Abstract
Background
Digital health interventions have potential to contribute to better health outcomes, better healthcare and lower costs. However, evidence for their effectiveness is variable. The development and content of digital health interventions are often not described in enough detail to enable others to replicate the research or improve on previous interventions. This has led to a call for transparent reporting of intervention content and development.
Purpose
To describe the development process and content of a digital self-management intervention for people with type 2 diabetes (HeLP-Diabetes) that has been found to achieve its target clinical outcome, the reduction of HbA1c, a measure of glycaemic control.
Method
We synthesised theory, data from existing research evidence and international guidelines, and new qualitative data from target users to identify the determinants of self-management and the content to be included in HeLP-Diabetes. Using an ongoing iterative participatory design approach the content of the intervention was written, produced, reviewed and changed.
Conclusion
It is possible to develop and transparently report self-management programmes for long-term conditions, which reflect current best evidence, theoretical underpinning and user involvement. We intend that reporting the development process and content will inform future digital intervention development.
Abbreviations: T2DM, Type 2 diabetes mellitus; MRC, Medical Research Council; HeLP Diabetes, Healthy Living for People with Type 2 Diabetes; HCPs, Health Care Professionals; NPT, Normalisation Process Theory; NICE, National Institute for Health Care Excellence; CBT, Cognitive Behaviour Therapy; LLTTF, Living Life to the Full; HealthTalk Online, HTO; RNIB, Royal National Institute of Blind People
Keywords: Diabetes mellitus, type 2; Self-management; Patient education as topic; Internet; Digital intervention development; Participatory design
Highlights
-
•
Uptake of group based self-management education by people with T2DM is low. Digital health interventions may provide an additional mode of delivery.
-
•
A participatory design approach provides a way of synthesising different sources of data to develop a self-management intervention for people living with a long-term condition.
-
•
It is important that the content and development process of interventions are described for other researchers to build on, so that science is cumulative.
1. Background
Type 2 diabetes mellitus (T2DM) is one of the commonest long-term conditions, affecting about 10% of the global population, or around 422 million people (NCD Risk Factor Collaboration (NCD-RisC), 2016). People with diabetes are more likely to have or develop health complications such as cardiovascular disease and to die prematurely than people without diabetes (National Collaborating Centre for Chronic Conditions, 2008). Many of these complications can be avoided if people with diabetes are supported to understand and self-manage their condition (Davies et al., 2008; Deakin, 2011; Khunti et al., 2012; Steinsbekk et al., 2012). Current international guidelines promote the provision of self-management support and diabetes education, usually through face-to-face group-based structured education sessions (National Institute of Health and Care Excellence (NICE) Guideline NG28, 2015; American Diabetes Association, 2015). However, uptake of such education is low. For example, in 2015 in the UK, <9% of patients reported attending a structured education session within one year of diagnosis (National Diabetes Audit, 2018), possibly because face-to-face group-based courses may not suit people who work, have caring responsibilities at home, have mobility problems, or who find group interactions difficult (Winkley et al., 2015; Horigan et al., 2016). Thus, there is an urgent need to find cost-effective and acceptable methods of delivering sustainable self-management education for people with T2DM.
One possibility is the use of digital health interventions (i.e. interventions delivered via digital technologies such as websites or smartphones) as an alternative or additional method of delivering self-management education. These have many potential advantages over group-based education, including convenience, accessibility and anonymity. They also have the potential to help meet healthcare's triple aim of better health outcomes, better healthcare and lower costs (Berwick et al., 2008; Wachter, 2015; Craig et al., 2011).
1.1. Digital health interventions for T2DM self-management
A systematic review and meta-analysis of randomised controlled trials of digital self-management interventions for people with T2DM, showed overall a small positive effect on glycaemic control (pooled effect on HbA1c = −0.21%; CI −0.37% to −0.05%; Z = 2.63) (Pal et al., 2013). Each 1% reduction in HbA1c is associated with a risk reduction of 21% for deaths related to diabetes and a 37% risk reduction for microvascular complications (Stratton et al., 2000). However, the review found no statistically significant differences between the control and intervention groups of the five studies that measured health-related quality of life. The effects of the individual interventions included were also inconsistent for secondary outcomes such as, knowledge, self-efficacy for managing diabetes, social support, health behaviours and emotional outcomes such as anxiety and depression. More recent studies that were not included in the review have shown that digital interventions developed for both people with type 1 and type 2 diabetes can be effective in reducing depressive symptoms and diabetes related distress compared to a wait list control (van Bastelaar et al., 2011) and an online psychoeducational programme (Nobis et al., 2015). The differences in effectiveness between these studies and those included in the review are likely to be related to differences in the content and delivery of the interventions as well as levels of user engagement. However, as these were rarely described in detail, it was not possible for the reviewers to identify factors associated with beneficial impacts (Pal et al., 2013).
This problem has been noted for health and behaviour change interventions more generally (Michie et al., 2009a), making it difficult for future researchers to replicate or improve on previous research. This lack of understanding in turn impacts on our ability to generate an accumulating knowledge base around such interventions, needed both for developing more effective interventions and for informing practice and policy (Murray et al., 2016). Attempts to improve the reporting of interventions include the Medical Research Council's (MRC) guidance on developing, evaluating and implementing complex intervention (Craig et al., 2008), and the TIDieR (template for intervention description and replication) guidelines on reporting of interventions (Hoffmann et al., 2014). The TIDieR guidelines focus on reporting the final content of interventions; however, the process of development can be as important as the final content. Moreover, as the development of digital health interventions for self-management is a relatively new field, it can be hard for researchers or practitioners to know how to approach the development process.
The aim of this paper is to describe the development process of a digital self-management intervention for people with T2DM (Healthy Living for People with type 2 Diabetes (HeLP-Diabetes: https://www.help-diabetes.org.uk)). HeLP-Diabetes has been found to be cost-effective and effective at reducing glycated haemoglobin (Hb1Ac), but not at reducing diabetes-related distress in a randomised controlled trial (Murray et al., 2015; Murray et al., 2017; Li et al., 2018). HeLP-Diabetes was intended to be used as an unguided intervention, which would support users from diagnosis through to the end of their illness journey with diabetes, unlike programmes such as DESMOND (Diabetes Education and Self Management for Ongoing and Newly Diagnosed), which are specifically aimed at newly diagnosed patients (Khunti et al., 2012). It is due to be widely implemented into routine NHS care, initially through a commissioning model by individual Clinical Commissioning Groups, and more recently through a license to NHS England. The work involved in developing HeLP-Diabetes took place between March 2011 and March 2013. The randomised controlled trial ran from 2013 to 2016. We hope this will provide transparency for readers and an example for others who want to develop digital health interventions in the future.
2. Methods
2.1. Design
We used the MRC framework for development of complex interventions (Craig et al., 2008) as an overarching guide to our development process. The framework suggests: 1) identifying appropriate theory, 2) collecting primary qualitative research to identify target users' needs, and 3) identifying existing research evidence in order to determine the content to be included within HeLP-Diabetes. A participatory design (Kushniruk and Nohr, 2016) approach was used to synthesise these three sources by mapping, integrating and revising to co-create the final intervention.
2.2. Theoretical frameworks and models
Based on our research group's previous experience in e-health (Kerr et al., 2006; Kerr et al., 2010; Linke et al., 2008; Wallace et al., 2011; McCarthy et al., 2012; Carswell et al., 2012) we identified three key areas for creating effective self-management digital interventions for long-term conditions that we wished to build on and would benefit from a strong theoretical underpinning. These were: a) understanding the overall impact of a long-term condition on a person's life and sense of self, and the importance of taking a holistic approach to the work required for self-management; b) behaviour change support (as so much of diabetes management requires changes to behaviours such as diet and physical activity; and c) the challenge of ensuring that the final intervention could be effectively implemented into routine healthcare.
