Abstract
The migration of working-aged men from Mexico to the United States fractures the family-centered support structures typical of Latin America and contributes to high levels of depression in women left behind in migratory sending communities in Mexico. Mujeres en Solidaridad Apoyandose (MESA) was developed to improve depression in women through social support in a resource poor setting. MESA is a promotora intervention that trains women in the community to lead social support groups over a five-week period. The MESA curriculum uses a combination of cognitive behavioral theory (CBT) techniques, psychoeducation, and social support activities aimed at alleviating or preventing depression in women. Results from this pilot efficacy study (n=39) show that depressed participants at baseline experienced declines in depression as measured by the CES-D at follow-up. Other findings demonstrate the complexity behind addressing social support and depression for women impacted by migration in different ways.
Keywords: Promotoras, Women, Depression, Intervention, Social Support, Mexico
BACKGROUND
Approximately 11.7 million Mexican immigrants live in the US, representing 29% of the US foreign-born population and 10.4% of the Mexican population.(1,2) While Mexican migrants to the US constitute a substantial population, their families who remain behind constitute an even larger proportion of the population.(2) While numerous studies have focused on the mental health of Mexican immigrants in the US (3–5) and offered strategies for the prevention and treatment of depression in this group,(6,7) considerably less attention has been directed towards how migration affects family members left behind in Mexico.
In Mexico, depression disproportionately impacts women (8) and particularly women either living in rural areas (9–11) or those affected by international migration.(12–14) When working-aged men migrate to the US, the women left behind must adjust to family reorganization, new roles, and decreased social support.(15) This erosion of support has mental health implications for these women since depression is associated with less social support, less close relationships, and smaller social networks.(16,17) Family separation experienced by women with migrant spouses or children is associated with depressive symptoms.(18) Perhaps most dramatically, Mexicans with a family member in the US were found to be at a higher risk for suicidal ideation and suicide attempts than Mexicans who have never migrated or did not have family in the US.(19)
Promotoras or lay health advisors represent a strategy to address the health of Mexican immigrant women in the US.(20) This approach is based on the theoretical framework of lay-health advocacy to promote health education for populations with limited access to health care.(21–23) Promotoras are considered effective in Latino communities since they have a thorough knowledge of community social networks, cultural values, and health needs and are able to communicate in a language that recognizes these attributes of their local communities.(24) Studies have shown that lay health advisors are seen as role models and provide social support for positive behaviors within their communities.(25,26) While promotoras have been used to address depression in Latinas in the US (27) and other health issues in Mexico, (28) we could not find examples of using promotoras to improve mental health in women in rural Mexico. Whether lay health advisor programs designed for Latina immigrants in the US can be adapted and successfully implemented in rural communities in Mexico remains an open question.
This paper describes a pilot efficacy study for a promotora intervention focused on improving depression in women through social support in a migratory sending community in Mexico. We named this intervention Mujeres en Solidaridad Apoyandose (MESA), which translates to Women in Solidarity and Support. MESA (table in Spanish) connotes women coming together at a table to cope with the emotional hardships associated with family migration by providing each other social support. MESA was modeled after a promotora intervention focused on mental health in Latina immigrants in the US named ALMA (29) and uses a combination of cognitive behavioral theory (CBT) techniques, psychoeducation, and social support activities for alleviating depression in women.
METHODS
Research setting
MESA was conducted in Santa Cruz de Juventino Rosas, Guanajuato, which is referred to as Juventino Rosas in short. Guanajuato has the largest share of international migrants among all states in Mexico(30) and the largest proportion of Mexican immigrants who relocate to central North Carolina.(31) The municipality of Juventino Rosas has a population of 79,214 with nearly 40% living in rural areas.(2) More than 16% of all households and 25% of rural households are impacted by international migration.(11) This setting was chosen due to a long-standing relationship between the University of North Carolina at Chapel Hill (UNC-CH) and local community leaders. Observing the lack of access to mental health services, local leaders expressed the need to address depression among the local population.
