Abstract
Background
Adverse childhood experiences (ACEs) can increase risks of health-harming behaviours and poor health throughout life. While increases in risk may be affected by resilience resources such as supportive childhood relationships, to date few studies have explored these effects.
Methods
We combined data from cross-sectional ACE studies among young adults (n = 14 661) in educational institutions in 10 European countries. Nine ACE types, childhood relationships and six health outcomes (early alcohol initiation, problem alcohol use, smoking, drug use, therapy, suicide attempt) were explored. Multivariate modelling estimated relationships between ACE counts, supportive childhood relationships and health outcomes.
Results
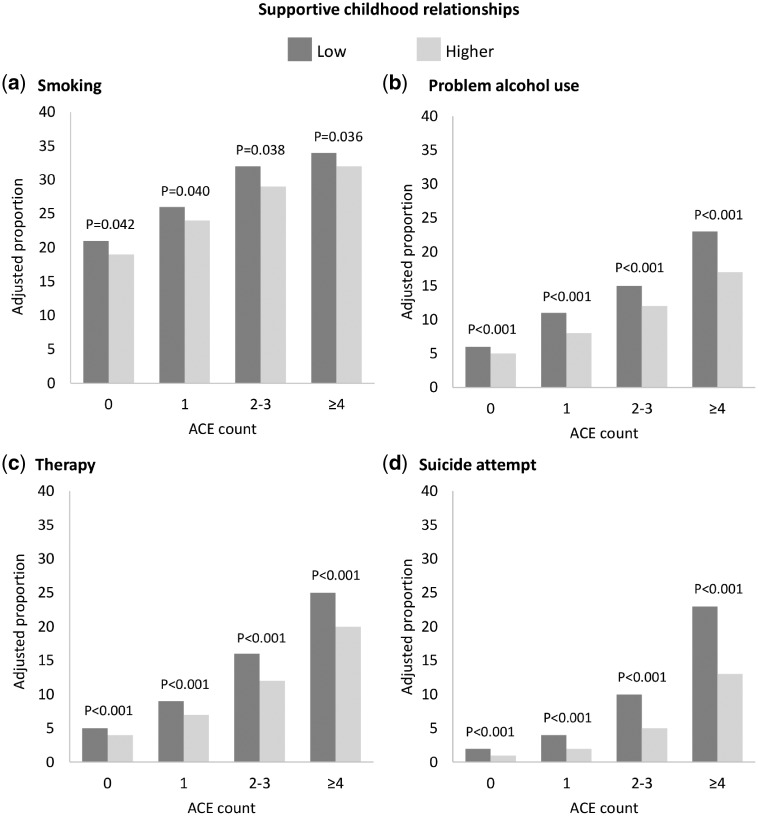
Almost half (46.2%) of participants reported ≥1 ACE and 5.6% reported ≥4 ACEs. Risks of all outcomes increased with ACE count. In individuals with ≥4 ACEs (vs. 0 ACEs), adjusted odds ratios ranged from 2.01 (95% CIs: 1.70–2.38) for smoking to 17.68 (95% CIs: 12.93–24.17) for suicide attempt. Supportive childhood relationships were independently associated with moderating risks of smoking, problem alcohol use, therapy and suicide attempt. In those with ≥4 ACEs, adjusted proportions reporting suicide attempt reduced from 23% with low supportive childhood relationships to 13% with higher support. Equivalent reductions were 25% to 20% for therapy, 23% to 17% for problem drinking and 34% to 32% for smoking.
Conclusions
ACEs are strongly associated with substance use and mental illness. Harmful relationships are moderated by resilience factors such as supportive childhood relationships. Whilst ACEs continue to affect many children, better prevention measures and interventions that enhance resilience to the life-long impacts of toxic childhood stress are required.
Introduction
The experiences that children have whilst growing up lay the foundations for their health and well-being throughout life. Providing children with the best start in life is a fundamental aspect of European health policy.1 However, over 55 million children in the European Region are estimated to be affected by child maltreatment and millions more will suffer other stressful experiences, such as witnessing domestic violence or living in a household affected by substance misuse or mental illness.2 The last decade has seen growing awareness of the damage that such adverse childhood experiences (ACEs) can have on child development, adult health and life opportunities.3–5 In particular, advances in neurodevelopmental and epigenetic research have identified how chronic early life stress imposed by ACEs can generate lasting changes in children’s developing neurological and physiological systems. In turn, these can embed susceptibility to health-damaging behaviours, mental illness and chronic disease.6,7 Corroboratively, research shows strong, cumulative relationships between ACEs and a wide range of health-related outcomes, with such effects being identified across an expanding range of geographies and populations.4
Increased understanding of the impacts of ACEs is driving multi-sector action to develop effective responses.8,9 Thus, work is focussing on prevention to reduce the risk of child maltreatment and other ACEs10 and, increasingly, the development of trauma-informed services to better support those affected by ACEs.11,12 There is also growing awareness of the role of resilience in protecting individuals that suffer ACEs from developing their harmful effects. Resilience can be thought of as the ability to overcome hardship, and the concept helps explain why some people manage to thrive despite significant childhood adversity.13,14 Thus, the relationship between ACEs and poor life-course health is not deterministic and building children’s resilience can help them overcome adversity. Key factors that contribute to the development of resilience in childhood include interpersonal skills, a sense of control over personal circumstances and strong links to cultural traditions. However, the strongest building block of resilience is considered to be the availability of stable, caring relationships with family members or other significant adults.13 While research suggests such relationships can reduce the risks of health-harming behaviours and poor mental health in those that suffer ACEs,15 relatively few studies have measured such effects.
