Abstract
Objective
Construction of reference centile chart of middle cerebral (MCA) and umbilical artery (UA) Doppler along with cerebroplacental ratio from 24 to 40 weeks gestation in Indian population.
Method
It was a cross-sectional observational study; antenatal women between 24 and 40 weeks gestation underwent the MCA and UA Doppler. The centile charts for MCA, UA and cerebroplacental ratio (CPR) were derived.
Results
Total 300 antenatal women were included; the MCA PI, RI, S/D ratio values showed a parabolic curve with the peak at 33–35 weeks; the umbilical artery Doppler and cerebroplacental ratio showed a linear decrease with increasing gestational age. The regression analysis showed a weak correlation between the Doppler parameters and the gestational age. The MOM values of all Doppler parameters, across the gestational age, were also derived.
Conclusion
The constructed MCA, UA and CPR charts along with their MOM values could be used as reference for the regional population.
Keywords: Cerebroplacental ratio, Second trimester Doppler, Third trimester Doppler, MOM
Introduction
The fetal cerebral blood flow evaluation has become an essential part of the assessment of high-risk pregnancies. The middle cerebral artery (MCA) Doppler findings are incorporated regularly into the management of fetuses at risk of developing placental insufficiency and fetal anemia [1–3]. It has been a routine practice to use UA-pulsatality index (PI) and MCA PI to distinguish between constitutionally small babies and growth-restricted ones, and it has been found to be supportive in deciding the best time, place and mode of delivery [1, 2].
The alterations in the UA Doppler flow either may lead to or might be the cause of feto-placental insufficiency; however, the fetal cerebral blood flow is found to increase, as a compensatory mechanism to sustained fetal hypoxia. Therefore, it is believed that the cerebroplacental ratio (CPR) measures the cardiac output redistribution from representative cerebral and feto-placental vessels from the cause to the affect and is evolving as an important parameter in the assessment of fetal well-being in early and late FGR [3, 4]. There is evidence from the previous studies that the Doppler parameters differ with race and ethnicity [5–7]. It is therefore recommended that the data from regional population should be available to be used as reference in clinical practice.
The study was done with the aim of constructing the reference centile chart of Doppler values of middle cerebral, umbilical artery and CPR from 24 to 40 weeks of gestation in Indian population.
Materials and Methods
It was an observational cross-sectional study, conducted from November 2015 to December 2017, after clearance from the institutional ethical committee. The sample size was derived taking the power of the study as 95% and significance of 5% using the formulae N = Zα*s 2/d2, where N sample size, Zα – Z value of α at 5%, s standard deviation and d 5% of mean. The sample size of 300 pregnant women was calculated. Antenatal women between 24 and 40 weeks gestation were selected, established on the basis of their last menstrual period or early ultrasound scan. The informed consent of the subjects was taken before inclusion in the study. Women with known congenital anomaly, fetal growth restriction, multiple pregnancy and having medical disorders like hypertension, diabetes and renal disease were excluded.
Selected subjects underwent transabdominal grayscale and Doppler ultrasound (Toshiba Nemio XG, Japan, 3–5 MHz probe). Axial section of the head was visualized on grayscale ultrasound (US); the axial section below the level of the thalamus showing the base of the skull was obtained. Using the color mode, the fetal MCA was localized arising anterolateral from the circle of Willis. The pulse Doppler was used to sample the MCA just after its origin from the circle of Willis, keeping the angle of insonation at nearly zero degrees. The umbilical artery Doppler velocimetry assessment was done in the free loop portion of the cord away from cord insertion. The Doppler parameters were recorded 3 times in each woman, and the mean of 3 measurements was taken; all scans were done by the single observer. The intra-observer reliability using Cronbach’s alpha score showed good level of agreement (values ranging between 0.9 13 and 0.978).
The women with normal outcome and adequate for gestational age babies were included in the study. The percentiles (5th, 50th and 95th) were established by SPSS software for the two weekly gestational age ranges starting from 24 to 40 weeks. There were exactly 95% observations between 1.645σ limits, and hence, these points acted as the 5th and 95th percentiles, and reference charts were constructed. The regression analysis was done using gestational age as the independent variable and the Doppler parameters as dependent variable. Pearson’s coefficient correlation was derived. The MOM values for the 5th and 95th centile of each Doppler value were calculated. For the centile chart of CPR, the 5th and 95th centile of each individual MCA PI/UA PI was taken. The SPSS version 19 software was used for statistical analysis. P value of ≤ 0.05 was taken as significant.