Intervention design
This pilot efficacy study was conducted among a convenience sample of women in Juventino Rosas during summer 2011. It tested a promotora-based intervention targeting depression developed through an iterative process during 2010 (Clark, unpublished manuscript). Employing a train-the-trainer model, the MESA intervention is designed to train lay persons to serve as promotoras to lead five weekly group sessions focused on alleviating depression through social support, mental health education, and coping techniques. The promotoras were trained to address common problems that can occur in groups to prepare them for their leadership roles. Each session began with an icebreaker activity, had a particular focus, and concluded with a relaxation exercise (Figure 1).
Figure 1:
MESA Five-Week Curriculum
During each MESA group session, the promotoras replicated the training they received from study personnel and a psychologist during a five-day intensive training program prior to the start of the intervention. Promotoras were provided notebooks outlining each of the MESA intervention session’s activities and goals. Flipcharts were used throughout to record ground rules (e.g., confianza or confidentiality) and key points. To practice concepts such as active listening and identifying negative automatic thoughts, promotoras employed role-playing. For the third session, a local psychologist joined the groups and discussed depression and anxiety. This intervention was approved by the UNC-CH Institutional Review Board. Given low literacy rates in the study community, verbal consent was utilized and acquired by study staff at baseline pre-intervention assessment.
Recruitment of Promotoras
Based on community recommendations, church catechists were recruited through the local Catholic parish to serve as promotoras. These women were targeted given their community leadership roles and literacy level. Eligibility criteria for the promotoras included being a female over 18 years of age, the ability to read and write, availability for the five-day promotora training, and few or no symptoms of depression as indicated by a score of less than 16 on the Center for Epidemiologic Studies Depression Scale (CES-D). (32) While most promotoras were catechists, some were recruited through word of mouth by other promotora candidates. A total of eight promotoras were recruited initially; one, however, withdrew prior to group recruitment due to health problems. Seven promotoras ultimately led groups.
MESA Participants
Upon completion of the promotora training, the promotoras recruited women over the age of 18 to participate in their own MESA support groups. The primary means of recruitment was through word of mouth and flyers promoting support groups for women in the promotoras’ communities or neighboring communities. To avoid stigmatization of volunteers, any willing volunteer was included in the intervention unless the following exclusion criteria were met: suicidality or pre-intervention CES-D score over 36 and assessment by study personnel as being unfit for participation. Volunteers excluded from the study were referred to a local psychologist per study protocol.
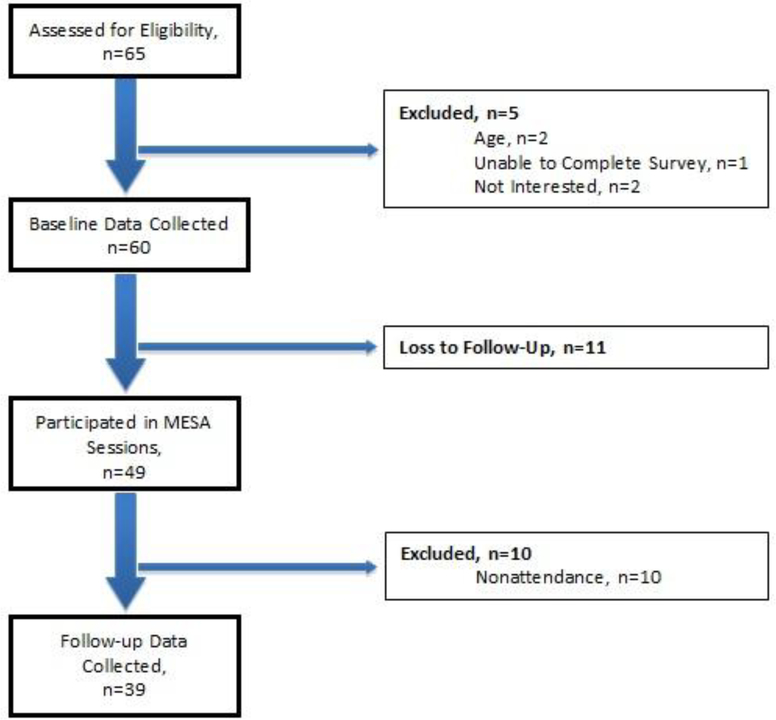
The promotoras recruited a total of 65 women as potential participants in the MESA program (Figure 2). Promotoras reported that the reasons for loss to follow-up included variable work schedules, health problems, family commitments, and uncertainty about participating in a community-based group. Follow-up data were collected for participants who attended at least four sessions (n=39), thereby excluding an additional 10 participants from data collection who did not meet attendance requirements. A comparison of baseline demographic, depression, and social support data between those excluded or lost to follow-up (n=21) and those who completed the intervention (n=39) revealed no significant difference between these two groups.
