Abstract
Background
Herlyn–Werner–Wunderlich syndrome is an uncommon entity characterized by uterus didelphys, obstructed hemivagina and ipsilateral renal agenesis (also called OHVIRA syndrome). Due to rarity and varied presentations, often correct diagnosis is missed out during work up, leading to management problems. We describe our dependence on detailed preoperative work up and minimally invasive endoscopic approach in management of the eight patients of OHVIRA syndrome.
Methods
In this retrospective case series study, eight patients of OHVIRA syndrome were managed from January 2012 to March 2018 with the help of improved imaging facility and diagnostic work up. Precise diagnosis helped in adopting minimally invasive approach in management. Patients were reviewed, focusing on presentation, radiologic findings and surgical management.
Results
Median age at diagnosis was 19 years (range 13–41 years). Abdominal pain and dysmenorrhea were the main presenting complaint. All patients except one had associated ipsilateral renal agenesis. Surgical excision of the obstructed hemivaginal septum and hematometra drainage was the main treatment. In seven patients, vaginoscopic resection of vaginal septum was done with resectoscope except one 41-year-old patient, where resection of vaginal septum was performed laparoscopically along with hysterectomy.
Conclusion
Vaginoscopic resection of obstructed hemivaginal septum is an effective method. Management has shifted to minimally invasive approach due to improved imaging, precise preoperative diagnosis and proper understanding of the disease.
Keywords: OHVIRA syndrome, Minimally invasive, Vaginoscopy, Laparoscopy, Hematometra
Introduction
Purslow in 1922 first described OHVIRA syndrome (obstructed hemivagina and ipsilateral renal anomaly), also named as Herlyn–Werner–Wunderlich syndrome [1]. It is a rare Mullerian anomaly. Early detection and surgical drainage of hematocolpos and hematometra relieves symptoms, prevents complications and adverse fertility outcome [2]. Lack of proper pre-op diagnosis leads to delay in diagnosis. With proper understanding of disease, unnecessary laparotomies can be avoided [3]. The purpose of this case series is to promote early recognition of this rare urogenital anomaly. Improved imaging and timely preoperative diagnosis also help in managing this uncommon entity with minimally invasive approach and preventing complications like hematosalpinx, endometriosis from retrograde flow of menstrual blood, pelvic adhesions and later infertility.
Materials and Methods
In this study, eight patients with uterine didelphys with obstructed hemivagina with or without ipsilateral renal agenesis were reviewed (Table 1). It is a retrospective analysis of existing data. The included patients had a median age of 19 years (range 13–41 years). The youngest age of presentation was 13 years, and the oldest was 41 years. Abdominal pain and dysmenorrhea were the main presenting complaints in all the eight patients. Out of these, three patients presented at onset of menarche and four patients came few years later. A 13-year-old patient in this study also observed abdominal mass due to progressive menstrual blood accumulation. Ultrasound imaging of this case showed uterine didelphys, large left hematometra, hematosalpinx and endometriotic cyst along with hematocolpos. One patient in our series remained undiagnosed till 41 years of age. This is an unusual finding as most of these patients usually present within a few years of onset of menses. Two patients of the study had also undergone unsuccessful surgical attempts in the past in which hematocolpos could not be drained, and patient were referred to us.
Table 1.
