Abstract
Background
We sought to identify predictors of splenic artery embolization (SAE) over observation for hemodynamically stable patients with blunt splenic injury (BSI), by Organ Injury Scale (OIS) grade.
Methods
This was a multi-institutional retrospective study of all adults (≥18) with BSI who were initially managed non-operatively between 2014 and 2016. Multivariate logistic regression analysis was used to identify predictors of SAE by OIS grade. Covariates included radiographic characteristics (presence/quantity of hemoperitoneum, blush, vascular injury), demographics (age, sex, cause), Injury Severity Score, vital signs, and hemoglobin values. We also examined outcomes of death, length of stay (LOS), intensive care unit (ICU) admission, blood products, and failed non-operative management (NOM).
Results
Among 422 patients with stable BSI, 93 (22%) had SAE and 329 (78%) were observed. The rate of SAE increased by grade (p<0.001). In grade I and II BSI, 7% had SAE; significant predictors of SAE were blush (OR: 5.9, p=0.02), moderate or large hemoperitoneum (OR: 3.0, p=0.01), and male sex (OR: 6.3, p=0.05). In grade III BSI, 26% had SAE; significant predictors included moderate or large hemoperitoneum (OR: 3.9, p=0.04), motor vehicle crash (OR: 6.1, p=0.005), and age (OR=1.4, 40% with each decade increase in age, p=0.02). The rate of SAE was 52% for grade IV and 85% for grade V BSI; there were no independent predictors of SAE in either grade. Clinical outcomes were comparable by NOM strategy and grade, except longer LOS with SAE in grades I–III (p<0.05) and longer ICU LOS with SAE in grades I–IV (p<0.05). Only 5 (1.2%) patients failed NOM (4 observation, 1 SAE).
Conclusion
These results strongly support SAE consideration for patients with stable grade IV and V BSI even if there are no other high-risk clinical or radiographic findings. For grades I–III, the identified predictors may help refine consideration for SAE.
Level of evidence
Level III, retrospective epidemiological study.
Keywords: spleen, stable, surgical management, embolization
Introduction
Blunt splenic injury (BSI) is managed with non-operative management (NOM) with either observation or splenic artery embolization (SAE) for patients who are hemodynamically stable and have no peritonitis or another abdominal surgical indication.1–3 SAE is considered an adjunct for patients with more severe injuries, although there is considerable variability in the use of SAE even across level I trauma centers.4 The American Association for the Surgery of Trauma (AAST) Organ Injury Scale (OIS) grade is conventionally used to grade the severity of BSI, with scores ranging from 1 to 5.5 The 1994 grading scale6 did not explicitly incorporate important radiographic findings used to determine the necessity for SAE, such as presence or size of contrast blush, quantity of hemoperitoneum, and pseudoaneurysm. In December 2018, the AAST updated the spleen OIS grading scale7 to incorporate CT diagnosed vascular injury, defined as a pseudoaneurysm or arteriovenous fistula. The OIS grade is revised to grade IV when a vascular injury is present and is further revised to grade V when active bleeding, defined as vascular contrast that increases in size or attenuation in delayed phase, extends into the peritoneum.
The 2018 OIS update does not address treatment strategies, specifically which OIS grade may prompt intervention. The 1994 OIS grading scale is used in the most recent treatment guidelines by the Eastern Association for the Surgery of Trauma (EAST, 2012)2 and the Western Trauma Association (WTA, 2016 update).8 The EAST guidelines state that patients with grade I–III injury should be observed, while SAE should be considered for patients with grade IV and V injury, as well as any patient regardless of grade with evidence of contrast blush, moderate or large hemoperitoneum, and pseudoaneurysm. The WTA guidelines use a combination of OIS grade and presence of contrast blush for SAE consideration: patients with grades I–III should be observed if there is no blush and should have angiography considered if there is blush; for grades IV and V, patients should have angiography considered if there is no blush and should have SAE if there is blush. These disparate guidelines highlight the lack of consensus on optimal NOM strategy in stable BSI.
The study objective was to refine patient selection for NOM strategy (ie, observation or SAE) in patients with stable BSI. Our approach differs from prior analyses in two important ways. First, the hypothesis is to determine which variables predict a greater likelihood of requiring SAE over observation, rather than focusing on the rate of failed NOM (fNOM) as the study outcome. Second, our analysis incorporates detailed radiographic findings in addition to OIS grade and presenting characteristics.
Methods
Setting, study design, and participants
This retrospective, multi-institutional cohort study was performed by the Injury Outcomes Network, a collaborative research network of six community-based, level I trauma centers: Swedish Medical Center, Englewood, CO; St Anthony Hospital, Lakewood, CO; Penrose Hospital, Colorado Springs, CO; Medical City Plano, Plano, TX; Research Medical Center, Kansas City, MO; and Wesley Medical Center, Wichita, KS.
The population included all consecutive hospital admissions between 1/1/2014 – 12/31/2016 who were admitted for a BSI, identified by the hospital trauma registry as International Classification of Diseases, Ninth Revision (ICD-9) diagnosis code of 865 or ICD-10 diagnosis code of S36.0, and Abbreviated Injury Scale codes 544299.2, 544210.2 through 544228.5 and 544240.3.
