Abstract
Objectives:
To describe the current evidence of studies examining the use of information technology for family caregivers of persons with cancer. We highlight emerging technologies and trends and discuss ethical and practical implications.
Data Sources:
Review scientific studies and systematic reviews of technology use to support caregivers of persons with cancer.
Conclusion:
The evidence base is growing; however, more studies are needed to test the effectiveness of technology.
Implications for Nursing Practice:
Several tools have potential to provide support to family caregivers but the selection of such tools needs to address access, privacy, interoperability, and usability considerations.
Keywords: information technology, caregiving, telehealth, artificial intelligence, usability
The National Cancer Institute estimated that more than 1.7 million new cases of cancer were diagnosed in 2018, and the number of new cancer cases is expected to rise by 22 million worldwide in the next two decades.1 Despite recent advances in cancer treatment, cancer deaths have remained relatively stable, declining less than 2%. For each patient diagnosed there are often additional members of one’s network (including family and others) greatly affected by the disease. Several of the gaps and challenges identified in the evidence base and care services for the dying identified two decades ago by the Institute of Medicine landmark report “Approaching Death: Improving Care at the End of Life,”2 still persist, and interventions for caregivers of advanced cancer patients have been sparse. Research consistently shows that family caregivers of patients with advanced illness face increased mortality and health issues as a result of caring for their loved ones.3–5 Recent systematic reviews regarding caregivers for cancer patients have concluded that caregivers are in need of information and skills training, tools to improve coping with the physical and emotional burden of caregiving, effective communication between caregiver and patient, and support in addressing barriers as they navigate the health care system.6,7
Supportive services for caregivers of patients with advanced cancer are not always readily available. Information technology has the potential to provide access to information sources and improve communication. The proliferation of mobile applications, communication, and wearable devices has introduced new opportunities to provide supportive tools, especially in cases where geographic distances may be an additional access barrier. Rural caregivers often face increased systemic challenges compared with their urban counterparts (eg, distance, lack of transportation, health care workforce shortages, and lack of specialized supportive services).8 Information technology may facilitate increased access to services designed for caregivers in rural areas.
While information technology is increasingly integrated into clinical services and supportive interventions, we are lacking a comprehensive assessment of the current evidence of their effectiveness and strategies to design and implement such tools to increase utility and acceptance. This article describes the current evidence of studies examining the use of various technologies for family caregivers of persons with cancer. We also highlight potential future directions for innovative tools based on emerging technologies and trends and discuss ethical and practical implications resulting from the use of information technologies in cancer care.
A Framework for the Integration of Technology in the Caregiving Experience
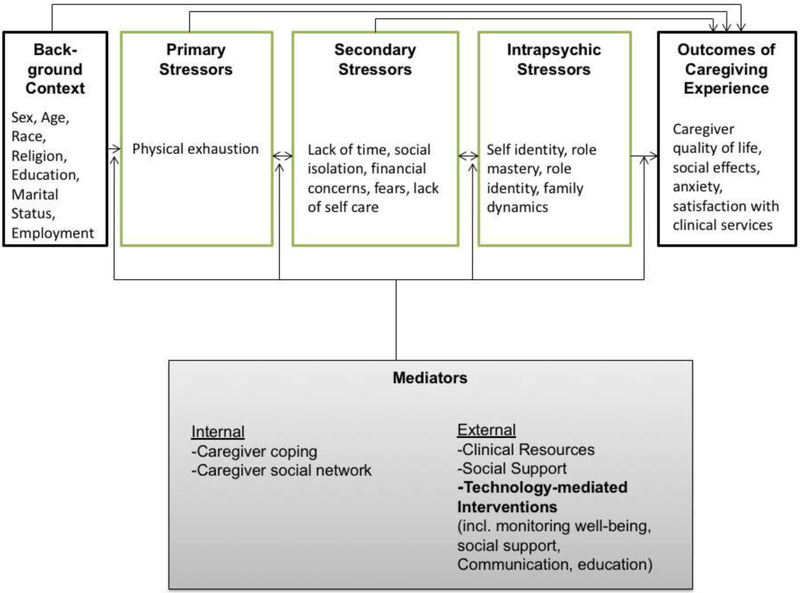
The introduction of information technology in the delivery of services to persons with cancer and their families is informed by the specific theoretical framework that dictates the specific intervention. More broadly however, the use of technology for family caregivers can be placed within the original stress and coping framework by Perlin and Schooler9 and its modified version by Meyers and Gray.10 This framework was expanded to showcase the role of technology for family caregivers in a conceptual model labeled ACT (Assessing Caregivers for Technology Interventions).11
The ACT model describes the caregiving trajectory recognizing the background context (including the environment and availability of resources), primary, secondary, and intrapsychic stressors, as well as the outcomes of the caregiving experience. In this model technology-based interventions can facilitate ongoing assessment of the background and all stressors, as well as targeted delivery of services and resources in every phase of this trajectory. The scientific premise of the model holds that assessment, prediction, and intervention by clinical and non- clinical stakeholders can serve as a mediator to the caregiving experience, resulting in improved caregiver outcomes such as reduced anxiety, quality of life, and satisfaction with provider services (see Fig. 1). Assessing the caregiver’s background, primary, secondary, and intrapsychic stressors, and tailoring a technology-based intervention enables providers to address any stressors that can mediate the response to the technology. Information technology tools are useful in the assessment, delivery, and evaluation of a broad range of interventions.