Details of the study cases
| Case | Age (years) | Complaint | Mullerian anomaly | Imaging modality | Management |
|---|---|---|---|---|---|
| 1 | 13 | Severe dysmenorrhea, pain abdomen and mass per abdomen | Uterus didelphys with obstructed left hemivagina with hematocolpos, hematometra, hematosalpinx with left endometriotic cyst with bilateral normal kidneys | Ultrasound, MRI abdomen and pelvis | Laparoscopic left endometriotic cystectomy + vaginoscopic vaginal septum resection |
| 2 | 15 | Severe dysmenorrhea, pain abdomen | Uterus didelphys left hematometra, hematocolpos with absent left kidney | Ultrasound, MRI abdomen and pelvis | Laparoscopy + vaginoscopic vaginal septum resection |
| 3 | 17 | Severe dysmenorrhea, pain abdomen | Uterus didelphys left hematocolpos left hematometra with absent left kidney | Ultrasound, MRI abdomen and pelvis | Laparoscopic endometriotic spot fulguration + vaginoscopic vaginal septum resection |
| 4 | 17 | Severe dysmenorrhea, pain abdomen | Uterus didelphys right hematocolpos right hematometra with absent right kidney | Ultrasound, MRI abdomen and pelvis | Laparoscopy + vaginoscopic vaginal septum resection |
| 5 | 19 | Severe dysmenorrhea, pain abdomen | Uterus didelphys right hematocolpos right hematometra with absent right kidney | Ultrasound, MRI abdomen and pelvis | Laparoscopic endometriotic spot fulguration + adhesiolysis + vaginoscopic vaginal septum resection |
| 6 | 20 | Severe dysmenorrhea, pain abdomen | Uterus didelphys right hematocolpos, right hematometra, right hematosalpinx with absent right kidney | Ultrasound, MRI abdomen and pelvis | Diagnostic laparoscopy + hematosalpinx drainage + vaginoscopic vaginal septum resection |
| 7 | 22 | Severe dysmenorrhea, pain abdomen | Uterus didelphys right hematocolpos with right kidney absent | Ultrasound, MRI abdomen and pelvis | Laparoscopy + vaginoscopic vaginal septum resection |
| 8 | 41 | Severe dysmenorrhea, pain abdomen | Uterus didelphys left hematocolpos left hematometra with absent left kidney | Ultrasound abdomen and pelvis | Total laparoscopic hysterectomy + hematocolpos drainage + laparoscopic vaginal septum resection |
All patients underwent physical, abdominal and vaginal examination, and the most significant finding was a bulge of hematocolpos in the lateral vaginal wall due to obstructed hemivagina by an oblique vaginal septum. But, in some cases, fullness with no vaginal bulge may be observed when collection of hematocolpos is high up and more lateral or when patient presents at very early stage when significant hematocolpos has not yet developed. These patients would have remained undiagnosed with normal menstrual cycle with no vaginal bulge on examination if further work in the form of imaging studies was not done. Ultrasound and/or MRI abdomen and pelvis (Fig. 1a, b) was used to identify uterine didelphys with one-sided hematocolpos with or without hematometra, endometriotic cyst and associated renal anomaly. All patients except one had hematometra, and two patients also had associated hematosalpinx. In this series, seven cases had ipsilateral renal agenesis and one patient had no associated renal anomaly. None of the patients had other variants of` renal anomalies in the study.
Fig. 1.
a MRI showing left hematocolpos and hematometra and right uterine horn (Hm hematometra, Hc hematocolpos, U normal uterine horn, B bladder). b MRI showing left hematocolpos and hematometra (Hm hematometra, Hc hematocolpos, B bladder)
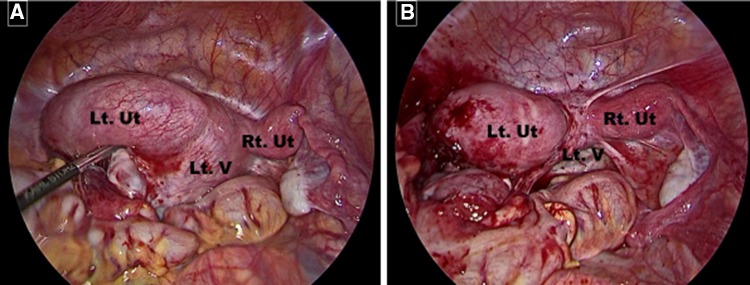
Surgical procedures Detailed written informed consent was obtained, and patient was planned for elective surgery. After giving general anaesthesia, laparoscopy (Fig. 2a, b) was done in all cases to diagnose and treat endometriosis and hematosalpinx drainage if required in same sitting. Bulge was observed on the side of hematocolpos, and ipsilateral uterus was found to be larger due to hematometra. Two cases also showed a large dilated hematosalpinx. In cases where endometriosis was seen, endometriotic cystectomy and endometriotic spot fulguration were done in the same sitting. Then, vaginal examination was done under anaesthesia, in which one cervix was identified with the vaginal bulge on one side of vagina where hematocolpos was present. In seven patients, hysteroscopic resectoscope (26Fr, Karl Storz) with Collins knife was used. Vaginoscopy was done (labia occluded for vaginal distension and proper visualization), cervical opening of normal uterus was identified and bulge on the vaginal wall of the side of hematocolpos was identified. With the help of resectoscope, a vertical incision was given on most prominent part of bulge, hematocolpos and hematometra were drained (Fig. 3a, b). After draining the collection, rest of the vaginal septum was excised with the resectoscope completely and cervix of the other uterine horn was identified. Vaginoscopy leads to better visualization of anomaly, and use of resectoscope helped in achieving good hemostasis. Concomitant hysteroscopy and cervical dilatation were not done as hematometra and hematosalpinx were seen draining in the same sitting. In one case, where spontaneous drainage of hematosalpinx was not observed, laparoscopic drainage of hematosalpinx was done by separating agglutinated fimbria.
