Abstract
There is limited research that has examined offense characteristics in homicides committed by individuals with mental illness and with differing psychiatric diagnoses. The aim of this systematic review is to synthesize previous findings of studies analyzing homicide behavior by mentally ill individuals, and reporting any associations between mental illness and method of homicide. We searched four databases (MedLine, PsychINFO, Web of Science and Embase), and identified 52 relevant articles for analysis. Of these 52 articles, nine reported specific information on mental illness and method of homicide. Five out of nine articles revealed an association between schizophrenia/delusional disorder and the use of sharp instruments as a method of homicide. Four out of nine studies revealed an association between mood disorders (bipolar disorder/major depression) and strangulation/asphyxiation/suffocation/drowning. Our review confirms consistency across studies reporting a significant association between close contact methods and schizophrenia/mood disorders. Also identified as possible influential factors concerning weapon choice are illness duration, victim characteristics and planning/lack of planning of the homicide. Additionally, studies revealed up to 96% of severely mentally ill offenders experienced psychiatric symptoms at the time of the homicide. Future research may examine the presence of specific psychiatric symptoms when a mentally ill offender commits a homicide and whether these may be more influential in the method of homicide used than the psychiatric diagnosis of the offender.
Keywords: Homicide method, Homicide, Severe mental illness, Schizophrenia, Mood disorders, Symptoms
1. Introduction
The United Nations Office on Drugs and Crimes (UNODC) estimates that in the year 2012 there were an approximate 437,000 deaths internationally, resulting from homicide. A more recent review from the Home Office Index for the year 2013/2014 reported 526 homicides in England and Wales. While it is only a minority of individuals with severe mental illness (SMI) that are likely to commit homicide, a large proportion of convicted homicide offenders are diagnosed with SMI (Joyal, Côté, Meloche & Hodgins, 2011). The societal impact of homicide is high, and understanding the possible proximal factors that promote homicidal behavior among individuals with SMI is an important first step in the prevention of homicide.
Research has long established an association between homicide and severe mental illness (Monahan, 1992; Côté & Hodgins et al., 1992). A study by Hodgins (2001) revealed 15% of murderers show a severe mental disorder. Indeed, several studies investigating the link between homicide and severe mental illness have found elevated rates of schizophrenia, bipolar disorder and major depression among individuals convicted of homicide (Gottlieb, Gabrielsen & Kramp, 1987; Shaw et al., 2006). Recent research also indicates there is a higher rate of severe mental illness between homicide offenders than in the general population (Schanda et al., 2004; Torrey, 2011; Fazel & Danesh, 2002). Furthermore, a recent study suggests that the prevalence of a mental disorder increases the risk of homicidal behavior by two-fold in men and six-fold in women (Richard-Devantoy, Olie & Gourevitch, 2009). However, the risk of homicidal behavior may differ across major mental disorders (Schanda et al., 2004). Only a handful of studies have examined whether different severe mental illnesses are linked with specific methods of homicide (Rodway et al., 2009; Catanesi et al., 2011). Moreover, research also suggests differences in homicide offense characteristics per diagnostic group (Appleby et al., 2001; Decker, 1993; Häkkänen & Laajasalo, 2006; Häkkänen-Nyholm et al., 2009). Our review hypothesizes that the method of homicide used by an offender with mental illness will be partly influenced by his/her psychiatric diagnosis.
1.1. Severe mental illness
Although there is no internationally agreed definition of severe mental illness (Ruggeri, Leese, Thornicroft, Bisoffi & Tansella, 2000), the term commonly refers to psychiatric diagnoses that require high levels of care and in which there is significant functional impairment. The most common SMIs are schizophrenia, bipolar disorder and major depression, which have high diagnostic validity (Putkonen et al., 2001; Häkkänen and Laajasalo, 2006) and are the SMIs most consistently linked with homicide (Schanda et al., 2004).
1.1.1. Schizophrenia
Although it is only a minor subgroup of individuals with schizophrenia who are at risk for violence (Joyal et al., 2011), previous research has also consistently linked schizophrenia to homicide (Golenkov et al., 2011; Shaw et al., 2006). Indeed, research does suggest, more generally, that individuals with schizophrenia are at increased risk for acting violently (Kooyman, Dean, Harvey & Walsh, 2007) as well as being at a higher risk than the general population of being convicted for violent offenses (Hodgins, 2008). For example, Wallace et al. (1998) found that schizophrenia was associated with a seven-fold increase in the rate of homicide convictions. A recent study reported individuals with schizophrenia are approximately 20 times more likely to commit homicide than the general population (Fazel, Gulati, Linsell, Geddes & Grann, 2009). Similarly, Schanda et al. (2004) revealed an increased likelihood of homicide in women suffering from schizophrenia.
Concerning specific offense characteristics of homicide offenders with schizophrenia, previous research mainly focuses on the presence of psychotic symptoms at the time of the crime and the frequent use of knives/sharp instruments among this group (Lanzkron, 1963; Taylor, 1998; Steury & Choinski, 1995). Indeed, Taylor and colleagues (1998) reported that at the time of the homicide, up to 81% of perpetrators with psychosis (including schizophrenia) were directly motivated by delusions and/or hallucinations. Similarly, Joyal (2004) revealed that approximately 60% of male homicide offenders with schizophrenia were motivated by psychotic symptoms. In addition, research has suggested that individuals experiencing psychotic symptoms and perceptions of threat tend to carry sharp weapons with them (Joyal et al., 2004). This is consistent with existing research reporting the majority of schizophrenic offenders use a sharp instrument as a homicide method, and were found to have the weapon on their person at the time of the crime (Meehan et al., 2006; Rodway et al., 2009).
1.1.2. Bipolar disorder
Although there is no established link in literature between bipolar disorder and homicide, studies indicate bipolar disorder is six times higher in adult prisons than in the general population (Robins & Regier, 1991). Furthermore, up to 7% of homicide offenders in England and Wales have a lifetime diagnosis of bipolar disorder (Oakley, Hynes & Clark, 2009). Findings of research examining the link between bipolar disorder and violence are mixed. For example, although recent studies revealed a greater risk of violence in bipolar disorder than in schizophrenia (Monahan et al., 2001; Oakley, Hynes & Clark, 2009), research also suggests bipolar disorder alone is not associated with an increased likelihood of homicide (Schanda et al., 2004). Indeed, recent studies conclude most violence in bipolar disorder is due to comorbid substance abuse (Pickard & Fazel, 2013; Fazel et al., 2010). However, research on homicide by individuals with bipolar disorder suggests an increased violence risk in bipolar disorder exists even when controlling for alcohol/substance misuse (Volavka, 2013). Additional research revealed a higher risk of violence during acute manic episodes of bipolar disorder (Wulach, 1983; Binder & McNiel 1988; Volavka, 2013). Conversely, Nielssen and Large (2012) suggest mania is not strongly associated with serious violence, and Yoon et al., (2011) found homicide risk to be higher in the depressive phase of bipolar. A more recent study highlights a direct link between the presence of bipolar disorder symptoms and committing a crime on 62% of offenders with bipolar disorder (Peterson et al., 2014), unfortunately, researchers do not specify on the symptoms reported. Additional research focusing on whether homicidal risk differs among depressive and manic episodes of bipolar disorder is needed.
There is a gap in research investigating homicide offense characteristics in bipolar disordered individuals. The small number of studies focusing on offenders with affective disorders and their behavior at the crime scene suggest that there is an association between violence and homicide risk among individuals with bipolar disorder (Oakley, Hynes & Clark, 2009; Rodway et al., 2009). In addition, a high proportion of homicide offenders with affective/mood disorders are female that are less likely to use violent methods than male homicide offenders (Flynn et al., 2013). Additional research investigating offense behaviors and characteristics concerning male and female homicide offenders with bipolar disorder is needed.
1.1.3. Major depression
The relationship between major depression and homicidal behavior has been historically overlooked (Oakley, Hynes & Clark, 2009; Malmquist, 1995). More recently, studies investigating the link between depression and homicide have mainly focused on homicide-suicide cases, where the perpetrators showing depressive symptoms commits suicide no more than one week after committing homicide (Marzuk, Tardiff & Hirsch, 1992). Indeed, up to 75% of offenders committing homicide-suicide have been reported to be clinically depressed at the time of the offense (Rosenbaum, 1990). However, research also indicates homicide-suicide cases share few characteristics with those who commit homicide. For example, homicide-suicide perpetrators are more likely to be older than homicide perpetrators (Saleva, Putkonen, Kiviruusu & Lonqvist, 2006). Previous studies suggest that the homicide-suicide and homicide groups are two different populations that should be examined separately (Rosenbaum, 1990; Malmquist, 1995).
Beyond homicide-suicide, a small number of studies suggest a strong relationship between homicide and depression. For example, Bénézech and Bourgeois (1992) study reported 16-28% of homicide offenders were depressed at the time of the crime. Another study reported mood disorder (mainly depression) to be the most common mental illness among filicide offenders (Flynn et al., 2013). Furthermore, studies have consistently reported high rates of depression among homicide offenders compared to the general population (Teplin, 1990; Oakley, Hynes & Clark, 2009). Indeed, a diagnosis of depression has been associated with a threefold increase of committing violent crime, including homicide or attempted homicide (Fazel, 2015).