Results
The mean age of women in the study was 24.9 (18–38, ± 3.1) years; 161(53.7%) cases were primiparous. The period of gestation ranged from 24 to 40 weeks of gestation.
Table 1 shows the reference range from 24 to 40 weeks gestation for MCA PI, S/D, RI values. All Doppler indices demonstrated a parabolic pattern of peak at 33–35 weeks gestation. The regression equation for MCA Doppler values was given as:
MCA PI = 0.0049x gestational age + 1.194 with R2 = 0.00275
MCA RI = 0.0044x gestational age + 0.5165 with R2 = 0.01091
MCA S/D = −0.0085x gestational age + 3.6676 R2 = 0.0005
MCA PSV = 1.3295x gestational age − 0.2146 R2 = 0.17188
Table 2 shows the reference range from 24 to 40 weeks gestation for UA PI, RI, S/D values. Although technically a positive correlation, the relationship between the variables was weak. The UA S/D ratio showed a negative correlation. The regression equation for UA Doppler was:
UA PI = 0.00558x gestational age + 0.72932, R2 = 0.0039
UA RI = 0.00141x gestational age + 0.52959 with R2 = 0.0007
UA S/D = −0.0085x gestational age + 3.6676 with R2 = 0.0092.
The CPR reference range was also calculated (Table 3). Although technically a negative correlation, the relationship between the variables was weak (Fig. 1). The regression equation was given as:
CPR = −0.0149x + 2.1497 with R2 = 0.00642
The mean 5th, 50th and 95th centile along with corresponding MOM values across the gestational age for all Doppler parameters of MCA, UA along with CPR Doppler between 24 and 40 weeks gestation was derived and is shown in Table 4. The 5th centile for MCA PI was 0.8 MOM, whereas that of CPR was 0.5 MOM. The 95th centile value of UA PI was 1.8 MOM, whereas it was 1.3 MOM for UA S/D ratio.
Table 1.
The 5th, median and 95th centile of the MCA Doppler PI, RI, S/D ratio from 24 to 40 weeks gestation
| Gestational age (weeks) | Pulsatility index | Resistance index | Systolic/diastolic ratio | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 5th centile | 50th centile | 95th centile | 5th centile | 50th centile | 95th centile | 5th centile | 50th centile | 95th centile | |
| 24–26 | 0.82 | 1.02 | 2.37 | 0.42 | 0.65 | 0.96 | 2.02 | 2.91 | 4.83 |
| 27–29 | 0.83 | 1.19 | 2.09 | 0.36 | 0.65 | 0.94 | 2.09 | 3.15 | 4.98 |
| 30–32 | 0.92 | 1.30 | 1.93 | 0.46 | 0.65 | 0.81 | 2.09 | 3.02 | 5.05 |
| 33–35 | 1.01 | 1.38 | 1.95 | 0.42 | 0.72 | 0.87 | 2.21 | 3.11 | 5.23 |
| 36–38 | 0.92 | 1.38 | 1.85 | 0.40 | 0.70 | 0.86 | 2.14 | 2.93 | 5.06 |
| 39–40 | 0.89 | 1.34 | 1.81 | 0.40 | 0.68 | 0.84 | 2.14 | 2.89 | 4.82 |
Table 2.