Fig. 2.
a Laparoscopic view showing left hematocolpos, left hematometra and normal right uterine horn (Lt. Ut. left uterine horn with hematometra, Lt. V left obstructed vagina with hematocolpos, Rt. Ut right normal uterine horn). b Laparoscopic view post drainage of left hematometra and hematocolpos after vaginoscopic septum resection (Lt. Ut. left uterine horn, Lt. V left vagina, Rt. Ut right normal uterine horn)
Fig. 3.
a Vaginoscopic view showing drainage of left hematocolpos following left hemivaginal septum resection (Rt Cx right cervix). b vaginoscopic view showing resected left hemivaginal septum both cervical opening (Rt Cx right cervix, Lt Cx left cervix, S resected left hemivaginal septum)
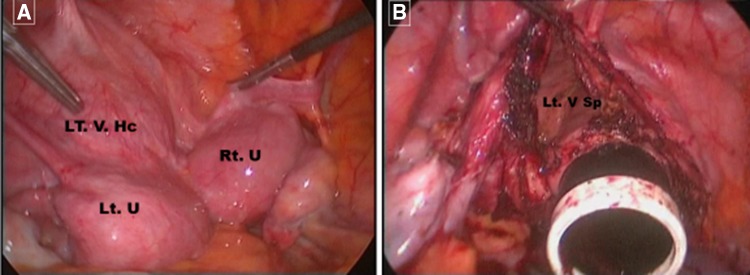
A patient presented at 41 years of age with severe dysmenorrhea. She was suspected to have vague ischiorectal collection. Since she was menstruating, hematocolpos was not suspected. She got married and also underwent caesarean section and still remained undiagnosed. She consulted many doctors for her excruciating abdominal pain and dysmenorrhea who prescribed her oral and injectable NSAIDs for pain relief. Later on, she consulted a psychiatrist and was diagnosed with depression and was started on antidepressants. She was planned for total laparoscopic hysterectomy and intraoperatively diagnosed to have uterine didelphys with hematocolpos with obstructed hemivagina (Fig. 4a, b). After completing the procedure, vaginal septum was excised laparoscopically with monopolar hook cautery followed by vault closure.
Fig. 4.
a Laparoscopic view of uterine didelphys with left obstructed hemivagina with left hematocolpos (Lt. V. Hc left hemivaginal hematocolpos, Lt. U left uterine horn, Rt. U right uterine horn). b laparoscopic view of left hemivaginal septum with patent right hemivagina after drainage of hematocolpos laparoscopically. (Lt. V Sp left hemivaginal septum)
None of the eight patients required any additional post-operative analgesia emphasizing the benefits of minimally invasive approach. Moreover, bladder catheter was removed after 6 h and all the patients were discharged on the very next day.
