Summary
In Ontario, Canada, wait times for magnetic resonance imaging (MRI) scans continue to exceed provincial targets. We sought to determine the incidence of inappropriate hip MRI scan referrals, based on accepted indications for hip MRI. We developed an algorithm to appraise each MRI referral based on a prescan patient questionnaire and the interpretation of the MRI by a musculoskeletal radiologist. After reviewing 84 patient questionnaires, we considered 32.1% of MRI referrals to be inappropriate; 25.9% of the inappropriate MRI referrals were ordered as a preoperative test for potential hip arthroscopy despite the patients showing severe osteoarthritis. Having no prior radiographic examination was the most common reason for inappropriate referrals, regardless of pathology (48.1%). With limited MRI scanner time available in Ontario, it is essential that guidelines and training be improved on the indications for hip MRI to reduce the wait times for these specialized tests.
Despite ongoing efforts and multiple government interventions, wait times for magnetic resonance imaging (MRI) continue to lag behind the provincial standard. Most recent reports suggest that the average Canadian in Ontario will wait 6 weeks for an MRI, despite the province setting a target of 28 days.1 This lag calls into question both the appropriateness and the increasing volumes of referrals for MRI scans.
The appropriateness of MRI referrals is an avenue that, to our knowledge, has not been fully explored as a possible intervention for reducing wait times. A recent survey found that while 96% of public MRI facilities in Ontario triage requests, only 42% use documented guidelines to help organize referrals and none use quality-assurance measures or have implemented appropriateness strategies to reduce the problematic wait times.2 Further insight is needed to determine whether the inappropriateness of MRI referrals from the ordering physician is responsible for the long wait times and health care expenditure on diagnostic imaging.
Magnetic resonance imaging has become a useful diagnostic tool for assessing a patient’s condition and determining the appropriate course of treatment owing to its high specificity and sensitivity to intra-articular cartilage pathologies and deformities.3 However, in many cases a less costly imaging technique, such as a plain radiograph imaging series, is sensitive enough to ascertain the same diagnosis. Additionally, MRI has become an important preoperative test when determining the indications for hip arthroscopy.3 Arthroscopy provides the ability to examine and surgically repair the cartilage of the hip joint. The minimal invasiveness and quicker estimated recovery period associated with this procedure has resulted in hip arthroscopy becoming the gold standard for the treatment of hip-related intra-articular pathologies, such as labral tears and femoroacetabular impingement (FAI).3
Hip arthroscopy is one of the fastest developing fields in orthopedic surgery, with a 600% increase in its utilization over a 5-year period.4 Proper patient selection is imperative at all stages to obtain the best possible results from this procedure. For example, it has been shown that hip arthroscopies performed in older patients, or even younger patients with joint space narrowing suggestive of osteoarthritis, have minimal benefit and a higher rate of subsequent total hip arthroplasty procedure3 than other types of patients.
We recently surveyed patients who were referred for MRI scans at a tertiary hospital in Ontario specializing in musculoskeletal radiology to identify the prevalence of inappropriate scan requests. Patients completed a questionnaire to collect information regarding clinical symptoms and the suspected diagnoses/reasons for referral. The subsequent interpretation of the MRI by a musculoskeletal radiologist was then used to determine an appropriateness classification. We cross-referenced patients’ questionnaire responses with each MRI scan interpretation from a musculoskeletal radiologist to verify the indication for the referral, elucidate the patients’ medical history and analyze the relevance from previous diagnostic test results. From there, we analyzed the referral through an appropriateness classification, categorizing the referrals as “appropriate MRI referral,” “may be an appropriate MRI referral,” or “not an appropriate MRI referral.”