Figure 2:
MESA Participant Flowchart
Data Collection & Measures
Pre- and post-intervention assessment of the participants and promotoras was conducted by study staff. Baseline and follow-up data collection consisted of basic demographic questions, migrant spouse status (i.e., no migrant spouse, returned migrant spouse, or current migrant spouse), the CES-D, and a modified Medical Outcomes Study (MOS) social support scale. The CES-D is used extensively and has been validated in Latino immigrant (31) and Mexican populations, (33) and applied in promotora-based interventions (range 0–60).(5) For Latina populations, CES-D scores from 16 to 23 indicate moderate depressive symptoms and scores of 24 or higher indicate severe depressive symptoms. (34) A five-point change in CES-D score from baseline to follow-up was considered clinically meaningful change in this study and is similar to other mental health interventions. (35) Social support was measured by a modified version of the MOS social support scale(36) adapted for Spanish speaking populations.(37,38) The MOS scale has been used in Latino populations in the US (39) and Spanish-speaking countries(38) and measures perceived social support using a five-point Likert scale based on level of agreement to nine statements regarding different types of social support.
Analysis
Statistical methods for MESA focused on assessing the goal of increasing social support and decreasing depression before and after the five-week intervention. Given the duration of the program, participants who attended fewer than four of the five sessions were excluded. Two-tailed paired t-tests were conducted to look at change in depression scores and levels of social support from baseline to follow-up. Subgroup analysis was performed on participants according to baseline depression level and migrant spouse status. Bivariate regression analyses were used to examine the association between variables of interest, such as migrant spouse status, and change in depression and social support scores. Descriptive statistics, tests of association, and regression analyses were computed using Stata 12.1.
RESULTS
MESA Participant Characteristics
The majority of the 39 participants (77%) who were present for preintervention and follow-up data collection attended all five weekly MESA meetings. Group sizes ranged from 3 to 12. The baseline characteristics revealed most participants were middle aged (mean age, 40.6 ± 13.9), married (64%), had children (85%), and had migrant family members (90%) (Table 1). Almost 30% of participants had a current or former spouse who was a return migrant, and 18% had a current migrant spouse in the US.