2.2.1. Corbin and Strauss' model of living with a long-term condition
A key theoretical model that describes the overall impact of a long-term condition on people's lives and sense of self is the Corbin and Strauss' model (Corbin and Strauss, 1988), which describes three areas of work required by those affected: illness work, everyday life work, and biographical work. This leads to three areas of self-management: medical management (e.g. remembering to take medications regularly, managing interactions with Health Care Professionals (HCPs), eating healthily and exercising more, and stopping or cutting down smoking and drinking alcohol); emotional management (e.g. managing the many cognitions and emotions such as anger, fear, anxiety, guilt, frustration, sadness, depression and denial, that are commonly experienced by people with a long-term condition); and role management (e.g. managing the biographical disruption and changes to identities and roles required by living with a long-term condition), with all three areas being equally essential.
2.2.2. Taxonomy of behaviour change techniques
There are many psychological theories predicting behaviour change, several of which include overlapping concepts (Armitage and Conner, 2000). Rather than opt for one specific theory, and because we were more interested in changing behaviour than predicting it, we adopted the Abraham and Michie taxonomy of behaviour change techniques (Abraham and Michie, 2008) rather than a single theory. Behaviour change techniques were selected based on research evidence for the user-defined target behaviours and behaviour change techniques from the qualitative data with target users.
2.2.3. Normalisation Process Theory (NPT)
A priority was to ensure that the final intervention could be easily implemented into routine care within the British National Health System (NHS). There were two reasons for this: first, that despite the potential of digital health interventions to improve care, there are few examples of their use in routine care, limiting their impact on health; and secondly, we hypothesised that integrating the intervention into routine care would enhance uptake and use by patients. This would help address two main concerns about digital health interventions, namely the problem of low use and low adherence to such interventions (Eysenbach, 2005), and the problem of the “digital divide”, or the way that such interventions may widen health inequalities between those who do and do not use digital interventions (Viswanath and Kreuter, 2007). To maximise the likelihood of our intervention being easily incorporated into routine health care (normalised), we applied the principles of Normalisation Process Theory (NPT) during the development process. NPT is a sociological theory focusing on the work of implementation and integration of complex interventions into routine health care (May and Finch, 2009). It has been used extensively to understand the success or failure of implementations and more recently, to predict and plan for successful implementation (May et al., 2018; Ross et al., 2018). There are four main components to the theory: coherence; cognitive participation; collective action and reflexive monitoring (May and Finch, 2009). For an intervention to ‘normalise’ HCPs need to: understand the purpose of the intervention (coherence); be prepared to invest time and energy into it (cognitive participation); feel that it fits well with their current work (collective action); and perceive the intervention to be worthwhile (reflexive monitoring). Thus our work with HCPs focused on identifying and including features that would promote these four factors, while avoiding those that would have a negative impact on them.
2.3. Identifying user requirements
Establishing user requirements for any proposed intervention is an essential first step (Bartholomew et al., 1998). Our target users were people with T2DM and the HCPs caring for them. We conceptualised user requirements as “wants”, which were features which would make them want to use it and “needs” which were features needed to improve health outcomes. For people with T2DM, our primary data collection method was focus groups which allowed participants to clarify their views through interactions with each other (Kitzinger, 1995) and explore their underlying reasons for differing perspectives allowing for consensus building around solutions which would meet a range of user requirements.
NPT predicted that integration of the intervention into routine health care (normalisation) required including features that maximised the coherence and cognitive participation of HCPs, while minimising the work of implementation (collective action) and promoting reflexive monitoring. A combination of individual interviews and focus groups were used to collect data from HCPs, because of the challenges of recruiting and bringing HCPs together at a mutually convenient time and location.
2.3.1. Ethics
Ethics approval was provided by the North West London Local Research Ethics Committee on behalf of the National Research Ethics Service (reference number: 10/H0722/86).
2.3.2. People with T2DM
Four focus groups and one interview were conducted in a community centre in London with a total of 20 people with T2DM. For details of the recruitment strategies, data collection and analytical procedures please see Pal et al. (2018). We advertised online and offline, aiming to recruit a maximum variety sample in terms of demographic factors (e.g. age, sex, and ethnicity) and clinical factors (e.g. duration of DM since diagnosis, current treatment). The number of participants in each focus group ranged from three to six. The majority of participants were white British (14/20) but Black, Asian and Other (Iranian) ethnicities were also represented. Just over half were male (12/20), with a mean age of 56.8 years (range 36–77 years). The time since diagnosis of diabetes ranged from three months to 36 years (see Table 1 for participant characteristics).
Table 1.
Participant characteristics for people with T2DM (N = 20).
| Characteristic | Number of participants | % |
|---|---|---|
| Gender | ||
| Male | 12 | 60 |
| Female | 8 | 40 |
| Employment status | ||
| Employed | 5 | 25 |
| Not working but looking for work | 2 | 10 |
| Retired | 8 | 40 |
| Retired (semi) | 1 | 5 |
| Not working and not looking for work | 2 | 10 |
| Other - full time student | 1 | 5 |
| Other - volunteer | 1 | 5 |
| Education | ||
| School leaver | 4 | 20 |
| A level | 5 | 25 |
| Degree | 11 | 55 |
| Ethnicity | ||
| White British | 14 | 70 |
| Black (African, Caribbean and Other) | 4 | 20 |
| Asian (Indian) | 1 | 5 |
| Other (Iranian) | 1 | 5 |
| Duration of diabetes | ||
| <1 year | 2 | 10 |
| 1–5 years | 7 | 35 |
| 6–10 years | 5 | 25 |
| >10 years | 6 | 30 |
| Diabetes management | ||
| Diet only | 3 | 15 |
| Diet + tablets | 10 | 50 |
| Diet + tablets + liraglutide injection | 1 | 5 |
| On insulin | 6 | 30 |
| Home internet access | ||
| Yes | 19 | 95 |
| No | 1 | 5 |
| Attended diabetes education | ||
| Yes | 12 | 60 |
| No | 8 | 40 |
| Used the internet to look up diabetes related information | ||
| Yes | 17 | 85 |
| No | 3 | 15 |
The focus groups with people with T2DM lasted 3 h and were led by at least two facilitators (EM, FS, CD & KP). At the start of the group, participants were asked to spend their time on individual computers using three self-management websites for T2DM that ranged in their content, tone, and complexity. Participants were given a maximum of 30 min to try each website to explore what they liked or disliked about it and how it might be useful to them. Participants then came together for a group discussion guided by one of the facilitators.
The topic guide for this discussion was semi-structured and informed by the components of NPT and Corbin and Strauss' model. Participants were asked about their overall impressions of the usefulness of the three websites, followed by specific likes and dislikes, and the reasons for these reactions. This led into a discussion of ideas for ‘ideal’ content on a website to aid self-management. Participants were encouraged to voice issues that were important to them, rather than respond to researcher prompts. Participants were also asked why and when they might use such a website, what would encourage them to use it, whether they would like to share health-related data with their HCPs, and whether they would like a health care professional to facilitate use, and if so, how.
2.3.3. Healthcare professionals
In parallel, four focus groups and seven individual interviews (N = 18) were conducted with a variety of HCPs (endocrinologists, general practitioners, a dietician, practice nurses, diabetes specialist nurses, a nurse consultant) recruited via advertising and snowball sampling. The number of participants recruited to take part in each focus group ranged from two to four. Over half were female (11/18), with a mean age of 49 years (range 32–64 years). Nearly all (17/18) HCPs were white British (see Table 2 for HCPs participant characteristics). For more details of the methods see Murray et al. (2018).
Table 2.
Participant characteristics for Health Care Professionals (N = 18).
| Characteristic | Number of participants | % |
|---|---|---|
| Gender | ||
| Male | 7 | 39 |
| Female | 11 | 61 |
| Profession | ||
| GP partner | 3 | 17 |
| Salaried GP | 5 | 28 |
| Practice nurse | 2 | 11 |
| GP trainee | 1 | 5 |
| Diabetes specialist nurse | 3 | 17 |
| Dietitian | 1 | 5 |
| Endocrinologist | 2 | 11 |
| Diabetes nurse consultant | 1 | 5 |
| Ethnicity | ||
| White British | 17 | 94 |
| Asian (Indian) | 1 | 6 |
The focus groups and interviews with HCPs lasted between 30 and 90 min and were led by at least one facilitator (FS, CD, KP). The topic guide was informed by NPT, and focused on features that would distinguish our proposed intervention from available websites (coherence), features that would encourage (or conversely discourage) HCPs from using the intervention and recommending it to their patients (cognitive participation), features that would make it easy to use in clinical practice (collective action), and information that would promote use (reflexive action), while using open questions to enable participants to think widely around the issues of self-management and to encourage them to bring up ideas that were important to them, rather than the research team.
