Introduction
Prostate cancer is the most common solid organ cancer in men with over 180,000 cases in the U.S. annually.1 The management of prostate cancer remains challenging given that many with the disease will not die of it even without any treatment, yet it continues to be the second leading cause of cancer death in men.1,2 Ongoing controversy around which men to treat has contributed to variations in care and an undue influence of non-clinical factors, such as financial incentives for physicians.3–6 Furthermore, as treatments have become more technologically advanced and expensive, healthcare spending for prostate cancer has grown to nearly $12 billion annually.7,8 Current health care reforms focused on optimizing value, high quality care delivered at a lower cost, are therefore particularly relevant for this disease.9
How urologists organize themselves (i.e., practice structure) may importantly impact the value of care delivered for prostate cancer, as urologists often act as gatekeepers to its treatment. The movement of urologists to larger single-specialty group practices, where financial bonuses are often tied to volume-based productivity, has been shown to increase utilization in the traditional fee-for-service environment.10 Moreover, vertical integration of related diagnostic and therapeutic services lines, such as intensity modulated radiation therapy (IMRT) vaults, by some practices may afford even stronger financial incentives for utilization, which can in turn increase spending for care. At the same time, however, these large groups have several possible advantages including a higher volume of clinical care and integrated service lines that may lead to more efficient care and reduced spending. Alternatively, urologists employed by hospitals or practicing as part of multi-specialty groups (MSGs) may not have as strong financial incentives for utilization.
In this national study, we examine Medicare payments for prostate cancer care as a function of urologist practice structure. We hypothesize that three elements of urologist practice structure may influence spending for prostate cancer care, including urologist participation within a MSG, practice size among single-specialty urologist groups and IMRT ownership within a practice.
Methods
Study population and data
We identified Medicare beneficiaries with newly diagnosed prostate cancer between 2011 and 2014 with at least 12 months of follow-up. We included beneficiaries who were eligible for both Part A and Part B throughout the study interval and excluded beneficiaries in Medicare managed care plans. By using a nationwide sample, we aimed to capture data most representative of spending patterns and urology practices on a national level. Incident prostate cancer cases within the 20% Medicare sample data were determined using previously published and validated (against SEER data) methods, with a specificity of 99.8% and positive predictive value of 88.7%.11 Patients were attributed to urologists using previously established methodology.12 Further, initial treatment was determined from claims and was categorized as “Radical Prostatectomy,” “Radiation therapy,” “Brachytherapy,” or “Other.” For this study, “other” included cryotherapy, observation (active surveillance and watchful waiting), and primary hormone therapy. Medicare claims from a 20% national sample were used for analyses of Medicare payments.
Characterizing urologist practice organization
We used National Provider Identifier numbers to link urologists to the 2012 Healthcare Relational Spheres provider files (IMS Health). This dataset provides detailed information to characterize practice organization including aspects of urologist affiliation (e.g., practice name, associated National Provider Identifiers) and business details [e.g., practice type (single versus multi-specialty)] and has been used in other work to characterize physician practices.13,14 We divided practices into multi-specialty (a practice including primary care physicians) versus single-specialty groups, which were further categorized by size: 1 to 2 urologists (solo), 3 to 5 urologists (small), 6 to 9 urologists (medium) and 10 or more urologists (large). Urologist practices that were entirely employed by a hospital or an academic medical center were categorized as MSGs. In a validation cohort of 300 urologists of known practice status (from internet searches of practice websites), the IMS Health data showed excellent overall agreement for assessment of practice type (solo, single-specialty or MSG) at 92% (kappa=0.82), with sensitivities of 81.8%, 91.6% and 94.7%, and specificities of 99.7%, 96.5% and 92.0%, for MSG, single-specialty group and solo practice status, respectively. We further verified practice affiliation and determined the size of the single-specialty urology groups by performing a manual internet search. For single-specialty groups, we also characterized IMRT ownership as either providing onsite IMRT or employing at least 1 radiation oncologist. These two definitions of IMRT ownership were strongly correlated (kappa=0.72). In addition, ownership of IMRT by group size followed a plausible progression, with 0% of solo, 2% of small, 12% of medium and 64% of large practices identified as owners.
