Abstract
Objectives:
Outcomes in cardiac surgery are benchmarked against national Society of Thoracic Surgeons (STS) data and include patients undergoing elective, urgent, emergent, and salvage operations. This practice relies on accurate risk adjustment in order to avoid risk-averse behavior. We hypothesize the STS risk calculator does not adequately characterize the risk of salvage operations due to their heterogeneity and infrequent occurrence.
Methods:
All cardiac surgery patients with an STS predicted risk score (2002–2017) were extracted from a regional database of 19 cardiac surgery centers. Patients were stratified by operative status for univariate analysis. Observed to expected (O:E) ratios for mortality and composite morbidity/mortality were calculated and compared among elective, urgent, emergent, and salvage patients.
Results:
A total of 76,498 patients met inclusion criteria. The observed-to-expected mortality ratios for elective, urgent, and emergent cases were 0.96, 0.98, and 0.93, respectively (all p-values >0.05). However, mortality was significantly higher than expected for salvage patients (O:E 1.41 p=0.04). Composite morbidity/mortality was lower than expected in elective (O:E 0.81, p =0.0001) and urgent (O:E 0.93, p =0.0001) cases but higher for emergent (O:E 1.13, p =0.0006) and salvage (O:E 1.24, p =0.01). Observed-to-expected ratios for salvage mortality were highly variable among each of the 19 centers.
Conclusion:
The current STS risk models do not adequately predict outcomes for salvage cardiac surgery patients. Based on these results, we recommend more detailed reporting of salvage outcomes to avoid risk aversion in these potentially life-saving operations.
Keywords: Cardiac Surgery, Public Policy, Outcomes Reporting
Introduction
Public reporting of cardiac surgery outcomes in the modern era began with the release of hospital mortality data by the Health Care Financing Administration in 1986. This unprecedented event was widely criticized due to its reliance on administrative data and inadequate risk adjustment.1 In response, the Society of Thoracic Surgeons (STS) initiated a national database of cardiac surgery patients in 1989.2 The STS adult cardiac surgery database now has over 6 million entries and captures more than 95% of cardiac operations in the United States each year.3 STS data has been used to develop and update risk models to predict operative morbidity and mortality. These risk models allow centers to benchmark their outcomes to national and regional data for quality control.
Recently, there has been an increased focus on transparency in healthcare, including public reporting of clinical outcomes data for use by healthcare consumers, payers, and policy makers.4 Several states have already mandated public outcomes reporting and others will likely follow this example. However, an enduring criticism of public outcomes reporting is that surgeons and hospitals avoid high-risk surgery due to fear of fallout from poor outcomes. There are considerable clinical and survey data that indicate physicians are less likely to intervene on high-risk patients in states where public reporting is mandatory.5–8 In theory, using predictive models to risk adjust outcomes should allay concerns that high-risk operations will negatively impact reported outcomes.9 However, evidence of risk-averse behavior persists despite validation of risk models.
Surgical outcomes will be increasingly scrutinized in the current healthcare landscape where transparency and value-based reimbursement are emphasized. Therefore, it is essential to develop reporting methods that do not deter surgeons from performing high risk, but potentially life saving interventions. The purpose of this study was to evaluate the accuracy of risk-adjusted outcomes used for public reporting in extreme-risk patients. Specifically, we hypothesize that current risk adjustment models do not adequately predict the risk of mortality for patients undergoing salvage cardiac surgery.
Methods
Patients
The Virginia Cardiac Services Quality Initiative (VCSQI) database represents 19 hospitals and cardiac surgery centers in the states of Virginia and North Carolina. Deidentified, patient level data including operative status, STS preoperative risk assessment, and operative morbidity and mortality were obtained from the regional database for all patients who underwent primary coronary artery bypass grafting (CABG), isolated valve, or CABG and valve operations with calculated preoperative risk score from January 2002 through 2017. Clinical data were collected by member institutions using standard STS definitions and data abstraction practices.10 Elective cases were those where the patient’s cardiac function had been stable preoperatively and urgent cases were procedures that were done during the same hospitalization to minimize the chance of deterioration. Operations labeled emergent were done for ongoing cardiac compromise not responsive to medical intervention. Salvage cases are defined as patients who are receiving cardiopulmonary resuscitation en route to the operating room or requiring mechanical circulatory support to maintain life. Due to the de-identified and retrospective nature of the database, this study was granted exemption from review by institutional review boards.
