Abstract
Using a concurrent mixed methods design, we investigated how knowledge, attitudes, values, and beliefs among women with osteoporosis can explain racial disparities in bone health. We recruited African American and White women ≥65 years of age with osteoporosis to participate in focus groups. We quantitatively compared scores of the “Osteoporosis & You” knowledge scale and each domain (internal, powerful others, and chance) of the Multidimensional Health Locus of Control scale by race using t-tests. We qualitatively explored potential racial differences in attitudes, values, and beliefs in the domains: 1) osteoporosis and bone health concerns, 2) knowledge about osteoporosis, 3) utilization of medical services for osteoporosis, 4) facilitators of osteoporosis prevention activities, and 5) barriers to osteoporosis prevention activities. A total of 48 women (White: 36; African American: 12) enrolled in the study. White women had a mean (SD) of 7.8 (0.92), whereas African American women score a 6.6 (2.6) (p=0.044) out of 10 on the Osteoporosis & You Scale. The powerful others domain was significantly higher among African American for both general and bone health [General Health - African American: 26.7 (5.9) vs. White: 22.3 (3.8); p=0.01]. Qualitative thematic analysis revealed differences by race in knowledge, types of physical activity, coping with comorbidities, physician trust, religion, and patient activation. Using both quantitative and qualitative methods, our study identified racial differences in knowledge, attitudes and beliefs in women with osteoporosis that could result in racial disparities in bone health, indicating the need to improve education and awareness about osteoporosis in African American women.
Keywords: Osteoporosis, Mixed-methods, Disparities, Epidemiology
Introduction
Osteoporosis is an age-related metabolic disease of the bone characterized by low bone mass and micro architectural changes which results in fragility of bone and causes bone fracture.[1] It has been estimated that 10-11 million adults 50+ years of age in the United States (US) have osteoporosis, and another 33-35 million have low bone mass.[2, 3] In the US, a women’s risk of hip fracture, the most adverse outcome of osteoporosis, is considered to be equal to that of breast cancer, ovarian cancer, and uterine cancer combined[4], and 20% of women who sustain a hip fracture related to osteoporosis die within the first year of their fracture.[1] Although the prevalence of osteoporosis is lower in African Americans than non-Hispanic Whites, the number of African Americans with osteoporosis and low bone mass is not trivial. Based on 2016 US Census data[5] and documented prevalence estimates,[2, 3] there are an estimated 200,000 African American women 65+ years of age with osteoporosis to nearly one million with low bone mass.
Previous studies have shown disparities in screening and treatment of osteoporosis in African American women. African-American women are 20-50% less likely to get screened, [6, 7] and African American women with osteoporosis are 5-20% less likely to receive treatment than their White counterparts.[8-10] Inequities in outcomes post osteoporotic fractures such as increased time to surgery, readmissions, surgical complications, and mortality have been reported.[11-13]
Reasons for disparities in osteoporosis screening and treatment offered by previous studies include: differences in disease awareness, social factors, physician factors, and presence of other severe comorbidities.[1] When comparing the level of awareness, only 25% of African American women were knowledgeable of the disease compared to 41% White women.[1] Another study found that African American women did not generally believe that they were at risk for developing osteoporosis, and prioritized other health conditions (such as breast cancer, heart disease, diabetes and Alzheimer’s disease) over bone health.[1]
The goal of this mixed methods study was to investigate patient-related factors focusing on knowledge, attitudes, values, and beliefs among women with osteoporosis that could be used to potentially explain disparities in the health care experience around bone health in older African American and White women.
Methods
We used a concurrent mixed methods design[14] to obtain complementary evidence from quantitative (survey) and qualitative (focus group discussion) data and to gain a more complete understanding of how patient-related factors can explain racial disparities in women’s bone health.
Setting
The study was conducted at The University of Alabama at Birmingham (UAB) Health System and was approved by the UAB Institutional Review Board (IRB). All participants reviewed and signed the informed consent document prior to study activities.
Recruitment
The UAB Health System physicians refer patients for osteoporosis screening, via dual energy X-ray absorptiometry (DXA) scanning, to The Kirklin Clinic (TKC) Osteoporosis Prevention and Treatment outpatient clinic. Prior to a DXA scan, patients complete a clinical questionnaire including demographic and comorbidity information used to compute the FRAX fracture risk prediction score.[15] The clinical questionnaire also asks patients if they are interested in participation in research studies at UAB with responses of “yes” or “no.” Per university IRB, a “yes” response allows researchers to contact patients regarding future research. DXA scan results and clinical questionnaire data are recorded and maintained in the clinic DXA database.
From this database, we identified African American and White women, ≥65 years of age with an osteoporosis diagnosis (T-score ≤−2.5) at the femoral neck or lumbar spine skeletal sites from scans performed between January 2011 and December 2015. We excluded women having a DXA order from a provider in Palliative Care, Hematology and Oncology, and Surgical Oncology, to identify potential participants with cancer and non-cancer related bone diseases. We also excluded patients living more than two hours (based on zip code) from Birmingham, AL as we considered distance as a barrier to focus group participation. Lastly, we excluded women with health conditions/status that would not make them good candidates for the study (e.g. frequent missing appointments, hearing issues, mobility issues, etc.) The study coordinator (MEM) reviewed the UAB Health System electronic health records to confirm study eligibility.
We then obtained the names, address, and phone numbers for identified potential participants. Using the US postal service, we mailed an invitation letter to introduce the focus group to women who expressed interest in future research and also met the study eligibility criteria (African American: 100; White: 500). Instructions in the letter asked recipients to call the study coordinator with interest to participate in a focus group. We made two attempts to reach persons through follow-up phone calls, and also mailed a second invitation letters following phone call attempts.