Outcomes
Our outcome of interest was Medicare payments for prostate cancer care. Medicare payments were evaluated from the initial prostate cancer diagnosis date through one year after diagnosis and included Medicare claims for any diagnosis using the national 20% Medicare sample. At the patient level, we measured payments using price-standardized amounts to remove differences related to geography and facility characteristics (e.g., indirect medical education funds, disproportionate share payments) and adjusted all payments for inflation to 2012 U.S. dollars.15
Analysis
Characteristics of prostate cancer patients were contrasted according to urologist practice type, size and ownership. Because payments can vary according to region, we included several regional characteristics at the level of the hospital referral region, including urologist and radiation oncologist density and managed care penetration using the Area Resource File. Socioeconomic status was categorized using a composite measure defined by Diez-Roux.16 Comorbidities were identified using claims from the 12-months prior to prostate cancer diagnosis.17
We assessed payments using generalized linear mixed models with a negative binomial distribution with a log link and compared payments according to practice type (MSG versus single-specialty group), single-specialty group practice size, and IMRT ownership for all patients diagnosed with prostate cancer. We also examined payments for the subgroup of patients receiving external beam radiation therapy as a primary treatment to account for variation in the proportion of patients treated with primary radiation across practice size, type and ownership. All models were adjusted for age, race, socioeconomic status, urban versus rural residence, regional market characteristics (i.e., supply of urologists and radiation oncologists, hospital beds, Medicare managed care penetration), and comorbidities. We accounted for clustering within hospital referral regions through the use of generalized models to provide robust standard errors. All analyses were performed using SAS statistical software (Cary, NC) and evaluated for significance by setting the probability of a type I error at 0.05. This study was deemed exempt by the University of Michigan Institutional Review Board.
Sensitivity Analyses
We performed several sensitivity analyses to further evaluate our findings. First, to make the payment comparisons potentially more specific to prostate cancer, we restricted claims assessed through the first year after diagnosis to those with a prostate cancer diagnosis code. Second, because care occurring outside the early diagnosis period may be unrelated directly to the initial management of prostate cancer, we compared payments for the 90-day episode of care after diagnosis, rather than a full year. Third, as the majority of IMRT ownership occurred in large single-specialty groups, we examined the isolated effect of group size by comparing payments by size among only single-specialty practices that did not own IMRT vaults. Fourth, to examine the extent of variation in average per beneficiary spending across practices for all prostate cancer patients and for patients receiving external beam radiation therapy as a primary treatment, we plotted the average risk and reliability adjusted payments for each single specialty group from lowest to highest. Risk and reliability adjustment was carried out using negative binomial mixed models adjusting for patient covariates, regional covariates, and group size. Then, we calculated the single specialty group specific payments using average empirical Bayes predictions. This method shrinks the single specialty group specific payments towards the overall mean payment based on the number of patients within each single specialty group.
Results
Patient Characteristics According to Practice Structure
We identified 35,929 men with newly diagnosed prostate cancer treated by 6,381 urologists during our study interval. Patient age, race and number of comorbidities varied minimally according to the treating urologist’s employment within a MSG, single-specialty group practice size or ownership of an IMRT vault (Table 1). Large, single-specialty practices and practices that owned an IMRT vault were more often located in urban areas with the highest concentration of urologists, radiation oncologists and hospital beds, and treated a greater proportion of patients in the highest socioeconomic tertile. MSGs were more likely to provide surgery as a primary prostate cancer treatment than large groups (27% versus 18%, p<0.001) and were less likely to treat with external beam radiation (29% versus 43%, p<0.001).
Table 1.
