Abstract
Introduction:
The growing number of older adults with multiple needs increases the pressure to reform existing healthcare systems. Integrated care may be part of such reforms. The aim of this systematic review was to identify important patient-related outcomes of integrated care provided to older adults.
Methods:
A systematic search of 5 databases to identify studies comprising older adults assessing hospital admission, length of hospital stay, hospital readmission, patient satisfaction and mortality in integrated care settings. Retrieved literature was analysed employing a narrative synthesis.
Results:
Twelve studies were included (2 randomised controlled trials, 7 quasi-experimental design, 2 comparison studies, 1 survey evaluation). Five studies investigated patient satisfaction, 9 hospital admission, 7 length of stay, 3 readmission and 5 mortality. Findings show that integrated care tends to have a positive impact on hospital admission rates, some positive impact on length of stay and possibly also on readmission and patient satisfaction but not on mortality.
Conclusions:
Integrated care may reduce hospital admission rates and lengths of hospital stay. However due to lack of robust findings, the effectiveness of integrated care on patient-related outcomes in later life remain largely unknown. Further research is needed to establish the effect of integrated care on these patient-related outcomes.
Prospero registration number:
CRD42018110491.
Keywords: integrated care, hospital admission, length of hospital stay, hospital readmission, patient satisfaction, mortality
Introduction
Ageing populations and the need of changes to care systems
Worldwide, the population of older people is increasing [1]. Older people’s health and social care needs are often complex requiring several health and social care providers and involves multiple transitions between care settings. These care transitions tend to negatively affect the continuity of care including lack of communication between care providers, errors in medication lists and insufficient quality of discharge protocols [3,4,5]. Subsequently, managing the health and social care of older people has become a major challenge [6]. The World Health Organization (WHO) therefore advocates for major reforms to health and social care systems [7] where integration and coordination between health and social care providers is seen as essential to address the needs of the older population [8].
Integrated care
Integrated care seeks to better coordinate health and social care around the individual’s needs with a commitment to improve the quality of care and overcome fragmented care through ongoing co-productive partnerships [2]. Integrated care can take many different forms. It may, for instance, take place between providers operating at the same level (horizontal integration) (e.g. bringing together acute hospitals) or between providers working at different levels (vertical integration) (e.g. linking hospitals with general practices and community care) [9]. Typologies of integrated care include clinical, organisational and systemic integration. Clinical integration refers to processes within or across professions through use of shared guidelines and protocols, organisational integration refers to co-ordinated provider networks or contracts that bring together separate organisations, and systemic integration involves coherence of rules and policies at all organisational levels. All degrees of integration are concerned with the processes of bringing organisations and professionals together with the purpose of improving the outcomes for patients such as patients’ experience and the quality of care provided [10].
Health and social care for older people in Sweden
This systematic review is part of a larger research project on integrated care in Stockholm, Sweden, investigating efficient ways of organising health and social care services for older people with complex health problems and severe needs. Sweden ranks high in cross-country comparisons of care for older people [11]. However, in recent years, Sweden has been criticised for inadequate coordination between hospitals, primary care and social care [12]. The Swedish health and social care system is highly decentralised [13]. The healthcare and the social services are managed separately and limited joint work has resulted in inadequate coordination between hospitals, primary care and social care services. Competition and privatisation in the healthcare sector including implementation of patient choice of primary care and social care providers has gradually been introduced in response to criticism for lack of cost control and inefficiency. However, it has turned out that the marketization of the healthcare has also made it more difficult to coordinate the care for those with complex care needs [12].
Since the Community Care Reform in the early 1990s, the number of hospital beds has more than halved and Sweden has now the lowest hospital bed rate per capita in the European Union [14]. In turn, the reduced number of hospital beds has led to shorter average length of stay in hospitals. Since year 2000, a third of the beds in municipal institutional care have been removed and replaced by municipal home help services, which is significantly cheaper [15]. Consequently, an increased number of older people with complex health problems including cognitive impairments are dependent on help to carry out everyday life activities in their homes. However, the reduction in the number of hospital beds and beds in municipal institutional care has not been compensated for by a corresponding increase in home help services. Not only have these structural changes increased the pressure on the municipal home help services but also on primary health care, and resulted in increased numbers of emergency department visits [13]. Therefore, for the Swedish context, hospital admission, length of stay and hospital readmission are outcomes of particular interest to be assessed against integrated care or in relation to it.
Previous studies on patient-related outcomes of integrated care
Earlier studies assessing patient-related outcomes, typically hospitalisation and lengths of hospital stay, in settings consisting of at least a few components of integrated care, have shown mixed results [16,17,18,19,20,21,22,23,24,25,26,27,28,29]. For instance, some studies have reported positive trends on hospitalisation, lengths of stay and hospital readmission [16,17,18,19,20,22,28]. However, only a few of these studies reported significant improvements in such outcomes [17,19,20]. Similarly, conflicting findings have also been reported in previous studies examining patient-satisfaction [16,17,18,19,20,21,22,23,24,25,26,27,28,30,31,32] and mortality [16,17,19,20,33,34,26,31,29,35], of which some studies have indicated positive trends [16,17,33,34,31,32,35], however effects remain unclear. Further, despite multi-morbidity (having two or more chronic conditions) becoming progressively more common with advanced age [36], this growing body of evidence mainly comes from studies that have evaluated disease-specific interventions. These studies have furthermore used different definitions and various components of integrated care [24,37,38,27]. Reviewing existing research in older adults with multimorbidity using a specific and well-established definition of integrated care has the potential to demonstrate patient-related outcomes of particular importance to integrated care.
Study rationale
Recent literature has concluded that to increase the effectiveness of integrated care, care of patients with complex needs should be targeted [35]. Thus, a systematic review of existing research on older adults with multimorbidity could help inform future models of integrated care. Further, whilst many previous studies on integrated care have examined a single patient-related outcome such as hospitalisation, fewer studies have considered investigating more than one patient-related outcome [39]. This systematic review focuses on a range of patient-related outcomes including hospital admission, length of hospital stay, hospital readmission, mortality and patient-satisfaction. Hospital admission and length of stay are outcomes of particular importance as they account for the majority of overall healthcare costs and constitute the starting point of further decline in health in older age [40]. Assessing patient-satisfaction is important to understand the care consumers’ satisfaction with the medical services provided and to identify the needs and expectations of the healthcare system [30]. Mortality is of interest to assess as it is one of the strongest indicators of treatment efficacy and considered the hardest outcome criterion conceivable [41].
A systematic review focusing on an array of patient-related outcomes has the potential to become a resource for current work and future research highlighting patient-related outcomes in integrated care settings of particular interest in the ageing population. The outcomes assessed in the current review will further help forming the knowledge base of the extended research project of which this study is part of.
Purpose
The aim of this systematic review is to investigate a range of patient-related outcomes to identify if any of them may be particularly important when assessing integrated care for older people with multi-morbidity. Patient-related outcomes explored in this review include patient satisfaction, hospital admission, length of hospital stay, hospital readmission and mortality.
Conceptual framework
A challenge when studying integrated care is the lack of a universal definition of the concept and the many terms used in the literature [42]. To make sure that the studies included in the review were as comparable as possible, we have to the largest extent possible used the following definition of integrated care by Kodner and Spreeuwenberg (2002) [43] “Integration is a coherent set of methods and models on the funding, administrative, organisational, service delivery and clinical levels designed to create connectivity, alignment and collaboration within and between the cure and care sectors. The goal of these methods and models is to enhance quality of care and quality of life, consumer satisfaction and system efficiency for patients with complex, long-term problems cutting across multiple services, providers and settings. The result of such multi-pronged efforts to promote integration for the benefit of these special patients groups is integrated care.” This definition’s goal of improving the quality of healthcare services is further reflected in Donabedian’s framework on quality of care which uses ‘outcome’ as an approach to assess medical care. This review focuses on patient-related outcomes and according to Donabedian, there are many advantages using patient-related outcomes to assess the quality of care as they tend to be measurable (e.g. length of stay in hospital) and precise (e.g. mortality). However Donabedian’s framework also recognises that other factors than medical care such as technology and time may influence the outcomes assessed [44]. The outcome approach of Donabedian’s framework has been applied to the analysis of the findings of this review in the Discussion section below.