Only a very small number of studies have examined offense characteristics among homicide offenders with depressive illness (Matejkowski et al., 2005). Findings suggest offenders are frequently young mothers killing their own children (Flynn et al., 2013) and intimate violent partners or spouses (Liem & Roberts, 2009). High rates of co-morbid alcohol and drug abuse are also frequently reported among homicide offenders with depression (Rosebaum et al., 1986; Matejkowski et al., 2005). Further research investigating offense characteristics and behavior at the time of the crime in cases of homicide committed by depressed individuals, and not followed by suicide, is needed.
1.2. Previous research on methods of homicide
Information concerning methods of homicide is accessible through official crime statistics and studies on characteristics of homicides in general. According to the United Nations Office on Drugs and Crime annual study on global homicide (UNODC, 2013) sharp instruments are more frequently used in Europe and Oceania, while firearms are the most frequent homicide method in the United States and Italy (Matejkowski et al., 2005; Saleva et al., 2006) arguably a result of less restrictive gun laws and homicides resulting from organized crime (Catanesi et al., 2011). Indeed, the Home Office Homicide Index (2016), in line with previous years, revealed the most common method of homicide in England and Wales to be by a knife or other sharp instrument accounting for 36% of all homicides. The second most common method for female victims is strangulation or asphyxiation, used in 10-20% of all homicides (Häkkänen, 2007). However, Kicking/hitting is the second most frequent method overall, accounting for approximately 18% of all homicides. Only 4% of all homicides in the UK involved killing by shooting. Other common methods reported include: blunt instruments, suffocation, death by fire and poisoning.
Particular homicide methods are associated with the victim-perpetrator relationship, as well as the victim’s and the offender’s gender. For example, research suggests methods involving close contact, such as stabbing and strangulation, commonly involve family members and intimate partners as victims (Appleby et al., 2016). In the case of stranger homicides, kicking/hitting is more likely to be used as a homicide method. Studies indicate that female victims of sexual murders are commonly killed by strangulation since this method is frequently used to overcome their resistance during the sexual act (Häkkänen, 2007). Furthermore, male offenders have been found more likely to use violent methods than female offenders (Flynn et al., 2013).
Only a handful of studies report on the effect of availability of lethal weapons, particularly guns and knives. Findings from a Canadian study suggest that restricting the availability of guns has resulted in a decrease in the rates of homicide by firearms but an increase in the use of all other methods of homicide (Bridges, 2004). Studies examining the use of knives in England report an association between unplanned homicide and the use of sharp weapons, and suggest sharp instruments are the most used homicide method due to their easy accessibility (Hughes et al., 2012).
1.3. Method of homicide and severe mental illness: is there a link?
The majority of studies that have included mentally ill offenders as part of their sample and report on type of mental disorder and homicide method do not directly examine the association between a specific mental illness and method of homicide. For example, a study by Putkonen et al. (2001) examined psychotic and personality disordered women that committed homicide. Although findings described stabbing as the most common method overall, the difference in method according to each diagnostic group of women was not reported. Nevertheless, associations between method of homicide and psychiatric diagnosis have been reported from early research, albeit mainly involving delusional disorders. For example, a study by Steury & Choinski (1995) suggested an association between psychotic offenders and knives.
More recently, a small number of studies have examined the relationship between methods of homicide and distinct mental illnesses. Findings suggest that the method of homicide used is related to the offender’s psychiatric diagnosis (Rodway et al., 2009; Catanesi et al., 2011; Häkkänen & Laajasalo, 2006). For example, Catanesi et al. (2011) found an association between depression and asphyxia, and delusional disorders and sharp instruments. Additional findings include associations between psychosis and knives, and personality disorder/alcohol misuse and hitting/kicking (Häkkänen & Laajasalo, 2006) and affective disorders and less violent methods (Rodway et al., 2009). However, the putative mechanisms underlying the association between SMI and method of homicide are less well understood (Blumenthal & Lavender, 2000).
1.4. Present research review
Diverse findings across research highlight the need for a systematic review to synthesize the results from previous studies examining the characteristics homicide committed by mentally ill individuals, specifically the link between psychopathology and method of homicide. Our aim is to identify which associations between a specific method of homicide and a SMI are consistent across studies from different countries. Our research hypothesizes that the homicide method will be indicative of the mental illness of an offender, as well as of his/her mental state at the time of the offense. Therefore, we also explore whether the method of homicide may be influenced by the presence of specific psychiatric symptoms. In this way, our review will aim to improve our understanding on the differences in homicidal behavior among mentally ill perpetrators according to their diagnostic group and mental state at the time of the homicide.
2. Methodology
2.1. Data Collection
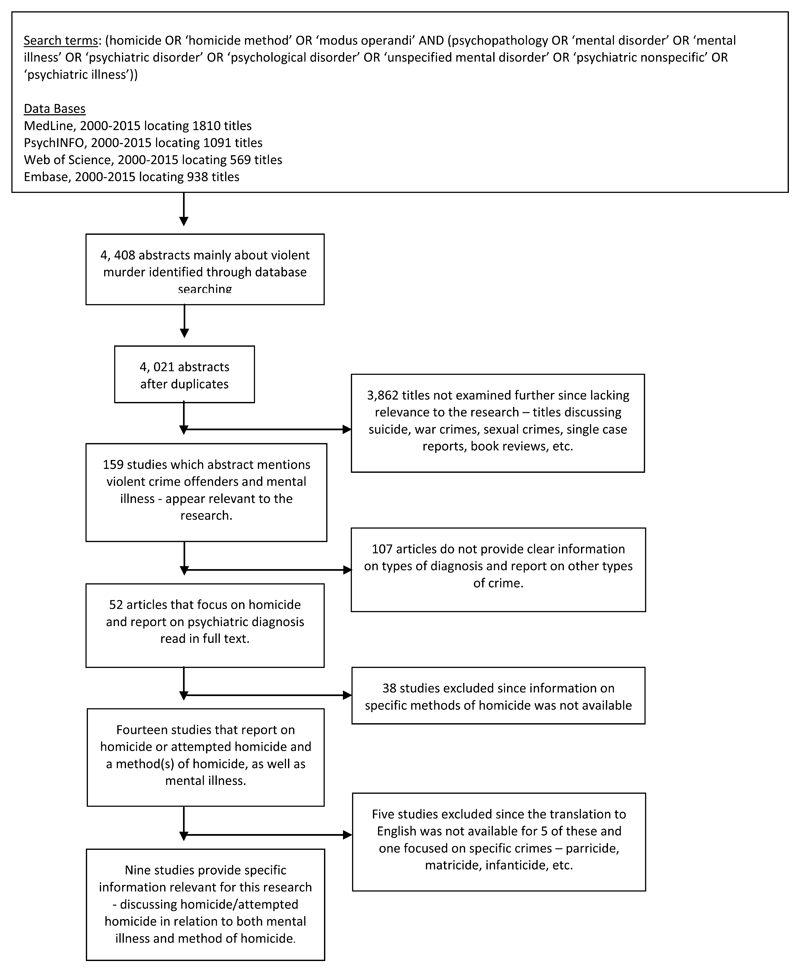
The review consisted of a systematic search of four databases: MedLine, PsychINFO, Web of Science and Embase. For our subject headings and sub headings we used MeSH terms [Homicide OR ‘Homicide Method’ OR ‘Modus Operandi’ AND (Psychopathology OR ‘Mental Disorder’ OR ‘Mental Illness’ OR ‘Psychiatric Disorder’OR ‘Psychological Disorder’ OR ‘Unspecified Mental Disorder’ OR ‘Psychiatric Nonspecific’ OR ‘Psychiatric Illness’)] (see Fig. 1). We included studies from various countries, and also those with a different methodology and sample size since previous research reporting on homicide method and psychopathology is very limited. Our search only reviewed studies including offenders who committed homicide or attempted homicide and provided data on psychopathology and the homicide method used. No studies were included through other sources. Restrictions regarding the date of publication of the paper (2000-2015) were applied to obtain the most recent findings on the subject. The search identified 4,408 records. All titles and abstracts were then reviewed and saved if they appeared relevant to the aims of this paper. Of these, the full texts of 52 studies reporting on both mental illness and homicide were read. Fourteen out of 52 studies were identified as relevant for this review. However, five were removed since four out of five did not have an available translation to the English language and one remaining study only examined a specific type of homicide: parricide. Nine studies that reported on psychiatric diagnosis and the offense characteristics of homicide (one of them being the method of homicide) were included as part of this systematic review.
Fig 1.