The 5th, median and 95th centile of the umbilical artery Doppler PI, RI, S/D ratio from 24 to 40 weeks gestation
| Gestational age (weeks) | Pulsatility index | Resistance index | Systolic/diastolic ratio | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 5th centile | 50th centile | 95th centile | 5th centile | 50th centile | 95th centile | 5th centile | 50th centile | 95th centile | |
| 24–26 | 0.59 | 0.92 | 1.48 | 0.60 | 0.70 | 0.82 | 1.72 | 2.29 | 2.91 |
| 27–29 | 0.59 | 0.88 | 1.34 | 0.56 | 0.66 | 0.80 | 1.71 | 2.24 | 2.75 |
| 30–32 | 0.57 | 0.81 | 1.28 | 0.49 | 0.58 | 0.78 | 1.70 | 2.20 | 2.68 |
| 33–35 | 0.56 | 0.79 | 1.24 | 0.44 | 0.55 | 0.73 | 1.69 | 2.19 | 2.53 |
| 36–38 | 0.55 | 0.78 | 1.20 | 0.42 | 0.53 | 0.70 | 1.67 | 2.18 | 2.50 |
| 39–40 | 0.54 | 0.76 | 1.16 | 0.41 | 0.51 | 0.66 | 1.66 | 2.16 | 2.46 |
Table 3.
The 5th, median and 95th reference centile chart of MCA/UA or cerebroplacental ratio (CPR) from 24 to 40 weeks gestation
| Gestational age (weeks) | MCA PI/UA–PI (CPR) | |||
|---|---|---|---|---|
| 5th centile | 10th centile | 50th centile | 95th centile | |
| 24–26 | 0.84 | 0.95 | 1.83 | 2.86 |
| 27–29 | 0.77 | 0.90 | 1.73 | 2.68 |
| 30–32 | 0.77 | 0.89 | 1.53 | 2.64 |
| 33–35 | 0.76 | 0.89 | 1.50 | 2.56 |
| 36–38 | 0.64 | 0.83 | 1.59 | 2.55 |
| 39–40 | 0.61 | 0.80 | 1.56 | 2.52 |
Fig. 1.
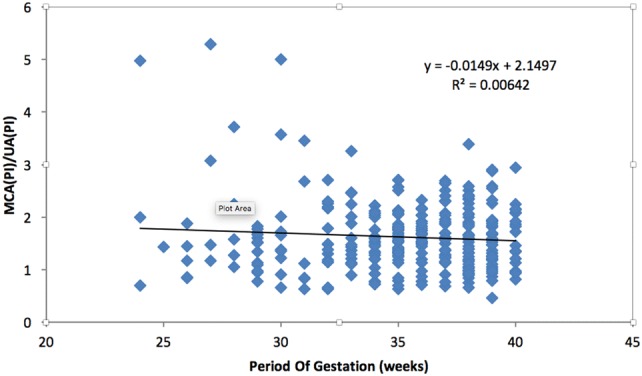
The regression analysis of cerebroplacental ratio as dependent variable and gestational age as an independent variable; there is decrease in values with advancing gestation
Table 4.
The mean, standard deviation, 5th, 50th and 95th centile with corresponding MOM values of middle cerebral and umbilical artery PI, RI, S/D ratio including cerebroplacental ratio or CPR across the gestational age from 24 to 40 weeks gestation
| Doppler | Mean | ±SD | 5th centile | MOM | 50th centile | MOM | 95th centile | MOM |
|---|---|---|---|---|---|---|---|---|
| MCA (PI) | 1.37 | 0.35 | 1.04 | 0.8 | 1.38 | 1.0 | 1.71 | 1.3 |
| MCA (RI) | 0.69 | 0.15 | 0.44 | 0.6 | 0.69 | 1.0 | 0.93 | 1.3 |
| MCA (S/D) | 3.37 | 1.33 | 1.18 | 0.4 | 3.03 | 1.0 | 5.56 | 1.8 |
| Umbilical artery (PI) | 0.93 | 0.31 | 0.59 | 0.7 | 0.83 | 1.0 | 1.56 | 1.8 |
| Umbilical artery (RI) | 0.58 | 0.14 | 0.36 | 0.6 | 0.56 | 1.0 | 1.48 | 2.6 |
| Umbilical artery (S/D) | 2.27 | 0.46 | 1.42 | 0.6 | 2.18 | 1.0 | 2.94 | 1.3 |
| MCA PI/UA PI | 1.60 | 0.58 | 0.71 | 0.4 | 1.57 | 1.0 | 2.52 | 1.6 |
Discussion
In the study, the percentile charts of the MCA and UA Doppler were constructed in relation to the gestational age. MCA values demonstrated a parabolic pattern, but the UA values showed a linear decrease with increasing gestational age. The regression equations were derived, which showed a weak correlation between the Doppler parameters and the gestational age, showing that there was very little variance in the values in the second half of pregnancy. The MOM of the mean across the gestational age from 24 to 40 weeks for the 5th, 50th and 95th centile was also derived for all MCA and UA parameters including CPR.