In Europe, the ‘Roadmap to Implementing the 2030 Agenda for Sustainable Development, Building on Health 2020, the European Policy for Health and Well-being’16 provides a framework that places strategic focus both on determinants that drive health inequalities (such as ACEs) and on establishing resilient communities (which are in part a product of resilient individuals17). Further, the 53 Member States of the World Health Organization (WHO) European Region have adopted ‘Investing in Children: The European Child Maltreatment Prevention Action Plan’,2 which aims to reduce child maltreatment through implementing prevention programmes that address risk and protective factors. In line with these and other key health policies, the WHO Regional Office for Europe has led a programme of work to prevent child maltreatment and other ACEs. This now includes ACE studies among young adults in 13 countries, and previous analyses of a selection of these studies identified strong relationships between ACEs and health-harming behaviours.18 A core commitment of the ‘2030 Agenda for Sustainable Development’ is ensuring ‘no-one is left behind’, and consequently supporting those who suffer ACEs requires understanding both the potential impacts of ACEs on health and factors that may ameliorate such impacts. Of the 13 countries that have conducted ACE surveys, 10 collected consistent data not only on ACEs, but also on a range of health outcomes and measures of supportive relationships in childhood. Here, we use this large dataset to explore associations between the number of ACEs individuals suffered (as an indicator of increasing levels of adversity) and outcomes related to substance use and mental health, and to examine the potentially protective effects of supportive childhood relationships on these associations.
Methods
We combined data from surveys of young adults in educational settings in the Czech Republic, Lithuania, Republic of Moldova, Montenegro, Poland, Romania, the Russian Federation, Serbia, Ukraine and the former Yugoslav Republic of Macedonia. In each country, surveys were coordinated by national violence prevention programme leads, with the support of Ministries of Health and WHO Regional Office for Europe. National ethics committee approval was obtained according to national regulations. Sampling procedures varied between countries but most used stratified random samples of higher educational institutions and students. Information on sampling procedures, survey dates (2010–17), settings (universities, colleges, vocational academies) and participation rates (≥75%) for each country are summarized in Supplementary table 1. All surveys used the Family Health History questionnaire developed by the US Centers for Disease Control and Prevention and Kaiser Permanente19 to measure ACEs, supportive childhood relationships and outcomes. Questionnaires were translated and piloted in each country prior to survey implementation. In some countries, questions were varied to suit local situations (see Supplementary table 2). A total of 17 091 respondents participated. However, for this study analysis was limited to those aged 18–25 years (n = 16 219) who provided data for all ACE questions (n = 14 675) and at least three supportive relationships questions (final sample, n = 14 661).
Nine ACEs in participants’ first 18 years of life were measured: physical abuse; emotional abuse; sexual abuse; parental separation or divorce; witnessing domestic violence and living with a household member who was depressed or suicidal; a problem drinker/alcoholic; a drug user or incarcerated (Supplementary table 2). The number of ACEs each respondent reported was summed and allocated to an ACE count category (0 ACEs, 1 ACE, 2–3 ACEs or ≥4 ACEs). Six questions measured supportive childhood relationships asking whether (in the first 18 years of life) participants: had someone in their family to help them feel important or special; felt loved; knew there was someone to take care of and protect them; whether people in their family looked out for each other; felt close to each other and whether their family was a source of strength and support. Response options were ‘never’, ‘rarely true’, ‘sometimes true’, ‘often true’ and ‘very often true’. Responses of ‘often true’ or ‘very often true’ were classed as positive and individuals with ≤3 (of six) positive responses were categorized as having low supportive relationships. For cases providing data for three to five questions only (n = 421), missing responses were set to the mean of answered questions. Cases missing data for >3 questions (n = 14) were excluded. Cronbach’s alpha for the six questions was 0.828 across the whole sample and ranged from 0.735 in Macedonia to 0.893 in Poland.
Health-related variables included: current smoking, early alcohol initiation (<15 years), problem alcohol use (lifetime), drug use (lifetime), receiving therapy (lifetime) and suicide attempt (lifetime; Supplementary table 2). The question on receiving therapy referred to whether participants had ever been under the care of a psychologist, psychiatrist or therapist and is used here as a proxy for mental health conditions. Demographic variables included country, gender, age group and childhood socio-economic status (SES). Participants were classed as having low childhood SES if they reported any of three markers: low parental education, based on their father (or mother if father’s data not provided) having no education, being illiterate, not completing secondary school, or attending elementary/primary education only; reporting their family did not own their own home for most of their childhood; and reporting they did not have enough to eat at some point in childhood.