We also identified women who had a missing response for the “interest in future research” question (African American: 76) on the clinical questionnaire. Based on IRB review, we had approval to mail the invitation letter, but not place a follow-up phone call.
Lastly, to increase participation of African American women, we screened clinic schedules and asked for clinician referrals from the Osteoporosis Prevention and Treatment Clinic. For a period of three months, MEM reviewed the clinic schedule of four physicians using the UAB Health System electronic health records for eligible African American participants (DXA and medical history). Three UAB clinicians monitored their appointments and introduced the focus group to African American women that met all study inclusion criteria, and referred interested persons to the MEM for follow-up phone contact.
Study Procedures
The study was conducted between April 2016 and October 2016. The goal was to recruit a total of 40 women in each race group. We provided participants with food and beverages, and the participants were compensated for parking and $25 for their participation. Our mixed methods study consisted of quantitative assessment of osteoporosis knowledge and health locus of control followed by a qualitative exploration of knowledge, attitudes, values and beliefs based on five major domains described below.
Quantitative Data
Participants completed a self-administered demographic questionnaire that included the following items: general health, comorbidity assessment, concern about osteoporosis and hip fracture, and rating of fracture risk compared to women their age.
We also administered the “Osteoporosis and You”[16] questionnaire to determine osteoporosis knowledge (Appendix 1). Questions on this 10-point scale queried participants about height loss, risk of osteoporosis after menopause, family history as a predictor of osteoporosis, calcium and vitamin D rich foods, exercise and rate of bone loss, osteoporosis prevention, osteoporosis before broken bones, simple activities that may lead to a broken bone, osteoporotic bone loss, and health problems related to osteoporosis. Responses ranged from strongly disagree (1) to strongly agree (5). Based on scoring instructions, “strongly disagree,” “disagree,” or “neither disagree or agree” responses were given a score of “0” and “agree” and “strongly agree” scores were given a score of “1”. [16]
Lastly, we administered the Multidimensional Health Locus of Control (MHLC),[17] an 18-item scale that includes three mutually exclusive belief dimensions: internal, chance, and powerful others. (Appendix 2) The participants were asked to rate their responses to questions in each of these domains from strongly disagree (1) to strongly agree (6). The participants completed the questionnaire twice, once with reference to their overall health (Form A), and then again with reference to their bone health (Form B). Each response was given a score 1-6, with a max score of 36 per domain. In each domain, a higher score represents that this domain plays a higher role in health locus of control. For example, a higher score on the internal domain suggests that a person feels that they play a larger role in control of their health decisions; whereas, a lower score on the powerful others domain would indicate that other people do not play a large role in a person’s health decisions.
Qualitative data
The focus group discussion questions were based on the following domains: 1) osteoporosis and bone health concerns, 2) knowledge about osteoporosis, 3) utilization of medical services for osteoporosis, 4) facilitators to performing osteoporosis prevention activities (prescribed therapies, non-prescribed therapies, physical activity), and 5) barriers to doing the osteoporosis prevention activities. The discussion guide (Appendix 3) was used to facilitate the focus groups. We used focus group methodology to solicit responses from participants.[18] Focus groups were recorded and MEM also took notes.
Analysis
We compared descriptive statistics for the demographic variables by race using chi-squared tests. We calculated the “Osteoporosis and You” score out of 10 and compared by race. Given the missing data in Osteoporosis and You scale, we also calculated the percentage of correct responses and evaluated the percentage correct by race. Similarly, we calculated the mean scores of each domain of the MHLC questionnaire, and compared values by race using t-tests. All statistical analyses were performed using Stata v. 15.
The recorded focus groups interviews were transcribed verbatim by a professional transcription company and analyzed using an inductive thematic analysis. Constant comparative method was used to compare new information with the coded data and to guide the analytical process. Two investigators (NW and IH) met regularly to discuss the codes and emergent themes and to create a code-book that was used to inform each subsequent step in the analysis. Analysis was conducted using NVivo 10 Pro (QSR International).
Results:
Recruitment & Enrollment Results
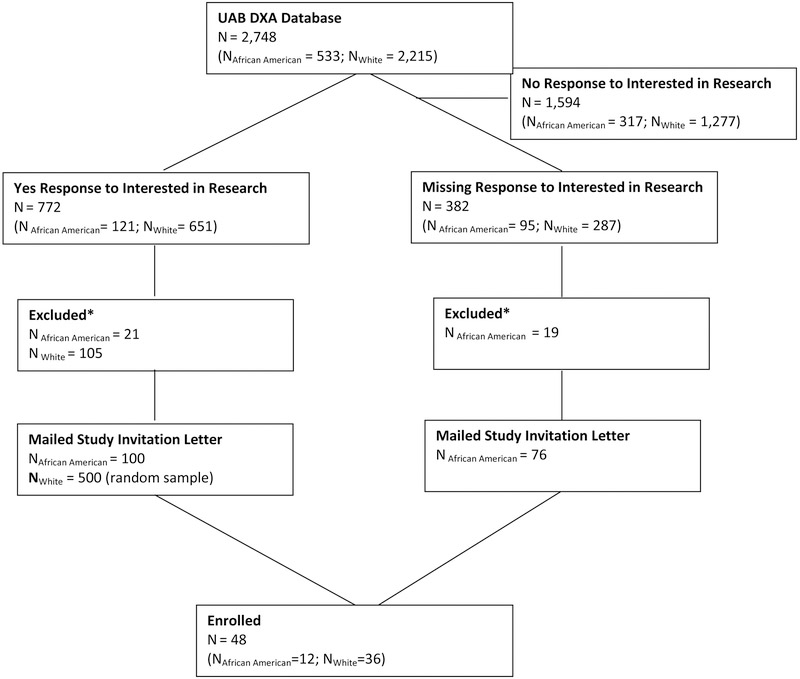
The UAB DXA database consisted of 2,748 African American and White women with DXA scans between 2011 and 2015. A total of 1,594 (58.0%) of the women were not interested in research, and were excluded from the study (Figure 1). Our eligible sample included the 772 (28.1%) (African American: 121 and White: 651 and) women who indicated they were interested in research participation and another 382 (13.9%) (African American: 95 and White: 287) who did not respond to the “interested in research” question. We excluded 21 (17.4%) of the African American women interested in research and we further excluded 19 (20%) of the African American women with missing research interest participation based on health status. Two physicians referred 14 patients, of which five (35.7%) reported having received the initial invitation letter in the mail.