Medicare patient characteristics by practice size, affiliation and IMRT ownership.
| Characteristics | Group Size/Affiliation | P-value | IMRT Ownership | P-value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Solo | Small | Medium | Large | MSG | No | Yes | |||
| Patients n=35,929 | 8719 | 6196 | 3863 | 9004 | 8147 | - | 29285 | 6644 | - |
| Urologists n= 6,381 | 1785 | 1058 | 662 | 1541 | 1647 | - | 5567 | 1126 | - |
| Age, years | <0.001 | 0.33 | |||||||
| 66-69 | 2404 (28) | 1835 (30) | 1221 (32) | 2740 (30) | 2755 (34) | 8901 (30) | 2054 (31) | ||
| 70-74 | 2891 (33) | 2033 (33) | 1321 (34) | 3073 (34) | 2810 (34) | 9866 (34) | 2262 (34) | ||
| 75-79 | 1983 (23) | 1443 (23) | 795 (21) | 1992 (22) | 1636 (20) | 6391 (22) | 1458 (22) | ||
| 80-84 | 1018 (12) | 606 (10) | 373 (10) | 857 (10) | 710 (9) | 2946 (10) | 618 (9) | ||
| 85+ | 423 (5) | 279 (5) | 153 (4) | 342 (4) | 236 (3) | 1181 (4) | 252 (4) | ||
| Race/ethnicity | <0.001 | 0.002 | |||||||
| White | 7668 (88) | 5537 (89) | 3488 (90) | 7810 (87) | 7298 (90) | 25945 (89) | 5856 (88) | ||
| Black | 742 (9) | 507 (8) | 283 (7) | 958 (11) | 595 (7) | 2459 (8) | 626 (9) | ||
| Other/unknown | 309 (4) | 152 (2) | 92 (2) | 236 (3) | 254 (3) | 881 (3) | 162 (2) | ||
| Initial Management | <0.001 | <0.001 | |||||||
| Radiation Therapy | 2963 (34) | 2074 (33) | 1326 (34) | 3856 (43) | 2349 (29) | 9345 (32) | 3223 (49) | ||
| Brachytherapy | 1517 (17) | 936 (15) | 504 (13) | 903 (10) | 950 (12) | 4257 (15) | 553 (8) | ||
| Surgery | 1321 (15) | 1138 (18) | 833 (22) | 1646 (18) | 2237 (27) | 6035 (21) | 1140 (17) | ||
| Other | 2918 (33) | 2048 (33) | 1200 (31) | 2599 (29) | 2611 (32) | 9648 (33) | 1728 (26) | ||
| Comorbidity | <0.001 | 0.88 | |||||||
| 0 | 4869 (56) | 3507 (57) | 2313 (60) | 5133 (57) | 4947 (61) | 16930 (58) | 3839 (58) | ||
| 1 | 2047 (23) | 1463 (24) | 860 (22) | 2131 (24) | 1762 (22) | 6749 (23) | 1514 (23) | ||
| 2 | 968 (11) | 652 (11) | 386 (10) | 941 (10) | 767 (9) | 3027 (10) | 687 (10) | ||
| 3+ | 835 (10) | 574 (9) | 304 (8) | 799 (9) | 671 (8) | 2579 (9) | 604 (9) | ||
| Socioeconomic status | <0.001 | <0.001 | |||||||
| Low | 3497 (40) | 2025 (33) | 1191 (31) | 2402 (27) | 2355 (29) | 9730 (33) | 1740 (26) | ||
| Medium | 2861 (33) | 2359 (38) | 1325 (34) | 2914 (32) | 2934 (36) | 10217 (35) | 2176 (33) | ||
| High | 2361 (27) | 1812 (29) | 1347 (35) | 3688 (41) | 2858 (35) | 9338 (32) | 2728 (41) | ||
| Residing in urban area | <0.001 | <0.001 | |||||||