Flow diagram of the systematic search for studies reporting on method of homicide and psychiatric diagnosis
2.2. Definitions of mental illness
For the purposes of this review, the term ‘mental illness’ will refer to the diagnostic groups most frequently found in the nine studies included: ‘delusional disorder’, ‘psychosis’, ‘schizophrenia’, ‘mood disorders’, ‘depressive illness’, ‘bipolar disorder’, ‘personality disorders’, ‘organic disorders’ (e.g. epilepsy) and ‘major depression’. However, the definition will exclude ‘alcohol and/or drug dependence/abuse’ due to a lack of consistency across studies reporting rates of comorbidity within diagnostic groups. Additionally, one of the aims of our research is to identify specific aspects of severe mental illness relating to homicide, while excluding ‘alcohol and/or drug dependence/abuse’, since research has already established comorbidity with ‘substance use disorder’ increases violence and homicide risk among mentally ill individuals (Walsh & Buchanan, 2003). Major mental disorders or SMIs will refer to ‘schizophrenia’ ‘bipolar disorder’ and ‘major depression’ only (Häkkänen & Laajasalo, 2006; Matejkowski et al., 2008; Rodway et al., 2009; Yoon et al., 2011; Catanesi et al., 2011). In addition, we will use the category of ‘mood disorders’ or ‘affective disorders’ to encompass both ‘bipolar disorder’ and ‘major depression’, since the majority of the studies reviewed encompass these two disorders in that definition. This is likely due to the fact that most of the studies we reviewed based their categories on the DSM-III-R and DSM-IV-TR classification of disorders, which includes depressive disorders in the same chapter as bipolar disorder, titled ‘Mood Disorders’ (American Psychiatric Association, 2000). However, it is worth noting that according to the DSM-5, both the criteria and classification of bipolar disorders and depressive disorders differs from one another, with the exception of ‘major depressive episode’ within bipolar disorders and ‘major depressive disorder’ within depressive disorders, which are almost identical (American Psychiatric Association, 2013).
Because of the differences in methodological approaches, as well as definitions of ‘homicide’ used across studies, we were unable to perform a meta-analysis. This was also due to the fact that the ‘mental illness’ category in most studies was not clearly defined and in some cases not mutually exclusive; an offender diagnosed with two mental disorders might be included twice in different mental illness categories. For example, in Matejkowski et al.’s (2008) study, the sum of diagnoses equals more than the total number of offenders in the sample since more than one diagnosis per offender was possible.
3. Results
3.1. Summary of included studies
Nine studies reported data on associations between method of homicide and mental illness/type of diagnosis. Three out of nine studies are from Finland (Häkkänen & Laajasalo, 2006; Häkkänen-Nyholm et al., 2009; Putkonen et al., 2001) two are from England and Wales (Rodway et al., 2009; Shaw et al., 2004) and one from England only (Hughes et al., 2012). The remaining studies are from USA, Italy and South Korea. Regarding sample size of homicide offenders, six out of nine studies have a relatively small sample of less than 250 offenders. Three out of nine studies have larger sample sizes, with two having over 1,000 offenders (Rodway et al., 2009; Shaw et al., 2004) and one with 676 perpetrators (Häkkänen-Nyholm et al., 2009). Seven out of nine studies present a sample of mostly males (Rodway et al., 2009; Catanesi et al., 2011; Häkkänen & Laajasalo, 2006; Matejkowski et al., 2008; Shaw et al., 2004; Häkkänen-Nyholm et al., 2009; Yoon et al., 2011). Only one study has an all-female sample (Putkonen et al., 2001) (see Table 1).
Table 1. Studies included.
|
SMI |
||||||||
|---|---|---|---|---|---|---|---|---|
| Studies | Country | Sample | Gender | Mentally ill | Schizophrenia | Mood disorders | Other diagnoses | Method of homicide |
| 1.Hughes,Macaulay and Crichton (2012) | England | 107 | N/A | 96% | 49 | 8 | 50 | (n=57) 100% sharp instrument |
| 2. Rodway, Flynn, Swinson, Roscoe, Hunt, Windfuhr, Kapur, Appleby and Shaw (2009) | England and Wales | 3930 | 90% male 10% female |
27% | 211 | 249 | 587 | (n=460) 48% sharp instrument 11% blunt instrument 3% gun 17% kicking/hitting 11% strangulation 6% suffocation/asphyxiation/drowning 12% other |
| 3. Catanesi, Carabellese, Troccoli, Candello, Grattagliano, Solarino and Fortunato (2011) | Italy | 103 | 85% male 15% female |
81% | 24 | 9 | 54 | (n=103) 39% sharp instrument 11% blunt instrument 20% gun 10% asphyxia 20% other |
| 4. Häkkänen and Laajasalo (2006) | Finland | 182 | 90% male 10% female |
48% | 43 | / | 102 | (n=43) 58% sharp instrument 31% blunt instrument 9% gun 14% kicking /hitting 14% strangulation |
| 5. Matejkowski, Solomon and Cullen (2008) | USA | 95 | 77% male 23% female |
100% | 27 | 72 | 14 | (n=95) 26% sharp instrument 14% blunt instrument 48% gun 13% strangulation/suffocation 4% drowning 4% other |
| 6. Shaw, Amons, Hunt, Flynn, Turnbull, Kapur and Appleby (2004) | England and Wales | 1594 | 87% male 13% female |
31% | 74 | 116 | 276 | (n=1432) 37% sharp instrument 13% blunt instrument 4% gun 19% kicking/hitting 10% strangulation/suffocation 13% other |
| 7. Häkkänen-Nyholm, Repo-Tiihonen, Lindberg, Salenius & Weizmann-Henelius (2009) | Finland | 676 | N/A | 84% | 68 | / | N/A | (n=613) 58% sharp instrument 16% strangulation/suffocation |
| 8. Putknonen, Collander, Marja-Liisa, Honkasalo and Lönnqvist (2001) | Finland | 125 | 100% female | 89% | 34 | / | 77 | (n=111) 64% sharp instrument 8% drowning 3% strangulation/suffocation |
| 9. Yoon, Kim, Choi, Lyu, Kwon, Jang and Park (2011) | Republic of Korea | 62 | 39% male 61% female |
100% | / | 62 | / | (n=62) 21% sharp instrument 14% blunt instrument 11% hitting 35% suffocation 13% other |
Note. Number of SMI offenders and other diagnosis may exceed the total of sample size since more than one diagnosis per offender is possible and offenders with no diagnosis were not included. More than one method of homicide per offender is possible.
Concerning the percentage of mentally ill offenders in their sample, only two out of nine studies presented a 100% sample consisting of all mentally ill offenders who committed or attempted homicide (Matejkowski et al., 2008; Yoon et al., 2011). Three studies consisted of samples with a majority (higher than 80%) of mentally ill offenders (Hughes et al., 2012; Catanesi et al., 2011; Putkonen et al., 2001). Another three presented samples of mentally ill offenders lower than 50% (Rodway et al., 2009; Häkkänen & Laajasalo, 2006; Shaw et al., 2004). Other psychiatric diagnoses reported in the nine studies include ‘personality disorder’ in seven studies (Hughes et al., 2012; Rodway et al., 2009; Catanesi et al., 2011; Häkkänen & Laajasalo, 2006; Shaw et al., 2004; Häkkänen-Nyholm et al., 2009) alcohol dependence in five out of nine studies (Rodway et al., 2009; Häkkänen & Laajasalo, 2006; Shaw et al., 2004; Häkkänen-Nyholm et al., 2009; Putkonen et al., 2001). Only two out of nine studies present diagnoses of organic brain disorder (Catanesi et al., 2011; Häkkänen-Nyholm et al., 2009) and other psychotic disorders (Matejkowski et al., 2008; Putkonen et al., 2001). The category of `other unspecified psychiatric disorder’ was included in two out of nine studies (Hughes et al., 2012; Shaw et al., 2004).
In studies one, five and seven (Hughes et al., 2012; Matejkowski et al., 2008; Häkkänen-Nyholm et al., 2009) the diagnostic categories of mental illness were not mutually exclusive, this means that a mentally ill offender could be classified under two or more psychiatric diagnoses in the same study. For example, study five (2008) findings revealed 73% of offenders as having diagnoses of major depression, bipolar disorder or mania, as well as 41% diagnosed with psychotic disorder, including schizophrenia. In study two (Rodway et al., 2009), the diagnostic categories were mutually exclusive, however over half (56%) shared co-morbid alcohol/drug dependence/misuse. In studies three, four, six and eight (Catanesi et al., 2011; Häkkänen & Laajasalo, 2006; Shaw et al., 2004; Putkonen et al., 2001) diagnostic categories were mutually exclusive. Finally study nine (Yoon et al., 2011) includes offenders with bipolar disorder I only; however comorbid substance use disorder was present in 4-20% of the offenders. It is important to clarify that although the diagnostic categories in a study may be mutually exclusive, this does not dismiss the possibility of dual diagnosis of the offender.
3.2. Associations between method of homicide and psychiatric diagnosis
Of the studies included in this review, the associations identified at least once include: (a) schizophrenia and the use of sharp weapons, (b) mood disorders and strangulation/asphyxiation/suffocation/drowning, (c) personality disorder or alcohol dependence and kicking and hitting, (d) organic disorders and blunt instruments and finally (e) depressive disorders and asphyxia. The associations most consistently found across the nine studies were: (a) schizophrenia/delusional disorder and the use of sharp weapons and (b) mood disorders and strangulation/asphyxiation/suffocation/drowning (Hughes et al., 2012; Häkkänen & Laajasalo, 2006; Häkkänen-Nyholm et al., 2009; Matejkowski et al., 2008; Putkonen et al., 2001; Rodway et al., 2009; Shaw et al., 2004; Yoon et al., 2011; Catanesi et al., 2011). The hypothesis that a severe mental disorder will have an influence on the method of homicide used seems to have found confirmation across different studies only when schizophrenia/delusional disorder and mood disorders were concerned. Consequently, this systematic review focuses on associations (a) schizophrenia/delusional disorder and sharp instruments and (b) mood disorders and strangulation/asphyxiation/suffocation/drowning.