Figure 1. Patient Enrollment Flowchart.
*Excluded based on history of heart failure, home bound, transplant, end stage renal disease, stroke, substance abuse, dementia, no diagnosis of OP, vision or hearing impairment, in a nursing care facility, no active appointment
A total of 48 women (African American: 12; White: 36) enrolled in the study, for an enrollment rate of 6.3% in African American and 7.2% in White women. We completed seven focus groups in the African American women and eight focus groups among the White women. There was no difference in age (p=0.69), with a mean (SD) age of 72.2 (7.5) in African American and 73.5 (10.0) years in White women (Table 1). We evaluated education at the population level using 2000 Census data. We found that 2 (16.7%) African American women lived in zip codes in which residents having less than high school education was >25%, compared to 0 (0.0%) of White women. Similarly, 2 (16.7%) African American women resided in zip codes in which <15% of residents had a high school diploma; whereas, no White women resided in those zip codes. Likewise, 2 (16.7%) of African American women resided in zip codes in which the proportion of residents had some college education was <25% compared to no White women. Only 1 (8.3%) African American woman resided in zip coded that had ≥50% of residents with bachelor’s or higher degrees compared to10 (27.8%) of White women. There was no difference in self-reported general health (p=0.33) or history of any of the co-morbidities assessed, with the exception of rheumatoid arthritis (RA). There was a larger proportion of RA in African American women compared to White women (30.0% vs. 3.1%; p=0.01) (Table 1). Concern about osteoporosis and hip fracture was similar between the two groups, and although not statistically different, a larger proportion of White women rated their risk of breaking a bone higher than other women their age than African American women (47.2% vs. 25.0%, p=0.16)
Table 1.
Demographic and Health Characteristics of the Sample by Race
| African American (n=12) |
White (n=36) |
p-value | |
|---|---|---|---|
| Age, mean (SD) | 72.2 (7.5) | 73.5 (10.0) | 0.69 |
| General Health, N (%) | 0.33 | ||
| Excellent | 0 (0.0) | 6 (16.7) | |
| Very Good | 6 (54.6) | 19 (52.8) | |
| Good | 3 (27.3) | 9 (25.0) | |
| Fair | 2 (18.2) | 2 (5.6) | |
| Poor | 0 (0.0) | 0 (0.0) | |
| History of Asthma, N (%) | 2 (16.7) | 4 (11.1) | 0.61 |
| History of Cancer, N (%) | 2 (16.7) | 4 (11.1) | 0.61 |
| History of Celiac’s Disease, N (%) | 0 (0.0) | 1 (2.8) | 0.56 |
| History of CKD, N (%) | 0 (0.0) | 1 (2.8) | 0.56 |
| History of Connective Tissue Disease, N (%) | 0 (0.0) | 1 (2.8) | 0.56 |
| History of Depression, N (%) | 2 (16.7) | 2 (5.6) | 0.23 |
| History of Type 1 Diabetes, N (%) | 1 (8.3) | 0 (0.0) | 0.08 |
| History of Type 2 Diabetes, N (%) | 1 (8.3) | 1 (2.8) | 0.40 |
| History of MI, N (%) | 0 (0.0) | 1 (2.8) | 0.56 |
| History of Heart Failure, N (%) | 0 (0.0) | 1 (2.8) | 0.56 |
| History of HTN, N (%) | 8 (66.7) | 14 (38.9) | 0.09 |
| History of High Cholesterol, N (%) | 5 (41.7) | 13 (36.1) | 0.73 |
| History of Liver Disease, N (%) | 1 (8.3) | 1 (2.8) | 0.40 |