| Non-urban | 2538 (29) | 1296 (21) | 795 (21) | 757 (8) | 1992 (24) | 6798 (23) | 580 (9) | ||
| Urban | 6181 (71) | 4900 (79) | 3068 (79) | 8247 (92) | 6155 (76) | 22487 (77) | 6064 (91) | ||
| Urologists per 100,000 | <0.001 | <0.001 | |||||||
| Low (≤ 34) | 3529 (40) | 2122 (34) | 1422 (37) | 2140 (24) | 2696 (33) | 10305 (35) | 1604 (24) | ||
| Intermediate | 3022 (35) | 2305 (37) | 1258 (33) | 2843 (32) | 2683 (33) | 9987 (34) | 2124 (32) | ||
| High (≥ 71) | 2168 (25) | 1769 (29) | 1183 (31) | 4021 (45) | 2768 (34) | 8993 (31) | 2916 (44) | ||
| Radiation oncologists per 100,000 | <0.001 | <0.001 | |||||||
| Low (≤ 13) | 3443 (39) | 2250 (36) | 1206 (31) | 2250 (25) | 2759 (34) | 10406 (36) | 1502 (23) | ||
| Intermediate | 3068 (35) | 2257 (36) | 1344 (35) | 2866 (32) | 2564 (31) | 9907 (34) | 2192 (33) | ||
| High (≥ 29) | 2208 (25) | 1689 (27) | 1313 (34) | 3888 (43) | 2824 (35) | 8972 (31) | 2950 (44) | ||
| Hospital beds per 100,000 | <0.001 | <0.001 | |||||||
| Low (≤ 3338) | 3379 (39) | 2167 (35) | 1211 (31) | 2703 (30) | 2538 (31) | 10085 (34) | 1913 (29) | ||
| Intermediate | 3072 (35) | 2145 (35) | 1318 (34) | 2717 (30) | 2797 (34) | 10038 (34) | 2011 (30) | ||
| High (≥ 6342) | 2268 (26) | 1884 (30) | 1334 (35) | 3584 (40) | 2812 (35) | 9162 (31) | 2720 (41) | ||
| Medicare Managed Care penetration | <0.001 | <0.001 | |||||||
| Low (≤ 13.5%) | 3093 (35) | 2368 (38) | 1480 (38) | 2285 (25) | 2690 (33) | 10237 (35) | 1679 (25) | ||
| Intermediate | 2623 (30) | 1918 (31) | 1365 (35) | 3430 (38) | 2612 (32) | 9497 (32) | 2451 (37) | ||
| High (≥ 25.0%) | 3003 (34) | 1910 (31) | 1018 (26) | 3289 (37) | 2845 (35) | 9551 (33) | 2514 (38) | ||
Payments According to Practice Structure
Medicare payments for men with newly diagnosed prostate cancer were significantly lower in MSGs and significantly higher among practices that had IMRT ownership (Table 2). We observed excess spending of $3,185 per beneficiary for large group practices compared to MSGs, and $3,639 in excess spending per beneficiary for practices with IMRT ownership compared to non-owning practices (p-values <0.001). When we restricted our analysis to patients who received external beam radiation as their primary treatment these patterns persisted with large groups spending $2,228 more per beneficiary and owners spending $1,440 more per beneficiary (p-values <0.001).
Table 2.
Mean adjusted payments for first year after prostate cancer diagnosis by practice size and IMRT ownership.
