Abstract
Background
Average life expectancy has stopped increasing for many countries. This has been attributed to causes such as influenza, austerity policies and deaths of despair (drugs, alcohol and suicide). Less is known on the inequality of life expectancy over time using reliable, whole population, data. This work examines all-cause and cause-specific mortality rates in Scotland to assess the patterning of relative and absolute inequalities across three decades.
Methods
Using routinely collected Scottish mortality and population records we calculate directly age-standardized mortality rates by age group, sex and deprivation fifths for all-cause and cause-specific deaths around each census 1981–2011.
Results
All-cause mortality rates in the most deprived areas in 2011 (472 per 100 000 population) remained higher than in the least deprived in 1981 (422 per 100 000 population). For those aged 0–64, deaths from circulatory causes more than halved between 1981 and 2011 and cancer mortality decreased by a third (with greater relative declines in the least deprived areas). Over the same period, alcohol- and drug-related causes and male suicide increased (with greater absolute and relative increases in more deprived areas). There was also a significant increase in deaths from dementia and Alzheimer’s disease for those aged 75+.
Conclusions
Despite reductions in mortality, relative (but not absolute) inequalities widened between 1981 and 2011 for all-cause mortality and for several causes of death. Reducing relative inequalities in Scotland requires faster mortality declines in deprived areas while countering increases in mortality from causes such as drug- and alcohol-related harm and male suicide.
Introduction
For several decades, many countries have seen steady increases in life expectancy. However recently, for some of these countries, there has been a flattening or decreasing trend in average life expectancy.1 This has been attributed to causes such as influenza epidemics among older people; austerity policies;2 and drug, alcohol and suicide deaths in deprived groups.3 In Scotland, between 1991 and 2001, mortality rates due to alcohol, drugs, suicide and assault increased for young men, particularly those in the most deprived areas.4 This has contributed to Scotland lagging behind other Western European countries when it comes to improvements in life expectancy.5
Inequalities in mortality have persisted in the UK for many years, with some suggesting that they are now at their highest level since 1921.6 Despite overall improvements in the health of the Scottish population, the gap between those with the best health and worst health persists and, for many health measures, the deprivation gap has widened. While some countries have struggled to reduce mortality inequalities, others have made considerable progress over recent years7 particularly in reducing absolute inequalities.8 Although relative reductions can be more difficult to achieve than absolute reductions when health is improving, it has been argued that ‘it is both possible and feasible to expect both absolute and relative measures of health inequalities to improve simultaneously given a conducive policy context’.9
Knowledge of how inequalities in mortality rates differ by key socio-economic factors, and are changing over the long-term, is crucial for monitoring public health and making progress on health inequalities.10 Previous work on inequalities in life expectancy and mortality has lacked reliable socio-economic data on the whole population across time.1 This paper uses population data from Scotland for the period 1981–2011 to give an overview of the changes to mortality rates over three decades, and describes current inequalities in all-cause and cause-specific mortality by age group, sex and area-level deprivation.
Methods
Population
We used census population estimates of the usually resident population on census day in Scotland. The estimated population was 5 178 248 in 1981 reducing to 5 106 135 in 1991 and to 5 062 011 in 2001 before rising to 5 295 403 in 2011.
Mortality
We obtained mortality information from vital events data held by National Records of Scotland for the periods 1980–82, 1991–92, 2000–02 and 2010–12. In total, there were 190 252 120 497, 171 592 and 161 807 deaths respectively. At least 99.6% of deaths within each period were linked to a Scottish postcode sector (i.e. ‘G12 8’). Note that there was a restructuring of some postcodes in the Scottish Grampian region in 1990. We therefore excluded deaths in 1990 from our analysis as it was not possible to assign death records to the new postcode sector boundaries. We looked at leading causes of death for males and females11 plus accidents and deaths of despair3 (drug- and alcohol-related harm and suicide). Together these causes of death accounted for 80% of the total deaths in Scotland in 1981 (and 74% of the total deaths in 2011). Causes of death (underlying) were coded in accordance with the International Classification of Diseases (ICD) using ICD-9 in 1980–82 and 1991–92 and ICD-10 in 2000–02 and 2010–12. Standard definitions of suicides12 and accidental deaths13 both record deaths due to drug and alcohol poisonings (already accounted for by drug- and alcohol-related deaths). To allow for the summing together of causes without overlap (as illustrated in figure 1), an alternative definition of suicides and accidental deaths that excludes poisonings is given in the Supplementary appendix.
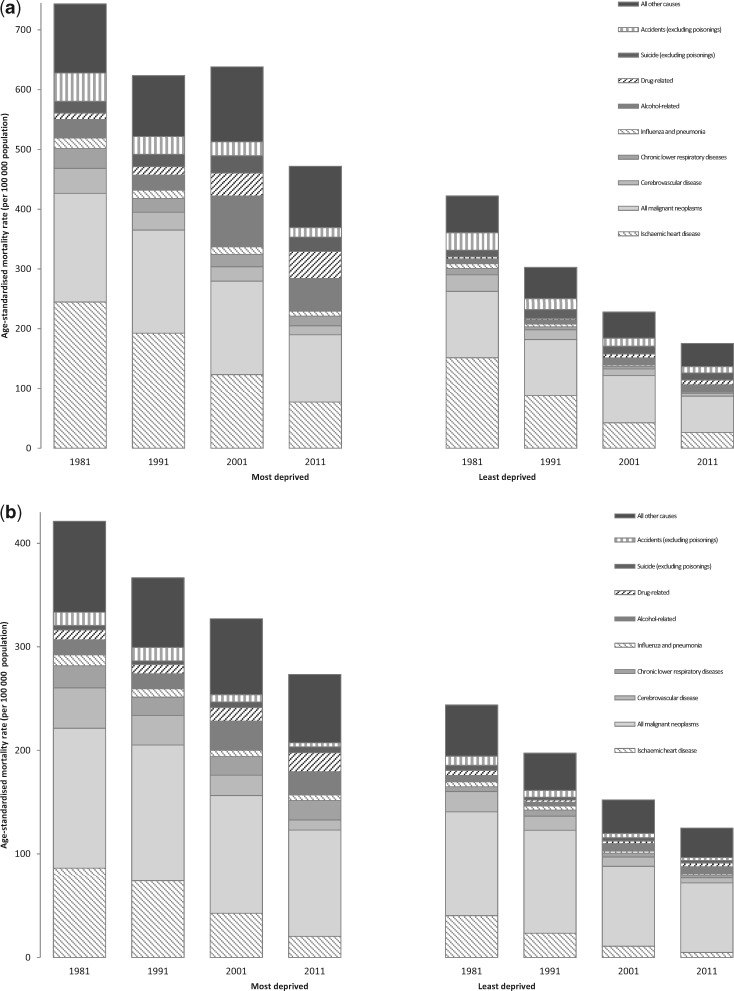
Figure 1.
