Abstract
Background
Walking in natural environments can be considered a dual-task (DT) scenario that requires increasing cognitive resources with advancing age. Previous reviews concluded that gait speed under DT conditions is equivalent to gait speed as a single task (ST) in the prediction of future falls in older people. However, without a clear taxonomy, these conclusions might be premature. The aim of this review is to use a taxonomy for classifying cognitive tasks of cognitive-motor interference (CMI) paradigms while walking to identify which task domains lead to more pronounced cognitive-motor decrements due to fall risk and concern about falling (CoF) in older people.
Methods
A systematic literature research following PRISMA guidelines was conducted using MEDLINE, Psych-Info and EMBASE. Inclusion criteria were: older people ≥60 years with a previous fall or CoF, use of a DT paradigm to discriminate fallers and non-fallers, straight overground walking, reported gait measurements during ST and DT conditions. A meta-analysis estimated the effect of DT costs for the cognitive task domain and spatiotemporal gait parameters.
Results
N = 3737 studies were found within the databases. Nineteen studies were included (n = 14 for meta-analysis). Fallers and people with CoF showed reduced walking speed for ST and DT conditions. Effects of DT were examined for mental tracking tasks. The combined odds ratio (OR [95% confidence interval]) for fallers vs. non-fallers for ST was 3.13 [0.47, 5.80] with moderate heterogeneity (I 2 = 48%). For DT, the OR was 5.17 [2.42, 7.93] with low heterogeneity (I 2 = 37%). Comparing participants with and without CoF, the OR for ST was 12.41 [9.97, 14.84] with high heterogeneity (I 2 = 85%) and OR for mental tracking DT was 10.49 [7.58, 13.40] with moderate heterogeneity (I 2 = 51%).
Conclusion
CMI was not significantly different between fallers and non-fallers or people with and without CoF; however, our taxonomy revealed a large variety of cognitive conditions and a higher number of studies using mental tracking tasks, which make it impossible to draw firm conclusions. Future studies should use a more standardised and ecologically valid approach when evaluating the validity of DT gait performance in the prediction of falls, CoF or other age-related conditions.
Trial registration
This review was registered at Prospero with the ID: CRD42017068912.
Keywords: Falls, Concern about falls, Fear of falling, Ageing, Dual-task, Dual task cost
Introduction
Walking in our natural environment can be considered a dual-task (DT) scenario that requires increasing cognitive resources with advancing age. Age-related decline of performance whilst walking in DT situations has been extensively investigated [1–5]. For instance, an age-related decline in gait performance has been observed when conducting arithmetic, memory or visual tasks concurrently with walking [5, 6]. Walking is not an automated task and requires structural and functional connectivity of neural brain networks. Changes in brain structure are common with ageing and require re-allocation of cognitive resources for fast and efficient operation of neural brain networks [7, 8] during complex activities. Higher age is further associated with reduced cognitive processing efficiency (e.g., decrease in nerve conduction speed and increased lateralization) [9], which is in turn associated with a decrease in cognitive performance such as diminished response time, working memory and processing of multiple tasks. These age-related cognitive changes affect daily-life task performance [10]. The level to which walking performance is affected by cognitive-motor interference is typically expressed as the dual-task cost (DTC). This is calculated as the percentage of decrements in performance in a dual- or multi-task relative to single task performance. It is proposed that, with advancing age, sensory and motor aspects of walking performance increasingly require cognitive control and attention. Several studies report a correlation between age-related declines in the sensory and motor system on the one hand and age-related declines in cognitive functioning on the other hand [11]. There is some evidence that decrements of gait performance in older people with a reduced postural reserve (motor abilities to maintain balance) can be independent of the cognitive performance [12]. Other studies showed that impaired executive function and attention affect walking performance of older fallers independent of physical ability [13, 14].
DT paradigms have become prominent to understand cognitive-motor interference (CMI) while walking in old age. These dual-task experiments have demonstrated that the extent to which the cognitive demand affects walking performance is exacerbated in old age [15], people with high risk for falls [16] and people with concerns about falling [17]. People’s tendencies to change their gait patterns during complex activities might result in an increased risk of falling [10]. Many studies reported more pronounced impairments of spatiotemporal gait parameters under dual-task conditions (including gait speed, step length, step width and double support time) in fallers compared to non-fallers [18–20]. Cognitive-motor interference in combinations with poorer physical abilities may increase a person’s risk of falling even further, especially in situations that require the adoption of a faster gait speed [21]. This is further impacted by poorer judgement of physical abilities, which has been linked to more collisions with oncoming cars in virtual reality experiments [22, 23]. The understanding of cognitive-motor interference in people with high fall risk or concerns about falling during walking under different cognitive dual-task conditions is still quite limited. Moreover, there is little information about which motor and cognitive task combinations require the highest attentional demands in older people and which mechanisms lead to insufficient resource allocation.
Theoretical models to explain cognitive-motor interference
Several theoretical models have been proposed to explain reduced walking performance in dual-task situations. The central bottleneck theory states that due to an information processing bottleneck only one task can be processed at a time; processing of a second task cannot commence until the first is complete. This bottleneck usually results in a longer response time for one of the two tasks [34–36]. The 4-dimensional multiple resource model [37] proposes that there will be greater interference between two tasks that utilise similar resources. Finally, the attentional resource theory suggests that declines in performance under DT conditions result from interference caused by competing demands for attentional resources, resulting in less attention available to each task [38, 39].
The attentional resource theory might especially apply to people with CoF. CoF is very common in older people and can lead to self-induced restriction of physical and social activities. In its most severe form, it can result in a persistent and dysfunctional disruption of attention. People with higher levels of CoF have difficulties to inhibit or ignore irrelevant information of the environment in the process of balance control. Therefore, CoF may compete for the limited resources of attentional focus to maintain balance control during complex activities [40] resulting in instability and increased fall risk. A meta-analysis by Ayoubi et al. [41] revealed that CoF is associated with increased gait variability during normal walking. This effect is amplified under DT conditions, due to reduced gait speed and step length (often referred to as cautious gait), especially in older people who also reduce their daily physical activity due to their CoF [42].
Performance is expected to deteriorate in complex situations if there are fewer resources available for performance than are required. Navon [43] defined resources as any internal input that is essential for processing and is available in limited quantities at any point in time. Walking requires coordination of peripheral sensory and neuromuscular systems, with higher-level cognitive processing, which gradually decline with age. It is therefore not surprising that with advancing age, cognitive-motor interference becomes more pronounced when performing complex daily activities [10, 36, 44]. Each task requires a reweighting of sensorimotor information depending on the requirements of the additional task [45]. When the sensory system delivers conflicting information, vision will dominate spatial processing, which impacts a person’s ability to coordinate sensory and cognitive processing to main upright [45]. In addition, studies indicate that increasing difficulty levels (from DT to multitask-performance or with different task complexities e.g. from processing speed to decision-making tasks; see Table 1) further amplify the effects of cognitive-motor interference on walking performance [46–51]. Systematic reviews have further highlighted that cognitive-motor interference rises based on the task domain and the individual’s abilities and resources [52, 53]. More specifically, tasks including controlled processes or motor components showed more decrements in DT performance of older people.
Table 1.
Proposed taxonomy for cognitive dual tasks
| A range of DT paradigms have been used to examine age-related changes in motor performance and cognitive capacities, and to understand the relationship between performance in motor and cognitive tasks [24]. Cognitive tasks can be classified according to their demands and the mental processes involved to execute them. Based on the most commonly used tasks in DT-studies, the following domains were defined; each domain is distinct from the other domains at a behavioral and/or cognitive level according to definitions of Colcombe and Kramer [25] and Al-Yahya et al. [1]: | |
| • Reaction time tasks (processing speed) refer to tasks that involve the measurement of elapsed time between a sensory stimulus and a behavioral response [26]. These tasks are used to measure processing speed, where a slowed processing might underlie an attentional deficit [27]; e.g., a simple reaction time test to press a button following a light stimulus. | |
| • Controlled processing tasks refer to tasks that involve decision making in addition to processing speed; e.g., to press a button when a star is presented on a screen. | |
| • Visuospatial tasks refer to task that require detecting or processing visual information; e.g. Benton Visual retention task [28] or naming the location of a stimulus. | |
| • Mental tracking tasks refer to tasks that require holding information in the mind while performing a mental process [27]. These tasks have been usually used to examine sustained attention and information processing speed [27, 29]. The most common mental tracking tasks are: | |
| a. Arithmetic tasks refer to tasks that require solving a mathematical equation or counting backwards in threes or sevens. | |
| b. Verbal fluency tasks refer to tasks that require word production, either spontaneously or under pre-specified search conditions; these tasks have recently been used to examine executive functions [26, 27]. | |
| • Working memory tasks refer to tasks that require holding information in the mind which is available for processing [30]. The differentiation between working memory and mental tracking tasks was adapted from brain imaging studies [31]. Tasks that require holding information only, are categorized into working memory tasks, while those that require holding information plus manipulation belong to the mental tracking category [31, 32]; e.g., a n-back task. | |
| • Discrimination tasks refer to tasks that require selective attention to a specific stimulus or feature and respond accordingly; they have been usually used to examine attention and response inhibition such as the Stroop paradigm [33] or a Go or no-go task. |
However, activities that heavily rely on postural control occasionally lead to an improved motor performance when combined with a secondary task [54]. The U-Shaped Non-Linear Interaction Model postulates that, depending on the complexity of the secondary task, motor and balance performance can increase or decrease [55]. For example, there might be a reduction of postural sway as a result of muscle co-contraction while concentrating on the cognitive task [56, 57], whereas postural sway may increase without additional cognitive performance with a secondary task [58]. The Supra-Postural Task Model [59, 60] provides additional details to explain the U-shape relationship between postural control and balance. The theory suggests that in specific situations the motor performance is necessary to reach the goal of the cognitive task (e.g. standing still to read a sign). In contrast to the U-shaped model, in the Supra-Postural Task Model effects are explained by situation awareness and not by task complexity [61].
Finally, the Task Prioritization Model [62] accounts for the strategies that an individual might use during complex activities. It postulates that older people are more likely to prioritize motor performance under threat of a loss of balance [63, 64]. This prioritization reduces the cognitive-motor interference and allows for reorganization of the cognitive-motor resources [65] to reduce the risk of falling. However, if the environment poses too many challenges (e.g. elevated surface), task prioritization is not always effective. Yogev-Seligmann and colleagues [66] found that older people with adequate balance abilities and capacity to identify hazards are able to focus on cognitive performance as long as balance is maintained. On the other hand, fallers are not able to shift attention in these situations [67], which could be explained by the impact of poor executive function and attention on walking performance of older fallers [13, 14].
Objectives
The primary objective of this review was to use a taxonomy for classifying cognitive tasks to gain insight in cognitive-motor interference within the study of falls in older people. Previous reviews concluded that gait speed under DT conditions is equivalent to gait speed as a single task in the prediction of future falls in older people [50, 68]. However, without a clear taxonomy of cognitive dual tasks, these conclusions might be premature. In addition, little is known about the effects of dual-task settings on older adults with CoF. A clear taxonomy will allow a better understanding of how cognitive-motor interference during complex activities is related to fall risk and concern about falls.
Methods
Search strategy
Databases were systematically searched by using OvidSp to search in Medline (1946 to 2019, Week 20), Embase (1974 to 2019, Week 20) and PsycINFO (1806 to 2019, Week 20). The search within the databases was limited to the English and German language. In addition, the reference lists of included articles were searched manually. Two reviewers (BW, MW) independently searched within titles and abstracts to identify all potentially eligible studies. Afterwards, these two reviewers independently assessed full paper copies of the identified potentially eligible studies to determine the studies to be included. Any disagreement on inclusion was resolved by discussion and through arbitration by a third reviewer (KvS, KD).
Inclusion and exclusion criteria
The inclusion criteria were: (i) older adults ≥ mean age of the sample was 60 years with a previous fall or CoF, (ii) the dual-task paradigm was used to discriminate fallers from non-fallers or people with high concerns about falling from people with low concerns about falling, (iii) utilized straight over ground walking at self-selected speed as the primary motor task, (iv) reported gait measurements during both single and dual-task performance, or the effect of dual-tasking on gait performance (more than one gait cycle), (v) clear description of the dual-task situation, (vi) reported adequate data to calculate effect sizes either from descriptive or inferential statistics, (vii) interventional studies were included if the effect of dual-tasking on gait at baseline was reported. The exclusion criteria included: (i) population with brain injuries or diagnosed cognitive decline, (ii) physical impairments (e.g. using a cane or walker) and (iii) chronic diseases (e.g., multiple sclerosis or Parkinson’s disease). Moreover, studies with a secondary analysis of previous reported results were also excluded.
Selection criteria
Studies comparing fallers and non-fallers were included if the method section reported of the number of falls. Prospective studies were considered if they compared fallers and non-fallers at baseline (retrospective) or at the follow-up measurement und ST and DT conditions.
Studies addressing CoF were included if they classified the participants according to the “falls efficacy scale international (FES-I)” [69] score, the activities-specific balance confidence (ABC) scale [70] or if they asked the participants using a single item question if they were afraid of falling during activities of daily life.
Studies that included walking under DT conditions were included. This includes studies that investigated at least one walking task (in a DT setting; according to the definitions of spatiotemporal gait parameters addressed in Table 2), studies that compare ST and DT performance, and studies that investigated DT performance in healthy or balance-impaired (fallers) older adults in either a randomized control trail (RCT), an experimental-control group design or an old-young comparison. Moreover, studies with a secondary motor task were also included. Additionally, every concurrent task was assigned to a “stimulus-response-condition” (visual-verbal, visual-manual, auditory-verbal, auditory-manual) and classified according to our taxonomy of cognitive tasks (see Table 1).
Table 2.