| History of Multiple Sclerosis, N (%) | 0 (0.0) | 0 (0.0) | 1.0 |
| History of Osteoarthritis, N (%) | 4 (33.3) | 11 (30.6) | 0.86 |
| History of Peptic Ulcer Disease, N (%) | 0 (0.0) | 0 (0.0) | 1.0 |
| History of Rheumatoid Arthritis, N (%) | 3 (25.0) | 1 (2.8) | 0.02 |
| History of Stroke or TIA, N (%) | 1 (8.3) | 0 (0.0) | 0.08 |
| Are you concerned about: | |||
| Osteoporosis (Yes), N (%) | 8 (72.7) | 30 (85.7) | 0.32 |
| Hip Fracture (Yes), N (%) | 7 (70.0) | 24 (72.7) | 0.87 |
| Compared to other women your age, how would you rate your own risk of breaking a bone, N(%) | 0.25 | ||
| Much lower | 0 (0.0) | 1 (2.8) | |
| A little lower | 2 (16.7) | 8 (22.2) | |
| About the same | 7 (58.3) | 10 (27.8) | |
| A little higher | 1 (8.3) | 13 (36.1) | |
| Much higher | 2 (16.7) | 4 (11.1) |
Quantitative Results
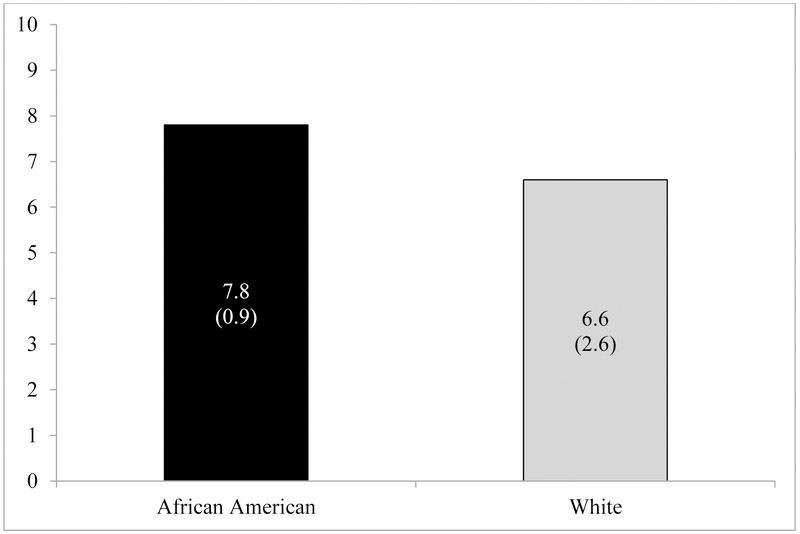
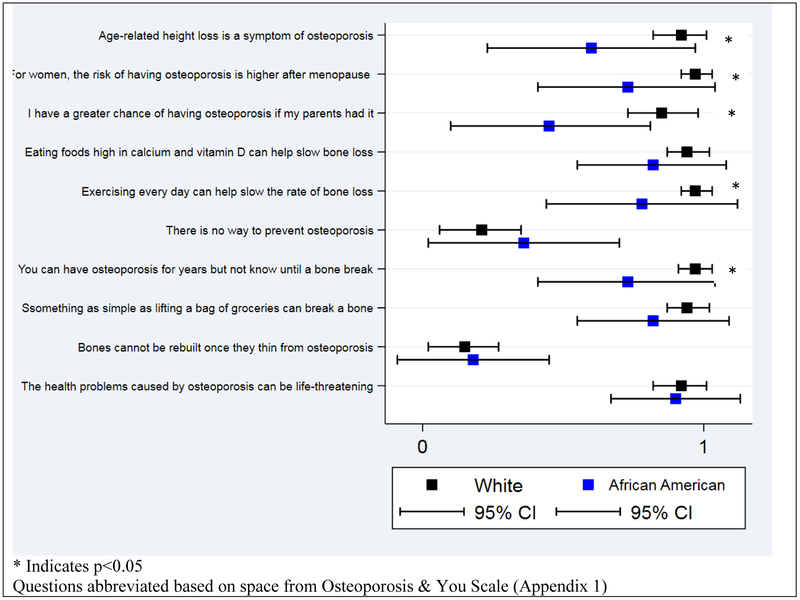
We observed lower knowledge about osteoporosis among African American women compared to their White counterparts. African American women had a mean (SD) score of 6.6 (2.6) out of 10 on the Osteoporosis & You Scale (Appendix 1), whereas, White women scored a mean (SD) of 7.8 (0.92)(p=0.044) (Figure 2A). When evaluating individual scores by question, Black women had statistically significant lower scores for questions 1, 2, 3, 5, and 7 (Figure 2B). When factoring in missing data and comparing a percentage correct, the African American women had a mean (SD) percent correct of 62.9% (22.2%) compared to 79.3% (10.1%) correct for the White women (p=0.012) (Figure 2C).
Figure 2 A-C. Osteoporosis Knowledge by Race.
A – Overall Score by Race: Score out of 10 (p = 0.044)
B - Individual Questions by Race**
C - Percent Correct by Race: Out of 100 (p = 0.012)
We also observed differences in the MHLC (Appendix 2A-B) by race. The internal and powerful others domains were significantly higher among African American women compared to White women (Table 2) when considering general health. However, only the powerful others domain remained significantly different between African American and White women when considering bone health (p-value = 0.011), with African American women having a mean (SD) of 26.7 (5.9) compared to 22.3 (3.8) in White women.
Table 2.
Multidimensional Health Locus of Control by Race
| African American |
White |
||
|---|---|---|---|
| Mean (SD) | Mean (SD) | p-value | |
| General Health | |||
| Internal | 27.2 (6.3) | 23.3 (4.8) | 0.041 |
| Powerful Others | 23.8 (6.0) | 18.5 (4.6) | 0.004 |
| Chance | 17.3 (7.0) | 15.8 (3.2) | 0.361 |
| Bone Health | |||
| Internal | 20.2 (6.3) | 21.7 (5.3) | 0.440 |
| Powerful Others | 26.7 (5.9) | 22.3 (3.8) | 0.011 |
| Chance | 14.3 (7.4) | 14.0 (4.6) | 0.892 |
Qualitative Results
Overall 10 themes emerged from our data including: getting information, talking about osteoporosis, reasons for testing, reactions to being diagnosed, treatment, knowledge of risk factors for osteoporosis, barriers to treatment adherence, barriers to being physically active, suggestions and other diseases. We reached saturation around these themes from our White participants even though we did not reach our target enrollment.
