Abstract
A strong and consistent association between migration and health has been found in many settings, but the overwhelming focus of this research has been on adults. In addition, identifying the effect of migration on health largely remains an unresolved challenge, due in part to the inability to distinguish between the effect of migration on health and the selection of children of differing health status into migration streams. In this research we examine the relationship between internal migration and child health in Malawi. We use longitudinal panel data with pre- and post-migration health measures for children and their mothers, which permits us to measure both migration health selection and the effect of migration on health. We also examine if child health changes over time in post-migration destinations. We do not find evidence of migration health selection: children who move have similar pre-migration health status to non-migrant children. We find that the impact of migration on child health is mediated by mothers’ characteristics. Before controlling for mothers’ health status, we find a strong negative impact of migration on health, particularly for children moving to rural areas or cities, and children moving due to changes in mothers’ marital status. After controlling for mothers’ health status, however, the negative impact of migration on child health disappears. We also find that child health is worse with longer durations spent in post-migration residence, compared to children who don’t move.
Keywords: child health, migration, selection
Introduction
A strong and consistent association between migration and health has been found in many settings (Anson, 2004; Feranil, 2006; Landale et al., 2000; Lu, 2008; Lu and Qin, 2014; Nauman et al., 2015; Rubia et al., 2002; Singh and Hiatt, 2006), including sub-Saharan Africa (SSA) (Anglewicz et al., 2018; Collinson et al., 2014; Ginsburg et al., 2016). Migration may impact health, and healthier individuals may be more likely to migrate. However, the vast majority of research has focused on adults, and very few studies have examined the relationship between migration and child health. The small body of research on migration and child outcomes has several important limitations, such as the predominant focus on two specific child outcomes (child mortality and immunization), and the use of cross-sectional data (e.g., (Antai et al., 2010; Brockerhoff, 1990, 1994; Ssengonzi et al., 2002). As a result, it’s perhaps not surprising that results have been mixed, and important gaps remain in research on the relationship between migration and child health in SSA.
The lack of knowledge on the relationship between migration and child health is of consequence for several reasons. First, child migration is a frequent occurrence in SSA: adult migration is common and children typically move with their parents in SSA (Floyd et al., 2008; Ford and Hosegood, 2005; Hosegood et al., 2004). Second, early life events, like migration, can have long-lasting consequences; research has shown that migration in young adulthood affects later life health (Gong et al., 2011; Montes de Oca et al., 2011). Third, the health of children who move has implications for health systems: tracking the health conditions of migrant groups can inform government strategies for health facility locations and amenities (Sime and Fox, 2015).
In this paper, we examine the relationship between internal migration and child health in the sub-Saharan context of Malawi. We have three main goals. First, we examine migration health selection by comparing the pre-migration health of children who move compared to those who remain in areas of origin. Second, we investigate the effect of migration on health for children who move, and if the effect differs by destination type (rural, town, urban) and the reason for migration. Third, we identify whether child health changes with longer durations spent at post-migration residences. We also examine whether characteristics of the mother and household mediate the relationship between child health and migration. Our longitudinal panel data enables a robust analysis of migration and child health that is not possible with cross sectional data.
Background
Migration and health among adults
Three mechanisms are typically employed to explain the relationship between migration and health among adults. First, differences in health for migrants may be due to health selection. Migrants may not move for health-related reasons per se, but the factors influencing migration may also impact health. Migration is a highly selective process; research has often found support for the “healthy migrant hypothesis,” the tendency for migrants to be healthier before migration than peers at both origin and destination (Landale et al., 2000; Lu, 2008; Palloni and Morenoff, 2001). This health advantage of migrants is thought to be due in part to the challenges involved in moving; frail individuals are less likely than healthy individuals to successfully relocate (Palloni and Morenoff, 2001). However, the pre-migration health advantage may depend on the reason for moving: individuals moving due to conflict or environmental shocks, or after marital dissolution may not have advantages over non-migrants (Anglewicz and Myroniuk, 2018; Avogo and Agadjanian, 2010).
Second, observed differences in health may be a direct effect of migration. Migration is often seen as disruptive: migration may interrupt or sever systems that individuals rely upon for health and well-being, such as the severing of networks of social and financial support, such as friends and family members who may provide advice or care, or resources to pay for medical care (Brockerhoff, 1990, 1994; Ssengonzi et al., 2002). This disruption occurs shortly before and/or after moving, and can potentially be long-lasting. Aside from disruption, there are also potential benefits of migration on health, such as better access to health facilities (Antai et al., 2010; Brockerhoff, 1990).
Finally, there is evidence that health changes with longer durations spent at post-migration residences. Migration may be initially disruptive, but with greater durations in post-migration destinations, migrants assimilate, resulting in changes to their attitudes and behaviors that reflect those of the residents of their destination, which can have a positive or negative impact on health. An example of adaptation that has a positive impact on health is more effective use of healthcare facilities and social support groups (Brockerhoff, 1990, 1994). However, migrant groups can also adopt negative health behaviors, such as poor diet resulting in obesity (Roshania et al., 2008). The speed and extent of adaptation varies across migrants, and may be related to socioeconomic factors (Brockerhoff, 1994). Faster adaptation may also be hindered by challenges faced in the destination, such as an arduous move, lack of support, financial/job instability, communication difficulties, and perceived or actual discrimination (Bhugra, 2004; Cantor-Graae and Selten, 2005; Carta et al., 2005; Maggi et al., 2010).
Child health and migration
While the above hypotheses are instructive, they were developed to explain adult migration and therefore require revision in order to apply to child health, which we describe here. In doing so, we highlight ways in which the relationship between migration and health could differ between adults and children.
Regarding health selection, many of the determinants of child health are also often associated with migration. For example, migration often selects women with more education, greater income, and better health (Amankwaa et al., 2003; Anglewicz, 2012; Brockerhoff, 1990; Brockerhoff and Eu, 1993; Schuyler et al., 2017), all of which are associated with better child outcomes (Brockerhoff, 1990; Ssengonzi et al., 2002). On the other hand, migration could occur to find better access to health care for a sick child, in which case children with relatively worse health would be selected to move- although the parent may or may not be in worse health themselves.
As with adults, the effect of migration on child health could be either positive or negative. Moving can disrupt systems that mothers rely on for the health and well being of her children, but connect mothers to better quality health care. However, migration may also separate children from parents. Research on the migration patterns of children in SSA shows that they typically move with one or both parents (Floyd et al., 2008; Ford and Hosegood, 2005; Hosegood et al., 2004), but parental death can also cause children to move (Ford and Hosegood, 2005; Madhavan et al., 2012). Parental separation after marital dissolution has detrimental impacts on child outcomes (Lahaie et al., 2009), which is important because migrants are more likely to experience marital dissolution in some settings (Anglewicz, 2012; Frank and Wildsmith, 2005). Migration may also negatively impact vaccination schedules for children (Antai et al., 2010).
With longer durations in destinations, migrants may become more adept at managing child illness through more effective use of healthcare facilities and support groups, and may learn to avoid negative environmental conditions or risk of accidents (Brockerhoff, 1990, 1994; Finch et al., 2007; Kana’Iaupuni et al., 2005; Xie and Greenman, 2011). However, behavior change is dependent on the mother, and can occur slowly, which may have a greater impact on the child than the mother (Brockerhoff, 1994). Furthermore, in some settings, the health of migrants’ children is better than the native population at the time of migration and shortly afterwards but then declines over time (Hamilton et al., 2011; Landale et al., 2000).
The relationship between migration and child health may also differ by characteristics of the move. For example, health outcomes may vary by destination: rural-to-urban migration may be beneficial for child health, due to more proximate and better quality health facilities in urban centers that may be beneficial for illness control (Antai et al., 2010; Brockerhoff, 1990). Moving to an urban area may also expose women to more modern child care practices that can improve child health (Brockerhoff, 1990). However, the crowding and unsanitary conditions in SSA cities facilitate the proliferation of infectious diseases (Githeko et al., 2000; Wilson, 1995). Urban areas of SSA are also characterized by higher levels of pollution (Batterman et al., 2009), and greater risk of road traffic accidents (Hyder et al., 2006).
The determinants of child health may also differ by the reason for moving. Those moving to find jobs may be relatively healthier, while individuals moving after marital dissolution may be in worse health due, for example, to the trauma of a recent divorce or death of a spouse. If women moving due to marital dissolution have worse health (Devries et al., 2011; Williams et al., 2008), this may in turn adversely impact the health of their children. Indeed, women who are divorced are more likely to experience child mortality (Clark and Hamplová, 2013). Similarly, women with children who start new marriage may have limited influence in how resources are distributed in the new household, which may not favor children from a previous marriage (Bledsoe, 1995).