Methods
Search strategy
A systematic search of English language literature published between 1st January 1995 and 10th October 2018 in the following 5 electronic databases was undertaken: MEDLINE, EMBASE, Cochrane Library, Web of Science Core Collection and Ageline (EBSCO). Restricting the literature search to 1995 and onwards was based on a bibliometric analysis of literature about integrated care which generated only a small number of studies published before 1995. Key search terms were developed by the research team and included ageing, integrated, care, hospitalisation, admission, readmission, length of stay, satisfaction and mortality. The search terms used are outlined in Appendix A. The protocol has been registered with Prospero (registration number CRD42018110491).
Eligibility criteria
In this paper, integrated care takes place on either an organisational level e.g. integration between health organisations and social care organisations, or on a systemic level i.e. the full spectrum of services including planning, financing and purchasing is integrated across the entire (or almost entire) health and social care sector [45].
Inclusion and exclusion criteria for considering studies in this review are summarised in Table 1. Studies included were of quantitative, qualitative and mixed-method design undertaken on an organisational or systemic level of integration targeting older people providing objective data on at least one of the following patient-oriented outcomes: mortality; hospital admission; length of hospital stay; hospital readmission; or subjective data on patient satisfaction. For intervention studies, the intervention group had to be compared with a control group receiving standard (non-integrated) care or with baseline measures of the intervention group. The intervention had to consist of pooled recourses (financial or human) on healthcare and social care. Interventions consisting of only multidisciplinary team, care co-ordination and care planning contents were excluded. Intervention studies addressing a single medical disease were also excluded. Due to large contextual differences between health care systems in low-, middle- and high-income countries only studies of integrated care in high income settings, based on the World Bank Groups list of high income countries for 2017, were included in this review. Studies were also excluded if no abstract was available or the study was a review of studies.
Table 1.
Study inclusion and exclusion criteria.
| Population | Older adults |
|---|---|
| Intervention | Inclusion: Organisational or systemic level of integration; Exclusion: interventions not consisting of pooled resources, interventions for hospitalised patients, interventions focusing on a single medical disease |
| Comparisons of interest | Comparison of no intervention i.e. usual care or comparison with baseline measures of the intervention group; Exclusion: Studies with no comparison |
| Outcomes | Any objective measure of hospital admission, length of hospital stay, hospital readmission, mortality, and subjective measure of patient satisfaction |
| Type of study | Inclusion: studies of any designs published between January 1995 to October 2018 written in English; Exclusion: Studies with no original data e.g. reviews, studies without an abstract |
Study selection and critical appraisal
References retrieved through the systematic searches were managed using Endnote X7 reference management software. Duplicates were removed and the remaining references were independently screened for eligibility by two researchers (FB and AL). Any disagreements were resolved through discussion between reviewers and with a third researcher (JA). Studies meeting the eligibility criteria were assessed for quality using the Critical Appraisal Skills Programme (CASP).
Data extraction, assessment of risk of bias and synthesis
The data were extracted and organised according to study outcome (patient satisfaction, hospital admission, length of stay, readmission and mortality) and level of health care integration (organisational or systemic) using a standardised data extraction form. The studies included were assessed for risk of biases from six sources (selection, performance, detection, attrition, reporting, conflict of interest) including interwoven risk of bias using relevant checklists for randomised controlled trials, observational studies and qualitative studies developed and provided by the Swedish Agency for Health Technology Assessment and Assessment of Social Services [46,47,48]. The studies were rated low, moderate or high on each of the six sources of bias and the ratings allowed for an interwoven risk of bias for each study. A narrative synthesis enabling handling a wide range of evidence from quantitative and qualitative research was used to compile the results of this review.
Results
Results of the literature search
A flowchart of the literature screening process is outlined in Figure 1. The literature search yielded a total of 6788 studies. After having removed duplicates the remaining 4734 studies were screened for eligibility of which 109 studies were considered potentially eligible and read in full text. Studies not meeting the eligibility criteria (n = 95) were excluded. The remaining 14 articles underwent CASP quality assessment. Results of the quality assessment of 14 studies are shown in Appendix B. Six of the studies were classified as having low risk of bias and five studies had a moderate risk of bias. Two studies were considered to have a high risk of bias and consequently excluded, resulting in a total of 12 studies included in the review.
Figure 1.
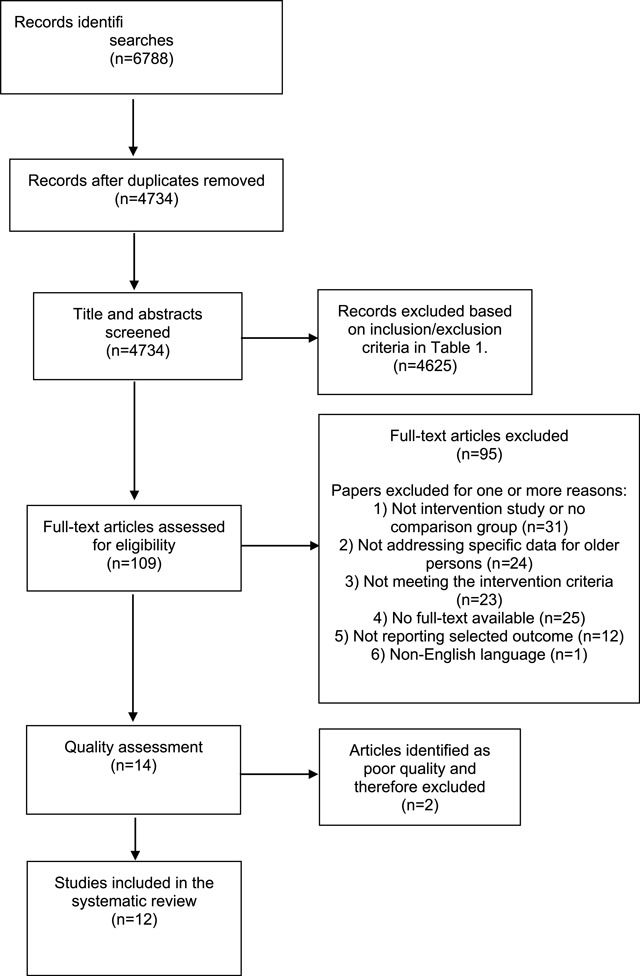
Study selection flowchart.
Description of the studies identified
The characteristics of the 12 studies included in this review are presented in Table 2. Nine studies were of quasi-experimental design, of which seven had concurrent control group, two studies were randomised controlled trials (RCTs), two were observational studies and one was of qualitative design. Four of the studies evaluated the impact on integrated care on a systemic level and eight studies on an organisational level of integration. Half of the studies were undertaken in North American and the remaining half in Western Europe.
Table 2.