Stack plot showing all-cause mortality rates (per 100 000 population) for (a) Males, aged 0–64, in the most and least deprived fifths 1981–2011 and (b) females, aged 0–64, in the most and least deprived fifths 1981–2011
Area-level deprivation
Area-level deprivation was measured using Carstairs deprivation scores. Scores were created from four census variables (car ownership, male unemployment, overcrowding and low social class) in 1981, 1991, 2001 and 201114–17 at the postcode sector level of geography. Postcode sectors were chosen as they were believed to be of sufficient size to reliably estimate rates of health events, including mortality.14 There were 1010 postcode sectors in Scotland in 2011 (average population size ∼5000 people, min: 52, max: 21 159).
Analyses
Using the 2013 European standard population, data were aggregated into five-year age bands to calculate directly age-standardized all-cause and cause-specific mortality rates for the periods 1980–82, 1991–92, 2000–02 and 2010–12. Note that the upper age band of the 2013 European standard population is 95+, although using an upper age limit of 90+ is recommended.18 In this study population estimates up to age 90+ are available at postcode sector level in 1991, 2001 and 2011 but only to 85+ in 1981. For 1981, the split of males and females in age groups 85–89 and 90+ in postcode sectors is approximated using population estimates available at the wider Health Board (n = 15, pre-April 2006) level. Age-standardized mortality rates, for males and females separately, are presented for 15 year age groups (0–14, 15–29, 30–44, 45–59, 60–74 and 75+), ages 0–64 and for all ages. We show the change in rates between 1981 and 2011 (2011 rate minus the 1981 rate, divided by the 1981 rate and expressed as a percentage) but it is also straightforward to calculate the change in rates between decades and absolute rate changes over time. We divided the population at each census into population-weighted fifths (most to least deprived) according to Carstairs deprivation score of the postcode sector of residence. Mortality rates by deprivation fifths are presented for premature mortality, an important indicator of the overall health of the population. Since the starting point of our analysis is 1980–82, when average life expectancy was lower, we define premature mortality here as deaths of those aged 0–64.
Results
All-cause mortality
Male and female all-cause mortality rates decreased between 1981 and 2011 across all age groups (table 1). Female mortality was 26% lower than males (for all ages) in 2011, compared to 36% lower in 1981. Rates decreased most in the youngest age group (0–14 years) and at 45–74 years. For males, the smallest declines in all-cause mortality between 1981 and 2011 were in age groups 15–29 and 30–44 (reductions of 22 and 6%, respectively). The reductions were lower than in other age groups due in part to an increase in rates between 1991 and 2001 (from 98 to 113 deaths per 100 000 population in the 15–29 age group and from 174 to 204 deaths per 100 000 population in the 30–44 age group). The slowest rate of decline for females was in the 15–29 age group (12%). For all ages, male and female mortality decreased by 43 and 34%, respectively, between 1981 and 2011. Rates of decline were steeper in the 0–64 age group (48% for males and 43% for females) than for all ages.
Table 1.
Age-standardized all-cause and cause-specific mortality rates (per 100 000 population) for males and females, 1980–82, 1991–92, 2000–02 and 2010–12 with % change showing overall percentage change in rates between 1981 and 2011
| Males | Females | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Years | % Change | Years | % Change | |||||||
| Age | 1980–82 | 1991–92 | 2000–02 | 2010–12 | 81–11 | 1980–82 | 1991–92 | 2000–02 | 2010–12 | 81–11 |
| All causes | ||||||||||
| 0–14 | 121 | 77 | 53 | 38 | −68 | 92 | 56 | 41 | 29 | −68 |
| 15–29 | 98 | 98 | 113 | 77 | −22 | 39 | 38 | 39 | 34 | −12 |
| 30–44 | 209 | 174 | 204 | 196 | −6 | 130 | 105 | 102 | 100 | −23 |
| 45–59 | 1069 | 810 | 687 | 525 | −51 | 617 | 492 | 416 | 347 | −44 |
| 60–74 | 4310 | 3668 | 2890 | 2049 | −52 | 2408 | 2147 | 1735 | 1377 | −43 |
| 75+ | 15 710 | 13 993 | 11 678 | 9830 | −37 | 10 881 | 9613 | 8783 | 7762 | −29 |
| 0–64 | 568 | 446 | 394 | 296 | −48 | 327 | 266 | 224 | 186 | −43 |
| All ages | 2424 | 2096 | 1739 | 1390 | −43 | 1551 | 1357 | 1196 | 1028 | −34 |
| Ischaemic heart disease (ICD-9 410–414; ICD-10 I20–25) | ||||||||||