Analyses were undertaken in SPSS v24 using chi-squared and logistic regression to examine independent relationships between ACEs, supportive childhood relationships and outcomes. Stratified logistic regression models included ACE count, supportive childhood relationships, age group, gender and childhood SES. An interactive term between ACE count and supportive childhood relationships was also included to examine any differences in the moderating effects of supportive relationships on outcomes related to ACEs. Survey country was included as a separate stratum to account for unmeasured differences between samples. For outcomes significantly (P < 0.05) related to both ACE count and supportive childhood relationships, adjusted means (estimated marginal means) for each ACE and childhood support category were calculated using generalized linear modelling and best fit logistic regression models (including variables that contributed significantly to each model). Differences between adjusted means were tested using pairwise contrast (Wald chi-squared test) functions.
Results
Variations between countries in sample demographics and proportions reporting ACEs and low supportive childhood relationships are shown in table 1 (and Supplementary table 3). Just under half (46.2%) of participants reported at least 1 ACE and 5.6% reported ≥4 ACEs (table 1). The most common ACE reported was parental separation (17.0%) and the least common was household drug use (2.7%; Supplementary table 3). Cross-over between ACE types is shown in Supplementary table 4. Emotional abuse and domestic violence were most likely to co-occur with other ACEs, with 92.2 and 86.6% of those reporting these ACEs respectively having at least one other ACE. Emotional abuse typically co-occurred with physical abuse, while over 4 in 10 of those witnessing domestic violence also reported household alcohol abuse, physical abuse and/or parental separation. One in six participants (16.2%) was categorized as having low supportive childhood relationships. The proportion with low supportive relationships increased with ACE count (0 ACEs, 9.4%; 1 ACE, 15.3%; 2–3 ACEs, 27.0%; ≥4 ACEs 53.4%; χ2=1318.107, P < 0.001).
Table 1.
Overall and country-level sample characteristics
| All (%) | Czech Republic (%) | Lithuania (%) | Republic of Moldova (%) | Montenegro (%) | Poland (%) | Romania (%) | Russian Federation (%) | Serbia (%) | TFYR Macedonia (%) | Ukraine (%) | χ2 | P | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 14 661) | (n = 1677) | (n = 1398) | (n = 1351) | (n = 1084) | (n = 1655) | (n = 1542) | (n = 1403) | (n = 2074) | (n = 1200) | (n = 1277) | ||||
| Gender | Male | 39.6 | 28.6 | 32.8 | 37.5 | 47.7 | 57.2 | 37.4 | 40.1 | 34.5 | 40.2 | 43.7 | ||
| Female | 60.4 | 71.4 | 67.2 | 62.5 | 52.3 | 42.8 | 62.6 | 59.9 | 65.5 | 59.8 | 56.3 | 393.169 | <0.001 | |
| Age group | 18–19 | 39.8 | 23.1 | 34.5 | 26.6 | 56.8 | 24.3 | 14.7 | 32.8 | 75.8 | 60.0 | 47.6 | ||
| 20–21 | 41.1 | 35.8 | 60.9 | 47.7 | 36.1 | 59.1 | 47.8 | 39.5 | 23.0 | 28.7 | 35.7 | |||
| 22–25 | 19.0 | 41.1 | 4.6 | 25.6 | 7.1 | 16.6 | 37.5 | 27.7 | 1.2 | 11.3 | 16.7 | 3399.4 | <0.001 | |
| Childhood SES | Not low | 79.5 | 90.0 | 78.2 | 77.5 | 75.2 | 81.8 | 72.0 | 72.5 | 84.2 | 78.8 | 80.0 | ||
| Low | 20.5 | 10.0 | 21.8 | 22.5 | 24.8 | 18.2 | 28.0 | 27.5 | 15.8 | 21.3 | 20.0 | 261.202 | <0.001 | |
| ACE count | 0 | 53.8 | 47.2 | 49.8 | 55.1 | 59.9 | 48.5 | 47.6 | 59.9 | 60.8 | 69.3 | 41.7 | ||
| 1 | 23.5 | 25.5 | 24.3 | 21.4 | 21.6 | 26.1 | 24.7 | 20.6 | 22.1 | 19.8 | 28.3 | |||
| 2–3 | 17.1 | 20.2 | 19.0 | 16.9 | 14.7 | 19.2 | 20.2 | 14.7 | 13.7 | 9.0 | 22.6 | |||
| ≥4 | 5.6 | 7.0 | 6.9 | 6.6 | 3.9 | 6.2 | 7.5 | 4.8 | 3.3 | 1.9 | 7.4 | 406.090 | <0.001 | |
| Supportive | Higher | 83.8 | 80.2 | 83.1 | 82.0 | 89.7 | 81.6 | 85.5 | 77.5 | 90.8 | 83.3 | 82.5 | ||
| childhood relationships | Low | 16.2 | 19.8 | 16.9 | 18.0 | 10.3 | 18.4 | 14.5 | 22.5 | 9.2 | 16.8 | 17.5 | 173.808 | <0.001 |
Notes: ACE, adverse childhood experiences; SES, socio-economic status; TFYR Macedonia, the former Yugoslav Republic of Macedonia.