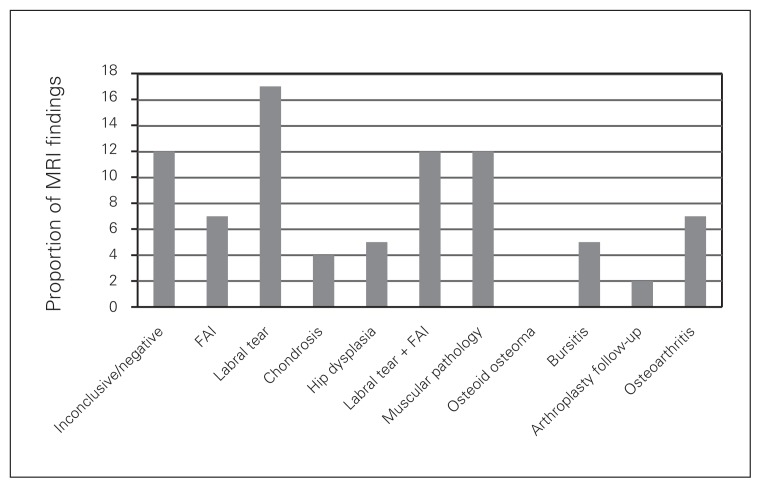
The results of the MRI exams are shown in Figure 1. The 2 most common appropriate pre-MRI differential diagnoses of hip pathology were labral tears (n = 32) and/or FAI (n = 21). It is worth mentioning that 4 of the pathological conclusions (chondrosis, hip dysplasia, osteoarthritis and osteoid osteoma) are typically diagnosed with plain radiographs. These conditions accounted for 21.4% (18/84) of the ordered MRI scans. Only 2 scans diagnosed hip fractures, which aligned with current literature supporting the use of plain radiographs as the gold standard imaging modality to identify this pathology rather than MRI scans, which are used in cases of occult fractures. Based on the musculoskeletal radiologists’ interpretations, plain radiographs were recommended in 2 different cases following their respective MRI scans. Finally, of the 12 inconclusive/normal results, 7 MRI scans were done to rule out labral tears or FAI.
Fig. 1.
Diagnoses based on magnetic resonance imaging (MRI) scans. FAI = femoroacetabular impingement.
Based on the appropriateness criteria, we considered 32.1% (27/84) of referrals to be inappropriate. Having no prior radiographic examination was the most common reason for inappropriate referrals, regardless of pathology (48.1%; 13/27). Most MRI referrals came from primary care sports doctors (n = 40); 42.5% (17/40) of these referrals were deemed inappropriate. Additionally, 25.9% (7/27) of the inappropriate MRI referrals were ordered as a preoperative test for potential hip arthroscopy, despite those patients showing severe osteoarthritis. An inappropriate referral related to hip arthroscopy was defined as patients recommended for this procedure despite their preprocedural MRI showing evidence of severe osteoarthritis or hip dysplasia (the most commonly cited contraindications for hip arthroscopy).
We acknowledge that our chosen method of data collection is subject to recall bias; however, these data suggest that more work is needed to determine the appropriateness of MRI scan referrals. Future studies should aim to obtain the referral reasons directly from the requisition or referring physician. Furthermore, a blinded panel of experts in the field should assess the appropriateness of these referrals.
Conclusion
With the number of MRI exams performed in Canada doubling from 0.69 million in 2003–04 to 1.7 million in 2011–12, and a hip MRI costing approximately $900, the potential savings in health care costs from discovering which medical indications are inappropriate for MRI referral are substantial.1 Currently, it is estimated that there is 1 MRI machine for every 278 000 people.1 Despite plans to add more MRI machines, they will not be able to match the increasing demand, as the waiting list is expected to grow by 12 000 patients annually.5 In 2014, the Canadian Institute for Health Information reported that 61 patients per 1000 received an MRI in Ontario. Assuming the predicted growth of demand for these scans since then, removing approximately 30% of inappropriate requests would save around $750 million.
Educating physicians on identifying contraindications in pre-MRI radiographs and on patient selection for hip arthroscopy would eliminate the need to refer patients to specialists and decrease orders for unnecessary MRI examinations. With the volume of MRI referrals increasing, this emphasizes an area where reducing the proportion of inappropriate referrals will substantially reduce health care spending.
Footnotes
This work was presented at the Ontario Medical Association Sports Medicine 2016 Conference.
Competing interests: None declared.
Contributors: All authors contributed substantially to the conception, writing and revision of this article and approved the final version for publication.
References
- 1.Barua B. Waiting your turn: wait times for health care in Canada, 2017 report. Fraser Institute; 2017. [accessed 2019 June 28]. Available: https://www.fraserinstitute.org/studies/waiting-your-turn-wait-times-for-health-care-in-canada-2017. [Google Scholar]
- 2.Emery DJ, Forster AJ, Shojania KG, et al. Management of MRI wait lists in Canada. Healthc Policy. 2009;4:76–86. [PMC free article] [PubMed] [Google Scholar]
- 3.Kelly BT, Williams RJ, Philippon MJ. Hip arthroscopy: current indications, treatment options, and management issues. Am J Sports Med. 2003;31:1020–37. doi: 10.1177/03635465030310060701. [DOI] [PubMed] [Google Scholar]
- 4.Bozic KJ, Chan V, Valone FH, et al. Trends in hip arthroscopy utilization in the United States. J Arthroplasty. 2013;28:140–3. doi: 10.1016/j.arth.2013.02.039. [DOI] [PubMed] [Google Scholar]
- 5.Kundhal P, Chatterjee S, Kundhal K. MRI supply in Canada: What are the issues? Univ Toronto Med J. 2001;79:68–9. [Google Scholar]