Statistical Analysis
The primary outcome of interest was the risk-adjusted mortality rate for each operative status, reported as the observed-to-expected ratio (O:E). O:E mortality was calculated by dividing operative mortality by the mean STS Predicted Risk of Mortality (PROM) for each of the 4 reported statuses. Secondary outcomes included the observed-to-expected ratio of composite morbidity or mortality, which was similarly calculated using operative major morbidity or mortality and mean STS Predicted Risk of Morbidity or Mortality (PROMM). Separately, risk-adjusted outcomes at each of the 19 VCSQI centers with and without salvage cases are reported as measures of variability.
Continuous variables are reported as mean ± standard deviation (SD) when normally distributed and median [interquartile range (IQR)] for non-normal distributions. Categorical data are summarized as count and corresponding proportion. Observed-to-expected ratios were calculated as previously described and reported with a 95% confidence interval (CI) with significance testing using Pearson chi-square analysis.11 Statistical significance was defined as a two-sided p-value <0.05 Statistical analyses were performed using SAS version 9.4 (SAS institute Inc, Cary, NC) and Prism 7 (GraphPad Software Inc, La Jolla, CA).
Results
Patient data
A total of 76,498 patients underwent isolated CABG, isolated valve, or combined CABG and valve operations with an STS preoperative risk calculation during the study period. The mean age was 64 years and 71.7% were male. Elective operations accounted for 35,237 (46%) of all cases and there were 38,669 (51%) urgent, 2,475 (3%) emergent, and 117 (0.15%) salvage operations. Of the salvage operations 107 (92%) were isolated coronary artery bypass grafts (CABG), 5 (4%) were isolated valves, and 5 (4%) were combined CABG and valve. There were similar rates of preoperative risk factors, including hypertension and end stage renal disease among each operative status. Salvage patients were less likely to have diabetes but more likely to be a reoperation or have had prior percutaneous coronary intervention (PCI) (Table 1).
Table 1:
Preoperative patient characteristics based on operative status
| Total | Elective | Urgent | Emergent | Salvage | |
|---|---|---|---|---|---|
| N | 76,498 | 35,237 | 38,669 | 2,475 | 117 |
| Age (mean, SD) | 64.7 (11.0) | 65.1 (10.8) | 64.4 (11.0) | 63.5 (11.6) | 63.9 (12.5) |
| Male | 54,874 (71.7%) | 25,396 (72.1%) | 27,717 (71.7%) | 1,681 (67.9%) | 80 (68.4%) |
| CABG | 62,318 (81.5%) | 24,927 (70.9%) | 35,008 (90.5%) | 2,276 (92.0%) | 107 (91.5%) |
| AVR | 5,508 (7.2%) | 4,457 (12.7%) | 1,018 (2.6%) | 30 (1.2%) | 3 (2.6%) |
| AVR/CABG | 3,701 (4.8%) | 2,435 (6.9%) | 1232 (3.2%) | 32 (1.3%) | 2 (1.7%) |
| MVR | 1,305 (1.7%) | 794 (2.3%) | 449 (1.2%) | 60 (2.4%) | 2 (1.7%) |
| MVR/CABG | 548 (0.7%) | 252 (0.7%) | 254 (0.7%) | 39 (1.6%) | 3 (2.6%) |
| MVr | 2,052 (2.7%) | 1845 (5.2%) | 198 (0.5%) | 9 (0.4%) | 0 |
| MVr/CABG | 1,018 (1.3%) | 481 (1.4%) | 508 (1.3%) | 29 (1.2%) | 0 |
| HTN | 62,536 (81.8%) | 28,758 (81.6%) | 31,822 (82.3%) | 1,863 (75.4%) | 93 (79.5%) |
| ESRD | 19,90 (2.6%) | 753 (2.1%) | 1,174 (3.0%) | 60 (2.4%) | 3 (2.6%) |