Characteristics of studies included in this systematic review.
| Author, year | Country | Study design | Study subjects | Length of follow-up | Integrated care programme | Outcomes reported |
|---|---|---|---|---|---|---|
| Atherly et al. 2004 | USA | survey | n = 402 community-dwellers; n = 235 enrolled to the Program for All-Inclusive Care of the Elderly (PACE) and n = 167 non-PACE community-dwellers | 18 months | PACE (The Program for All-Inclusive Care of the Elderly) involves comprehensive integration of medical and social services and care including care planning with family members. | Patient satisfaction |
| Beland et al. 2006 | Canada | RCT | n = 1297 community-dwellers aged >64 years with moderate or severe functional problems (assessed using the Functional Autonomy Measurement System) of which n = 606 assigned to SIPA and n = 624 assigned to the usual services available | 22 months | SIPA (System of Integrated Care for Older Persons) a publicly managed and funded system of community-based multidisciplinary teams with full clinical responsibility for delivering integrated care through the provision of community health and social services and the coordination of hospital and nursing home care. | Hospital admission, patient satisfaction, mortality |
| Bernabei et al. 1998 | Italy | RCT | n = 200 community-dwellers aged ≥65 years with frailty based on their physical, mental and cognitive health identified through existing home health services or home assistance programmes; n = 100 intervention and n = 100 controls who received care as usual | 12 months | Intervention involving case management and care planning by the community geriatric evaluation unit consisting of 2 case managers (performing assessments, monitoring the provision of services), 1 social worker, 1 geriatrician, nurses and general practitioners. | Hospital admission, length of stay, mortality |
| Brown et al. 2003 | UK | mixed-methods | n = 393 community-dwellers aged >64 years; n = 195 integrated care, n = 198 care as usual | 18 months | Joint working primary and social care consisting of two co-located integrated teams, one based in a general practice and the other in a health centre attached to a general practice. | Patient satisfaction |
| Ham et al. 2003 | USA, England | comparative study | Data from medical records presented in numbers per 100 000 population consisting of people aged ≥65 years | n/a | Kaiser-Permanente: a medical care program that involves voluntary enrolment, prepayment for services, comprehensive benefits, preventive medical care, integrated hospital-based health care facilities, and provision of physician services through group medical practice vs NHS (National Health Service): the universal and free healthcare programme in England. | Hospital admission, length of stay |
| Hebert et al. 2010 | Canada | quasi-experimental | n = 920 community-dwellers aged ≥75 years at risk of functional decline (assessed using the Functional Autonomy Measurement System); n = 501 assigned to PRISMA and n = 419 controls receiving care as usual | 4 years | PRISMA (Program of Research to Integrate Services for the Maintenance of Autonomy) an embedded model with a single entry point using all the public, private, or voluntary health and social service organisations involved in caring for older people in a given area where every organisation keeps its own structure but agrees to participate under an umbrella system and to adapt its operations and resources to the agreed requirements and processes. Case manager included in PRISMA could be any clinical healthcare professional and is responsible for conducting a thorough assessment of the patient’s needs, planning the required services, arranging patient admission to these services, etc. | Hospital admission, patient satisfaction, length of stay, readmission, mortality |
| Landi et al. 1999 | Italy | quasi-experimental | n = 115 community-dwellers, mean age 77.5 years (+/– 11.7) assessed pre/post intervention | 6 months | Case managers and the geriatric evaluation unit designed and implemented individualised care plans in agreement with general practitioners, and determined the services for which patients were eligible. The approved services were then provided by multidisciplinary teams, with the case manager coordinating the delivery and facilitating the integration process between social and healthcare professionals. | Hospital admission, length of stay |
| Landi et al. 2001 | Italy | quasi-experimental | n = 1204 community-dwellers, mean age 77.4 years (+/– 9.7) assessed pre/post intervention | 12 months | National model that integrates all the community-based services provided either by the health agency or by the municipality into one “single enter” centre. | Hospital admission, length of stay |
| Looman et al. 2014 | The Netherlands | quasi-experimental | n = 417 community-dwellers aged ≥75 years who were frail (assessed with the Groningen Frailty Indicator); n = 205 assigned to WICM and n = 212 received care as usual | 3 months | WICM (Walcheren Integrated Care Model) includes a single entry point system through the general practice known for patient data being shared across teams and focus on prevention. Case managers organise admittance to the required services, the planning and co-ordination of care delivery and periodical evaluation and monitoring of the treatment plan in cooperation with multidisciplinary teams. | Patient satisfaction |
| Schiotz et al. 2011 | USA, Denmark | comparison study | Data from medical records of people aged ≥65 years with one or more of the following 5 chronic conditions: angina, heart failure, COPD, hypertension and diabetes. | n/a | Kaiser-Permanente: a medical care programme that involves voluntary enrolment, prepayment for services, comprehensive benefits, preventive medical care, integrated hospital-based health care facilities, and provision of physician services through group medical practice vs Danish Healthcare system (DHS): the universal and free healthcare programme in Denmark. | Hospital admission, length of stay, readmission, mortality |
| de Stampa et al. 2014 | France | quasi-experimental | n = 428 community-dwellers aged >64 years classified as very frail (assessed using Katz ADL, Lawton IADL, the cognitive performance scale, the depression rating scale, etc.); n = 105 assigned to COPA intervention and n = 323 received care as usual | 12 months | COPA (Coordination of care for the elderly) single entry point system connecting primary care and hospital care, home-based geriatric assessment, individualised care plan, interdisciplinary protocols, case manager organises planned hospital visits. | Hospital admission |
| Tourigny et al. 2004 | Canada | quasi-experimental | n = 482 people aged ≥75 years (2/3 living in own home, 1/3 in private seniors’ residence) reporting functional decline (based on Katz ADL, Lawton IADL, etc.); n = 272 in geographical area where ISD is provided and n = 210 in different geographical area where there was no ISD network | 5 years | ISD (Integrated service delivery) network of health and social services is a single entry service designed to manage both home and institutional care that involves exchange of clinical information across institutions. The service is run by case managers who develop individual service plans for enrolled patients. | Hospital admission, length of stay, readmission, mortality |
Findings on the outcome measures
Table 3 presents a summary of the findings for each study. A summary of studies related to each of the patient-related outcomes is presented in Figure 2.
Table 3.
Summary of findings on patient-related outcomes of integrated care comprising older adults.
| Author, year | Level of integration | Patient satisfaction | Hospital admission | Length of stay | Readmission | Mortality |
|---|---|---|---|---|---|---|
| Atherly et al. 2004 | Systemic | Significantly greater satisfaction in level of concern and attentiveness displayed by staff (p < 0.01) and patient’s decisions about their care (p < 0.01) but not access to medical specialists (p = 0.54) among PACE-enrolled participants compared to non-participants completing the 23-item PACE satisfaction survey. | n/a | n/a | n/a | n/a |
| Beland et al. 2006 | Systemic | No significant difference between intervention and control groups using the 8-item Client Satisfaction Questionnaire. No effect size reported. | No significant difference between intervention and control groups. No effect size reported. | n/a | n/a | No significant difference between intervention and control groups. No effect size reported. |
| Bernabei et al. 1998 | Organisational | n/a | Significantly reduced risk in the intervention group. HR: 0.74 95% CI 0.56–0.97, p < 0.05 | n/a | n/a | No significant difference between intervention and control group. HR 0.99 95% CI 0.89–1.09 |
| Brown et al. 2003 | Organisational | No major differences between intervention and control group regarding their satisfaction with the services received – question asked in qualitative interview. No effect size reported. | n/a | n/a | n/a | n/a |
| Ham et al. 2003 | Systemic | n/a | Lower admission rates in KP compared to NHS in 6 of 11 common causes. No effect size reported. | Shorter stay for patients in KP compared to NHS no matter reason for admission. No effect size reported. | n/a | n/a |
| Hebert et al. 2010 | Organisational | Significant improvements in satisfaction with services, delivery of care, and organisation of care and services (all p < 0.001) in intervention group and no changes in control group using the 26-item Health Care Satisfaction Questionnaire | No significant differences in admissions rates in intervention group (rates remained the same) and control group (rates increased) p = 0.578 | No difference observed between intervention and control group. No effect size reported. | No difference observed between intervention and control group. No effect size reported. | No difference observed between intervention and control group p > 0.05 |
| Landi et al. 1999 | Organisational | n/a | Significant decrease in admission rates post intervention compared to pre intervention p < 0.001 | Significantly shorter stays post intervention compared to pre intervention p < 0.01 | n/a | n/a |
| Landi et al. 2001 | Organisational | n/a | Significant decrease in admission rates post intervention compared to pre intervention p < 0.001 | Significantly shorter stays post intervention compared to pre intervention p = 0.01 | n/a | n/a |
| Looman et al. 2014 | Organisational | No significant difference between intervention and control group using study-specific consumer quality index with questions on client-orientation, knowledge of care needs, joint decision making, attention to social-emotional aspects, information, and approach | n/a | n/a | n/a | n/a |
| Schiotz et al. 2011 | Systemic | n/a | Significantly higher admission rates in DHS compared to KP: 5.21 hospitalisations/100 persons 95% CI 5.17–5.26 in DHS and 2.02 hospitalisations/100 persons 95% CI 1.98–2.06 in KP | No significant difference between DHS and KP (4.08 days in DHS, 3.91 days in KP) | Significantly higher readmission rates in DHS compared to KP (OR 1.10 95% CI 1.03–1.16) | No significant difference between DHS and KP (effect size reported for each condition, no effect size on overall findings) |
| de Stampa et al. 2014 | Organisational | n/a | Significantly reduced risk of having at least one unplanned hospitalisation in the intervention group. OR: 0.39 95% CI 0.16–0.98 | n/a | n/a | n/a |
| Tourigny et al. 2004 | Organisational | n/a | No significant difference between intervention and control group p = 0.11 | No significant difference in average hospitalisation duration between intervention and control group p = 0.28 | No significant difference between intervention and control group p = 0.17 | No significant difference between intervention and control group p = 0.37 |
Figure 2.