Study exclusions were as follows: age <18; dead on arrival or died in the ED; not acutely transferred within 24 hours of the injury; and transfers with inadequate documentation of the initial assessment or CT findings (n=82 total exclusions).
For this analysis, we also excluded patients: who were hemodynamically unstable defined by chart notation or presenting systolic blood pressure (SBP) <90 mm Hg (n=66); who went directly to the operating room for another abdominal surgical indication (n=41) or for splenectomy (n=21); without a documented OIS grade (n=19); with missed splenic injury (n=4); and with peritonitis (n=1).
Study variables
The following radiographic findings were abstracted from the electronic medical record: (A) CT scanner characteristics. The standard for trauma patients is a combination of chest/abdomen/pelvis with intravenous contrast on a 64-slice or greater CT in venous phase. More recently, scans include biphasic scans with multiplanar reformatting and additional delayed, postcontrast images. (B) OIS grade (initial grade, final grade). The 1994 scale was used during the study period.6 (C) Presence of contrast blush and size of blush, as noted by radiology as small, moderate, large blush or blush size in millimeters). In the majority of cases, a small blush was defined by radiology report as small, otherwise it was defined as a blush size <10 mm. (D) Hemoperitoneum and quantity (small, moderate, large). The quantity of hemoperitoneum was quantified from CT findings as small (perisplenic blood or blood in Morison’s pouch), moderate (presence of blood in one or both pericolic gutters) and large (additional finding of free blood in the pelvis).9 10 This definition uses the Federle score, which quantifies hemoperitoneum based on the count of compartments in the peritoneal cavity affected by the effusion.11 (E) Presence of vascular injury, defined as a pseudoaneurysm or arteriovenous fistula.7 (F) Presence of a non-surgical abdominal injury.
Additional variables that were abstracted from the electronic medical record included: hemoglobin levels during the first 24 hours (g/dL), total units of blood products received, patient blood type, and initial intervention technique and definitive intervention technique (eg, patients initially observed but later treated with SAE).
The following demographic, clinical, and outcome characteristics were obtained from the trauma registries: admission date; transfer status; age, years; gender; cause of injury (motor vehicle crash (MVC), fall, other cause); Injury Severity Score (ISS); admission vital signs including Glasgow Coma Scale score (GCS, 3–8 or 9–15), SBP (<90 or ≥90 mm Hg), pulse (<120 or 120 beats per minute) and respiratory rate (<12 or >20 vs. 12–20 breaths per minute); in-hospital mortality; intensive care unit (ICU) length of stay (LOS), days; and hospital LOS, days.
Statistical analyses
The primary outcome was definitive intervention strategy. We used univariate statistics (Pearson’s χ2 tests, Fisher’s exact tests, and Wilcoxon rank-sum tests) to determine the association between study covariates and intervention strategy (observation vs. SAE) by OIS grade. Univariate statistics were also used to examine covariates and outcomes by OIS grade.
We used multiple logistic regression analysis to examine, by OIS grade, which of the marginally associated covariates from the univariate analysis (p<0.20) were associated with increased odds of SAE. In grades III and IV there were four and one fNOM, respectively, and these five patients were not excluded from the regression analysis. The regression models in these OIS grades were used to determine which of the marginally associated covariates from the univariate analysis (p<0.20) were associated with increased odds of SAE or fNOM (eg, decreased odds of successful observation). The Firth method was used, which is an approach to reducing small sample size bias in maximum likelihood estimates. Results are presented as adjusted ORs and 95% CIs. We performed a receiver operating characteristic curve analysis to assess the models, and the area under the receiver operating characteristic curve (AUROC) is presented for the full model. All statistical analyses were two tailed with a p value <0.05 defined as significant and were conducted using SAS V.9.4 (SAS Institute).
Results
Patient characteristics
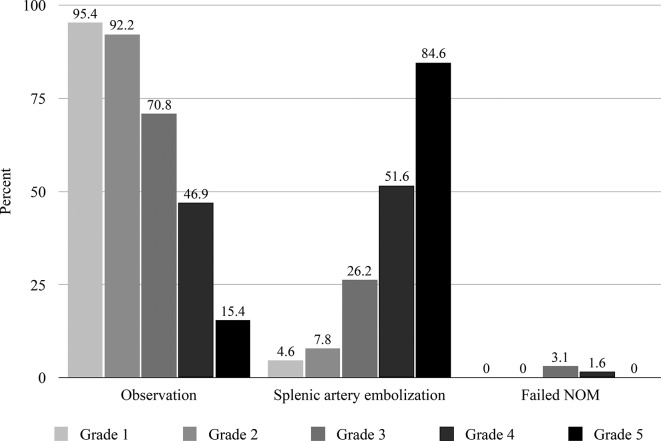
A total of 422 patients with BSI were initially managed non-operatively (figure 1). The patient population was predominantly injured in an MVC (73%), were younger (median age 36 years), were male (69%), and with a median ISS of 18. The majority (59%) presented with hemoperitoneum, of which 57% were moderate or large. Only 12% of patients had blush and 4% had a vascular injury. The size of blush was not documented in 21% of patients. In the remaining patients with blush, the majority (67%) were small. A 64-slice or greater CT scanner was used in 95% of patients and 92% of patients had intravenous contrast CT, and this proportion increased with OIS grade (91% grades I and II, 93% grade III, 95% grade IV, 100% grade V).