2.3.4. Data analysis
Data analysis was undertaken in parallel with data collection, which continued until thematic saturation had been reached, defined as no new codes or themes emerging in subsequent transcripts. All focus groups and interviews were audio taped and transcribed verbatim, with initial analyses focused on determining the content and design features of the intervention. This analysis was based on a coding framework agreed in a multidisciplinary meeting comprising of a medical sociologist, health psychologists and GPs. Transcripts were independently read by each researcher and themes were extracted. Focus groups and interviews continued until no new data emerged regarding content (e.g. data saturation). An overview of the findings is shown in Table 3.
Table 3.
Users requirements from a digital self-management intervention to facilitate use and to improve health outcomes.
| People with T2DM (N = 20) | Health Care Professionals (N = 18) | |
|---|---|---|
| Likes/features to include | - Lots of information provision (e.g. medical, dietary, physical activity, alternative medicine, pregnancy, health services, practical advice about day to day living with diabetes including dealing with emotions) - Tools to track self-monitoring data - Links to other useful websites - Ask the Expert function - Frequently Asked Questions - Personal stories - Quizzes to test knowledge and provide feedback |
- Tailored Information and advice - Patient stories - Help with emotional management - Summary data for each user |
| Dislikes/barriers to use | - Messy/Lots of writing - Non-British - Complicated/medical language - Broken links - Difficult to navigate - Advertisements |
- Increase workload - Negative impact on HP-Pt relationship - Limited reach/increasing the digital divide |
| Presentation | - Consistent format - Easy to navigate - Minimise scrolling - Pages can be printed - Up to date - Colourful - Clear, concise, accessible language - Interactive and visual (e.g. quizzes, videos, images) |
- Simple - Interactive and Visual (e.g. graphics and videos) |
| Tone | - Positive (e.g. what I can do rather than cannot do) - Encouraging and Supportive - Fun - Humorous - Professional |
- Positive - Motivating |
| Engagement | - Easy to use - Trust content (e.g. recommended by HP or recognised body) - Tailored to them - Features to enable sharing with others (e.g. forum) - Features to improve communication with HPs (summary printouts of health information in one place) - Email/Text prompts (e.g. content updates, encouragement, appointments, prescriptions) |
- Time saving - Patient led - Effective (e.g. positive outcome data such as improved glucose control, blood pressure etc.) - Incentives (e.g. fits with the Quality and Outcomes Framework) - Fits in with current practice (e.g. care planning framework). |
2.3.5. Researcher's background
Being explicit about values and beliefs is an integral part of qualitative research (Barker and Pistrang, 2005; Elliott et al., 1999) and our multi-disciplinary team (psychologists, sociologists, GPs) provided a range of perspectives in planning and conducting the research as well as informing analytic discussions.
2.4. Process of synthesis
We synthesised the data using an iterative participatory design approach with 3 main steps: mapping and writing; integrating; and revising. This approach was chosen as research has shown that interventions developed using participatory design are more likely to be acceptable, are more likely to be engaging (e.g. lower attrition) and are more likely to be effective (DeSmet et al., 2016).
2.4.1. Mapping & writing
A core interdisciplinary writing team consisting of 2 psychologists (CD, JR), 3 general practitioners (EM, KP, EG) and 3 dieticians mapped the information to be covered on to initial intervention components (see Table 3). Components were then written by team members according to areas of expertise and experience. This content was then reviewed and agreed upon with the rest of the team. All content was evidence-based, in that it reflected current best practice (represented by the National Institute for Health and Care Excellence (NICE) clinical guidelines) (National Institute of Health and Care Excellence (NICE) Guideline NG28, 2015), and current evidence on factors like maximising accessibility to people with low literacy skills or low vision.
2.4.2. Integrating
We worked with software engineers and a web designer to integrate the written content onto a website. This ensured that content was presented in a user friendly way that was easy to navigate with a professional finish. The software engineers were able to integrate the functionality of the interactive components (e.g. forum, quizzes, self-assessments, action planning, goal setting, reviewing & feedback on goals, reminders, integrating videos and previously developed digital interventions) so that the content could be tailored to individual users.
2.4.3. Revising
Iterations of the integrated content were shown and tested by two complementary participatory design groups: one of HCPs (GPs, practice and diabetes specialist nurses) and one of people with T2DM.
The Health Care Professional (HCPs) group had four sessions where they focused on ensuring that the content was accurate, evidence-based and consistent with NICE guidelines and best clinical practice; the programme could be used in routine care; likely to be acceptable to HCPs; and whether anything was missing or could be improved.
The T2DM participatory design group was made up of a number of people with T2DM who regularly used the website at home and in sessions with the research team and were heavily involved in providing feedback on all the content created. Feedback included whether it met their needs, how it was presented, the design and name of the website and creating or suggesting new content. This on-going involvement meant that users shaped whole additional components of the website. For example, for the physical activity components of the website, users suggested that videos demonstrating how to perform a range of physical activities would be useful as there was some uncertainty about what to do. Users were also clear that it was important that the people doing the activities in these videos were real people with T2DM (rather than what one user called “lycra lovelies” with a range of abilities (Beginners & reduced mobility, Intermediate, Advanced)). Based on this feedback we worked with a film director, personal trainer and three people with T2DM to make a range of physical activity videos. These were integrated within the website by our software engineers and reviewed by our users again. In this second iteration of feedback users suggested some sort of playlist function so that different physical activity videos could be viewed as a circuit. We worked with the software engineers to integrate these suggestions on the website. Users were asked to confirm whether the changes and integrations had been made in line with their suggestions.
Additional feedback was given on the pre-existing interventions Down Your Drink and Living Life To The Full that were incorporated into HeLP-Diabetes (see Results section) in order to tailor the existing content to people with T2DM. For example, information was added to Down Your Drink about the effects of alcohol on blood glucose levels. Diabetes-related behaviours that may cause stress (e.g. taking medicines as prescribed, eating out) were added to the Living Life to the Full audios.
The regular website users participatory design group met on eight sessions which were facilitated by CD and JR. In-between each session the core writing team met to discuss suggestions and where feasible implement them. If changes were not made the reasons for these were explained to the group at the next session (e.g. the group's suggestion to encourage website users to monitor their blood glucose levels would conflict with current evidence based recommendations from NICE (National Institute of Health and Care Excellence (NICE) Guideline NG28, 2015) on blood glucose monitoring for people with T2DM). Additionally, two separate groups of people with T2DM who only occasionally used the website met less regularly (four sessions per group) in order to provide insight from a new user's point of view.
2.5. Additional feedback and usability testing
A multidisciplinary steering group (e.g. psychologists, medical sociologists, patient representatives, GPs, diabetes consultants, cardiologists, primary care specialists) also reviewed and commented on the intervention content and usability. In addition, a number of naïve users with no experience of the intervention took part in usability testing sessions where they had to carry out a series of pre-defined tasks and ‘think aloud’ while completing them (e.g. where would you go to find out about diabetes and holidays?) This allowed the web designer to optimise the navigation, look and feel of the intervention and improve the usability of the interactive features (e.g. quizzes, self-assessments, action planning, goal setting, feedback etc.). Thorough proofreading and editing were essential for credibility and maintaining users' trust in the intervention (Kerr et al., 2006). A professional editor reviewed and edited all content for any errors in writing.
2.6. Facilitating engagement
Data from our qualitative work with both users emphasised the importance of ensuring that the intervention was used in interactions with HCPs, and was perceived as an integral part of the total care package, not an optional add-on. We therefore developed a 5–10 min registration and facilitation process where a health care professional (e.g. usually a practice or research nurse or health care assistant) registered a user, introduced users briefly to each of the sections of the intervention and went into detail around one area that the user wanted to work on (e.g. losing weight, or understanding medication). A step-by-step booklet was produced for HCPs so that they could easily navigate the intervention without prior experience. In addition a patient user activity booklet was developed with some details of where to find commonly requested information and activities to do using the interactive tools (e.g. goal setting, action planning, setting a prompt). These were developed by CD and JR and reviewed by the core team and participatory design groups.