One patient who had small right-sided hematocolpos high up with no hematometra intraoperatively came with recurrence of dysmenorrhea 3 months’ post-surgery. Ultrasound was done which showed hematocolpos with hematometra. She underwent repeat surgery for the same and is now asymptomatic. Therefore, long-term follow-up of these patients in future is needed to determine the true outcome.
Discussion
The exact incidence of OHVIRA syndrome is unknown. In few studies, reported incidence of uterine didelphys with obstructed hemivagina is approximately 1 in 2000 to 1 in 28,000 [4]. Its association with unilateral renal agenesis is seen in majority of cases [4].
The OHVIRA syndrome results from anomalous development of both the Mullerian and the Wolffian ducts [5]. On the side where the Wolffian duct is absent, Mullerian duct is displaced laterally and fails to fuse with the contralateral Mullerian duct leading to uterine didelphys [6]. The displaced Mullerian duct leads to an obstructed hemivagina as it cannot come in contact with urogenital sinus and contralateral Mullerian duct which fuses with urogenital sinus normally leads to development of vagina [6]. The distal part of vagina which arises from the urogenital sinus develops normally.
Maldevelopment of the mesonephric and paramesonephric ducts is usually associated with renal and urinary tract anomalies [7]. The most common renal anomaly in OHVIRA syndrome is renal agenesis, and other anomalies are renal ectopy, cystic renal dysplasia and double ureters [8]. However, seven patients in the present study had absent ipsilateral kidney with none having other renal anomalies. Evaluation of renal system should be done in all patients before surgery.
Patient usually presents few months after onset of menses with cyclic abdominal pain, dysmenorrhea and palpable pelvic mass due to collection of blood in half of vagina, uterus and tubes. It may remain undetected in many patients as unobstructed part of vagina leads to normal menses but they have associated severe dysmenorrhea due to obstruction on contralateral side [9]. Prescription of NSAIDs and oral contraceptive pills may further delay the diagnosis. These patients may have some relief of symptoms with these drugs and if further imaging is not done, this syndrome may remain undiagnosed for years. Unawareness in the part of treating gynaecologist may also lead to unnecessary laparotomies [3].
If this entity is not kept in mind, even after proper imaging, diagnosis can be missed. This was seen in one of the patients in this study who underwent caesarean section and still remained undiagnosed. In a case report by Ahmad et al., 22-year-old female evaluated for primary infertility with ultrasound pelvis showing left endometriotic cyst with uterine didelphys underwent laparotomy, adhesiolysis and left ovarian cystectomy. Later on when she had 3 months of amenorrhea with urine pregnancy test negative, she underwent MRI abdomen–pelvis for further evaluation and was diagnosed with OHVIRA syndrome for which she underwent vaginal resection of the obstructed hemivaginal septum after 3 months [3].
Often correct diagnosis is difficult during work up due to varied presentation, leading to management problems. Endometriosis and infertility may also develop later on due to backflow of menses and this can be prevented by early diagnosis of the disease with proper imaging studies [10]. Better imaging in the form of ultrasound and MRI had made the exact diagnosis possible. Ultrasound is cheap and readily available. Ultrasound may reveal two uterine cavities with collection in one due to hematometra and hematometra. A well-defined, unilocular or multilocular, cystic masses containing diffuse, homogeneous, low-level internal echoes may be seen in associated endometriosis [6]. As ultrasound is investigator-dependent, diagnosis may be missed. In doubtful cases, MRI is superior to ultrasonography, which helps in locating the exact site of obstruction and associated renal anomaly [11]. Laparoscopy at the time of surgery will reconfirm the exact diagnosis and help to treat associated endometriosis, adhesions and drain hematosalpinx in the same sitting. But endometriosis does require follow-up and may require repeated surgery in future.
Early detection and management leads of this uncommon Mullerian anomaly lead to a good prognosis [12] and prevent [3] long-term complication like hematosalpinx, endometriosis from back flow of menstrual blood, pelvic adhesions, pyocolpos, pyosalpinx, hydronephrosis and later infertility [13].