| 0–14 | 0 | 0 | 0 | 0 | – | 0 | 0 | 0 | 0 | – |
| 15–29 | 1 | 1 | 1 | 1 | – | 0 | 0 | 0 | 0 | – |
| 30–44 | 46 | 28 | 20 | 16 | −65 | 9 | 7 | 5 | 4 | −60 |
| 45–59 | 432 | 287 | 160 | 101 | −77 | 115 | 84 | 41 | 24 | −79 |
| 60–74 | 1556 | 1285 | 736 | 374 | −76 | 734 | 589 | 327 | 146 | −80 |
| 75+ | 4054 | 3675 | 2667 | 1630 | −60 | 2574 | 2388 | 1770 | 1025 | −60 |
| 0–64 | 200 | 139 | 79 | 46 | −77 | 62 | 47 | 24 | 12 | −81 |
| All ages | 720 | 607 | 398 | 232 | −68 | 378 | 331 | 223 | 122 | −68 |
| Cancer (ICD-9 140–208; ICD-10 C00–97) | ||||||||||
| 0–14 | 6 | 3 | 3 | 2 | −62 | 4 | 4 | 2 | 2 | – |
| 15–29 | 9 | 6 | 6 | 5 | −45 | 8 | 6 | 5 | 5 | −35 |
| 30–44 | 37 | 32 | 25 | 21 | −42 | 52 | 44 | 33 | 30 | −42 |
| 45–59 | 282 | 253 | 208 | 158 | −44 | 253 | 239 | 195 | 164 | −35 |
| 60–74 | 1186 | 1186 | 1038 | 839 | −29 | 672 | 739 | 672 | 617 | −8 |
| 75+ | 2542 | 2742 | 2658 | 2533 | 0 | 1315 | 1412 | 1536 | 1545 | 17 |
| 0–64 | 141 | 128 | 112 | 83 | −41 | 119 | 113 | 93 | 80 | −33 |
| All ages | 492 | 503 | 460 | 404 | −18 | 294 | 309 | 297 | 282 | −4 |
| Stroke (ICD-9 430–438; ICD-10 I60–69, G45) | ||||||||||
| 0–14 | 0 | 0 | 0 | 0 | – | 1 | 0 | 0 | 0 | – |
| 15–29 | 3 | 2 | 1 | 1 | – | 2 | 1 | 1 | 1 | – |
| 30–44 | 10 | 6 | 5 | 5 | −53 | 11 | 7 | 5 | 3 | −76 |
| 45–59 | 62 | 40 | 29 | 18 | −71 | 55 | 38 | 25 | 14 | −74 |
| 60–74 | 456 | 313 | 202 | 103 | −77 | 339 | 231 | 150 | 77 | −77 |
| 75+ | 2482 | 1992 | 1553 | 931 | −62 | 2350 | 1858 | 1512 | 952 | −60 |
| 0–64 | 34 | 22 | 16 | 9 | −73 | 29 | 19 | 13 | 7 | −76 |
| All ages | 314 | 241 | 181 | 106 | −66 | 282 | 215 | 167 | 102 | −64 |
| Chronic lower respiratory diseases (ICD-9 490–494, 496; ICD-10 J40–47) | ||||||||||
| 0–14 | 1 | 0 | 0 | 0 | – | 1 | 0 | 0 | 0 | – |
| 15–29 | 1 | 1 | 1 | 0 | – | 1 | 1 | 1 | 0 | – |
| 30–44 | 3 | 1 | 1 | 2 | – | 2 | 2 | 1 | 1 | – |
| 45–59 | 37 | 21 | 17 | 14 | −62 | 24 | 14 | 17 | 15 | −37 |
| 60–74 | 256 | 194 | 171 | 122 | −52 | 86 | 118 | 131 | 123 | 42 |
| 75+ | 918 | 885 | 739 | 561 | −39 | 175 | 230 | 384 | 423 | 142 |
| 0–64 | 21 | 13 | 11 | 8 | −61 | 11 | 10 | 9 | 9 | −21 |
| All ages | 133 | 116 | 99 | 74 | −45 | 36 | 44 | 60 | 62 | 74 |
| Influenza and pneumonia(ICD-9 480–488; ICD-10 J09–J18) | ||||||||||
| 0–14 | 3 | 1 | 0 | 1 | – | 3 | 1 | 1 | 0 | – |
| 15–29 | 2 | 1 | 0 | 1 | – | 1 | 1 | 0 | 0 | – |
| 30–44 | 5 | 3 | 2 | 2 | −56 | 3 | 2 | 1 | 2 | – |
| 45–59 | 20 | 15 | 12 | 8 | −62 | 13 | 10 | 7 | 5 | −58 |
| 60–74 | 161 | 104 | 56 | 43 | −73 | 92 | 61 | 32 | 25 | −73 |
| 75+ | 1766 | 1443 | 732 | 557 | −67 | 1229 | 1036 | 580 | 436 | −65 |
| 0–64 | 12 | 9 | 6 | 4 | −66 | 8 | 5 | 4 | 3 | −65 |
| All ages | 191 | 151 | 78 | 59 | −69 | 130 | 106 | 59 | 45 | −65 |
| Dementia and Alzheimer’s disease (ICD-9 290, 331.0; ICD-10 F01, F03, G30) | ||||||||||
| 0–14 | 0 | 0 | 0 | 0 | – | 0 | 0 | 0 | 0 | – |
| 15–29 | 0 | 0 | 0 | 0 | – | 0 | 0 | 0 | 0 | – |
| 30–44 | 0 | 0 | 0 | 0 | – | 0 | 0 | 0 | 0 | – |
| 45–59 | 1 | 0 | 0 | 0 | – | 0 | 1 | 0 | 0 | – |
| 60–74 | 9 | 10 | 18 | 24 | 173 | 8 | 10 | 15 | 19 | 130 |
| 75+ | 105 | 209 | 423 | 683 | 550 | 126 | 241 | 528 | 804 | 537 |
| 0–64 | 0 | 0 | 0 | 1 | – | 0 | 0 | 0 | 0 | – |
| All ages | 11 | 21 | 41 | 66 | 494 | 13 | 24 | 50 | 76 | 490 |
| Alcohol-related (ICD-9 291, 303, 3050, 4255, 5710–5715, 5718–5719, E860; ICD-10 F10, K70, K73, X45, X65, Y15, G31.2, G62.1, I42.6, K29.2, K74.0–K74.2, K74.6, K86.0) | ||||||||||
| 0–14 | 0 | 0 | 0 | 0 | – | 0 | 0 | 0 | 0 | – |
| 15–29 | 1 | 1 | 2 | 2 | – | 0 | 0 | 1 | 1 | – |
| 30–44 | 12 | 13 | 27 | 21 | 85 | 6 | 7 | 12 | 12 | 91 |
| 45–59 | 35 | 35 | 88 | 61 | 76 | 17 | 18 | 38 | 29 | 69 |
| 60–74 | 41 | 40 | 98 | 77 | 87 | 20 | 20 | 35 | 29 | 41 |
| 75+ | 22 | 22 | 38 | 37 | 65 | 12 | 11 | 14 | 13 | 8 |
| 0–64 | 15 | 15 | 38 | 28 | 81 | 8 | 8 | 16 | 13 | 65 |
| All ages | 19 | 18 | 44 | 33 | 80 | 9 | 10 | 17 | 15 | 55 |
| Drug-related (ICD-9 292, 304, 305.2–305.8, E850–858, E950.0–E950.5, E962.0, E980.0–E980.5; ICD-10 F11–16, F19, X40–44, X60–64, X85, Y10–14) | ||||||||||
| 0–14 | 0 | 0 | 0 | 0 | – | 0 | 0 | 0 | 0 | – |
| 15–29 | 7 | 13 | 33 | 23 | 233 | 3 | 6 | 9 | 7 | 101 |
| 30–44 | 7 | 10 | 29 | 47 | 537 | 8 | 5 | 10 | 16 | 94 |
| 45–59 | 8 | 6 | 9 | 18 | 128 | 12 | 6 | 6 | 12 | −3 |
| 60–74 | 5 | 4 | 3 | 6 | 10 | 8 | 4 | 5 | 5 | −37 |
| 75+ | 5 | 4 | 3 | 4 | −4 | 4 | 4 | 2 | 3 | – |
| 0–64 | 6 | 7 | 17 | 22 | 287 | 7 | 5 | 6 | 9 | 38 |
| All ages | 6 | 7 | 14 | 19 | 227 | 6 | 4 | 6 | 8 | 23 |