Bivariate relationships between outcomes and demographics, ACEs and childhood relationships are presented in table 2. More males than females reported current smoking, early alcohol initiation, problem alcohol use and drug use, whereas more females reported suicide attempt. Smoking, drug use and therapy were more commonly reported by older participants. All outcomes were associated with low childhood SES and having low supportive childhood relationships. Proportions reporting all outcomes increased with ACE count (table 2).
Table 2.
Bivariate relationships between outcome variables and demographics, ACE count and supportive childhood relationships
| Current smoker | Early alcohol initiation | Problem alcohol use | Drug use | Therapy | Suicide attempt | ||
|---|---|---|---|---|---|---|---|
| All | n | 14 534 | 14 381 | 14 553 | 14 610 | 14 396 | 14 574 |
| % | 22.7 | 18.9 | 7.5 | 16.1 | 8.7 | 3.5 | |
| Gender | Male | 26.5 | 25.6 | 10.0 | 20.6 | 8.7 | 2.3 |
| Female | 20.2 | 14.5 | 5.9 | 13.2 | 8.6 | 4.3 | |
| χ2 | 79.554 | 273.368 | 83.925 | 138.456 | 0.090 | 41.215 | |
| P | <0.001 | <0.001 | <0.001 | <0.001 | 0.764 | <0.001 | |
| Age group | 18–19 | 20.1 | 19.4 | 7.2 | 12.3 | 8.8 | 3.3 |
| 20–21 | 23.5 | 18.9 | 7.4 | 18.7 | 8.1 | 3.6 | |
| 22–25 | 26.2 | 17.9 | 8.6 | 18.6 | 9.7 | 3.7 | |
| χ2 | 44.262 | 2.695 | 5.881 | 102.986 | 6.582 | 1.585 | |
| P | <0.001 | 0.260 | 0.053 | <0.001 | 0.037 | 0.453 | |
| Childhood SES | Not low | 22.3 | 18.5 | 6.5 | 15.7 | 8.1 | 2.7 |
| Low | 24.3 | 20.3 | 11.6 | 17.9 | 10.7 | 6.7 | |
| χ2 | 5.326 | 4.774 | 90.205 | 8.686 | 19.019 | 114.558 | |
| P | 0.021 | 0.029 | <0.001 | 0.003 | <0.001 | <0.001 | |
| ACE count | 0 | 18.7 | 15.3 | 4.6 | 10.8 | 4.7 | 0.9 |
| 1 | 24.6 | 20.8 | 8.3 | 18.3 | 8.6 | 2.6 | |
| 2–3 | 29.3 | 24.6 | 11.7 | 24.8 | 15.8 | 7.4 | |
| ≥4 | 32.7 | 27.6 | 19.2 | 31.7 | 25.5 | 20.0 | |
| χ2 | 187.993 | 165.192 | 322.284 | 463.572 | 605.318 | 927.148 | |
| P | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| Supportive childhood relationships | Higher | 21.7 | 18.0 | 6.5 | 15.3 | 7.6 | 2.3 |
| Low | 27.7 | 23.4 | 13.0 | 20.8 | 14.4 | 9.5 | |
| χ2 | 41.535 | 36.922 | 120.119 | 44.690 | 114.782 | 302.908 | |
| P | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Notes: ACE, adverse childhood experiences; SES, socio-economic status.
Cumulative associations between ACE count and outcomes remained in multivariate analyses (table 3). Risks were significantly elevated even in those with 1 ACE and greatest in those with ≥4 ACEs. Thus, compared with those with no ACEs, those with ≥4 ACEs were twice as likely to report current smoking and early alcohol initiation, around 4 times as likely to report problem alcohol use and drug use, 6 times as likely to report therapy and 17 times more likely to have attempted suicide. Low supportive childhood relationships was independently associated with smoking, problem drinking, therapy and suicide attempt but not with early alcohol initiation and drug use. Interactive terms exploring differences in relationships between outcomes and supportive relationships at different ACE counts were not significant.
Table 3.