Limitations of previous research
The relationship between migration and child health has seldom been empirically tested with the appropriate methodological approaches, primarily due to data limitations. Although studies on migration and child mortality frequently emphasize the importance of selection (Antai et al., 2010; Brockerhoff, 1990; Ssengonzi et al., 2002), they often do not measure health selection since longitudinal data that include health status for mothers and children both before and after migration are rare. For example, studies using data from Demographic and Health Surveys (DHS) do not contain measures of characteristics before migration, only post-migration, and some of these characteristics could change as a result of migration, even in a short period of time. Similarly, examining the effect of migration on child health requires data both before and after migration, to show how health status and other characteristics change over time, and these data are very rare, particularly in SSA.
Most of the research on migration and child health in SSA has focused on two outcomes. There is a substantial body of research on migration and child mortality (e.g., Amankwaa et al., 2003; Antai et al., 2010; Brockerhoff, 1990, 1994; Hildebrandt et al., 2005; Islam and Azad, 2008; Mberu and Mutua, 2015; Omariba and Boyle, 2010; Ssengonzi et al., 2002; Stephenson et al., 2003), as well as on migration and immunization (e.g., Antai, 2010; Kiros and White, 2004; Kusuma et al., 2010; Smith-Greenaway and Madhavan, 2015). Other child health outcomes, such as specific illnesses (fever, cough, diarrhea) or birth weight have been examined in a few studies (Avogo and Agadjanian, 2010; Hildebrandt et al., 2005), and a small number of studies have measured general child health status (examples are Donato and Duncan, 2011; Kana’Iaupuni et al., 2005, both of which involve migrants between the United States and Mexico).
Results from this research are mixed. In some settings, the health of children whose mothers move from rural to urban areas is better than those remaining in rural areas but worse than permanent urban residents (Amankwaa et al., 2003; Brockerhoff, 1990, 1994; Islam and Azad, 2008). However, some have found no disadvantage among migrants compared to other groups (Antai, 2010; Smith-Greenaway and Madhavan, 2015), and others have found no statistically significant relationship between migration and child outcomes after controlling for other characteristics that differ between migrants and non-migrants (Ssengonzi et al., 2002; Stephenson et al., 2003). These studies do not, however, use longitudinal panel designs with information both before and after moving, which may impact the results.
Overall, much remains unknown about the relationship between migration and child health in SSA. Study designs are nearly all cross-sectional, which precludes the accurate identification of selection and disruption due to the lack of pre-migration data. The child health measures of interest have typically been child mortality or immunization; other measures, like general child health have not been studied in SSA. The literature has often examined rural-to-urban migration and child health (Amankwaa et al., 2003; Antai et al., 2010; Brockerhoff, 1990, 1994; Islam and Azad, 2008), but other migration pathways, such as rural-to-rural migration - while relatively more common - have seldom been investigated. Variation in migrant outcomes by the reason for moving has also been examined rarely. Here, we use longitudinal panel data from Malawi to address some of the common limitations of previous research on migration and child health.
Setting
Malawi exemplifies the rapid transition from rural to urban residence throughout SSA. Malawi is both one of the least urbanized countries in the world, and has one of the highest rates of urban population growth (UN, 2009). But, like other countries in SSA, rural residence is predominant: the vast majority of the Malawian population resides in rural areas, and the majority of rural migrants move to other rural areas instead of urban centers (Anglewicz et al., 2017; Chalasani et al., 2013).
Among adults, internal migration in Malawi occurs primarily for work and marriage-related reasons (Anglewicz et al., 2017; Chalasani et al., 2013; Englund, 2002), with men primarily moving for work and women more likely to move for marriage (Anglewicz, 2012). Marriage-related migration typically occurs at the beginning or end of a marital union, but patterns of marital migration vary by gender and ethnicity (Mtika and Doctor, 2002; Reniers, 2003). Divorce, widowhood and remarriage are relatively common in Malawi, leading to frequent marriage-related migration patterns (Anglewicz and Reniers, 2014; Reniers, 2003).
HIV infection and migration are closely connected in Malawi. Malawi has a generalized HIV epidemic, with a prevalence estimate of 9.1% (UNAIDS, 2018), and significant differences in prevalence between rural and urban areas: the 2010 Malawi Demographic and Health Survey estimated an HIV prevalence of 17.4% in urban centers, compared with 8.9% in rural areas (National Statistics Office and ICF Macro, 2011). As elsewhere, migrants in Malawi are significantly more likely to be HIV infected than non-migrants: HIV infected individuals from rural Malawi had more than two times greater odds of migration than those who were HIV uninfected (Anglewicz et al., 2016).
Migration is common among children in Malawi (Ansell and Van Blerk, 2004). As elsewhere in SSA, children typically move with their parents, and with the mother if parents do not move together: even for the Tumbuka, who practice a Patrilocal marital tradition, children typically stay with the mother after marital dissolution (Wanda, 1988). During the course of the HIV/AIDS epidemic, children have also increasingly moved due to the sickness or death of parents (Dennis, 2008), or due to stress caused by the loss of resources in a household even with both parents intact (Ansell and Van Blerk, 2004).
Data and Methods
A full examination of migration and child health requires measures of health status prior to migration (in order to evaluate health selection) as well as post-migration data for the same individuals (in order to assess the effect of migration on health, and how the relationship changes by duration after moving). We use data from two related sources that fulfill these requirements: the Malawi Longitudinal Study of Families and Health (MLSFH), and the Migration and Health in Malawi (MHM) Project. The MLSFH was designed in 1998 as a longitudinal couples’ survey, targeting a population-based representative sample of approximately 1,500 ever-married women and 1,000 of their husbands in three rural sites of Malawi. Following a household enumeration in the three designated survey sites in 1998, a random sample of approximately 500 ever-married women aged 15–49 was selected in each site, along with all of their spouses. Follow up surveys took place in 2001, 2004, 2006, 2008 and 2010, and the sample was supplemented with young adults, parents of existing MSLFH respondents, and new spouses for those who married between waves. MLSFH initiated HIV testing for all respondents in 2004, with follow-up testing in 2006 and 2008. Descriptions of the MLSFH data, sampling, and HIV testing are presented in Kohler et al., 2014.
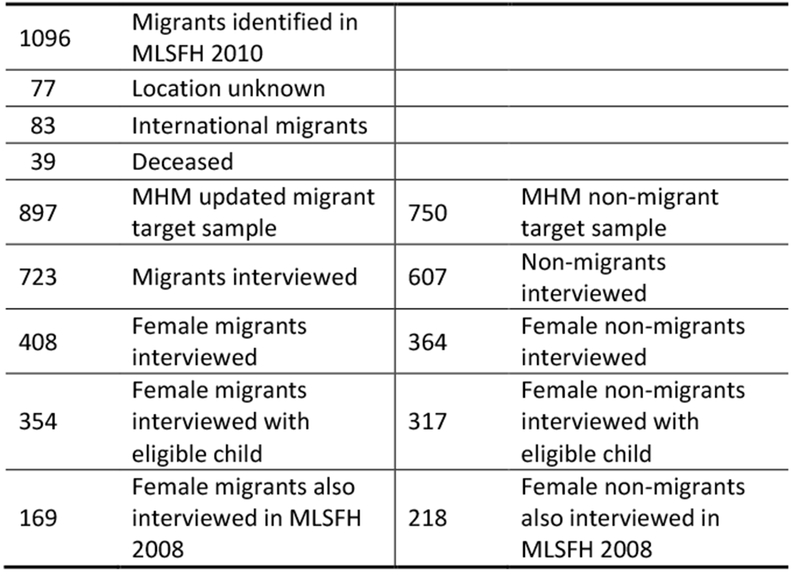
In all waves of the MLSFH, the most common reason for non-response was migration out of the study sites. The Migration and Health in Malawi (MHM) Project was designed to trace and interview MLSFH respondents who previous resided in an MLSFH sample village but moved to another part of rural or urban Malawi. Using data from the 2010 MLSFH, the MHM identified 1,096 individuals who were interviewed by MSLFH at least once since the third wave (in 2004), but were reported by friends or family members as migrants by 2010. To qualify as a “migrant”, the individual had to have moved from the MLSFH village to another location outside at least 20km of the MLSFH study site, with the expectation that the move is permanent.
In 2013, the MHM returned to the previous MLSFH village of residence for these migrants, and requested information on their current location from friends and family members. The location was unknown for only 77 of 1,096 migrants (5.1%), an additional 83 (5.5%) moved internationally, and 39 (2.6%) died. These groups were left out of the final target sample for migrants, leaving the final target sample size at 897. As a comparison group, the MHM selected a random sample of 750 “non-migrants” (435 women and 315 men) who permanently resided in the MLSFH target villages through 2010. It is important to note that the “non-migrants” in the MHM were sampled randomly and therefore should be representative of the full sample of MLSFH women. Data collection took place for both groups in 2013, and the study found and interviewed 723 migrants (80.6% success rate) and 607 non-migrants (80.9%). A full description of the MHM study can be found in (Anglewicz et al., 2017).