| Diabetes | 30614 (40.0%) | 13556 (38.5%) | 16,151 (41.8%) | 872 (35.3%) | 35 (29.9%) |
| Reoperation | 11,955 (15.6%) | 6,521 (18.5%) | 5,007 (13.0%) | 402 (16.2%) | 25 (21.4%) |
| Prior PCI | 16,526 (21.6%) | 7.234 (20.3%) | 8,568 (22.%) | 784 (31.7%) | 40 (34.2%) |
| PROM (mean, SD) | 2.5% (4.2) | 1.87% (2.3) | 2.62% (3.8) | 9.34% (11.2) | 32.72% (20.6) |
| PROMM (mean, SD) | 16% (12.5) | 13.31% (8.9) | 16.8% (12.7) | 37.07% (21.9) | 64.59% (21.6) |
Categorical data are summarized as count and corresponding proportion. Continuous variables are reported as mean (standard deviation). CABG, coronary artery bypass grafting; AVR, aortic valve replacement; MVR, mitral valve replacement; MVr, mitral valve repair; HTN, hypertension; ESRD, end stage renal disease; PCI, percutaneous coronary intervention, PROM, predicted risk of mortality; PROMM, predicted risk of morbidity or mortality
Mortality
The mean STS PROM for elective, urgent, emergent, and salvage cases were 1.9%, 2.6%, 9.3%, and 32.7% respectively. For elective, urgent, and emergent cases, the observed to expected ratio (O:E) for mortality was less than 1, but not significantly different than expected (all p-values > 0.05) (Table 2). However, the O:E for salvage cases was 1.41 (CI 1.06–1.84 p=0.04), which was significantly higher than predicted by STS PROM (Figure 1).
Table 2:
Expected and observed rates of operative mortality and composite major morbidity based on operative status
| Elective | Urgent | Emergent | Salvage | |
|---|---|---|---|---|
| Expected Mortality | 1.87 % | 2.62% | 9.34% | 32.72% |
| Observed Mortality | 1.79% | 2.56% | 8.69% | 46.15% |
| O:E Mortality (95% CI) | 0.96 (0.88–1.03) | 0.98 (0.921.04) | 0.93 (0.811.05) | 1.41 (1.06–1.84) |
| Expected Morbidity/Mortality | 13.31% | 16.86% | 37.07% | 64.59% |
| Observed Morbidity/Mortality | 10.74% | 15.71% | 41.9% | 80.34% |
| O:E Morbidity or Mortality (95% CI) | 0.81 (0.780.83) | 0.93 (0.910.96) | 1.13 (1.06–1.2) | 1.24 (1.01.52) |
Observed-to-expected ratios are reported with a 95% confidence interval (CI). O:E, observed to expected ratio; CI, confidence interval *composite major morbidity includes permanent stroke, prolonged ventilation, renal failure, reoperation, and deep sternal wound infection
Figure 1:
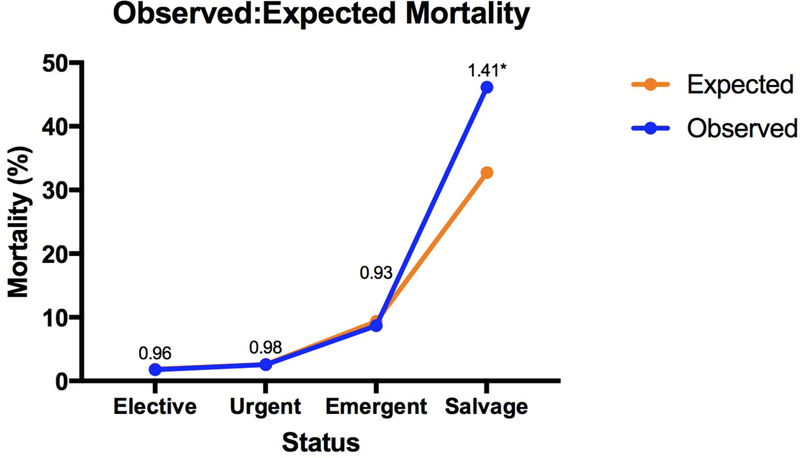
Operative mortality rate (blue), mean Society of Thoracic Surgeons predicted risk of mortality (orange), and observed to expected mortality ratio (numeral) for elective, urgent, emergent, and salvage cardiac surgery patients in a regional consortium of cardiac surgery centers. Mortality ratios were calculated by dividing operative mortality by mean predicted risk of mortality and significance was determined using Pearson chi-square analysis. * denotes significance (p<0.05)
Morbidity
The O:E ratios for composite morbidity or mortality for elective and urgent cases were 0.81 (95% CI 0.78 – 0.83, p=0.0001) and 0.93 (95% CI 0.91 – 0.96, p=0.0001), respectively. In contrast, emergent and salvage morbidity or mortality ratios were 1.13 (95% CI 1.06 – 1.2, p=0.0006) and 1. 24 (95% CI 1.0 – 1.52, p=0.01), both significantly higher than predicted by the STS risk calculators. The rates of each of the major morbidities for each status are shown in Table 3.
