Abstract
Several studies have debated the rehabilitation merits of functional electrical stimulation (FES) for the treatment of spinal radiculopathies. Many of the related studies have been performed on elite athletes. We utilized the Russian stimulation in three cases to improve outcomes in foot drop secondary to lumbar radiculopathy. These stimulations had positive results, giving patients an increase in strength in the lower limbs after each session. These outcomes suggest that Russian stimulation has potential as an affordable option in the rehabilitation of foot drop from lumbar radiculopathy when used with exercise-based physical therapy.
Keywords: Functional electrical stimulation, Russian stimulation, foot drop, lumbar radiculopathy
Spinal radiculopathies resulting from degenerative changes or traumas are a common reason for referral to physical medicine and rehabilitation or physical therapy. Options for radiculopathy treatment is limited—physicians instruct patients to rest and use pain-relieving medications as needed, administer corticosteroid injections, or refer them to physical therapy.1–3 Surgical options are typically a last resort; some success has been observed in treating the symptoms (e.g., weakness, foot drop, pain, paresthesia) of lumbar radiculopathy with surgical procedures.4,5
“Russian stimulation” or “Russian currents” functional electric stimulation (FES) has been beneficial for improving muscle force-generating ability as part of a physical therapy regimen.6 It is a medium frequency generator that uses frequencies in the range of 2400 to 2500 Hz and is often used conjunctively in management of athletic injuries, such as anterior cruciate ligament (ACL) tears, with physical therapy programs to improve strength.7,8 In particular, Russian stimulation has been used to treat arthrogenic inhibition of the quadriceps muscle group post ACL repair.7,8
To date, no studies have reviewed the use of Russian stimulation in foot drop related to lumbar radiculopathy. We present three cases of nonathlete individuals who presented with foot drop resulting from lumbar radiculopathies and were treated with FES utilizing the Russian stimulation method.
MATERIALS AND METHODS
All patients were diagnosed with a lumbar radiculopathy from physical examination and imaging by a physical medicine and rehabilitation physician. All patients were evaluated by a neurosurgeon who recommended conservative treatment before consideration of surgical interventions. The patients underwent Russian stimulation with a single physical therapist. Manual muscle testing was conducted in accordance to the Medical Research Council classification.8 Informed consent was obtained prior to interventions and collecting patient data.
Russian stimulation was applied to the tibialis anterior muscle belly. A burst frequency of 50bps with 70mACC with 10/50 seconds on/off over 12 minutes and 50-percent duty cycle 50 percent was applied to the muscle to achieve tetany with volitional dorsiflexion to the best of the patient’s abilities. The physical therapist assisted foot dorsiflexion during the “on” cycle to ease pain. All patients were able to tolerate stimulation with a minimal amount of discomfort and no adverse effects.
Each patient underwent neuromuscular re-education and manual therapy post-stimulation. They were given therapeutic exercise after each FES session. Manual therapy was applied with Grade V talocrural scoop, Grade III talocrural AP, and passive dorsiflexion stretch. Kinesiotape was applied for tibialis anterior facilitation to assist dorsiflexion during gait.
Dynamic neuromuscular stabilization techniques included flexion patterning to improve dorsiflexion facilitation. Patients were instructed to assist dorsiflexion using a loop dog leash around the front of the foot below their toes. Patients were told to attempt to pull their toes to their nose and hold for five seconds, followed by relaxation. Patient was instructed to repeat the exercise 30 times until fatigue 2 to 3 times daily.
RESULTS
Case 1. A 35-year-old male patient presented with symptoms of back pain and associated left lower limb weakness and paresthesia about 11 months prior to undergoing Russian stimulation. He denied history of trauma and reported onset of pain after lifting 50lb boxes at his work. Magnetic resonance imaging (MRI) revealed a L5-S1 disc bulge with moderate-to-severe left neural foraminal narrowing, leading to a diagnosis of left L5 radiculopathy. Physical exam approximately 10 months after symptom onset demonstrated continued weakness in the left lower limb (Table 1). Physical exam one month after this evaluation did not show improvement. After treatment with Russian stimulation, sustained improvement in strength of the left lower limb was observed. Strength improvement was sustained on subsequent follow-up, and the patient declined additional sessions of treatment. The patient continued to experience axial back pain.