Inclusion criteria for analysis
We focus on women who have co-residing children aged 10 years old or less in 2008 (we select the cutoff point of 10 years in 2008 because these children are still likely to be living in the mother’s household by 2013, when the oldest have reached age 16). Men were not included in the sample for two reasons: first, since women are the primary caregivers for children in Malawi, their assessment of child health is likely more accurate than their husbands’; second, there were very few instances of households with eligible children where the father was interviewed but not the mother. Women who did not have any children aged 10 or younger in the same household were not included the analysis.
For our analysis of migration selection (i.e., information from before migration), our sample includes 962 women who completed the 2008 MLSFH survey and HIV test and have 2,131 co-resident children age 10 or younger. Of these 962 women, 102 moved by 2010 and 860 remained in their rural home (along with 206 children who moved and 1925 who remained).
Our analysis of migration effect includes women who were interviewed both in the 2008 MLSFH and the 2013 MHM (i.e., before and after migration), both those who moved and a non-migrant comparison group. As described above, the MHM study did not attempt to interview all “non-migrants” from the MLSFH, so we do not expect to have information for all 962 from the 2008 MLSFH. Among the 962 women in the selection analysis, a total of 387 (218 non-migrants and 169 migrants) were included in the 2013 MHM study, and these women in turn report on the health of 757 children. A sampling flow chart is provided in Appendix Figure 1. We compared characteristics between children with information in both 2008 and 2013 with those who have information only in 2013, and found no statistically significant differences, as shown in Appendix Table 1.
Measurement: child health
Our primary measure of interest is child’s health, which is measured in the household and family listing that is part of every round of MLSFH and MHM data collection. All MLSFH/MHM respondents are asked to list all biological children, after which participants provide information for each household or family member, including “How would you rate (NAME)’s health in general?” (response options include excellent, very good, good, fair, poor; scores range from one (poor) to five (excellent)). Research shows that mothers’ reports of child health are generally accurate, and have been shown to predict child morbidity and mortality in the future (Idler and Benyamini, 1997).
Measurement: migration
The key determinant of interest is migration, and we capture different features of migration in this research. The first step is a simple, binary measure of migration. The MHM data also permit us to identify migration origin and destination: rural–rural migrants are respondents who moved from a MLSFH village to another rural part of Malawi, at least 20km outside of an MLSFH sample area. Individuals moving to one of Malawi’s three regional capitals (Mzuzu in the North, Lilongwe in the Central, and Blantyre in the South), and the third largest city (and former capital), Zomba, were considered rural–urban migrants. Rural–town migrants are those who moved to the capital of one of Malawi’s 28 districts. Finally, we also separate migrants by their mothers’ reason for moving. As elsewhere (Anglewicz, 2012), we create a three category reason for mothers’ migration measure: work related, marriage-related (moving to start a new marriage or after marital dissolution), and all other reasons. The “other” category groups all reasons for migration that did not fit into the above categories—for example, to attend school, to visit a relative, to follow parents or relatives to a new location, and because of imprisonment.
Measurement: covariates
To select covariates in our analysis, we conducted a literature review to identify factors that are associated with both migration and child health in SSA. We included all relevant measures in our analysis, regardless of the strength of association in bivariate or multivariate analysis. We focus on three sets of characteristics, measured for children, mothers, and households. For children’s characteristics we include gender, age, level of education, and an indicator for the child sleeping in the household the previous night. Mother’s characteristics include age, marital status, region of residence, level of education, and number of living children. Mother’s health is also of interest, so we include mothers’ self-reported general health, measured the same as for children. We also include mother’s HIV status. Finally, as household characteristics we include the region of residence (southern, central, northern), whether the woman’s husband resides in the household, and overall household wealth (measured by an index created using principal components analysis of 12 household assets). We also tested other measures that theoretically might be associated with migration and child health, such as the number of people who provide assistance (financial and non-financial) to the mother and the number of lifetime marriages. These measures were not associated with our outcomes so were not included in the final analyses.
Analytic Methods
Our analysis proceeds in three parts to separately estimate: 1) migration health selection; 2) the effect of migration on health; and 3) the influence of migration duration on health.
We begin with migration health selection, in which we examine whether children with different health status are selected into migration. For this analysis, we use pre-migration from the 2008 MLSFH. We use logistic regressions where the dependent variable is the log odds that the child will migrate between the 2008 MLSFH wave (baseline) and the 2010 MLSFH wave. All independent variables are measured in 2008, to ensure that variables predicting migration, such as health status, are all measured prior to the move. The independent variables we include are measured for the child, mother, and household. Child measures include age, education, sex, and if they slept in the same household as the mother in the previous night. Characteristics of the mother are general health, number of living children, age, marital status, education, and HIV status. Household characteristics are the region of residence, household wealth, and whether the father stays in the household.
We conduct our analysis in three steps. The first step includes only migration and pre-migration child health. In the second step we add other measures for the child (child age, sex, level of education, slept in the household last night). In the third and final step, we add the mother and household characteristics to see if the estimated relationships change.
To assess the effect of migration on health, we use the longitudinal data from 2008 MLSFH and the 2013 MHM, and conduct fixed-effects regression models. In addition to health status, it is likely that individuals who migrate are different from non-migrants on many other characteristics, such as early-life impacts on health, genetic composition, risk-taking propensity, intelligence, and charisma. While some characteristics that differ between migrants and non-migrants are relatively easily observed in data (e.g. level of education), other characteristics, like those listed above, are difficult to measure or are not measured at all. This is an important challenge for migration research, because many such unobserved characteristics are likely to be associated with both migration and health status. Therefore, any empirical model that does not account for unobserved characteristics of migrants is likely to present biased estimates.
To address this issue, we use fixed effects regression that decomposes the residual into a fixed component that reflects fixed unobserved endowments (e.g., individual risk aversion, genetic and early-life components of health, preferences, etc.) and a time-varying component. The use of fixed effects is appealing because it enables us to control for any time-invariant (observed or unobserved) differences across respondents that may affect health status.
If unobserved time-invariant characteristics of individuals are correlated with migration and health (a likely scenario given that migration is likely to selective with respect to health and some of its unobserved determinants), then this will be correlated with the independent variables. Such a correlation between the error term and the independent variables in the above equation may lead to biased estimates. Fixed effects regression is an approach that eliminates possible correlation between the error term and independent variables by utilizing difference scores for all variables between waves if fixed individual characteristics are the primary source of such a correlation. Because fixed factors of individuals remain constant over time, they are eliminated when the difference scores are created. In doing so, all observed variables whose effect is constant (such as age or level of schooling), along with any unobserved time-invariant characteristics drop out of the model. Thus, if certain respondents have a greater risk tolerance that simultaneously affects migration and health, this unobserved characteristic will be differenced out of the above equation when using fixed effects (Allison 2005). The use of difference scores makes fixed effects less efficient, and impacts the independent variables used in the regression models. Any individual who does not change in the dependent variable over time is dropped from the fixed effects regression model. Also, all time-invariant measures, such as age and region of residence, are dropped. To verify this approach, we conducted Hausman tests to compare fixed effects estimates with random effects; results indicated that random effects would be inappropriate for most models and fixed effects models are less affected by biases (Allison 2005).
We conduct two types of fixed effects regressions, which differ by how migration is measured. We begin with migration measured as binary (0=non migrant and 1=migrant). Next, to examine if the relationship between migration and child health differs by destination, we separate migrants into different categories of destination types (comparing rural-to-rural migrants, rural-to-town migrants, and rural-urban migrants to non-migrants). Finally, we separate migrants by their reason for moving (work-related, marriage-related, other), again compared to non-migrants. As above, we use three steps for each set of regressions (step 1: child migration and year only, step 2: adding child characteristics, step 3: adding mother/household characteristics). As implied by the above, all measures included in the models are time-varying between 2008 and 2013, and any time-invariant measures (e.g., sex) are dropped from the fixed effects models.
We use data from the MHM 2013 to examine the relationship between child health and duration spent at post-migration residence. The survey instrument for the MHM included a full residence history, which captured the amount of time spent at each residence. Because the MHM migrants may have moved as early as 2004 (described above), the maximum duration of time spent at destination is nine years. In this analysis, we conduct OLS regressions where the dependent variable is child health, and the independent variable of primary interest is the number of years spent at the post-migration residence, measured in categories of 0-1 years, 1-2 years, 2-3 years, 3-5 years, and 5-9 years. As previously, we conduct this analysis in three steps.