Spatiotemporal gait parameters
| Gait – the medical term used to describe the locomotor movement of walking – is simple in terms of execution, but complex in terms of biomechanics and motor control [73]. During steady-state straight forward gait, commonly examined gait variables can be classified into parameters of rhythm (e.g. single and double support time or cadence) and pace (e.g. speed or stride length). This review follows the Guidelines for Assessment of Gait and Reference Values for Spatiotemporal Gait Parameters in Older Adults [73] by defining spatiotemporal gait parameters as: | |
| • Stride length: a stride is the distance from heel strike of one extremity to the next heel strike of the same extremity. Stride length is the distance that one part of a foot travels between the same instant in two consecutive gait cycles. | |
| • Step length: step length is the distance that one part of the foot travels in front of the same part of the other foot during each step. | |
| • Cadence: measure of the number of steps per unit time. Cadence increases if step length shortens when gait speed is held constant. | |
| • Walking speed: distance travelled divided by the ambulation time. Speed was expressed in centimetres per second (cm/sec). | |
| • Double support time: amount of time spent with both feet in contact with the ground. The gait cycle is divided into the stance phase, when the foot is in contact with the floor, and the swing phase, when it is not. The double support time is approximately 20% of the gait cycle during which both feet are in ground contact. |
Quality assessment
Quality assessment of the included articles was based on the Standard Quality Assessment Criteria (SQAC) for evaluating primary research papers proposed by the Alberta Heritage Foundation for Medical Research [71]. As the review did not focus on RCTs, the quality criteria for RCTs were not assessed. The quality criteria, as described in SQAC, were: (1) sufficient description of the question/objective; (2) appropriate study design; (3) appropriate method of participant selection or source of information/ input variables; (4) sufficient description of participant characteristics; (5) report of means of assessment with outcome measures well defined and robust" to measurement or misclassification bias (6) appropriate sample size; (7) appropriate analytic methods and method description; (8) report of estimate of variance in main results; (9) control for confounding; (10) sufficiently detailed report of results; and (11) conclusions supported by the results.
Participant selection was verified by comparing the sample with the conclusions drawn from the experimental results. A full point for appropriate sample size was given when either an a priori calculation of sample size had been described or the sample size was a full cohort. Based on the analytic methods employed (8), important statistical values (according to the APA-Manual [72]) had to be included to obtain a full quality score. BW and MW or KvS performed the assessment independently and the results presented in Table 3 were concurred on. Each criterion scored one point if partly fulfilled and two points if completely fulfilled. Points were added up and resulted in the quality score. The necessary score for a study of high quality was defined to be 17 out of 22 (75%) and 10–16 points for standard quality according to the SQAC. No point was given if general remarks had to be made (indicated by brackets; Table 3). Moreover, we reported some general methodological issues (cf. column general marks). Studies were included in the meta-analysis if they had quality score of 7 or more.
Table 3.
Quality score
| Author | Year | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Quality score | Remarks |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Asai [87] | 2014 | (x) | (x) | x | x | (x) | x | x | x | no | x | x | 17 | design is not clearly identified; differences in subgroups variables sex (f/m), no studies for accuracy of accelerometer, SEM or validity |
| Auvinet [74] | 2017 | x | x | x | x | (x) | (x) | (x) | x | (x) | x | (x) | 17 | no studies for accuracy of equipment, SEM or validity; study is mainly descriptive: no control for baseline characteristics; sample size for subgroup “cautious gait” (< 10) low |
| Bauer [75] | 2010 | (x) | (x) | x | (x) | x | x | x | (x) | no | x | x | 16 | design is not clearly identified |
| Beauchet [19] | 2008 | x | (x) | x | x | no | x | x | x | no | x | x | 17 | design is not clearly identified; stopwatch as measurement |
| Bootsma-van der Wiel [76] | 2003 | x | x | x | (x) | no | x | x | (x) | x | (x) | x | 17 | no description of BMI or weight; no report of variance; stopwatch as primary measurement tool |
| Donoghue [88] | 2013 | x | x | x | x | x | x | x | no | no | x | x | 18 | no reporting of estimate variance in results and confounding |
| Freire Junior [21] | 2017 | x | (x) | (x) | (x) | x | x | x | no | x | x | x | 17 | design is not clearly identified; no sufficient description of the population group; no medications or comorbidities reported |
| Howcroft [77] | 2016 | x | (x) | x | no | x | (x) | x | no | no | x | x | 14 | no gait specifications: design is not clearly identified; no description of BMI, cognition or number of medications, no baseline comparison reported |
| Johannsson [78] | 2016 | (x) | x | (x) | x | x | x | (x) | x | x | x | x | 19 | no mention of clear gait parameters (“challenging gait conditions”); research question and hypothesis missing; no sufficient information; in the method section |
| Mirelman [79] | 2012 | x | (x) | x | x | x | x | x | x | no | x | x | 19 | design is not clearly identified |
| Muhaidat [20] | 2013 | x | (x) | x | (x) | no | (x) | x | no | (x) | x | x | 14 | design is not clearly identified; no description number of medications/drugs or disease; stopwatch used as primary measurement tool; pilot study with small sample size (no sample size calculation); differences of baseline characteristics reported but no statistical analysis done |
| Nordin [80] | 2010 | x | x | x | x | x | x | x | no | no | (x) | x | 17 | only medians reported |
| Reelick [81] | 2011 | (x) | (x) | (x) | x | x | (x) | (x) | x | no | x | x | 15 | no gait specifications; design is not clearly identified, no description of BMI or height; small sample size |
| Reelick [89] | 2009 | x | (x) | (x) | x | x | (x) | (x) | x | no | x | x | 16 | design is not clearly identified, small sample size |
| Springer [82] | 2006 | x | (x) | (x) | (x) | (x) | (x) | x | (x) | x | (x) | x | 15 | no sufficient information about study design; no description number of medications/drugs or disease |
| Toulotte [83] | 2006 | (x) | x | x | (x) | x | (x) | x | x | x | x | x | 19 | research question is not precise; no description number of global cognition and medication use or diseases |
| Toulotte [84] | 2006 | x | (x) | x | (x) | x | (x) | (x) | x | x | x | x | 18 | No description of global cognition; report of means and estimate of variance in main results are missing |
| Verghese [85] | 2017 | (x) | (x) | x | (x) | x | x | x | (x) | no | (x) | x | 15 | research question is unclear; study design unclear; no report of variance |
| Wollesen [90] | 2017 | x | x | x | x | x | x | x | x | x | x | x | 22 | |
| Yamada [86] | 2011 | (x) | (x) | no | (x) | (x) | no | (x) | no | no | no | no | 5 | research question and hypothesis missing; insufficient information of the other items |
Legend: x: yes, (x): partially with general remarks, no: no/unclear. Item 1, sufficient description of question/objective; 2, appropriate study design; 3, appropriate method of participant selection or source of information/input variables; 4, sufficient description of patient characteristics; 5, report of means of assessment with outcome measures well defined and robust to measurement/misclassification bias; 6, appropriate sample size; 7, appropriate analytic methods and method description; 8, report of estimate of variance in main results; 9, control for confounding; 10, sufficiently detailed report of results; 11 conclusions supported by the results. Specifications: 1: clearly description, mention of specific gait parameters (no generalization e.g. gait changes), 2 / 3: precise information of in- and exclusion criteria and recruitment, 4: specific baseline characteristics of population (older people) must include: age, distribution male/female, global cognition, BMI or height/weight, number of medications or chronic disease/comorbidities, and for healthy older people: TuG, SPPB or comparable test of physical abilities, 5: Primary and secondary outcome must be clearly described. Error of measurement must be discussed, 6: sample size calculation should be reported 8: Means and estimate of variance (SD or IQR) must be reported for main outcome
Data extraction
Table 4 provides an overview of all included studies including the authors, year of publication, study design and aims, population with discrimination to fallers/non-fallers or participants with concerns or no CoF, observed walking parameters and description of the DT setting. The main results of the studies were extracted to Table 5. This includes task order, outcome measures used to assess and report the concurrent tasks performance and instructions given to participants, and study results. Data were recorded as a mean and standard deviation (SD) if reported, with sample size and number analyses in each group (fallers vs. non-fallers or participants with concerns or no CoF).
Table 4.
Included studies with fallers
| Author | Title | Study design | Study aims | No. of subjects | Age (yr) | Dual-task type |
|---|---|---|---|---|---|---|
| Auvinet et al., 2017 [74] | Gait disorders in the elderly and dual task gait analysis | Prospec-tive cohort study |
1. To assess the value of gait instability as a clinical symptom, 2. To quantify gait disorders by means of the DTC in order to differentiate between peripheral pathologies and central nervous system pathologies, 3. To identify motor phenotypes according to the DTC for stride frequency and gait regularity 4. To identify correlations between these motor phenotypes and conventional brain MRI findings. |
Overall (n = 103), Gait instability (n = 46), Recurrent falls (N = 30), Memory impairment (n = 19), Cautious Gait (n = 8) Falls assessment of previous falls in the last 12 months |
Overall (76 ± 7), Gait instability (77 ± 8), Recurrent falls (77 ± 8), Memory impairment (76 ± 5), Cautious Gait (81 ± 5) |
Arithmetic DT: Walking + counting aloud backwards from 50 subtracting serial 1 s (one by one) SR: auditory-verbal |
| Bauer et al., 2010 [75] | First Results of Evaluation of a Falls Clinic | Cross-sectional study | To assess risk factors for falls in community dwelling older people and to recommend targeted interventions |
Fallers (n = 42) Non-fallers (n = 19) Previous falls in the last 12 months were assessed by questionnaire |
Fallers (75.95) Non-fallers (75.35) No SD reported |
Arithmetic DT: 1. Walking+ counting backwards from 50 subtracting serial 1 s (one by one) 2. walking + subtracting serial 3 s from 100 Verbal fluency task: Walking + naming animals SR: auditory verbal |
| Beauchet et al., 2008 [19] | Recurrent falls and dual task-related decrease in walking speed: is there a relationship? | Prospec-tive cohort study | To determine whether DT–related changes in walking speed were associated with recurrent falls in frail older people |
Fallers (n = 37) vs Non-Fallers (n = 156) vs Recurrent fallers (n = 20) Falls assessment of previous falls in the last 12 months |
Fallers (84.7 ± 5.1) vs Non-Fallers (83.9 ± 5.5) vs. Recurrent fallers (87.2 ± 5.7) |
Arithmetic DT: Walking + subtracting serial 1 s (one by one) from 50 SR: auditory verbal |
| Bootsma-van der Wiel et al., 2003 [76] | Walking and talking as predictors of falls in the general population | Prospective population-based follow-up study | To compare the added value of DT in predicting falling in the general population of oldest old with that of an easy-to-administer ST |
None (n = 22), One (n = 87), and Recurrent (n = 71) Previous falls in the last 12 months and the last month assessed by questionnaire |
Leiden 85-plus Study (no precise information) |
Verbal fluency task: Walking + reciting names of animals or professions during a 30-s period SR: auditory verbal |
| Freire Junior et al., 2017 [21] | The effects of a simultaneous cognitive or motor task on the kinematics of walking in older fallers and non-fallers | Cohort study | Comparing kinematics of ST gait, cognitive DT gait, and motor DT gait in both older fallers and non-fallers |
No Falls (n = 35) vs. One fall (n = 27) Previous falls in the last 6 months and the last month assessed by questionnaire |
No Falls (67.97 ± 4.82) vs One fall (67.96 ± 5.7) |
1. Verbal fluency task: Walking + naming animals SR: auditory verbal 2. Secondary motor task: Walking + transferring a coin from one pocket to another SR: auditory-manual |
| Howcroft et al., 2016 [77] | Analysis of dual-task elderly gait in fallers and non-fallers using wearable sensors | Prospective population-based follow-up study |
Use wearable sensors to detect gait differences between: (1) fallers and non-fallers for ST walking, (2) between fallers and non-fallers for DT walking, (3) ST and DT walking for fallers, and (4) ST and DT walking for non-fallers. |
Fallers (n = 24), Non-Fallers (n = 76) Previous falls in the last 6 months and the last month assessed by questionnaire |
Fallers (76.3 ± 7,0), Non-Fallers (75,2 ± 6,6) |
Verbal fluency task: Walking + naming words starting with A, F or S) SR: auditory verbal |
| Johansson et al., 2016 [78] | Greater Fall Risk in Elderly Women Than in Men Is Associated With Increased Gait Variability During Multitasking | Prospective observational study |
1. investigate variability in gait patterns among men and women aged 70 years during progressively challenging gait conditions. 2. investigate associations of gender with gait patterns and the risk of incident falls. |
Non-Fallers (1202), Fallers (148) Falls assessment of previous falls in the last six and 12 months |
Fallers (70), Non. Fallers (70), Inclusion criteria: age of exactly 70 years at the time of testing. |
Arithmetic task: Walking + subtracting 1 s from the number 100 SR: auditory verbal |
| Mirelman et al., 2012 [79] | Executive function and falls in older adults | Cohort study (Follow Up) |
(1) Evaluate if reduced Executive Function is a risk factor for future falls, (2) assess whether ST and DT walking abilities, an alternative window into EF, were associated with fall risk. |