Fig. 1.
The ACT theoretical model.
Reviewing the evidence base
While technology is anticipated to assist in addressing the needs of caregivers, the documented evidence of technology-mediated interventions targeting caregivers is still in early phases and growing. In 2015 Chi and Demiris12 conducted a systematic review of telehealth tools and interventions for family caregivers and found only 65 articles that either solely targeted the caregiver or included patients and caregivers as the recipients of the intervention. This review did not focus on cancer exclusively, and indicates that there is limited evidence on such studies targeting caregivers (with half of all articles including interventions for parents of pediatric patients). When focusing on cancer specifically, published evidence of the effectiveness of technology use for family caregivers is even more limited. Heynsergh et al13 conducted a review of technology-based interventions for informal caregivers of patients with cancer. They specifically focused on studies that examined new software tools and not interventions that were using existing programs or applications, they identified only six studies. One of the most frequently studied uses of information technology to support family caregivers is informed by the CHESS (Center for Health Enhancement System Studies) framework.14 The CHESS Web-based platform supports communication among patients and their caregivers to track symptoms and access resources, which has been tested with various populations. Namkoong et al,15 for example, used the CHESS platform to support patients with advanced lung cancer and their family caregivers. The system was expanded to include a report of the patient’s symptoms for review by the treating clinician, and engaging multiple stakeholders (patients, family caregivers, clinicians) in accessing and processing the data. Moreover, the system offered different responses based on the severity of the symptoms reported.14 This platform reduced cancer caregivers’ perceived burden and improved their overall mood.14 Other efforts have facilitated couples-based interventions targeting cancer patients and their spouse or partner. Song et al16 tested a couples-based intervention designed to improve quality of life of patients and their caregivers by providing information and training for couples. Similarly, Scott and Beatty17 designed an online intervention for persons living with cancer and expanded the focus to include and test with family caregivers.
Shin et al18 reviewed scientific literature to identify health technology tools that support cancer caregivers more broadly (not only those that involved the development of new hardware or software). They identified 18 articles. Their review concluded that there are substantial gaps in knowledge regarding effectiveness of these systems and level of adaption by health systems. When examining existing studies, the use of technology in supporting family caregivers can be used to serve the functions outlined below.
Education and service coordination
One of the most frequent uses of information technology is to facilitate the delivery of educational interventions (including access to information resources). Collinge et al19 evaluated a multi-media educational program for family caregivers with the goal to provide them with tools and strategies focusing on touch-based techniques at home to provide comfort to patients with cancer. Caregivers were randomly assigned to either the intervention group or an attention control group. Findings indicated that the multimedia instruction in touch methods offered caregivers increased satisfaction with caregiving and self-efficacy as well as decreased patient pain, depression, and other symptoms.
Technological tools can also facilitate coordination of services and scheduling to support task management for caregivers. Walsh et al20 designed and implemented a Web-based intervention called “Home Medication Support” for home-based medication management. The application includes a medication schedule and calendar, tools for communication, conversion charts, and information about side effects. The system was tested for usability and feasibility; medical record reviews and surveys were conducted to assess medication error rates and perceived usefulness for family caregivers, demonstrating the potential of such a system for caregivers who have to manage complex medication management tasks for patients with cancer. Similarly, the Oncology Family App,21 a mobile app developed and tested in Australia to support families of children with cancer and assist with health care appointments, contacts, and access to blood test results, was found to be an efficient and convenient approach to support family caregivers.