| Suicide (ICD-9 E950–959, 980–989; ICD-10 X60–84, Y87.0, Y10–34, Y87.2) | ||||||||||
| 0–14 | 0 | 0 | 1 | 0 | – | 0 | 0 | 1 | 0 | – |
| 15–29 | 18 | 28 | 38 | 24 | 36 | 5 | 8 | 9 | 9 | 71 |
| 30–44 | 26 | 30 | 41 | 42 | 64 | 12 | 9 | 12 | 13 | 9 |
| 45–59 | 29 | 25 | 28 | 32 | 8 | 21 | 11 | 10 | 12 | −42 |
| 60–74 | 26 | 21 | 23 | 15 | −44 | 15 | 9 | 9 | 6 | −62 |
| 75+ | 25 | 25 | 20 | 16 | −35 | 12 | 10 | 7 | 5 | −60 |
| 0–64 | 20 | 22 | 28 | 25 | 28 | 11 | 8 | 9 | 9 | −18 |
| All ages | 21 | 22 | 26 | 23 | 11 | 11 | 8 | 8 | 8 | −28 |
| Accidents (ICD-9 E800–929; ICD-10 V01-X59, Y85–86) | ||||||||||
| 0–14 | 17 | 10 | 5 | 2 | −85 | 9 | 7 | 3 | 1 | −93 |
| 15–29 | 47 | 33 | 21 | 22 | −52 | 10 | 9 | 6 | 6 | −34 |
| 30–44 | 36 | 23 | 21 | 38 | 6 | 8 | 7 | 4 | 9 | 6 |
| 45–59 | 45 | 29 | 23 | 25 | −45 | 17 | 9 | 8 | 11 | −35 |
| 60–74 | 70 | 49 | 40 | 34 | −51 | 40 | 26 | 17 | 18 | −55 |
| 75+ | 338 | 256 | 189 | 202 | −40 | 378 | 237 | 187 | 166 | −56 |
| 0–64 | 38 | 25 | 20 | 23 | −39 | 12 | 9 | 6 | 7 | −38 |
| All ages | 69 | 49 | 37 | 41 | −41 | 49 | 32 | 24 | 23 | −53 |
Rates are shown for all ages and for broad age groups. Rates for 0–64 years and for all ages are shown in bold/italic. Mortality rates are rounded to the nearest whole number while % change shows the percentage change in actual (unrounded) rates. Note that % change is not calculated, for a particular age group, when cause-specific mortality rates are consistently <5 per 100 000 population over time.
Cause-specific mortality
There were large declines in ischaemic heart disease deaths for males and females in all age groups (table 1). Cancer mortality rates decreased between 1981 and 2011 with most of the reduction in younger age groups. There was no reduction in rates of cancer mortality for males aged 75+ while rates for females aged 75+ increased by 17%. Rates for deaths due to stroke, influenza and pneumonia decreased by over 60% between 1981 and 2011. Mortality rates from chronic lower respiratory diseases almost halved for males between 1981 and 2011 while rates increased by 74% for females over the same period. Deaths from dementia and Alzheimer’s disease have increased substantially for males and females in the oldest age group. Rates of alcohol-related deaths and drug-related deaths also increased. For males, alcohol-related death rates increased by 80% and drug-related deaths rates by 227%. Most of the increase in drug-related deaths occurred in the 30–44 age group and rates for those aged 30+ have continued to increase over the last decade. For females, alcohol- and drug-related death rates increased by 55 and 23%, respectively, between 1981 and 2011. Mortality rates due to suicide increased for males aged 15–59 and for females aged 15–44; however, there was a noticeable decline (37%) in male suicide of those aged 15–29 between 2001 and 2011. Rates of accidental deaths reduced (by 41 and 53% for males and females, respectively) with reductions across most age groups. There was a modest increase in the rate of accidental deaths for males and females aged 30–44.
Mortality by deprivation
There is a strong correlation between mortality and deprivation in Scotland, which has persisted over time (Supplementary appendix figure A1). Between 1981 and 2011, mortality rates for males aged 0–64 in the most deprived areas declined by 271 per 100 000 population compared to 247 per 100 000 population in the least deprived areas. In contrast, there was a relative reduction in rates of 37% in the most deprived areas compared to 58% in the least deprived (table 2). For females there were greater absolute declines in mortality rates in the most deprived areas (148 per 100 000 population compared to 119 per 100 000 population in the least deprived areas) but relative reductions were less (35% in the most deprived areas compared to 49% in the least deprived). For most causes of death, relative reductions in mortality rates between 1981 and 2011 were greater in the least deprived areas, compared to the most deprived (one exception is strokes in females where the relative reductions in rates over time were roughly comparable across deprivation groups). For alcohol- and drug-related deaths and male suicide, relative increases (or absolute increases where rates are relatively low) were higher in more deprived areas. Note that dementia and Alzheimer’s disease mortality rates are not shown in table 2 due to insufficient deaths at ages 0–64.
Table 2.