256 Participant recorded there falls in a falls calendar |
76.4 ± 4.5 |
Arithmetic task Walking + subtracting 3 s from a predefined 3 digit number SR: auditory verbal |
| Muhaidat et al., 2013 [20] | Exploring gait-related dual task tests in community-dwelling fallers and non-faller | Pilot study | Assess differences in DT performance between the two groups on both primary and secondary tasks to help narrow down the potential choices of tasks, using simple clinical outcome measures that only require the use of a stopwatch, for future research. |
Fallers (n = 12), Non-Fallers (n = 15) Falls assessment of previous falls in the last 12 months |
Fallers (75.5 (8.5 IQR), Non-Fallers 72 (4 IQR) |
Arithmetic tasks: 1. Walking + subtracting 3 s 2. Walking + subtracting 7 s Verbal fluency tasks: 3. Walking + Generating words e starting with the letter I, N, or O 4. Walking + Generating animal names Visual spatial task: 5. Walking + clock task SR 1.-5.: auditory verbal Secondary motor task: 6. Walking + carrying a cup SR: auditory- manual Discrimination task: 7. Walking + Stroop (high/ low; different pitches) SR: auditory verbal |
| Nordin et al., 2010 [80] | Changes in step-width during dual-task walking predicts falls | Cohort study (Follow Up) | Evaluate whether gait pattern changes between single- and DT conditions were associated with risk of falling in older people |
Fallers (n = 120), Non-Fallers (n = 110) Participant recorded there falls in a falls dairy |
Non-Fallers (78) Fallers (80) No SD available |
1. Secondary motor task: Walking + carrying a cup on a tray) SR: auditory-manual 2. Verbal fluency task: Walking + naming animals 3. Arithmetic task: Walking + subtracting 3 s from 50 SR 2. + 3.: auditory verbal |
| Reelick et al., 2011 [81] | Increased intra-individual variability in stride length and reaction time in recurrent older fallers | Cross-sectional study | To compare mean performance measures as well as intra-individual variability measures of stride length and reaction time in vulnerable recurrent and non-recurrent older fallers. |
Non- fallers (n = 38), Recurrent fallers (n = 22) Falls assessment of previous falls in the last 6 months |
Non-recurrent Fallers (75.8 ± 7.2), recurrent Fallers (75.7 ± 5.6) |
1. Arithmetic task Walking + subtracting 7 from 100 2. Verbal fluency task: Walking + naming words starting with a certain letter SR: auditory verbal |
| Springer et al., 2006 [82] | Dual-tasking effects on gait variability: The role of aging, falls, and executive function | Cross-sectional study |
Test if the DT effect on gait variability is larger 1) in healthy older people vs healthy young people; 2) in idiopathic older fallers vs healthy older people; 3) and if DT has effects on gait variability are correlated with executive function |
YA (n = 19), Non- fallers (n = 24), Fallers (n = 17) Falls assessment of previous falls in the last 6 months |
YA (29,4 ± 4,4), Non-Fallers (71.0 ± 5.9), Fallers (76.1 ± 4.8) |
1. Listening memory task Walking + listening to a text; answering questions afterwards SR: auditory verbal 2. Arithmetic task Walking + subtracting 7 from 500 SR: auditory verbal |
| Toulotte et al., 2006a [83] | Effects of training and detraining on the static and dynamic balance in elderly fallers and non-fallers | Pilot study | Evaluate the effects of training on static and dynamic balance in ST and DT conditions to analyze the effects of detraining on static and dynamic balance in healthy older fallers and non-fallers. |
Fallers (n = 8), Non-Fallers (n = 8) Falls assessment of previous falls in the last 24 months |
Fallers (71.1 ± 5.0), Non-Fallers (68.4 ± 4.5) |
Secondary motor task: Walking + carrying a glass SR: auditory-manual |
| Toulotte et al., 2006b [84] | Identification of healthy elderly fallers and non-fallers by gait analysis under dual-task conditions | Case comp-arison study | Compare healthy older fallers and non-fallers to identify balance disorders associated with falling under ST and DT conditions |
Fallers (n = 21), Non-Fallers (n = 19) Falls assessment of previous falls in the last 24 months |
Fallers (70.43 ± 6.43), Non-Fallers (67.05 ± 4.81) |
Secondary motor task: Walking + carrying a glass SR: auditory-manual |
| Verghese et al., 2017 [85] | Brain activation in high-functioning older adults and falls | Prospective cohort study | To determine whether brain activity over the prefrontal cortex measured in real time during walking predicts falls in high-functioning older people |
166 71 fallers 95 non-fallers Falls were prospectively ascertained over a 50-month period |
74.95 ± 6.07 |
Letter memory task: Walking + reciting alternate letters SR: auditory-manual |
| Yamada et al., 2011 [86] | The reliability and preliminary validity of game-based fall risk assessment in community-dwelling older adults | Randomized controlled trial | Examine whether the Nintendo Wii Fit program could be used for fall risk assessment in healthy, community-dwelling older people |
Faller (n = 16), Non-Fallers (n = 28) Previous falls in the last 12 months assessed by question-naire |
Fallers (84.8 ± 10.1), Non-Fallers (80.2 ± 6.4) |
Arithmetic task: Walking + counting backwards from 50 SR: auditory-manual |
| Asai et al. 2014 [87] | Effects of dual-tasking on control of trunk movement during gait: respective effect of manual- and cognitive-task | Cross-sectional study |
1. to assess the effects of a cognitive task and a manual task on trunk movements during gait. 2. to examine the effect of FoF on trunk movement in both dual-task walking conditions: cognitive task and manual-task gaits. |
Overall (n = 117), nFoF (n = 85), FoF (n = 32) Previous falls in the last 12 months assessed by questionnaire FOF was assessed by one question |
Overall (73.7 ± 4.0), nFoF (73.7 ± 4.0), FoF (74.5 ± 4.0) |
1. Arithmetic task: Walking + subtracting 1 s from 100 SR: auditory-manual 2. Secondary motor task: Walking + motor task carrying a ball on a tray SR: auditory-manual |
| Donoghue et al., 2013 [88] | Effects of fear of falling and activity restriction on normal and dual task walking in community dwelling older adults | Prospective cohort study |
1. to examine the relationship between FOF, activity restriction and gait characteristics in normal and dual task walking and 2. to determine if these relationships persist after adjusting for potentially underlying factors |
No FOF (n = 961), FOF-NAR (n = 250), FOF-AR (n = 96) FOF was assessed by one question |
No FOF (72.3 ± 5.6), FOF-NAR (74.9 ± 5.8), FOF-AR (73.9 ± 5.6) |
Verbal memory task: Walking + recite alternate letters of the alphabet (A-C-E, etc.) SR: auditory-manual |
| Reelick et al., 2009 [89] | The influence of fear of falling on gait and balance in older people | Cross-sectional study | The purpose of this study was to examine the association between FoF and gait and balance in older people during walking with and without dual-tasking. |
FoF (n = 29) vs NFOF (n = 65) FOF was assessed by the ABC-NL scale |
FOF (80.6 ± 4.2) vs. NFOF (80.5 ± 3.7) |
Arithmetic task: Walking + subtracting 7 s from 100 SR: auditory-manual |
| Wollesen et al., 2017 [90] | Does dual task training improve walking performance of older adults with concern of falling? | Single blind randomized controlled trial | The primary aim of this study was to compare the effects of a DT training integrating task managing strategies for independent living older people with and without concern about falling to a non-training control group on walking performance under ST and DT conditions. | Intervention with FES-I < 20 (n = 26) vs Intervention with FES-I > 20 (n = 30) vs Control group with FES-I < 20 (n = 19) vs Control group with FES-I (n = 20) |
Intervention with FES-I < 20 (72.2 ± 4.6) vs Intervention with FES-I > 20 (69.8 ± 5.7) vs Control group with FES-I < 20 (72.9 ± 4.4) vs Control group with FES-I (72.7 ± 5.3) |
Discrimination task: Walking + Stroop task (colors) SR: visual-verbal |
Legend: SR Stimulus-reponse condition, YA Young adults, nFOF No fear of falling, FOF Fear of falling, FOF NAR=, ABC-NL Advanced balance scale Netherlands, FES-I Falls efficacy scale- international
Table 5.
Data extraction fallers/ non-fallers
| Author | Dual-task category | Stimulus-Response condition | Recording of the gait parameters | Gait parameters Single & Dual Task | Results |
|---|---|---|---|---|---|
| Auvinet et al., 2017 [74] | walking+ arithmetic (counting backwards from 50 subtracting serial 1 s) | auditory -verbal | 3-D-acceleration sensor, Locometrix (electronic walkway), stopwatch, 30 (m) distance |
walking speed (m/s) stride frequency (Hz) and the stride regularity (dimensionless) |
1. Non-Fallers: walking speed (m/s) ↓, stride frequency (Hz) ↓ and the stride regularity (dimensionless) ↓ 2. Fallers: walking speed (m/s) ↓, stride frequency (Hz) ↓ and the stride regularity (dimensionless) ↓ Walking speed and stride regularity differed between subgroups under ST and DT (p < 0.01 and 0.05, respectively, for both conditions). |
| Beauchet et al., 2008 [19, 96] | walking+ arithmetic (counting backward (counting backwards from 50 subtracting serial 1 s) | auditory -verbal | Stopwatch, 10 (m) | walking speed (cm/s), cadence (steps/min) |
1. Non-Fallers (0 falls): walking speed (cm/s) ↓, cadence (steps/min) ↓ 2. Non-multiple Fallers (0 or 1 fall): walking speed (cm/s) ↓, cadence (steps/min) ↓ 3. Fallers (1 or more falls): walking speed (cm/s) ↓, cadence (steps/min) ↓ 4. Multiple Fallers (2 or more falls (walking speed (cm/s) ↓, cadence (steps/min) ↓ Single and recurrent fallers walked more slowly than non-fallers under ST and DT conditions |
| Bauer et al. 2010 [75] |
walking+ arithmetic (counting backwards from 50 subtracting serial 1 s) walking + arithmetic (counting backwards from 100 subtracting serial 3 s) walking + verbal fluency (naming animals starting with a specific letter) |
auditory verbal | GAITRite system | walking speed (cm/s) |
Fallers walked slower than non-fallers under ST and DT conditions. Both non-fallers and fallers showed comparable reduced DT performance for the task conditions. The verbal fluency task had a higher amount of DCT in comparison to the arithmetic task (cf. Fig. 5) |
| Bootsma et al., 2003 [76] | walking + verbal fluency (reciting names of animals or professions during a 30-s period) | auditory -verbal | Stopwatch, 12 (m) |
walking time (s) Number of steps (n), Number of complete stops (n) |
1. Non-Fallers (0 falls): walking time (s) ↑, Number of steps (n) ↑ 2. non-multiple Faller (0 or 1 fall): walking time (s) ↑, Number of steps (n) ↑ 3. Fallers (1 or more falls): walking time (s) ↑, Number of steps (n) ↑ |
| Freire Junior et al., 2017 [21] |
1. walking + word task (naming animals starting with a specific letter) 2. walking + motor task (transferring a coin from one pocket to another) |
1. auditory - verbal 2. manual |
GAITRite, 8(m), 25–36 steps were collected to examine variability | gait speed (m/s), cadence (steps/min), step length (cm) stride time (s), single support time (as percentage of the gait cycle), and stride time variability (CoV (%)) |
1. Non-Fallers (0 falls) and Fallers (1 or more falls) + word task: gait speed (m/s) ↓, cadence (steps/min) ↓, stride time (s) ↑, step length (cm) ↓, single support time ↓, and stride time variability (CoV (%))↑ 2. Non-Fallers (0 falls) and Fallers (1 or more falls) + motor task: gait speed (m/s) ↓, cadence (steps/min) ↓, stride time (s) ↑, step length (cm) ↓, single support time (↓, and stride time variability (CoV (%)) ↑ There were no significant main effects of group and interaction effects between group and task. |
| Howcroft et al., 2016 [77] | walking + word fluency task (recite words starting with A, F or S) | auditory – verbal | Stopwatch, Pressure-sensing insoles (F-Scan 3000E, Tekscan, Boston, MA), Accelerometers (X16-1C, Gulf Coast Data Concepts, Waveland, MS), 7,62 (m) | cadence (steps/min), double support time (%), speed (m/s) CoP path (s), Min CoP Vel (m/s), Mean Cop Vel (m/s), Median CoP Vel (m/s), Cadence (steps/min), stride time (s), stance time (s), swing time (s), stride time CoV, percent stance time (%), stride time symmetry index, Impulse (Foot-strike to first peak (Ns/kg), Min to second peak (Ns/kg), Second peak to foot-off (Ns/kg), Foot strike (Ns/kg) |
1. Non-Fallers (0 falls): cadence (steps/min) ↓, Percent double support time (%) ↓, gait speed (m/s) ↓ 2. Non-multiple fallers (0 or one falls): cadence (steps/min) ↓, Percent double support time (%) ➔ no data, gait speed (m/s) ↓ 3. Fallers (1 or more falls): cadence (steps/min) ↓, Percent double support time (%) ↓, gait speed (m/s) ↓ 4. Multiple Fallers (2 or more falls): cadence (steps/min) ↓, Percent double support time (%) ➔ no data, gait speed (m/s) ↓ Accelerometer: Differences were found between fallers and non-fallers for the head and posterior pelvis accelerometers. |
| Johansson et al., 2016 [78] | walking+ arithmetic task (counting backwards from 10 by subtracting serial 1 s) | auditory – verbal | GAITRite, 8.6 (m) | Double support time CV(%), gait speed (m/s) at baseline (normal speed) -- > All gait parameters present as Coefficient of Variations (CVs; SD/M × 100) | For Non-Fallers (0 falls) and Fallers (1 or more falls): step width CV (%) ↑, stride width CV (%) ↑, step length CV (%) ↑, stride length CV (%) ↑, step time CV (%) ↑, stance time CV (%) ↑, stride time CV (%) ↑, stride velocity CV (%) ↑, swing time CV(%) ↑, DST CV(%) ↑ |
| Mirelman et al., 2012 [79] | walking + arithmetic task (counting backwards from a predefined 3 digit number by subtracting serial 3 s) | auditory - verbal | force-sensitive insoles, stopwatch, 25 (m) |
gait speed (m/s) gait variability (%) |
1. Non-fallers (0 falls), Non-multiple fallers (1 fall), Multiple fallers (2 or more falls): gait speed (m/s) ↓ |
| Muhaidat et al., 2013 [20] |
1. walking + arithmetic task (counting backwards by subtracting serial 3 s/ 7 s) 2. walking + Stroop task (identify incongruency between the words high/low in different pitches) 3. walking + word task (generating words starting with I, N, O or naming animals) 4. walking + visuospatial task (clock task) 5. walking + motor task (carrying a cup) |
1. auditory-verbal 2. auditory -verbal 3. auditory -verbal 4. visual-spatial (manual) 5. manual |
stopwatch, 10 (m) | Gait speed (m/s) |
Gait speed (m/s) ↓ for all subgroup form ST to DT A trend of a difference in complexity of secondary and absolute values of task performance was shown between community-dwelling fallers and non-fallers (p ≤ 0.05). |
| Nordin et al., 2010 [80] |