3.2.1. Schizophrenia/delusional disorder and sharp instruments
The first five studies present associations between schizophrenia and the use of sharp instruments as a method of homicide (see table 2). In study one by Hughes et al. (2012) 46% of offenders that stabbed their victim had a diagnosis of schizophrenia. In study two (Rodway et al., 2009) 55% of schizophrenic offenders used a sharp instrument. Study three (Catanesi et al., 2011) reported a strong correlation between delusional disorder and the use of sharp instruments (O.R. = 4.7 X2 = 7.23; p ≤ 0.05). In study four (Häkkänen & Laajasalo, 2006) 58% of the schizophrenic offenders used a sharp instrument. Finally, for study five (Matejkowski et al., 2008) 30% of the offenders with schizophrenia used a sharp instrument. The remaining four studies did not present data on this association. Although studies six and seven included offenders with schizophrenia in their sample, they do not specify the homicide method used according to each diagnostic group. Study eight reported 47% of psychotic offenders in their sample to have used a sharp instrument. However, it does not specify the percentage concerning schizophrenia only. Finally, study nine included bipolar disordered offenders only.
Table 2. Main limitations of studies and their associations between method of homicide and type of diagnosis.
| Study | Key findings relevant to hypothesis | Main limitations of study |
|---|---|---|
| Hughes, Macaulay and Crichton (2012) | Evidence of association between unplanned homicide and perpetrators who have had contact with mental health services in England. Schizophrenia: Evidence of association between unplanned homicide and kitchen knife use in offenders with schizophrenic illness |
Psychiatric reports available only in 96% of cases. Sharp weapons are will also be more used because of their immediate availability. Small sample and selection of cases may have focused on domestic unplanned homicide only. Kitchen knife use may be a broader problem within English society (not relating to a specific type of homicide) – as gun control is in America. Study focused on sharp instrument method only. |
| Rodway, Flynn, Swinson, Roscoe, Hunt, Windfuhr, Kapur, Appleby and Shaw (2009) | Perpetrators with a lifetime history of mental illness were more likely to use a sharp instrument. Schizophrenia: 96% used a violent method 55% used sharp instruments as a method of homicide as opposed to 40% when compared to other mental illnesses Mood disorders: 88% used a violent method 22% used strangulation/suffocation/drowning as method of homicide as opposed to 13% when compared to other mental illnesses 31% were mentally ill at the time of the offense |
Psychiatric reports available only in 57% of cases. Of the 433 perpetrators with severe mental illness (schizophrenia/other delusional disorders/mood disorders) over half had co-morbid alcohol/drug dependence/misuse. Violent methods were more likely used by dual diagnosis perpetrators than by perpetrators with a severe mental illness, and no history of alcohol/drug misuse/dependence. Bipolar disorder and depression were joined due to the small number of offenders with a diagnosis of bipolar disorder. |
| Catanesi, Carabellese, Troccoli, Candello, Grattagliano, Solarino and Fortunato (2011) | 100% of psychiatric reports obtained Schizophrenia: Results show significant correlation between delusional disorders and the use of sharp weapons (O.R. = 4.7; X2 7.23; p≤0.05) Mood disorders: Depressive disorders were found more associated with asphyxia (O.R. = 15.9; X2 = 13.19; p≤0.05) The use of sharp weapons was more frequent in cases where the homicide was the result of an impulsive reaction 36% were mentally ill at the time of the offense |
Highly occurrence of disorders like schizophrenia and other delusional disorders were highly represented. Due to Italian law, availability of firearms is very low and this may affect the results in which this method was used by the offender. |
| Häkkänen and Laajasalo (2006) | 100% of psychiatric reports obtained Use of sharp weapon was most frequent in schizophrenic group Schizophrenia: 58% used sharp instrument as opposed to 48% when compared to other mental illnesses |
Some information was absent and coded as missing. Sample size is moderate and study should be replicated with a larger sample that can lead to more significant results. Dividing offenders between mentally ill and non-mentally ill is not sufficient; different diagnoses will differ in crime scene behaviors. More than one method of homicide per offender is possible and not specified in study data. |
| Matejkowski, Solomon and Cullen (2008) | 100% of psychiatric reports obtained Schizophrenia: 30% used a sharp instrument as opposed to 27% when compared to other mental illnesses Mood disorders: 15% used strangulation/suffocation/drowning as opposed to 12% when compared to other mental illnesses |
Small sample Firearms most common homicide method reported across all diagnoses for their easy availability More than one diagnosis per offender possible. More than one method of homicide per offender is possible. |
| Shaw, Amons, Hunt, Flynn, Turnbull, Kapur and Appleby (2004) | Perpetrators were found more likely to have a history of drug misuse than a history of contact with mental health services 32% were mentally ill at the time of the offense |
Psychiatric reports available only in 73% of cases. Studies included over-represent homicide by strangers. The loss of the psychiatric reports that were not available may have inflated proportion of perpetrators with mental illness since reports with diagnosis of mental illness are more likely to be used in court. |
| Häkkänen-Nyholm, Repo-Tiihonen, Lindberg, Salenius and Weizmann-Henelius (2009) | 100% of forensic examination reports obtained |
Study mainly focused on reporting cases of sexual homicide, although full sample involves all types of homicide offenders, reported data concerns 18 cases of sexual homicide. |
| Putknonen, Collander, Marja-Liisa, Honkasalo and Lönnqvist (2001) | 100% of psychiatric reports obtained Results show that women most often kill men by stabbing in a quarrel |
The diagnostic reliability of personality disorders in general has been suggested to be somewhat poor. Figures for neuroses and alcoholism may also be underestimates. |
| Yoon, Kim, Choi, Lyu, Kwon, Jang and Park (2011) | 100% of psychiatric reports obtained Suffocation was the most common method of homicide in the depressive phase group of Bipolar I disorder Stabbing was most common method of homicide in the mania group Mood disorders: 35% used strangulation/suffocation/drowning |
Study only looks at offenders with bipolar I disorder. Only offenders with serious psychopathology were enrolled, hence it presents limitations when generalizing findings to all offenders with bipolar I disorder. Mental status examination in Korea is not a routine and is therefore requested only when previous psychiatric history was found; because of this, patients in manic phase can be over-represented since patients in depressive phase may be considered as normal at that moment. Data was collected though a retrospective chart review, instead of prospective which would result in more precise data. |
3.2.2. Mood disorders (bipolar disorder and major depression) and strangulation/asphyxiation/suffocation/drowning
An association between mood disorders and strangulation/asphyxiation/suffocation/drowning was revealed in studies two, three, five and nine. According to study two (Rodway et al., 2009), offenders with mood disorders were significantly more likely to use strangulation than any other homicide method. In study three (Catanesi et al., 2011), depressive disorders were strongly correlated with asphyxia (O.R. = 15.9; X2 = 13.19; p ≤0.05). In study five by Matejkowski et al. (2008) 33% of offenders with bipolar disorder used strangulation/asphyxiation/suffocation/drowning methods. However, most offenders with major depression used a firearm or sharp instrument and only 17% used strangulation/asphyxiation/suffocation/drowning. Study nine (Yoon et al., 2011) on offenders with bipolar disorder reported suffocation as the most used method of homicide in the depression group. However, stabbing was the most common method in the mania group. The remaining five studies did not present data on this association. The sample of only eight offenders with mood disorders in study one was too small to establish any associations. Study four only included SMIs of schizophrenia and personality disorders. Although study six reported affective disorders to be the most common diagnosis in their sample, they failed to identify any associations between diagnosis and homicide method. Finally, studies seven and eight did not include any offenders diagnosed with mood disorders in their sample.
4. Discussion
This systematic review is the first to our knowledge to identify associations between mental illness and method of homicide reported in previous research. We examined the homicide studies published in recent years (2000-2015), particularly those involving samples of perpetrators with different psychiatric diagnoses. Nine studies reporting on homicide method used and psychiatric diagnosis of the offender were included. Five out of nine studies directly addressed the question concerning whether or not a SMI may influence the method of homicide used (Rodway et al., 2009; Catanesi et al., 2011; Matejkowski et al., 2008; Häkkänen & Laajasalo, 2006; Yoon et al., 2011), and confirmed a link between SMI and method of homicide. Two main findings are discussed: (1) the association between schizophrenia/delusional disorder and sharp instruments reported in five out of nine studies, (2) the association between mood disorders (bipolar disorder and major depression) and strangulation/asphyxiation/suffocation/drowning reported in four out of nine studies. Our review confirms consistent findings across studies indicating the methods of homicide vary between perpetrators with different mental illnesses. In addition, our review identified factors such as the duration of the illness, victim characteristics and planning of the homicide may also to be influential in the use of a specific method of homicide by an offender with mental illness. Future research may focus on the presence of specific psychotic symptoms at the time of the homicide and across different mental disorders.