Delivery of clinical care
The use of telehealth platforms has the potential to connect patients and families in their homes or community settings with clinicians and experts in clinical sites and support the delivery of actual health care services. The family caregiver can play an active role in these “virtual” sessions and in some cases even act not only as a liaison but as the proxy decision-maker. Oliver et al22 tested an intervention called ACTIVE (Assessing Caregivers for Team intervention via Video Encounters) that was designed to use Web conferencing technology to address the practical challenges of having family caregivers actively involved in the discussion of individual care plans in hospice care. Caregivers who participated in the study felt more involved in the decision-making and reported having more information readily available to them, and being able to develop positive relationships with the hospice staff. They reported challenges, such as occasional issues with technology and feeling rushed when participating virtually in team meetings. Home telehealth has also been used to conduct “virtual visits” by a clinician. For example, Stern et al23 examined the use of videophones with optional remote monitoring features for palliative cancer care patients and their families to have access to specialist nurses 24 hours per day. Pain management was the most frequent reason for the family caregiver to initiate a session with the clinician, followed by the need for emotional support. Technical problems were identified as a challenge as well as a perceived lack of integration of services into the formal system of care.
Delivery of caregiver-specific cognitive behavioral interventions
Technological platforms can facilitate the delivery of behavioral interventions designed to assist caregivers in a cost-effective manner without requiring additional travel and resources for in-person settings. This introduces opportunities to enhance services provided to families that may otherwise not have been feasible. Demiris et al24 tested a problem-solving therapy intervention called PISCES (Problem Solving Intervention to Support Caregivers in End of Life Care Settings) using a three-arm randomized clinical trial design whereby family caregivers were randomized to either an attention control group, or a group receiving PISCES via in-person sessions, or a group receiving PISCES via video conferencing. PISCES has been developed specifically for the hospice setting and includes a structured curriculum delivered in three sessions. The intervention is designed to motivate caregivers to adopt a positive attitude, describe problems by collecting facts, set goals, and explore solutions. Compared with the attention control group, caregivers in the face-to-face group experienced both a statistically and clinically significant reduction of anxiety and improvement of quality of life. However, there were no differences in outcomes for caregivers in the video conferencing group compared with the attention control group. This finding calls for further investigation as to whether the technology platform may reduce the effectiveness of an intervention that could be delivered in person and whether a relationship established between the caregiver and the therapist in person may be necessary before proceeding with video mediated sessions. Washington et al25 tested the same intervention PISCES in the outpatient palliative care setting. In this study, video conferencing was used to support the delivery of the intervention as a cost-effective approach. Caregivers who received PISCES reported statistically significantly less anxiety than those who received only usual care.
Peer support
The wide adoption of online tools and social media has enabled individuals to connect with others who may be facing similar challenges. Caregivers of persons with cancer often appreciate the opportunity to exchange information and advice or share experiences with other peers. Oliver et al26 examined the role of a secret Facebook support group of hospice caregivers. This initiative was informed by the practice standards for social workers by the National Association of Social Workers to guide technology use in social work practice. The Facebook group included caregivers of hospice patients and was monitored by a social worker who facilitated discussion. The group was found to be a feasible platform for caregivers to provide mutual support and exchange information. Wittenberg-Lyles et al27 conducted a mixed methods study to evaluate a secret Facebook group for bereaved hospice caregivers. The study followed 16 caregivers over a period of 9 months. Caregivers discussed restoration and loss, and shared loss orientation through storytelling, sharing advice, and highlighting how to best manage challenges of coping. Caregiver anxiety and depression decreased post-intervention. Online communities can provide a supportive environment. The Association of Cancer Online Resources28 includes a collection of online cancer communities for both patients and family caregivers. The sustainability of an online community requires ongoing monitoring to ensure effective and ongoing communication that promotes mutual validation and respect. There may be conflicting guidelines as to the optimal group size and structure; however, more recently researchers are using algorithms to examine the attributes of an online community that maximize the productivity and improve dynamics for the group.29 This information can inform the development of future online peer support groups for cancer caregivers. In addition to linking caregivers facing similar challenges, tools have been developed to assess a caregiver’s social connectedness so as to prevent or mitigate social isolation. Fuentes et al,30 for example, tested a mobile system called “EmotionMingle” that is based on the visualization of a tree that maps a caregiver’s social network as a strategy to reduce social isolation. The system informs caregivers as to how their emotions relate to daily communication practices.