| Practice Size | ||||||
|---|---|---|---|---|---|---|
| Solo | Small | Medium | Large | MSG | p-value | |
| All prostate cancer patients | $21,016 | $20,841 | $20,337 | $22,366 | $19,181 | p<0.001* |
| Patients receiving primary RT | $30,842 | $31,672 | $31,060 | $32,142 | $29,913 | p<0.001* |
| IMRT Ownership | ||||||
| Non-owners | Owners | p-value | ||||
| All prostate cancer patients | $20,162 | $23,801 | p<0.001 | |||
| Patients receiving primary RT | $30,182 | $31,622 | p<0.001 | |||
p-value for comparison of MSG payments to large group practice payments
RT: radiation therapy
Our sensitivity analysis examining mean adjusted payments for only prostate cancer related claims in the first year after prostate cancer diagnosis also demonstrated statistically significant differences in payments according to practice type (large single-specialty versus MSG) and IMRT ownership although smaller in magnitude (differences of $2,605 and $3,279 respectively, p-values <0.001). Similar patterns were noted when limiting payments to a 90-day episode window after diagnosis. When we restricted our analysis to non-owning single-specialty practices to examine the effect of single-specialty group size alone, we found no significant differences in payments across practices (p=0.48). Payments for non-owning single-specialty practices were still higher than among MSG practices at $1,233 per beneficiary (p<0.001).
Practice Variation in Spending on Prostate Cancer Care
We identified 561 single specialty groups who had any prostate cancer patients attributed to them via urologists (Figure 1). The mean spending per beneficiary among these groups was $20,675 (range $13,557-$32,526). 5% of these single specialty groups had an average per beneficiary spending significantly below the overall mean, and 10% had an average per beneficiary spending significantly higher than the overall mean. Among those single specialty groups that spent significantly lower than the mean, 7% were IMRT owners. Among those single specialty groups that spent significantly higher than the mean, 56% were IMRT owners.
Figure 1:
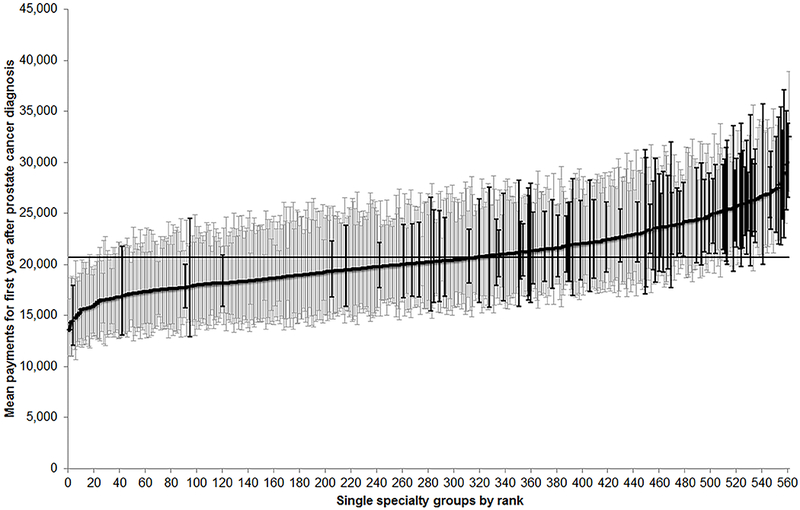
Mean risk and reliability adjusted Medicare payments for each single specialty urology practice (n=561) within a year after diagnosis for men with newly diagnosed prostate cancer from 2011-2014, ranked from lowest to highest. Vertical bars represent 95% confidence intervals around the mean estimate for each practice. Black bars represent practices with ownership of IMRT devices.
We identified 513 single specialty groups who had prostate cancer patients treated primarily with external beam radiation therapy attributed to them via urologists (Figure 2). The mean spending per beneficiary among these groups was $30,642 (range $22,313-$46,399). 5% of these single specialty groups had an average per beneficiary spending significantly below the overall mean, and 8% had an average per beneficiary spending significantly higher than the overall mean. Among those single specialty groups that spent significantly lower than the mean, 22% were IMRT owners. Among those single specialty groups that spent significantly higher than the mean, 38% were IMRT owners.