Figure 1.
Study population. BSI, blunt splenic injury; ED, emergency department; OR, operating room.
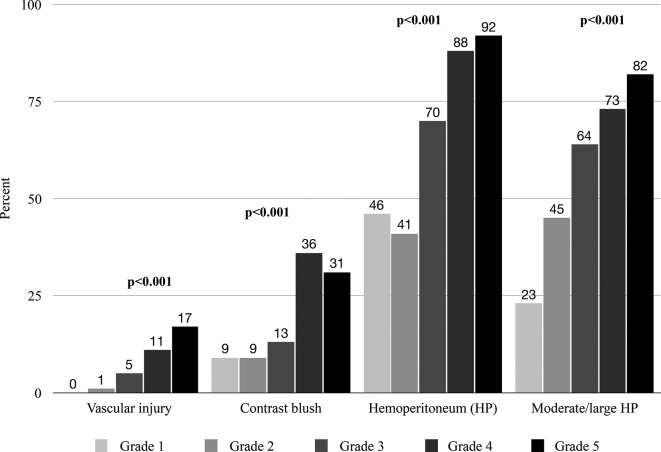
Patients were managed non-operatively as follows: 93 (22%) with SAE and 329 (78%) with observation. There were 17 patients who were initially observed and required SAE as their definitive management (grades I–V: n=1, 1, 9, 4, 2), and one patient who had angiography without embolization and thus was observed (grade III). The rate of SAE increased with OIS grade: 5% of grade I, 8% of grade II, 26% of grade III, 52% of grade IV, and 85% of grade V (p<0.001, figure 2).
Figure 2.
Non-operative management (NOM) of stable blunt splenic injury, by American Association for the Surgery of Trauma (AAST) grade.
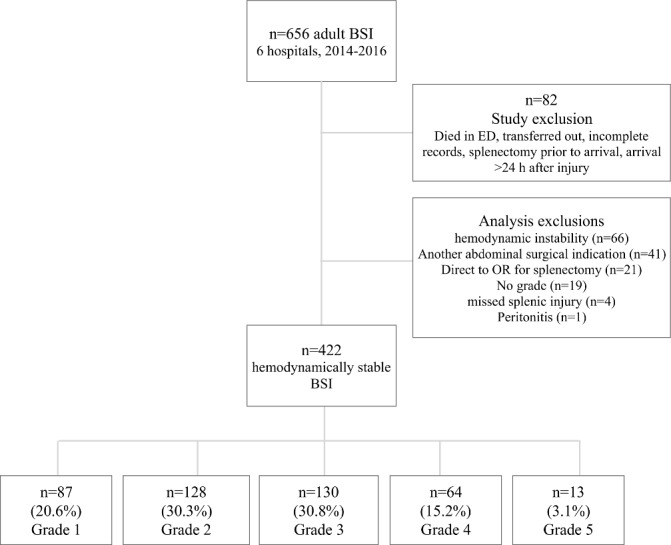
There were a few significant differences by OIS grade. Grade IV BSI was more likely to have a fall injury (table 1). As expected, the median ISS increased with grade IV and V BSI and radiographic findings of blush, hemoperitoneum, and pseudoaneurysm increased with OIS grade (figure 3). There were no differences in age, sex, blood type, hemoglobin levels, other non-surgical abdominal findings, GCS scores, and all vital signs.
Table 1.
Characteristics and outcomes by spleen grade
| Variable, n (%) | Grade 1 (n=87) |
Grade 2 (n=128) |
Grade 3 (n=130) |
Grade 4* (n=64) |
Grade 5 (n=13) |
P value |
| Median age, years | 37 (27–54) | 35 (24.5–55) | 35 (25–55) | 39.5 (25–55) | 26 (22–36) | 0.25 |
| Age ≥65 years | 6 (6.9) | 15 (11.7) | 15 (11.5) | 9 (14.1) | 0 (0) | 0.42 |
| Female sex | 27 (31.0) | 43 (33.6) | 41 (31.5) | 14 (21.9) | 8 (61.5) | 0.08 |
| Cause of injury | 0.03 | |||||
| Vehicular cause | 74 (85.1) | 97 (75.8) | 89 (68.5) | 37 (57.8) | 11 (84.6) | |
| Fall cause | 9 (10.3) | 18 (14.1) | 22 (16.9) | 15 (23.4) | 1 (7.7) | |
| Other cause | 4 (4.6) | 13 (10.2) | 19 (14.6) | 12 (18.8) | 1 (7.7) | |
| ISS, median | 17 (9–27) | 17 (9–22) | 19 (11–27) | 25 (17–29) | 35 (22–38) | < 0.001 |
| ED GCS score 3–8 | 12 (13.8) | 22 (17.2) | 15 (11.5) | 6 (9.4) | 0 (0) | 0.29 |
| ED RR <12 or >20 | 18 (22.8) | 35 (30.2) | 27 (21.6) | 17 (27.2) | 2 (18.2) | 0.54 |
| ED HR >120 | 11 (12.8) | 12 (9.5) | 12 (9.5) | 6 (9.4) | 4 (30.8) | 0.18 |
| ED SBP <90 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | NA |
| Blood type O | 36 (41.4) | 40 (31.3) | 45 (34.6) | 29 (45.3) | 5 (38.5) | 0.31 |
| First Hgb <10^ | 9 (10.3) | 18 (14.1) | 11 (8.5) | 8 (12.5) | 4 (30.8) | 0.15 |
| Outcomes | ||||||
| Mortality | 1 (1.2) | 5 (3.9) | 4 (3.1) | 2 (3.1) | 0 (0) | 0.76 |
| ICU admission | 62 (71.3) | 104 (81.3) | 115 (88.5) | 61 (95.3) | 12 (92.3) | < 0.001 |
| Number of blood products, median | 8.5 (3–25) | 3.5 (2.5–6.5) | 2.0 (2–6) | 4.0 (2–6) | 2.0 (2–8) | 0.18 |
| Hospital LOS, median | 7 (2–12) | 6 (3–10.5) | 6 (4–13) | 6 (4.5–11.5) | 6 (4–10) | 0.59 |
| ICU LOS, median | 2 (1–6) | 2 (1–6) | 3 (92–6) | 3.5 (2–7) | 4 (2–5) | 0.09 |
| Failed NOM | 0 (0) | 0 (0) | 4 (3.1) | 1 (1.6) | 0 (0) | 0.15 |
*Four patients were initially grade III and one patient was initially a grade V, all were revised to grade IV.
†P values from Fishers exact test, Pearson’s χ2 test, or Wilcoxon rank-sum test for differences between grades. Bolding denotes significance <0.05.