Future Directions
Most of the published studies examining the use of information technology have focused on widely available platforms such as social media, mobile applications, Web-based video conferencing, or multimedia modules for education. Emerging technologies and methodologies are anticipated to introduce new opportunities to provide effective support to caregivers both at a population and an individual level. Powerful data-processing tools highlight the potential of data analytics when applied to large data sets in identifying or even predicting needs and trajectories of specific population groups. For example, Yoon et al31 explored how to apply data mining methods to discover new behavioral risk knowledge and predict caregiver stress using large behavioral data sets. Similar tools can be applied to large data sets to identify caregivers of patients with cancer who may be at increased risk to experience significant negative effects from the caregiving experience and deliver early on interventions tailored to facilitate effective support and mitigate the potential impact of caregiving on caregivers’ own mortality and morbidity.
Individual caregivers may benefit from emerging artificial intelligence tools that are designed to provide support and companionship, often referred to as conversational agents. Conversational technologies involve the use of intuitive, natural language, on the part of both the user and the system. Conversational technologies (including voice-based personal assistants such as the Amazon Alexa and Google Home) are envisioned to be more intuitive to use and not require extensive training to operate compared with non-conversational technologies.32 In health care, conversational agents have been used in patient education (eg, “virtual nurse agents” to explain medical documents to patients33), clinician training,34 delivery of behavioral interventions,35 and promoting physical activity.36 Utami and colleagues37 conducted an experiment to test a virtual conversational palliative care coach currently under development that works with individuals in the last year of their life and their family member to help them cope and manage symptoms and reduce stress. Applications that are founded in artificial intelligence and conversational features may play a greater role in playing an ambient supportive role and mediate stress responses during a stressful time.
Discussion
The introduction of technology tools in the context of health care introduces ethical, clinical, and practical challenges (see Table 1). One such challenge is the concern that new tools may exacerbate health disparities rather than reduce the so-called digital divide. Caregivers residing in isolated areas without the necessary infrastructure (for example, high-speed wireless Internet) or resources to acquire and maintain new hardware, may be at a further disadvantage when it comes to accessing high-quality supportive services. Another consideration is that of accessibility of the technology. The design of new tools needs to be informed by the broad spectrum of varying abilities and level of experience with technologies that can be found among family caregivers. During this caregiving time that can be physically and emotionally challenging, it is not always appropriate or feasible to require that caregivers as users receive training in operating new systems. Additionally, usability considerations must ensure that caregivers with diverse functional, visual, and cognitive abilities can use a system safely and as intuitively as possible. This requires that actual caregivers are included in the design phases of new systems. Engaging them in the early stages of the development of a new technology can ensure tools that are more widely accepted and perceived as useful and user-friendly.
Table 1.
Challenges when using technology-based tools.
|
Privacy and confidentiality are important considerations for systems that collect data from or about a caregiver and/or a patient. Systems that become formal parts of a health information system must adhere to HIPAA standards. However, many mobile apps or other consumer technologies often bypass these requirements by being labeled as “lifestyle” applications rather than medical ones. For caregivers to provide full informed consent to use these technologies, we must examine how complex technological terms and processes can be communicated in lay language for individuals to understand potential risks. Even with the use of widely available platforms like social media, consumers are often not fully aware of the possibility of security breaches and this challenge is magnified when using these same platforms for the delivery of health-related interventions.
Finally, the challenge of interoperability is one that persists even as new systems are designed and implemented. With new technologies produced to capture data pertaining to patients’ and caregivers’ health status and needs, the ability to exchange data among systems becomes critical. Several systems perform as stand-alone units and do not exchange data with other formal systems of care (such as an Electronic Medical Record system), leading to redundancies in data documentation and an increased chance for data to get lost or become under-utilized. Considerations for the impact of a new tool on existing workflow are necessary to understand how processes can be optimized to improve data flow. For example, a new system that allows caregivers to record information about their own needs that does not provide a way for these data sets to become easily accessible in a format that is meaningful to clinicians and enhances clinical decision-making is not going to become a sustainable solution. Issues of accountability and liability are additional challenges when utilizing systems that generate new large data sets about patients and caregivers.
Evidence on the effectiveness of technology use to support family caregivers of persons with cancer is growing, but we are still lacking a solid evidence base. The majority of projects examining innovative technology tools focus on feasibility and acceptance with studies of limited sample size and exploratory in nature. Randomized clinical trials testing these tools are in many cases still needed. Additionally, longitudinal examinations of technology use beyond the narrow window of time that is the focus of an experimental study can provide further insight into issues of acceptance and sustainability. Related to this, cost-effectiveness studies are needed to demonstrate the financial implications of technology use. As technology continues to evolve and permeate all aspects of our daily living, the question is not whether it will play a role for family caregivers in the context of cancer care, but rather how to ensure that it becomes an acceptable and effective tool in improving the caregiver experience.