Table 3:
Rates of each major morbidity based on operative status
| Elective | Urgent | Emergent | Salvage | |
|---|---|---|---|---|
| Permanent stroke | 385 (1.09%) | 585 (1.51%) | 66 (2.67%) | 7 (5.98%) |
| Prolonged Vent | 2,274 (6.45%) | 4,258 (11.01%) | 909 (36.73%) | 71 (60.68%) |
| Renal failure | 868 (2.46%) | 1,437 (3.72%) | 203 (8.2%) | 29 (24.79%) |
| Reoperation | 890 (2.53%) | 1,034 (2.67%) | 127 (5.13%) | 17 (14.53%) |
| DSWI | 25 (0.07%) | 26 (0.07%) | 3 (0.12%) | 0 |
Categorical data are summarized as count and corresponding proportion. Prolonged vent, prolonged ventilation (>24 hours); DSWI, deep sternal wound infection
Variability
Salvage operations were performed at 15 of 19 centers during the study period and the calculated risk of mortality for these patients varied widely. The mean PROM among centers was 32.72% with a standard deviation of ±20.73 and a range of 5.3–56.2%. Observed-to-expected ratios for salvage mortality were greater than 1 at 11 centers (73%), 2 centers had no operative mortalities (O:E ratio=0), and 2 centers reported better than expected mortality (Figure 2). When broken down by STS data version, the O:E mortality after the exclusion of salvage cases was similar to the O:E for all patients at most centers. Overall, the mean change in O:E mortality after the exclusion of salvage cases ranged from 0.00–0.04 in each of the data versions but centers were not affected equally. (supplemental table).
Figure 2:
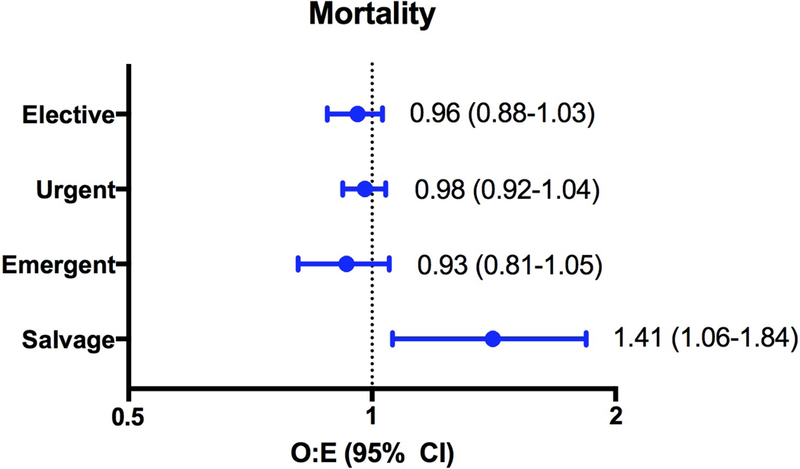
Observed to expected mortality ratios and 95% confidence intervals for elective, urgent, emergent, and salvage cardiac surgery patients. Mortality ratios were calculated by dividing operative mortality by mean Society of Thoracic Surgeons predicted risk of mortality.