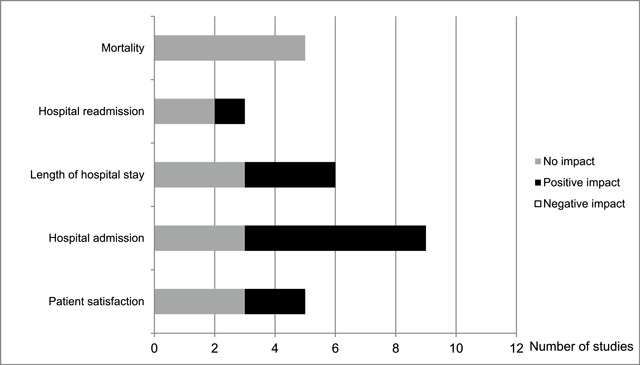
Summary of studies related to each of the patient-related outcomes assessed.
Patient satisfaction
Five of the 12 studies included in this review examined how satisfied patients were with the healthcare provided. At 4-year follow-up, Hebert et al. (2010) [49] assessed satisfaction using the 26-item Health Care Satisfaction Questionnaire showing significant improvements in satisfaction with services, delivery of care, and organisation of care in the intervention group compared to the control group. A 24-item survey developed to measure satisfaction in the Program for All-Inclusive Care of the Elderly (PACE) reported patient satisfaction in the form of level of concern and attentiveness displayed by staff, and patient’s decisions about their care, but not in terms of access to medical specialists 18 months after the intervention was introduced [50]. Three studies using different assessment tools (a self-constructed consumer quality index, interview questionnaire and the 8-item Client Satisfaction Questionnaire, respectively) and different length in follow-up (3 months, 18 months and 22 months, respectively) did not report any differences in patient satisfaction with the healthcare provided [51,52,38].
Hospital admission
Nine studies reported on hospital admission rates. Two Italian studies observed lower hospital admission rates after the implementation of an individualised integrated home care plan based on a geriatric assessment [53] and after implementation of a “single enter” health and social care centre providing all community-based services available [54], respectively. Similarly, a 12-month intervention study conducted in France observed a significant decline in hospital admission rates [55]. Studies comparing large-scale healthcare programmes showed that the national Danish Healthcare programme, a universal and free of charge care system, has 2.5 times higher rates of hospital admission compared to Kaiser Permanente, a medical programme that involves voluntary enrolment, prepayment for services and provides integrated care [56]. However, when comparing Kaiser-Permanente with the English National Health Service, which is universal and free of charge, similar patterns of hospital admission were reported in both systems [57].
A Canadian intervention study using a 4-year follow-up reported that the number of hospital admissions remained the same in the intervention group but increased in the control group over time albeit not at a statistically significant level [49]. Another two Canadian studies reported no significant differences in hospital admission between the intervention and control groups [58,52].
Length of hospital stay
Compared to Kaiser Permanente, the length of stay in hospital was longer in both the Danish Healthcare system [56] and the English National Health Service [57]. The difference observed between the Danish Healthcare system and Kaiser Permanente was however not significant. Some intervention studies reported that compared to the control group, participants in the intervention group stayed fewer number of days in the first 6 months [53] and 12 months [54] after the study was implemented. Contrary, studies with longer follow-up reported no difference between the intervention and control groups after 4 years [49] and 5 years [58], respectively.
Patient readmission
Only three of the studies reported on patient readmission to the emergency department after initial hospital admission. Shiotz et al. (2011) [56] reported a small significant difference between Kaiser Permanente and the Danish Healthcare system with higher rates of readmission in Denmark. Tourigney et al. (2004) [58] observed that the number of return visits to the emergency department within 10 days of a first visit was lower in the intervention group compared to the control group but the findings were not statistically significant. Similarly, no significant difference in readmission was observed in the intervention study by Hebert et al. (2010) [49].
Mortality
Nearly half of the studies (n = 5) examined mortality as an outcome [58,52,49,56]. None of the studies reported significant changes in mortality rates.
Discussion
This review has reported on a range of patient-related outcomes assessed in previous studies on integrated care provided to older adults. The findings suggest that integrated care may have a positive impact on hospital admission rates, some positive impact on length of stay and possibly also on patient satisfaction and readmission. Integrated care did not have an impact (positive or negative) on mortality. None of the studies reported integrated care having a negative impact on any of the outcomes assessed.
The positive impact of integrated care on hospital admissions and length of hospital stay is supported by a recent umbrella review of systematic reviews on hospital outcomes in integrated care for the general population [27]. In the umbrella review, 11 of 21 studies reported significantly reduced hospital admissions of which 4 out of 5 intervention studies focused on care of a chronic condition such as heart disease. In our systematic review, apart from the 2 studies that compared hospital admissions in national health programmes [57,56], the remaining 4 intervention studies demonstrating a decline in hospital admissions either involved case management [59,53] or a single entry point system [54,55]. However, no firm conclusions of the impact of case management and single entry point system can be drawn based on these components as 2 other studies in our systematic review using a single entry point system reported no significant reduction in hospital admission rates [58,49]. Besides single entry point systems, case management has previously also shown to be largely ineffective in reducing hospital admission rates [27]. A recent systematic review on complex healthcare interventions targeting older people has concluded that understanding the context including existing routines and the needs of the staff, and having knowledge of the target population are essential to demonstrate effectiveness of the healthcare intervention [60]. Hospital admission rates and length of hospital stay are largely financially driven outcomes [40], and may therefore primarily demonstrate an effect in structural interventions that involve reallocation of funding such as the in Kaiser Permanente [57,56]. Speculatively, time to follow-up may also influence the outcome as studies that showed a reduction in hospital admission rates had a follow-up of 12 months or less [59,53,54,55], whereas studies with a follow-up of 22 months or longer did not report a reduction [58,52,49]. Restricting the eligibility criteria to non-specific conditions may further have influenced this finding as reductions in hospital admissions have been found to be substantially greater in condition-specific admission compared to all-cause admissions [27].