Adjusted odds ratios for health outcomes in demographic, ACE count and supportive childhood relationship groups
| Current smoker | Early alcohol initiation | Problem alcohol use | Drug use | Therapy | Suicide attempt | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 14 534 | n = 14 381 | n = 14 553 | n = 14 610 | n = 14 396 | n = 14 574 | |||||||||
| AOR | (95% CIs) | AOR | (95% CIs) | AOR | (95% CIs) | AOR | (95% CIs) | AOR | (95% CIs) | AOR | (95% CIs) | |||
| Country | (Ref) Romania | |||||||||||||
| Czech Republic | 0.73 | (0.62–0.85) | 1.00 | (0.83–1.20) | 0.50 | (0.36–0.70) | 1.30 | (1.08–1.58) | 1.98 | (1.55–2.52) | 0.73 | (0.50–1.08) | ||
| Lithuania | 1.05 | (0.89–1.24) | 2.90 | (2.44–3.45) | 1.40 | (1.06–1.84) | 2.82 | (2.33–3.41) | 0.36 | (0.25–0.53) | 1.10 | (0.76–1.59) | ||
| Republic of Moldova | 0.33 | (0.27–0.40) | 0.90 | (0.74–1.10) | 2.02 | (1.56–2.62) | 0.60 | (0.47–0.76) | 0.86 | (0.63–1.17) | 0.72 | (0.47–1.10) | ||
| Montenegro | 0.42 | (0.35–0.52) | 0.90 | (0.73–1.11) | 1.31 | (0.98–1.77) | 0.79 | (0.61–1.01) | 1.52 | (1.13–2.04) | 0.95 | (0.60–1.52) | ||
| Poland | 0.42 | (0.35–0.50) | 0.63 | (0.52–0.76) | 0.68 | (0.51–0.91) | 3.77 | (3.15–4.51) | 2.22 | (1.74–2.83) | 1.39 | (0.97–1.99) | ||
| Russian Federation | 0.59 | (0.50–0.70) | 0.48 | (0.38–0.60) | 1.73 | (1.32–2.25) | 0.33 | (0.25–0.44) | 0.39 | (0.27–0.57) | 1.20 | (0.82–1.75) | ||
| Serbia | 0.55 | (0.47–0.65) | 0.88 | (0.73–1.05) | 1.14 | (0.87–1.49) | 1.15 | (0.93–1.42) | 1.69 | (1.32–2.17) | 0.62 | (0.41–0.94) | ||
| TFYR Macedonia | 0.91 | (0.76–1.08) | 1.66 | (1.37–2.00) | 1.18 | (0.87–1.60) | 0.46 | (0.34–0.61) | 0.72 | (0.50–1.02) | 1.31 | (0.85–2.03) | ||
| Ukraine | 0.56 | (0.47–0.67) | 0.97 | (0.80–1.17) | 1.14 | (0.86–1.51) | 0.93 | (0.75–1.16) | 2.13 | (1.65–2.75) | 0.97 | (0.66–1.42) | ||
| Gendera | Female | 0.65 | (0.60–0.70) | 0.44 | (0.40–0.48) | 0.55 | (0.48–0.62) | 0.61 | (0.55–0.67) | ns | 2.12 | (1.71–2.63) | ||
| Age group | (Ref) 18–19 | |||||||||||||
| 20–21 | 1.16 | (1.06–1.28) | 1.30 | (1.16–1.46) | ||||||||||
| 22–25 | 1.26 | (1.12–1.42) | 1.59 | (1.38–1.84) | ||||||||||
| Childhood SESa | Low | 1.30 | (1.12–1.50) | 1.36 | (1.11–1.67) | |||||||||
| ACE count | (Ref) 0 | |||||||||||||
| 1 | 1.39 | (1.26–1.53) | 1.44 | (1.29–1.60) | 1.88 | (1.59–2.21) | 1.71 | (1.52–1.93) | 1.78 | (1.51–2.09) | 2.70 | (1.97–3.69) | ||
| 2–3 | 1.79 | (1.60–1.99) | 1.92 | (1.71–2.16) | 2.70 | (2.28–3.20) | 2.60 | (2.30–2.93) | 3.47 | (2.97–4.06) | 6.83 | (5.14–9.07) | ||
| ≥4 | 2.01 | (1.70–2.38) | 2.25 | (1.89–2.68) | 4.32 | (3.45–5.41) | 3.72 | (3.12–4.43) | 6.17 | (5.00–7.60) | 17.68 | (12.93–24.17) | ||
| Supportive childhood relationshipsa | Low | 1.12 | (1.01–1.25) | ns | 1.39 | (1.19–1.62) | ns | 1.34 | (1.15–1.56) | 2.03 | (1.66–2.49) | |||
Notes: ACE, adverse childhood experiences; AOR, adjusted odds ratio; 95% CIs, 95% confidence intervals; ns, not significant; Ref, reference category; SES, socio-economic status. Interactive terms exploring differences in relationships between outcomes and supportive relationships at different ACE counts were not significant in any model and therefore have not been included in the table. Iterative steps for associations between ACEs and outcome measures are shown in Supplementary table 5.
Reference categories for gender, childhood SES and supportive childhood relationships are male, not low and higher respectively.
For outcomes associated with both ACE count and supportive childhood relationships, modelling estimated absolute differences in each outcome by ACE count, stratified by supportive childhood relationship status (figure 1a–d). Across ACE count levels, adjusted proportions of suicide attempt were approximately halved when childhood support was higher. Thus, in those with ≥4 ACEs, suicide attempt reduced from 23% with low supportive childhood relationships to 13% with higher childhood support (figure 1d). Equivalent reductions (in those with ≥4 ACEs) were from 25 to 20% for therapy, from 23 to 17% for problem drinking and from 34 to 32% for smoking (figure 1a–c).
Figure 1.