Age-standardized all-cause and cause-specific mortality rates (per 100 000 population) for males and females aged 0–64 in 1980–82, 1991–92, 2000–02 and 2010–12 with % change showing overall percentage change in rates between 1981 and 2011
| Males | Females | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Years | % Change | Years | % Change | |||||||
| 1980–82 | 1991–92 | 2000–02 | 2010–12 | 81–11 | 1980–82 | 1991–92 | 2000–02 | 2010–12 | 81–11 | |
| All causes | ||||||||||
| Most deprived | 743 | 624 | 638 | 472 | −37 | 421 | 367 | 327 | 273 | −35 |
| 2 | 617 | 502 | 448 | 346 | −44 | 356 | 291 | 247 | 211 | −41 |
| 3 | 550 | 424 | 370 | 278 | −49 | 314 | 253 | 218 | 181 | −42 |
| 4 | 507 | 383 | 314 | 234 | −54 | 299 | 218 | 182 | 154 | −48 |
| Least deprived | 422 | 303 | 228 | 175 | −58 | 244 | 197 | 152 | 125 | −49 |
| All Scotland | 568 | 446 | 394 | 296 | −48 | 327 | 266 | 224 | 186 | −43 |
| Ischaemic heart disease (ICD-9 410–414; ICD-10 I20–25) | ||||||||||
| Most deprived | 245 | 192 | 123 | 77 | −68 | 86 | 74 | 43 | 20 | −76 |
| 2 | 220 | 160 | 94 | 55 | −75 | 72 | 56 | 28 | 15 | −79 |
| 3 | 199 | 136 | 77 | 44 | −78 | 56 | 43 | 21 | 12 | −79 |
| 4 | 186 | 117 | 63 | 35 | −81 | 56 | 34 | 18 | 9 | −84 |
| Least deprived | 152 | 88 | 43 | 26 | −83 | 40 | 23 | 11 | 5 | −88 |
| All Scotland | 200 | 139 | 79 | 46 | −77 | 62 | 47 | 24 | 12 | −81 |
| Cancer (ICD-9 140–208; ICD-10 C00–97) | ||||||||||
| Most deprived | 182 | 173 | 157 | 113 | −38 | 135 | 131 | 114 | 103 | −24 |
| 2 | 151 | 140 | 122 | 95 | −37 | 124 | 121 | 98 | 84 | −32 |
| 3 | 137 | 121 | 107 | 80 | −42 | 121 | 108 | 93 | 80 | −34 |
| 4 | 121 | 114 | 100 | 74 | −38 | 114 | 103 | 86 | 71 | −38 |
| Least deprived | 111 | 94 | 79 | 61 | −45 | 100 | 99 | 77 | 67 | −33 |
| All Scotland | 141 | 128 | 112 | 83 | −41 | 119 | 113 | 93 | 80 | −33 |
| Stroke (ICD-9 430–438; ICD-10 I60–69, G45) | ||||||||||
| Most deprived | 42 | 30 | 24 | 15 | −64 | 39 | 28 | 20 | 10 | −75 |
| 2 | 38 | 25 | 18 | 11 | −70 | 33 | 20 | 16 | 9 | −73 |
| 3 | 35 | 23 | 15 | 8 | −76 | 27 | 21 | 13 | 7 | −75 |
| 4 | 30 | 19 | 12 | 8 | −74 | 28 | 14 | 10 | 5 | −82 |
| Least deprived | 28 | 16 | 11 | 5 | −83 | 20 | 14 | 9 | 5 | −74 |
| All Scotland | 34 | 22 | 16 | 9 | −73 | 29 | 19 | 13 | 7 | −76 |
| Chronic lower respiratory diseases (ICD-9 490–494, 496; ICD-10 J40–47) | ||||||||||
| Most deprived | 33 | 23 | 21 | 16 | −52 | 21 | 18 | 18 | 19 | −12 |
| 2 | 24 | 15 | 13 | 11 | −56 | 12 | 10 | 12 | 12 | 2 |
| 3 | 20 | 13 | 11 | 8 | −62 | 9 | 10 | 7 | 8 | −13 |
| 4 | 15 | 9 | 6 | 5 | −65 | 8 | 7 | 5 | 5 | −40 |
| Least deprived | 11 | 5 | 4 | 3 | −77 | 5 | 6 | 4 | 3 | −45 |
| All Scotland | 21 | 13 | 11 | 8 | −61 | 11 | 10 | 9 | 9 | −21 |
| Influenza and pneumonia (ICD-9 480–488; ICD-10 J09-J18) | ||||||||||
| Most deprived | 18 | 14 | 13 | 8 | −52 | 11 | 8 | 6 | 5 | −50 |
| 2 | 12 | 10 | 7 | 6 | −52 | 10 | 5 | 4 | 4 | −62 |
| 3 | 12 | 7 | 4 | 4 | −72 | 7 | 4 | 3 | 2 | −68 |
| 4 | 11 | 9 | 4 | 2 | −78 | 8 | 4 | 2 | 2 | −77 |
| Least deprived | 8 | 5 | 3 | 2 | −81 | 5 | 4 | 2 | 1 | −69 |
| All Scotland | 12 | 9 | 6 | 4 | −66 | 8 | 5 | 4 | 3 | −65 |
| Alcohol-related (ICD-9 291, 303, 3050, 4255, 5710–5715, 5718–5719, E860; ICD-10 F10, K70, K73, X45, X65, Y15, G31.2, G62.1, I42.6, K29.2, K74.0-K74.2, K74.6, K86.0) | ||||||||||
| Most deprived | 31 | 25 | 85 | 55 | 76 | 14 | 14 | 28 | 23 | 58 |
| 2 | 14 | 19 | 48 | 36 | 146 | 9 | 11 | 20 | 16 | 90 |
| 3 | 12 | 15 | 31 | 25 | 105 | 6 | 7 | 15 | 12 | 103 |
| 4 | 11 | 11 | 24 | 17 | 53 | 5 | 6 | 11 | 9 | 100 |
| Least deprived | 8 | 7 | 11 | 10 | 29 | 6 | 3 | 7 | 6 | 6 |
| All Scotland | 15 | 15 | 38 | 28 | 81 | 8 | 8 | 16 | 13 | 65 |
| Drug-related (ICD-9 292, 304, 305.2–305.8, E850–858, E950.0-E950.5, E962.0, E980.0-E980.5; ICD-10 F11–16, F19, X40–44, X60–64, X85, Y10–14) | ||||||||||
| Most deprived | 11 | 14 | 39 | 45 | 327 | 10 | 9 | 13 | 18 | 90 |
| 2 | 6 | 9 | 18 | 27 | 381 | 8 | 5 | 8 | 10 | 26 |
| 3 | 6 | 6 | 13 | 17 | 198 | 5 | 3 | 6 | 8 | 64 |
| 4 | 4 | 5 | 9 | 13 | 266 | 6 | 3 | 3 | 5 | −9 |
| Least deprived | 3 | 2 | 6 | 8 | 124 | 5 | 2 | 2 | 4 | −25 |
| All Scotland | 6 | 7 | 17 | 22 | 287 | 7 | 5 | 6 | 9 | 38 |
| Suicide (ICD-9 E950–959, 980–989; ICD-10 X60–84, Y87.0, Y10–34, Y87.2) | ||||||||||
| Most deprived | 29 | 33 | 41 | 35 | 19 | 13 | 11 | 13 | 13 | −7 |
| 2 | 20 | 23 | 33 | 31 | 58 | 12 | 8 | 10 | 10 | −17 |
| 3 | 19 | 18 | 27 | 24 | 25 | 10 | 7 | 9 | 9 | −9 |
| 4 | 17 | 20 | 22 | 22 | 29 | 9 | 5 | 6 | 8 | −17 |
| Least deprived | 14 | 17 | 16 | 14 | 0 | 9 | 5 | 5 | 5 | −50 |
| All Scotland | 20 | 22 | 28 | 25 | 28 | 11 | 8 | 9 | 9 | −18 |
| Accidents (ICD-9 E800–929; ICD-10 V01-X59, Y85–86) | ||||||||||