Results
Sample characteristics
Table 1 shows background characteristics for the 2008 MLSFH sample (pre-migration) and the 2013 MHM study participants, separately for migrants and non-migrants. The average age of children in 2008 is 4.70 for migrants and 5.03 among non-migrants, and increases to 9.79 and 10.03 by 2013. One third of children have at least some primary education in 2008, which increases to over 90% by 2013. Nearly all children slept in the household of their mother on the previous night. The mothers average age is between 33 and 39, and they have an average of between four and six children. The majority are currently married and have at least some primary education. Among migrants, the majority moved to another rural area and migrated for marriage-related reasons.
Table 1:
Characteristics of migrants and non-migrants, children, mothers and households, MLSFH 2008 and MHM 2013
| MLSFH 2008 | MHM 2013 | |||
|---|---|---|---|---|
| Non-migrant | Future migrant | Non-migrant | Migrant | |
| Child characteristics | ||||
| Mean child’s health (1-5) | 4.12 | 4.25 | 4.72 | 4.46 |
| Mean age | 5.03 | 4.70 | 10.03 | 9.79 |
| Level of education | ||||
| None | 60.56% | 68.71% | 3.06% | 2.76% |
| Primary | 39.44% | 31.29% | 91.27% | 90.18% |
| Secondary or higher | --- | --- | 5.68% | 7.06% |
| Male | 48.91% | 52.76% | 49.13% | 51.20% |
| Slept in household last night | 93.01% | 93.25% | 91.30% | 84.80% |
| Child N= | 1925 | 206 | 517 | 373 |
| Mother characteristics | ||||
| Mean mother’s health (1-5) | 3.04 | 3.11 | 3.60 | 3.33 |
| Mean number of children | 4.53 | 4.02 | 5.61 | 4.85 |
| Mean mother’s age | 35.28 | 33.66 | 38.47 | 36.52 |
| Mother’s marital status | ||||
| Currently married | 93.09% | 86.76% | 90.72% | 82.70% |
| Divorced/separated | 4.88% | 6.37% | 7.35% | 14.05% |
| Widowed | 2.02% | 6.86% | 1.93% | 3.24% |
| Mother’s education | ||||
| None | 24.90% | 12.14% | 29.27% | 11.38% |
| Primary | 67.96% | 76.21% | 65.45% | 80.76% |
| Secondary or higher | 7.14% | 11.65% | 5.28% | 7.86% |
| HIV infected | 5.69% | 16.99% | 5.35% | 18.28% |
| Household characteristics | ||||
| Region of residence | ||||
| Central | 32.30% | 48.54% | 30.56% | 43.70% |
| South | 32.76% | 21.36% | 40.43% | 26.01% |
| North | 34.94% | 30.10% | 29.01% | 30.29% |
| Mean household wealth | 0.14 | 0.07 | 0.01 | −0.09 |
| Husband resides in household | 89.03% | 78.16% | 87.04% | 72.39% |
| Household/female N= | 860 | 102 | 262 | 128 |
| Migration characteristics | ||||
| Mean years duration at residence1 | 13.71 | 7.92 | ||
| Migration stream | ||||
| Rural-rural migrant | 72.92% | |||
| Rural-town migrant | 19.84% | |||
| Rural-urban migrant | 7.24% | |||
| Reason for migration | ||||
| Work-related | 30.57% | |||
| Marriage-related | 51.72% | |||
| Other | 17.71% | |||
| Duration of migration | ||||
| 0-1 years | 18.47% | |||
| 1-2 years | 5.97% | |||
| 2-3 years | 14.49% | |||
| 3-5 years | 11.93% | |||
| 5-9 years | 49.15% | |||
Notes:
= mean years of duration at residence is measured only for those who migrated once or more (647 children, 224 women).
Migration health selection
Table 2 shows results for logistic regressions of pre-migration (2008) characteristics on future (2008-2010) migration. In short, we do not find evidence of migration child health selection: there is no significant association between child health in 2008 and migration between 2008 and 2010. In model 1, we do not find that 2008 health status for children is associated with migration between 2008 and 2010. In model 2, none of the additional 2008 characteristics of children are associated with moving in the future. Factors associated with migration between 2008 and 2010 are primarily associated with the mother and household (model 3). Specifically, women who are HIV infected in 2008 are more likely to migrate between 2008 and 2010 than those who are uninfected. Women with primary and secondary or higher education in 2008 are also more likely to move than women with no education, and those from the southern and northern region are less likely to move than women from the central region. Women who co-reside with their spouse are less likely to move in the future.
Table 2:
Migration selection: Logistic regression results for the association between migration in the future and pre-migration characteristics, 2008-2010 MLSFH
| Model 1- Child health | Model 2- Child characteristics | Model 3- Children, mothers, households | ||||
|---|---|---|---|---|---|---|
| Odds Ratios | 95% CI | Odds Ratios | 95% CI | Odds Ratios | 95% CI | |
| Child characteristics | ||||||
| Child health | 1.22 | 0.925-1.598 | 1.22 | 0.928-1.604 | 1.19 | 0.913-1.561 |
| Age | 0.97 | 0.903-1.040 | 1.01 | 0.932-1.085 | ||
| Level of education | ||||||
| None (reference) | ---- | ---- | ---- | ---- | ||
| Primary | 0.99 | 0.608-1.622 | 0.93 | 0.561-1.527 | ||
| Male | 0.91 | 0.674-1.229 | 0.94 | 0.686-1.284 | ||
| Slept in household last night | 1.24 | 0.589-2.609 | 1.38 | 0.647-2.959 | ||
| Mother characteristics | ||||||
| Mother’s health | 1.07 | 0.788-1.461 | ||||
| Number of children | 0.96 | 0.816-1.128 | ||||
| Mother’s age | 0.99 | 0.957-1.028 | ||||
| Mother’s marital status | ||||||
| Currently married (reference) | ---- | ---- | ||||
| Divorced/separated | 0.57 | 0.175-1.863 | ||||
| Widowed | 1.34 | 0.393-4.590 | ||||
| Mother’s education | ||||||
| None (reference) | ---- | ---- | ||||
| Primary | 2.10 | 0.992-4.433 | ||||
| Secondary or higher | 3.53 | 1.053-11.800 | ||||
| HIV infected | 3.41 | 1.747-6.656 | ||||
| Household characteristics | ||||||
| Region of residence | ||||||
| Central (reference) | ---- | ---- | ||||
| South | 0.45 | 0.235-0.845 | ||||
| North | 0.47 | 0.262-0.835 | ||||
| Household wealth | 0.95 | 0.835-1.087 | ||||
| Husband resides in household | 0.42 | 0.180-0.964 | ||||
| N= | 2131 children, 962 mothers/households | |||||
Notes: standard errors are clustered by mother/household; instances where 95% CIs do not overlap with 1 are in bold font. Other measures such as the number of people who provide assistance (financial and non-financial) to the mother, and number of lifetime marriages were not associated with the outcome and were dropped from the final analyses.
The effect of migration on health
We find a strong negative effect of migration on child health. Our fixed effects results (Table 3) show that among children, moving causes a decline in health of 0.32 points on the five point scale (95% confidence interval −0.607- −0.043). These results are maintained even after adding other child characteristics, none of which are statistically associated with health status. After controlling for mother and household characteristics, however, the impact of migration on child health is not statistically significant. We find that other characteristics of the mother and household are significantly associated with changes in health status, particularly mother’s health: after controlling for migration, a one point increase in mothers’ health status is associated with a 0.44 point increase in child health (95% confidence interval 0.303-0.566).