Adjusted mean percentage with each health outcome (a, smoking; b, problem alcohol use; c, therapy; d, suicide attempt) by ACE count, stratified by supportive childhood relationships. Note: Adjusted means are calculated using all significant terms in the logistic regression models for each outcome (see table 3). No figure is included for early alcohol initiation or drug use as supportive childhood relationships did not contribute significantly to the model
Discussion
European health policy promotes a life-course approach that includes strategies to address the determinants of health, build resilient communities and ensure ‘no-one is left behind’.16 This study adds to a growing evidence base suggesting childhood adversity is a major determinant of poor health.4 Across samples of young adults from 10 European countries, we found the more ACEs individuals reported, the more likely they were to have adopted substance use (cigarettes, alcohol and drugs) and developed poor mental health. While ACEs were positively correlated with all outcomes, relative increases in risk varied considerably. Compared with individuals with no ACEs, those with ≥4 ACEs were twice as likely to report early alcohol initiation and current smoking. However, they were around four times as likely to report drug use or problem alcohol use. Outcomes related directly to mental health showed the greatest increases in risk, with accessing therapy 6 times more likely in those with ≥4 ACEs (vs. none) and attempted suicide 17 times more likely. The strength of these relationships reflects other work showing outcomes with a strong mental health component to be highly affected by ACEs.4,20
Mental disorders are a leading cause of disease burden among 15–49-year-olds in the WHO European region.21 They are estimated to affect over a third of the Region’s population each year and WHO highlight the need for accelerated progress in this area.16 The European mental health action plan (2013–20)22 already emphasizes the importance of reducing ACEs by raising awareness, increasing recognition and ensuring early intervention. There is a developing evidence base for programmes that prevent ACEs.23,24 Such interventions include home visiting programmes25 and parenting programmes,26 which can prevent child maltreatment, improve parenting skills and strengthen parent–child relationships. They also provide opportunities for professionals to identify and assist parents with difficulties including mental illness, substance misuse and domestic violence.27
Over half of participants that reported witnessing domestic violence also reported at least one form of child maltreatment (Supplementary table 4), highlighting the intergenerational nature of violence. In most countries, domestic violence questions focussed on violence towards mothers. Violence against women (VAW) and child maltreatment share many risk factors, including harmful alcohol use, drug use and mental illness and children who suffer abuse are at increased risk of involvement in VAW in later life.28 The relationships identified in this study also highlight the intergenerational nature of ACEs and ill health,29 and thus the importance of breaking these cycles. Children that suffer adversity are at increased risk of developing behaviours (e.g. substance use) and conditions (e.g. mental illness) that can later become ACEs for their own children; consequently increasing the risk of such behaviours and conditions being transmitted across generations. Evidence-based frameworks for preventing violence against children have been developed by WHO and international partners.30
While preventing ACEs is critical, equally important is developing and enhancing factors that provide protection to those exposed to ACEs.31 Despite the concept of resilience increasingly featuring in health and social policy, evidence on assets that provide resilience against the poor outcomes associated with ACEs remains limited. The European ACE surveys have allowed initial exploration of potential protective effects associated with supportive childhood relationships; considered the most important foundation of resilience.13 Supportive relationships with caregivers or other trusted adults enable children to learn to cope with stress and thus develop healthy stress response systems. Such relationships can provide children who suffer ACEs with a ‘safe space’ to recover, providing protection against the toxic effects of extreme stress on brain development.32 In the absence of supportive relationships, individuals can develop higher allostatic loads, increasing vulnerability to physical and mental illness.7 Here, greater childhood support was associated with reduced risk of smoking, problem alcohol use, therapy and suicide attempt. For suicide attempt, the reduction in risk was substantial; among individuals with ≥4 ACEs, prevalence reduced from 23% with low supportive childhood relationships to 13% with higher support. For therapy, smoking and problem alcohol use, reductions were less marked but still significant. However, there were no significant relationships with early alcohol or lifetime drug use. Our study does not provide insight into why these issues did not respond to supportive childhood relationships. However, alcohol provision to children is often by parents who, regardless of the evidence, may believe it to be neutral or even beneficial to child development.33 Further, drug use was measured on a lifetime basis with no detail on drug type or duration of use. Recreational drug use is common among young Europeans.34 It may be that supportive childhood relationships have limited impact on such recreational risk taking yet help prevent its transition to continued or problematic levels. Such effects could be explored in future research using longitudinal designs. Alcohol, drug and tobacco use are leading risk factors for disease burden in Europe.21 Currently, however, addressing ACEs as an underlying contributor to harmful substance use is typically missing from national and international policy.
While findings indicate benefits to individuals that suffer ACEs from supportive childhood relationships, they also show these individuals are less likely to have such relationships. Over half of those with ≥4 ACEs had low childhood support compared with less than 1 in 10 of those with no ACEs. While programmes that strengthen family relationships can foster such support within the home, where this is not possible, ensuring children have access to trusted and supportive relationships through extended families, communities or public services may help bridge this gap.35 Ensuring children exposed to toxic stress receive therapeutic and other support is also essential and the forthcoming WHO guidelines for the health sector response to child maltreatment will highlight effective support programmes.36
This study has a number of limitations. Samples were recruited in higher educational settings and may under-represent young adults from more socially deprived groups, who can be disproportionately affected by ACEs.23,37 Equally, ACEs are associated with poorer educational attainment5 and individuals suffering the greatest burden from ACEs are less likely to reach higher education. Like other retrospective ACE surveys, findings may be affected by recall or reporting issues, while cultural and resource differences between countries may affect reporting of certain behaviours or experiences as well as access to services (i.e. for therapy). While therapy was used here as a proxy for mental health conditions, the actual prevalence of such conditions is likely to be higher as not all those affected will seek such services or have access to them. Questionnaires were piloted in each country prior to implementation and our analysis accounted for differences between country samples. While the ACE tool has been used across multiple countries, there is limited data available on its psychometric properties. However, adapted versions have been validated, 38,39 and retrospective reports of easily-defined ACEs such as those measured here are considered to have acceptable psychometric properties.40 Finally, our study design is cross-sectional; for most ACEs (except sexual abuse, see Supplementary table 2) age of first exposure was not recorded while outcome measures were largely measured on a lifetime basis; this limits inference on causality.