| Most deprived | 48 | 30 | 25 | 41 | −15 | 13 | 14 | 7 | 14 | 3 |
| 2 | 40 | 28 | 22 | 23 | −42 | 13 | 8 | 5 | 7 | −44 |
| 3 | 38 | 25 | 20 | 21 | −45 | 12 | 10 | 6 | 8 | −37 |
| 4 | 35 | 25 | 19 | 17 | −53 | 12 | 6 | 6 | 4 | −63 |
| Least deprived | 30 | 18 | 13 | 15 | −49 | 9 | 7 | 4 | 4 | −58 |
| All Scotland | 38 | 25 | 20 | 23 | −39 | 12 | 9 | 6 | 7 | −38 |
Rates are shown by Carstairs deprivation score (most to least deprived fifth). Rates for the whole of Scotland are shown in bold/italic. Mortality rates are rounded to the nearest whole number while % change shows the percentage change in actual (unrounded) rates.
Additional causes of death
Included in Supplementary appendix tables A1–A3 are breakdowns of cancer deaths by selected causes. Lung cancer mortality declined by 44% for males but increased for females in older age groups (Supplementary appendix table A1). Female breast cancer mortality rates decreased by 29% between 1981 and 2011 while prostate cancer mortality rates increased by 25% over the same period. There were reductions in rates of death due to colorectal cancer between 1991 and 2011 and stomach cancer between 1981 and 2011. Deaths due to lung cancer and colorectal cancer, in the under 65 s, decreased most in the least deprived areas (Supplementary appendix table A2) while for other cancers evidence of a deprivation gradient was less clear.
For suicides excluding poisonings (Supplementary appendix table A1), patterns were similar to all suicides although rates were lower across all time points and for all ages. For accidental deaths excluding poisonings, rates only differed to all accidental deaths in 2011 for age groups 15–74 (reflecting rule changes, with effect from 2011, to how ‘drug abuse’ deaths from ‘acute intoxication’ are coded. Previously recorded as ‘mental and behavioural disorders due to psychoactive substance use’, ‘drug abuse’ deaths from ‘acute intoxication’ are now coded as ‘poisoning’19). Compared to mortality rates for alcohol-related deaths, rates for alcohol-specific deaths20 tend to be slightly lower but with a similarly strong deprivation gradient.
Contribution of specific causes to all-cause mortality rates
Figure 1 shows the contribution of the cause-specific mortality rates to all-cause mortality rates between 1981 and 2011 in the most and least deprived areas for (i) males and (ii) females, aged 0–64. To avoid causes of death overlapping, suicides and accidents excluding poisonings were included in the plots. Rates for these nine causes of death (taken from table 2 and Supplementary appendix table A2) sum to the overall all-cause mortality rate together with the rate for ‘all other causes’. It is clear that despite reductions in mortality rates between 1981 and 2011 rates in the most deprived areas in 2011 remained higher than in the least deprived areas in 1981. As the contribution from deaths due to cancer, circulatory and respiratory causes to all-cause mortality declines over time, we can see the increasing contribution from alcohol- and drug-related causes.
Discussion
All-cause mortality rates in Scotland have declined over the last 30 years. The (absolute and relative) gap between male and female mortality rates has narrowed and there have been reductions in mortality rates across all age groups. We have shown that death rates fell for males aged 15–44 between 2001 and 2011, following a period of increase between 1991 and 2001.4 Of all age groups, the greatest reduction in male mortality between 2001 and 2011 occurred in the 15–29 year age group (32% reduction) while the smallest decline was in the 30–44 year age group (4% reduction). The causes of death driving this finding appear to be drug-related deaths and suicide both of which reduced in the 15–29 year age group between 2001 and 2011 but rose in the 30–44 year age group; suggesting a possible cohort effect for these causes of death.21,22 Despite reductions in all-cause mortality rates across deprivation fifths, rates were higher in the most deprived areas in 2011 than in the least deprived areas in 1981. There were greater absolute reductions in all-cause mortality in the most deprived areas between 1981 and 2011, but relative reductions were highest in the least deprived areas. Overall, absolute inequalities in all-cause mortality in Scotland narrowed between 1981 and 2011 while relative inequalities widened. Narrowing absolute inequalities and widening relative inequalities have been reported elsewhere.7,9,23 Within Europe, some Southern European countries have been successful in reducing relative inequalities.24 This has been attributed to smaller inequalities in smoking and alcohol-related deaths in these countries.