TABLE 1.
Manual muscle testing before and after Russian stimulation in Cases 1–3.
| CASE # | MEASUREMENT | SESSION 1 | SESSION 2 | SESSION 3 | SESSION 4 | ||||
|---|---|---|---|---|---|---|---|---|---|
| STRENGTH BEFORE | STRENGTH AFTER | STRENGTH BEFORE | STRENGTH AFTER | STRENGTH BEFORE | STRENGTH AFTER | STRENGTH BEFORE | STRENGTH AFTER | ||
| Case 1 | Knee extension | 3 | 4 | NA | NA | NA | NA | NA | NA |
| Ankle dorsiflexion | 2 | 4 | |||||||
| EHL | 2 | 3 | |||||||
| Ankle plantarflexion | 3 | 4 | |||||||
| Case 2 | Knee extension | 2 | 3 | 3 | 4 | 4 | 4 | ||
| Ankle dorsiflexion | 3 | 4 | 5 | 5 | 5 | 5 | NA | NA | |
| EHL | 4 | 4 | 5 | 5 | |||||
| Ankle plantarflexion | |||||||||
| Case 3 | Knee extension | ||||||||
| Ankle dorsiflexion | 1 | 2 | 2 | 2 | 3 | 4 | 3 | 4 | |
| EHL | 4 | 4 | 5 | 5 | 5 | 5 | 5 | 5 | |
| Ankle plantarflexion | |||||||||
EHL: extensor hallucis longus; NA: not applicable
Case 2. A 60-year-old female patient with a history of hypertension presented to the clinic with a two-day history of right foot weakness, bowel and bladder loss, and severe low back pain after lifting patients in her healthcare profession. MRI completed at the time of presentation showed right-sided L4-5 and mid L5 level disc extrusion versus sequestration, effacing the exiting right L5 nerve sleeve and nearby thecal sac (Figure 1). The patient received a course of oral prednisone, and all pain was resolved. Three weeks later at a follow-up visit, residual right lower limb weakness and numbness was still present. At this point, the first Russian stimulation was conducted. Two additional sessions were conducted one week later followed by a third session two weeks after that. The patient reported improvement in strength after each session, with sustained improvement to four-fifths strength. She was able to successfully return to work.
FIGURE 1.
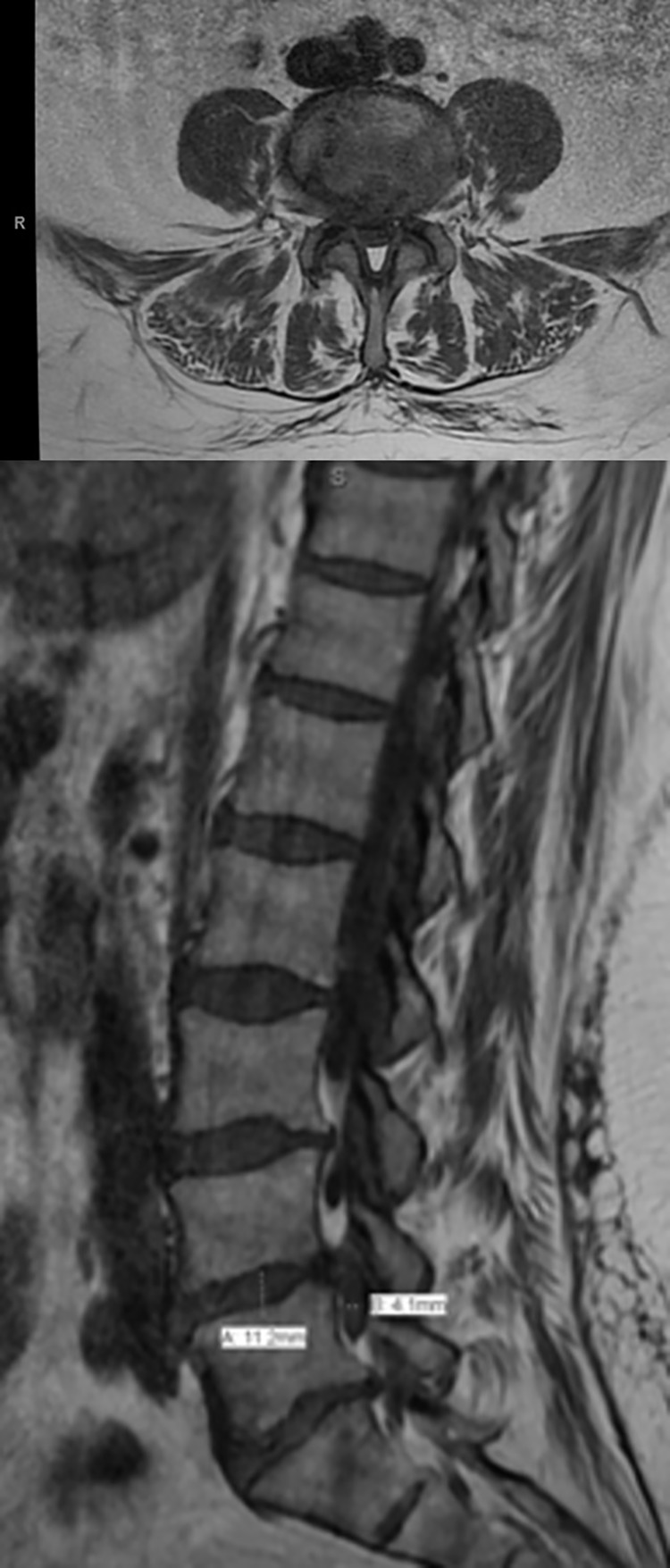
Case 2 magnetic resonance imaging (MRI) on T1 sagittal and T2 axial shows a right-sided L4-5 and mid-L5 level disc extrusion versus sequestration, effacing the exiting right L5 nerve sleeve and nearby thecal sac.