1. walking + motor task (carrying a cup) 2. walking + motor task (carrying a tray) 3. walking + word/verbal fluency task (animals naming) 4. walking + arithmetic task (counting backwards from 50 by subtracting serial 3 s) |
1. manual 2. auditory -verbal 3. auditory -verbal |
GAITRite, 10 (m) |
walking speed (m/s), step length (cm), double support time (ms) step width (mm), step time (ms) |
1a. Non-fallers (0 falls) and Fallers (1 or more falls) + motor task (cup): walking speed (m/s) ↑ 1b. Non-fallers (0 falls) and Fallers (1 or more falls) + motor task (tray): walking speed (m/s) ↑ 1c. Non-fallers (0 falls) and Fallers (1 or more falls) + word task: walking speed (m/s) ↓ 1d. Non-fallers (0 falls) and Fallers (1 or more falls) + arithmetic task: walking speed (m/s) ↓ |
| Reelick et al., 2011 [81] |
1. walking + arithmetic task (counting backwards from 100 by subtracting serial 7 s) 2. walking + word task (naming words starting with a given letter) |
1. auditory -verbal 2. auditory -verbal |
GAITRite, 6.1 (m) |
gait velocity (cm/s), stride length (cm) Number of strides (n), stride length CV (%), stride time (cm), stride time CV, stride width (cm), stride with CV (%) |
1. Non-multiple Fallers (0 or 1 fall) and Multiple Fallers (zer0o or 1 fall) + arithmetic task: gait velocity (cm/s) ↓, Number of strides (n) ↑, stride length (cm) ↓, stride length CV (%) ↑ 2. Non-multiple Fallers (0 or 1 fall) and Multiple Fallers (0 or 1 fall) + word task: gait velocity (cm/s) ↓, Number of strides (n) ↑, stride length (cm) ↓, stride length CV (%) ↑ Stride-length CV was higher when participants performed a DT, and higher in recurrent fallers compared with non-recurrent fallers, although this difference was only significant during performance of the verbal fluency task |
| Springer et al., 2006 [82] |
1. walking + listening 2. walking + listening plus answering questions3. walking + arithmetic task (counting backwards from 500 by subtracting serials 7 s) |
1. auditory -verbal2. auditory -verbal | force-sensitive insoles, 25 (m) |
gait speed (m/sec) ➔ Gait speed was normalized with height, average swing time (%) swing time variability CV (%) |
In swing time variability fallers and elderly non-fallers differed (p = 0.003) |
| Toulotte et al., 2006a [83] | walking + motor task (carrying a glass) | manual | VICON 370 system (Oxford Metrics), Three AMTI force plates (250 Hz), 10 (m) |
cadence (steps/min), walking speed (m/s), stride length (m) stride time (s), step time (s), single-support time (s) |
1. Non-Fallers (0 Falls): cadence (steps/min) ↓, walking speed (m/s) →, stride length (m) ↑, stride time (s), single-support time (s) 2. Fallers (1 or more falls): cadence (steps/min) ↓, walking speed (m/s) ↓, stride length (m) ↓ |
| Toulotte et al., 2006b [84] | walking + motor task (carrying a glass) | manual | VICON 370 system (Oxford Metrics), Three AMTI force plates (250 Hz), 10 (m) | cadence (steps/min), walking speed (m/s), stride length (cm), step length (cm), single support time (s) |
1. Non-Fallers (0 Falls): cadence (steps/min) ↓, walking speed (m/s) ↓, stride length (cm) ↓, step length (cm) ↑, stride time (s) ↑, step time (s) ↓, single-support time (s) ↓ 2. Fallers (1 or more falls): cadence (steps/min) ↓, walking speed (m/s) ↓, stride length (cm) ↓, step length (cm) ↓, stride time (s) ↑, step time (s) ↓, single-support time (s) ↑ Significant difference (P < 0.05) between the fallers and non-fallers under DT-conditions for cadence, walking speed, stride time, step time and single-support time. |
| Verghese et al., 2017 [85] | walking + word task (reciting alternate letters of the alphabet) | auditory -verbal | electronic walkway (Zenometrics LLC, Peekskill, NY), 14 (ft) | cadence (steps/min), walking speed (m/s), stride length (cm), step length (cm), double support time (%) stride time (s), step time (s) | 1. Non-fallers (0 falls) and Non-multiple fallers (0 or 1 fall) Fallers (1 or more falls), Multiple fallers (2 or more falls):cadence (steps/min) ↓, walking speed (m/s) ↓, stride length (cm) ↓, step length (cm) ↓, stride time (s), step time (s), double support time (%) ↑ |
| Asai et al., 2014 [87] |
1. walking + arithmetic task (counting backwards from 100 by subtracting serials 1 s) 2. walking + motor task (carrying a ball on a tray) |
1. auditory- verbal 2. auditory- motor |
triaxial accelerometer, 20(m) |
walking speed (m/s) STV (%), RMS in the ML direction (m/s2), RMS in the AP direction (m/s2), Standardized RMS in the ML direction (%), Standardized RMS in the AP direction (%) |
1. no-FOF and FOF and arithmetic task: walking speed (m/s) ↓, STV (%) ↑, Standardized RMS in the ML direction (%) ↑, Standardized RMS in the AP direction (%) ↑ 1b.no-FOF and FOF and motor task: walking speed (m/s) ↓, STV (%) ↑, Standardized RMS in the ML direction (%) ↓, Standardized RMS in the AP direction (%) ↓ Subjects with FoF walked slower during cognitive-task gait than subjects without FoF and walked with greater STV during single-task gait than subjects without. |
| Donoghue et al., 2013 [88] | walking + verbal fluency task (recite alternate letters of the alphabet (A-C-E, etc.)) | auditory- verbal | GAITRite, 4.88 (m) |
gait speed (m/s), stride length (m), Double support phase (%), stride length CV(%), stride time CV (%), step width (cm) |
1. no-FOF, FOF-NAR, FOF-AR: gait speed (m/s) ↓, stride length (m) ↓, Double support phase (%) ↑, stride length CV (%) ↑, stride time CV (%) ↑, step width (cm)↑ FOF-NAR and FOF-AR groups significantly different to no-FOF group in gait speed (p > 0.001), stride length (p > 0.001), an DSP (p > 0.001). |
| Reelick et al., 2009 [89] |
1. walking +arithmetic task (counting backwards by subtracting serial 7 s) 2. walking +verbal fluency task |
1. auditory- verbal 2. auditory- motor |
GAITRite, Balance during walking(SwayStar), 10 (m) |
gait velocity (cm/s) Stride-length variability (% CV), Stride-time variability (% CV), Mediolateral angular displacement (deg.), Mediolateral angular velocity (deg./s |
1. no-FOF and FOF and arithmetic task: gait velocity (cm/s) ↓, Stride-length variability (% CV) ↑, Stride-time variabilit (% CV) ↑, Mediolateral angular displacement (deg.) ↑, Mediolateral angular velocity (deg./s) ↑ 2. no-FOF and FOF and verbal fluency task: gait velocity (cm/s) ↓, Stride-length variability (% CV) ↑, Stride-time variability (% CV) ↑, Mediolateral angular displacement (deg.) ↑, Mediolateral angular velocity (deg./s) ↑ Significantly lower gait velocity for walking at the preferred velocity and during the performance of both dual tasks in the FoF group compared to the no-FoF group. Stride-length and stride time variability were significantly higher in the FoF group dur.ing DT Stride-time variability was also significantly higher in the FoF group when walking at the preferred gait velocity and while performing the arithmetic task. |
| Wollesen et al., 2017 [90] | walking + visual Stroop task (recite colours, not words) | auditory- verbal | treadmill (h/p/cosmos, Zebris; Isny, Germany: FDM-T) |
step length (cm) step width (cm), and gait line (mm) |
Intervention with FES-I < 20: and FES-I > 20 step length (cm) ↑, step width (cm) ↓, and gait line (mm) ↑ Control group with FES-I < 20: step length (cm) ↓, step width (cm) ↑, and gait line (mm) ↑ Control group with FES-I > 20: step length (cm) ↑, step width (cm) ↑, and gait line (mm) ↑: |
Legend: FOF Fear of falling, FOF-NAR Fear of falling with no activity restriction, FOF-AR Fear of falling with activity restriction, CoF Concern of falling, DSP Double support phase, CV Coefficient of variation, COP Center of pressure, COP-Vel Center of pressure velocity, ML Medio-lateral direction, AP Anterior-posterior direction
Statistical analysis of the meta-analysis
For each of the outcome variables of interest (gait speed, cadence, stride length, step length; see Table 2) we collected the gait data for single and dual-task performance. The gait data was presented as differences in means (MD), since the outcome measurements were made or could be converted on the same scale (e.g., meters per seconds). Most of the studies reported means and SDs permitting effect size estimation, otherwise, they were derived from other summary statistics reported in the articles, such as t-values or p-values. The gait data from individual studies were then pooled in meta-analyses to estimate the overall effect of cognitive-motor interference of gait. Studies were grouped by cognitive task domain and individual meta-analyses were conducted for each outcome: gait speed, cadence, stride length and step length.
In order to determine whether studies shared the same overall effect size or whether the overall effect for a given outcome was modified by certain factors, we conducted a subgroup analyses on studies that directly compared two factors of interest (e.g., arithmetic task vs. verbal fluency tasks) or two groups of participants (e.g., fallers vs. non-fallers) within the same study. Subgroup analyses were conducted using a mixed-effects model and the summary effects within subgroups were computed using a random-effects model. Moreover, to further analyse the differences between fallers and non-fallers as well as participants with and without CoF, DTC were calculated by subtracting the DT values from the ST values. A random-effects model with a generic inverse variance method was used in the pooled analyses, which gives more weight to studies with less variance. Results are presented as effect size with 95% confidence interval (CI) and respective values for null hypothesis tests (e.g., cognitive-motor interference has no effect on gait). Heterogeneity between studies was investigated by calculating the Q-value and I2 statistic which quantified the proportion variation that is due to heterogeneity rather than chance. Quantitative syntheses and meta-analyses were produced using Review Manager 5 Software (RevMan 5).
Results
Databases and references identified 2,670 unique articles for consideration. After abstract consideration and title screening, a total of 71 studies were included for further consideration. Reasons for exclusion were studies using participants with neurological disease (e.g., Multiple Sclerosis, Stroke), studies using obstacle negotiation or Reviews. After applying the inclusion criteria, 19 studies were assessed for quality and 16 papers were included in the meta-analysis (cf. Fig. 1; for excluded studies cf. Table 6 and Table 7).
Fig. 1.
Flow chart of the systematic review procedure
Table 6.
Excluded paper
| Excluded papers | Reason for exclusion |
|---|---|
| Beauchet, O., Allali, G., Annweiler, C., Berrut, G., Maarouf, N., Herrmann, F. R., & Dubost, V. (2008). Does change in gait while counting backward predict the occurrence of a first fall in older adults? Gerontology, 54(4), 217–223. [96] | Similar study with the same data set included in the study |
| Faulkner, K. A., Redfern, M. S., Cauley, J. A., Landsittel, D. P., Studenski, S. A., Rosano, C., et al. (2007). Multitasking: Association between poorer performance and a history of recurrent falls: Association between poorer performance and a history of recurrent falls. Journal of the American Geriatrics Society, 55(4), 570–576. [10] | No discrimination between Fallers and Non-Fallers possible for ST and DT gait data |
| Kressig, R. W., Herrmann, F. R., Grandjean, R., Michel, J. P., & Beauchet, O. (2008). Gait variability while dual-tasking: Fall predictor in older inpatients? Aging Clinical & Experimental Research, 20(2), 123–130. [97] | Observed Inpations and only falls in hospital |
| Hadjistavropoulos, T., Carleton, R. N., Delbaere, K., Barden, J., Zwakhalen, S., Fitzgerald, B., et al. (2012). The relationship of fear of falling and balance confidence with balance and dual tasking performance. Psychology & Aging, 27(1), 1–13. [98] | No discrimination between Fallers and Non-Fallers possible |
| Halvarsson, A., Oddsson, L., Olsson, E., Faren, E., Pettersson, A., & Stahle, A. (2011). Effects of new, individually adjusted, progressive balance group training for elderly people with fear of falling and tend to fall: A randomized controlled trial. [Erratum appears in Clin Rehabil. 2012 Nov;26(11):1055 Note: Oddsson, Lars [added]]. Clinical Rehabilitation, 25(11), 1021–1031. [99] | No discrimination between Fallers and Non-Fallers possible |
| Halvarsson, A., Franzén, E., Farén, E., Olsson, E., Oddsson, L., & Ståhle, A. (2013). Long-term effects of new progressive group balance training for elderly people with increased risk of falling - a randomized controlled trial. Clinical Rehabilitation, 27(5), 450–458. [100] | No discrimination between Fallers and Non-Fallers possible |
| Herman, T., Mirelman, A., Giladi, N., Schweiger, A., & Hausdorff, J. M. (2010). Executive Control Deficits as a Prodrome to Falls in Healthy Older Adults: A Prospective Study Linking Thinking, Walking, and Falling. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 65A(10), 1086–1092. [101] | Similar study with the same data set included in the study |
| MacAulay, R. K., Allaire, T. D., Brouillette, R. M., Foil, H. C., Bruce-Keller, A. J., Han, H., et al. (2015). Longitudinal assessment of neuropsychological and temporal/spatial gait characteristics of elderly fallers: Taking it all in stride. Frontiers in Aging Neuroscience, 7 2015. [102] | No mean and SD discrimination between Fallers and Non-Fallers possible |
| Rinaldi, N. M., & Moraes, R. (2016). Older adults with history of falls are unable to perform walking and prehension movements simultaneously. Neuroscience, 316, 249–260. [103] | No discrimination between Fallers and Non-Fallers possible |
| Rogan S., Taeymans J., Bangerter C., Simon S., Terrier P., Hilfiker R. (2019). Einfluss von Einfach- und Doppelaufgaben auf Gangstabilitat und Ganggeschwindigkeit bei alteren Menschen: Eine explorative Studie, Influence of single and dual tasks on gait stability and gait speed in the elderly: An explorative study. Zeitschrift fur Gerontologie und Geriatrie.52, (1), 23–27 [104] | No discrimination between Fallers and Non-Fallers possible |
| Yamada, M., Aoyama, T., Nakamura, M., Tanaka, B., Nagai, K., Tatematsu, N., et al. (2011). The reliability and preliminary validity of game-based fall risk assessment in community-dwelling older adults. Geriatric Nursing, 32(3), 188–194. [86] | Low Quality score |
| Yogev, G., Plotnik, M., Peretz, C., Giladi, N., & Hausdorff, J. M. (2007). Gait asymmetry in patients with Parkinson’s disease and elderly fallers: When does the bilateral coordination of gait require attention? Experimental Brain Research, 177(3), 336–346. [105] | Similar study with the same data set included in the study |
Table 7.