The comparison of themes and subthemes between the two race groups revealed specific differences in knowledge, types of physical activity, coping with comorbidities, physician trust, religion, and patient activation. First, it was clear that knowledge about osteoporosis was lower in African American women. For example with respect to DXA results, one of the African American participants said, “I never read mine. I just recently got a doctor maybe four years ago who sends me test results… [I] don’t really want them to tell me;” whereas, one of the White participants said, “They give an overall generic explanation. However, I researched and found the answers…”
Types of physical activity differed between the two groups. Both groups recognized the importance of walking on bone health, but White women recognized the importance of other strength based exercises as well. For example, one of our African American participants said “I don’t mind walking. I walk a lot. But 15 minutes of exercise, sit ups and all that, no,” compared to one of our White participants who said “…. My thing now, I get a good walk in, …because of my hip therapy, I have enjoyed the weights you can put on your shoes, I will do the little light weights, and the IT bands,… I have gotten hooked on those bands…”
Next, coping with co-morbidity was also different between the groups. We noted that osteoporosis was not the biggest concern when coping with more than one medical condition in African American women. For example, one of our African American participants said “So when you think about osteoporosis compared to maybe some of the other things that you may be dealing with health wise, does it take…is it a top priority? …I take three blood pressure pills, an antidepressant, and I take a vitamin pill, cod liver oil …I think that the blood pressure is the high priority to take because I don’t take a pill for the bones;” whereas, our White participants were highly knowledgeable and activated to perform positive bone health activities.
Trust in health care providers was a theme that emerged in African American women that did not emerge in our White participants. For example, an African American participant said “Well, I’m afraid to take half of it. I do basically what the doctor tells me because I understand that I don’t have the knowledge and all that, but I don’t think I need 70, 80 milligrams of anything. I’ve got to trust the person when I take it because I just don’t want to just take something and not know because I want to know that I’m getting better…”
Religion was another theme that was present in African American women that was not present in White women with osteoporosis. For example, one of our African American participants said…“Every morning …. I get my bible and read it I pray and I ask the Lord for protection. And I don’t need all this medicine, it makes me sick. He gonna take care of me. Y’all might think I’m crazy but that’s it.”
We found triangulation of the quantitative data for external locus of control results and qualitative themes related to trust of health care providers and religion. External locus of control was higher in African American than White women and our African American women expressed that trust was a key element needed between them and their health care professional, and faith and religion was something highly valued.
Discussion
The goal of our study was to see if and how race was associated with the attitudes, values and beliefs of women with osteoporosis using quantitative and qualitative methods. We found quantitatively that on a scale of 10 points, osteoporosis knowledge is 1.2 points, or 15.3%, lower in African American women compared to White women. Using a measure of locus of control related to health, we found that African American women had significantly higher mean scores in the “powerful others” domain in both general health and bone health, suggesting a higher externality of control related to health. Qualitatively, we also found knowledge about osteoporosis was lower; African American women were less activated by their diagnosis, particularly around taking prescribed or non-prescribed bone protective medications like calcium and vitamin D. African American women with osteoporosis also expressed that a level of trust and relationship building is needed in their health care provider, and religion was an important element to them; whereas these sentiments were not shared in their White counterparts with osteoporosis. Lastly, osteoporosis seemed to fall at a lower priority when dealing with multiple health conditions in African American women than in White women.
We used the Osteoporosis & You scale to assess the osteoporosis knowledge of our participations. This scale was also used in the Patient Activation after DXA Notification (PAADRN) study, a randomized-controlled trial assessing if a tailored DXA result notification letter versus standard of care improved guideline concordant medication usage, patient activation, calcium and vitamin D usage, and patient satisfaction.[19] In a sub-study, racial differences in a number of outcomes, including osteoporosis knowledge was assessed. [20] In 3,484 White women and 1,041 African American women from three sites in the US, the mean (SD) baseline osteoporosis knowledge in White and African American women was 8.2 (1.4) and 7.1 (1.8), which was statistically different (p<0.001).[20] The absolute difference 1.1 point is similar to the 1.2 point difference observed in our study although the PAADRN study participants were younger (mean age: African American: 66.4; White: 66.9).
Although not specifically using the Osteoporosis & You scale, others have found significant lack of awareness around osteoporosis in African American women compared to White women. [21] For example, Collins et al. found that 25% of African American women were familiar with osteoporosis compared to 41% of White women. [21] Our qualitative findings also showed lower osteoporosis knowledge in African American women compared to White women.
The use of a mixed methods approach allowed us to obtain corroborating evidence from the quantitative and qualitative results related to external locus of control, trust of health care providers, and religion between African American and White women. We found a higher external health locus of control (e.g. powerful others) in African American women with osteoporosis compared to White women. Racial differences in powerful other scores have previously been shown.[22] There have not been studies specifically examining MHLC in women with osteoporosis, but in patients with stroke, one study showed that Hispanic patients have higher scores in the powerful other domain than non-Hispanic White patients.[23]
Health care providers can serve as a “powerful other” for external control with respect to health care decision making. One of our participants commented that a solid relationship between the patient and provider is needed for them to comply with disease management. Again, there is little research specifically assessing physician trust in the women with osteoporosis, but this theme is not unique in the osteoporosis field. In work by Abrums, mistrust in a predominantly White-dominant health care system was prevalent in a study of working-class African American women.[24] Other studies in conditions such as diabetes,[25] cancer,[26, 27] and autoimmune diseases have found lack of physician trust was associated with adverse outcomes.[28] Similarly, religion or spirituality can be a “powerful other.” Our African American patients relied in faith and trust in God or their higher power for healing. Previous studies have shown African American older adults have higher religiosity scores than White older adults.[29] Again, studies in conditions such as heart disease [30] and dementia caregiving [31] have shown that higher scores on religion/spirituality scales had lower use of relevant medical services. This external control may prevent African American women in being more active in the bone health.
Lastly, qualitatively, it appeared that when coping with multiple health conditions, osteoporosis was lower on the priority list in our African American participants than our White participants. Our White women had more knowledge about skeletal health and were more proactive to prevent outcomes associated with poor skeletal health.