Treatment includes incision of obstructing hemivaginal septum and drainage of the hematocolpos and hematometra. [14]. In our series, all cases were operated successfully as a single step procedure which is patient friendly. Some studies have described two stage procedures which involve draining the haematocolpos and excising the rest of the septum tissue after a period of wound healing and vaginal remodelling in cases of anatomical distortion preventing satisfactory assessment of the vagina. Precise preoperative diagnosis helped in single sitting minimally invasive vaginoscopic approach and good outcome. Some difficulty may be encountered in previously operated patients and those with small hematocolpos high up in vagina. A case series of four patients by Ludwin et al. [15] introduced a unique concept of hymen-sparing management with the use of transrectal ultrasound-guided vaginoscopic septoplasty.
The patient should be followed up for prevention of the complications like dyspareunia, vaginal stenosis and recurrence of obstruction. Infertility is not very frequent in these patients [16]. One patient of this study who was diagnosed at 41 years of age had normal obstetric outcome. Obstetric complications are rare, but patient may have prematurity, foetal growth retardation necessitating good antenatal care [16].
OHVIRA syndrome is a rare entity, and most studies are the random case reports and case series. A recent study by Uribe et al. in 2019 is a retrospective analysis of nine women with OHVIRA syndrome in a 20-year period. Right side anomaly was observed in about half of the patients. Patients presented with symptoms like dysmenorrhea (44%), recurrent abdominal pain (22%) and urinary dysfunction (22%) and complications included hematocolpos and pyocolpos. Septal resection (44%) was performed in only post-pubertal patients [17].
Conclusion: Early diagnosis and treatment of OHVIRA syndrome is essential for symptomatic relief and prevention of long-term adverse effects. Long-term follow-up in younger patient is also mandatory. The preferred treatment modality is the minimally invasive vaginoscopic resection of the obstructed hemivaginal septum.
Alka Kriplani
is a consultant and head of Department of Minimally Invasive Gynecology, Obstetrics and ART in Paras Hospitals, Gurgaon. She is a former professor and head of department of obstetrics and gynaecology in All India Institute of Medical Sciences, New Delhi. She has special interest in gynaecology laparoscopic surgeries.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Standards
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent
Informed consent was obtained from patient for being included in the study.
Footnotes
Dr. Alka kriplani, M.D. Obstetrics and Gynaecology, Consultant at Paras Hospital, Gurgaon. She was a former professor and head of department of obstetrics and gynaecology, AIIMS, New Delhi. Dr. Venus Dalal, M.D. Obstetrics and gynaecology, Consultant at Mahendru Hospital, New Delhi (former senior resident, AIIMS). Dr. Garima Kachhawa, M.D. Obstetrics and gynaecology, Associate professor at Obstetrics and Gynaecology department, AIIMS, New Delhi. Dr. Reeta Mahey, M.D. Obstetrics and Gynaecology, Associate professor at Obstetrics and gynaecology department, AIIMS, New Delhi. Dr. Vikas Yadav, M.D. Obstetrics and Gynaecology, Senior resident at Obstetrics and Gynaecology Department, AIIMS, New Delhi. Dr. Isha Kriplani, M.D. Obstetrics and Gynaecology, Senior resident at Obstetrics and Gynaecology Department, AIIMS, New Delhi.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Schlomer B, Rodriguez E, Baskin L. Obstructed hemivagina and ipsilateral renal agenesis (OHVIRA) syndrome should be redefined as ipsilateral renal anomalies: cases of symptomatic atrophic and dysplastic kidney with ectopic ureter to obstructed hemivagina. J Pediatr Urol. 2015;11(2):77.e1–77.e6. doi: 10.1016/j.jpurol.