Table 3:
Migration effect: Fixed effects regression results for the impact of migration on child health, 2008-2013 MHM/ MLSFH
| Model 1- Child health | Model 2- Child characteristics | Model 3- Children, mothers, households | ||||
|---|---|---|---|---|---|---|
| Coef. | 95% CI | Coef. | 95% CI | Coef. | 95% CI | |
| Children’s characteristics | ||||||
| Migrated | −0.32 | −0.607- −0.043 | −0.32 | −0.599- −0.037 | −0.12 | −0.376-0.138 |
| Level of education | ||||||
| None (reference) | ---- | ---- | ---- | ---- | ||
| Primary | 0.08 | −0.230-0.395 | 0.03 | −0.278-0.340 | ||
| Secondary | −0.12 | −0.655-0.422 | 0.10 | −0.391-0.599 | ||
| Slept in household last night | −0.06 | −0.321-0.210 | 0.00 | −0.273-0.274 | ||
| Mother characteristics | ||||||
| Mother’s health | 0.44 | 0.303-0.566 | ||||
| Number of children | −0.06 | −0.208-0.097 | ||||
| Mother’s marital status | ||||||
| Currently married (reference) | ---- | ---- | ||||
| Divorced/separated | −0.11 | −0.702-0.490 | ||||
| Widowed | 0.05 | −0.641-0.746 | ||||
| Mother’s education | ||||||
| None (reference) | ---- | ---- | ||||
| Primary | −0.14 | −0.479-0.202 | ||||
| Secondary or higher | −0.57 | −1.253-0.106 | ||||
| HIV infected | −0.36 | −1.168-0.456 | ||||
| Household characteristics | ||||||
| Household wealth | −0.06 | −0.151-0.027 | ||||
| Father co-resides in household | 0.13 | −0.370-0.640 | ||||
| Survey wave/year | 0.66 | 0.485-0.837 | 0.64 | 0.444-0.829 | 0.37 | 0.144-0.598 |
| N= | 757 children, 387 mothers/households | |||||
Notes: standard errors are clustered by mother/household; instances where 95% CIs do not overlap with 1 are in bold font. Other measures such as the number of people who provide assistance (financial and non-financial) to the mother, and number of lifetime marriages were not associated with the outcome and were dropped from the final analyses. Sex is dropped from fixed effects regression because it is time-invariant; age (for mother and child) is also dropped because there is no variation across respondents in fixed effects regression.
We also find that the relationship between migration and child health varies by migration location. In models 1 and 2, we find that women who move to other rural areas and urban areas experience significant declines in the health of their children, compared to non-migrants (Table 4). After controlling for the characteristics of the mother, however, there is no impact of migration to any destination on child health.
Table 4:
Migration effect: Fixed effects regression results for the impact of migration on child health, by migration destination 2008-2013 MHM/MLSFH
| Model 1- Child health | Model 2- Child characteristics | Model 3- Children, mothers, households | ||||
|---|---|---|---|---|---|---|
| Coef. | 95% CI | Coef. | 95% CI | Coef. | 95% CI | |
| Children’s characteristics | ||||||
| Migration destination | ||||||
| Non-migrant (reference) | ---- | ---- | ---- | ---- | ---- | ---- |
| Rural-rural migrant | −0.34 | −0.655- −0.019 | −0.34 | −0.655- −0.020 | −0.14 | −0.426-0.152 |
| Rural-town migrant | −0.13 | −0.661-0.379 | −0.13 | −0.648-0.396 | 0.00 | −0.423-0.429 |
| Rural-urban migrant | −0.72 | −1.038- −0.534 | −0.72 | −0.957- −0.485 | −0.36 | −0.973-0.259 |
| Level of education | ||||||
| None (reference) | ---- | ---- | ---- | ---- | ||
| Primary | 0.08 | −0.226-0.394 | 0.03 | −0.276-0.340 | ||
| Secondary | −0.10 | −0.643-0.451 | 0.12 | −0.380-0.616 | ||
| Slept in household last night | −0.04 | −0.307-0.219 | 0.00 | −0.270-0.276 | ||
| Mother characteristics | ||||||
| Mother’s health | 0.43 | 0.300-0.565 | ||||
| Number of children | −0.05 | −0.208-0.098 | ||||
| Mother’s marital status | ||||||
| Currently married (reference) | ---- | ---- | ||||
| Divorced/separated | −0.12 | −0.727-0.491 | ||||
| Widowed | 0.01 | −0.686-0.715 | ||||
| Mother’s education | ||||||
| None (reference) | ---- | ---- | ||||
| Primary | −0.14 | −0.475-0.203 | ||||
| Secondary or higher | −0.52 | −1.187-0.156 | ||||
| Mother HIV infected | −0.34 | −1.153-0.474 | ||||
| Household characteristics | ||||||
| Household wealth | −0.06 | −0.147-0.028 | ||||
| Father co-resides in household | 0.11 | −0.418-0.631 | ||||
| Survey wave/year | 0.66 | 0.485-0.837 | 0.64 | 0.444-0.829 | 0.37 | 0.145-0.600 |
| N= | 757 children, 387 mothers/households | |||||
Notes: standard errors are clustered by mother/household; instances where 95% CIs do not overlap with 1 are in bold font. Other measures such as the number of people who provide assistance (financial and non-financial) to the mother, and number of lifetime marriages were not associated with the outcome and were dropped from the final analyses. Sex is dropped from fixed effects regression because it is time-invariant; age (for mother and child) is also dropped because there is no variation across respondents in fixed effects regression.
The effect of migration on child health also differs by the reason for moving. As shown in Table 5, there was no association between a mother moving for work and child health. However, we find that children who move because their mother experienced marital dissolution or started a new marriage experienced a significant decline in their health status, compared to children who don’t move.
Table 5:
Migration effect: Fixed effects regression results for the impact of migration on child health, by reason for migration 2008-2013 MHM/MLSFH
| Model 1- Child health | Model 2- Children characteristics | Model 3- Children, mothers, households | ||||
|---|---|---|---|---|---|---|
| Coef. | 95% CI | Coef. | 95% CI | Coef. | 95% CI | |
| Children’s characteristics | ||||||
| Reason for migration | ||||||
| Non-migrant (reference) | ---- | ---- | ---- | ---- | ---- | ---- |
| Work-related | −0.27 | −0.286-0.630 | −0.27 | −0.287-0.669 | 0.04 | −0.221-0.526 |
| Marriage-related | −0.41 | −0.766- −0.056 | −0.39 | −0.745- −0.039 | −0.19 | −0.532-0.154 |
| Other reason | 0.17 | −0.717-0.181 | 0.19 | −0.705-0.169 | 0.15 | −0.405-0.483 |
| Level of education | ||||||
| None (reference) | ---- | ---- | ---- | ---- | ||
| Primary | 0.15 | −0.155-0.456 | 0.13 | −0.168-0.421 | ||
| Secondary | −0.06 | −0.595-0.469 | 0.22 | −0.268-0.713 | ||
| Slept in household last night | −0.09 | −0.357-0.184 | −0.06 | −0.339-0.219 | ||
| Mother characteristics | ||||||
| Mother’s health | 0.44 | 0.302-0.567 | ||||
| Number of children | −0.10 | −0.231-0.040 | ||||
| Mother’s marital status | ||||||
| Currently married (reference) | ---- | ---- | ||||
| Divorced/separated | −0.05 | −0.678-0.582 | ||||
| Widowed | −0.16 | −0.738-0.409 | ||||
| Mother’s education | ||||||
| None (reference) | ---- | ---- | ||||
| Primary | 0.03 | −0.272-0.332 | ||||
| Secondary or higher | −0.33 | −0.971-0.316 | ||||
| Mother HIV infected | −0.26 | −0.811-0.299 | ||||
| Household characteristics | ||||||
| Household wealth | −0.04 | −0.135-0.048 | ||||
| Father co-resides in household | 0.14 | −0.403-0.684 | ||||
| Survey wave/year | 0.66 | 0.485-0.837 | 0.62 | 0.428-0.811 | 0.39 | 0.157-0.613 |
| N = | 757 children, 387 mothers/households | |||||
Notes: standard errors are clustered by mother/household; instances where 95% CIs do not overlap with 1 are in bold font. Other measures such as the number of people who provide assistance (financial and non-financial) to the mother, and number of lifetime marriages were not associated with the outcome and were dropped from the final analyses. Sex is dropped from fixed effects regression because it is time-invariant; age (for mother and child) is also dropped because there is no variation across respondents in fixed effects regression.
Migration duration
Finally, we find evidence that child health varies by duration spent at post-migration destinations. As shown in Table 6, we find that, in 2013, migrants who have resided at new locations for less than a year have significantly worse child health than non-migrants. Child health does not, however, improve with greater duration: migrant children residing at new locations for 3 to 5 years or 5 to 9 years have significantly worse health than non-migrant children. Although children of migrants residing in location for 0-1 and 3-5 years do not have significantly different health status after controlling for mothers’ characteristics, the relationship between duration of 5 to 9 years and health is consistent in all three models.