The authors of the recent umbrella review on hospital outcomes in integrated care further reported that length of stay was the outcome most likely to improve with 9 out of 16 reviews reporting positive associations [27]. Nevertheless, the authors reported that gains were often modest, in some studies by as little as 1.5–2 days. Reducing the number of days in acute hospital is essential as prolonged stay increases the risk of hospital-acquired infections and disrupts patient flow due to bed shortages [61]. Thus, in view of the risks of staying in hospital, even a small reduction in length of hospital stay may be beneficial [62]. However, shortening the length of stay to achieve higher patient turnover increases the risk of hospital readmission and may affect the quality of care negatively [63]. In the general population, integrated care models focusing on discharge management for patients seem to be effective in reducing length of hospital stay and hospital readmission [27]. In our review on older adults, it was however impossible to conclude what component(s) of integrated care contributed to reduced hospitalisation due to major differences in the design of the studies. Similarly, we could not draw any conclusions in terms of the potential positive impact on patient satisfaction and readmission because of the inconsistency in the findings observed in the small number of studies reporting on each of these outcomes. For example, five studies reported on patient satisfaction of which 2 reported a positive impact and the remaining 3 studies reported no impact. The inconsistency in the findings on patient satisfaction may be explained by a variety in the patients’ expectations and the health status of the patients as perceived quality of integrated care has previously been shown to be most prominent in older people at the risk of frailty [64]. Many older people regard deteriorating health as normal and may report being satisfied with the care provided because of lower expectations [65]. On the other hand, older people who receive support from informal carers are often very satisfied with their help and may therefore not rank professional social care higher than informal care [50]. This may at least partly explain why older people participating in integrated care interventions are not necessarily more satisfied with the care compared to the control group. However, contrary to these potential reasons, research has also shown that older people, both those who are robust and those who are frail, fear (further) deterioration of health and loss of independence [66]. Hence, inconsistency in the findings on patient satisfaction could also be due to other reasons including data being self-reported and assessed using various questions and scales. For example, the satisfaction survey developed for the PACE study was directed towards community-dwelling older people deemed to be eligible for nursing home care yet still living at home. The applicability of these questions to other patient groups and settings remains however unknown [50].
One of the included studies also showed that increased productivity had a positive impact on patient satisfaction. Despite fewer contacts with nurses, the intervention group reported greater satisfaction with services, the delivery of care and services, and the organisation of care and services, compared to the control group [49]. The authors concluded that their intervention had been successful in targeting those likely to benefit the most and that the findings demonstrated ‘real effectiveness’. Successfully distributing the resources to target those in greatest need is further considered the biggest challenge facing the Swedish health and social care system [12]. Following the patient choice of primary care provider reform introduced in 2010, hundreds of new private primary care practices that operate for profit have been established across the country. Recent research has shown that being able to choose primary care provider has improved access and increased the number of visits to primary care but this has particularly benefitted wealthier people with lower healthcare needs and failed to prioritise those with greater needs [67]. People who consider themselves in need of seeing a medical doctor seem to seek care at the emergency departments rather than primary care clinics where, depending on their health problems, they may be seen by a nurse. Local initiatives have, however, shown that developing and implementing integrated care between hospitals, primary care and social care reduces the number of hospital admissions and readmissions [68,69]. For example, at a primary care clinic in Borgholm, a municipality in the south of Sweden with the oldest population in the country, dramatic changes have been made to improve access to healthcare. This includes patients being guaranteed a same day home visit by a medical doctor, which has reduced the burden on ambulatory staff and the number of visits to the emergency department. Improved exchange of patient information between hospital and primary care following a hospital admission has allowed for quicker follow-up once the patient has been discharged. Such follow-ups include prevention of further illness and thus readmission to the hospital [69]. Another small-scale example of integrated care in Sweden is the Tiohundra project in Norrtälje where the municipality and the county mutually provide all health and social services to the population of Norrtälje. This allows for changes in operations and management to swiftly be translated into changes in the delivery of care. The project involves case managers overlooking the planning and implementation process which is developed together with the patient and their relatives following hospital discharge. The development of strategies for caring of older people with complex needs also involves outlining pathways and plans around transitions in and out of hospital from nursing homes to hospital [68].
The challenge of providing integrated health and social care in a decentralised system where these two facets of care are funded and controlled by different levels of government is not unique for Sweden [68]. It is however clear that the existing fragmented and silo-based health and social care will not be able to meet the complex health and social care needs of the rapidly growing number of older adults with multi-morbidity [70]. Thus, future comprehensive studies using measurable outcomes that allow for statistical assessments of the impact of integrated care are needed to conclude what an optimal health and social care system should involve.
Examining outcomes as measures of quality of care is supported by Donabedian who favours outcomes that are concrete and clearly defined [44]. Donabedian argues that outcomes such as hospital admission rates reflect the influence of health sciences on achievement of certain results. Indeed our findings on hospital admission and length of stay support positive achievements in previous research in health sciences [27]. Nonetheless, Donabedian stresses that the limitations of the outcomes assessed must be recognised including the outcome assessed possibly being irrelevant for the study. When applying Donabedian’s framework to our findings, the complete lack of association between integrated care for older adults and mortality suggests that mortality may not have been a relevant measure. Donabedian also argues that the time aspect can act as a limitation e.g. long periods of time that must elapse before relevant outcomes are manifest, potentially delaying the availability of the results. Thus, mortality may be more relevant when studying younger and middle-aged adults which allow for longer follow-up.
Strengths and limitations
Strengths of the study include that this is one of the first systematic reviews on non-disease specific integrated care assessing multiple outcomes related to older patients. The search strategy comprised of five different patient-related outcomes of integrated care, was developed together with two well-experienced librarians and applied to 5 different databases. Limitations include that 25 studies were excluded due to full-text versions being unavailable (mainly conference abstracts), and searches did not include grey-zone literature and non-English literature, possibly resulting in relevant data not being taken into account. Further, the number of studies examining each of the outcomes was often small including only 3 eligible studies investigating readmission making it impossible to draw any conclusions. Furthermore, in some of the included studies the authors speculated whether lack of statistical power might have explained the lack of associations [58,49]. Also, due to methodological and interventional heterogeneity of the studies, statistical calculations of objectively assessed outcome measures could not be undertaken. The variety of interventions presented were due to local circumstances, which may not have to be considered a weakness per se. Nevertheless, as a consequence it remains unclear whether the findings are statistically significant.
Conclusions
This systematic review has explored multiple patient-related outcomes of integrated care targeting older people. The findings suggest that integrated care may have a positive impact on hospital admission rates in older age. Integrated care may also positively influence the length of hospital stay and possibly also patient satisfaction and readmission. In contrast, integrated care did not have an impact on mortality. However due to lack of robust findings, the effectiveness of integrated care on patient-related outcomes in later life remain largely unknown. Whilst this review has tried to identify patient-related outcomes important in integrated care provided to older adults, further theory-based research is needed to assess the effect on these outcomes in integrated care settings.
Acknowledgements
We would like to thank Klas Moberg and Carl Gornitzki, librarians at the Karolinska Institutet University Library, for their support in developing search strategies and performing the literature searches. The research was partly funded by the Swedish Research Council for Health, Working Life and Welfare (FORTE) (grant 2017-01431 and 2017-02155) and carried out as part of the Social Inequalities in Ageing (SIA) project, funded by NordForsk, project number 74637.