Conclusions
Evidence demonstrating the life-long harms to health and social well-being from ACEs continues to grow. Our study has identified substantially increased risks of substance use and mental illness faced by young Europeans that have suffered ACEs. The European ACE studies are building awareness of the impact of ACEs across the region and driving action to prevent and respond to them.10 Equally important is ensuring that children who suffer ACEs receive appropriate support, including opportunities to develop resilience to help avoid the harmful effects of early toxic stress. Supportive childhood relationships are considered a key foundation of resilience and our findings indicate their potential protective effects against the development of harmful substance use and mental illness. However, resilience does not provide a panacea to ACEs. Developing multi-agency approaches that implement effective early prevention at scale along with resilience building opportunities for those affected by ACEs is essential in breaking cycles of ACEs and ill health, and consequently a critical aspect of achieving European health policy.
Supplementary Material
Acknowledgements
We are very grateful to the team of researchers that contributed to study development, implementation and data preparation in each country. We are also grateful to the authorities and educational establishments that supported this work. We thank all the young people who participated voluntarily in the study.
Conflicts of interest: None declared.
Funding
Analysis of the combined datasets was funded by the World Health Organization Regional Office for Europe.
Key points
Almost half of young adult students surveyed across 10 European countries reported having suffered at least one adverse childhood experience.
Risks of smoking, early alcohol initiation, problem alcohol use, drug use, suicide attempt and therapy increased with the number of ACEs suffered.
Supportive childhood relationships were independently associated with reduced risks of smoking, drug use, suicide attempt and having used therapy; even in those that suffered ACEs.
Early interventions that prevent ACEs such as child maltreatment and strengthen family relationships are critical in establishing children on a healthy life-course.
Children that suffer ACEs and lack supportive relationships within the home environment may benefit from developing support through extended family, communities and public services.
References
- 1.World Health Organization Regional Office for Europe. Health 2020: A European Framework and Strategy for the 21st Century. Copenhagen: World Health Organization Regional Office for Europe, 2013. [Google Scholar]
- 2.World Health Organization Regional Office for Europe. Investing in Children: The European Child Maltreatment Prevention Action Plan 2015-2020. Copenhagen: World Health Organization Regional Office for Europe, 2015. [Google Scholar]
- 3. Jimenez ME, Wade R, Lin Y, et al. Adverse experiences in early childhood and kindergarten outcomes. Pediatrics 2016;137:e20151839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hughes K, Bellis MA, Hardcastle KA, et al. The impact of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health 2017;2:e356–66. [DOI] [PubMed] [Google Scholar]
- 5. Metzler M, Merrick MT, Klevens J, et al. Adverse childhood experiences and life opportunities: shifting the narrative. Child Youth Serv Rev 2017;72:141–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Teicher MH, Samson JA, Anderson CM, Ohashi K. The effects of child maltreatment on brain structure, function and connectivity. Nat Rev Neurosci 2016;17:652–66. [DOI] [PubMed] [Google Scholar]
- 7. Danese A, McEwen BS. Adverse childhood experiences, allostatis, allostatic load, and age-related disease. Physiol Behav 2012;106:29–39. [DOI] [PubMed] [Google Scholar]
- 8. Bethell CD, Solloway MR, Guinosso S, et al. Prioritizing possibilities for child and family health: an agenda to address adverse childhood experiences and foster the social and emotional roots of well-being in paediatrics. Acad Pediatr 2017;17:S36–50. [DOI] [PubMed] [Google Scholar]
- 9.Welsh Government. Prosperity for All: The National Strategy. Cardiff: Welsh Government, 2017. [Google Scholar]
- 10. Sethi D, Yon Y, Parekh N, et al. European Status Report on Preventing Child Maltreatment. Copenhagen: World Health Organization Regional Office for Europe, 2018. [Google Scholar]
- 11.NHS Education for Scotland. Transforming Psychological Trauma: A Knowledge and Skills Framework for the Scottish Workforce. Edinburgh: NHS Education for Scotland, 2017. [Google Scholar]
- 12. Leitch L. Action steps using ACEs and trauma-informed care: a resilience model. Health Justice 2017;5:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Center on the Developing Child at Harvard University. Supportive relationships and active skill-building strengthen the foundations of resilience. Working Paper 13 2015. Available at: http://www.developingchild.harvard.edu (17 August 2018, date last accessed).