Acknowledgments
This work was supported in part by the National Institute Of Nursing Research of the National Institutes of Health (grant no. R01NR012213). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cronin KA, Lake AJ, Scott S, et al. Annual report to the nation on the status of cancer, part I: National cancer statistics. Cancer. 2018;124:2785–2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Institute of Medicine, Committee on Care at the End of Life, Field MJ, Cassel CK, editors. Approaching death: improving care at the end of life. Washington, DC: National Academies Press; 1997. [PubMed] [Google Scholar]
- 3.Schulz R, Beach SR. Caregiving as a risk factor for mortality: the caregiver health effects study. JAMA. 1999;282:2215–2219. [DOI] [PubMed] [Google Scholar]
- 4.Roth DL, Haley WE, Hovater M, Perkins M, Wadley VG, Judd S. Family caregiving and all-cause mortality: findings from a population-based propensity-matched analysis. Am J Epidemiol. 2013;178:1571–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rossi Ferrario S, Cardillo V, Vicario F, Balzarini E, Zotti AM. Advanced cancer at home: caregiving and bereavement. Palliat Med. 2004;18:129–136. [DOI] [PubMed] [Google Scholar]
- 6.Bee PE, Barnes P, Luker KA. A systematic review of informal caregivers’ needs in providing home-based end-of-life care to people with cancer. J Clin Nurs. 2009;18:1379–1393. [DOI] [PubMed] [Google Scholar]
- 7.Garvelink M, Adekpedjou R, Diouf NT, Goh L, Blair L, Légaré F. A synthesis of knowledge about caregiver decision making finds gaps in support for those who care for aging loved ones. Health Aff (Millwood). 2016;35:619–626. [DOI] [PubMed] [Google Scholar]
- 8.Chwalisz K, Buckwalter KC, Talley RC. Caregiving in rural America: a matter of culture. In: Talley RC, Chwalisz K, Buckwalter KC, editors. Rural caregiving in the United States: research, practice, policy. New York, NY: Springer; 2011: pp 1–14. [Google Scholar]
- 9.Pearlin LI, Schooler C. The structure of coping. J Health Soc Behav. 1978;19:2–21. [PubMed] [Google Scholar]
- 10.Meyers JL, Gray LN. The relationships between family primary caregiver characteristics and satisfaction with hospice care, quality of life, and burden. Oncol Nurs Forum. 2001;28:73–82 [PubMed] [Google Scholar]
- 11.Demiris G, Oliver DP, Wittenberg-Lyles E. Assessing caregivers for team interventions (ACT): a new paradigm for comprehensive hospice quality care. Am J Hosp Palliat Care. 2009;26:128–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chi NC, Demiris G. A systematic review of telehealth tools and interventions to support family caregivers. J Telemed Telecare. 2015;21:37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heynsbergh N, Heckel L, Botti M, Livingston PM. Feasibility, useability and acceptability of technology-based interventions for informal cancer carers: a systematic review. BMC Cancer. 2018;18:244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chih MY, DuBenske LL, Hawkins RP, et al. Communicating advanced cancer patients’ symptoms via the internet: a pooled analysis of two randomized trials examining caregiver preparedness, physical burden, and negative mood. Palliat Med. 2013;27:533–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Namkoong K, DuBenske LL, Shaw BR, et al. Creating a bond between caregivers online: effect on caregivers’ coping strategies. J Health Commun. 2012;17:125–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Song L, Rini C, Deal AM, et al. Improving couples’ quality of life through a web-based prostate cancer education intervention. Oncol Nurs Forum. 2015;42:183–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scott K, Beatty L. Feasibility study of a self-guided cognitive behaviour therapy internet intervention for cancer carers. Aust J Prim Health. 2013;19:270–274. [DOI] [PubMed] [Google Scholar]
- 18.Shin JY, Kang TI, Noll RB, Choi SW. Supporting caregivers of patients with cancer: a summary of technology-mediated interventions and future directions. Am Soc Clin Oncol Educ Book. 2018;38:838–849. [DOI] [PubMed] [Google Scholar]