Appendix A
Search terms used
Population
aged
aging/ageing
old/older
elderly/elders
geriatric*
psychogeriatric*
dementia/demented
alzheimer*
community-dwelling
late-life*
retired/retirement
senior citizen*
pensioner*
Integrated care
Delivery of Health Care
Integrat*
Continuity of Patient Care/
Comprehensive Health Care/
Coordinated/co-ordinated
Comprehensive
Collaborative
Transmural
Continuity
interdisciplinar*
multidisciplinar*
multiprofessional
multiagency
multisector
seamless
shared
whole
interface
locality
interaction
modelling
health*
care*
delivery
system/systems
service*
clinic/clinics
care or disease or health
management/managed
community
program*
plan*
team*
Patient-related outcomes
surviv*
mortality
hospitalization
Length of Stay
readmission*/re-admission*
Patient Admission
Patient Readmission
satisfact*
Patient Satisfaction
Appendix B
Results of quality assessment of the included quantitative studies
| Author (year) | Study design | Selection bias | Risk of performance bias | Risk of detection bias | Risk of attrition bias | Risk of reporting bias | Risk of conflict of interest | Interweaved risk of bias |
|---|---|---|---|---|---|---|---|---|
| Atherly et al. (2004) | Quasi-experimental | Moderate | Low | Moderate | Moderate | Low | Moderate | Moderate |
| Beland et al. (2006) | RCT | Low | Low | Low | Moderate | Low | Low | Low |
| Bernabei et al. (1998) | RCT | Low | Low | Low | Low | Low | Low | Low |
| Ham et al. (2003) | Retrospective cohort | Moderate | Moderate | Low | Low | Low | Low | Low |
| Hebert et al. (2009) | Quasi-experimental Study | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Landi et al. (1999) | Quasi-experimental study | Low | Low | Low | Low | Moderate | Moderate | Low |
| Landi et al. (2001) | Quasi-experimental study | Low | Low | Low | Moderate | Low | Moderate | Low |
| Looman et al. (2014) | Quasi-experimental Study | Low | Low | Moderate | Low | Low | Moderate | Low |
| Schiotz et al. (2011) | Retrospective cohort | Moderate | Moderate | Moderate | Low | Low | Low | Moderate |
| de Stampa et al. (2014) | Quasi-experimental Study | Low | Low | Low | Moderate | Low | Low | Low |
| Tourigny et al. (2004) | Quasi-experimental | Low | Low | Low | Low | Low | Moderate | Low |
Results of the quality assessment for the qualitative study
| Author (year) | Study design | Well defined aim | Risk of Selection bias | Risk of data collection bias | Risk of analysis bias | Risk of reporting bias | Interweaved risk of bias | |
|---|---|---|---|---|---|---|---|---|
| Brown et al. (2003) | Non-randomised comparative study | Yes | Low | Low | Low | Low | Low | |
Funding Statement
We would like to thank Klas Moberg and Carl Gornitzki, librarians at the Karolinska Institutet University Library, for their support in developing search strategies and performing the literature searches. The research was partly funded by the Swedish Research Council for Health, Working Life and Welfare (FORTE) (grant 2017-01431 and 2017-02155) and carried out as part of the Social Inequalities in Ageing (SIA) project, funded by NordForsk, project number 74637.
Reviewers
Tamara Alhambra Borrás, PhD., Researcher, Polibienestar Research Institute – University of Valencia, Spain.
Ronald Uittenbroek PhD., Head of school of nursing, Windesheim university of applied science, The Netherlands.
Competing Interests
The authors have no competing interests to declare.
References
- 1.World Health Organization (WHO). World report on ageing and health Geneva; 2015. [Google Scholar]
- 2.Goodwin, N, Dixon, A, Anderson, G and Wodchis, WP. Providing integrated care for older people with complex needs. Lessons from seven international case studies; 2014. Available from: https://pdfs.semanticscholar.org/7981/12c57a7ade2239037ea96ec32a4a8039a5a4.pdf. [DOI] [PMC free article] [PubMed]
- 3.Coleman, EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc, 2003; 51(4): 549–555. DOI: 10.1046/j.1532-5415.2003.51185.x [DOI] [PubMed] [Google Scholar]
- 4.Kripalani, S, Jackson, AT, Schnipper, JL and Coleman, EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med, 2007; 2(5): 314–323. DOI: 10.1002/jhm.228 [DOI] [PubMed] [Google Scholar]
- 5.Stange, KC. The problem of fragmentation and the need for integrative solutions. Ann Fam Med, 2009; 7(2): 100–103. DOI: 10.1370/afm.971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brodsky, J, Habib, J, Hirschfeld, M and Siegel, B. Care of the frail elderly in developed and developing countries: the experience and the challenges. Aging clinical and experimental research, 2002; 14(4): 279–286. DOI: 10.1007/BF03324451 [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization (WHO). Integrated care for older people (ICOPE). Guidelines on community-level interventions to manage declines in intrinsic capacity; 2017. Available from: http://www.who.int/ageing/WHO-ALC-ICOPE_brochure.pdf?ua=1 DOI: 10.1093/geroni/igx004.2477 [DOI] [PubMed]
- 8.Rechel, B, Doyle, Y, Grundy, E and McKee, M. How can health systems respond to population ageing? 2009. Available from: http://www.euro.who.int/__data/assets/pdf_file/0004/64966/E92560.pdf. [DOI] [PubMed]
- 9.Ham, C. Making sense of integrated care systems, integrated care partnerships and accountable care organisations in the NHS in England; 2018. Available from: https://www.kingsfund.org.uk/publications/making-sense-integrated-care-systems.
- 10.Lewis, RQ, Rosen, R, Goodwin, N and Dixon, J. Where Next for Integrated Care Organisations in the English NHS? London: The Nuffield Trust; 2010. [Google Scholar]
- 11.Tandon, A, Murray, CJL, Lauer, JA and Evans, DB. Measuring overall health system performance for 191 countries. GPE Discussion Paper Series: No. 30; 1998. Available from: http://www.who.int/healthinfo/paper30.pdf.