Discussion
By comparing risk adjusted morbidity and mortality for over 70,000 patients undergoing elective, urgent, emergent, and salvage operations in a large statewide consortium of cardiac surgery centers, we demonstrated current risk adjustment methods do not perform well for salvage operations. Observed rates of surgical morbidity and mortality are significantly higher than expected for salvage patients in the entire cohort and, when viewed at the center level, are widely variable for these cases compared to more common, lower risk operations.
The Patient Protection and Affordable Care Act of 2010 called for increased transparency in healthcare including a push for public reporting.12 Coincidentally, the STS has emerged as a national leader in public reporting with the development of their own voluntary rating system that incorporates STS risk adjusted outcomes along with National Quality Forum endorsed metrics.13, 14 Based on the current healthcare environment and the positive reception and broad appeal of the current STS model, risk- adjusted outcomes will likely be a key driver of public perception, accreditation, and reimbursement in the future. However, if risk adjustment is not accurate for all patients, public reporting of outcomes may have unintended consequences.
The decision of whether or not to intervene on patients who present for cardiac surgery requiring cardiopulmonary resuscitation or mechanical circulatory support to maintain life is obviously complex. It is important to keep in mind that salvage cases represent a heterogeneous group of patients and, as our findings confirm, it is difficult to predict how they will do postoperatively. Often, the decision to operate is made on a compassionate basis. However, in the present study 54% of patients survived until hospital discharge which is consistent with reports from European countries that have also shown nearly half of patients are still alive 5 years later, indicating that meaningful recovery is possible despite a dismal outlook initially.15, 16 When presented with an emergent consult, surgeons should be able to focus on all available information to make the best decision for their patient. Competing interest such as fiscal responsibility and institutional reputation, while important, are secondary concerns and should not deter surgeons from offering life-saving operations.
One of the earliest and most persistent objections to public outcomes reporting was that it would alter physician behavior to the detriment of the sickest patients. While the evidence for risk aversion amongst cardiac surgeons is debated, changes in referral patterns and time to intervention for high-risk patients have been documented in response to mandatory public outcomes reporting.5, 7, 8, 17 Additionally, analysis of interventional cardiology data from states where public reporting is mandatory have demonstratively shown lower rates of intervention in patients who present in cardiogenic shock after acute myocardial infarction.18–21
Some have proposed that a potential solution to the problem of risk aversion is accurate risk adjustment for publically reported outcomes.9 Current risk models are based on retrospective data from the STS adult cardiac surgery database (ACSD). The ACSD is the largest clinical database of its kind and sets the industry standard due to careful collection, auditing, and maintenance of patient level clinical data. Several authors have validated STS risk model precision in elective as well as high-risk patients groups.22–24 However, the model’s precision depends upon the definition of high risk. Previous work by our group demonstrated that the relationship between expected mortality and the probability of death for patients undergoing CABG diverges in extreme risk groups, particularly when PROM is greater than 25%.25 In the current study the average PROM of salvage patients is over 30%, above the threshold for decreased model precision and far above previous definitions of high-risk. 24 In terms of the overall effect of salvage cases on outcomes reporting, the relatively low number of instances keeps them from becoming statistically significant. However, we remain concerned surgeons overestimate their influence when faced with the challenging decision of whether or not to operate.
To aid decision-making we should first reevaluate what it means to be a salvage operation. The current broad definition of requiring cardiopulmonary resuscitation or mechanical circulatory support is inadequate given that there are now multiple devices capable of providing varying levels of circulatory support. This technology allows for preoperative stabilization of critically ill patients, which affects postoperative outcomes. Added granularity is warranted to further differentiate and risk-stratify these patients. STS predictive risk scores are based largely on standard risk patients and are excellent predictors of outcomes in that group. However, there are other models that have been developed for extreme-risk patients that are more relevant to the salvage population.26–28 These models are not necessarily more complex and could be easily be incorporated into the decision making process once patients are identified as salvage cases.
This study has several limitations. Due to its retrospective nature it is vulnerable to selection bias and inability to determine causation. While the study represents results from 19 independent hospitals in multiple states, including large and small practices in academic and private settings, these results may not be generalizable to other populations. Finally, the low volume of salvage cases makes thorough statistical interpretation challenging and evaluating our hypothesis in a larger dataset could be confirmatory.