- 19.Collinge W, Kahn J, Walton T, et al. Touch, caring, and cancer: Randomized controlled trial of a multimedia caregiver education program. Support Care Cancer. 2013;21:1405–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Walsh KE, Biggins C, Blasko D, et al. Home medication support for childhood cancer: family-centered design and testing. J Oncol Pract. 2014;10:373–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Slater PJ, Fielden PE, Bradford NK. The oncology family app: Providing information and support for families caring for their child with cancer. J Pediatr Oncol Nurs. 2018;35:94–102. [DOI] [PubMed] [Google Scholar]
- 22.Oliver DP, Albright DL, Kruse RL, Wittenberg-Lyles E, Washington K, Demiris G. Caregiver evaluation of the ACTIVE intervention: “It was like we were sitting at the table with everyone”. Am J Hosp Palliat Care. 2014;31:444–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stern A, Valaitis R, Weir R, Jadad AR. Use of home telehealth in palliative cancer care: a case study. J Telemed Telecare. 2012;18:297–300. [DOI] [PubMed] [Google Scholar]
- 24.Demiris G, Parker Oliver D, Washington K, Pike K. A problem-solving intervention for hospice family caregivers: a randomized clinical trial. J Am Geriatr Soc. 2019. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Washington KT, Demiris G, Parker Oliver D, Albright DL, Craig KW, Tatum P. Delivering problem-solving therapy to family caregivers of people with cancer: a feasibility study in outpatient palliative care. Psychooncology. 2018;27:2494–2499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oliver DP, Washington K, Wittenberg-Lyles E, Gage A, Mooney M, Demiris G. Lessons learned from a secret Facebook support group. Health Soc Work. 2015;40:125–133. [DOI] [PubMed] [Google Scholar]
- 27.Wittenberg-Lyles E, Washington K, Oliver DP, et al. “It is the ‘starting over’ part that is so hard”: using an online group to support hospice bereavement. Palliat Support Care. 2015;13:351–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dolce MC. The internet as a source of health information: experiences of cancer survivors and caregivers with healthcare providers. Oncol Nurs Forum. 2011;38:353–359. [DOI] [PubMed] [Google Scholar]
- 29.Wang YC, Kraut RE, Levine JM. Eliciting and receiving online support: using computer-aided content analysis to examine the dynamics of online social support. J Med Internet Res. 2015;17:e99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fuentes C, Hernandez C, Escobedo L, Herskovic V, Tentori T. Promoting self-reflection of social isolation through persuasive mobile technologies: the case of mother caregivers of children with cancer. Int J Hum Comput Interact. 2014;30:802–814. [Google Scholar]
- 31.Yoon S, Patrao M, Schauer D, Gutierrez J. Prediction models for burden of caregivers applying data mining techniques. Big Data Info Anal. 2017;2:209–217. [Google Scholar]
- 32.Cassell J, Bickmore T, Billinghurst MN, et al. Embodiment in conversational interfaces: Rea. In: CHI ‘99 Proceedings of the SIGCHI conference on Human Factors in Computing Systems. New York City, NY: Association for Computing Machinery, Inc.; 1999:520–527. [Google Scholar]
- 33.Bickmore TW, Pfeifer LM, Paasche-Orlow MK. Using computer agents to explain medical documents to patients with low health literacy. Patient Educ Couns. 2009;75:315–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carpenter C, Osterberg L, Sutcliffe G. SAMHT - Suicidal avatars for mental health training. In: Youngblood GM, McCarthy PM, editors. Proceedings of the Twenty-Fifth International Florida Artificial Intelligence Research Society Conference. Palo Alto, CA: The AAAI Press; 2012:484–487. [Google Scholar]
- 35.Lisetti C, Amini R, Yasavur U, Rishe N. I can help you change! An Empathic virtual agent delivers behavior change health interventions. ACM Trans Mgmt Info Sys (TMIS). 2013;4:1–28. [Google Scholar]
- 36.Kanaoka T, Mutlu B. Designing a motivational agent for behavior change in physical activity. In: CHI 2015 Extended Abstracts Publication of the 33rd Annual CHI Conference on Human Factors in Computing Systems. New York City, NY: Association for Computing Machinery, Inc; 2015:1445–1450. [Google Scholar]
- 37.Utami D, Bickmore T, Nikolopoulou A, Paasche-Orlow M. Talk about death: End of life planning with a virtual agent. In: Beskow J, Peters C, Castellano G, O’Sullivan C, Leite I, Kopp S, editors. Intelligent Virtual Agents: 17th International Conference, IVA 2017 Stockholm, Sweden, August 27–30, 2017 Proceedings. Cham, Switzerland: Springer Nature; 2017:441–450. [Google Scholar]