Excluded paper meta-analysis
| Excluded papers | Reason for exclusion |
|---|---|
| Bootsma-van, d., Gussekloo, J., de, C., van, E., Bloem, B. R., & Westendorp, R. G. (2003). Walking and talking as predictors of falls in the general population: The Leiden 85-Plus Study. Journal of the American Geriatrics Society, 51(10), 1466–1471. | No Means and SD (only Median and IQR) |
| Johansson, J., Nordström, A., & Nordström, P. (2016). Greater Fall Risk in Elderly Women Than in Men Is Associated With Increased Gait Variability During Multitasking. Journal of the American Medical Directors Association, 17(6), 535–540. | No mean and SD discrimination between Fallers and Non-Fallers possible |
| Reelick, M. F., Kessels, R. P., Faes, M. C., Weerdesteyn, V., Esselink, R. A., & Rikkert, M. G. O. (2011). Increased intra-individual variability in stride length and reaction time in recurrent older fallers. Aging clinical and experimental research, 23(5–6), 393–399.LL | No mean and SD discrimination between Fallers and Non-Fallers possible |
Thirteen studies showed high quality scores (> 16) and seven studies were of good quality (according to [71]). The study by Yamada et al. [86] was excluded due to a quality score < 10. Table 4 gives an overview of all included studies addressing the comparison of fallers vs. non-fallers and participants with and without concerns about falling. The study by Wollesen et al. [90] could not be integrated into the meta-analysis because they used a fixed gait speed in their measurement design.
Fallers vs. non-fallers
Description of the included studies comparing fallers and non- fallers (N = 15)
The mean age of the study population was between 67 years [21, 84, 85] and 87 years [19]. The sample sizes of the studies varied between N = 16 [84, 85] and N = 1350 [78].
Five studies included a prospective design [19, 74, 76, 77, 85].
The included studies used the following dual-task settings:
Arithmetic tasks: n = 7 studies used counting backward tasks [19, 20, 74, 75, 80–82], conducted as counting in steps of one (n = 3), three (n = 3) or seven (n = 3) (cf. Table 3).
Verbal fluency tasks: n = 7 studies used verbal fluency tasks [20, 21, 75–77, 80, 81]
Motor tasks: n = 5 studies used a motor task [20, 21, 80, 83, 85]
Other tasks: visuo-spatial task [20], Stroop task [20], listening and memory task [82] and reciting of letters of the alphabet [85].
A total number of six studies analysed more than one task [20, 21, 75, 80–82].
Overall, the studies comparing fallers and non-fallers examined 32 different gait quality variables. Gait speed or velocity was assessed by n = 14 studies [19–21, 74, 75, 77–85]. Other gait measures included duration to walk a defined distance (n = 2) [19, 77], step length (n = 3) [21, 80, 85], stride length (n = 4) [14, 83–85], cadence (n = 6) [19, 21, 77, 83–85], step time (n = 3) [80, 83, 85], stride time (n = 5) [21, 77, 81, 83, 85] and double support time (n = 3) [77, 80, 85]. Several studies used gait parameters of variability (n = 14; eg.: stride time variability (n = 3), gait speed variability (n = 2) and swing time variability (n = 2)). In addition, some studies focused on Center of pressure (CoP) or Center of mass (CoM) displacements, or mechanical power in anterior (AP) and medio-lateral (ML) direction during gait cycles. These outcomes were not included into the meta-analysis because of lack of consistency in calculation methods among studies or infrequent use. To measure gait characteristics, a stopwatch (n = 6; from 10 m up to 30 m distance), the GAITrite rite system or another electronic walkway (n = 8; from 8 m up to 12 m), camera systems (e.g., Vicon n = 3) or insoles (e.g., F-Scan n = 3) were used.
Differences on cognitive-motor dual task performance between non-fallers and fallers
Four studies could not be integrated into the meta-analysis because the mean values and SD for the analysed gait data were not reported in comparison of non-fallers and fallers and unavailable after attempting to contact the authors [76, 78, 81]. Independent of the task settings, there were no differences of the gait decrements under DT conditions between fallers and non-fallers (cf. Table 5). Mostly, fallers showed reduced performance of the spatiotemporal gait parameters in comparison to non-fallers. Only two studies used a coefficient of variation [81, 82] and revealed significant differences between fallers and non-fallers with increased variation in fallers. Reelick [81] found a significantly reduced walking performance for the verbal fluency task in comparison to the arithmetic task. Nordin et al. [80] also revealed differences for their task conditions; gait speed increased for the motor-tasks (carrying a cup or a tray) and gait speed decreased for the cognitive conditions (verbal fluency and counting backwards) fallers compared to non-fallers.
Results of the meta-analysis fallers vs. non-fallers
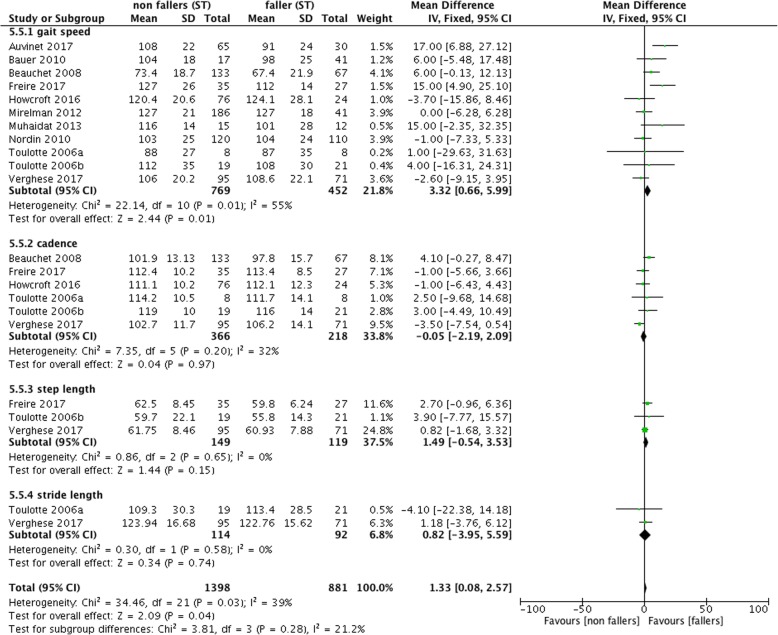
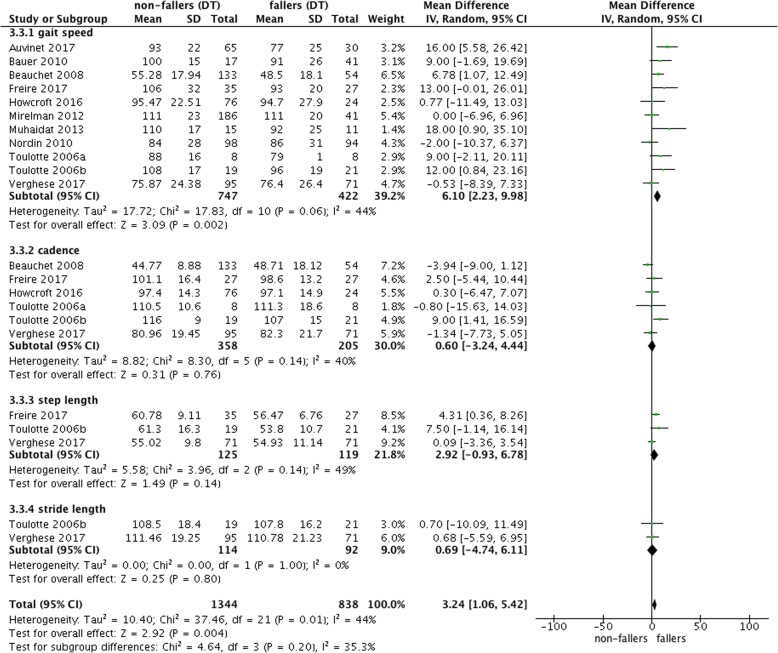
The forest plot of Fig. 2 shows significant mean difference of 3.32 [95% confidence interval 0.66–5.99] between non-fallers and fallers for ST gait speed with reduced performance for fallers. However, these results were heterogeneous (I2 = 39%; cf. Fig. 2). There were no effects for step length or stride length. Under DT conditions, fallers had a reduced gait speed in comparison to non-fallers with a mean difference of 6.10 [2.23–9.98] (I2 = 44%; cf. Fig. 3).
Fig. 2.
Forest plot meta-analysis of ST performance between non-fallers and fallers
Fig. 3.
Forest plot meta-analysis of dual-task effect on gait different gait measurement between non-fallers and fallers
Figure 4 repeats the findings for gait speed under ST and DT conditions and shows the mean difference in DTC (defined as DT minus ST). The meta-analysis showed that there were higher decrements in gait speed for fallers in comparison to non-fallers under DT conditions. However, if the DTC were calculated (Fig. 4), there were no reduced DTC observed for non-fallers.
Fig. 4.
Comparisons of ST and DT gait speed and resulting dual task costs (DTC)
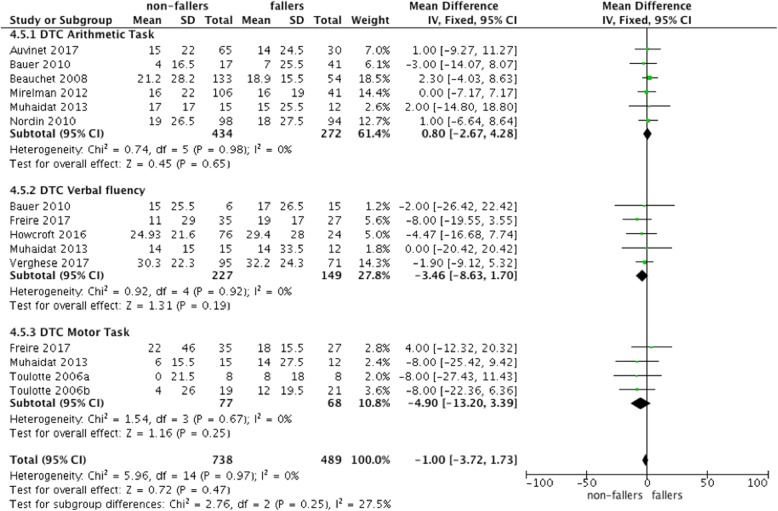
Figure 5 visualizes the DTC for the different cognitive task domains. Increased DTC for fallers compared to non-fallers could only be observed for verbal fluency and motor dual-tasks but failed to be significant. The overall effect of the different task conditions was also not significant.
Fig. 5.
Comparisons of ST and DT and resulting DTC for the different task conditions
Participants with concerns about falling vs no concerns about falling
Description of the includes studies (N = 4) comparing participants with CoF
The mean age of the study population was 69.8 years [90] up to 80.6 years [89]. Sample sizes varied between N = 85 [90] and N = 1307 [88]. The included studies used different dual-task settings:
Arithmetic tasks: The study by Reelick [100] used a counting backward tasks (subtracting 7 s) and the study by Asai [87] used a counting backward task (subtracting 1 s) (cf. Table 4).
Verbal fluency tasks: Donoghue et al. [88] (recite alternative letters of the alphabet) and Reelick et al. [89] (naming animal species as much as possible) used a verbal fluency task.
Other tasks: The RCT by Wollesen et al. [90] was conducted with a visual-verbal Stroop task.
Studies comparing participants with and without CoF examined 16 different gait variables (cf. Table 5); i.e. gait speed (n = 3), stride time variability (n = 1), step width (n = 2), step length (n = 1), stride length (n = 2). Two studies used different variability calculations (n = 2). Moreover, two studies [87, 89] focused on CoP or CoM displacements in AP and ML direction during gait cycles. To measure gait performance, the GAITrite system or another electronic walkway (n = 2; from 5 m up to 10 m), a triaxial accelerometer (n = 1) or a treadmill (n = 1) were used (cf. Table 5).