Case 3. A 56-year-old female patient with a history of hypertension presented a week after onset of radiating lower back pain and right foot drop. Onset of pain was not related to lifting or trauma. Her profession required prolonged sitting and driving. MRI findings were significant for L4-5 disc bulge and osteophytes, hypertrophy of facets and ligamentum flavum, severe spinal canal stenosis, and moderate right neural foraminal stenosis. The patient was diagnosed with a right L5 radiculopathy. Symptoms had not improved at a two-month follow-up visit. The patient was started on an oral neuropathic agent for pain control, and received one session of Russian stimulation. Three additional sessions were performed at one, two, and four weeks after initial Russian stimulation session. Patient had sustained improvement in strength after each session with improvement to four-fifths strength by three months. The weakness in other myotomes seemed secondary to pain rather than a true weakness. The patient was able to fully return to work. She continued to experience numbness in the L5 dermatome.
DISCUSSION
Disc herniation and spinal stenosis (on L4/5 level) are two of the most common causes for lumbosacral radiculopathy.1,6 The prevalence of mild motor paresis has been reported to be as high as 50 percent in patients with disc herniation, but surgical intervention with discectomy does not seem to improve severe extensor weakness, especially painless foot drop.9 This might be due to the peronei, extensor hallucis longus (EHL), and tibialis anterior typically having the least capacity for full strength recovery.5 Given the equivocal scientific evidence for surgery, surgical intervention is usually delayed until all conservative efforts are pursued.10
Because of the great number of patients affected by lumbar radiculopathy and the invasive nature of surgery, the need for a conservative treatment option is important.1,6 FES is a noninvasive treatment option that can be used on denervated muscles to preserve or restore muscle strength and reduce subsequent muscle atrophy.11,12 Modlin et al13 used FES in spinal cord injuries and observed an increase in muscle mass and quality. Other investigators have examined the role of FES in the treatment of lumbosacral plexus avulsion trauma with associated lower extremity monoparesis, and peripheral nerve lesions of the median, ulnar, and peroneal nerves.14,15 However, no study to date has examined the use of FES, specifically Russian stimulation, in severe lumbar radiculopathies resulting in foot drop.