Conclusion
In a regional consortium of over 70,000 cardiac surgery cases over a 16 year period, salvage cases had significantly higher than expected risk adjusted morbidity and mortality indicating current risk models do not adequately predict outcomes for these extremely high risk operations. Based on these findings, we recommend more detailed definitions and separate reporting for salvage cases to avoid risk aversion in potentially life saving operations.
Supplementary Material
Figure 3:
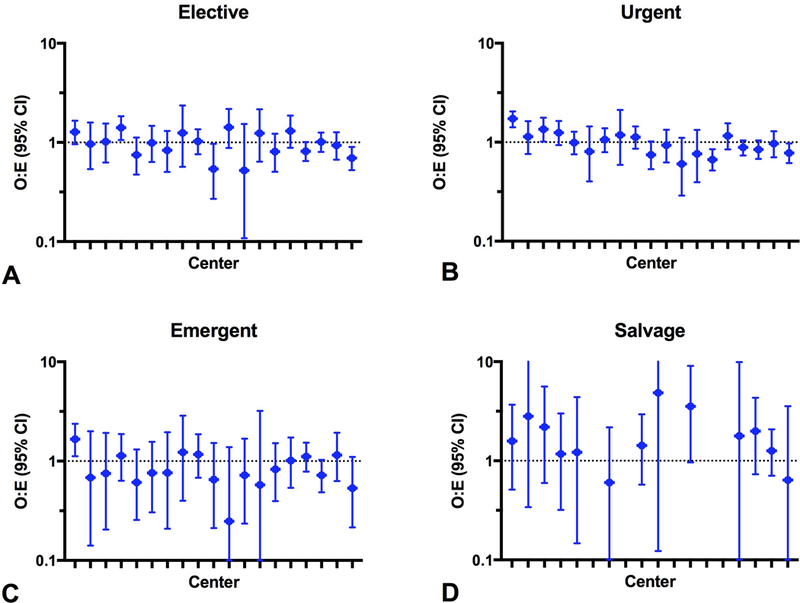
Observed to expected mortality ratios and 95% confidence intervals for elective (A), urgent (B), emergent (C), and salvage (D) cardiac surgery patients at each center in a regional consortium of cardiac surgery centers. Mortality ratios were calculated by dividing operative mortality by mean Society of Thoracic Surgeons predicted risk of mortality Video: Dr. William Chancellor discusses the results of a multi-institutional collaborative study on the accuracy of preoperative risk assessment in high-risk cardiac surgery patients..
Central Message
Current risk models are not accurate for extreme-risk cardiac surgery patients. To avoid risk aversion, salvage operations should be better defined and separately reported.
Perspective Statement
Accurate risk adjustment is essential to avoid unintended consequences of public outcomes reporting, such as the denial of care to high-risk patients. This study demonstrates that current risk models, while excellent for standard-risk patients, are inadequate for salvage operations. To avoid risk aversion, these extreme-risk cases should be more clearly defined to allow for accurate risk adjustment.
Acknowledgments
Funding:This work was supported by the National Heart, Lung, and Blood Institute (grants UM1 HL088925 and T32 HL007849).
Abbreviations
- STS
Society of Thoracic Surgeons
- VCSQI
Virginia Cardiac Services Quality Initiative
- CABG
coronary artery bypass grafting
- O:E
observed-to-expected ratio
- PROM
predicted risk of mortality
- PROMM
predicted risk of morbidity or mortality
- ACSD
adult cardiac surgery database
- PCI
percutaneous coronary intervention
Footnotes
Presentation: 44th Annual Meeting of the Western Thoracic Surgical Association, Goleta, CA from June 27–30, 2018
Conflicts of Interest: Dr. Ailawadi is a consultant for Abbott, Edwards, Medtronic, Cephea, and Admedus. Dr. Speir is a member of the Medtronic North American Cardiac Surgery Advisory Board.