Table 1:
Demographic Characteristics of Participants (n=39)
| Mean | SD | |
| Age | 40.6 | 13.9 |
| Household Size | 4.7 | 1.9 |
| Number of children (n=33) | 3.0 | 2.4 |
| N | % | |
| Civil Status | ||
| Married | 25 | 64.1% |
| Single | 8 | 20.5% |
| Partnered | 2 | 5.1% |
| Divorced | 3 | 7.7% |
| Widowed | 1 | 2.6% |
| Have children | 33 | 84.6% |
| Employed | 14 | 35.6% |
| Family Migration | ||
| Currently has migrant family members | 35 | 89.7% |
| Has ever received remittances from US | 13 | 33.3% |
| Current Migrant Spouse in the US | 7 | 18.0% |
| Return Migrant Spouse | 11 | 28.2% |
Outcomes
CES-D
Table 2 shows baseline and follow-up depression scores for MESA participants. At baseline, approximately 70% of participants were considered depressed (mean CES-D, 22.9 ±12.3). Overall, there was a decrease of 2.4 points in CES-D score for all participants (p=.23). When grouped according to baseline CES-D score, change in depressive symptomology varied across groups. For those with no depressive symptoms at baseline (n=12), CES-D scores went up by 3.9 (p=.23), but remained below the threshold for depression. Participants with moderate depressive symptoms (n=8) experienced a decrease from baseline to follow-up of 3.9 (p=.10). For those with high depressive symptoms who represented almost half of MESA participants (n=19), the reduction in depressive symptoms was 5.6 (p=.09). When grouped according to migration status of spouse, those with current migrant spouses (n=7) experienced an increase of 2.0 (p=.06) in depressive symptoms. Having a current migrant spouse was the only demographic factor associated with a decreased odds of improvement in depressive symptoms (OR=.17, p=.097; 95% CI 0.02, 1.38). Respondents with return migrant spouses (n=11) experienced a decrease of 4.9 (p=.33) in CES-D scores, while those with no migrant spouse (n=21) experienced a decrease of 2.4 (p=.35).
Table 2:
Mean (SD) Baseline and Follow-up Depression Scores
| n | Baseline CES-D | Follow-up CES-D | Change in CES-D | p value | |
|---|---|---|---|---|---|
| All participants | 39 | 22.9 (12.3) | 20.5 (12.3) | −2.4 | 0.23 |
| According to baseline depression level (n=39) | |||||
| No depressive symptoms | 12 | 9.3 (5.3) | 13.2 (11.1) | 3.9 | 0.23 |
| Moderate depressive symptoms | 8 | 18.8 (2.7) | 14.9 (6.3) | −3.9 | 0.10 |
| High Depressive symptoms | 19 | 33.1 (7.7) | 27.5 (11.3) | −5.6* | 0.09 |
| According to migrant spouse status (n=39) | |||||
| Current Migrant Spouse | 7 | 21.4 (14.5) | 23.4 (14.4) | 2.0* | 0.06 |
| Return Migrant Spouse | 11 | 22.6 (14.3) | 17.7 (13.6) | −4.9 | 0.33 |
| No migrant Spouse‡ | 21 | 23.4 (11.0) | 21.0 (11.2) | −2.4 | 0.35 |
Note: Reported p-values are for a two-tailed paired t-test.
p<0.10
p<0.05.
This group consists of 12 married and 9 single participants.
Outcomes
Social Support Scale
Mean social support was 31.0 for all groups at baseline (Table 3). Participants with no depressive symptoms reported higher levels of social support at baseline (33.3±4.9) than those with moderate (29.9±8.2) or high depressive symptoms (30.0±9.0). Overall, reported social support increased by 2.1 points from baseline to follow-up for MESA participants (p=.06). When grouped by degree of depression, participants with no depressive symptoms at baseline experience a 3.5 point increase (p=.09) in social support. Participants with moderate and high depressive symptoms at baseline experienced non-significant 1.6 and 1.5 increases in social support, respectively. When examining social support by migrant spouse status, participants with current migrant spouses had similar baseline levels of social support (30.6±6.3) as those with return migrant spouses (32.5±7.2) or no migrant spouse (30.3±8.7). Those with return migrant spouses experienced an increase in social support of 3.8 (p=.07), while those without migrant spouses experienced an increase of 1.4 (p=.38) and those with current migrant spouses experienced a 1.7 (p=.58) increase in social support.