Table 6:
Duration at residence: OLS regression results for the association between number of years spent at post-migration residence and child health, 2013 MHM
| Model 1- Child health | Model 2- Children characteristics | Model 3- Children, mothers, households | ||||
|---|---|---|---|---|---|---|
| Coef. | 95% CI | Coef. | 95% CI | Coef. | 95% CI | |
| Children’s characteristics | ||||||
| Years at post-migration residence | ||||||
| Non-migrant (reference) | ---- | ---- | ---- | ---- | ---- | ---- |
| 0-1 years | −0.27 | −0.542- −0.008 | −0.28 | −0.539-−0.017 | −0.16 | −0.376-0.047 |
| 1-2 years | −0.19 | −0.553-0.180 | −0.16 | −0.523-0.199 | −0.13 | −0.525-0.266 |
| 2-3 years | −0.09 | −0.331-0.149 | −0.09 | −0.327-0.149 | −0.16 | −0.348-0.019 |
| 3-5 years | −0.32 | −0.587- −0.056 | −0.33 | −0.590-−0.067 | −0.09 | −0.399-0.212 |
| 5-9 years | −0.28 | −0.448- −0.104 | −0.28 | −0.451-−0.104 | −0.15 | −0.285-−0.014 |
| Age | 0.00 | −0.015-0.009 | −0.01 | −0.017-0.004 | ||
| Level of education | ||||||
| None (reference) | ---- | ---- | ---- | ---- | ||
| Primary | 0.14 | −0.004-0.280 | 0.14 | 0.011-0.266 | ||
| Secondary | 0.22 | −0.052-0.492 | 0.28 | 0.033-0.526 | ||
| Male | 0.06 | −0.026-0.139 | 0.06 | −0.007-0.131 | ||
| Slept in household last night | 0.00 | −0.129-0.127 | −0.01 | −0.120-0.096 | ||
| Mother characteristics | ||||||
| Mother’s health | 0.43 | 0.334-0.517 | ||||
| Number of children | 0.00 | −0.026-0.031 | ||||
| Mother’s age | 0.00 | −0.004-0.010 | ||||
| Mother’s marital status | ||||||
| Currently married (reference) | ---- | ---- | ||||
| Divorced/separated | 0.09 | −0.157-0.337 | ||||
| Widowed | 0.18 | −0.123-0.477 | ||||
| Mother’s education | ||||||
| None (reference) | ---- | ---- | ||||
| Primary | 0.08 | −0.045-0.205 | ||||
| Secondary or higher | 0.31 | 0.062-0.565 | ||||
| HIV infected | −0.03 | −0.180-0.127 | ||||
| Household characteristics | ||||||
| Region of residence | ||||||
| Central (reference) | ---- | ---- | ||||
| South | 0.08 | −0.037-0.195 | ||||
| North | 0.11 | −0.029-0.258 | ||||
| Household wealth | −0.02 | −0.060-0.015 | ||||
| Husband resides in household | 0.08 | −0.112-0.264 | ||||
| N= | 786 children, 273 mothers/households | |||||
Notes: standard errors are clustered by mother/household; instances where 95% CIs do not overlap with 1 are in bold font. Other measures such as the number of people who provide assistance (financial and non-financial) to the mother, and number of lifetime marriages were not associated with the outcome and were dropped from the final analyses. Additional analysis with migrants of duration 0-1 years as the reference group did not change the substantive conclusions.
Discussion
We find that children who move experience a significant decline in their overall health status. When we control for mothers’ health, however, there is no statistically significant impact of migration on child health. Thus, the impact of migration on child health appears to be mediated by characteristics of the mother. This result is consistent with previous research showing that adaptation to the new environment among children largely depends on the mother (Brockerhoff, 1994).
Differences in health status after migration are not due to the selection of healthier/less healthy children into migration. We do not find any pre-migration differences in health between children who move and those who remain in rural areas. Thus, child health status in itself does not appear to be a prominent motivation for moving in rural Malawi. Moreover, mothers’ characteristics are stronger predictors of migration than child characteristics, which likely reflects that fact that decisions to migrate are made by the mother, not by the child. In contrast to the “healthy migrant” hypothesis, which focuses on positive attributes of migrants, we find that pre-migration factors associated with moving are mixed: female migrant mothers are younger and better-educated than non-migrants, but they are also more likely to be infected with HIV, and less likely to be married.
Contrary to the “adaptation” hypothesis, this disadvantage for migrants appears to persist over time after moving. Children who have been in post-migration locations for five to nine years have significantly worse health than non-migrants, even after controlling for characteristics of the child, mother, and household. Our results are therefore consistent with research showing that migrants are continuously at a disadvantage, regardless of time spent at post-move destinations (Brockerhoff, 1990, 1994; Mberu and Mutua, 2015).
Why does migration cause a decline in child health, before controlling for mothers’ health? Some insight can be found in the analysis of migrant sub-groups. The decline in health occurs for children who move to rural areas and cities, compared to children who do not move. The negative influence of moving to a city has been found elsewhere (Antai et al., 2010; Brockerhoff, 1994; Islam and Azad, 2008), and is likely due to increased exposure to infectious diseases, social alienation, crime, and pollution in urban areas (McMichael, 2000; Szreter, 1997).
The decline for children who move to another rural area is likely due to marriage-related migration; previous research has shown that rural-to-rural migration among women in Malawi is primarily for marriage-related reasons (Anglewicz et al., 2017; Chalasani et al., 2013). Women moving with their children to start a new marriage or after marital dissolution may experience declines in child health because marital dissolution has a negative impact on the health of women (Devries et al., 2011; Williams et al., 2008), which may then impact the health of their children. Indeed, women who are divorced are more likely to experience child mortality (Clark and Hamplová, 2013). Similarly, women with children who start new marriage may be limited in how resources are distributed in the new household, which may not favor children from a previous marriage (Bledsoe, 1995), which may also explain why child health declines over time.
Our research contributes to methodological approaches in studying the relationship between migration and health. First, we demonstrate the value of acknowledging diversity among migrant groups, which we measure by differences in (1) destinations, and (2) reasons for moving. Declines in health resulting from migration are not for all migrants, but primarily those moving for marriage-related reasons, and to urban and other rural areas (not towns). The use of longitudinal panel data is also notable, since it enables us to (1) differentiate between health selection and the effect of migration on health, and (2) use fixed effects regression to control for unobserved time-invariant characteristics that affect both migration and health. Furthermore, unlike previous research on child outcomes, which primarily focus on child mortality or immunization, we examine the impact on overall health status. We also benefit from having data for both mothers and children, which permits us to examine if the relationship between migration and health is mediated by characteristics of the mother.
While our data and approach addressed several potential biases that often affect research on migration and health, there are some important limitations in this research. Although fixed effects eliminates the effect of unobserved stable characteristics, there are likely to be unobserved time-varying characteristics that we did not control for and may be associated with the dependent variable. For example there may be changes in some of the proximate determinants or socioeconomic factors over time but are not captured in the MLSFH or MHM surveys (examples are nutritional information and access to a health facility). There are also some limitations in our sampling approach. We do not have information for children who did not move with their mother, and, given the strong connection between mothers’ and child health, it seems likely that health outcomes could differ for these children. It is also possible that the migrants not found by the MHM study were systematically different from those interviewed by MHM. However, the MHM cohort profile tested for pre-migration differences between migrants interviewed and not interviewed, and the only notable difference was that the study was more likely to find women (Anglewicz et al. 2017), which does not impact the results of this study, since only women were used. But it is possible that those not found differ in post-migration outcomes, or pre-migration outcomes not measured by the MHM. This research would also benefit from additional measures of child health, such as height and weight, illness, or visits to the hospital or health center; and measures of the environment, such as the quality of health facilities. In addition to other measures, it’s possible that child health may vary within the year. For example, the MHM and MLSFH studies may have been conducted at a time when malaria rates were relatively low, and the relationship between migration and child health may be different during peak malaria season. We also note that the results apply only to internal migration, and may not be broadly applicable due to differences in patterns of internal migration across countries in SSA. However, other studies have found similar patterns of internal migration, such as the connection between migration and marriage (e.g.,Arnaldo, 2004; Boerma et al., 2002). Finally, although we know if the husband resides in the household, we do not know if the husband is the biological father of the child. Since women who move are more likely to have experienced marital dissolution, whether the husband is the biological father may differ by migration status.
Our results have important implications for health policies in developing settings. While migrants are often seen as a group with advantages in health, education, and wealth (Anglewicz et al., 2018; Landale et al., 2000; Lu, 2008; Palloni and Morenoff, 2001), our research shows that some migrants do not have a pre-migration health advantage, and some experience declines in health as a result of migration. Urban population growth has important implications for health, planning, and development, and reductions in health as a result of migration may place additional burden on urban health systems in SSA. Finally, our research suggests that the best way to avoid declines in child health is to ensure that mothers’ health is robust, reinforcing the central role of the mother in the health of her children.
Highlights: Internal Migration and Child Health in Malawi.
-
-
The relationship between migration and child health has seldom been examined
-
-
We find a strong negative impact of migration on the health of children
-
-
The impact of migration on child health is mediated by mothers’ characteristics.