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Tong J, Zhu L, Lang J. Clinical characteristics of 70 patients with Herlyn–Werner–Wunderlich syndrome. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet. 2013;121(2):173–175. doi: 10.1016/j.ijgo.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 3.Ahmad Z, Goyal A, Das CJ, et al. Herlyn–Werner–Wunderlich syndrome presenting with infertility: role of MRI in diagnosis. Indian J Radiol Imaging. 2013;23(3):243–246. doi: 10.4103/0971-3026.120283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Del Vescovo R, Battisti S, Di Paola V, et al. Herlyn–Werner–Wunderlich syndrome: MRI findings, radiological guide (two cases and literature review), and differential diagnosis. BMC Med Imaging. 2012;9(12):4. doi: 10.1186/1471-2342-12-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gungor Ugurlucan F, Bastu E, Gulsen G, et al. OHVIRA syndrome presenting with acute abdomen: a case report and review of the literature. Clin Imaging. 2014;38(3):357–359. doi: 10.1016/j.clinimag.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 6.Mishra N, Ng S. Sonographic diagnosis of obstructed hemivagina and ipsilateral renal anomaly syndrome: a report of two cases. Australas J Ultrasound Med. 2014;17(4):153–158. doi: 10.1002/j.2205-0140.2014.tb00238.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haddad B, Barranger E, Paniel BJ. Blind hemivagina: long-term follow-up and reproductive performance in 42 cases. Hum Reprod Oxf Engl. 1999;14(8):1962–1964. doi: 10.1093/humrep/14.8.1962. [DOI] [PubMed] [Google Scholar]
- 8.Fedele L, Bianchi S, Agnoli B, et al. Urinary tract anomalies associated with unicornuate uterus. J Urol. 1996;155(3):847–848. doi: 10.1016/S0022-5347(01)66323-7. [DOI] [PubMed] [Google Scholar]
- 9.Mandava A, Prabhakar RR, Smitha S. OHVIRA syndrome (obstructed hemivagina and ipsilateral renal anomaly) with uterus didelphys, an unusual presentation. J Pediatr Adolesc Gynecol. 2012;25(2):e23–e25. doi: 10.1016/j.jpag.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 10.Vercellini P, Daguati R, Somigliana E, et al. Asymmetric lateral distribution of obstructed hemivagina and renal agenesis in women with uterus didelphys: institutional case series and a systematic literature review. Fertil Steril. 2007;87(4):719–724. doi: 10.1016/j.fertnstert.2007.01.173. [DOI] [PubMed] [Google Scholar]
- 11.Troiano RN, McCarthy SM. Mullerian duct anomalies: imaging and clinical issues. Radiology. 2004;233(1):19–34. doi: 10.1148/radiol.2331020777. [DOI] [PubMed] [Google Scholar]
- 12.Dhar H, Razek YA, Hamdi I. Uterus didelphys with obstructed right hemivagina, ipsilateral renal agenesis and right pyocolpos: a case report. Oman Med J. 2011;26(6):447–450. doi: 10.5001/omj.2011.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu W-C, Chang W-C, Yeh L-S, et al. Didelphic uterus and obstructive hemivagina with ipsilateral renal agenesis complicated by pyocolpos. J Obstet Gynecol. 2007;46(3):295–298. doi: 10.1016/S1028-4559(08)60040-6. [DOI] [PubMed] [Google Scholar]
- 14.Smith NA, Laufer MR. Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome: management and follow-up. Fertil Steril. 2007;87(4):918–922. doi: 10.1016/j.fertnstert.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 15.Ludwin A, Ludwin I, Bhagavath B, et al. Virginity-sparing management of blind hemivagina in obstructed hemivagina and ipsilateral renal anomaly syndrome. Fertil Steril. 2018;110(5):976–978. doi: 10.1016/j.fertnstert.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 16.Heinonen PK. Clinical implications of the didelphic uterus: long-term follow-up of 49 cases. Eur J Obstet Gynecol Reprod Biol. 2000;91(2):183–190. doi: 10.1016/S0301-2115(99)00259-6. [DOI] [PubMed] [Google Scholar]
- 17.[Clinical characteristics and complications in patients with OHVIRA (obstructed hemivagina and ipsilateral renal anomaly) syndrome. Our experience]. PubMed–NCBI [Internet]. [cited 2019 Mar 19]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/?term=Cir+Pediatr.+2019+Jan+21%3B32(1)%3A11-16. [PubMed]