Table 3:
Mean (SD) Baseline and Follow-up Social Support Scores
| n | Baseline Social Support | Follow-up Social Support | Change in Social Support | p value | |
|---|---|---|---|---|---|
| All participants | 39 | 31.0 (7.8) | 33.1 (7.8) | 2.1* | 0.06 |
| According to baseline depression level (n=39) | |||||
| No depressive symptoms | 12 | 33.3 (4.9) | 36.8 (5.1) | 3.5* | 0.09 |
| Moderate depressive symptoms | 8 | 29.9 (8.2) | 31.5 (9.0) | 1.6 | 0.61 |
| High Depressive symptoms | 19 | 30.0 (9.0) | 31.5 (8.2) | 1.5 | 0.34 |
| According to migrant spouse status (n=39) | |||||
| Current Migrant Spouse | 7 | 30.6 (6.3) | 32.3 (9.3) | 1.7 | 0.58 |
| Return Migrant Spouse | 11 | 32.5 (7.2) | 36.3 (8.2) | 3.8* | 0.07 |
| No migrant Spouse‡ | 21 | 30.3 (8.7) | 31.8 (6.9) | 1.4 | 0.38 |
Note: Reported p-values are for a two-tailed paired t-test.
p<0.10
p<0.05.
This group consists of 12 married and 9 single participants.
DISCUSSION
This study was designed to evaluate a brief group intervention focused on improving depression through social support for women impacted by migration in rural Mexico. Depression scores declined modestly (2.4) overall, and perceived social support increased significantly from baseline to follow-up, especially for non-depressed participants or those with return migrant spouses. Depression outcomes among participants varied according to baseline level of depression and migrant spouse status. Participants with high depressive symptoms at baseline experienced a significant decrease of 5.6 in mean CES-D scores and approached a transition from high to moderate depressive symptoms. When results were grouped according to current, return, or no migrant spouse, depressive symptoms increased significantly among those with a current migrant spouse, while the other groups experienced decreases in depressive symptoms from baseline to follow-up.
Cultural context and feasibility issues in the study community influenced the development of MESA. Mental health problems such as depression are not well recognized among Latin Americans, especially those with low socioeconomic status;(40) thus, cultural beliefs may inhibit depressed adults from seeking traditional mental health care services. When compared to US-born whites, Latina immigrants are more likely to report concerns about stigma regarding mental health care. (41) Similarly, rural Mexicans are highly unlikely to seek care from mental health specialists, due in part to limited access and health-seeking behaviors focused on self-care or social network support.(42) Since mental health represents a new area for promotoras (27,43) the ability to compare our findings to similar interventions is limited. A review of randomized controlled trials comparing peer support to usual care for depression found that peer support resulted in better outcomes than usual care and similar outcomes to group therapy.(44) Our results show a decrease in depressive symptoms for those with depression that is close to a clinically meaningful decrease of 5 points on the CES-D scale. Given the cultural context surrounding mental health, limitations of clinical mental health interventions in rural Mexico and the benefits of peer support, a community-based promotora intervention is likely a culturally acceptable and feasible way to address depression in Mexican migratory sending communities.
While social support has been shown to be protective against depression(10) and to be negatively impacted by the migration of family members,(43) the exact mechanism of this effect is unclear. Our work confirms the finding that social support is protective against depression, as those in our study with the highest perceived social support both at baseline and at follow-up were those who were either not depressed or who had a return migrant spouse. In addition, these groups experienced the largest and only significant increases in social support, perhaps because they are better equipped to accept or perceive additional social support through a promotora intervention. In addition, MESA may not provide sufficient social support to compensate for support lost from spousal migration, explaining why this group’s depression scores did not improve. On the other hand, the decrease in CES-D scores for the depressed groups may have been due to factors other than social support. Other aspects of the MESA curriculum, such as coping strategies and mindfulness exercises, could contribute to a decrease in depression. Further work will be needed to fully explore how the MESA intervention improves social support and depression, and identify the appropriate target population and duration of the intervention.