-
-
Children who move have similar pre-migration health status to non-migrant children
Appendix Table A1:
Tests of difference in characteristics between children merged between waves and those only in 2008, MHM and MLSCH
| 2008 only | Both 2008 & 2013 | |
|---|---|---|
| Child’s health | 4.10 | 4.14 |
| Age | 4.94 | 5.12 |
| Level of education | ||
| None | 22.6% | 21.5% |
| Primary | 71.1% | 73.1% |
| Secondary | 6.3% | 5.4% |
| Male | 49.8% | 51.7% |
| Slept in household last night | 88.6% | 89.7% |
Appendix Figure 1:
Sampling Flow Chart for MHM Study, 2013
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Philip Anglewicz, Johns Hopkins Bloomberg School of Public Health, Department of Population, Family, and Reproductive Health, 615 N. Wolfe Street, Baltimore MD 21205.
Rachel Kidman, Assistant Professor of Family, Population and Preventive Medicine, Department of Family, Population and Preventive Medicine, Division of Evaluative Sciences, Division of Community Health, Program in Public Health, OFFICE: HSC 3-071.
Sangeetha Madhavan, Associate Professor, Associate Director, Maryland Population Research Center, Departments of African American Studies & Sociology, University of Maryland, 1119 Taliaferro Hall College Park, MD 20742.
References
- Allison P Fixed Effects Regression Methods for Longitudinal Data Using SAS® Reviews. [Google Scholar]
- Amankwaa AA, Bavon A, and Nkansah PT (2003). Rural-urban migration and its effects on infant and child mortality in Ghana. Afr. Popul. Stud. 18, 1–26. [Google Scholar]
- Anglewicz P (2012). Migration, marital change, and HIV infection in Malawi. Demography 49, 239–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anglewicz P, and Myroniuk TW (2018). Shocks and migration in Malawi. Demogr. Res. 38, 321–334. [Google Scholar]
- Anglewicz P, and Reniers G (2014). HIV status, gender, and marriage dynamics among adults in Rural Malawi. Stud. Fam. Plann. 45, 415–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anglewicz P, VanLandingham M, Manda-Taylor L, and Kohler H-P (2016). Migration and HIV infection in Malawi. AIDS 30, 2099–2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anglewicz P, VanLandingham M, Manda-Taylor L, and Kohler H-P (2017). Cohort profile: internal migration in sub-Saharan Africa—The Migration and Health in Malawi (MHM) study. BMJ Open 7, e014799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anglewicz P, VanLandingham M, Manda-Taylor L, and Kohler H-P (2018). Health Selection, Migration, and HIV Infection in Malawi. Demography 55, 979–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ansell N, and Van Blerk L (2004). Children’s migration as a household/family strategy: coping with AIDS in Lesotho and Malawi. J. South. Afr. Stud. 30, 673–690. [Google Scholar]
- Anson J (2004). The migrant mortality advantage: a 70 month follow-up of the Brussels population. Eur. J. Popul. Eur. Démographie 20, 191–218. [Google Scholar]
- Antai D (2010). Migration and child immunization in Nigeria: individual-and community-level contexts. BMC Public Health 10, 116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antai D, Wedrén S, Bellocco R, and Moradi T (2010). Migration and child health inequities in Nigeria: a multilevel analysis of contextual-and individual-level factors. Trop. Med. Int. Health 15, 1464–1474. [DOI] [PubMed] [Google Scholar]
- Arnaldo C (2004). Ethnicity and marriage patterns in Mozambique. African Population Studies/Etude de la Population Africaine, 19, 143–164. [Google Scholar]
- Avogo WA, and Agadjanian V (2010). Forced migration and child health and mortality in Angola. Soc. Sci. Med. 1982 70, 53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batterman S, Chernyak S, Gouden Y, Hayes J, Robins T, and Chetty S (2009). PCBs in air, soil and milk in industrialized and urban areas of KwaZulu-Natal, South Africa . Environ. Pollut. Barking Essex 1987 157, 654–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhugra D (2004). Migration and mental health. Acta Psychiatr. Scand. 109, 243–258. [DOI] [PubMed] [Google Scholar]
- Bledsoe C (1995). Marginal members: Children of previous unions in Mende households in Sierra Leone. Situating Fertil. Anthropol. Demogr. Inq. Camb. Univ. Press Camb 130–153. [Google Scholar]
- Boerma JT, Urassa M, Nnko S, Ng’weshemi J, Isingo R, Zaba B, and Mwaluko G (2002). Sociodemographic context of the AIDS epidemic in a rural area in Tanzania with a focus on people9s mobility and marriage. Sex. Transm. Infect. 78, i97–i105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brockerhoff M (1990). Rural-to-urban migration and child survival in Senegal . Demography 27, 601–616. [PubMed] [Google Scholar]
- Brockerhoff M (1994). The impact of rural-urban migration on child survival. Health Transit. Rev 127–149. [PubMed] [Google Scholar]
- Brockerhoff M, and Eu H (1993). Demographic and socioeconomic determinants of female rural to urban migration in Sub-Saharan Africa. Int. Migr. Rev. 27, 557–577. [PubMed] [Google Scholar]
- Cantor-Graae E, and Selten J-P (2005). Schizophrenia and migration: a meta-analysis and review. Am. J. Psychiatry 162, 12–24. [DOI] [PubMed] [Google Scholar]
- Carta MG, Bernal M, Hardoy MC, and Haro-Abad JM (2005). Migration and mental health in Europe (the state of the mental health in Europe working group: appendix 1). Clin. Pract. Epidemiol. Ment. Health 1, 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalasani S, Mensch BS, and Hewett PC (2013). Migration among adolescents from rural Malawi. In Annual Meeting of the Population Association of America, p. [Google Scholar]
- Clark S, and Hamplová D (2013). Single Motherhood and Child Mortality in Sub-Saharan Africa: A Life Course Perspective. Demography 50, 1521–1549. [DOI] [PubMed] [Google Scholar]
- Collinson MA, White MJ, Bocquier P, McGarvey ST, Afolabi SA, Clark SJ, Kahn K, and Tollman SM (2014). Migration and the epidemiological transition: insights from the Agincourt sub-district of northeast South Africa. Glob. Health Action 7, 23514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M (2008). Children on the brink 2002: A joint report on orphan estimates and program strategies (DIANE Publishing; ). [Google Scholar]
- Devries K, Watts C, Yoshihama M, Kiss L, Schraiber LB, Deyessa N, Heise L, Durand J, Mbwambo J, Jansen H, et al. (2011). Violence against women is strongly associated with suicide attempts: Evidence from the WHO multi-country study on women’s health and domestic violence against women. Soc. Sci. Med. 73, 79–86. [DOI] [PubMed] [Google Scholar]
- Donato KM, and Duncan EM (2011). Migration, Social Networks, and Child Health in Mexican Families. J. Marriage Fam. 73, 713–728. [Google Scholar]
- Englund H (2002). The village in the city, the city in the village: migrants in Lilongwe. J. South. Afr. Stud. 28, 137–154. [Google Scholar]
- Feranil AB (2006). Anaemia among migrant and non-migrant mothers in disadvantaged areas in the Visayas, the Philippines. In Migration and Health in Asia, (Routledge), pp. 118–133. [Google Scholar]
- Finch BK, Lim N, Perez W, and Do DP (2007). Toward a Population Health Model of Segmented Assimilation: The Case of Low Birth Weight in Los Angeles. Sociol. Perspect. 50, 445–468. [Google Scholar]
- Floyd S, Crampin AC, Glynn JR, Mwenebabu M, Mnkhondia S, Ngwira B, Zaba B, and Fine PE (2008). The long-term social and economic impact of HIV on the spouses of infected individuals in northern Malawi. Trop. Med. Int. Health 13, 520–531. [DOI] [PubMed] [Google Scholar]
- Ford K, and Hosegood V (2005). AIDS mortality and the mobility of children in KwaZulu Natal, South Africa. Demography 42, 757–768. [DOI] [PubMed] [Google Scholar]
- Frank R, and Wildsmith E (2005). The Grass Widows of Mexico: Migration and Union Dissolution in a Binational Context. Soc. Forces 83, 919–947. [Google Scholar]
- Ginsburg C, Bocquier P, Béguy D, Afolabi S, Augusto O, Derra K, Herbst K, Lankoande B, Odhiambo F, and Otiende M (2016). Healthy or unhealthy migrants? Identifying internal migration effects on mortality in Africa using health and demographic surveillance systems of the INDEPTH network. Soc. Sci. Med. 164, 59–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Githeko AK, Lindsay SW, Confalonieri UE, and Patz JA (2000). Climate change and vector-borne diseases: a regional analysis. Bull. World Health Organ. 78, 1136–1147. [PMC free article] [PubMed] [Google Scholar]
