et al. Expansion of cancer care and control in countries of low and middle income: A call to action. Lancet. 2010;376:1186–93. doi: 10.1016/S0140-6736(10)61152-X. [DOI] [PubMed] [Google Scholar]
- 2.Ammari AB, Hendriksen C, Rydahl-Hansen S. Recruitment and reasons for non-participation in a family-coping-orientated palliative home care trial (FamCope) J Psychosoc Oncol. 2015;33:655–74. doi: 10.1080/07347332.2015.1082168. [DOI] [PubMed] [Google Scholar]
- 3.Leow M, Chan S, Chan M. A pilot randomized, controlled trial of the effectiveness of a psychoeducational intervention on family caregivers of patients with advanced cancer. Oncol Nurs Forum. 2015;42:E63–72. doi: 10.1188/15.ONF.E63-E72. [DOI] [PubMed] [Google Scholar]
- 4.Kinoshita H, Maeda I, Morita T, Miyashita M, Yamagishi A, Shirahige Y, et al. Place of death and the differences in patient quality of death and dying and caregiver burden. J Clin Oncol. 2015;33:357–63. doi: 10.1200/JCO.2014.55.7355. [DOI] [PubMed] [Google Scholar]
- 5.Northouse LL, Katapodi MC, Song L, Zhang L, Mood DW. Interventions with family caregivers of cancer patients: Meta-analysis of randomized trials. CA Cancer J Clin. 2010;60:317–39. doi: 10.3322/caac.20081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caswell G, Pollock K, Harwood R, Porock D. Communication between family carers and health professionals about end-of-life care for older people in the acute hospital setting: A qualitative study. BMC Palliat Care. 2015;14:35. doi: 10.1186/s12904-015-0032-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ewing G, Austin L, Diffin J, Grande G. Developing a person-centred approach to carer assessment and support. Br J Community Nurs. 2015;20:580–4. doi: 10.12968/bjcn.2015.20.12.580. [DOI] [PubMed] [Google Scholar]
- 8.Nielsen MK, Neergaard MA, Jensen AB, Bro F, Guldin MB. Psychological distress, health, and socio-economic factors in caregivers of terminally ill patients: A nationwide population-based cohort study. Support Care Cancer. 2016;24:3057–67. doi: 10.1007/s00520-016-3120-7. [DOI] [PubMed] [Google Scholar]
- 9.Luker K, Cooke M, Dunn L, Lloyd-Williams M, Pilling M, Todd C. Development and evaluation of an intervention to support family caregivers of people with cancer to provide home-based care at the end of life: A feasibility study. Eur J Oncol Nurs. 2015;19:154–61. doi: 10.1016/j.ejon.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 10.Schenker Y, White D, Rosenzweig M, Chu E, Moore C, Ellis P, et al. Care management by oncology nurses to address palliative care needs: A pilot trial to assess feasibility, acceptability, and perceived effectiveness of the CONNECT intervention. J Palliat Med. 2015;18:232–40. doi: 10.1089/jpm.2014.0325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sun V, Grant M, Koczywas M, Freeman B, Zachariah F, Fujinami R, et al. Effectiveness of an interdisciplinary palliative care intervention for family caregivers in lung cancer. Cancer. 2015;121:3737–45. doi: 10.1002/cncr.29567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Angioli R, Capriglione S, Aloisi A, Miranda A, de Cicco Nardone C, Terranova C, et al. Economic impact among family caregivers of patients with advanced ovarian cancer. Int J Gynecol Cancer. 2015;25:1541–6. doi: 10.1097/IGC.0000000000000512. [DOI] [PubMed] [Google Scholar]
- 13.Lee GL, Ow MY, Akhileswaran R, Pang GS, Fan GK, Goh BH, et al. Quality of life domains important and relevant to family caregivers of advanced cancer patients in an Asian population: A qualitative study. Qual Life Res. 2015;24:817–28. doi: 10.1007/s11136-014-0832-3. [DOI] [PubMed] [Google Scholar]
- 14.Lund L, Ross L, Petersen MA, Groenvold M. The interaction between informal cancer caregivers and health care professionals: A survey of caregivers’ experiences of problems and unmet needs. Support Care Cancer. 2015;23:1719–33. doi: 10.1007/s00520-014-2529-0. [DOI] [PubMed] [Google Scholar]
- 15.Mosher CE, Ott MA, Hanna N, Jalal SI, Champion VL. Coping with physical and psychological symptoms: A qualitative study of advanced lung cancer patients and their family caregivers. Support Care Cancer. 2015;23:2053–60. doi: 10.1007/s00520-014-2566-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paiva BS, de Carvalho AL, Kolcaba K, Paiva CE. Validation of the holistic comfort questionnaire-caregiver in portuguese-Brazil in a cohort of informal caregivers of palliative care cancer patients. Support Care Cancer. 2015;23:343–51. doi: 10.1007/s00520-014-2370-5. [DOI] [PubMed] [Google Scholar]
- 17.Lkhoyaali S, El Haj MA, El Omrani F, Layachi M, Ismaili N, Mrabti H, et al. The burden among family caregivers of elderly cancer patients: Prospective study in a Moroccan population. BMC Res Notes. 2015;8:347. doi: 10.1186/s13104-015-1307-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mor V, Allen S, Malin M. The psychosocial impact of cancer on older versus younger patients and their families. Cancer. 1994;74:2118–27. doi: 10.1002/1097-0142(19941001)74:7+<2118::aid-cncr2820741720>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 19.Deckx L, van Abbema DL, van den Akker M, van den Broeke C, van Driel M, Bulens P, et al. A cohort study on the evolution of psychosocial problems in older patients with breast or colorectal cancer: Comparison with younger cancer patients and older primary care patients without cancer. BMC Geriatr. 2015;15:79. doi: 10.1186/s12877-015-0071-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Deshields TL, Rihanek A, Potter P, Zhang Q, Kuhrik M, Kuhrik N, et al. Psychosocial aspects of caregiving: Perceptions of cancer patients and family caregivers. Support Care Cancer. 2012;20:349–56. doi: 10.1007/s00520-011-1092-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