Differences on cognitive-motor-performance between participants with and without concerns about falling
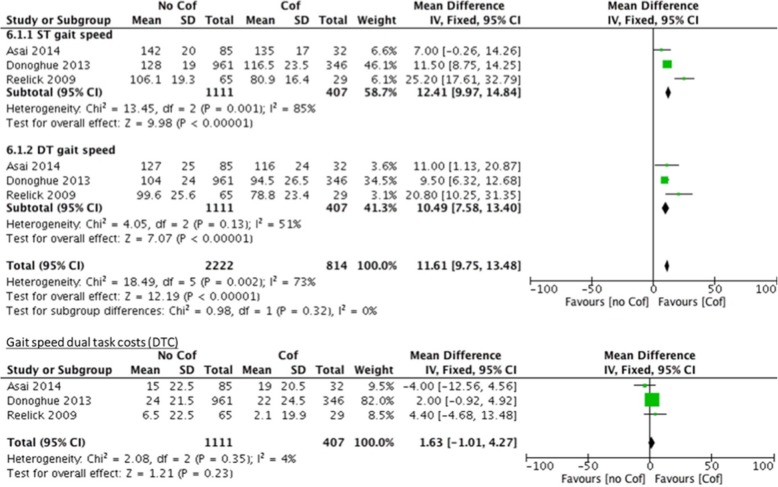
As reported in Table 5 participants with and without CoF showed comparable DTC. Moreover, all studies showed that participants with CoF had a poorer walking quality (e.g., reduced walking speed with accompanying step length or increased variability) in the ST condition compared to people without CoF. With regard to the different task settings, the two studies that examined two different cognitive dual-tasks found different reactions in all participants according to the task. The study of Asai et al. [87] analysed an arithmetic DT situation and a motor-motor DT situation; and found that both tasks resulted in reduced walking speed. The motor-motor DT resulted in reduced (and therefore improved) body sway in ML and AP direction in comparison to the arithmetic DT situation. Reelick et al. [90] investigated an arithmetic DT situation and a verbal fluency task, and found no task differences. The meta-analysis revealed a significant difference of gait speed between participants with and without CoF under ST (mean difference: 12.41 [9.97–14.84]) and DT (mean difference: 10.61 [7.58–13.40]) conditions. The differences for the DTC failed to show significance (mean difference: 1.63 [− 1.01–4.27]; cf. Fig. 6).
Fig. 6.
Comparisons of ST and DT and resulting DTC for participants with and without concerns about falling
Discussion
The aim of this systematic review and meta-analysis was to provide a taxonomy of different dual-task settings and test their relations to cognitive-motor decrements with fall risk and CoF. Additionally, the cognitive tasks were regarded separately with the purpose to find a dual-task taxonomy or classification of the DT settings that are most beneficial to identify cognitive-motor interference in older fallers and older people with CoF.
Differences of DT performance on spatiotemporal gait parameters between non-fallers and fallers
The results of the meta-analysis suggested that gait speed and cadence in ST and DT conditions can discriminate between fallers and non-fallers. Studies classifying people as fallers and non-fallers were based primarily on retrospective falls, with only two studies being prospective [19, 96]. These results confirm previous systematic review evidence which showed differences in gait speed between fallers and non-fallers [50, 68]. With regard to the associated DTC, only five of eleven studies found higher decrements in gait speed from ST to DT for fallers in comparison to non-fallers (Fig. 4). The overall DTC failed to be significant between these two groups in our meta-analysis. There were only small amounts of DTC for both groups and the standard deviations were large. In line with the results of other studies that could not be included in the meta-analysis, fallers and non-fallers both show decrements in gait speed in ST and DT conditions (cf. Table 5 and Fig. 4). These decrements are not significantly different between groups which is inconsistent with the hypothesis that non-fallers and fallers differ in their ability of task prioritization [16, 67]. Fallers walk significantly slower than non-fallers in ST conditions; however, step length and stride length, which are known to be highly correlated with gait speed [91], did not differ significantly between groups. Specific recommendations on whether or not cognitive-motor-interference increases fall risk cannot be provided. These results confirm the findings by Zijlstra et al. [68] and Menant et al. [50] who also reported no additional benefit of DT walking as a measurement to discriminate fallers from non-fallers. Nevertheless, it is important to note that gait performance includes different components of functional performance such as maximal walking velocity, gait economy, walking effectiveness, efficiency and safety. These aspects might be more relevant to estimate fall risk. Therefore, future studies should address these components of gait performance in tailored DT settings.
Differences of DT performance between participants with and without CoF
People with CoF showed greater gait decrements under ST and DT conditions compared to people without CoF. The overall effects from the meta-analysis suggested that the effects of CoF were larger (11.61; CI: 9.75–13.48) in fallers compared to non-fallers (4.12; CI: 2.20–6.03). CoF is common in people with and without a previous fall history and the prevalence rates are higher than falls themselves [93]. It has been suggested that people with CoF have difficulty inhibiting or ignoring irrelevant information of the environment when controlling their balance in complex and DT situations [40]. Many daily life activities include some level of dual-tasking in which executive functioning or performance (i.e. inhibition) are required. CoF might compete for these limited resources of attentional focus to maintain their balance [52], which would result in a more pronounced slowing of their walking speed under DT conditions (cf. Fig. 6) in people with CoF irrespective of their fall history or fall risk. However, our analyses were not able to confirm this hypothesis as DTC was not significantly different between people with and without CoF.
Influence of the task condition
A large variety of cognitive tasks have been used to assess cognitive-motor interference in the literature. As part of this review, a total of 11 different DT-conditions were used to compare non-fallers and fallers on DT walking performance (Fig. 5). According to the proposed taxonomy (Table 1) mental tracking tasks, especially counting backward tasks by numbers in 1 s, 3 s or 7 s are the most commonly used task sets. Overall, we were able to compare three types of cognitive dual-tasks (i.e. arithmetic, verbal fluency and motor tasks) within the meta-analysis of this review. Two of them belong to the same category of our taxonomy (mental tracking, cf. Table 1). The third one included an additional motor task. However, all task settings affected DTC similarly, and the pooled effect (mean difference: − 1.00 [− 3.72–1.73]) had low heterogeneity (I2 = 0%).
Other cognitive tasks such as reaction time and decision making tasks for processing speed and controlled processing tasks, [92] were not integrated in the task setting of the included studies but could be relevant for navigating in daily traffic situations. In addition, previous studies have suggested that more complex tasks such as working memory tasks, discrimination tasks or visuospatial tasks would have a greater impact on the DTC (for an overview see Lacour et al. [52]) but this could not be confirmed by this review due to the limited studies using these tasks. Furthermore, within the available data there were also no marked differences between the different types of cognitive tasks. On the other hand, there is evidence that mental tracking tasks like verbal fluency tasks increase the DTC more significantly for fallers compared to non-fallers [81], due to the additional load on the working memory for these tasks. However, this review was not able to confirm this hypothesis. Finally, motor-motor DT condition also did not show significant differences in DTC between non-fallers and fallers. Both studies by Toulotte et al. [83, 84] suggested a more pronounced DTC when carrying in glass of water, suggesting this would slow participants down as they need to observe the glass of water in their hand. However, other studies have suggested the opposite [80], as a result of a forward flexion of the trunk when carrying a tray with a glass of water in front of the body.
Implications of the results
Similar to previous reviews, we were not able to confirm differences between fallers and non-fallers in DTC. One reason for this result might be that we were only able to compare three types of dual-task settings (i.e. arithmetic, verbal fluency and motor tasks) within the meta-analysis. Therefore, additional studies are required to examine the discriminatory ability of walking performance with and without concurrent reaction time, controlled processing, visuospatial, working memory and discrimination tasks. Study designs comparing different DT-settings in smaller samples [20] or randomised trials with a representative larger sample size could be used to systematically address different cognitive processes and their complexities. In addition, it might be important to consider an individual’s biography before deciding on a DT. One might argue, that a maths teacher might find a counting backwards task more intuitive, while a librarian might be more comfortable with verbal fluency tasks. More work is required to test this hypothesis. Tasks that include visuo-spatial information processing or higher executive functions (e.g., inhibition within a Stroop-task) [2] might have greater potential in discriminating between fallers and non-fallers. These tasks may be less dependent on people’s biography. However, these task-settings might be difficult to use in clinical settings and with short walking distances. In addition to the cognitive dimensions of the task settings, the walking conditions and parcourse need to be reflected, as a straight walking course does not sufficiently address real-life gait. The ongoing development of wearable technology might be one solution to overcome measurement set up problems.
Limitations
Overall, the quality of the included studies was good. Nevertheless, there are some issues that need to be discussed. First, spatiotemporal gait parameters were assessed using diverse measurement methods, varying between the crude use of a stopwatch to accelerometers and electronic walkways [94]. Second, there is not a common length of the walking tracks with many studies using distances that are too short to see a DT effect. According to Lindemann et al. [95], the distance to achieve a steady walking state increases with higher gait speed. Third, studies report different spatiotemporal gait parameters. Especially, spatiotemporal gait parameters related to balance, such as step width, double support time, gait stability and variability, were not reported frequently enough to be included in the meta-analysis. It is possible that the effect of DTC would be visible on such measures before it affects gait speed especially over short distances. Fourth, the short distances might influence prioritisation of the motor and cognitive tasks. The short distances also limit the time available for the cognitive dual-task, which might explain why the meta-analysis could not show a different cognitive-motor interference on gait between fallers and non-fallers. Finally, most of the studies did not report the motor and the cognitive DTC. This means that there is no control for the attentional focus of the participants, rendering it unclear if the performance decrements result from the attentional focus or from cognitive-motor interferences. Finally, to gain information about the influence of the DT taxonomy on DTC, this review integrated only studies with straight walking. This was necessary to overcome the problem that gait execution while changing directions, walking in curves or reacting to external perturbation, has a different impact on spatiotemporal gait parameters as well on the cognitive performance.
Conclusions
Overall, the large diversity of studies and types of cognitive dual-tasks do not allow us to provide conclusive recommendations for clinical testing of cognitive-motor interference while walking. In agreement with previous studies [50, 78], we found no additional benefit of DT gait analysis to differentiate between fallers and non-fallers. Similar results were found when comparing people with and without CoF. However, our analyses also reveal that several domains of cognitive dual-tasks have not yet been investigated. The proposed cognitive task taxonomy will assist in systematic assessment of these tasks and their effect on gait.
Acknowledgements
We thank Liesann Seydell for her assistance in formatting the manuscript including the tables.
Appendix
Table 8.
Search strategy
| Keywords | Papers identified | ||
|---|---|---|---|
| Medline | EMBASE | PsycInfo | |
| 1. "Age" or "old$" or "elder$" or "aged" or "advanced age" or "senior$" or "geriatric$" or "eldest" or "aging" or "gerontic" or "faller$" or "fear of falling" | 10.451.411 | 7.016.103 | 1.097.778 |
| 2. "corresponding task$" or "coupled task$" or "dual task$" or "dual task paradigm$" or "secondary task" or "conflicting task" or "task prioritisation" or "inattentional blindness" | 4.200 | 167.739 | 56.654 |
| 3. "gait" or "step length" or "cadence" or "step count" or "step width" or "stance time" or "swing time" or "single support time" or "stride time" or "stride width" or "stride length" or "gait line" or "maximum force forefoot" or "maximum force midfoot" or “maximum force heel” or “double support time” or “gait speed” or “stride speed” or “motion” or “movement$” or “motor$” or “locomotion” or “walking” or “balance” or “posture” not “slipping” (not “perturbation”) | 1.198.325 | 1.374.933 | 349.516 |
| 4. “cognitive” or “neurocognitive” or “cognition$” or “executive” or “processing” or “spatial” or “visuospatial” or “memory” or “reaction$” or “speed” or “decision-making” or “mental” or “attention” or “cognitive-motor” or “motor-cognitive” or “reaction$” or “planning” or inhibition | 4.885.498 | 7.293.833 | 1.589.107 |
| 5. Combination of 1 and 2 and 3 and 4 | 1.515 | 658 | 1.134 |
Authors’ contributions
The manuscript was written by BW with the help of MS, KVS and KD. The search was conducted by BW and MW independently. The quality assessment was done by BW and MS and reviewed by KVS. The meta-analysis was done by BW and KD. All authors read and approved the final manuscript.
Funding
There was no funding received for this study.
Availability of data and materials
The supporting data is available via the corresponding author.
Ethics approval and consent to participate
There was no Ethical approval required as the study was a systematic review. This review was registered at Prospero with the ID: CRD42017068912.