Engagement was also encouraged through regular emails and/or texts (Alkhaldi et al., 2017) that contained links to topical content within the intervention (e.g. information around flu vaccinations in winter). The content of these was suggested by our participatory design groups and then written by the team. They were reviewed by the participatory design group for acceptability and then sent to all registered users.
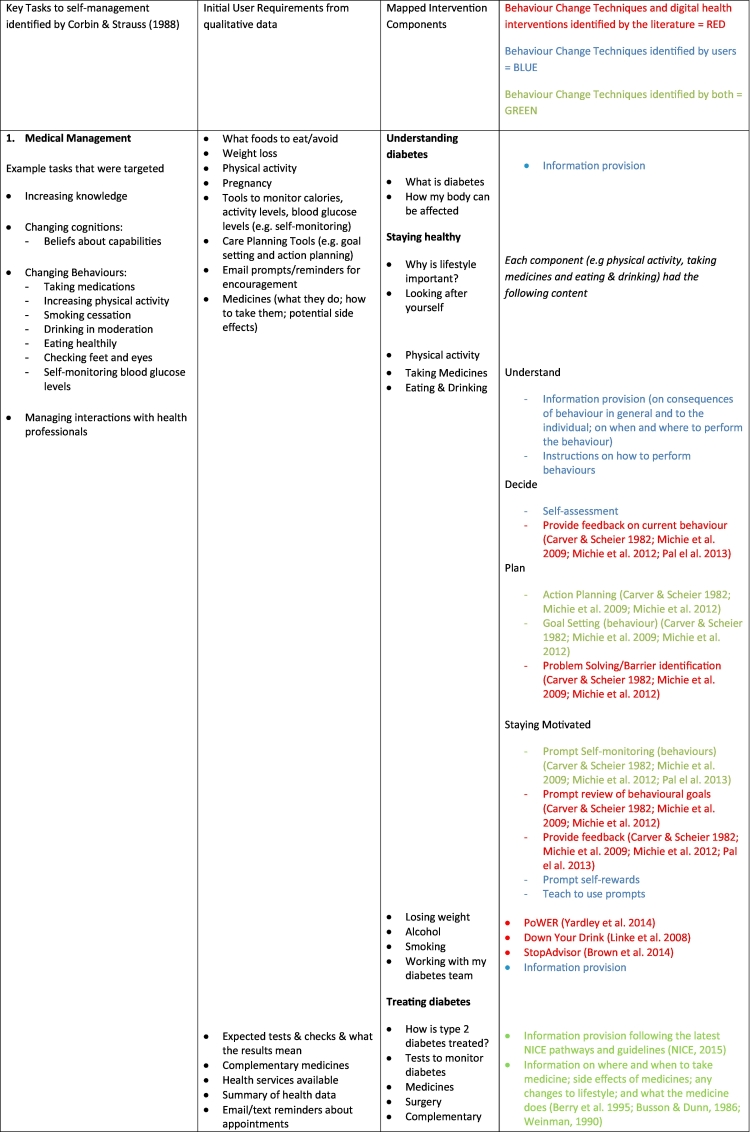
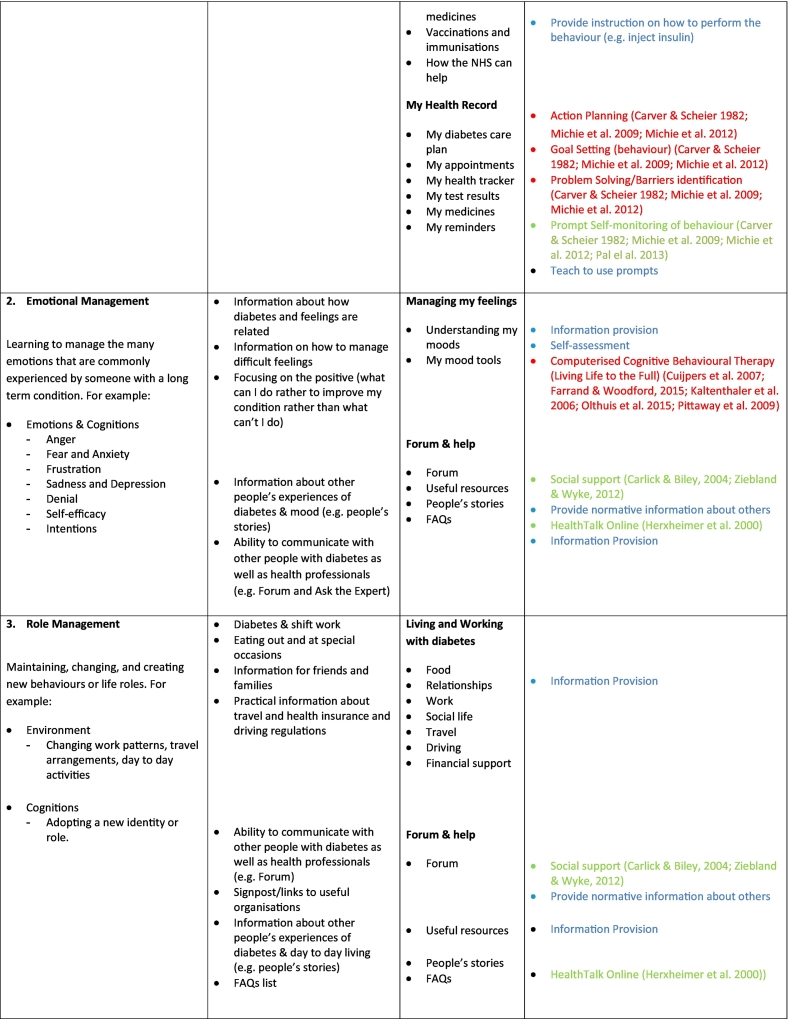
3. Results
The primary qualitative data on user requirements is summarised in Table 3, Table 4. Table 4 shows how the primary qualitative data were mapped onto Corbin & Strauss' model of self-management. Using Normalisation Process Theory allowed us to identify intervention features that were needed to improve the chances of engagement and normalisation of the intervention. Integrating the results of the analyses of the qualitative data with the Corbin and Strauss model enabled us to generate an overall list of required components to be included within the intervention (see column 3 of Table 4). We then reviewed the existing research evidence in terms of empirical papers, systematic reviews and clinical guidelines to identify best practice, strategies and interventions that have been shown to be effective at targeting these components.
Table 4.
How theory, qualitative data from target users, and evidence-based techniques or strategies were mapped on to HeLP-Diabetes overall components.
As Table 4 makes clear, the final intervention required a great deal of content. We wanted to avoid duplicating efforts already made by leading researchers in the field of digital health interventions, and therefore decided that where there were existing interventions that could be usefully and easily incorporated into our intervention, we would do so. We developed criteria to guide selection of existing interventions which were: that they were readily available to the research team (i.e. we already knew about them, or they were easily located through literature searches and we could easily negotiate permission to license their content); developed using theory and user input (as this reflected best practice); had been evaluated and had some evidence of effectiveness; and could be easily incorporated into our intervention (this included technical compatibility, being in English, and having a tone and approach to self-management that reflected the ethos of the main intervention). External content that was licensed in is described in the relevant sections below.
3.1. Medicine and treatments
NICE guidelines and pathways were reviewed to provide the content for the current medications and treatments for people with T2DM (National Institute of Health and Care Excellence (NICE) Guideline NG28, 2015). Patients value being given written information about the medicines they have been prescribed (Busson and Dunn, 1986; Weinman, 1990), and in particular the answers to the questions: What are the side effects? What does the medicine do? What lifestyle changes are involved in taking the medicines (e.g. Can I still drive? Can I drink alcohol?); and How do I take the medicine (e.g. When, how much, with food or on an empty stomach?) (Berry et al., 1995). This guided the information that needed to be written in the intervention. How medicines information was presented followed recommendations for risk communication (e.g. presenting data using absolute risk reduction and frequencies rather than percentages) (Gigerenzer and Edwards, 2003).