4.1. Schizophrenia/delusional disorder and sharp instruments
A significant association between schizophrenia/delusional disorder and the use of sharp instruments was identified in the first five of nine studies in our review. This finding across studies is consistent with previous literature on weapon choice by individuals with schizophrenia, indicating psychotic offenders use knives more frequently than other homicide methods (Steury & Choinski, 1995). Use of knives is thought due to their immediate and easy availability (Joyal et al, 2004; Häkkänen & Laajasalo, 2006). In addition, previous studies suggest that individuals with schizophrenia are likely to carry easily available weapons (e.g., knives) with them, mainly in response to paranoid thinking (Joyal et al., 2004; De Zulueta, 2006). Indeed, studies in our review reported a high proportion of offenders with schizophrenia were found to have carried the sharp instrument on their person before committing the homicide, rather than finding it at the crime scene (Rodway et al., 2009; Häkkänen & Laajasalo, 2006).
Another possible factor underlining the association between schizophrenia and sharp instruments is the impulsivity that is associated with schizophrenia (Häkkänen & Laajasalo, 2006). Indeed, impulsivity experienced by schizophrenic offenders at the time of the crime was reported in three studies included in our review (Hughes et al., 2012; Putkonen et al., 2010; Catanesi et al., 2011). Furthermore, the use of sharp weapons has been linked to unplanned homicide and homicides resulting from an impulsive reaction (Hughes et al., 2012).
With regard to victim characteristics, the literature suggests homicide offenders with schizophrenia are more likely to kill a relative (Daly & Wilson, 1988; Steury & Choinski, 1995). This was consistent with six out of nine studies in the present review: offenders with schizophrenia/delusional disorder were significantly more likely to kill a parent/son/partner or other family relative (Hughes et al., 2012; Rodway et al., 2009; Catanesi et al., 2011; Matejkowski et al., 2008; Putkonen et al., 2010; Häkkänen & Laajasalo, 2006). Use of knives may make sense in this context as research suggests homicide methods of close contact, such as stabbing, are frequently used to kill family members (Appleby et al., 2006). Indeed, four studies in our review reported sharp instruments to be significantly more used in homicides involving g family members as victims, rather than strangers (Shaw et al., 2004; Häkkänen & Laajasalo, 2006; Rodway et al., 2009; Häkkänen-Nyholm et al., 2009).
4.2. Mood disorders and strangulation/asphyxiation/suffocation/drowning
The association between mood disorders and the use of strangulation/asphyxiation/suffocation/drowning was found to be significant in four out of nine studies in our review. However, only studies two and six specifically used mood disorders to collapse across both bipolar disorder and depressive illness (Rodway et al., 2009; Shaw et al., 2004). Study two indicated offenders with mood disorders used violent methods significantly less than offenders with other diagnoses (Rodway et al., 2009). This finding is consistent with recent research suggesting homicide offenders diagnosed with mood disorders are more likely to use less violent homicide methods, such as drowning/suffocation/asphyxiation (Flynn et al., 2013). Three studies reported an association between strangulation/asphyxiation/suffocation/drowning and bipolar disorder and major depression separately (Catanesi et al., 2011; Yoon et al., 2011; Matejkowski et al., 2008). Study three reported a significant association between depressive illness and asphyxia; the number of offenders with only bipolar disorder was too small (n=2) to identify any significant association with a homicide method (Catanesi et al., 2011). The entire sample of study nine consisted of offenders with only bipolar I disorder; an association between asphyxiation/suffocation and offenders in the depressive phase of bipolar disorder was reported. Conversely, this study also reported that offenders experiencing the manic phase of bipolar were found more likely to use sharp instruments as a method of homicide (Yoon et al., 2011). Study five (Matejkowski et al., 2008) also suggests an association between bipolar disorder and strangulation/asphyxiation/suffocation/drowning. However, major depression was linked to the use of sharp instruments/shooting, rather than strangulation/asphyxiation/suffocation/drowning. This was the only study that reported the use of sharp instruments among depressed offenders. An association concerning depression and a homicide method was not reported in the remaining four studies due to the sample not including offenders diagnosed with depressive illness – not necessarily because of a lack of relationship between the two.
With regard to victim and offense characteristics, previous literature on homicide by individuals with mood disorders, states both high rates of altruistic motivation and the perpetrators frequently being young mothers killing their own children as possible reasons for the choice of a less violent method that does not spill blood, such as suffocation/asphyxiation/drowning (Flynn et al., 2013). This is consistent with two studies included in our review reporting children were at high risk of being victims of homicide by offenders with depressive illness (Rodway et al., 2009; Catanesi et al., 2011).
4.3. Duration of the illness, type of victim and planning of the homicide may be influential in the homicide method used
Previous research on SMI has established that an individual’s propensity for violence varies depending on the stage of the illness (Modestin & Ammann, 1996; Walsh & Buchanan, 2003). For example, research suggests the rate of homicide in the first episode of psychosis is much higher than after initial treatment (Nielssen & Large, 2010). Conversely, another study reported that as schizophrenic illness progresses delusions may become more complex and risk of life-threatening behavior towards others may increase (Humphreys, Johnstone, MacMillan & Taylor, 1992). According to a study from our review, over 60% of offenders with schizophrenia had been diagnosed before the homicide (Catanesi et al., 2011). Concerning mood disorders, previous literature suggests homicide risk assessment in depressive patients is commonly overlooked (Oakley, 2009). Indeed, studies in our review revealed that over 50% of homicide offenders with major depression were in contact with Mental Health Services in the three months preceding the homicide (Yoon et al., 2011). Overall, findings from our review indicate that perpetrators with a lifetime history of mental illness are more likely than perpetrators without history of mental illness to use sharp instruments and strangulation than any other homicide methods (Hughes et al, 2012; Rodway et al., 2009). However, there is a lack of research investigating links between illness duration of schizophrenia and mood disorders and the homicide method used. Further research needs to examine whether specific stages of different SMIs will relate to the use of distinct homicide methods, as well as variations in homicide risk depending on the stage of each mental illness.
Previous research also indicates that differences in methods of homicide are related to the type of victim. For example, family members are usually killed by methods of close contact, while strangers and acquaintances are more frequently killed by shooting (Appleby et al., 2006). However, only a handful of studies have reported whether associations between method of homicide and type of victim differ by types of mental illness. Study one from our review, reported that 45% of victims by stabbing to be family member/partner or ex-partner (Hughes et al., 2012). Study two, three and nine (Rodway et al., 2009; Catanesi et al., 2011; Yoon et al., 2011) reported the methods of suffocation/asphyxiation are more likely to be used to kill young children by female offenders with affective disorder. Furthermore, in four of nine studies, over half of schizophrenic offenders killed a family member using a sharp instrument (Hughes et al., 2012; Rodway et al., 2009; Catanesi et al., 2011; Häkkänen & Laajasalo, 2006). Studies two and six also reported offenders with alcohol misuse or personality disorder were more likely to use kicking/hitting to kill acquaintances (Rodway et al., 2009; Shaw et al., 2004). Study seven indicates strangulation is more frequently used to kill females in sexual homicides (Häkkänen-Nyholm et al., 2009). Study eight only reported differences in homicide methods according to victim age, but unfortunately does not specify any further (Putkonen et al., 2010). Overall, six studies from our review reported significant differences in the homicide method used according to victim-perpetrator relationship, victim gender and victim age in homicides by mentally ill offenders with different psychiatric diagnoses.
Previous research reported an association between the degree of planning and the method of homicide used in samples of offenders with mental illness, such as the use of knives by psychotic offenders in impulsive homicides. This is consistent with four studies in our review reporting a link between sharp instruments and, impulsive unplanned homicide by schizophrenics (Hughes et al., 2012; Rodway et al., 2009; Häkkänen & Laajasalo, 2006; Catanesi et al., 2011). Additionally, study nine suggests a link between planned homicide by depressed patients and the use of suffocation (Yoon et al., 2011; Yoon et al., 2011). Findings from our review suggest differences in methods of homicide will be evident depending on the premeditation of the homicide (Häkkänen & Laajasalo, 2006).
4.4. Future research
4.4.1. The presence of active symptoms across disorders and their influence in the method of homicide used
Studies in our review consistently reported a high proportion of offenders experienced symptoms of mental illness at the time of the homicide. For example, study two revealed 96% of schizophrenic offenders in their sample reported delusions/hallucinations at the time of the crime (Rodway et al., 2009). Similarly, study three and four reported nearly all schizophrenic offenders experienced delusions/hallucinations when committing the homicide (Catanesi et al., 2011; Häkkänen & Laajasalo, 2006). Study nine on bipolar disordered offenders revealed 41% of manic offenders and 42% depressed offenders were experiencing psychotic symptoms at the time of the homicide (Yoon et al., 2011). Study two reported 75% of offenders with mood disorders experienced symptoms of the illness at the time of the homicide, unfortunately symptoms are not specified (Rodway et al., 2009). Appelbaum et al. (2000) suggests that active symptoms are probably more significant as a risk factor than the presence of an identifiable disorder. Two studies in our review suggest that offenders experiencing different symptoms at the time of the crime were likely to use different homicide methods, even when diagnosed with the same mental illness. Study two reported perpetrators diagnosed with mood disorders were more likely to use suffocation/asphyxiation/drowning if experiencing mental illness symptoms. However, mood disordered offenders without symptoms of mental illness at the time of the homicide were more likely to use kicking/hitting. Study nine revealed that offenders with bipolar disorder were likely to use different homicide methods at different phases of the disorder. Perpetrators experiencing manic symptoms were significantly more likely to use sharp instruments, whereas perpetrators experiencing depressive symptoms were found more likely to use suffocation. Future research may examine whether differences in psychiatric symptoms reported at the time of the crime within a single diagnostic group, may be linked to differences in homicide methods and other offense characteristics.