- Gong F, Xu J, Fujishiro K, and Takeuchi DT (2011). A life course perspective on migration and mental health among Asian immigrants: The role of human agency. Soc. Sci. Med. 73, 1618–1626. [DOI] [PubMed] [Google Scholar]
- Hamilton ER, Cardoso JB, Hummer RA, and Padilla YC (2011). Assimilation and emerging health disparities among new generations of U.S. children. Demogr. Res. 25, 783–818. [Google Scholar]
- Hildebrandt N, McKenzie DJ, Esquivel G, and Schargrodsky E (2005). The Effects of Migration on Child Health in Mexico [with Comments]. Economia 6, 257–289. [Google Scholar]
- Hosegood V, McGrath N, Herbst K, and Tim\a eus IM. (2004). The impact of adult mortality on household dissolution and migration in rural South Africa. Aids 18, 1585–1590. [DOI] [PubMed] [Google Scholar]
- Hyder AA, Labinjo M, and Muzaffar SSF (2006). A New Challenge to Child and Adolescent Survival in Urban Africa: An Increasing Burden of Road Traffic Injuries. Traffic Inj. Prev. 7, 381–388. [DOI] [PubMed] [Google Scholar]
- Idler EL, and Benyamini Y (1997). Self-Rated Health and Mortality: A Review of Twenty-Seven Community Studies. J. Health Soc. Behav. 38, 21–37. [PubMed] [Google Scholar]
- Islam MM, and Azad KMAK (2008). Rural–urban migration and child survival in urban Bangladesh: Are the urban migrants and poor disadvantaged? J. Biosoc. Sci. 40, 83–96. [DOI] [PubMed] [Google Scholar]
- Kana’Iaupuni SM, Donato KM, Thompson-Colon T, and Stainback M (2005). Counting on kin: Social networks, social support, and child health status. Soc. Forces 83, 1137–1164. [Google Scholar]
- Kiros G-E, and White MJ (2004). Migration, community context, and child immunization in Ethiopia. Soc. Sci. Med. 59, 2603–2616. [DOI] [PubMed] [Google Scholar]
- Kohler H-P, Watkins SC, Behrman JR, Anglewicz P, Kohler IV, Thornton RL, Mkandawire J, Honde H, Hawara A, Chilima B, et al. (2014). Cohort profile: The Malawi longitudinal study of families and health (MLSFH). Int. J. Epidemiol. 44, 394–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kusuma YS, Kumari R, Pandav CS, and Gupta SK (2010). Migration and immunization: determinants of childhood immunization uptake among socioeconomically disadvantaged migrants in Delhi, India. Trop. Med. Int. Health 15, 1326–1332. [DOI] [PubMed] [Google Scholar]
- Lahaie C, Hayes JA, Piper TM, and Heymann J (2009). Work and family divided across borders: the impact of parental migration on Mexican children in transnational families. Community Work Fam. 12, 299–312. [Google Scholar]
- Landale NS, Oropesa RS, and Gorman BK (2000). Migration and infant death: Assimilation or selective migration among Puerto Ricans? Am. Sociol. Rev. 888–909. [Google Scholar]
- Lu Y (2008). Test of the ‘healthy migrant hypothesis’: a longitudinal analysis of health selectivity of internal migration in Indonesia. Soc. Sci. Med. 67, 1331–1339. [DOI] [PubMed] [Google Scholar]
- Lu Y, and Qin L (2014). Healthy migrant and salmon bias hypotheses: a study of health and internal migration in China. Soc. Sci. Med. 102, 41–48. [DOI] [PubMed] [Google Scholar]
- Madhavan S, Schatz E, Clark S, and Collinson M (2012). Child mobility, maternal status, and household composition in rural South Africa. Demography 49, 699–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maggi S, Ostry A, Callaghan K, Hershler R, Chen L, D’Angiulli A, and Hertzman C (2010). Rural-urban migration patterns and mental health diagnoses of adolescents and young adults in British Columbia, Canada: a case-control study. Child Adolesc. Psychiatry Ment. Health 4, 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mberu BU, and Mutua M (2015). Internal migration and early life mortality in Kenya and Nigeria. Popul. Space Place 21, 788–808. [Google Scholar]
- McMichael AJ (2000). The urban environment and health in a world of increasing globalization: issues for developing countries. Bull. World Health Organ. 78, 1117–1126. [PMC free article] [PubMed] [Google Scholar]
- Montes de Oca V, García TR, Sáenz R, and Guillén J (2011). The Linkage of Life Course, Migration, Health, and Aging: Health in Adults and Elderly Mexican Migrants. J. Aging Health 23, 1116–1140. [DOI] [PubMed] [Google Scholar]
- Mtika MM, and Doctor HV (2002). Matriliny, Patriliny, and Wealth Flow Variations in Rural Malawi. Afr. Sociol. Rev. Rev. Afr. Sociol. 6, 71–97. [Google Scholar]
- National Statistics Office and ICF Macro The DHS Program - Malawi: Standard DHS, 2010. [Google Scholar]
- Nauman E, VanLandingham M, Anglewicz P, Patthavanit U, and Punpuing S (2015). Rural-to-urban migration and changes in health among young adults in Thailand. Demography 52, 233–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omariba DWR, and Boyle MH (2010). Rural–urban migration and cross-national variation in infant mortality in less developed countries. Popul. Res. Policy Rev. 29, 275–296. [Google Scholar]
- Palloni A, and Morenoff JD (2001). Interpreting the paradoxical in the Hispanic paradox: demographic and epidemiologic approaches. Ann. N. Y. Acad. Sci. 954, 140–174. [DOI] [PubMed] [Google Scholar]
- Reniers G (2003). Divorce and Remarriage in Rural Malawi. Demogr. Res. S1, 175–206. [Google Scholar]
- Roshania R, Narayan KV, and Oza-Frank R (2008). Age at arrival and risk of obesity among US immigrants. Obesity 16, 2669–2675. [DOI] [PubMed] [Google Scholar]
- Rubia M, Marcos I, and Muennig PA (2002). Increased risk of heart disease and stroke among foreign-born females residing in the United States. Am. J. Prev. Med. 22, 30–35. [DOI] [PubMed] [Google Scholar]
- Schuyler AC, Edelstein ZR, Mathur S, Sekasanvu J, Nalugoda F, Gray R, Wawer MJ, Serwadda DM, and Santelli JS (2017). Mobility among youth in Rakai, Uganda: Trends, characteristics, and associations with behavioural risk factors for HIV. Glob. Public Health 12, 1033–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sime D, and Fox R (2015). Migrant Children, Social Capital and Access to Services Post-Migration: Transitions, Negotiations and Complex Agencies. Child. Soc. 29, 524–534. [Google Scholar]
- Singh GK, and Hiatt RA (2006). Trends and disparities in socioeconomic and behavioural characteristics, life expectancy, and cause-specific mortality of native-born and foreign-born populations in the United States, 1979–2003. Int. J. Epidemiol. 35, 903–919. [DOI] [PubMed] [Google Scholar]
- Smith-Greenaway E, and Madhavan S (2015). Maternal migration and child health: An analysis of disruption and adaptation processes in Benin. Soc. Sci. Res. 54, 146–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ssengonzi R, De Jong GF, and Stokes CS (2002). The effect of female migration on infant and child survival in Uganda. Popul. Res. Policy Rev. 21, 403–431. [Google Scholar]
- Stephenson R, Matthews Z, and McDonald JW (2003). The impact of rural–urban migration on under-two mortality in India. J. Biosoc. Sci. 35, 15–31. [DOI] [PubMed] [Google Scholar]
- Szreter S (1997). Economic growth, disruption, deprivation, disease, and death: on the importance of the politics of public health for development. Popul. Dev. Rev. 693–728. [Google Scholar]
- UN (2009). World Urbanization Prospects: the 2009 Revision. U. N. Dep. Econ. Soc. Aff; N. Y. USA. [Google Scholar]
- UNAIDS (2018). Malawi | UNAIDS. [Google Scholar]
- Wanda BP (1988). Customary family law in Malawi: Adherence to tradition and adaptability to change. J. Leg. Plur. Unoff. Law 20, 117–134. [Google Scholar]
- Williams DR, Herman A, Stein DJ, Heeringa SG, Jackson PB, Moomal H, and Kessler RC (2008). Twelve-month mental disorders in South Africa: prevalence, service use and demographic correlates in the population-based South African Stress and Health Study. Psychol. Med. 38, 211–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson ME (1995). Infectious diseases: an ecological perspective. BMJ 311, 1681–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie Y, and Greenman E (2011). THE SOCIAL CONTEXT OF ASSIMILATION: TESTING IMPLICATIONS OF SEGMENTED ASSIMILATION THEORY. Soc. Sci. Res. 40, 965–984. [DOI] [PMC free article] [PubMed] [Google Scholar]