3.2. Changing behaviour
From the combined qualitative data and theory described above we identified a number of behaviours which people with T2DM may need to modify in order to successfully self-manage their condition. These included: dietary intake, weight management, levels of physical activity, alcohol consumption, smoking and taking medications. We identified three pre-existing behaviour change interventions that met our criteria for inclusion in our intervention: 1) Down Your Drink (DYD), a digital intervention that aimed to help hazardous and harmful drinkers to reduce their alcohol consumption (Linke et al., 2008; Wallace et al., 2011), 2) PoWER, which targeted weight loss (Yardley et al., 2014) and 3) StopAdvisor, a digital smoking cessation intervention (Brown et al., 2014).
We were unable to identify digital behaviour change interventions, which met our criteria for eating healthily, being more physically active and taking medicines as prescribed so we designed our own. To do this, we selected appropriate behaviour change techniques using Abraham and Michie's taxonomy (Abraham and Michie, 2008), which have been shown to be effective in previous research. Goal setting (behaviour); Action planning; Prompt review of behavioural goals; Barrier identification/Problem solving; Prompt self-monitoring of behaviour and Provide feedback on performance were chosen as this cluster of techniques have been found to be associated with positive outcomes of previous behaviour change interventions (Michie et al., 2009b; Michie et al., 2012) and are consistent with Self-regulation (control) Theory (Carver and Scheier, 1982). Prompt self-monitoring of behaviour and Provide feedback on performance were also the most commonly used techniques in digital health interventions that had an impact on glucose control (Pal et al., 2013).
3.3. Changing affect
Corbin and Strauss' model (Corbin and Strauss, 1988) suggests that managing the many strong negative emotions (e.g. anxiety depression, anger, guilt, stigma and shame) that are associated with having a long-term condition are key determinants to good self-management. This was also confirmed in the focus group data with both people with T2DM and HCPs stressing the emotional impact caused by T2DM. Research evidence has also found high levels of depression and diabetes-related distress for people with diabetes (Nicolucci et al., 2013). We reviewed the literature and found the evidence for internet Cognitive Behaviour Therapy (CBT) for managing depression, anxiety and a range of other mental health problems was strong (Kaltenthaler et al., 2006; Cuijpers et al., 2007; Olthuis et al., 2015; Farrand and Woodford, 2015) and likely to be effective in helping our users to manage their emotions. Rather than develop our own content, we searched for existing digital interventions that had been shown to be effective in reducing mild to moderate anxiety and depression. Living Life to the Full (LLTTF) was chosen as it met our criteria of availability, evidence of effectiveness, and fitting with the overall approach of our intervention (Pittaway et al., 2009). It mapped onto our user requirements better than alternative digital interventions (e.g. Beating the Blues) in that it was UK centric and the approach taken is informed by CBT to give people the skills to manage low mood and stress, rather than treat clinical depression or anxiety.
3.4. Improving perceived social support
The data from our users identified that hearing or reading about other people's experiences and responses to similar challenges (e.g. the diagnosis) could be useful in managing their emotions. This view was supported by the research evidence where hearing or reading about other people's stories has the potential to improve a person's sense of social support and how they cope with some of the emotions related to illness (Carlick and Biley, 2004; Ziebland and Wyke, 2012) in addition to providing information that may impact decisions about self-management. Moreover, there is increasing evidence supporting the use of narrative as a form of communication, as it can facilitate information processing (particularly by people with low literacy, and/or low health literacy (Wise et al., 2008)) and address emotional and existential issues (Kreuter et al., 2007; Hinyard and Kreuter, 2007). Rather than create our own range of people's stories we approached the world leader in provision of such “personal stories” called HealthTalk Online (HTO) (previously DiPEX; (Herxheimer et al., 2000)) to incorporate their module of patient experiences for T2DM. This included 40 videos and transcripts of interviews with people from range of ethnic and socio-economic backgrounds, (as it is important that viewers can identify with the narrator (Slater et al., 2003)). The interviews were carefully curated to present a balanced and comprehensive overview of patient experiences.
In addition to the HTO personal stories, we included a moderated forum, as users requested this as a means of sharing their thoughts and emotions with others. There was also evidence supporting this suggesting that forums can have impact on a person's sense of social support as well as providing experiential knowledge on how to cope with conditions and stressful situations (Kummervold et al., 2002). There is also an emerging literature of importance of identifying the various ‘systems of support’ that are available to individuals (Rogers et al., 2011). A moderated forum provides a means of expanding users' social network. We appreciated that not all users would want to use the forum, so it was available but with no compulsion to use it. Alongside this, we wanted to provide users with tailored information about the local resources available to them in their location in terms of health care professionals, non-health care professionals and voluntary and community groups.
3.5. Changes in role and identity
Corbin and Strauss' model (Corbin and Strauss, 1988) emphasises the work of managing biographical disruption (changes to their and roles) caused by a diagnosis of T2DM. This was confirmed in our primary data with users describing this disruption as a feeling of loss (Pal et al., 2018). Users were particularly interested in content that would enable them to continue with actions that had previously been “taken for granted”, such as social occasions, holidays, travel, insurance, eating in restaurants, cafes or work canteens, and variable working hours, such as with shift work. Users wanted tools to help manage changes to roles within relationships and families. We could find little evidence on the effectiveness of interventions addressing these issues, and so were mainly guided by our user data. The resulting content included acknowledgement that the diagnosis of diabetes can be life-changing, that some previously routine activities and relationships can become challenging, and providing information on how to manage them. This information ranged from practical advice about managing medication and diet when working shifts, to resources around employment law. Users identified again that hearing other people's experience about living and working with T2DM may be useful to realise they are not alone in experiencing these problems and to feel supported. The HTO videos described above included how other people had felt and their methods of managing these challenges (e.g. sexual problems, medication side effects). We also envisaged the forum as a place where users could exchange information about specific practical challenges (Kummervold et al., 2002).
3.6. Presentation of information
We took a patient centred approach to presenting information, in a positive (e.g. what I can do rather than cannot do), non-judgemental way in order to empower, motivate and increase confidence. We followed the best practice guidance from the Royal National Institute of Blind People (RNIB) to ensure the website was accessible for people with visual impairments and available checklists for the content to be included in patient information materials (Coulter et al., 1999). We used a range of modes to communicate information (e.g. written, pictures, videos) in order to suit a range of user preferences.
3.7. Final intervention
The above steps determined the components of the intervention and how this information should be presented. The final intervention was (and is) a very large website, with over 560 pages.
3.7.1. Content
The overall content was broken down into eight sections:
-
1.
Understanding diabetes (145 pages; information about the nature and causes of diabetes, and how it affects the body);
-
2.
Staying healthy (107 pages; motivational material about how to maintain optimal physical and emotional health and the importance of self-management; new behaviour change modules and previously validated programmes for diet, weight loss, physical activity, smoking cessation, moderating alcohol intake, and taking medicines);
-
3.
Treating diabetes (70 pages; information about medications used in diabetes, including information about indications, side effects and monitoring; importance of managing cardiovascular risk factors as well as glycaemic levels; importance of regular monitoring to prevent retinopathy, neuropathy and nephropathy; and types and roles of different HCPs in caring for people with diabetes);
-
4.
Living and working with diabetes (87 pages; focus on managing social and work situations, such as shift work, parties, or holidays; impact on relationships, including sexual relationships; and possible impact on emotions and feelings of self-worth);
-
5.
Managing my feelings (61 pages; self-assessment tools for identifying low mood; CBT modules; mindfulness-based approaches);
-
6.
My health record (45 pages; opportunity to record appointments with HCPs and results of tests or self-monitoring, with opportunities for graphical displays and feedback);
-
7.
News and research (16 pages; updates about diabetes treatment, in-depth articles about seminal research papers); and information for HCPs such as NICE guidelines;
-
8.