The outcomes from the implementation of this brief intervention are encouraging but have limitations and point to the need for a larger study to confirm the hypothesis that MESA improves depression in women through social support. A small sample size (n=39) limits our ability to ascertain the effectiveness of this intervention across a wider population and to investigate meaningful associations among hypothesized relationships. Our results point to a change in depression for MESA participants that most benefits those with higher levels of depression; however depression tends to attenuate over time and thus regression to the mean cannot be excluded as a possible explanation for our results. Given the challenges of performing a controlled trial in this setting, we could not compute the impact of the intervention as compared to placebo and solely focused on program participants. MESA is a five-week intervention with promising results; however, most effective community-based programs focused on peer social support and depression are at least 8 weeks long.(45) This short duration might have a dose response effect on depression and social support scores at follow-up. While group sessions were designed to last an hour and a half, promotoras reported that group meetings often lasted longer, possibly impacting attrition. Because promotora groups varied in size and composition, we were unable to measure whether some promotoras were more effective group leaders than others given the small sample size and potential confounding factors. The social support instrument we used was found to be reliable in our sample, but future tests with larger samples are needed to establish the validity of this instrument for Mexican women. In-depth qualitative work with promotoras and program participants is needed to better to understand how the MESA curriculum, group dynamics, and promotora effectiveness could be improved.
Understanding the health impacts of migration means addressing both the health of those who left and currently reside in a foreign country, such as immigrant health in the United States, and tackling how migration impacts those left behind. Decreased migration between the US and Mexico in recent years highlights the need to address the mental health implications of migration since the separation and loss of social support experienced by families across borders is now more permanent than in the past.(44,46) Addressing mental health for a vulnerable population through a community-based approach has the potential to improve depression and social support in communities of migration, and a lay health provider model may be the most feasible approach in low-resource settings. Programs like MESA have the potential to raise awareness about mental health and ultimately lead to health behaviors that contribute to the quality of life in communities who are by necessity unstable. While international migration is impacted by forces beyond the scope of a public health intervention, the development of community based approaches to mental health care represent a step towards addressing the health impacts of migration on the other side of the border and warrants further attention.
REFERENCES
- 1.Acosta Y, de la Cruz GP: The Foreign Born From Latin America and the Caribbean: 2010. American Community Survey Briefs. 2011:1–6. http://www.census.gov/prod/2011pubs/acsbr10-15.pdf. Accessed April 5, 2012.
- 2.(INEGI): Censo de Población y Vivienda 2010. 2010. http://www.inegi.org.
- 3.Alderete E, et al. : Depressive symptomatology: Prevalence and psychosocial risk factors among Mexican migrant farmworkers in California. J. Community Psychol 1999;27(4):457–471. [Google Scholar]
- 4.Fox JA, Kim-Godwin Y: Stress and depression among Latina women in rural southeastern North Carolina. J. Community Health Nurs. October 2011;28(4):223–232. [DOI] [PubMed] [Google Scholar]
- 5.Heilemann M, et al. : Protective strength factors, resources, and risks in relation to depressive symptoms among childbearing women of Mexican descent. Health Care Women Int. January 2004;25(1):88–106. [DOI] [PubMed] [Google Scholar]
- 6.Cardemil EV, et al. : Developing a culturally appropriate depression prevention program: the family coping skills program. Cultural diversity & ethnic minority psychology May 2005;11(2):99–112. [DOI] [PubMed] [Google Scholar]
- 7.Williams DM: La promotora. Linking disenfranchised residents along the border to the U.S. health care system. Health Aff. (Millwood). May-Jun 2001;20(3):212–218. [DOI] [PubMed] [Google Scholar]
- 8.Bello M, et al. : [Prevalence and diagnosis of depression in Mexico]. Salud Publica Mex. 2005;47 Suppl 1:S4–11. [PubMed] [Google Scholar]