Figure 2:
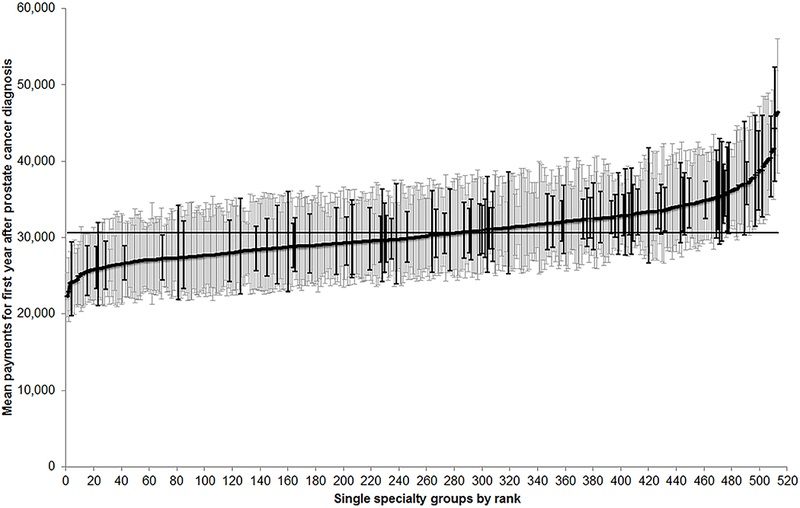
Mean risk and reliability adjusted Medicare payments for each single specialty urology practice (n=513) within a year after diagnosis for men with newly diagnosed prostate cancer managed with external beam radiation therapy from 2011-2014, ranked from lowest to highest. Vertical bars represent 95% confidence intervals around the mean estimate for each practice. Black bars represent practices with ownership of IMRT devices.
Discussion
Our findings suggest urologist practice structure is associated with payments for prostate cancer care in the year following a prostate cancer diagnosis. Despite similar patient populations across practice settings, MSGs demonstrated the lowest Medicare payments per episode of prostate cancer care whereas practices with ownership of IMRT devices had the highest.
How physicians organize themselves has evolved over the last two decades. Whereas the autonomy assured with solo or small group practice was attractive in the past, the changing dynamics of healthcare delivery have promoted the development of large group practices.18,19 Large groups are better equipped to handle the administrative complexities of health care payment and have leverage for price negotiation with health plans. Further, they allow for economies of scale that have the potential to reduce overhead and to enhance profitability. In addition, large groups have the ability to pool resources and capital, enabling them to purchase expensive service lines.20
We observed the highest spending after a prostate cancer diagnosis among single-specialty practices that owned an IMRT vault. Spending was somewhat lower, with no differences by group size, among non-owning practices. Specifically, owning practices were more likely to treat newly diagnosed prostate cancer patients with external beam radiation therapy over surgery, which was a major contributor to their higher average spending. In addition, even after restricting the analysis to men primarily managed with external beam radiation therapy, payments were still higher, suggesting that IMRT owning practices incur additional expenses related to other aspects of care, such as on imaging.21 These findings are consistent with previously published work showing an association between ownership and utilization of IMRT for prostate cancer.10,22
Our findings show that the MSG practice model is associated with lower spending for prostate cancer care, even compared to single-specialty groups without ownership of IMRT devices. Previous work examining care in MSGs has focused on primary care or the management of chronic medical conditions, demonstrating a modest positive effect to contain costs and improve quality; our study results support the potential financial benefits of this model in a specialty driven context such as prostate cancer.23,24
The study findings should be interpreted in the context of several limitations. First, our study cohorts were restricted to Medicare beneficiaries so findings may not be generalizable to patients younger than 65 years of age or with other forms of health insurance. Nevertheless, the majority of new prostate cancer patients are Medicare enrollees. Second, our examination of payments did not include adjustment for cancer characteristics so it is possible that some of the observed differences across practice structure were related to differences in tumor risk. However, in previously published work utilizing SEER-Medicare data, there no meaningful differences in D’Amico risk groups or comorbidities among patients treated in various practice types, suggesting their patient populations are relatively similar across practices.25 Third, it may be difficult to attribute all aspects of spending to care delivered by the urology practices. However, in sensitivity analyses we demonstrated that our findings are robust across a range of scenarios. Additionally, other external and policy incentives that we have not considered in this study may exist and influence the Medicare spending for men with prostate cancer. For example, Medicare Accountable Care Organizations (ACOs) aim to reduce spending for Medicare beneficiaries. While an analysis of ACOs is outside of the scope of this analysis, one reason that multispecialty groups generate lower spending for men with prostate cancer may be increased participation in ACOs or other programs that incentivize cost control. Finally, our classification of IMRT ownership status may have been imperfect. Nevertheless, any misclassification would tend to bias towards the null, suggesting that any differences we observed by ownership status are conservative estimates.