4.5. Limitations
There are several limitations to our review. Firstly, the lack of homogeneity among studies concerning the definition of mental illness and the differences in categories included. This heterogeneity is also present in the legal definition of homicide in different countries. For example, the terminology relating to homicide in England (murder, manslaughter, involuntary manslaughter) differs from definitions in Finland (murder, manslaughter, second-degree manslaughter, infanticide, involuntary manslaughter) and the United States (felony murder, murder, manslaughter, justifiable homicide) (Liem & Pridemore, 2011; Häkkänen & Laajasalo, 2006).
In addition, differences in availability of weapons among countries will also influence weapon choice. The US has the highest rates of firearm deaths due to less restrictive laws regarding gun acquisition (Catanesi et al., 2011), and frequently report firearms as the most common method of homicide used by mentally and non-mentally ill offenders, followed by sharp instruments (Smith & Cooper, 2013). This is consistent with our review, only in study five from the US was the use of a firearm revealed to be the most common homicide method across all diagnoses (Matejkowski et al., 2008). However, this is the exception rather than the norm, since research indicates sharp instruments to be the most frequently used weapon in homicides across western European countries –excluding homicides by organized crime-(Catanesi et al., 2011). Future research needs to investigate the US as a special case and consider the effect of gun availability among different countries, as well as the influence this may have on weapon choice. Furthermore, research suggests control of gun ownership and interventions to reduce availability of knives may decrease the number of homicides (Hughes et al., 2012). However, findings indicate that although restricting gun and knife availability may decrease homicides involving these methods, rates of homicides by other methods tend to increase (Bridges, 2004).
Another limitation concerns homicide-suicide cases, only one study included in our review reported data on previous homicide attempts among offenders with mood disorders (Matejkowski et al., 2008). Furthermore, no studies specified on the method of suicide used by homicide offenders. Previous research indicates the incidence of homicide-suicide cases to be considerably lower than homicide cases, and suggests the higher the homicide rate in a country, the lower the rate of homicide-suicide (Saleva et al., 2007). Moreover, studies suggest homicide-suicide to be a distinct phenomenon from homicide, and recommend homicide-suicide cases to be examined separately (Saleva et al, 2007). For this reason, information on accompanying suicide, as well as the methods used in suicide were not reported in our review since the focus was directed at methods of homicide used in homicide cases only. Further research may focus on homicide-suicide cases and the differences in methods, as well as any links with SMIs, such as mood disorders.
The availability of psychiatric reports was not complete in three out of nine studies (Hughes et al., 2012; Rodway et al., 2009; Shaw et al., 2004). Furthermore, courts are more likely to request psychiatric reports on perpetrators with severe mental health problems. Consequently, more reports are available on mentally ill offenders, leading to potential bias in case selection since this may translate into an inflation of the proportion of mentally ill offenders reported. Samples of the study were generally small or moderate; other associations might have been statistically significant in a larger sample size (Hughes et al., 2012; Catanesi et al., 2011; Matejkowski et al., 2008; Putkonen et al., 2010). Additionally, information was based both on self-reports of symptoms and clinical judgements resulting in diagnoses by psychiatrists or psychologists with different training, and over periods of several years (Häkkänen & Laajasalo, 2006).
Regarding method of homicide, our review came across two main limitations. Firstly, that in three out of nine studies, a small proportion of the offenders used more than one method of homicide and were therefore counted twice when obtaining percentages of methods of homicide used per diagnostic group; this is problematic in analysis since it leads to percentages in method of homicide used exceed 100% (Matejkowski et al., 2008; Häkkänen & Laajasalo, 2006; Putkonen et al., 2001). Secondly, only a small number of offenders used the methods of (1) strangulation, (2) asphyxiation/suffocation and (3) drowning (Matejkowski et al., 2008; Shaw et al., 2004; Putkonen et al., 2010). The latter two of these three methods are normally grouped together across studies. However, our review also added the strangulation method in this grouping, since offenders with mood disorders typically used one of these three. This is similarly the case in the mood disorders group presented in our review, consisting of aggregating offenders with bipolar disorder and major depression due to the small number of perpetrators with these diagnoses (Rodway et al., 2009).
Additional problems were incurred by limiting the scope of our systematic review to methods of homicide used by severely mentally ill perpetrators. Not included in our research were factors such as co-morbidity with alcohol and/or substance abuse, criminal history and the impact these have on weapon choice. It is important to note that previous studies have revealed severely mentally ill offenders with comorbid alcoholism and/or drug abuse/dependence are more likely to use violent homicide methods than mentally ill patients with no history of substance abuse/dependence (Rodway et al., 2009). This is consistent with previous research; revealing comorbid substance abuse/dependence increases likelihood of homicide in schizophrenia, bipolar disorder and major depression (Côté & Hodgins, 1992; Schanda et al., 2004). Finally, the association of personality disorder and the method ‘kicking/hitting’ was not included in the main findings due to the lack of consistency across the nine studies included and the low diagnostic validity of personality disorder diagnosis across countries (Putkonen et al., 2001; Häkkänen & Laajasalo, 2006).
5. Conclusions
Findings from studies in our review confirmed different mental illnesses are linked to different methods of homicide. This systematic review identified the two most consistent associations reported across recent studies between method of homicide and psychiatric diagnosis, specifically concerning SMIs: the first between (1) schizophrenia/delusional disorder and sharp instruments and the second between (2) mood disorders and strangulation/asphyxiation/suffocation/drowning. This might mean homicides by individuals with schizophrenia tend to be impulsive and therefore linked to sharp instruments due to their immediate availability. Furthermore, homicides by individuals with mood disorders frequently involve mothers killing their own children by less violent methods, such as strangulation/asphyxiation/suffocation/drowning. Data also suggests the duration of the illness, type of victim and planning of the homicide may also influence the choice of homicide method by mentally ill perpetrators. Finally, our review revealed most studies reported a high proportion of offenders experienced symptoms of mental illness when committing the homicide. Future research might examine the associations between active symptoms and homicide methods among offenders in a single diagnostic group and across mental illnesses, as well as whether these differ from associations between mental illness and homicide method. Consistency across studies concerning the two main associations identified between homicide method and mental illness might indicate that specific close contact homicide methods are prone to offenders with schizophrenia and mood disorders. Differences in homicide methods across diagnoses indicate the need for prevention strategies targeted to each diagnosis, such as weapon carrying among individuals with schizophrenia, with the hope of reducing adverse outcomes, such as lethal violent crime.
Acknowledgements
This research is supported by the funding source Consejo Nacional de Ciencia y Tecnología to Valeria Abreu Minero (CONACyT).