- 9.Donato KM, et al. : Migration in the Americas: Mexico and Latin America in Comparative Context. The Annals of the American Academy of Political and Social Science 2010;630(1):6–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fleischer NL, et al. : Depressive symptoms in low-income women in rural Mexico. Epidemiology November 2007;18(6):678–685. [DOI] [PubMed] [Google Scholar]
- 11.Minnesota Population Center: Integrated Public Use Microdata Series, International: Version 6.1 [Machine-readable database]. Minnesota: University of Minnesota; 2011. Accessed April 5, 2012. [Google Scholar]
- 12.Bojorquez I, et al. : International migration of partner, autonomy and depressive symptoms among women from a mexican rural area. The International journal of social psychiatry July 2009;55(4):306–321. [DOI] [PubMed] [Google Scholar]
- 13.Familiar I, et al. : Mexican migration experiences to the US and risk for anxiety and depressive symptoms. J. Affect. Disord. April 2011;130(1–2):83–91. [DOI] [PubMed] [Google Scholar]
- 14.Wilkerson JA, et al. : Effects of husbands’ migration on mental health and gender role ideology of rural Mexican women. Health Care Women Int. July 2009;30(7):614–628. [DOI] [PubMed] [Google Scholar]
- 15.Caballero M, et al. : [Women who are left behind: the impact of international migration on the process of seeking health care]. Salud Publica Mex. May-June 2008;50(3):241–250. [DOI] [PubMed] [Google Scholar]
- 16.Hovey JD: Acculturative stress, depression, and suicidal ideation in Mexican immigrants. Cultural diversity & ethnic minority psychology May 2000;6(2):134–151. [DOI] [PubMed] [Google Scholar]
- 17.Kawachi I, Berkman LF: Social ties and mental health. Journal of urban health : bulletin of the New York Academy of Medicine September 2001;78(3):458–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Silver A Families across borders: The effects of migration on family members remaining at home [1438724]. United States -- North Carolina, The University of North Carolina at Chapel Hill; 2006. [Google Scholar]
- 19.Borges G, et al. : Immigration and suicidal behavior among Mexicans and Mexican Americans. Am. J. Public Health April 2009;99(4):728–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ayala GX, et al. : Outcome effectiveness of the lay health advisor model among Latinos in the United States: an examination by role. Health Educ. Res. October 2010;25(5):815–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Balcazar H, et al. : A promotora de salud model for addressing cardiovascular disease risk factors in the US-Mexico border region. Preventing chronic disease January 2009;6(1):A02. [PMC free article] [PubMed] [Google Scholar]
- 22.Ingram M, et al. : The impact of promotoras on social support and glycemic control among members of a farmworker community on the US-Mexico border. The Diabetes educator Jun 2007;33 Suppl 6:172S–178S. [DOI] [PubMed] [Google Scholar]
- 23.Nuno T, et al. : A Promotora-administered group education intervention to promote breast and cervical cancer screening in a rural community along the U.S.-Mexico border: a randomized controlled trial. Cancer causes & control : CCC March 2011;22(3):367–374. [DOI] [PubMed] [Google Scholar]
- 24.Rhodes SD, et al. : Lay health advisor interventions among Hispanics/Latinos: a qualitative systematic review. Am. J. Prev. Med November 2007;33(5):418–427. [DOI] [PubMed] [Google Scholar]
- 25.Koval AE, et al. : CAPRELA (Cancer Prevention for Latinas): findings of a pilot study in Winston-Salem, Forsyth County. N. C. Med. J Jan-Feb 2006;67(1):9–15. [PubMed] [Google Scholar]
- 26.Fernandez-Esquer ME, et al. : A su salud: a quasi-experimental study among Mexican American women. American journal of health behavior September-October 2003;27(5):536–545. [DOI] [PubMed] [Google Scholar]
- 27.Waitzkin H, et al. : Promotoras as mental health practitioners in primary care: a multi-method study of an intervention to address contextual sources of depression. J. Community Health April 2011;36(2):316–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rodriguez-Garcia R, et al. : A community-based approach to the promotion of breastfeeding in Mexico. Journal of obstetric, gynecologic, and neonatal nursing : JOGNN / NAACOG Sep-Oct 1990;19(5):431–438. [DOI] [PubMed] [Google Scholar]
- 29.Corbie-Smith G, et al. : Development of an interinstitutional collaboration to support community-partnered research addressing the health of emerging Latino populations. Academic medicine : journal of the Association of American Medical Colleges April 2010;85(4):728–735. [DOI] [PubMed] [Google Scholar]
- 30.(INEGI): Principales resultados del Censo de Población y Vivienda 2010. 2011:27.