- 12.Statens offentliga utredningar (SOU) Effektiv vård. Efficient care. Report SOU 2016:2. 2016. [In Swedish: ]. Available from: http://www.sou.gov.se/wp-content/uploads/2016/01/SOU-2016_2_Hela4.pdf. [Google Scholar]
- 13.Johansson, L and Schön, P. Country Report Sweden CEQUA Long Term Care Network, London School of Economics and Political Science. Brussels; 2017. [Google Scholar]
- 14.OECD. Health at a Glance 2017: OECD Indicators Paris; 2017. DOI: 10.1787/health_glance-2017-en [DOI] [Google Scholar]
- 15.Fritzell, J, Salen, L, Nelson, K, Palme, J and Schön, P. European Social Policy Network (ESPN) Country Profile: Sweden. Chapter 2. Systems and policies affecting social outcomes, 2016; 29–43. [Google Scholar]
- 16.Philbin, EF. Comprehensive multidisciplinary programs for the management of patients with congestive heart failure. J Gen Intern Med, 1999; 14(2): 130–135. DOI: 10.1046/j.1525-1497.1999.00291.x [DOI] [PubMed] [Google Scholar]
- 17.Rich, MW. Heart failure disease management: a critical review. J Card Fail, 1999; 5(1): 64–75. DOI: 10.1016/S1071-9164(99)90026-X [DOI] [PubMed] [Google Scholar]
- 18.Moser, DK. Heart failure management: optimal health care delivery programs. Annu Rev Nurs Res, 2000; 18: 91–126. DOI: 10.1891/0739-6686.18.1.91 [DOI] [PubMed] [Google Scholar]
- 19.McAlister, FA, Lawson, FM, Teo, KK and Armstrong, PW. A systematic review of randomized trials of disease management programs in heart failure. Am J Med, 2001; 110(5): 378–384. DOI: 10.1016/S0002-9343(00)00743-9 [DOI] [PubMed] [Google Scholar]
- 20.McAlister, FA, Lawson, FM, Teo, KK and Armstrong, PW. Randomised trials of secondary prevention programmes in coronary heart disease: systematic review. BMJ, 2001; 323(7319): 957–962. DOI: 10.1136/bmj.323.7319.957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johri, M, Beland, F and Bergman, H. International experiments in integrated care for the elderly: a synthesis of the evidence. International Journal of Geriatric Psychiatry, 2003; 18(3): 222–235. DOI: 10.1002/gps.819 [DOI] [PubMed] [Google Scholar]
- 22.Sin, DD, McAlister, FA, Man, SF and Anthonisen, NR. Contemporary management of chronic obstructive pulmonary disease: scientific review. JAMA, 2003; 290(17): 2301–2312. DOI: 10.1001/jama.290.17.2301 [DOI] [PubMed] [Google Scholar]
- 23.Ouwens, M, Wollersheim, H, Hermens, R, Hulscher, M and Grol, R. Integrated care programmes for chronically ill patients: a review of systematic reviews. Int J Qual Health Care, 2005; 17(2): 141–146. DOI: 10.1093/intqhc/mzi016 [DOI] [PubMed] [Google Scholar]
- 24.Eklund, K and Wilhelmson, K. Outcomes of coordinated and integrated interventions targeting frail elderly people: a systematic review of randomised controlled trials. Health & social care in the community, 2009; 17(5): 447–458. DOI: 10.1111/j.1365-2524.2009.00844.x [DOI] [PubMed] [Google Scholar]
- 25.Rosenberg, T. Acute hospital use, nursing home placement, and mortality in a frail community-dwelling cohort managed with Primary Integrated Interdisciplinary Elder Care at Home. Journal of the American Geriatrics Society, 2012; 60(7): 1340–1346. DOI: 10.1111/j.1532-5415.2012.03965.x [DOI] [PubMed] [Google Scholar]
- 26.Stewart, MJ, Georgiou, A and Westbrook, JI. Successfully integrating aged care services: a review of the evidence and tools emerging from a long-term care program. International Journal of Integrated Care, 2013; 13: e003 DOI: 10.5334/ijic.963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Damery, S, Flanagan, S and Combes, G. Does integrated care reduce hospital activity for patients with chronic diseases? An umbrella review of systematic reviews. BMJ Open, 2016; 6(11): e011952 DOI: 10.1136/bmjopen-2016-011952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Balaban, RB, Zhang, F, Vialle-Valentin, CE, Galbraith, AA, Burns, ME, Larochelle, MR, et al. Impact of a Patient Navigator Program on Hospital-Based and Outpatient Utilization Over 180 Days in a Safety-Net Health System. J Gen Intern Med, 2017; 32(9): 981–989. DOI: 10.1007/s11606-017-4074-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Di Pollina, L, Guessous, I, Petoud, V, Combescure, C, Buchs, B, Schaller, P, et al. Integrated care at home reduces unnecessary hospitalizations of community-dwelling frail older adults: a prospective controlled trial. BMC Geriatr, 2017; 17(1): 53 DOI: 10.1186/s12877-017-0449-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pini, A, Sarafis, P, Malliarou, M, Tsounis, A, Igoumenidis, M, Bamidis, P, et al. Assessment of Patient Satisfaction of the Quality of Health Care Provided by Outpatient Services of an Oncology Hospital. Glob J Health Sci, 2014; 6(5): 196–203. DOI: 10.5539/gjhs.v6n5p196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Costa-de Lima, K, Peixoto-Veras, R, Pereira-Caldas, C, Motta, LB, Bonfada, D, Marques-Dos Santos, M, et al. Effectiveness of intervention programs in primary care for the robust elderly. Salud Publica Mex, 2015; 57(3): 265–274. DOI: 10.21149/spm.v57i3.7566 [DOI] [PubMed] [Google Scholar]
- 32.Blom, J, den Elzen, W, van Houwelingen, AH, Heijmans, M, Stijnen, T, Van den Hout, W, et al. Effectiveness and cost-effectiveness of a proactive, goal-oriented, integrated care model in general practice for older people. A cluster randomised controlled trial: Integrated Systematic Care for older People—the ISCOPE study. Age Ageing, 2016; 45(1): 30–41. DOI: 10.1093/ageing/afv174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ouwens, M, Hulscher, M, Hermens, R, Faber, M, Marres, H, Wollersheim, H, et al. Implementation of integrated care for patients with cancer: a systematic review of interventions and effects. Int J Qual Health Care, 2009; 21(2): 137–144. DOI: 10.1093/intqhc/mzn061 [DOI] [PubMed] [Google Scholar]
- 34.Ellis, G, Whitehead, MA, O’Neill, D, Langhorne, P and Robinson, D. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev, 2011; (7): CD006211 DOI: 10.1002/14651858.CD006211.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Baxter, S, Johnson, M, Chambers, D, Sutton, A, Goyder, E and Booth, A. The effects of integrated care: a systematic review of UK and international evidence. BMC Health Serv Res, 2018; 18(1): 350 DOI: 10.1186/s12913-018-3161-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Garin, N, Koyanagi, A, Chatterji, S, Tyrovolas, S, Olaya, B, Leonardi, M, et al. Global Multimorbidity Patterns: A Cross-Sectional, Population-Based, Multi-Country Study. The Journals of Gerontology: Series A, 2015; 71(2): 205–214. DOI: 10.1093/gerona/glv128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kodner, DL. All together now: a conceptual exploration of integrated care. Healthc Q, 2009; 13 Spec No: 6–15. DOI: 10.12927/hcq.2009.21091 [DOI] [PubMed] [Google Scholar]
- 38.Looman, WM, Fabbricotti, IN and Huijsman, R. The short-term effects of an integrated care model for the frail elderly on health, quality of life, health care use and satisfaction with care. International Journal of Integrated Care, 2014; 14: e034 DOI: 10.5334/ijic.1010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Struckmann, V, Leijten, FRM, van Ginneken, E, Kraus, M, Reiss, M, Spranger, A, et al. Relevant models and elements of integrated care for multi-morbidity: Results of a scoping review. Health Policy, 2018; 122(1): 23–35. DOI: 10.1016/j.healthpol.2017.08.008 [DOI] [PubMed] [Google Scholar]
- 40.Creditor, MC. Hazards of hospitalization of the elderly. Ann Intern Med, 1993; 118(3): 219–223. DOI: 10.7326/0003-4819-118-3-199302010-00011 [DOI] [PubMed] [Google Scholar]
- 41.Ahrens, B. Reduced mortality, the ultimate indicator of treatment efficacy. Review and perspectives. Pharmacopsychiatry, 1994; 27(Suppl 1): 37–40. DOI: 10.1055/s-2007-1014326 [DOI] [PubMed] [Google Scholar]