ED, emergency department; GCS, Glasgow Coma Scale; HR, heart rate; Hgb, hemoglobin; ICU, intensive care unit; ISS, Injury Severity Score; LOS, length of stay; NA, not applicable; NOM, non-operative management; RR, respiratory rate; SBP, systolic blood pressure.
Figure 3.
Radiographic findings by blunt splenic injury grade.
Predictors of SAE, by grade
Among grades I and II, 14 (6.5%) patients had SAE. Factors associated with SAE that were identified by univariate analysis (p<0.20) included sex, cause of injury, GCS, tachycardia, blush, quantity of hemoperitoneum, and vascular injury (table 2). After adjustment for these variables (except for vascular injury, which only occurred in one patient), the following covariates were independently associated with SAE: presence of blush (OR=5.9, p=0.02), moderate or large hemoperitoneum (OR=3.0, p=0.01), and male gender (OR=6.3, p=0.047) (table 3). The GCS score 3–8 was no longer significantly associated with having SAE, after adjustment. The AUROC was 0.90, indicating excellent accuracy of the model.
Table 2.
Characteristics by definitive management and Organ Injury Scale grade
| Covariates | Grades I and II | Grade III | Grade IV | Grade V | ||||
| Observation (n=201) | SAE (n=14) | Observation (n=92) | SAE (n=34) | Observation (n=30) | SAE (n=33) | Observation (n=2) | SAE (n=11) | |
| Median age, years | 36 (26–54) | 41.5 (24–60) | 31 (23.5–52) | 45 (32–60)** | 33 (25–51) | 43 (30–56) | 26.5 (22–31) | 26 (21–44) |
| Female sex | 69 (34.3) | 1 (7.1)** | 28 (30.4) | 12 (35.3) | 6 (20.0) | 7 (21.2) | 2 (100) | 6 (54.6) |
| Vehicular cause | 161 (80.1) | 10 (71.4)* | 56 (60.9) | 29 (85.3)** | 16 (53.3) | 20 (60.6) | 2 (100) | 9 (81.8) |
| Fall cause | 23 (11.4) | 4 (28.6) | 19 (20.7) | 3 (8.8) | 7 (23.3) | 8 (24.2) | 0 (0) | 1 (9.1) |
| Other cause | 17 (8.5) | 0 (0) | 17 (18.5) | 2 (5.9) | 7 (23.3) | 5 (15.2) | 0 (0) | 1 (9.1) |
| ISS, median | 17 (9–22) | 15.5 (9–27) | 19 (10.5–27) | 17 (14–27) | 23 (16–29) | 26 (20–29)* | 30 (22–38) | 35 (21–38) |
| ED GCS score 3–8 | 28 (13.9) | 6 (42.9)** | 13 (14.1) | 2 (5.9) | 2 (6.7) | 4 (12.1) | 0 (0) | 0 (0) |
| ED RR <12 or >20 | 49 (27.1) | 4 (28.6) | 15 (16.7) | 10 (32.3)* | 7 (24.1) | 10 (31.3) | 0 (0) | 2 (22.2) |
| ED HR >120 | 20 (10.1) | 3 (21.4)* | 11 (12.4) | 1 (3.0)* | 0 (0) | 6 (18.2)** | 1 (50) | 3 (27.3) |
| Blood type O | 70 (34.8) | 6 (42.9) | 27 (29.4) | 16 (47.1)* | 10 (33.3) | 18 (54.5)* | 0 (0) | 5 (45.5) |
| First Hgb <10 | 27 (13.4) | 0 (0) | 9 (9.8) | 1 (2.9) | 3 (10.0) | 5 (15.2) | 0 (0) | 4 (36.4) |
| Other torso finding | 18 (9.0) | 0 (0) | 12 (13.0) | 3 (8.8) | 3 (10.0) | 4 (12.1) | 0 (0) | 2 (18.2) |
| Blush (any) | 14 (7.8) | 4 (28.6)** | 9 (10.5) | 6 (17.7) | 6 (25.0) | 13 (41.9)* | 1 (50.0) | 3 (27.3) |
| HP (any) | 67 (39.4) | 11 (84.6)** | 52 (70.3) | 23 (74.2) | 22 (84.6) | 26 (89.7) | 1 (50.0) | 10 (100)* |
| Moderate/large HP | 23 (34.3) | 6 (54.5)* | 29 (31.5) | 19 (55.9)** | 15 (50.0) | 20 (60.6) | 0 (0) | 9 (81.8)* |
| Vascular injury | 0 (0) | 1 (8.3)* | 1 (1.2) | 5 (14.7)** | 2 (8.3) | 3 (10.3) | 0 (0) | 2 (20.0) |
*Patients who failed non-operative management (NOM) were not tabulated (grade 1, n=0; grade 2, n=0; grade 3, n=4; grade 4, n=1; grade 5, n=0). *P <0.20; **p<0.05.