- 14. Kalisch R, Baker DG, Basten U, et al. The resilience framework as a strategy to combat stress-related disorders. Nat Hum Behav 2017;1:784–90. [DOI] [PubMed] [Google Scholar]
- 15. Bellis MA, Hardcastle K, Ford K, et al. Does continuous trusted adult support in childhood impart life-course resilience against adverse childhood experiences—a retrospective study on adult health-harming behaviours and mental well-being. BMC Psychiatry 2017;17:110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization Regional Office for Europe. Roadmap to implement the 2030 Agenda for Sustainable Development, building on Health 2020, the European policy for health and well-being. Budapest: Regional Committee for Europe, 2017. [Google Scholar]
- 17. Morton MJ, Lurie N. Community resilience and public health practice. Am J Public Health 2013;103:1158–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bellis MA, Hughes K, Leckenby N, et al. Adverse childhood experiences and associations with health-harming behaviours in young adults: surveys in eight eastern European countries. Bull World Health Organ 2014;92:641–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. Family health history questionnaire. Available at: https://www.cdc.gov/violenceprevention/acestudy/about.html (23 May 2018, date last accessed).
- 20. Kessler RC, McLaughlin KA, Green JG, et al. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Br J Psychiatry 2010;97:378–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Institute for Health Metrics. GBD compare. 2018. Available at: https://vizhub.healthdata.org/gbd-compare/ (2 June 2018, date last accessed).
- 22.World Health Organization Regional Office for Europe. The European Mental Health Action Plan 2013-2020. Copenhagen: World Health Organization Regional Office for Europe, 2015. [Google Scholar]
- 23. Sethi D, Bellis MA, Hughes K, et al. European Report on Preventing Child Maltreatment. Copenhagen: World Health Organization Regional Office for Europe, 2013. [Google Scholar]
- 24. Flynn AB, Fothergill KE, Wilcox HC, et al. Primary care interventions to prevent or treat traumatic stress in childhood: a systematic review. Acad Pediatr 2015;15:480–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Casillas KL, Fauchier A, Derkash BT, Garrido EF. Implementation of evidence-based home visiting programs aimed at reducing child maltreatment: a meta-analytic review. Child Abuse Negl 2016;53:64–80. [DOI] [PubMed] [Google Scholar]
- 26. Chen M, Chan KL. Effects of parenting programs on child maltreatment prevention: a meta-analysis. Trauma Violence Abuse 2016;17:88–104. [DOI] [PubMed] [Google Scholar]
- 27. Prosman G, Lo Fo Wong SH, Van der Wouden JC, Lagro-Janssen ALM. Effectiveness of home visiting in reducing partner violence for families experiencing abuse: a systematic review. Fam Pract 2015;32:247–56. [DOI] [PubMed] [Google Scholar]
- 28. Guedes A, Bott S, Garcia-Moreno C, Colombini M. Bridging the gaps: a global review of intersections of violence against women and violence against children. Glob Health Action [Internet] 2016;9:31516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Le Scherban F, Wang X, Boyle-Steed KH, Pachter LM. Intergenerational associations of parent adverse childhood experiences and child health outcomes. Pediatrics 2018; 141:e20174274. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization. INSPIRE: Seven Strategies for Ending Violence against Children. Geneva: World Health Organization, 2016. [Google Scholar]
- 31. Boparai SKP, Au V, Koita K, et al. Ameliorating the biological impacts of childhood adversity: a review of intervention programs. Child Abuse Negl 2018;81: 82–105. [DOI] [PubMed] [Google Scholar]
- 32. Wadsworth ME. Development of maladaptive coping: a functional adaptation to chronic, uncontrollable stress. Child Dev Perspect 2015;9:96–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jones SC. Parental provision of alcohol: a TPB-framed review of the literature. Health Promot Int 2016;31:562–71. [DOI] [PubMed] [Google Scholar]
- 34.European Monitoring Centre for Drugs and Drug Addiction. European Drug Report 2018: Trends and Developments. Luxembourg: Publication Office of the European Union, 2018. [Google Scholar]
- 35. Lewing B, Doubell L, Beevers T, Acquah D. Building Trusted Relationships for Vulnerable Children and Young People with Public Services. London: Early Intervention Foundation, 2018. [Google Scholar]
- 36.World Health Organization. Guidelines for the Health Sector Response to Child Maltreatment. Geneva: WHO, in press. Available at: http://www.who.int/violence_injury_prevention/violence/child/child_maltreatment_guidelines/en/ (22 August 2018, date last accessed. [Google Scholar]
- 37. Bellis MA, Hughes K, Leckenby N, et al. Measuring mortality and the burden of adult disease associated with adverse childhood experiences in England: a national survey. J Public Health 2015;37:445–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kazeem OT. A validation of the adverse childhood experiences scale in Nigeria. Res Humanities Hum Sci 2015;5:18–23. [Google Scholar]
- 39. Ford DC, Merrick MT, Parks SE, et al. Examination of the factorial structure of adverse childhood experiences and recommendations for three subscale scores. Psychol Violence 2014;4:432–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J Child Psychol Psychiatry 2004;45:260–73. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.