- 31.Gill HE: The Latino migration experience in North Carolina : new roots in the Old North State. Chapel Hill: University of North Carolina Press; 2010. [Google Scholar]
- 32.Radloff LS: The CES-D Scale. Applied Psychological Measurement June 1, 1977. 1977;1(3):385–401. [Google Scholar]
- 33.Vega WA, et al. : Depressive symptomatology in northern Mexico adults. Am. J. Public Health September 1987;77(9):1215–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vega WA, et al. : Depressive symptoms and their correlates among immigrant Mexican women in the United States. Soc. Sci. Med 1986;22(6):645–652. [DOI] [PubMed] [Google Scholar]
- 35.Balfour L, et al. : A randomized controlled psycho-education intervention trial: Improving psychological readiness for successful HIV medication adherence and reducing depression before initiating HAART. AIDS Care October 2006;18(7):830–838. [DOI] [PubMed] [Google Scholar]
- 36.Sherbourne CD, Stewart AL: The MOS social support survey. Soc. Sci. Med 1991;32(6):705–714. [DOI] [PubMed] [Google Scholar]
- 37.Costa Requena G: [Validity of the questionnaire MOS-SSS of social support in neoplastic patients]. Med. Clin. (Barc) 2007;128(18):687–691. [DOI] [PubMed] [Google Scholar]
- 38.De La Revilla AL LdCJ, Bailon ME, Medina MI: [Validation of a Questionnaire to Measure Social Support in Primary Care]. Medicina de Familia 2005;6(1):10–18. [Google Scholar]
- 39.Nandi A, et al. : Access to and use of health services among undocumented Mexican immigrants in a US urban area. Am. J. Public Health November 2008;98(11):2011–2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.de Toledo Piza Peluso E, Blay SL: Community perception of mental disorders - a systematic review of Latin American and Caribbean studies. Soc. Psychiatry Psychiatr. Epidemiol December 2004;39(12):955–961. [DOI] [PubMed] [Google Scholar]
- 41.Salgado-de Snyder VN, et al. : [A model for integrating mental health care resources in the rural population of Mexico]. Salud Publica Mex. January-February 2003;45(1):19–26. [DOI] [PubMed] [Google Scholar]
- 42.Stacciarini JM, et al. : Promotoras in mental health: a review of english, spanish, and portuguese literature. Fam. Community Health April 2012;35(2):92–102. [DOI] [PubMed] [Google Scholar]
- 43.Gallegos-Carrillo K, et al. : Relationship between social support and the physical and mental wellbeing of older Mexican adults with diabetes. Revista de investigacion clinica; organo del Hospital de Enfermedades de la Nutricion September-October 2009;61(5):383–391. [PubMed] [Google Scholar]
- 44.Van Hook J, Zhang W: Who Stays? Who Goes? Selective Emigration Among the Foreign-Born. Population Research and Policy Review 2011;30(1):1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pfeiffer PN, et al. : Efficacy of peer support interventions for depression: a meta-analysis. Gen. Hosp. Psychiatry Jan-Feb 2011;33(1):29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rendall MS, et al. : Declining return migration from the United States to Mexico in the late-2000s recession: a research note. Demography August 2011;48(3):1049–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]