ED, emergency department; GCS, Glasgow Coma Scale;HP, hemoperitoneum; HR, heart rate;Hgb, hemoglobin;ISS, Injury Severity Score;ISS, Injury Severity Score; RR, respiratory rate; SAE, splenic artery embolization.
Table 3.
Logistic regression modeling the need for SAE or failing non-operative management, vs. successful observation
| Covariate | Overall (AUROC: 0.87) | Grades I and II (AUROC: 0.90) | Grade III (AUROC: 0.84) | Grade IV (AUROC: 0.71) | Grade V (AUROC: 0.90) | |||||
| OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | |
| Moderate/large HP vs. small | 3.0 (1.3 to 6.7) | 0.001 | 3.0 (0.7 to 11.9) | 0.01 | 3.9 (0.9 to 16.1) | 0.04 | NA | 19.0 (0.3 to >999) | 0.27 | |
| Blush vs. not | 1.5 (0.7 to 3.2) | 0.29 | 5.9 (1.3 to 26.7) | 0.02 | NA | NA | NA | |||
| HR ≥120 vs. HR <120 | 1.2 (0.5 to 2.9) | 0.71 | 3.2 (0.6 to 15.8) | 0.16 | 0.2 (0.02 to 1.3) | 0.08 | 10.6 (0.4 to 262) | 0.15 | NA | |
| Male sex vs. female | 1.3 (0.7 to 2.5) | 0.41 | 6.3 (1.0 to 38.5) | 0.047 | NA | NA | NA | |||
| Vehicular vs. fall cause | 1.3 (0.6 to 3.0) | 0.27 | 0.4 (0.1 to 1.8) | 0.48 | 6.1 (1.3 to 27.3) | 0.02 | NA | NA | ||
| Vascular injury vs. not | 10.8 (2.2 to 53.7) | 0.004 | NA | 4.8 (0.6 to 40.0) | 0.15 | 1.5 (0.2 to 9.4) | 0.67 | NA | ||
| ISS (10-unit increase) | 1.2 (0.9 to 1.6) | 0.28 | NA | NA | 1.4 (0.7 to 2.9) | 0.3 | NA | |||
| GCS score 3–8 vs. 9–15 | NA | 3.1 (0.9 to 10.8) | 0.08 | NA | NA | NA | ||||
| Blood type O vs. other | NA | NA | 1.9 (0.7 to 5.2) | 0.19 | NA | NA | ||||
| Abnormal RR vs. RR 12–20 | NA | NA | 1.5 (0.5 to 4.6) | 0.48 | NA | NA | ||||
| Age (10-unit increase) | NA | NA | 1.4 (1.1 to 1.8) | 0.02 | NA | NA | ||||
| BSI grade (continuous) | 2.7 (1.9 to 3.8) | < 0.001 | NA | NA | NA | |||||
*Variables marginally associated in the univariate analysis (p<0.20) were included in the final multivariate logistic regression model. NA indicates that the covariate was not examined in the specific model. Bolding denotes significance <0.05.
AUROC, area under the receiver operating characteristic curve; BSI, blunt splenic injury;GCS, Glasgow Coma Scale;HP, hemoperitoneum;HR, heart rate;ISS, Injury Severity Score;RR, respiratory rate; SAE, splenic artery embolization.
In grade III BSI, 26% had SAE and 3% (n=4) fNOM. Factors associated with SAE that were identified by univariate analysis (p<0.20) included age, cause of injury, blood type O, tachycardia, abnormal respiratory rate, quantity of hemoperitoneum, and vascular injury (table 2). After adjustment, variables independently associated with SAE or fNOM were MVC injury (OR=6.1, p=0.005), moderate or large hemoperitoneum (OR=3.9, p=0.04), and age (OR=1.40, representing 40% decreased odds of successful observation with each decade increase in age; p=0.02) (table 3). The AUROC was 0.84, indicating good accuracy of this model.