For many causes of death (ischaemic heart disease, cancer, stroke, chronic lower respiratory diseases, influenza and pneumonia and accidents), premature mortality rates decreased over time but generally at a higher rate in the least deprived areas compared to the most deprived. Conversely, premature mortality rates for drug- and alcohol-related deaths and male suicide increased over time with larger increases in more deprived areas. Faster declines in mortality in deprived areas for leading causes of death and at least a flattening of deaths due to drug- and alcohol-related mortality and male suicide would help to decrease widening relative inequalities and reduce premature mortality in Scotland. Recent work has shown that lifespan variation, summarizing the inequality in age of death, is generally lower in countries with higher life expectancy, and countries that have been able to reduce lifespan variation are those which have been more successful in reducing premature mortality.25 A focus on reducing premature deaths in Scotland could lead to lower lifespan variation, in line with other countries,26 and an increase in average life expectancy.
The increase in deaths at younger ages due to alcohol, drugs and suicide, observed in Scotland between 1991 and 2001,4 has since been seen in the USA.3 There appears to be little effect of an upturn in mortality rates due to deaths of despair so far in Europe, but some have suggested the possibility of a lag.27 In Scotland, suicide and alcohol-related mortality rates declined after 2001 but remain above 1991 levels. Rates of drug-related mortality have continued to rise between 2001 and 2011 with Scotland having the highest rate of drug-related deaths in Europe.28 At older ages, deaths due to heart disease, cancer and stroke continue to decline while mortality from dementia and Alzheimer’s disease has increased significantly over each of the last three decades, a trend that looks set to continue. In Europe, only Finland has higher death rates due to dementia and Alzheimer’s disease.
Following a period of stalling life expectancy rates in Scotland, latest estimates suggest that there has been a small decrease in life expectancy for both males and females.29 This has also been observed in the rest of the UK and the USA.1 While other high income countries have also seen recent small declines in average life expectancy, which tend to be driven by mortality (such as respiratory, cardiovascular and Alzheimer’s disease) at older ages, the declines have been offset by previous increases in life expectancy. In the USA almost all the decline was attributable to drug abuse and external causes.1 Scotland not only faces increasing drug-related mortality at younger ages but also increasing deaths at older ages from dementia and Alzheimer’s disease.
Strengths and limitations
This is a large population study examining trends in mortality over a 30 year period allowing assessment of overall progress towards lower mortality rates and reducing inequalities. Over time, there have been changes to how some deaths are coded. An ICD revision in 1999 has meant that some causes of deaths have been assigned to different categories. As a result, any observed changes between 1991 and 2001 (or overall change between 1981 and 2011) may appear larger than it actually is. This should not however affect recent changes in mortality rates between 2001 and 2011. The Carstairs deprivation measure has been subject to some criticism about the variables included in its construction and their appropriateness for use today,30 however, recent work has shown the relative usefulness of Carstairs deprivation scores compared to other deprivation indices.31
Conclusions and policy implications
Despite all-cause mortality rates in Scotland decreasing over the last three decades, rates in the most deprived areas in 2011 remained higher than in the least deprived areas some 30 years previously. For several causes of death, mortality rates reduced most in the least deprived areas. For causes of death due to drug- and alcohol-related harm and male suicide, rates increased at a faster pace in deprived areas. Overall we saw a reduction in absolute inequalities in all-cause mortality. Although this is important from a public health perspective, so too is progress in the reduction of relative inequalities,32 brought about by faster improvements in the health and mortality outcomes of those in the most disadvantaged groups.
Medical advances have been responsible for vast improvements in mortality rates for many causes of death over the last three decades; however, the increases in deaths due to drug and alcohol abuse and suicide need upstream preventative policies which tackle the root causes of these deaths. Deaths from these causes have offset improvements in young adult age groups. Encouragingly, rates have started to decrease over the last 10 years in some age groups where they had previously risen and recent Government policies33–36 may help to drive these rates down further.
Supplementary Material
Acknowledgements
We are grateful to National Records of Scotland for the provision of data. We would like to thank our project steering group for helpful comments on the manuscript.
Funding
This research was funded by the Medical Research Council (MC_UU_12017/13) and the Scottish Government Chief Scientist Office (SPHSU13).
Conflicts of interest: None declared.
Key points
Relative inequalities in all-cause mortality continue to widen in Scotland while absolute inequalities are decreasing.
All-cause mortality rates in the most deprived areas in 2011 were higher than in the least deprived areas in 1981.
Part of the explanation for widening relative inequalities is that for several causes of death rates have reduced but the reductions have been greater in the least deprived areas compared to the most deprived.
Another part of the explanation is that deaths due to drug- and alcohol-related harms and male suicide have increased and at a faster rate in more deprived areas.
Targeting causes due to drug- and alcohol-related harms and male suicide in deprived areas, particularly at younger age groups, may help to reduce widening relative inequalities.
References
- 1. Ho JY, Hendi AS. Recent trends in life expectancy across high income countries: retrospective observational study. BMJ 2018;362:k2562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hiam L, Harrison D, McKee M, Dorling D. Why is life expectancy in England and Wales ‘stalling’? J Epidemiol Community Health 2018;72:404–8. [DOI] [PubMed] [Google Scholar]
- 3. Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci USA 2015;112:15078–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Leyland AH, Dundas R, McLoone P, Boddy FA. Cause-specific inequalities in mortality in Scotland: two decades of change. A population-based study. BMC Public Health 2007;7:172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Glasgow Centre for Population Health. Accounting for Scotland’s Excess Mortality: Towards a Synthesis. Available at: https://www.gcph.co.uk/assets/0000/1080/GLA147851_Hypothesis_Report__2_.pdf (25 November 2018, date last accessed).
- 6. Thomas B, Dorling D, Smith GD. Inequalities in premature mortality in Britain: observational study from 1921 to 2007. BMJ 2010;341:c3639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. de Gelder R, Menvielle G, Costa G et al. Long-term trends of inequalities in mortality in 6 European countries. Int J Public Health 2017;62:127–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mackenbach JP, Kulhanova I, Artnik B et al. Changes in mortality inequalities over two decades: register based study of European countries. BMJ 2016; 353:i1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McCartney G, Popham F, Katikireddi SV et al. How do trends in mortality inequalities by deprivation and education in Scotland and England & Wales compare? A repeat cross-sectional study. BMJ Open 2017; 7:e017590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scottish Government. Long-term Monitoring of Health Inequalities, 2017. Available at: http://www.gov.scot/Resource/0051/00515868.pdf (10 August 2018, date last accessed).