Our study is not without limitations. First, although recruitment rates were similar in both groups, our overall African American women sample size was small. Although our sample size was low, we found consistency in findings around knowledge with the large PAADRN cohort. Although we reached saturation from our White focus groups, the different qualitative themes that emerged were based on comments from one or two African American women. It is possible different themes could have emerged with a larger sample size. However, the themes that did emerge are consistent with disparities literature from other health conditions.
It is well known that educational attainment differs by race, particularly in the Deep South and among older adults, and that educational attainment is an important factor in health outcomes. Educational attainment is not systematically collected or recorded during routine clinical care, thus many clinical encounters and decisions occur without factoring in educational attainment and/or health literacy, another important construct for health outcomes. Although, we did not collect information on the education attainment of our participants individually, we evaluated education at a population level using Census data. We did observe racial differences in education with African American women having a larger proportion of residents from zip codes with low educational attainment and White women having higher proportions from zip codes with higher educational attainment. The purpose of our study was to evaluate racial differences in knowledge, attitudes, and beliefs about osteoporosis, and showing that there are indeed differences between African Americans and Whites further stresses that race is an important constructt in the development of osteoporosis educational materials as well as in the clinical management of osteoporosis.
Our study is one of the first contemporary studies to report on the racial differences in knowledge, and is one of the first to look at attitudes and beliefs in women with osteoporosis using both quantitative and qualitative methods. Our results clearly show that improvements in education and awareness about osteoporosis in African American women are necessary and may be a significant contribution to enriching osteoporosis quality of care in patients.
Acknowledgements:
We would like to thank the participants of this study. This study was supported by K12 HS023009 and a pilot project from the Deep South Resource Center for Minority Aging Research.
Appendix 1: Osteoporosis & You Questionnaire
Now we will ask some questions about your knowledge about osteoporosis and bone health. Beside each statement is a scale which ranges from strongly disagree (1) to strongly agree (5). For each item we would like you to circle the number that represents the extent to which you agree or disagree with that statement.
| Strongly Disagree |
Disagree | Neither Disagree nor Agree |
Agree | Strongly Agree |
|
|---|---|---|---|---|---|
| Age-related height loss is a symptom of osteoporosis | 1 | 2 | 3 | 4 | 5 |
| For women, the risk of having osteoporosis is higher after menopause | 1 | 2 | 3 | 4 | 5 |
| I have a greater chance of having osteoporosis if my mother or father has/had it | 1 | 2 | 3 | 4 | 5 |
| Eating foods high in calcium and vitamin D can help slow the rate of bone loss | 1 | 2 | 3 | 4 | 5 |
| Exercising every day can help slow the rate of bone loss | 1 | 2 | 3 | 4 | 5 |
| There is no way to prevent osteoporosis | 1 | 2 | 3 | 4 | 5 |
| A person may have osteoporosis for years but not know this until they break a bone | 1 | 2 | 3 | 4 | 5 |
| If a person has osteoporosis, something as simple as lifting a bag of groceries can break a bone | 1 | 2 | 3 | 4 | 5 |
| Bones cannot be rebuilt once they thin from osteoporosis | 1 | 2 | 3 | 4 | 5 |
| The health problems caused by osteoporosis can be life-threatening | 1 | 2 | 3 | 4 | 5 |
Appendix 2: Multidimensional Health Locus of Control Questionnaire
A – General Health
Each item below is a belief statement about your overall health with which you may agree or disagree. Beside each statement is a scale which ranges from strongly disagree (1) to strongly agree (6). For each item we would like you to circle the number that represents the extent to which you agree or disagree with that statement. The more you agree with a statement, the higher will be the number you circle. The more you disagree with a statement, the lower will be the number you circle. Please make sure that you answer EVERY ITEM and that you circle ONLY ONE number per item. This is a measure of your personal beliefs; there are no right or wrong answers.
| 1=STRONGLY DISAGREE (SD) 2=MODERATELY DISAGREE (MD) 3=SLIGHTLY DISAGREE (D) 4=SLIGHTLY AGREE (A) 5=MODERATELY AGREE (MA) 6=STRONGLY AGREE (SA) | |||||||
|---|---|---|---|---|---|---|---|
| SD | MD | D | A | MA | SA | ||
| 1 | If I get sick, it is my own behavior which determines how soon I get well again. | 1 | 2 | 3 | 4 | 5 | 6 |
| 2 | No matter what I do, if I am going to get sick, I will get sick. | 1 | 2 | 3 | 4 | 5 | 6 |
| 3 | Having regular contact with my physician is the best way for me to avoid illness. | 1 | 2 | 3 | 4 | 5 | 6 |
| 4 | Most things that affect my health happen to me by accident. | 1 | 2 | 3 | 4 | 5 | 6 |
| 5 | Whenever I don't feel well, I should consult a medically trained professional. | 1 | 2 | 3 | 4 | 5 | 6 |
| 6 | I am in control of my health. | 1 | 2 | 3 | 4 | 5 | 6 |
| 7 | My family has a lot to do with my becoming sick or staying healthy. | 1 | 2 | 3 | 4 | 5 | 6 |
| 8 | When I get sick, I am to blame. | 1 | 2 | 3 | 4 | 5 | 6 |
| 9 | Luck plays a big part in determining how soon I will recover from an illness. | 1 | 2 | 3 | 4 | 5 | 6 |
| 10 | Health professionals control my health. | 1 | 2 | 3 | 4 | 5 | 6 |
| 11 | My good health is largely a matter of good fortune. | 1 | 2 | 3 | 4 | 5 | 6 |
| 12 | The main thing which affects my health is what I myself do. | 1 | 2 | 3 | 4 | 5 | 6 |
| 13 | If I take care of myself, I can avoid illness. | 1 | 2 | 3 | 4 | 5 | 6 |
| 14 | Whenever I recover from an illness, it's usually because other people (for example, doctors, nurses, family, friends) have been taking good care of me. | 1 | 2 | 3 | 4 | 5 | 6 |
| 15 | No matter what I do, I 'm likely to get sick. | 1 | 2 | 3 | 4 | 5 | 6 |
| 16 | If it's meant to be, I will stay healthy. | 1 | 2 | 3 | 4 | 5 | 6 |
| 17 | If I take the right actions, I can stay healthy. | 1 | 2 | 3 | 4 | 5 | 6 |
| 18 | Regarding my health, I can only do what my doctor tells me to do. | 1 | 2 | 3 | 4 | 5 | 6 |
B – Bone Health
The next set of belief statements are about your bone health with which you may agree or disagree. Beside each statement is a scale which ranges from strongly disagree (1) to strongly agree (6). For each item we would like you to circle the number that represents the extent to which you agree or disagree with that statement. The more you agree with a statement, the higher will be the number you circle. The more you disagree with a statement, the lower will be the number you circle. Please make sure that you answer EVERY ITEM and that you circle ONLY ONE number per item. This is a measure of your personal beliefs; again, there are no right or wrong answers.