Forum and help (28 pages; moderated forum; videos of personal stories about diabetes used with license from healthtalk.org; additional resources, including local resources tailored to the CCG).
Each section combined written information with videos and other graphics. There were interactive and tailored components in each section apart from news and research. Behaviour change and emotional management sections included opportunities for self-assessment, in the form of validated questionnaires with automated feedback which contained recommendations for action. Users could set the programme to send them automated texts or email reminders and alerts when new entries were posted in the forum. They could opt out of the regular engagement emails and newsletters described above.
More details of the website's content, with screen shots, are provided in Appendix 1, with a site map in Appendix 2. The TIDIER check list forms Appendix 3.
4. Discussion and implications
4.1. Main findings
We have described the different sources (e.g. theory, research evidence, primary data from users, clinical guidelines) that guided the content and presentation of HeLP-Diabetes and our methods of combining them using participatory design. The intervention has been evaluated and found to improve diabetes control but not diabetes-related distress (Murray et al., 2015; Murray et al., 2017), to be highly cost-effective with users having better health outcomes and reduced health care costs (Li et al., 2018) and implemented in general practices across the UK where it has been shown to be used by a wide demographic (Ross et al., 2018; Poduval et al., 2018). Over half our users are from Black and Minority Ethnic (BME) backgrounds, a third left school at minimum school leaving age with either no, or minimal qualifications, and a third described their computer skills as “basic”. This combination of effectiveness, cost-effectiveness, use by a wide demographic, and subsequent large-scale implementation is unique amongst digital diabetes self-management programmes. We hope by describing the content and development other researchers will be able build in future research so that science is cumulative. This is particularly important in the field of digital health interventions for self-management where the development and content of such interventions is rarely described in detail making it difficult for other researchers and practitioners to know how to start the development process (Michie et al., 2009a). We hope that by reporting the process we used this may act as an exemplar for other researchers or clinicians wanting to develop self-management interventions for other long-term conditions in the future.
4.2. Strengths & limitations
Particular strengths of our approach to intervention development included using participatory design methods, where prospective users worked with us as partners to determine the content and design. The explicit use of theory was also essential, with the Corbin and Strauss model (Corbin and Strauss, 1988) providing an overarching guide to content, the Abraham and Michie behaviour change technique taxonomy (Abraham and Michie, 2008) guiding specific content around behaviour change, and NPT (May and Finch, 2009) ensuring we thought about implementation at every step of the process. Having a diverse multi-disciplinary team which included health psychologists, sociologists, clinicians, information scientists, software engineers, web-designers and editors was beneficial. The use of evidence from a wide range of disciplines, such as human-computer interaction and health education as well as the more traditional biomedical literature was a strength.
There were also some limitations to our work. In hindsight, the research team could have included human-computer interaction (HCI) expertise, rather than relying on commercial software and web design partners. Such expertise may have helped us with our participatory design and user testing methods, and helped us communicate with our commercial partners. Our emphasis on participatory design meant that, almost by definition, our patient partners were those most interested in self-management, and hence not representative of patients for whom self-management is a lower priority. Our selection and combination of theoretical models can be criticised; however, we found that they were fit for purpose and were easily combined, and would recommend this combination for future similar projects. Finally, there is no doubt that the process initial development was long (two years) and expensive. This can only be justified where there is a large potential population who can benefit from the intervention, or where there is significant learning which can be applied to help future clinical and academic development. Both factors apply in this case.
4.3. Conclusion
It is possible to use participatory design principles to integrate theory and evidence to create acceptable and effective digital health interventions.
The following are the supplementary data related to this article.
Description of the intervention.
Sitemap of HeLP-Diabetes.
TiDIER CHECKLIST.
Funding
This paper presents independent research supported by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research Programme (grant reference number RP-PG-0609-10135). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. AF is an NIHR Senior Investigator and receives funding from Oxford NIHR Biomedical Research Centre.
Competing interest
EM is the managing director of a not-for-profit community interest company established to disseminate HeLP-Diabetes across the NHS.
Human rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Welfare of animals
This article does not contain any studies with animals performed by any of the authors.
Acknowledgments
We are grateful to Orla O'Donnell for outstanding project management, and all the health professionals and people with type 2 diabetes who contributed to the development of HeLP-Diabetes.
References
- Abraham C., Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol. 2008;27(3):379–387. doi: 10.1037/0278-6133.27.3.379. (May 2008) [DOI] [PubMed] [Google Scholar]
- Alkhaldi G., Modrow K., Hamilton F., Pal K., Ross J., Murray E. Promoting engagement with a digital health intervention (HeLP-Diabetes) using email and text message prompts: mixed-methods study. Interact. J. Med. Res. 2017;6(2) doi: 10.2196/ijmr.6952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Diabetes Association 4. Foundations of care: education, nutrition, physical activity, smoking cessation, psychosocial care, and immunization. Diabetes Care. 2015;38(Supplement 1):S20–S30. doi: 10.2337/dc15-S007. [DOI] [PubMed] [Google Scholar]
- Armitage C., Conner M. Social cognition models and health behaviour: a structured review. Psychol. Health. 2000;15(2):173–189. [Google Scholar]
- Barker V., Pistrang N. Quality criteria under methodological pluralism: implications for conducting and evaluating research. Am. J. Community Psychol. 2005;35(3–4):201–212. doi: 10.1007/s10464-005-3398-y. [DOI] [PubMed] [Google Scholar]
- Bartholomew L.K., Parcel G.S., Kok G. Intervention mapping: a process for developing theory and evidence-based health education programs. Health Educ. Behav. 1998;25(5):545–563. doi: 10.1177/109019819802500502. [DOI] [PubMed] [Google Scholar]
- Berry D.C., Gillie T., Banbury S. What do patients want to know: an empirical approach to explanation generation and validation. Expert Syst. Appl. 1995;8:419–428. [Google Scholar]
- Berwick D.M., Nolan T.W., Whittingdon J. The triple aim: care, health and cost. Health Aff. 2008;27(3):759–769. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- Brown J., Michie S., Geraghty A.W., Yardley L., Gardner B., Shahab L., Stapleton J.A., West R. Internet-based intervention for smoking cessation (StopAdvisor) in people with low and high socioeconomic status: a randomised controlled trial. Lancet Respir. Med. 2014;2(12):997–1006. doi: 10.1016/S2213-2600(14)70195-X. [DOI] [PubMed] [Google Scholar]
- Busson M., Dunn A.P.M. Patients' knowledge about prescribed medicines. J. Pharm. 1986:624–626. [Google Scholar]
- Carlick A., Biley F.C. Thoughts on the therapeutic use of narrative in the promotion of coping in cancer care. Eur. J. Cancer Care. 2004;13(4):308–317. doi: 10.1111/j.1365-2354.2004.00466.x. [DOI] [PubMed] [Google Scholar]