References
- 1.Aaron Prosser B, Penney MSR, Psych PC. Review protocol. 2015 [Google Scholar]
- 2.American Psychiatric Association. DSM-III-R: Diagnostic and statistical manual of mental disorders. American Psychiatric Association; 1980. [Google Scholar]
- 3.American Psychiatric Association. Task Force on DSM-IV. DSM-IV options book: Work in progress (7/1/91) American Psychiatric Press; 1991. [Google Scholar]
- 4.American Psychiatric Association, & American Psychiatric Association. Diagnostic and statistical manual-text revision (DSM-IV-TRim, 2000) American Psychiatric Association; 2000. [Google Scholar]
- 5.Appelbaum PS, Robbins PC, Monahan J. Violence and delusions: Data from the MacArthur violence risk assessment study. American Journal of Psychiatry. 2000;157(4):566–572. doi: 10.1176/appi.ajp.157.4.566. [DOI] [PubMed] [Google Scholar]
- 6.Appleby L, Shaw J, Amos T, McDonnell R. Safer services: National confidential inquiry into suicide and homicide by people with mental illness. Department of Health; London: 1999. [Google Scholar]
- 7.Benezech M, Bourgeois M. Homicide is strongly correlated to depression and not to mania. [L'homicide est fortement correle a la depression et pas a la manie] L'Encephale. 1992;18(Spec 1):89–90. [PubMed] [Google Scholar]
- 8.Binder RL, McNiel DE. Effects of diagnosis and context on dangerousness. The American Journal of Psychiatry. 1998;145(6):728–732. doi: 10.1176/ajp.145.6.728. [DOI] [PubMed] [Google Scholar]
- 9.Blumenthal S, Lavender A. Violence and mental disorder: A critical aid to the assessment and management of risk. Zito Trust; 2000. [Google Scholar]
- 10.Bowen R, Wang Y, Balbuena L, Houmphan A, Baetz M. The relationship between mood instability and depression: Implications for studying and treating depression. Medical Hypotheses. 2013;81(3):459–462. doi: 10.1016/j.mehy.2013.06.010. [DOI] [PubMed] [Google Scholar]
- 11.Bridges FS. Gun control law (Bill C-17), suicide, and homicide in Canada. Psychological reports. 2004;94(3):819–826. doi: 10.2466/pr0.94.3.819-826. [DOI] [PubMed] [Google Scholar]
- 12.Broome MR, Saunders KE, Harrison PJ, Marwaha S. Mood instability: Significance, definition and measurement. The British Journal of Psychiatry: The Journal of Mental Science. 2015;207(4):283–285. doi: 10.1192/bjp.bp.114.158543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Catanesi R, Carabellese F, Troccoli G, Candelli C, Grattagliano I, Solarino B, Fortunato F. Psychopathology and weapon choice: A study of 103 perpetrators of homicide or attempted homicide. Forensic Science International. 2011;209(1):149–153. doi: 10.1016/j.forsciint.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 14.Corruble E, Ginestet D, Guelfi J. Comorbidity of personality disorders and unipolar major depression: A review. Journal of Affective Disorders. 1996;37(2):157–170. doi: 10.1016/0165-0327(95)00091-7. [DOI] [PubMed] [Google Scholar]
- 15.Côté G, Hodgins S. The prevalence of major mental disorders among homicide offenders. International Journal of Law and Psychiatry. 1992;15(1):89–99. doi: 10.1016/0160-2527(92)90029-z. [DOI] [PubMed] [Google Scholar]
- 16.Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Medicine. 2013;11:126. doi: 10.1186/1741-7015-11-126. 7015-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Zulueta F. From pain to violence: The traumatic roots of destructiveness. John Wiley & Sons; 2006. [Google Scholar]
- 18.Decker SH. Exploring victim-offender relationships in homicide: The role of individual and event characteristics. Justice Quarterly. 1993;10(4):585–612. [Google Scholar]
- 19.Dobson R. Method of homicide is associated with psychiatric diagnosis. 2019 [Google Scholar]
- 20.Fazel S, Danesh J. Serious mental disorder in 23 000 prisoners: A systematic review of 62 surveys. The Lancet. 2002;359(9306):545–550. doi: 10.1016/S0140-6736(02)07740-1. [DOI] [PubMed] [Google Scholar]
- 21.Fazel S, Grann M. Psychiatric morbidity among homicide offenders: A Swedish population study. American Journal of Psychiatry. 2004;161(11):2129–2131. doi: 10.1176/appi.ajp.161.11.2129. [DOI] [PubMed] [Google Scholar]
- 22.Fazel S, Wolf A, Chang Z, Larsson H, Goodwin GM, Lichtenstein P. Depression and violence: A Swedish population study. The Lancet Psychiatry. 2015;2(3):224–232. doi: 10.1016/S2215-0366(14)00128-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Flynn SM, Shaw JJ, Abel KM. Filicide: Mental illness in those who kill their children. PloS One. 2013;8(4):e58981. doi: 10.1371/journal.pone.0058981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Golenkov A, Large M, Nielssen O, Tsymbalova A. Characteristics of homicide offenders with schizophrenia from the russian federation. Schizophrenia Research. 2011;133(1):232–237. doi: 10.1016/j.schres.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 25.Gonzalez-Pinto A, Gutierrez M, Mosquera F, Ballesteros J, Lopez P, Ezcurra J, et al. de Leon J. First episode in bipolar disorder: Misdiagnosis and psychotic symptoms. Journal of Affective Disorders. 1998;50(1):41–44. doi: 10.1016/s0165-0327(98)00032-9. [DOI] [PubMed] [Google Scholar]
- 26.Goodwin FK, Jamison KR. Manic-depressive illness: Bipolar disorders and recurrent depression. Oxford University Press; 2007. [Google Scholar]
- 27.Gottlieb P, Gabrielsen G, Kramp P. Psychotic homicides in Copenhagen from 1959 to 1983. Acta Psychiatrica Scandinavica. 1987;76(3):285–292. doi: 10.1111/j.1600-0447.1987.tb02897.x. [DOI] [PubMed] [Google Scholar]
- 28.Green CM. Matricide by sons. Medicine, Science and the Law. 1981;21(3):207–214. doi: 10.1177/002580248102100309. [DOI] [PubMed] [Google Scholar]
- 29.Häkkänen H, Laajasalo T. Homicide crime scene behaviors in a Finnish sample of mentally ill offenders. Homicide Studies. 2006;10(1):33–54. [Google Scholar]
- 30.Häkkänen-Nyholm H, Repo-Tiihonen E, Lindberg N, Salenius S, Weizmann-Henelius G. Finnish sexual homicides: Offence and offender characteristics. Forensic Science International. 2009;188(1):125–130. doi: 10.1016/j.forsciint.2009.03.030. [DOI] [PubMed] [Google Scholar]
- 31.Harvey A, Watkins E, Mansell W, Shafran R. Cognitive behavioural processes across disorders. 2004. [Google Scholar]
- 32.Hatters Friedman S, Resnick PJ. Child murder by mothers: Patterns and prevention. World Psychiatry: Official Journal of the World Psychiatric Association (WPA) 2007;6(3):137–141. [PMC free article] [PubMed] [Google Scholar]
- 33.Hiroeh U, Appleby L, Mortensen PB, Dunn G. Death by homicide, suicide, and other unnatural causes in people with mental illness: A population-based study. The Lancet. 2001;358(9299):2110–2112. doi: 10.1016/S0140-6736(01)07216-6. [DOI] [PubMed] [Google Scholar]
- 34.Hodgins S. The major mental disorders and crime: Stop debating and start treating and preventing. International Journal of Law and Psychiatry. 2001;24(4):427–446. doi: 10.1016/s0160-2527(01)00077-2. [DOI] [PubMed] [Google Scholar]
- 35.Hodgins SE. This Book Emerged from a Meeting of the Advanced Study Institute on Crime and Mental Disorder. 1993. Mental disorder and crime. [Google Scholar]
- 36.Hodgins S, Mednick SA, Brennan PA, Schulsinger F, Engberg M. Mental disorder and crime: Evidence from a Danish birth cohort. Archives of General Psychiatry. 1996;53(6):489–496. doi: 10.1001/archpsyc.1996.01830060031004. [DOI] [PubMed] [Google Scholar]
- 37.Hodgins S. Violent behaviour among people with schizophrenia: A framework for investigations of causes, and effective treatment, and prevention. Philosophical Transactions of the Royal Society of London.Series B, Biological Sciences. 2008;363(1503):2505–2518. doi: 10.1098/rstb.2008.0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hughes NS, Macaulay AM, Crichton JH. Kitchen knives and homicide by mentally disordered offenders: A systematic analysis of homicide inquiries in England 1994–2010. Journal of Forensic Psychiatry & Psychology. 2012;23(5-6):559–570. [Google Scholar]
- 39.Humphreys MS, Johnstone EC, MacMillan JF, Taylor PJ. Dangerous behaviour preceding first admissions for schizophrenia. The British Journal of Psychiatry. 1992;161(4):501–505. doi: 10.1192/bjp.161.4.501. [DOI] [PubMed] [Google Scholar]
- 40.Joyal CC, Côté G, Meloche J, Hodgins S. Severe mental illness and aggressive behavior: On the importance of considering subgroups. International Journal of Forensic Mental Health. 2011;10(2):107–117. [Google Scholar]
- 41.Krueger RF, Markon KE, Patrick CJ, Benning SD, Kramer MD. Linking antisocial behavior, substance use, and personality: An integrative quantitative model of the adult externalizing spectrum. Journal of Abnormal Psychology. 2007;116(4):645. doi: 10.1037/0021-843X.116.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lanzkron J. Murder and insanity: A survey. American Journal of Psychiatry. 1963;119(8):754–758. [Google Scholar]
- 43.Liem MC, Pridemore WA. Handbook of European homicide research: Patterns, explanations, and country studies. Springer Science & Business Media; 2011. [Google Scholar]
- 44.Link BG, Stueve A, Phelan J. Psychotic symptoms and violent behaviors: Probing the components of “threat/control-override” symptoms. Social Psychiatry and Psychiatric Epidemiology. 1998;33(1):S55–S60. doi: 10.1007/s001270050210. [DOI] [PubMed] [Google Scholar]