| 1=STRONGLY DISAGREE (SD) 2=MODERATELY DISAGREE (MD) 3=SLIGHTLY DISAGREE (D) 4=SLIGHTLY AGREE (A) 5=MODERATELY AGREE (MA) 6=STRONGLY AGREE (SA) | |||||||
|---|---|---|---|---|---|---|---|
| SD | MD | D | A | MA | SA | ||
| 1 | If my condition worsens, it is my own behavior which determines how soon I will feel better again. | 1 | 2 | 3 | 4 | 5 | 6 |
| 2 | As to my condition, what will be will be. | 1 | 2 | 3 | 4 | 5 | 6 |
| 3 | If I see my doctor regularly, I am less likely to have problems with my condition. | 1 | 2 | 3 | 4 | 5 | 6 |
| 4 | Most things that affect my condition happen to me by chance. | 1 | 2 | 3 | 4 | 5 | 6 |
| 5 | Whenever my condition worsens, I should consult a medically trained professional. | 1 | 2 | 3 | 4 | 5 | 6 |
| 6 | I am directly responsible for my condition getting better or worse. | 1 | 2 | 3 | 4 | 5 | 6 |
| 7 | Other people play a big role in whether my condition improves, stays the same, or gets worse. | 1 | 2 | 3 | 4 | 5 | 6 |
| 8 | Whatever goes wrong with my condition is my own fault. | 1 | 2 | 3 | 4 | 5 | 6 |
| 9 | Luck plays a big part in determining how my condition improves. | 1 | 2 | 3 | 4 | 5 | 6 |
| 10 | In order for my condition to improve, it is up to other people to see that the right things happen. | 1 | 2 | 3 | 4 | 5 | 6 |
| 11 | Whatever improvement occurs with my condition is largely a matter of good fortune. | 1 | 2 | 3 | 4 | 5 | 6 |
| 12 | The main thing which affects my condition is what I myself do. | 1 | 2 | 3 | 4 | 5 | 6 |
| 13 | I deserve the credit when my condition improves and the blame when it gets worse. | 1 | 2 | 3 | 4 | 5 | 6 |
| 14 | Following doctor's orders to the letter is the best way to keep my condition from getting any worse. | 1 | 2 | 3 | 4 | 5 | 6 |
| 15 | If my condition worsens, it's a matter of fate. | 1 | 2 | 3 | 4 | 5 | 6 |
| 16 | If I am lucky, my condition will get better. | 1 | 2 | 3 | 4 | 5 | 6 |
| 17 | If my condition takes a turn for the worse, it is because I have not been taking proper care of myself. | 1 | 2 | 3 | 4 | 5 | 6 |
| 18 | The type of help I receive from other people determines how soon my condition improves. | 1 | 2 | 3 | 4 | 5 | 6 |
Appendix 3: Discussion Guide
Q1 Were you concerned about your bone health before your bone density test?
- Q2. Did you get the results of your bone density test?
- Q2.1. Was there an explanation about the results?
- Q2.2. What did the results mean to you?
Q3. Does your primary care doctor regularly talk to you about your bone health?
Now we are going to talk about things that make it easier or harder for you to do things that help protect your bones. The two examples I will give are taking medications prescribed by your doctor and performing weight-bearing activities like walking fast outside or on a treadmill or climbing stairs.
Q4. What are some things that make it easier for you to do things that help protect your bones like take medications that are prescribed by your doctor?
Q5. What are some things that make it harder for you to that are prescribed by your doctor to protect your bone health?
Q6. What are some things that make it easier for you to do weight bearing activities to protect your bones?
Q7. What are some things that make it harder for you to do weight bearing activities to protect your bones?
Footnotes
Other Financial Conflict of Interests
NCW – Research: Amgen; Expert Witness: Pfizer; Honorarium: Columbia University Medical Center
MEM – Research: Amgen
MS – None
IH – None
SD – None
EBL – Research: Amgen; Advisory Boards: Amgen; Consultant: Novartis
KGS – research grant, consulting (Amgen, Mereo, Radius, Roche)
NVI - None
References
- 1.Thomas PA, Racial and ethnic differences in osteoporosis. J Am Acad Orthop Surg, 2007. 15 Suppl 1: p. S26–30. [DOI] [PubMed] [Google Scholar]
- 2.Looker AC, et al. , Trends in osteoporosis and low bone mass in older US adults, 2005-2006 through 2013-2014. Osteoporos Int, 2017. 28(6): p. 1979–1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wright NC, et al. , The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res, 2014. 29(11): p. 2520–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cauley JA, et al. , Incidence of fractures compared to cardiovascular disease and breast cancer: the Women's Health Initiative Observational Study. Osteoporos Int, 2008. 19(12): p. 1717–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Population 65 Years and Over in the United States 2016 American Community Survey 1-Year Estimates. 2016. [cited 2018 September 7]; Available from: https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_15_1YR_S0103&prodType=table.