References
- 1.Rosen HM, Green BA. The HCFA excess mortality lists: a methodological critique. Hosp Health Serv Adm. 1987;32:119–127. [PubMed] [Google Scholar]
- 2.Clark RE. The development of The Society of Thoracic Surgeons voluntary national database system: genesis, issues, growth, and status. Best Pract Benchmarking Healthc. 1996;1:62–69. [PubMed] [Google Scholar]
- 3.D’Agostino RS, Jacobs JP, Badhwar V, et al. The Society of Thoracic Surgeons Adult Cardiac Surgery Database: 2018 Update on Outcomes and Quality. Ann ThoracSurg. 2018;105:15–23. [DOI] [PubMed] [Google Scholar]
- 4.Shahian DM. Public reporting of cardiac surgery outcomes--what do we know, what can we expect? J Card Surg. 2010;25:710–712. [DOI] [PubMed] [Google Scholar]
- 5.Omoigui NA, Miller DP, Brown KJ, et al. Outmigration for coronary bypass surgery in an era of public dissemination of clinical outcomes. Circulation. 1996;93:27–33. [DOI] [PubMed] [Google Scholar]
- 6.Burack JH, Impellizzeri P, Homel P, Cunningham JN Jr. Public reporting of surgical mortality: a survey of New York State cardiothoracic surgeons. Ann Thorac Surg. 1999;68:1195–1200; discussion 1201–1192. [DOI] [PubMed] [Google Scholar]
- 7.Werner RM, Asch DA. The unintended consequences of publicly reporting quality information. Jama. 2005;293:1239–1244. [DOI] [PubMed] [Google Scholar]
- 8.Bridgewater B, Grayson AD, Brooks N, et al. Has the publication of cardiac surgery outcome data been associated with changes in practice in northwest England: an analysis of 25,730 patients undergoing CABG surgery under 30 surgeons over eight years. Heart. 2007;93:744–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hannan EL, Siu AL, Kumar D, Racz M, Pryor DB, Chassin MR. Assessment of coronary artery bypass graft surgery performance in New York. Is there a bias against taking high-risk patients? Med Care. 1997;35:49–56. [DOI] [PubMed] [Google Scholar]
- 10.Jacobs JP, Shahian DM, Prager RL, et al. Introduction to the STS National Database Series: Outcomes Analysis, Quality Improvement, and Patient Safety. Ann Thorac Surg. 2015;100:1992–2000. [DOI] [PubMed] [Google Scholar]
- 11.Carriere KC, Roos LL. Comparing standardized rates of events. Am J Epidemiol. 1994;140:472–482. [DOI] [PubMed] [Google Scholar]
- 12.Services USDoHaH. Key features of the Affordable Care Act by year. [Google Scholar]
- 13.Shahian DM, Edwards FH, Ferraris VA, et al. Quality measurement in adult cardiac surgery: part 1--Conceptual framework and measure selection. Ann Thorac Surg. 2007;83:S3–12. [DOI] [PubMed] [Google Scholar]
- 14.O’Brien SM, Shahian DM, DeLong ER, et al. Quality measurement in adult cardiac surgery: part 2--Statistical considerations in composite measure scoring and provider rating. Ann Thorac Surg. 2007;83:S13–26. [DOI] [PubMed] [Google Scholar]
- 15.Santarpino G, Ruggieri VG, Mariscalco G, et al. Outcome in Patients Having Salvage Coronary Artery Bypass Grafting. Am J Cardiol. 2015;116:1193–1198. [DOI] [PubMed] [Google Scholar]
- 16.Axelsson TA, Mennander A, Malmberg M, Gunn J, Jeppsson A, Gudbjartsson T. Is emergency and salvage coronary artery bypass grafting justified? The Nordic Emergency/Salvage coronary artery bypass grafting study. Eur J CardiothoracSurg. 2016;49:1451–1456. [DOI] [PubMed] [Google Scholar]
- 17.Dranove DKD, McClellan M, Satterwaite M‥ Is more information better? The effects of “report cards” on health care providers‥ J Polit Ecom. 2003;111:555–588. [Google Scholar]
- 18.Moscucci M, Eagle KA, Share D, et al. Public reporting and case selection for percutaneous coronary interventions: an analysis from two large multicenter percutaneous coronary intervention databases. J Am Coll Cardiol. 2005;45:1759–1765. [DOI] [PubMed] [Google Scholar]