The findings demonstrated increase in MCA Doppler values till 33–35 weeks and then a decline till 40 weeks of gestation. The MCA Doppler showed a parabolic curve and was comparable to study by Bahlmann et al. [8] in the German population. In the present study, it showed the peak at 32–35 weeks; however, in the study by Ebbing et al. [9] the peak was at 28–32 weeks. In the present study, the values were found to be lesser compared to their study. In 2009, Tan et al. [10] did the study in 329 Asian women and found that there were essential differences in MCA PSV range between the Asian and non-Asian population. The fifth centile for the Asian population was consistently lower, and the gradient of the curves was less steep as compared to previous studies done in the non-Asian population [10]. In the present study also, the coefficient of correlation was found to be low, showing little difference in values with advancing gestation. Akolekar et al. [4] in their study also found racial differences in the values of MCA Doppler with the lower value in east Asian women. This stresses upon the need for regional charts for clinical use for the local population. The MOM derived in our study and in the study by Akolekar et al. [4] were similar (5th, 50th and 95th centile of MCA PI was 0.7, 1.0. 1.23, respectively, compared to 0.8, 1.0 and 1.3 in the present study).
The UA Doppler parameters, however, decreased with increasing gestational age. The umbilical PI and RI have been seen to decrease with increasing gestational age in previous studies also. The umbilical RI percentile charts were comparable to Acharya et al. [11] study. The CPR reference centile chart also showed a linear decrease with the gestational age. The adverse outcome is found to be associated with lower value of CPR; different studies have taken different lower cutoffs for CPR ranging from 5th centile, 10th centile or 1.1; some studies have also taken the threshold of 0.67 MOM as abnormal [11]. In the present study, the 5th centile was 0.71 (0.4 MOM).
The weakness of the study was that the gestation earlier than 24 weeks was not included. The strength of the study was its cross-sectional study design. It has been observed that the longitudinal studies require more complex statistical calculations and are also liable to have observer bias. Another strength of the study was that all cases were followed till delivery and cases with fetal growth restriction or other adverse outcome were excluded.
The CPR is considered to be an important predictor of adverse pregnancy outcome and is frequently used for the assessment of fetal well-being in small for gestational age (SGA) babies remote from term [12]. Dunn et al. [13] did a review of report on utility of CPR at term; they concluded that it had a strong association with adverse obstetric and perinatal outcomes. They suggested that the predictive utility of CPR at term was promising; however, there was insufficient evidence to demonstrate its value as a stand-alone test. It is also considered to be of use in evaluation of fetal well-being in post-dated pregnancies [14]. The CPR ratio centile chart meant for Indian population can be of clinical use in these situations.
Tarul Umarwal
has done her MBBS and MS from the prestigious lady Hardinge Medical College. She has keen interest in high-risk pregnancy and fetal medicine. This article is a part of her MD thesis dissertation.
Author Contribution
TU helped in design and conduct of study, drafting, editing; MK contributed to concept, plan and conduct of study, drafting, editing.
Compliance with Ethical Standards
Conflict of interest
There are no potential conflicts of interest among authors.
Ethical Standard
Ethical clearance was taken before the study.
Informed Consent
The Research involved Human participants; informed consent was taken before the study.