- 6.Gillespie CW and Morin PE, Trends and Disparities in Osteoporosis Screening Among Women in the United States, 2008-2014. Am J Med, 2017. 130(3): p. 306–316. [DOI] [PubMed] [Google Scholar]
- 7.Neuner JM, et al. , Racial and socioeconomic disparities in bone density testing before and after hip fracture. J Gen Intern Med, 2007. 22(9): p. 1239–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Curtis JR, et al. , Population-based fracture risk assessment and osteoporosis treatment disparities by race and gender. J Gen Intern Med, 2009. 24(8): p. 956–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu SK, et al. , Quality of osteoporosis care of older Medicare recipients with fragility fractures: 2006 to 2010. J Am Geriatr Soc, 2013. 61(11): p. 1855–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Navarro RA, et al. , Minimizing disparities in osteoporosis care of minorities with an electronic medical record care plan. Clin Orthop Relat Res, 2011. 469(7): p. 1931–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dy CJ, et al. , Racial and Socioeconomic Disparities in Hip Fracture Care. J Bone Joint Surg Am, 2016. 98(10): p. 858–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacobsen SJ, et al. , Race and sex differences in mortality following fracture of the hip. Am J Public Health, 1992. 82(8): p. 1147–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lo JC, et al. , Trends in mortality following hip fracture in older women. Am J Manag Care, 2015. 21(3): p. e206–14. [PubMed] [Google Scholar]
- 14.Plano Clark VI, N. V, Mixed methods research: A guide to the field. 2016, Thousand Oaks, CA: Sage. [Google Scholar]
- 15.Kanis JA, et al. , FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int, 2008. 19(4): p. 385–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brenneman SK, B.E., Chen Y, Abbott TA, Validation of a patient questionnaire, "Osteoporosis and You', designed to assess osteoporosis-related attitudes, knowledge and behavior. J Bone Miner Res, 2002. 17 (Suppl 1). [Google Scholar]
- 17.Wallston KA, Wallston BS, and DeVellis R, Development of the Multidimensional Health Locus of Control (MHLC) Scales. Health Educ Monogr, 1978. 6(2): p. 160–70. [DOI] [PubMed] [Google Scholar]
- 18.Loeb S, Penrod J, and Hupcey J, Focus groups and older adults: Tactics for success. J Gerontol Nurs, 2006. 32(3): p. 32–8. [DOI] [PubMed] [Google Scholar]
- 19.Edmonds SW, et al. , The PAADRN study: a design for a randomized controlled practical clinical trial to improve bone health. Contemp Clin Trials, 2013. 34(1): p. 90–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cram P, et al. , Racial Differences and Disparities in Osteoporosis-related Bone Health: Results From the PAADRN Randomized Controlled Trial. Med Care, 2017. 55(6): p. 561–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Collins KS, S.C., Joseph S, et al. , Health Concerns Across a Woman's Lifespan: The Commonwealth Fund 1998 Survey of Women's Health. 1999, The Commonwealth Fund: New York, NY. [Google Scholar]
- 22.Wrightson KJ and Wardle J, Cultural variation in health locus of control. Ethn Health, 1997. 2(1-2): p. 13–20. [DOI] [PubMed] [Google Scholar]
- 23.Martinez M, et al. , Identification of Barriers to Stroke Awareness and Risk Factor Management Unique to Hispanics. Int J Environ Res Public Health, 2015. 13(1): p. ijerph13010023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abrums M, "Jesus will fix it after awhile": meanings and health. Soc Sci Med, 2000. 50(1): p. 89–105. [DOI] [PubMed] [Google Scholar]
- 25.Williams IC, et al. , The Role of Perceived Discrimination and Other Psychosocial Factors in Explaining Diabetes Distress Among Older African American and White Adults. J Appl Gerontol, 2018: p. 733464817750273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Do YK, et al. , Race, healthcare access and physician trust among prostate cancer patients. Cancer Causes Control, 2010. 21(1): p. 31–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sheppard VB, et al. , Reducing Racial Disparities in Breast Cancer Survivors' Ratings of Quality Cancer Care: The Enduring Impact of Trust. J Healthc Qual, 2016. 38(3): p. 143–63. [DOI] [PubMed] [Google Scholar]
- 28.Berrios-Rivera JP, et al. , Trust in physicians and elements of the medical interaction in patients with rheumatoid arthritis and systemic lupus erythematosus. Arthritis Rheum, 2006. 55(3): p. 385–93. [DOI] [PubMed] [Google Scholar]
- 29.Taylor RJ, Chatters LM, and Jackson JS, Religious and spiritual involvement among older african americans, Caribbean blacks, and non-Hispanic whites: findings from the national survey of american life. J Gerontol B Psychol Sci Soc Sci, 2007. 62(4): p. S238–50. [DOI] [PubMed] [Google Scholar]
- 30.Kressin NR, et al. , Racial differences in cardiac catheterization as a function of patients' beliefs. Am J Public Health, 2004. 94(12): p. 2091–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Merritt MM and McCallum TJ, Too much of a good thing?: Positive religious coping predicts worse diurnal salivary cortisol patterns for overwhelmed African American female dementia family caregivers. Am J Geriatr Psychiatry, 2013. 21(1): p. 46–56. [DOI] [PMC free article] [PubMed] [Google Scholar]