Our findings have important implications relevant to current models of health care reform, including provisions in the Affordable Care Act and the Medicare Access & CHIP Reauthorization Act (MACRA).26 A signature component of both is the accountable care organization (ACO). ACOs were initially formed under the Affordable Care Act and now form a basis for the alternative payment models of MACRA. Current iterations of ACOs have focused around primary care physicians, with limited involvement of surgical specialists.27 Only half of all Medicare Shared Savings Program ACOs have any urologist participation and within these organizations participation is highly variable.28 For diseases that are managed almost entirely by specialists, such as prostate cancer, engaging them in emerging models such as ACOs will be key to increasing value. The findings we noted in this study for MSGs represent a potential preview of the impact a value-focused, highly integrated model, such as ACOs, may have on cost savings for such care delivery. The reforms embedded in MACRA will put increasing pressure on physicians to improve value.29 As an increasing number of restrictions, reporting measures, practice requirements and other administrative burdens are placed on urologist groups, solo and small urologist practices are likely to increasingly join larger urologist groups or multispecialty groups. Our study results suggest how these smaller groups choose to align themselves will likely have a strong impact on the overall value of prostate cancer care.
Funding:
This study was supported by AHRQ R01HS025707. The views expressed in this article do not reflect the views of the federal government.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA: a cancer journal for clinicians. 2016;66(1):7–30. [DOI] [PubMed] [Google Scholar]
- 2.Welch HG, Albertsen PC, Nease RF, Bubolz TA, Wasson JH. Estimating treatment benefits for the elderly: the effect of competing risks. Ann Intern Med. 1996;124(6):577–584. [DOI] [PubMed] [Google Scholar]
- 3.Shahinian VB, Kuo YF, Gilbert SM. Reimbursement policy and androgen-deprivation therapy for prostate cancer. N Engl J Med. 2010;363(19):1822–1832. [DOI] [PubMed] [Google Scholar]
- 4.Cooperberg MR, Broering JM, Carroll PR. Time trends and local variation in primary treatment of localized prostate cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2010;28(7):1117–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krupski TL, Kwan L, Afifi AA, Litwin MS. Geographic and socioeconomic variation in the treatment of prostate cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2005;23(31):7881–7888. [DOI] [PubMed] [Google Scholar]
- 6.Thompson I, Thrasher JB, Aus G, et al. Guideline for the management of clinically localized prostate cancer: 2007 update. The Journal of urology. 2007;177(6):2106–2131. [DOI] [PubMed] [Google Scholar]
- 7.Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010–2020. Journal of the National Cancer Institute. 2011;103(2):117–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roehrig C, Miller G, Lake C, Bryant J. National health spending by medical condition, 1996–2005. Health Aff (Millwood). 2009;28(2):w358–367. [DOI] [PubMed] [Google Scholar]
- 9.Porter ME. What is value in health care? N Engl J Med. 2010;363(26):2477–2481. [DOI] [PubMed] [Google Scholar]
- 10.Mitchell JM. Urologists’ use of intensity-modulated radiation therapy for prostate cancer. N Engl J Med. 2013;369(17):1629–1637. [DOI] [PubMed] [Google Scholar]