Consent for publication
All authors have approved the manuscript and agree with its submission to “European Review of Aging and Physical activity”.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
B. Wollesen, Email: bettina.wollesen@uni-hamburg.de
M. Wanstrath, Email: Matthias.Wanstrath@bgw-online.de
K. S. van Schooten, Email: k.vanschooten@neura.edu.au
K. Delbaere, Email: k.delbaere@neura.edu.au
References
- 1.Al-Yahya E, Dawes H, Smith L, Dennis A, Howells K, Cockburn J. Cognitive motor interference while walking: A systematic review and meta-analysis. Neurosci Biobehav Rev. 2011;35(3):715–728. doi: 10.1016/j.neubiorev.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 2.Bock O. Dual-task costs while walking increase in old age for some, but not for other tasks: an experimental study of healthy young and elderly persons. J Neuroeng Rehabil. 2008;5(1):27. doi: 10.1186/1743-0003-5-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hollman JH, Kovash FM, Kubik JJ, Linbo RA. Age-related differences in spatiotemporal markers of gait stability during dual task walking. Gait Posture. 2007;26(1):113–119. doi: 10.1016/j.gaitpost.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 4.Wollesen B, Mattes K, Rönnfeldt J. Influence of age, gender and test conditions on the reproducibility of dual-task walking performance.Aging clinical and experimental research. 2017;29(4):761-69. [DOI] [PubMed]
- 5.Beurskens R, Bock O. Age-related deficits of dual-task walking: a review. Neural Plast. 2012;2012(4):1–9. doi: 10.1155/2012/131608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lindenberger U, Marsiske M, Baltes PB. Memorizing while walking: increase in dual-task costs from young adulthood to old age. Psychol Aging. 2000;15(3):417–436. doi: 10.1037/0882-7974.15.3.417. [DOI] [PubMed] [Google Scholar]
- 7.Collin G, van den Heuvel MP. The ontogeny of the human connectome: development and dynamic changes of brain connectivity across the life span. Neuroscientist. 2013;19(6):616–628. doi: 10.1177/1073858413503712. [DOI] [PubMed] [Google Scholar]
- 8.Hedman AM, van Haren NEM, Schnack HG, Kahn RS, Hulshoff Pol HE. Human brain changes across the life span: a review of 56 longitudinal magnetic resonance imaging studies. Hum Brain Mapp. 2012;33(8):1987–2002. doi: 10.1002/hbm.21334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hedden T, Gabrieli JDE. Insights into the ageing mind: a view from cognitive neuroscience. Nat Rev Neurosci. 2004;5(2):87–96. doi: 10.1038/nrn1323. [DOI] [PubMed] [Google Scholar]
- 10.Faulkner KA, Redfern MS, Cauley JA, Landsittel DP, Studenski SA, Rosano C, et al. Multitasking: association between poorer performance and a history of recurrent falls. J Am Geriatr Soc. 2007;55(4):570–576. doi: 10.1111/j.1532-5415.2007.01147.x. [DOI] [PubMed] [Google Scholar]
- 11.Li KZH, Lindenberger U. Relations between aging sensory/sensorimotor and cognitive functions. Neurosci Biobehav Rev. 2002;26(7):777–783. doi: 10.1016/S0149-7634(02)00073-8. [DOI] [PubMed] [Google Scholar]
- 12.Holtzer R, Wang C, Verghese J. Performance variance on walking while talking tasks: theory, findings, and clinical implications. Age. 2014;36(1):373–381. doi: 10.1007/s11357-013-9570-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cornu V, Steinmetz J-P, Federspiel C. Deficits in selective attention alter gait in frail older adults. GeroPsych. 2016;29(1):29–36. doi: 10.1024/1662-9647/a000137. [DOI] [Google Scholar]
- 14.MacAulay RK, Allaire TD, Brouillette RM, Foil HC, Bruce-Keller AJ, Han H, et al. Longitudinal assessment of neuropsychological and temporal/spatial gait characteristics of elderly fallers: taking it all in stride. Front Aging Neurosci. 2015;7:70. doi: 10.3389/fnagi.2015.00034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Amboni M, Barone P, Hausdorff JM. Cognitive contributions to gait and falls: evidence and implications. Mov Disord. 2013;28(11):1520–1533. doi: 10.1002/mds.25674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muir-Hunter SW, Wittwer JE. Dual-task testing to predict falls in community-dwelling older adults: a systematic review. Physiotherapy. 2016;102(1):29–40. doi: 10.1016/j.physio.2015.04.011. [DOI] [PubMed] [Google Scholar]
- 17.van Schooten KS, Freiberger E, Smitt MS, Keppner V, Sieber C, Lord SR, Delbaere K. Concern About Falling Is Associated With Gait Speed, Independently From Physical and Cognitive Function. Physical Therapy. 2019;pzz032:1-21. 10.1093/ptj/pzz032. [DOI] [PubMed]
- 18.Maki BE. Gait changes in older adults: predictors of falls or indicators of fear. J Am Geriatr Soc. 1997;45(3):313–320. doi: 10.1111/j.1532-5415.1997.tb00946.x. [DOI] [PubMed] [Google Scholar]
- 19.Beauchet O, Annweiler C, Allali G, Berrut G, Herrmann FR, Dubost V. Recurrent falls and dual task–related decrease in walking speed: is there a relationship? J Am Geriatr Soc. 2008;56(7):1265–1269. doi: 10.1111/j.1532-5415.2008.01766.x. [DOI] [PubMed] [Google Scholar]
- 20.Muhaidat J, Kerr A, Evans JJ, Skelton DA. The test–retest reliability of gait-related dual task performance in community-dwelling fallers and non-fallers. Gait Posture. 2013;38(1):43–50. doi: 10.1016/j.gaitpost.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 21.Freire Júnior RC, Porto JM, Marques NR, Magnani PE, Abreu DC. The effects of a simultaneous cognitive or motor task on the kinematics of walking in older fallers and non-fallers. Hum Mov Sci. 2017;51:146–152. doi: 10.1016/j.humov.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 22.Nagamatsu LS, Voss M, Neider MB, Gaspar JG, Handy TC, Kramer AF, Liu-Ambrose TYL. Increased cognitive load leads to impaired mobility decisions in seniors at risk for falls. Psychol Aging. 2011;26(2):253–259. doi: 10.1037/a0022929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Neider MB, Gaspar JG, McCarley JS, Crowell JA, Kaczmarski H, Kramer AF. Walking and talking: dual-task effects on street crossing behavior in older adults. Psychol Aging. 2011;26(2):260–268. doi: 10.1037/a0021566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Craik FI, Salthouse TA, editors. The handbook of aging and cognition. New York: Psychology Press; 2011. p. 3.
- 25.Colcombe S, Kramer AF. Fitness effects on the cognitive function of older adults: a meta-analytic study. Psychol Sci. 2003;14(2):125–130. doi: 10.1111/1467-9280.t01-1-01430. [DOI] [PubMed] [Google Scholar]
- 26.Strauss E, Sherman EM, Spreen O. A compendium of neuropsychological tests: Administration, norms, and commentary. New York: Oxford University Press; 2006. p.3
- 27.Lezak MD, Howieson DB, Loring DW, Fischer JS. Neuropsychological assessment. USA: Oxford University Press; 2004. [Google Scholar]
- 28.Manna CG, Alterescu K, Borod JC, Bender HA. Encyclopedia of clinical neuropsychology. New York: Springer; 2011. Benton visual retention test; pp. 392–394. [Google Scholar]
- 29.Williams JMG, Mathews A, MacLeod C. The emotional Stroop task and psychopathology. Psychol Bull. 1996;120(1):3. doi: 10.1037/0033-2909.120.1.3. [DOI] [PubMed] [Google Scholar]
- 30.Baddeley A, Logie R, Bressi S, Sala SD, Spinnler H. Dementia and working memory. Q J Exp Psychol A Hum Exp Psychol. 1986;38(4):603–618. doi: 10.1080/14640748608401616. [DOI] [PubMed] [Google Scholar]
- 31.D'Esposito M, Postle BR, Ballard D, Lease J. Maintenance versus manipulation of information held in working memory: an event-related fMRI study. Brain Cogn. 1999;41(1):66–86. doi: 10.1006/brcg.1999.1096. [DOI] [PubMed] [Google Scholar]
- 32.Barde LH, Thompson-Schill SL. Models of functional organization of the lateral prefrontal cortex in verbal working memory: evidence in favor of the process model. J Cogn Neurosci. 2002;14(7):1054–1063. doi: 10.1162/089892902320474508. [DOI] [PubMed] [Google Scholar]
- 33.MacLeod CM. Half a century of research on the Stroop effect: an integrative review. Psychol Bull. 1991;109(2):163. doi: 10.1037/0033-2909.109.2.163. [DOI] [PubMed] [Google Scholar]
- 34.Pashler H. Dual-task interference in simple tasks: data and theory. Psychol Bull. 1994;116(2):220–244. doi: 10.1037/0033-2909.116.2.220. [DOI] [PubMed] [Google Scholar]
- 35.Pashler H, Johnston JC, Ruthruff E. Attention and performance. Annu Rev Psychol. 2001;52(1):629–651. doi: 10.1146/annurev.psych.52.1.629. [DOI] [PubMed] [Google Scholar]
- 36.Welford AT. Single-channel operation in the brain. Acta Psychol. 1967;27:5–22. doi: 10.1016/0001-6918(67)90040-6. [DOI] [PubMed] [Google Scholar]
- 37.Wickens CD. Multiple resources and performance prediction. Theor Issues Ergon Sci. 2002;3(2):159–177. doi: 10.1080/14639220210123806. [DOI] [Google Scholar]
- 38.Sherrington C, Tiedemann A, Fairhall N, Close JCT, Lord SR. Exercise to prevent falls in older adults: an updated meta-analysis and best practice recommendations. N S W Public Health Bull. 2011;22(4):78. doi: 10.1071/NB10056. [DOI] [PubMed] [Google Scholar]
- 39.Eysenck MW, Derakshan N, Santos R, Calvo MG. Anxiety and cognitive performance: attentional control theory. Emotion. 2007;7(2):336. doi: 10.1037/1528-3542.7.2.336. [DOI] [PubMed] [Google Scholar]
- 40.Young WR, Mark Williams A. How fear of falling can increase fall-risk in older adults: applying psychological theory to practical observations. Gait Posture. 2015;41(1):7–12. doi: 10.1016/j.gaitpost.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 41.Ayoubi F, Launay CP, Annweiler C, Beauchet O. Fear of falling and gait variability in older adults: a systematic review and meta-analysis. J Am Med Dir Assoc. 2015;16(1):14–19. doi: 10.1016/j.jamda.2014.06.020. [DOI] [PubMed] [Google Scholar]
- 42.Donoghue OA, Dooley C, Kenny RA. Usual and dual-task walking speed: implications for pedestrians crossing the road. J Aging Health. 2016;28(5):850–862. doi: 10.1177/0898264315614004. [DOI] [PubMed] [Google Scholar]
- 43.Navon D, Gopher D. On the economy of the human-processing system. Psychol Rev. 1979;86(3):214–255. doi: 10.1037/0033-295X.86.3.214. [DOI] [Google Scholar]
- 44.Spirduso WW, Francis KL, MacRae PG. Physical dimensions of aging. 2. Champaign: Human Kinetics; 2005. [Google Scholar]
- 45.Guttman SE, Gilroy LA, Blake R. Hearing what the eyes see: auditory encoding of visual temporal sequences. Psychol Sci. 2005;16(3):228–235. doi: 10.1111/j.0956-7976.2005.00808.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Patel P, Lamar M, Bhatt T. Effect of type of cognitive task and walking speed on cognitive-motor interference during dual-task walking. Neuroscience. 2014;260:140–148. doi: 10.1016/j.neuroscience.2013.12.016. [DOI] [PubMed] [Google Scholar]
- 47.Hall CD, Echt KV, Wolf SL, Rogers WA. Cognitive and motor mechanisms underlying older adults’ ability to divide attention while walking. Phys Ther. 2011;91(7):1039–1050. doi: 10.2522/ptj.20100114. [DOI] [PubMed] [Google Scholar]
- 48.Li C, Verghese J, Holtzer R. A comparison of two walking while talking paradigms in aging. Gait Posture. 2014;40(3):415–419. doi: 10.1016/j.gaitpost.2014.05.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Maclean LM, Brown LJE, Khadra H, Astell AJ. Observing prioritization effects on cognition and gait: the effect of increased cognitive load on cognitively healthy older adults’ dual-task performance. Gait Posture. 2017;53:139–144. doi: 10.1016/j.gaitpost.2017.01.018. [DOI] [PubMed] [Google Scholar]
- 50.Menant JC, Schoene D, Sarofim M, Lord SR. Single and dual task tests of gait speed are equivalent in the prediction of falls in older people: a systematic review and meta-analysis. Ageing Res Rev. 2014;16:83–104. doi: 10.1016/j.arr.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 51.Venema DM, Bartels E, Siu KC. Tasks matter: a cross-sectional study of the relationship of cognition and dual-task performance in older adults. J Geriatr Phys Ther. 2013;36(3):115–122. doi: 10.1519/JPT.0b013e31827bc36f. [DOI] [PubMed] [Google Scholar]
- 52.Lacour M, Bernard-Demanze L, Dumitrescu M. Posture control, aging, and attention resources: models and posture-analysis methods. Clin Neurophysiol. 2008;38(6):411–421. doi: 10.1016/j.neucli.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 53.Riby L, Perfect T, Stollery B. The effects of age and task domain on dual task performance: A meta-analysis. Eur J Cogn Psychol. 2004;16(6):863–891. doi: 10.1080/09541440340000402. [DOI] [Google Scholar]
- 54.Swan L, Otani H, Loubert PV, Sheffert SM, Dunbar GL. Improving balance by performing a secondary cognitive task. Br J Psychol. 2004;95(1):31–40. doi: 10.1348/000712604322779442. [DOI] [PubMed] [Google Scholar]
- 55.Huxhold O, Li S-C, Schmiedek F, Lindenberger U. Dual-tasking postural control: aging and the effects of cognitive demand in conjunction with focus of attention. Brain Res Bull. 2006;69(3):294–305. doi: 10.1016/j.brainresbull.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 56.Riley MA, Baker AA, Schmit JM. Inverse relation between postural variability and difficulty of a concurrent short-term memory task. Brain Res Bull. 2003;62(3):191–195. doi: 10.1016/j.brainresbull.2003.09.012. [DOI] [PubMed] [Google Scholar]
- 57.Wulf G, Mercer J, McNevin N, Guadagnoli MA. Reciprocal influences of attentional focus on postural and suprapostural task performance. J Mot Behav. 2004;36(2):189–199. doi: 10.3200/JMBR.36.2.189-199. [DOI] [PubMed] [Google Scholar]
- 58.Vuillerme N, Nafati G. How attentional focus on body sway affects postural control during quiet standing. Psychol Res. 2007;71(2):192–200. doi: 10.1007/s00426-005-0018-2. [DOI] [PubMed] [Google Scholar]
- 59.Stoffregen TA, Pagulayan RJ, Bardy BG, Hettinger LJ. Modulating postural control to facilitate visual performance. Hum Mov Sci. 2000;19(2):203–220. doi: 10.1016/S0167-9457(00)00009-9. [DOI] [Google Scholar]
- 60.Stoffregen TA, Smart LJ, Bardy BG, Pagulayan RJ. Postural stabilization of looking. J Exp Psychol Hum Percept Perform. 1999;25(6):1641–1658. doi: 10.1037/0096-1523.25.6.1641. [DOI] [Google Scholar]
- 61.Stoffregen TA, Hove P, Bardy BG, Riley M, Bonnet CT. Postural stabilization of perceptual but not cognitive performance. J Mot Behav. 2007;39(2):126–138. doi: 10.3200/JMBR.39.2.126-138. [DOI] [PubMed] [Google Scholar]
- 62.Yogev-Seligmann G, Rotem-Galili Y, Mirelman A, Dickstein R, Giladi N, Hausdorff JM. How does explicit prioritization alter walking during dual-task performance? Effects of age and sex on gait speed and variability. Phys Ther. 2010;90(2):177–186. doi: 10.2522/ptj.20090043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Brown LA, Sleik RJ, Polych MA, Gage WH. Is the prioritization of postural control altered in conditions of postural threat in younger and older adults? J Gerontol A Biol Sci Med Sci. 2002;57(12):M785–M792. doi: 10.1093/gerona/57.12.M785. [DOI] [PubMed] [Google Scholar]
- 64.Chapman GJ, Hollands MA. Evidence that older adult fallers prioritise the planning of future stepping actions over the accurate execution of ongoing steps during complex locomotor tasks. Gait Posture. 2007;26(1):59–67. doi: 10.1016/j.gaitpost.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 65.Li KZ, Lindenberger U, Freund AM, Baltes PB. Walking while memorizing: age-related differences in compensatory behavior. Psychol Sci. 2001;12(3):230–237. doi: 10.1111/1467-9280.00341. [DOI] [PubMed] [Google Scholar]
- 66.Yogev-Seligmann G, Hausdorff JM, Giladi N. Do we always prioritize balance when walking? Towards an integrated model of task prioritization. Mov Disord. 2012;27(6):765–770. doi: 10.1002/mds.24963. [DOI] [PubMed] [Google Scholar]
- 67.Schaefer S, Schumacher V. The interplay between cognitive and motor functioning in healthy older adults: findings from dual-task studies and suggestions for intervention. Gerontology. 2011;57(3):239–246. doi: 10.1159/000322197. [DOI] [PubMed] [Google Scholar]
- 68.Zijlstra A, Ufkes T, Skelton DA, Lundin-Olsson L, Zijlstra W. Do dual tasks have an added value over single tasks for balance assessment in fall prevention programs? A mini-review. Gerontology. 2008;54(1):40–49. doi: 10.1159/000117808. [DOI] [PubMed] [Google Scholar]
- 69.Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C. Development and initial validation of the falls efficacy scale-international (FES-I) Age Ageing. 2005;34(6):614–619. doi: 10.1093/ageing/afi196. [DOI] [PubMed] [Google Scholar]
- 70.Powell LE, Myers AM. The activities-specific balance confidence (ABC) scale. J Gerontol Ser A Biol Med Sci. 1995;50(1):M28–M34. doi: 10.1093/gerona/50A.1.M28. [DOI] [PubMed] [Google Scholar]
- 71.Kmet LM, Cook LS, Lee RC. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Alberta: Alberta Heritage Foundation for Medical Research; 2014. https://www.ihe.ca/download/standard_quality_assessment_criteria_for_evaluating_primary_research_papers_from_a_variety_of_fields.pdf,08.07.19.