- 11.GOV.UK. Research and Analysis. Chapter 2: Trends in Mortality. Available at: https://www.gov.uk/government/publications/health-profile-for-england-2018/chapter-2-trends-in-mortality#leading-causes-of-death-in-2016 (25 November 2018, date last accessed).
- 12.National Records of Scotland. Probable Suicides: Deaths Which Are the Result of Intentional Self-Harm or Events of Undetermined Intent. Available at: https://www.nrscotland.gov.uk/statistics-and-data/statistics/statistics-by-theme/vital-events/deaths/suicides/the-definition-of-the-statistics (10 August 2018, date last accessed).
- 13.National Records of Scotland. Accidental Deaths. The Definition of the Statistics. Available at: https://www.nrscotland.gov.uk/statistics-and-data/statistics/statistics-by-theme/vital-events/deaths/accidental-deaths/the-definition-of-the-statistics (10 August 2018, date last accessed).
- 14. Carstairs V, Morris R. Deprivation and Health in Scotland. Aberdeen: Aberdeen University Press, 1991. [Google Scholar]
- 15. McLoone P. Carstairs Scores for Scottish Postcode Sectors from the 1991 Census. Glasgow: Public Health Research Unit, University of Glasgow, 1994. [Google Scholar]
- 16. McLoone P. Carstairs Scores for Scottish Postcode Sectors from the 2001 Census. Glasgow: MRC Social & Public Health Sciences Unit, University of Glasgow, 2004. [Google Scholar]
- 17. Brown D, Allik M, Dundas R, Leyland AH. Carstairs Scores for Scottish Postcode Sectors, Datazones & Output Areas from the 2011 Census. Glasgow: MRC/CSO Social and Public Health Sciences Unit, University of Glasgow, 2014. [Google Scholar]
- 18.Office for National Statistics. Impact of Varying the 2013 ESP Upper Age Limit on Mortality Statistics. Available at: http://webarchive.nationalarchives.gov.uk/20160106020035/http://www.ons.gov.uk/ons/guide-method/user-guidance/health-and-life-events/revised-european-standard-population-2013–2013-esp-/index.html (10 August 2018, date last accessed).
- 19.National Records of Scotland. Changes to the Coding of Causes of Death between 2010 and 2011. Available at: https://www.nrscotland.gov.uk/files/statistics/vital-events/changes-to-coding-of-causes-of-death-between-2010–2011.pdf (10 August 2018, date last accessed).
- 20.Office for National Statistics. The Impact of Using the New Definition of Alcohol-Specific Deaths. Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/theimpactofusingthenewdefinitionofalcoholspecificdeaths/2017–10–27 (10 August 2018, date last accessed).
- 21. Parkinson J, Minton J, Lewsey J et al. Recent cohort effects in suicide in Scotland: a legacy of the 1980s?. J Epidemiol Community Health 2017;71:194–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Parkinson J, Minton J, Lewsey J et al. Drug-related Deaths in Scotland 1979–2013: Evidence of a Vulnerable Cohort of Young Men Living in Deprived Areas. Available at: https://osf.io/ecbpn/ (10 August 2018, date last accessed). [DOI] [PMC free article] [PubMed]
- 23. Tanaka H, Toyokawa S, Tamiya N et al. Changes in mortality inequalities across occupations in Japan: a national register based study of absolute and relative measures, 1980–2010. BMJ Open 2017;7:e015764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mackenbach JP, Kulhanova I, Menvielle G et al. Trends in inequalities in premature mortality: a study of 3.2 million deaths in 13 European countries. J Epidemiol Community Health 2015;69:207–17. [DOI] [PubMed] [Google Scholar]
- 25. Seaman R, Leyland AH, Popham F. How have trends in lifespan variation changed since 1950? A comparative study of 17 Western European countries. Eur J Public Health 2016;26:360–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Vaupel JW, Zhang Z, van Raalte AA. Life expectancy and disparity: an international comparison of life table data. BMJ Open 2011;1:e000128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Office of Health Economics. Why are Mortality Rates Rising for Middle-Aged White Non-Hispanic Americans? Could it Happen in Europe? Available at: https://www.ohe.org/publications/why-are-mortality-rates-rising-middle-aged-white-non-hispanic-americans-could-it-happen# (25 November 2018, date last accessed).
- 28.EMCDDA. European Drugs Report 2018: Trends and Developments. Available at: http://www.emcdda.europa.eu/system/files/publications/8585/20181816_TDAT18001ENN_PDF.pdf (25 November 2018, date last accessed).
- 29.National Records of Scotland. National Life Tables for Scotland 2015–17. Available at: https://www.nrscotland.gov.uk/files//statistics/life-expectancy-15–17/nat-life-tabs-15–17-pub.pdf (25 November 2018, date last accessed).
- 30. Allik M, Brown D, Dundas R, Leyland AH. Developing a new small-area measure of deprivation using 2001 and 2011 census data from Scotland. Health Place 2016; 39:122–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bertin M, Chevrier C, Pele F et al. Can a deprivation index be used legitimately over both urban and rural areas? Int J Health Geogr 2014;13:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Low A, Low A, Health e. Importance of relative measures in policy on health inequalities. BMJ 2006; 332:967–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Scottish Government. Suicide Prevention Strategy 2013–2016. Available at: http://www.gov.scot/resource/0043/00439429.pdf (10 August 2018, date last accessed).
- 34.Scottish Government. Choose life: A National Strategy and Action Plan to Prevent Suicide in Scotland 2005. Available at: http://www.gov.scot/Resource/Doc/46932/0013932.pdf (10 August 2018, date last accessed).
- 35.Scottish Government. The Road to Recovery: A New Approach to Tackling Scotland’s Drug Problem 2008. Available at: http://www.gov.scot/Resource/Doc/224480/0060586.pdf (10 August 2018, date last accessed).
- 36.Scottish Government. Changing Scotland’s Relationship with Alcohol: A Framework for Action 2009. Available at: http://www.gov.scot/Resource/Doc/262905/0078610.pdf (10 August 2018, date last accessed).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.