In our case study, the use of intermittent Russian stimulation demonstrated sustained functional recovery. The mechanism is most likely secondary to muscle fiber recovery and an increase in cross-sectional muscle size. Kern et al17 observed that only single muscle twitches are elicited at the initiation of FES, and later throughout the course, tetanic contraction of the muscle is elicited, thus improving the structural and metabolic state of the denervated muscles. Kern et al17 estimated that approximately 2 to 4 million fibers in quadricep muscles were restored in patients with complete conus cauda lesion following FES treatment. Similarly, in their study of denervated tibilias anterior muscles of rats, Bueno et al18 demonstrated an increase in cross-sectional area of the tibilias anterior using the Russian stimulation technique.
In administering FES, investigators have encouraged the use of long-term FES at a low duration for patient comfort. This technique employs a high number of stimulations over a longer length of time to induce muscle mass preservation.16,19 Despite clinical functionality of this method, few insurance providers cover the high cost of a FES unit over a long period of time. Therefore, we elected to use Russian stimulation at a higher amplitude and duration during therapy visits to efficiently facilitate muscle contraction and strength recovery, thereby eliminating the cost associated with a home FES unit. Prior studies report that 56 to 75 percent of patients recover to Medical Research Council4 Grade 4 or 5 by six months with nonoperative treatment.1
Limitations. Limitations of this study include the small sample size and lack of control, which temper our findings. Larger randomized, controlled studies are needed to better understand the effects of FES and Russian stimulation on strength and sensory recovery due to lumbar radiculopathy.
CONCLUSION
Though our patients did not fully recover limb strength following treatment with FES, they did achieve immediate and sustained improvement in their symptoms, allowing them to return to work and daily function more quickly than other nonsurgical options, such as bed rest, oral analgesics, lumbar support, muscle relaxants, spinal manipulation, physiotherapy, and epidural steroid injections. Hastened recovery is beneficial for quality of life and socioeconomic participation. Our findings suggest that FES using Russian stimulation might serve as an effective nonsurgical optoin for patients with lumbar radiculopathy resulting in foot drop.
REFERENCES
- 1.Sharma H, Lee SW, Cole AA. The management of weakness caused by lumbar and lumbosacral nerve root compression. J Bone Joint Surg Br. 2012;94(11):1442–1447. doi: 10.1302/0301-620X.94B11.29148. [DOI] [PubMed] [Google Scholar]
- 2.Cribb GL, Jaffray DC, Cassar-Pullicino VN. Observations on the natural history of massive lumbar disc herniation. J Bone Joint Surg Br. 2007;89(6):782–784. doi: 10.1302/0301-620X.89B6.18712. [DOI] [PubMed] [Google Scholar]
- 3.Lewis R, Williams N, Matar HE, et al. The clinical effectiveness and cost-effectiveness of management strategies for sciatica: systematic review and economic model. Health Technol Assess. 2011;15:1–578. doi: 10.3310/hta15390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aono H, Iwasaki M, Ohwada T, et al. Surgical outcome of drop foot caused by degenerative lumbar diseases. Spine. 2007;32:262–266. doi: 10.1097/01.brs.0000259922.82413.72. [DOI] [PubMed] [Google Scholar]