In grade IV BSI, 52% had SAE and one patient fNOM. Factors associated with SAE that were identified by univariate analysis (p<0.20) included ISS, tachycardia, blood type O, and presence of blush (table 2). However, after adjustment, none of these variables were significantly associated with SAE or fNOM.
Nearly all (85%) of patients with grade V had SAE, with no fNOM. Only moderate or large hemoperitoneum was associated with SAE in univariate analysis (table 2), which was not associated with increased odds of SAE in the regression model (p=0.27).
When grades IV and V were combined (n=77), 39% presented with contrast blush or vascular injury while 61% did not have another indication for SAE other than OIS grade. There were no significant predictors of increased odds of SAE in the regression model in this high-grade subset (data not shown).
Predictors of SAE, overall
In the final overall model, OIS grade remained a significant predictor of increased odds of SAE or fNOM (OR=2.7, p<0.001) (table 3). In addition, vascular injury (OR=10.8, p=0.004) and moderate or large hemoperitoneum (OR=3.0, p=0.001) independently increased the odds of SAE. The AUROC was 0.87, indicating very good accuracy of the overall model.
Clinical outcomes
Study outcomes were as follows: mortality was 2.8%, median units of blood products was 4 (2–7), median hospital LOS was 6 (3–12) days, median ICU LOS was 3 (1–6) days, and the fNOM rate was 1.2% (n=5; 4 observation and 1 SAE). Four of five fNOM were grade III injuries who were initially observed but had delayed deterioration (15 hours, 2 days, 4 days, and 6 days after arrival). The fifth patient was a 54-year-old woman with grade IV injury with large hemoperitoneum, blush, and vascular injury. She initially underwent SAE but the spleen was not salvageable. All patients with fNOM were involved in an MVC and all survived.
Clinical outcomes by OIS grade are shown in table 1. Only ICU admission was significantly greater with higher grade. Clinical outcomes by NOM strategy and OIS grade are shown in online supplementary table 1. Compared with observation, hospital LOS was longer for patients who had SAE with grades I–III, and ICU LOS was longer for patients who had SAE for grades I–IV. There were no significant differences by NOM and OIS grade for mortality, ICU admission, and total number of blood products received. We also examined whether outcomes differed for patients with SAE who were initially managed as such (early SAE) compared with patients who were initially observed (late SAE). Compared with early SAE, late SAE was associated with longer hospital LOS (7 days vs. 11 days, p=0.03) and ICU LOS (4 days vs. 7 days, p=0.01).
tsaco-2019-000323supp001.pdf (59.8KB, pdf)
Discussion
This study demonstrates that, across all patients with hemodynamically stable BSI, only radiographic findings of vascular injury, moderate or large hemoperitoneum, and higher OIS grade significantly increased the odds of having SAE or fNOM. Interpreted another way, patients without high-risk radiographic findings have significantly greater odds of being safely observed, independent of demographics, injury characteristics, or clinical presentation.
When examined by OIS grade, the results of our study have two main implications. First, we identified variables that may be used to optimize management of patients with lower grade I–III BSI. Patients with grade III injuries had greater odds of having SAE or fNOM if they had moderate or large hemoperitoneum, were involved in an MVC, and were older. In patients presenting with grade I–II BSI, the odds of having SAE increased with moderate or large hemoperitoneum, contrast blush, and for men. These models had excellent accuracy for predicting the need for SAE. These results may help refine criteria for SAE in lower grade BSI.
The second implication of these results is that there were no demographic, clinical, or radiographic covariates that increased odds of SAE in higher grade IV–V BSI, so we strongly encourage considering SAE even if vital signs are normal and there are no other high-risk radiographic findings. It is possible that there are other variables that we did not capture that would improve our model. Another possibility is that the OIS grade indirectly captures radiologic findings and injury severity, and used alone, can determine which patients might require SAE. We doubt this is the case, because 61% of grade IV BSI did not have another indication for SAE (blush or vascular injury), yet the rate of SAE was still 49% in this subset. A third possibility is that we were unable to find any independent predictors of SAE because the procedure was performed ‘prophylactically,’ that is, based on hospital guidelines and not for therapeutic reasons. This is also unlikely to explain our findings because 43% of patients with grade IV–V BSI were observed. One hospital’s management guideline for grade IV–V BSI was mandatory SAE, which they followed 92% of the time (11 of 12 patients). Even after removing this hospital from the logistic regression analysis there were still no predictors of SAE in grade IV–V BSI.