- 72.American Psychological Association . Publication manual. Washington, DC: American Psychological Association; 2016. [Google Scholar]
- 73.Beauchet O, Allali G, Sekhon H, Verghese J, Guilain S, Steinmetz JP, et al. Guidelines for assessment of gait and reference values for spatiotemporal gait parameters in older adults: the biomathics and Canadian gait consortiums initiative. Front Hum Neurosci. 2017;11:353. doi: 10.3389/fnhum.2017.00353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Auvinet B, Touzard C, Montestruc F, Delafond A, Goeb V. Gait disorders in the elderly and dual task gait analysis: a new approach for identifying motor phenotypes. J Neuroeng Rehabil. 2017;14(1):7. doi: 10.1186/s12984-017-0218-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bauer C, Gröger I, Glabasnia A, Bergler C, Gassmann KG. First results of evaluation of a falls clinic. Int J Gerontol. 2010;4(3):130–136. doi: 10.1016/S1873-9598(10)70036-3. [DOI] [Google Scholar]
- 76.Bootsma-van der Wiel A, Gussekloo J, De Craen AJ, Van Exel E, Bloem BR, Westendorp RG. Walking and talking as predictors of falls in the general population: the Leiden 85-plus study. J Am Geriatr Soc. 2003;51(10):1466–1471. doi: 10.1046/j.1532-5415.2003.51468.x. [DOI] [PubMed] [Google Scholar]
- 77.Howcroft J, Kofman J, Lemaire ED, McIlroy WE. Analysis of dual-task elderly gait in fallers and non-fallers using wearable sensors. J Biomech. 2016;49(7):992–1001. doi: 10.1016/j.jbiomech.2016.01.015. [DOI] [PubMed] [Google Scholar]
- 78.Johansson J, Nordström A, Nordström P. Greater fall risk in elderly women than in men is associated with increased gait variability during multitasking. J Am Med Dir Assoc. 2016;17(6):535–540. doi: 10.1016/j.jamda.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 79.Mirelman A, Herman T, Brozgol M, Dorfman M, Sprecher E, Schweiger A, et al. Executive function and falls in older adults: new findings from a five-year prospective study link fall risk to cognition. PLoS One. 2012;7(6):e40297. doi: 10.1371/journal.pone.0040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nordin E, Moe-Nilssen R, Ramnemark A, Lundin-Olsson L. Changes in step-width during dual-task walking predicts falls. Gait Posture. 2010;32(1):92–97. doi: 10.1016/j.gaitpost.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 81.Reelick MF, Kessels RP, Faes MC, Weerdesteyn V, Esselink RA, Rikkert MGO. Increased intra-individual variability in stride length and reaction time in recurrent older fallers. Aging Clin Exp Res. 2011;23(5–6):393–399. doi: 10.1007/BF03337764. [DOI] [PubMed] [Google Scholar]
- 82.Springer S, Giladi N, Peretz C, Yogev G, Simon ES, Hausdorff JM. Dual-tasking effects on gait variability: the role of aging, falls, and executive function. Mov Disord. 2006;21(7):950–957. doi: 10.1002/mds.20848. [DOI] [PubMed] [Google Scholar]
- 83.Toulotte C, Thevenon A, Fabre C. Effects of training and detraining on the static and dynamic balance in elderly fallers and non-fallers: a pilot study. Disabil Rehabil. 2006;28(2):125–133. doi: 10.1080/09638280500163653. [DOI] [PubMed] [Google Scholar]
- 84.Toulotte C, Thevenon A, Watelain E, Fabre C. Identification of healthy elderly fallers and non-fallers by gait analysis under dual-task conditions. Clin Rehabil. 2006;20(3):269–276. doi: 10.1191/0269215506cr929oa. [DOI] [PubMed] [Google Scholar]
- 85.Verghese Joe, Wang Cuiling, Ayers Emmeline, Izzetoglu Meltem, Holtzer Roee. Brain activation in high-functioning older adults and falls. Neurology. 2016;88(2):191–197. doi: 10.1212/WNL.0000000000003421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yamada M, Aoyama T, Nakamura M, Tanaka B, Nagai K, Tatematsu N, et al. The reliability and preliminary validity of game-based fall risk assessment in community-dwelling older adults. Geriatr Nurs. 2011;32(3):188–194. doi: 10.1016/j.gerinurse.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 87.Asai T, Misu S, Doi T, Yamada M, Ando H. Effects of dual-tasking on control of trunk movement during gait: respective effect of manual-and cognitive-task. Gait Posture. 2014;39(1):54–59. doi: 10.1016/j.gaitpost.2013.05.025. [DOI] [PubMed] [Google Scholar]
- 88.Donoghue OA, Cronin H, Savva GM, O’Regan C, Kenny RA. Effects of fear of falling and activity restriction on normal and dual task walking in community dwelling older adults. Gait Posture. 2013;38(1):120–124. doi: 10.1016/j.gaitpost.2012.10.023. [DOI] [PubMed] [Google Scholar]
- 89.Reelick MF, van Iersel MB, Kessels RP, Rikkert MGO. The influence of fear of falling on gait and balance in older people. Age Ageing. 2009;38(4):435–440. doi: 10.1093/ageing/afp066. [DOI] [PubMed] [Google Scholar]
- 90.Wollesen B, Schulz S, Seydell L, Delbaere K. Does dual task training improve walking performance of older adults with concern of falling? BMC Geriatr. 2017;17(1):213. doi: 10.1186/s12877-017-0610-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Perry J. Gait analysis: normal and pathodological function. 2. New York: SLACK Inc.; 2010. [Google Scholar]
- 92.Aksan N, Anderson SW, Dawson J, Uc E, Rizzo M. Cognitive functioning differentially predicts different dimensions of older drivers’ on-road safety. Accid Anal Prev. 2015;75:236–244. doi: 10.1016/j.aap.2014.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rochat S, Büla CJ, Martin E, Seematter-Bagnoud L, Karmaniola A, Aminian K, et al. What is the relationship between fear of falling and gait in well-functioning older persons aged 65 to 70 years? Arch Phys Med Rehabil. 2010;91(6):879–884. doi: 10.1016/j.apmr.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 94.Youdas JW, Hollman JH, Aalbers MJ, Ahrenholz HN, Aten RA, Cremers JJ. Agreement between the GAITRite walkway system and a stopwatch–footfall count method for measurement of temporal and spatial gait parameters. Arch Phys Med Rehabil. 2006;87(12):1648–1652. doi: 10.1016/j.apmr.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 95.Lindemann U, Najafi B, Zijlstra W, Hauer K, Muche R, Becker C, Aminian K. Distance to achieve steady state walking speed in frail elderly persons. Gait Posture. 2008;27(1):91–96. doi: 10.1016/j.gaitpost.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 96.Beauchet O, Allali G, Annweiler C, Berrut G, Maarouf N, Herrmann FR, Dubost V. Does change in gait while counting backward predict the occurrence of a first fall in older adults? Gerontology. 2008;54(4):217–223. doi: 10.1159/000127318. [DOI] [PubMed] [Google Scholar]
- 97.Kressig RW, Herrmann FR, Grandjean R, Michel JP, Beauchet O. Gait variability while dual-tasking: fall predictor in older inpatients? Aging Clin Exp Res. 2008;20(2):123–130. doi: 10.1007/BF03324758. [DOI] [PubMed] [Google Scholar]
- 98.Hadjistavropoulos T, Carleton RN, Delbaere K, Barden J, Zwakhalen S, Fitzgerald B, et al. The relationship of fear of falling and balance confidence with balance and dual tasking performance. Psychol Aging. 2012;27(1):1–13. doi: 10.1037/a0024054. [DOI] [PubMed] [Google Scholar]
- 99.Halvarsson A, Olsson E, Farén E, Pettersson A, Ståhle A. Effects of new, individually adjusted, progressive balance group training for elderly people with fear of falling and tend to fall: a randomized controlled trial. Clin Rehabil. 2011;25(11):1021–1031. doi: 10.1177/0269215511411937. [DOI] [PubMed] [Google Scholar]
- 100.Halvarsson A, Franzén E, Farén E, Olsson E, Oddsson L, Ståhle A. Long-term effects of new progressive group balance training for elderly people with increased risk of falling - a randomized controlled trial. Clin Rehabil. 2013;27(5):450–458. doi: 10.1177/0269215512462908. [DOI] [PubMed] [Google Scholar]
- 101.Herman T, Mirelman A, Giladi N, Schweiger A, Hausdorff JM. Executive control deficits as a prodrome to falls in healthy older adults: a prospective study linking thinking, walking, and falling. J Gerontol A Biol Sci Med Sci. 2010;65(10):1086–1092. doi: 10.1093/gerona/glq077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.MacAulay RK, Allaire TD, Brouillette RM, Foil HC, Bruce-Keller AJ, Han H, et al. Longitudinal assessment of neuropsychological and temporal/spatial gait characteristics of elderly fallers: taking it all in stride. Front Aging Neurosci. 2015;7:34. doi: 10.3389/fnagi.2015.00034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Rinaldi NM, Moraes R. Older adults with history of falls are unable to perform walking and prehension movements simultaneously. Neuroscience. 2016;316:249–260. doi: 10.1016/j.neuroscience.2015.12.037. [DOI] [PubMed] [Google Scholar]
- 104.Rogan S, Taeymans J, Bangerter C, Simon S, Terrier P, Hilfiker R. Einfluss von Einfach- und Doppelaufgaben auf Gangstabilitat und Ganggeschwindigkeit bei alteren Menschen: Eine explorative Studie, [Influence of single and dual tasks on gait stability and gait speed in the elderly : an explorative study] Z Gerontol Geriatr. 2019;52(1):23–27. doi: 10.1007/s00391-017-1279-2. [DOI] [PubMed] [Google Scholar]
- 105.Yogev G, Plotnik M, Peretz C, Giladi N, Hausdorff JM. Gait asymmetry in patients with Parkinson’s disease and elderly fallers: when does the bilateral coordination of gait require attention? Exp Brain Res. 2007;177(3):336–346. doi: 10.1007/s00221-006-0676-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The supporting data is available via the corresponding author.