Footnotes
Tarul Umarwal is a Senior Resident, Department of Obstetrics and Gynecology, LHMC, Lady Hardinge Medical College, New Delhi-110001, India. Manisha Kumar is a Professor, Department of Obstetrics and Gynecology, LHMC, Lady Hardinge Medical College, New Delhi-110001, India.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Severi FM, Bocchi C, Visentin A, et al. Uterine and fetal cerebral Doppler predict the outcome of third-trimester small-for-gestational age fetuses with normal umbilical artery Doppler. Ultrasound Obstet Gynecol. 2002;19(3):225–228. doi: 10.1046/j.1469-0705.2002.00652.x. [DOI] [PubMed] [Google Scholar]
- 2.Khalil A, Morales-Rosello J, Khan N, et al. Is cerebroplacental ratio a marker of impaired fetal growth velocity and adverse pregnancy outcome? Am J Obstet Gynecol. 2017;216(6):606.e1–606.e10. doi: 10.1016/j.ajog.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 3.Flatley C, Greer RM, Kumar S. Magnitude of change in fetal cerebroplacental ratio in third trimester and risk of adverse pregnancy outcome. Ultrasound Obstet Gynecol. 2017;50(4):514–519. doi: 10.1002/uog.17371. [DOI] [PubMed] [Google Scholar]
- 4.Akolekar R, Sarno L, Wright A, et al. Fetal middle cerebral artery and umbilical artery pulsatility index: effects of maternal characteristics and medical history. Ultrasound Obstet Gynecol. 2015;45(4):402–408. doi: 10.1002/uog.14824. [DOI] [PubMed] [Google Scholar]
- 5.Valiño N, Giunta G, Gallo DM, et al. Biophysical and biochemical markers at 30–34 weeks’ gestation in the prediction of adverse perinatal outcome. Ultrasound Obstet Gynecol. 2016;47(2):194–202. doi: 10.1002/uog.14928. [DOI] [PubMed] [Google Scholar]
- 6.Bakalis S, Akolekar R, Gallo DM, et al. Umbilical and fetal middle cerebral artery Doppler at 30–34 weeks’ gestation in the prediction of adverse perinatal outcome. Ultrasound Obstet Gynecol. 2015;45(4):409–420. doi: 10.1002/uog.14822. [DOI] [PubMed] [Google Scholar]
- 7.Ciobanu A, Wright A, Syngelaki A, et al. Fetal Medicine Foundation reference ranges for umbilical artery and middle cerebral artery pulsatility index and cerebroplacental ratio. Ultrasound Obstet Gynecol. 2018 doi: 10.1002/uog.20157. [DOI] [PubMed] [Google Scholar]
- 8.Bahlmann F, Fittschen M, Reinhard I, et al. Blood flow velocity waveforms of the umbilical artery in a normal population: reference value from 18 to 42 weeks of gestation. Ultraschall Med. 2012;33:E80–E87. doi: 10.1055/s-0031-1281647. [DOI] [PubMed] [Google Scholar]
- 9.Ebbing C, Rasmussen S, Kiserud T. Middle cerebral artery blood flow velocities and pulsatility index and the cerebroplacental pulsatility ratio: longitudinal reference ranges and terms for serial measurements. Ultrasound Obstet Gynecol. 2007;30(3):287–296. doi: 10.1002/uog.4088. [DOI] [PubMed] [Google Scholar]
- 10.Tan KB, Fook-Chong SM, Lee S, et al. Foetal peak systolic velocity in the middle cerebral artery: an Asian reference range. Singapore Med J. 2009;50(6):584–586. [PubMed] [Google Scholar]
- 11.Acharya G, Wilsgaard T, Berntsen GK, et al. Reference ranges for serial measurements of umbilical artery Doppler indices in the second half of pregnancy. Am J Obstet Gynecol. 2005;192(3):937–944. doi: 10.1016/j.ajog.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 12.Royal College of Obstetricians and Gynaecologists: the investigation and management of the small-for-gestational-age fetus. Greentop guidelines no. 31. London, RCOG, 2014.
- 13.Dunn L, Sherrell H, Kumar S. Review: systematic review of the utility of the fetal cerebroplacental ratio measured at term for the prediction of adverse perinatal outcome. Placenta. 2017;54:68–75. doi: 10.1016/j.placenta.2017.02.006. [DOI] [PubMed] [Google Scholar]
- 14.Maged AM, Abdelhafez A, Al Mostafa W, et al. Fetal middle cerebral and umbilical artery Doppler after 40 weeks gestational age. J Matern Fetal Neonatal Med. 2014;27(18):1880–1885. doi: 10.3109/14767058.2014.892068. [DOI] [PubMed] [Google Scholar]