- 5.Girardi FP, Cammisa FP, Huang RC, et al. Improvement of preoperative foot drop after lumbar surgery. J Spinal Disord Tech. 2002;15:490–494. doi: 10.1097/00024720-200212000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Kim KM, Croy T, Hertel J, Saliba S. Effects of neuromuscular electrical stimulation after anterior cruciate ligament reconstruction on quadriceps strength, function, and patient-oriented outcomes: a systematic review. J Orthop Sports Phys Ther. 2010;40(7):383–391. doi: 10.2519/jospt.2010.3184. [DOI] [PubMed] [Google Scholar]
- 7.Ward A, Shkuratova N. Russian electrical stimulation: the early experiments. Phys Ther. 2002;82(10):1019–1030. [PubMed] [Google Scholar]
- 8.Vanpee G, Hermans G, Segers J, Gosselink R. Assessment of limb muscle strength in critically ill patients: a systematic review. Crit Care Med. 2014;42(3):701–711. doi: 10.1097/CCM.0000000000000030. [DOI] [PubMed] [Google Scholar]
- 9.Marshall RW. The functional relevance of neurological recovery 20 years or more after lumbar discectomy. J Bone Joint Surg Br. 2008;90(5):554–555. doi: 10.1302/0301-620X.90B5.20896. [DOI] [PubMed] [Google Scholar]
- 10.Rhee JM, Schaufele M, Abdu WA. Radiculopathy and the herniated lumbar disc: controversies regarding pathophysiology and management. J Bone Joint Surg Am. 2006;88(9):2070–2080. doi: 10.2106/00004623-200609000-00023. [DOI] [PubMed] [Google Scholar]
- 11.Robinson AJ. Physiology of muscle and nerve. In: Robinson AJ, Snyder-Mackler L, editors. Clinical electrophysiology: electrotherapy and electrophysiologic testing. Baltimore: Lippincott Williams & Wilkins. 2008:71–105. [Google Scholar]
- 12.Cavalcante EV, Silva LG, Montenegro EJ, Pontes NT. Efeito da eletroestimulação no músculo desnervado de animais: revisão sistemática. Fisioter Mov. 2012;25(3):669–678. (abstract) [Google Scholar]
- 13.Modlin M, Forstner C, Hofer C, et al. Electrical stimulation of denervated muscles: first results of a clinical study. Artif Organs. 2005;29(3):203–206. doi: 10.1111/j.1525-1594.2005.29035.x. [DOI] [PubMed] [Google Scholar]
- 14.Cakmak A. Electrical stimulation of denervated muscles. Disabil Rehabil. 2004;26(7):432–433. doi: 10.1080/09638280410001663157. [DOI] [PubMed] [Google Scholar]
- 15.Boonstra AM, van Weerden TW, Eisma WH, et al. The effect of low-frequency electrical stimulation on denervation atrophy in man. Scand J Rehabil Med. 1987;19(3):127–134. [PubMed] [Google Scholar]
- 16.Pieber K, Herceg M, Paternostro-Sluga T, Schuhfried O. Optimizing stimulation parameters in functional electrical stimulation of denervated muscles: a cross-sectional study. J Neuroeng Rehabil. 2015;12:51. doi: 10.1186/s12984-015-0046-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kern H, Hofer C, Mödlin M, et al. Denervated muscles in humans: limitations and problems of currently used functional electrical stimulation training protocols. Artif Organs. 2002;26(3):216–218. doi: 10.1046/j.1525-1594.2002.06933.x. [DOI] [PubMed] [Google Scholar]
- 18. Bueno CRS, Pereira M, Favaretto IA, Jr, et al. Electrical stimulation attenuates morphological alterations and prevents atrophy of the denervated cranial tibial muscle Einstein (Sao Paulo). 2017. 15 1 71 76 English, Portuguese. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Filipovic A, Kleinöder H, Dörmann U, Mester J. Electromyostimulation—a systematic review of the influence of training regimens and stimulation parameters on effectiveness in electromyostimulation training of selected strength parameters. J Strength Cond Res. 2011;25(11):3218–3238. doi: 10.1519/JSC.0b013e318212e3ce. [DOI] [PubMed] [Google Scholar]