- Carswell K., McCarthy O., Murray E., Bailey J.V. Integrating psychological theory into the design of an online intervention for sexual health: the Sexunzipped website. JMIR Res. Protoc. 2012;1(2) doi: 10.2196/resprot.2114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver C.S., Scheier M.E. Control theory: a useful conceptual framework for personality-social, clinical, and health psychology. Psychol. Bull. 1982;92(1):111–135. [PubMed] [Google Scholar]
- Corbin J.M., Strauss A.L. Jossey-Bass Publishers; San Francisco, CA: 1988. Unending Work and Care: Managing Chronic Illness at Home; p. 1988. [Google Scholar]
- Coulter A., Entwistle V., Gilbert D. Sharing decisions with patients: is the information good enough? Br. Med. J. 1999;318(7179):318–322. doi: 10.1136/bmj.318.7179.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig P., Dieppe P., Macintyre S., Michie S., Nazareth I., Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. Br. Med. J. 2008;337 doi: 10.1136/bmj.a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig C., Eby D., Whittington J. IHI Innovation Series White Paper. Institute for Healthcare Improvement; Cambridge, Massachusetts: 2011. Care coordination model: better care at lower cost for people with multiple health and social needs.http://www.ihi.org/resources/Pages/IHIWhitePapers/IHICareCoordinationModelWhitePaper.aspx (Accessed 27 Sept 2016) [Google Scholar]
- Cuijpers P., van Straten A., Andersson G. Internet-administered cognitive behavior therapy for health problems: a systematic review. J. Behav. Med. 2007;31(2):169–177. doi: 10.1007/s10865-007-9144-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies M.J., Heller S., Skinner T.C. Effectiveness of the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed Type 2 diabetes: cluster randomised controlled trial. Br. Med. J. 2008;336:491–495. doi: 10.1136/bmj.39474.922025.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deakin T. The diabetes pandemic: is structured education the solution or an unnecessary expense? Pract. Diabetes. 2011;28(8):1–14. [Google Scholar]
- DeSmet A., Thompson D., Baranowski T., Palmeira A., Verloigne M., De Bourdeaudhuij I. Is participatory design associated with the effectiveness of serious digital games for healthy lifestyle promotion? A meta-analysis. J. Med. Internet Res. 2016;18(4) doi: 10.2196/jmir.4444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott R., Fischer C.T., Rennie D.L. Evolving guidelines for publication of qualitative research studies in psychology and related fields. Br. J. Clin. Psychol. 1999;38(3):215–229. doi: 10.1348/014466599162782. [DOI] [PubMed] [Google Scholar]
- Eysenbach G. The law of attrition. J. Med. Internet Res. 2005;7(1) doi: 10.2196/jmir.7.1.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrand P., Woodford J. Effectiveness of cognitive behavioural self-help for the treatment of depression and anxiety in people with long-term physical health conditions: a systematic review and meta-analysis of randomised controlled trials. Ann. Behav. Med. 2015;49(4):579–593. doi: 10.1007/s12160-015-9689-0. [DOI] [PubMed] [Google Scholar]
- Gigerenzer G., Edwards A. Simple tools for understanding risks: from innumeracy to insight. Br. Med. J. 2003;327(7417):741–744. doi: 10.1136/bmj.327.7417.741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herxheimer A., McPherson A., Miller R., Shepperd S., Yaphe J., Ziebland S. Database of patients' experiences (DIPEx): a multi-media approach to sharing experiences and information. Lancet. 2000;355(9214):1540–1543. doi: 10.1016/S0140-6736(00)02174-7. [DOI] [PubMed] [Google Scholar]
- Hinyard L.J., Kreuter M.W. Using narrative communication as a tool for health behavior change: a conceptual, theoretical, and empirical overview. Health Educ. Behav. 2007;34(5):777–792. doi: 10.1177/1090198106291963. [DOI] [PubMed] [Google Scholar]
- Hoffmann T.C., Glasziou P.P., Boutron I., Milne R., Perera R., Moher D. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. Br. Med. J. 2014;348 doi: 10.1136/bmj.g1687. [DOI] [PubMed] [Google Scholar]
- Horigan G., Davies M., Findlay-White F., Chaney D., Coates V. Reasons why patients referred to diabetes education programmes choose not to attend: a systematic review. Diabet. Med. 2016;34:14–26. doi: 10.1111/dme.13120. [DOI] [PubMed] [Google Scholar]
- Kaltenthaler E., Brazier J., De Nigris E., Tumur I., Ferriter M., Beverley C., Parry G., Rooney G., Sutcliffe P. Computerised cognitive behaviour therapy for depression and anxiety update: a systematic review and economic evaluation. Health Technol. Assess. 2006;10(33) doi: 10.3310/hta10330. (iii, xi-iii,168) [DOI] [PubMed] [Google Scholar]
- Kerr C., Murray E., Stevenson F., Gore C., Nazareth I. Internet interventions for long-term conditions: patient and caregiver quality criteria. J. Med. Internet Res. 2006;8(3) doi: 10.2196/jmir.8.3.e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr C., Murray E., Noble L., Morris R., Bottomley C., Stevenson F., Patterson D., Peacock R., Turner I., Jackson K., Nazareth I. The potential of Web-based interventions for heart disease self-management: a mixed methods investigation. J. Med. Internet Res. 2010;12(4) doi: 10.2196/jmir.1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khunti K., Gray L.J., Skinner T.C. Effectiveness of a diabetes education and self management programme (DESMOND) for people with newly diagnosed Type 2 diabetes mellitus: three year follow-up of a cluster randomised controlled trial in primary care. Br. Med. J. 2012;344 doi: 10.1136/bmj.e2333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitzinger J. Qualitative research: introducing focus groups. Br. Med. J. 1995;311:299. doi: 10.1136/bmj.311.7000.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreuter M.W., Green M.C., Cappella J.N., Slater M.D., Wise M.E., Storey D., Clark E.M., O'Keefe D.J., Erwin D.O., Holmes K., Hinyard L.J., Houston T., Woolley S. Narrative communication in cancer prevention and control: a framework to guide research and application. Ann. Behav. Med. 2007;33(3):221–235. doi: 10.1007/BF02879904. [DOI] [PubMed] [Google Scholar]
- Kummervold P.E., Gammon D., Bergvik S., Johnsen J.A., Hasvold T., Rosenvinge J.H. Social support in a wired world: use of online mental health forums in Norway. Nord. J. Psychiatry. 2002;56(1):59–65. doi: 10.1080/08039480252803945. [DOI] [PubMed] [Google Scholar]
- Kushniruk A., Nohr C. Participatory design, user involvement and health IT evaluation. Stud. Health Technol. Inform. 2016;222:139–151. [PubMed] [Google Scholar]
- Li J., Parrott S., Sweeting M., Farmer A., Ross J., Dack C., Pal K., Yardley L., Barnard M., Hudda M., Alkhaldi G., Murray E. Cost-effectiveness of facilitated access to a self-management website, compared to usual care, for patients with type 2 diabetes (HeLP-Diabetes): randomized controlled trial. J. Med. Internet Res. 2018;20(6) doi: 10.2196/jmir.9256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linke S., McCambridge J., Khadjesari Z., Wallace P., Murray E. Development of a psychologically enhanced interactive online intervention for hazardous drinking. Alcohol Alcohol. 2008;43(6):669–674. doi: 10.1093/alcalc/agn066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May C., Finch T. Implementation, embedding, and integration: an outline of Normalization Process Theory. Sociology. 2009;43(3):535–554. [Google Scholar]
- May C.R., Cummings A., Girling M., Bracher M., Mair F.S., May C.M., Murray E., Myall M., Rapley T., Finch T. Using Normalization Process Theory in feasibility studies and process evaluations of complex healthcare interventions: a systematic review. Implement. Sci. 2018;13(1):80. doi: 10.1186/s13012-018-0758-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy O., Carswell K., Murray E., Free C., Stevenson F., Bailey J.V. What young people want from a sexual health website: design and development of Sexunzipped. J. Med. Internet Res. 2012;14(5) doi: 10.2196/jmir.2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S., Fixsen D., Grimshaw J.M., Eccles M.P. Specifying and reporting complex behaviour change interventions: the need for a scientific method. Implement. Sci. 2009;4:40. doi: 10.1186/1748-5908-4-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S., Abraham C., Whittington C., McAteer J., Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009;28(6):690–701. doi: 10.1037/a0016136. [DOI] [PubMed] [Google Scholar]
- Michie S., Whittington C., Hamoudi Z., Zarnani F., Tober G., West R. Identification of behaviour change techniques to reduce excessive alcohol consumption. Addiction. 2012;107:1431–1440. doi: 10.1111/j.1360-0443.2012.03845.x. [DOI] [PubMed] [Google Scholar]