There is much debate about the significance of blush in patients with BSI. As previously stated, presence of blush was paramount in the WTA guidelines8 but not in the EAST guidelines.2 The World Society of Emergency Surgery guidelines only use presence of blush for lower grades I–III in their algorithm.12 Bhullar and colleagues reported blush to be predictive of fNOM only in patients with grade IV–V BSI,13 then in a subsequent publication the authors suggested contrast blush mandates angiography for all patients irrespective of OIS grade, and further that the absence of blush does not reliably exclude active bleeding in patients with high grade IV–V BSI.14 Our study did not identify contrast blush to be predictive of SAE overall or in high-grade IV–V injury, while presence of blush increased the odds of requiring SAE nearly sixfold in lower grades. Only 12% of patients had contrast blush, which falls in the wide range of 7% to 32% previously reported.15
Quantity of hemoperitoneum has been identified as a ‘high risk’ for SAE or fNOM previously.9 16 We also identified moderate or large hemoperitoneum to be associated with SAE in our overall population and in patients with lower grade I–III injuries. Moderate or large hemoperitoneum was prevalent (57%), similar to the 59% to 64% rate previously reported.15
Our rate of fNOM was 1.2% and only 4% of stable BSI was excluded because they went directly to the operating room, suggesting that patients with stable BSI are overwhelmingly managed non-operatively with great success. We suspect the low rate of fNOM in our study is because SAE was used liberally across our participating hospitals. A recent analysis of the National Trauma Data Bank presented a 14% rate of SAE for grade III–V BSI in 2014, up from 6% in 2008,17 whereas the rate of SAE was 38% for patients with grade III–V BSI in our study. Three advancements likely to affect increased patient selection for SAE are published guidelines for selective SAE, higher resolution CT technology that can identify smaller volumes of blood, and increased availability of interventional radiology.
There are limitations to the study. First, due to its retrospective nature, we were unable to examine the 2018 OIS revision. The OIS grade would have been revised upwards to an OIS 2018 grade IV due to a documented vascular injury in nine patients; delayed imaging was not standard during our study, so we were unable to discern which patients with active bleeding were within the splenic capsule (OIS 2018 grade IV) or into the peritoneum (OIS 2018 grade V). Second, each hospital had a slightly different management algorithm (online supplementary table 2). However, hospitals did not follow their own algorithms. For instance, 55% of patients had a protocol indication for SAE yet only 22% of patients had SAE. We were surprised to find that hospitals were not following their own practice, but this unintended finding strengthens the analysis and its generalizability. Third, there was no uniform way to define hemodynamic instability across hospitals. For our study, patients were categorized as being hemodynamically unstable either by chart notation or if the presenting SBP was <90 mm Hg. We did not use other markers of hemodynamic instability such as abnormal hemoglobin or lactate values or abnormal respiratory rate or pulse, although these might have been captured in patients with hemodynamic instability noted in the chart. Fourth, there was incomplete documentation of important covariates, including blush status missing in 9%, pseudoaneurysm status missing in 9.5%, and hemoperitoneum status missing in 15%. Rather than exclude patients without these radiographic data from the logistic regression analysis, we recategorized patients with missing data as having a negative finding (‘none/missing’), which might have resulted in misclassification. Lastly, at the time of this study from 2014 to 2016, hospital CT protocols used venous phase scanning. More recent guidelines include biphasic scanning with additional delayed postcontrast images.
tsaco-2019-000323supp002.pdf (14.1KB, pdf)
Conclusions
The OIS grade remained a significant predictor of SAE after taking into account other radiographic and demographic characteristics. Moderate or large quantity hemoperitoneum, contrast blush, and male sex predicted the need for SAE in grade I–II BSI, while moderate or large hemoperitoneum, older age, and MVC injury may be helpful to determine which patients with grade III BSI require SAE or fNOM. Because there were no independent predictors of SAE in higher grade IV and V BSI, we strongly encourage consideration of SAE even if vital signs are normal and there are no other high-risk radiographic findings. We are planning a validation analysis of these data to develop practice guidelines for stable BSI by OIS grade.
Acknowledgments
We acknowledge the study coordinators who performed the data abstraction: Jennifer Pekarek, RN; Diane Redmond, RN; Carolyn Blue, RN; Jamie Shaddix, RN; and Kathy Rodkey, CCRC.
Footnotes
Contributors: All authors contributed to study conception and/or data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding: Funding was provided by Swedish Medical Center, St Anthony Hospital, Medical City Plano, Penrose-St Francis Medical Center, Wesley Medical Center, and Research Medical Center Kansas City.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: This study received Institutional Review Board approval at all participating centers and was granted a waiver of consent and HIPAA authorization.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article.