- 42.Armitage, GD, Suter, E, Oelke, ND and Adair, CE. Health systems integration: state of the evidence. International Journal of Integrated Care, 2009; 9: e82 DOI: 10.5334/ijic.316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kodner, DL and Spreeuwenberg, C. Integrated care: meaning, logic, applications, and implications – a discussion paper. International Journal of Integrated Care, 2002; 2: e12 DOI: 10.5334/ijic.67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Donabedian, A. Evaluating the Quality of Medical Care. Milbank Quarterly, 2005; 83(4): 691–729. DOI: 10.1111/j.1468-0009.2005.00397.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.de Carvalho, IA, Epping-Jordan, J, Pot, AM, Kelley, E, Toro, N, Thiyagarajan, JA, et al. Organizing integrated health-care services to meet older people’s needs. Bulletin of the World Health Organization, 2017; 95(11): 756–763. DOI: 10.2471/BLT.16.187617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.The Swedish Agency for Health Technology Assessment. Utvärdering av metoder i hälso- och sjukvården och insatser i socialtjänsten. Mall för kvalitetsgranskning av randomiserade studier. [Assessment of Social Services Evaluation – Methods in Health and Social Care. Template for quality assessment of randomised trials.] 2014. [in Swedish: ] Available from: https://www.sbu.se/globalassets/ebm/metodbok/mall_randomiserade_studier.pdf. [Google Scholar]
- 47.The Swedish Agency for Health Technology Assessment. Utvärdering av metoder i hälso- och sjukvården och insatser i socialtjänsten. Mall för kvalitetsgranskning av observationsstudier. [Assessment of Social Services Evaluation methods in health and social care. Template for quality assessment of observational studies.] 2014. [in Swedish: ] Available from: https://www.sbu.se/globalassets/ebm/metodbok/mall_observationsstudier.pdf. [Google Scholar]
- 48.The Swedish Agency for Health Technology Assessment. Utvärdering av metoder i hälso- och sjukvården och insatser i socialtjänsten. Mall för kvalitetsgranskning av studier med kvalitativ forskningsmetodik – patientupplevelser. [Assessment of Social Services Evaluation methods in health and social care. Template for quality assessment of qualitative research – patients’ perceptions.] 2014. [in Swedish: ] Available from: http://www.sbu.se/globalassets/ebm/metodbok/mall_kvalitativ_forskningsmetodik.pdf. [Google Scholar]
- 49.Hebert, R, Raiche, M, Dubois, M-F, Gueye, NDR, Dubuc, N, Tousignant, M, et al. Impact of PRISMA, a coordination-type integrated service delivery system for frail older people in Quebec (Canada): A quasi-experimental study. The journals of gerontology. Series B, Psychological sciences and social sciences, 2010; 65B(1): 107–118. DOI: 10.1093/geronb/gbp027 [DOI] [PubMed] [Google Scholar]
- 50.Atherly, A, Kane, RL and Smith, MA. Older adults’ satisfaction with integrated capitated health and long-term care. The Gerontologist, 2004; 44(3): 348–357. DOI: 10.1093/geront/44.3.348 [DOI] [PubMed] [Google Scholar]
- 51.Brown, L, Tucker, C and Domokos, T. Evaluating the impact of integrated health and social care teams on older people living in the community. Health & social care in the community, 2003; 11(2): 85–94. DOI: 10.1046/j.1365-2524.2003.00409.x [DOI] [PubMed] [Google Scholar]
- 52.Beland, F, Bergman, H, Lebel, P, Clarfield, AM, Tousignant, P, Contandriopoulos, A-P, et al. A system of integrated care for older persons with disabilities in Canada: results from a randomized controlled trial. The journals of gerontology. Series A, Biological sciences and medical sciences, 2006; 61(4): 367–373. DOI: 10.1093/gerona/61.4.367 [DOI] [PubMed] [Google Scholar]
- 53.Landi, F, Gambassi, G, Pola, R, Tabaccanti, S, Cavinato, T, Carbonin, PU, et al. Impact of integrated home care services on hospital use. Journal of the American Geriatrics Society, 1999; 47(12): 1430–1434. DOI: 10.1111/j.1532-5415.1999.tb01562.x [DOI] [PubMed] [Google Scholar]
- 54.Landi, F, Onder, G, Russo, A, Tabaccanti, S, Rollo, R, Federici, S, et al. A new model of integrated home care for the elderly: impact on hospital use. J Clin Epidemiol, 2001; 54(9): 968–970. DOI: 10.1016/S0895-4356(01)00366-3 [DOI] [PubMed] [Google Scholar]
- 55.de Stampa, M, Vedel, I, Buyck, J-F, Lapointe, L, Bergman, H, Beland, F, et al. Impact on hospital admissions of an integrated primary care model for very frail elderly patients. Archives of gerontology and geriatrics, 2014; 58(3): 350–355. DOI: 10.1016/j.archger.2014.01.005 [DOI] [PubMed] [Google Scholar]
- 56.Schiotz, M, Price, M, Frolich, A, Sogaard, J, Kristensen, JK, Krasnik, A, et al. Something is amiss in Denmark: a comparison of preventable hospitalisations and readmissions for chronic medical conditions in the Danish Healthcare system and Kaiser Permanente. BMC Health Serv Res, 2011; 11: 347 DOI: 10.1186/1472-6963-11-347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ham, C, York, N, Sutch, S and Shaw, R. Hospital bed utilisation in the NHS, Kaiser Permanente, and the US Medicare programme: analysis of routine data. BMJ, 2003; 327(7426): 1257 DOI: 10.1136/bmj.327.7426.1257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tourigny, A, Durand, P, Bonin, L, Hebert, R and Rochette, L. Quasi-experimental study of the effectiveness of an integrated service delivery network for the frail elderly. Canadian Journal on Aging, 2004; 23(3): 231–246. DOI: 10.1353/cja.2004.0038 [DOI] [PubMed] [Google Scholar]
- 59.Bernabei, R, Landi, F, Gambassi, G, Sgadari, A, Zuccala, G, Mor, V, et al. Randomised trial of impact of model of integrated care and case management for older people living in the community. BMJ, 1998; 316(7141): 1348–1351. DOI: 10.1136/bmj.316.7141.1348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Smit, LC, Schuurmans, MJ, Blom, JW, Fabbricotti, IN, Jansen, APD, Kempen, G, et al. Unravelling complex primary-care programs to maintain independent living in older people: a systematic overview. J Clin Epidemiol, 2018; 96: 110–119. DOI: 10.1016/j.jclinepi.2017.12.013 [DOI] [PubMed] [Google Scholar]
- 61.Toh, HJ, Lim, ZY, Yap, P and Tang, T. Factors associated with prolonged length of stay in older patients. Singapore medical journal, 2017; 58(3): 134–138. DOI: 10.11622/smedj.2016158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kohn, L, Corrigan, J and Donaldson, M. To err is human: building a safer health system Washington DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 63.Heggestad, T. Do Hospital Length of Stay and Staffing Ratio Affect Elderly Patients’ Risk of Readmission? A Nation-wide Study of Norwegian Hospitals. Health services research, 2002; 37(3): 647–665. DOI: 10.1111/1475-6773.00042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Uittenbroek, RJ, Kremer, HPH, Spoorenberg, SLW, Reijneveld, SA and Wynia, K. Integrated Care for Older Adults Improves Perceived Quality of Care: Results of a Randomized Controlled Trial of Embrace. J Gen Intern Med, 2017; 32(5): 516–523. DOI: 10.1007/s11606-016-3742-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kasper, JD and Riley, G. Satisfaction with medical care among elderly people in fee-for-service care and an HMO. J Aging Health, 1992; 4(2): 282–302. DOI: 10.1177/089826439200400207 [DOI] [PubMed] [Google Scholar]
- 66.Spoorenberg, SL, Wynia, K, Fokkens, AS, Slotman, K, Kremer, HP and Reijneveld, SA. Experiences of Community-Living Older Adults Receiving Integrated Care Based on the Chronic Care Model: A Qualitative Study. PLoS One, 2015; 10(10): e0137803 DOI: 10.1371/journal.pone.0137803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Burström, B, Burström, K, Nilsson, G, Tomson, G, Whitehead, M and Winblad, U. Equity aspects of the Primary Health Care Choice Reform in Sweden – a scoping review. International Journal for Equity in Health, 2017; 16(29). DOI: 10.1186/s12939-017-0524-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Andersson Bäck, M and Calltorp, J. The Norrtaelje model: a unique model for integrated health and social care in Sweden. International Journal of Integrated Care, 2015; 15: e016 DOI: 10.5334/ijic.2244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ström, M. Kan Borgholm-modellen bli lösningen för framtidens sjukvård? [Could the Borgholm model become the model of future healthcare?] Läkartidningen [Journal of the Swedish Medical Association]. [in Swedish: ] 2018; 03(115:EX47). [Google Scholar]
- 70.Klinga, C. The only constant is change. Exploring the evolvement of health and social care integration Stockholm; 2018. [Google Scholar]