- 11.Hollenbeck BK, Bierlein MJ, Kaufman SR, et al. Implications of evolving delivery system reforms for prostate cancer care. The American journal of managed care. 2016;22(9):569–575. [PMC free article] [PubMed] [Google Scholar]
- 12.Shahinian VB, Kuo YF, Freeman JL, Goodwin JS. Determinants of androgen deprivation therapy use for prostate cancer: role of the urologist. Journal of the National Cancer Institute. 2006;98(12):839–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nyweide DJ, Weeks WB, Gottlieb DJ, Casalino LP, Fisher ES. Relationship of primary care physicians’ patient caseload with measurement of quality and cost performance. Jama. 2009;302(22):2444–2450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rittenhouse DR, Casalino LP, Shortell SM, et al. Small and medium-size physician practices use few patient-centered medical home processes. Health Aff (Millwood). 2011;30(8):1575–1584. [DOI] [PubMed] [Google Scholar]
- 15.Gottlieb DJ, Zhou W, Song Y, Andrews KG, Skinner JS, Sutherland JM. Prices don’t drive regional Medicare spending variations. Health Aff (Millwood). 2010;29(3):537–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345(2):99–106. [DOI] [PubMed] [Google Scholar]
- 17.Klabunde C, Potosky A, Legler J, Warren J. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53:1258–1267. [DOI] [PubMed] [Google Scholar]
- 18.Casalino LP, Pham H, Bazzoli G. Growth of single-specialty medical groups. Health Aff (Millwood). 2004;23(2):82–90. [DOI] [PubMed] [Google Scholar]
- 19.Schlossberg S Supergroups and economies of scale. The Urologic clinics of North America. 2009;36(1):95–100, vii. [DOI] [PubMed] [Google Scholar]
- 20.Pham HH, Devers KJ, May JH, Berenson R. Financial pressures spur physician entrepreneurialism. Health Aff (Millwood). 2004;23(2):70–81. [DOI] [PubMed] [Google Scholar]
- 21.Hollingsworth JM, Birkmeyer JD, Zhang YS, Zhang L, Hollenbeck BK. Imaging use among employed and self-employed urologists. The Journal of urology. 2010;184(6):2480–2484. [DOI] [PubMed] [Google Scholar]
- 22.Bekelman JE, Suneja G, Guzzo T, Pollack CE, Armstrong K, Epstein AJ. Effect of practice integration between urologists and radiation oncologists on prostate cancer treatment patterns. The Journal of urology. 2013;190(1):97–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hwang W, Chang J, Laclair M, Paz H. Effects of integrated delivery system on cost and quality. The American journal of managed care. 2013;19(5):e175–184. [PubMed] [Google Scholar]
- 24.Weeks WB, Gottlieb DJ, Nyweide DE, et al. Higher health care quality and bigger savings found at large multispecialty medical groups. Health Aff (Millwood). 2010;29(5):991–997. [DOI] [PubMed] [Google Scholar]
- 25.Hollenbeck BK, Kaufman SR, Yan P, et al. Urologist Practice Affiliation and Intensity-modulated Radiation Therapy for Prostate Cancer in the Elderly. Eur Urol. 2018;73(4):491–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schwartz AL, Landon BE, McWilliams JM. Discretionary Interpretations of Accountable Care Organization Data-Reply. JAMA Intern Med. 2016;176(3):412. [DOI] [PubMed] [Google Scholar]
- 27.Dupree JM, Patel K, Singer SJ, et al. Attention to surgeons and surgical care is largely missing from early medicare accountable care organizations. Health Aff (Millwood). 2014;33(6):972–979. [DOI] [PubMed] [Google Scholar]
- 28.Hawken SR, Ryan AM, Miller DC. Surgery and Medicare Shared Savings Program Accountable Care Organizations. JAMA Surg. 2016;151(1):5–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clough JD, McClellan M. Implementing MACRA: Implications for Physicians and for Physician Leadership. Jama. 2016;315(22):2397–2398. [DOI] [PubMed] [Google Scholar]