- Murray E., Dack C., Barnard M. HeLP-Diabetes: randomised controlled trial protocol. BMC Health Serv. Res. 2015;15:578. doi: 10.1186/s12913-015-1246-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray E., Hekler E.B., Andersson G., Collins L.M., Doherty A., Hollis C., Rivera D.E., West R., Wyatt J.C. Evaluating digital health interventions: key questions and approaches. Am. J. Prev. Med. 2016;51(5):843–851. doi: 10.1016/j.amepre.2016.06.008. (2016 Nov) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray E., Sweeting M., Dack C., Pal K., Modrow K., Hudda M., Li J., Ross J., Alkhaldi G., Barnard M., Farmer A., Michie S., Yardley L., May C., Parrott S., Stevenson F., Knox M., Patterson D. Web-based self-management support for people with type 2 diabetes (HeLP-Diabetes): randomised controlled trial in English primary care. Br. Med. J. Open. 2017;7 doi: 10.1136/bmjopen-2017-016009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray E., Ross J., Pal K., Li J., Dack C., Stevenson F., Sweeting M., Parrott S., Barnard M., Yardley L., Michie S., May C., Patterson D., Alkhaldi G., Fisher B., Farmer A., O'Donnell O. A web-based self-management programme for people with type 2 diabetes: the HeLP-Diabetes research programme including RCT. NIHR Program. Grants Appl. Res. 2018;06(05) [PubMed] [Google Scholar]
- National Collaborating Centre for Chronic Conditions . Royal College of Physicians; London: 2008. Type 2 Diabetes: National Clinical Guideline for Management in Primary and Secondary Care (Update) [PubMed] [Google Scholar]
- National Diabetes Audit National Diabetes Audit 2016–2017: care processes and treatment targets. 2018. https://www.hqip.org.uk/wp-content/uploads/2018/03/National-Diabetes-Audit-2016-17-Report-1-Care-Processes-and-Treatment-T....pdf Available from: (Accessed on February 1st, 2019)
- National Institute of Health and Care Excellence (NICE) Guideline NG28 Type 2 diabetes in adults: management. 2015. https://www.nice.org.uk/guidance/ng28 [PubMed]
- NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4·4 million participants. Lancet. 2016;387(10027):1513–1530. doi: 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolucci A., Kovacs Burns K., Holt R.I.G., Comaschi M., Hermanns N., Ishii H., Kokoszka A., Pouwer F., Skovlund S.E., Stuckey H., Tarkun I., Vallis M., Wens J., Peyrot M., the DAWN2 Study Group Diabetes attitudes, wishes and needs second study (DAWN2™): cross-national benchmarking of diabetes-related psychosocial outcomes for people with diabetes. Diabet. Med. 2013;30:767–777. doi: 10.1111/dme.12245. [DOI] [PubMed] [Google Scholar]
- Nobis S., Lehr D., Ebert D.D., Baumeister H., Snoek F., Riper H., Berking M. Efficacy of a web-based intervention with mobile phone support in treating depressive symptoms in adults with type 1 and type 2 diabetes: a randomized controlled trial. Diabetes Care. 2015;38(5):776–783. doi: 10.2337/dc14-1728. [DOI] [PubMed] [Google Scholar]
- Olthuis J.V., Watt M.C., Bailey K., Hayden J.A., Stewart S.H. Therapist-supported Internet cognitive behavioural therapy for anxiety disorders in adults. Cochrane Database Syst. Rev. 2015;5(3) doi: 10.1002/14651858.CD011565. [DOI] [PubMed] [Google Scholar]
- Pal K., Eastwood S.V., Michie M., Farmer A.J., Barnard M.L., Peacock R., Wood B., Innis J.D., Murray E. Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. Cochrane Database Syst. Rev. 2013;(3) doi: 10.1002/14651858.CD008776.pub2. (Mar 28) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pal K., Dack C., Ross J., Michie S., May C., Stevenson F., Farmer A., Yardley L., Barnard M., Murray E. Digital health interventions for adults with type 2 diabetes: qualitative study of patient perspectives on diabetes self-management education and support. J. Med. Internet Res. 2018;20(2) doi: 10.2196/jmir.8439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pittaway S., Cupitt C., Palmer D., Arowobusoye N., Milne R., Holttum S., Pezet R., Patrick H. Comparative, clinical feasibility study of three tools for delivery of cognitive behavioural therapy for mild to moderate depression and anxiety provided on a self-help basis. Ment Health Fam Med. 2009;6(3):145–154. [PMC free article] [PubMed] [Google Scholar]
- Poduval S., Ahmed S., Marston L., Hamilton F., Murray E. Crossing the digital divide in online self-management support: analysis of usage data from HeLP-Diabetes. J. Med. Internet Res. Diabetes. 2018;3(4) doi: 10.2196/10925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers A., Vassilev I., Sanders C., Kirk S., Chew-Graham C., Kennedy A., Protheroe J., Bower P., Blickem C., Reeves D., Kapadia D., Brooks H., Fullwood C., Richardson G. Social networks, work and network-based resources for the management of long-term conditions: a framework and study protocol for developing self-care support. Implement. Sci. 2011;6:56. doi: 10.1186/1748-5908-6-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross J., Stevenson F., Dack C., Pal K., May C., Michie S., Barnard M., Murray E. Developing an implementation strategy for a digital health intervention: an example in routine healthcare. BMC Health Serv. Res. 2018;18(1):794. doi: 10.1186/s12913-018-3615-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slater M.D., Buller D.B., Waters E., Archibeque M., LeBlanc M. A test of conversational and testimonial messages versus didactic presentations of nutrition information. J. Nutr. Educ. Behav. 2003;35(5):255–259. doi: 10.1016/s1499-4046(06)60056-0. [DOI] [PubMed] [Google Scholar]
- Steinsbekk A., Rygg L.O., Lisulo M. Group based diabetes self-management education compared to routine treatment for people with Type 2 diabetes mellitus. A systematic review with meta-analysis. BMC Health Serv. Res. 2012;12:213. doi: 10.1186/1472-6963-12-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stratton I.M., Adler A.I., Neil H.A. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. Br. Med. J. (Clin. Res. Ed.) 2000;321(7258):405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Bastelaar K.M., Pouwer F., Cuijpers P., Riper H., Snoek F.J. Web-based depression treatment for type 1 and type 2 diabetic patients: a randomized, controlled trial. Diabetes Care. 2011;34(2):320–325. doi: 10.2337/dc10-1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viswanath K., Kreuter M.W. Health disparities, communication inequalities, and e-health: a commentary. Am. J. Prev. Med. 2007;32(5 Suppl):S131–S133. doi: 10.1016/j.amepre.2007.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wachter R.M. Making IT Work: harnessing the power of health information technology to improve care in England. Report of the National Advisory Group on Health Information Technology in England. 2015. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/550866/Wachter_Review_Accessible.pdf (Accessed 27 Sept 2016)
- Wallace P., Murray E., McCambridge J., Khadjesari Z., White I.R., Thompson S.G., Kalaitzaki E., Godfrey C., Linke S. On-line randomized controlled trial of an internet based psychologically enhanced intervention for people with hazardous alcohol consumption. PLoS ONE. 2011;6(3) doi: 10.1371/journal.pone.0014740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinman J. Providing written information for patients: psychological considerations. J. R. Soc. Med. 1990;83:303–305. doi: 10.1177/014107689008300508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkley K., Evwierhoma C., Amiel S.A., Lempp H.K., Ismail K., Forbes A. Patient explanations for non-attendance at structured diabetes education sessions for newly diagnosed Type 2 diabetes: a qualitative study. Diabet. Med. 2015;32(1):120–128. doi: 10.1111/dme.12556. [DOI] [PubMed] [Google Scholar]
- Wise M., Han J.Y., Shaw B., McTavish F., Gustafson D.H. Effects of using online narrative and didactic information on healthcare participation for breast cancer patients. Patient Educ. Couns. 2008;70(3):348–356. doi: 10.1016/j.pec.2007.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yardley L., Ware L.J., Smith E.R., Williams S., Bradbury K.J., Arden-Close E.J., Mullee M.A., Moore M.V., Peacock J.L., Lean M.E., Margetts B.M., Byrne C.D., Hobbs R.F., Little P. Randomised controlled feasibility trial of a web-based weight management intervention with nurse support for obese patients in primary care. Int. Behav. Nutr. Phys. Act. 2014;11:67. doi: 10.1186/1479-5868-11-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziebland S., Wyke S. Health and illness in a connected world: how might sharing experiences on the internet affect people's health? Milbank Q. 2012;90(2):219–249. doi: 10.1111/j.1468-0009.2012.00662.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of the intervention.
Sitemap of HeLP-Diabetes.
TiDIER CHECKLIST.