References
- 1. Scarborough JE, Ingraham AM, Liepert AE, Jung HS, O'Rourke AP, Agarwal SK. Nonoperative management is as effective as immediate splenectomy for adult patients with high-grade blunt splenic injury. J Am Coll Surg 2016;223:249–58. 10.1016/j.jamcollsurg.2016.03.043 [DOI] [PubMed] [Google Scholar]
- 2. Stassen NA, Bhullar I, Cheng JD, Crandall ML, Friese RS, Guillamondegui OD, Jawa RS, Maung AA, Rohs TJ, Sangosanya A, et al. . Selective nonoperative management of blunt splenic injury: an eastern association for the surgery of trauma practice management guideline. J Trauma Acute Care Surg 2012;73(5 Suppl 4):S294–300. 10.1097/TA.0b013e3182702afc [DOI] [PubMed] [Google Scholar]
- 3. Sclafani SJ, Shaftan GW, Scalea TM, Patterson LA, Kohl L, Kantor A, Herskowitz MM, Hoffer EK, Henry S, Dresner LS, et al. . Nonoperative salvage of computed tomography-diagnosed splenic injuries: utilization of angiography for triage and embolization for hemostasis. J Trauma 1995;39:818–25. [DOI] [PubMed] [Google Scholar]
- 4. Banerjee A, Duane TM, Wilson SP, Haney S, O'Neill PJ, Evans HL, Como JJ, Claridge JA. Trauma center variation in splenic artery embolization and spleen salvage: a multicenter analysis. J Trauma Acute Care Surg 2013;75:69–75. 10.1097/TA.0b013e3182988b3b [DOI] [PubMed] [Google Scholar]
- 5. Olthof DC, van der Vlies CH, van der Vlies CH, Joosse P, van Delden OM, Jurkovich GJ, Goslings JC, . PYTHIA Collaboration Group . Consensus strategies for the nonoperative management of patients with blunt splenic injury: a Delphi study. J Trauma Acute Care Surg 2013;74:1567–74. 10.1097/TA.0b013e3182921627 [DOI] [PubMed] [Google Scholar]
- 6. Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR. Organ injury scaling: spleen and liver (1994 revision). J Trauma 1995;38:323–4. [DOI] [PubMed] [Google Scholar]
- 7. Kozar RA, Crandall M, Shanmuganathan K, Zarzaur BL, Coburn M, Cribari C, Kaups K, Schuster K, Tominaga GT, et al. AAST Patient Assessment Committee . Organ injury scaling 2018 update: spleen, liver, and kidney. J Trauma Acute Care Surg 2018;85:1119–22. 10.1097/TA.0000000000002058 [DOI] [PubMed] [Google Scholar]
- 8. Rowell SE, Biffl WL, Brasel K, Moore EE, Albrecht RA, DeMoya M, Namias N, Schreiber MA, Cohen MJ, Shatz DV, et al. . Western trauma association critical decisions in trauma: management of adult blunt splenic trauma-2016 updates. J Trauma Acute Care Surg 2017;82:787–93. 10.1097/TA.0000000000001323 [DOI] [PubMed] [Google Scholar]
- 9. Peitzman AB, Heil B, Rivera L, Federle MB, Harbrecht BG, Clancy KD, Croce M, Enderson BL, Morris JA, Shatz D, et al. . Blunt splenic injury in adults: multi-institutional study of the eastern association for the surgery of trauma. J Trauma 2000;49:177–89. discussion 87-9 10.1097/00005373-200008000-00002 [DOI] [PubMed] [Google Scholar]
- 10. Powell M, Courcoulas A, Gardner M, Lynch J, Harbrecht BG, Udekwu AO, Billiar TR, Federle M, Ferris J, Meza MP, et al. . Management of blunt splenic trauma: significant differences between adults and children. Surgery 1997;122:654–60. 10.1016/S0039-6060(97)90070-2 [DOI] [PubMed] [Google Scholar]
- 11. Federle MP, Jeffrey RB. Hemoperitoneum studied by computed tomography. Radiology 1983;148:187–92. 10.1148/radiology.148.1.6856833 [DOI] [PubMed] [Google Scholar]
- 12. Coccolini F, Montori G, Catena F, Kluger Y, Biffl W, Moore EE, Reva V, Bing C, Bala M, Fugazzola P, et al. . Splenic trauma: WSES classification and guidelines for adult and pediatric patients. World J Emerg Surg 2017;12:40 10.1186/s13017-017-0151-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bhullar IS, Frykberg ER, Siragusa D, Chesire D, Paul J, Tepas JJ, Kerwin AJ. Selective angiographic embolization of blunt splenic traumatic injuries in adults decreases failure rate of nonoperative management. J Trauma Acute Care Surg 2012;72:1127–34. 10.1097/TA.0b013e3182569849 [DOI] [PubMed] [Google Scholar]
- 14. Bhullar IS, Frykberg ER, Tepas JJ, Siragusa D, Loper T, Kerwin AJ. At first blush: absence of computed tomography contrast extravasation in grade IV or V adult blunt splenic trauma should not preclude angioembolization. J Trauma Acute Care Surg 2013;74:105–11. discussion 11-2 10.1097/TA.0b013e3182788cd2 [DOI] [PubMed] [Google Scholar]
- 15. Watson GA, Hoffman MK, Peitzman AB. Nonoperative management of blunt splenic injury: what is new? Eur J Trauma Emerg Surg 2015;41:219–28. 10.1007/s00068-015-0520-1 [DOI] [PubMed] [Google Scholar]
- 16. Bhangu A, Nepogodiev D, Lal N, Bowley DM. Meta-Analysis of predictive factors and outcomes for failure of non-operative management of blunt splenic trauma. Injury 2012;43:1337–46. 10.1016/j.injury.2011.09.010 [DOI] [PubMed] [Google Scholar]
- 17. Dolejs SC, Savage SA, Hartwell JL, Zarzaur BL. Overall splenectomy rates stable despite increasing usage of angiography in the management of high-grade blunt splenic injury. Ann Surg 2018;268:179–85. 10.1097/SLA.0000000000002246 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
tsaco-2019-000323supp001.pdf (59.8KB, pdf)
tsaco-2019-000323supp002.pdf (14.1KB, pdf)