- 45.Malmquist CP. Depression and homicidal violence. International Journal of Law and Psychiatry. 1995;18(2):145–162. doi: 10.1016/0160-2527(95)00003-z. [DOI] [PubMed] [Google Scholar]
- 46.Marneros A. The Overlap of Affective and Schizophrenic Spectra. Cambridge University Press; Cambridge: 2007. The paradigma of overlapping affective and schizophrenic spectra: Schizoaffective conditions; pp. 1–24. [Google Scholar]
- 47.Marwaha S, Broome MR, Bebbington PE, Kuipers E, Freeman D. Mood instability and psychosis: Analyses of british national survey data. Schizophrenia Bulletin. 2014;40(2):269–277. doi: 10.1093/schbul/sbt149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Matejkowski JC, Cullen SW, Solomon PL. Characteristics of persons with severe mental illness who have been incarcerated for murder. The Journal of the American Academy of Psychiatry and the Law. 2008;36(1):74–86. doi:36/1/74 [pii] [PubMed] [Google Scholar]
- 49.Milton J, Amin S, Singh SP, Harrison G, Jones P, Croudace T, et al. Brewin J. Aggressive incidents in first-episode psychosis. The British Journal of Psychiatry: The Journal of Mental Science. 2001;178:433–440. doi: 10.1192/bjp.178.5.433. [DOI] [PubMed] [Google Scholar]
- 50.Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, Swann AC. Psychiatric aspects of impulsivity. American Journal of Psychiatry. 2001;158(11):1783–1793. doi: 10.1176/appi.ajp.158.11.1783. [DOI] [PubMed] [Google Scholar]
- 51.Monahan J. Mental disorder and violent behavior: Perceptions and evidence. American Psychologist. 1992;47(4):511. doi: 10.1037//0003-066x.47.4.511. [DOI] [PubMed] [Google Scholar]
- 52.Appleby L. Safer services. Department of Health; Great Britain: 1999. National Confidential Inquiry into Suicide and Homicide by People with Mental Illness. [Google Scholar]
- 53.Nielssen O, Large M. Rates of homicide during the first episode of psychosis and after treatment: A systematic review and meta-analysis. Schizophrenia Bulletin. 2010;36(4):702–712. doi: 10.1093/schbul/sbn144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nielssen OB, Malhi GS, Large MM. Mania, homicide and severe violence. Australian & New Zealand Journal of Psychiatry. 2012;46(4):357–363. doi: 10.1177/0004867411433217. [DOI] [PubMed] [Google Scholar]
- 55.Oakley C, Hynes F, Clark T. Mood disorders and violence: A new focus. Advances in Psychiatric Treatment. 2009;15(4):263–270. [Google Scholar]
- 56.Ouzir M. Impulsivity in schizophrenia: A comprehensive update. Aggression and Violent Behavior. 2013;18(2):247–254. [Google Scholar]
- 57.Perroud N, Baud P, Mouthon D, Courtet P, Malafosse A. Impulsivity, aggression and suicidal behavior in unipolar and bipolar disorders. Journal of Affective Disorders. 2011;134(1):112–118. doi: 10.1016/j.jad.2011.05.048. [DOI] [PubMed] [Google Scholar]
- 58.Peterson JK, Skeem J, Kennealy P, Bray B, Zvonkovic A. How often and how consistently do symptoms directly precede criminal behavior among offenders with mental illness? Law and Human Behavior. 2014;38(5):439. doi: 10.1037/lhb0000075. [DOI] [PubMed] [Google Scholar]
- 59.Potash JB, Willour VL, Chiu Y, Simpson SG, MacKinnon DF, Pearlson GD, et al. McInnis MG. The familial aggregation of psychotic symptoms in bipolar disorder pedigrees. American Journal of Psychiatry. 2001 doi: 10.1176/appi.ajp.158.8.1258. [DOI] [PubMed] [Google Scholar]
- 60.Putkonen H, Collander J, Honkasalo M, Lönnqvist J. Personality disorders and psychoses form two distinct subgroups of homicide among female offenders. Journal of Forensic Psychiatry. 2001;12(2):300–312. [Google Scholar]
- 61.Reagu S, Jones R, Kumari V, Taylor PJ. Angry affect and violence in the context of a psychotic illness: A systematic review and meta-analysis of the literature. Schizophrenia Research. 2013;146(1):46–52. doi: 10.1016/j.schres.2013.01.024. [DOI] [PubMed] [Google Scholar]
- 62.Reddy LF, Lee J, Davis MC, Altshuler L, Glahn DC, Miklowitz DJ, Green MF. Impulsivity and risk taking in bipolar disorder and schizophrenia. Neuropsychopharmacology. 2014;39(2):456–463. doi: 10.1038/npp.2013.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Richard-Devantoy S, Olie JP, Gourevitch R. Risk of homicide and major mental disorders: A critical review. [Risque d'homicide et troubles mentaux graves: revue critique de la litterature] L'Encephale. 2009;35(6):521–530. doi: 10.1016/j.encep.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 64.Robins LN, Regier DA. Psychiatric disorders in America: The epidemiologic catchment area study. Free Press; 1991. [Google Scholar]
- 65.Rodway C, Flynn S, Swinson N, Roscoe A, Hunt IM, Windfuhr K, Shaw J. Methods of homicide in England and Wales: A comparison by diagnostic group. The Journal of Forensic Psychiatry & Psychology. 2009;20(2):286–305. [Google Scholar]
- 66.Saleva O, Putkonen H, Kiviruusu O, Lönnqvist J. Homicide–suicide—an event hard to prevent and separate from homicide or suicide. Forensic Science International. 2007;166(2):204–208. doi: 10.1016/j.forsciint.2006.05.032. [DOI] [PubMed] [Google Scholar]
- 67.Rosenbaum M, Bennett B. Homicide and depression. American Journal of Psychiatry. 1986;143(3):367–370. doi: 10.1176/ajp.143.3.367. [DOI] [PubMed] [Google Scholar]
- 68.Schanda H, Knecht G, Schreinzer D, Stompe T, Ortwein-Swoboda G, Waldhoer T. Homicide and major mental disorders: A 25-year study. Acta Psychiatrica Scandinavica. 2004;110(2):98–107. doi: 10.1111/j.1600-0047.2004.00305.x. [DOI] [PubMed] [Google Scholar]
- 69.Schlesinger LB. Explorations in criminal psychopathology: Clinical syndromes with forensic implications. Charles C Thomas Publisher; [Google Scholar]
- 70.Shaw J, Amos T, Hunt IM, Flynn S, Turnbull P, Kapur N, Appleby L. Mental illness in people who kill strangers: Longitudinal study and national clinical survey. BMJ (Clinical Research Ed.) 2004;328(7442):734–737. doi: 10.1136/bmj.328.7442.734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shaw J, Hunt IM, Flynn S, Meehan J, Robinson J, Bickley H, et al. Appleby L. Rates of mental disorder in people convicted of homicide. national clinical survey. The British Journal of Psychiatry: The Journal of Mental Science. 2006;188:143–147. doi: 10.1192/bjp.188.2.143. doi:188/2/143 [pii] [DOI] [PubMed] [Google Scholar]
- 72.Smith EL, Cooper A. Homicide in the US known to law enforcement, 2011. Washington, DC: US Department of Justice Bureau of Justice Statistics; 2013. [Google Scholar]
- 73.Steury EH, Choinski M. “Normal” crimes and mental disorder: A two-group comparison of deadly and dangerous felonies. International Journal of Law and Psychiatry. 1995;18(2):183–207. doi: 10.1016/0160-2527(95)00005-3. [DOI] [PubMed] [Google Scholar]
- 74.Swann AC, Lijffijt M, Lane SD, Kjome KL, Steinberg JL, Moeller FG. Criminal conviction, impulsivity, and course of illness in bipolar disorder. Bipolar Disorders. 2011;13(2):173–181. doi: 10.1111/j.1399-5618.2011.00900.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Taylor PJ. When symptoms of psychosis drive serious violence. Social Psychiatry and Psychiatric Epidemiology. 1998;33(1):S47–S54. doi: 10.1007/s001270050209. [DOI] [PubMed] [Google Scholar]
- 76.Taylor PJ, Gunn J. Violence and psychosis. I. risk of violence among psychotic men. Bmj. 1984;288(6435):1945–1949. doi: 10.1136/bmj.288.6435.1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Taylor PJ, Gunn J. Homicides by people with mental illness: Myth and reality. The British Journal of Psychiatry: The Journal of Mental Science. 1999;174:9–14. doi: 10.1192/bjp.174.1.9. [DOI] [PubMed] [Google Scholar]
- 78.Thompson RJ, Berenbaum H, Bredemeier K. Cross-sectional and longitudinal relations between affective instability and depression. Journal of Affective Disorders. 2011;130(1):53–59. doi: 10.1016/j.jad.2010.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Torrey EF. Stigma and violence: Isn't it time to connect the dots? Schizophrenia Bulletin. 2011;37(5):892–896. doi: 10.1093/schbul/sbr057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Volavka J, Citrome L. Heterogeneity of violence in schizophrenia and implications for long-term treatment. International Journal of Clinical Practice. 2008;62(8):1237–1245. doi: 10.1111/j.1742-1241.2008.01797.x. [DOI] [PubMed] [Google Scholar]
- 81.Volavka J. Violence in schizophrenia and bipolar disorder. Psychiatria Danubina. 2013;25(1):24–33. [PubMed] [Google Scholar]
- 82.Walsh E, Buchanan A. Criminal and violent behaviour in schizophrenia. The Epidemiology of Schizophrenia. 2003;343 [Google Scholar]
- 83.Weinberger DR, Goldberg TE. RDoCs redux. World Psychiatry. 2014;13(1):36–38. doi: 10.1002/wps.20096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wulach JS. Mania and crime: A study of 100 manic defendants. Journal of the American Academy of Psychiatry and the Law Online. 1983;11(1):69–75. [PubMed] [Google Scholar]
- 85.Yoon J, Kim J, Choi SS, Lyu MK, Kwon J, Jang Y, Park G. Homicide and bipolar I disorder: A 22-year study. Forensic Science International. 2011;217(1):113–118. doi: 10.1016/j.forsciint.2011.10.037. [DOI] [PubMed] [Google Scholar]