- 19.Apolito RA, Greenberg MA, Menegus MA, et al. Impact of the New York State Cardiac Surgery and Percutaneous Coronary Intervention Reporting System on the management of patients with acute myocardial infarction complicated by cardiogenic shock. Am Heart J. 2008;155:267–273. [DOI] [PubMed] [Google Scholar]
- 20.Joynt KE, Blumenthal DM, Orav EJ, Resnic FS, Jha AK. Association of public reporting for percutaneous coronary intervention with utilization and outcomes among Medicare beneficiaries with acute myocardial infarction. Jama. 2012;308:1460–1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Waldo SW, McCabe JM, O’Brien C, Kennedy KF, Joynt KE, Yeh RW. Association between public reporting of outcomes with procedural management and mortality for patients with acute myocardial infarction. J Am Coll Cardiol. 2015;65:1119–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jin R, Furnary AP, Fine SC, Blackstone EH, Grunkemeier GL. Using Society of Thoracic Surgeons risk models for risk-adjusting cardiac surgery results. Ann ThoracSurg. 2010;89:677–682. [DOI] [PubMed] [Google Scholar]
- 23.Puskas JD, Kilgo PD, Thourani VH, et al. The society of thoracic surgeons 30- day predicted risk of mortality score also predicts long-term survival. Ann Thorac Surg. 2012;93:26–33; discussion 33–25. [DOI] [PubMed] [Google Scholar]
- 24.Englum BR, Saha-Chaudhuri P, Shahian DM, et al. The impact of high-risk cases on hospitals’ risk-adjusted coronary artery bypass grafting mortality rankings. Ann Thorac Surg. 2015;99:856–862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.LaPar DJ, Filardo G, Crosby IK, et al. The challenge of achieving 1% operative mortality for coronary artery bypass grafting: a multi-institution Society of Thoracic Surgeons Database analysis. The Journal of thoracic and cardiovascular surgery. 2014;148:2686–2696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Muller G, Flecher E, Lebreton G, et al. The ENCOURAGE mortality risk score and analysis of long-term outcomes after VA-ECMO for acute myocardial infarction with cardiogenic shock. Intensive Care Med. 2016;42:370–378. [DOI] [PubMed] [Google Scholar]
- 27.Schmidt M, Burrell A, Roberts L, et al. Predicting survival after ECMO for refractory cardiogenic shock: the survival after veno-arterial-ECMO (SAVE)-score. Eur Heart J. 2015;36:2246–2256. [DOI] [PubMed] [Google Scholar]
- 28.Poss J, Koster J, Fuernau G, et al. Risk Stratification for Patients in Cardiogenic Shock After Acute Myocardial Infarction. J Am Coll Cardiol. 2017;69:1913–1920. [DOI] [PubMed] [Google Scholar]
- 29.Sherwood MW, Brennan JM, Ho KK, et al. The impact of extreme-risk cases on hospitals’ risk-adjusted percutaneous coronary intervention mortality ratings.JACC CardiovascInterv 2015;8:10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hannan EL, Cozzens K, King SB 3rd, Walford G, Shah NR. The New York State cardiac registries: history, contributions, limitations, and lessons for future efforts to assess and publicly report healthcare outcomes. J Am Coll Cardiol. 2012;59:2309–2316. [DOI] [PubMed] [Google Scholar]
- 31.McCabe JM, Waldo SW, Kennedy KF, Yeh RW. Treatment and Outcomes of Acute Myocardial Infarction Complicated by Shock After Public Reporting Policy Changes in New York. JAMA Cardiol. 2016;1:648–654. [DOI] [PubMed] [Google Scholar]
- 32.Rab T, Interventional C, Wilson H, Board of G. Public Reporting of Mortality After PCI in Cardiac Arrest and Cardiogenic Shock: An Opinion From the Interventional Council and the Board of Governors of the American College of Cardiology. JACC Cardiovasc Interv. 2016;9:496–498. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


