Abstract
BACKGROUND:
The “safety culture” within hospital systems is increasingly recognized as important to delivery of high-quality care. We examine the safety culture in a statewide hospital quality improvement collaborative and its associations with surgical outcomes.
STUDY DESIGN:
A modified Safety Attitudes Questionnaire was sent to administrators, quality improvement teams, nurses, anesthesiologists, and surgeons in 49 hospitals participating in the Illinois Surgical Quality Improvement Collaborative in 2015. Associations between positive safety culture, as measured by percentage of positive responses on the Safety Attitudes Questionnaire, and the following NSQIP 30-day adverse outcomes: hospital-level risk-adjusted morbidity, mortality, death, or serious morbidity and readmission rates. Linear regression models with hospitals clustered by system were used to assess the relationship between safety culture and patient outcomes.
RESULTS:
Operating room safety culture scores were highest (97.7% positive) compared with the other domains, and ratings of hospital management were lowest (75.9% positive). Hospital administrators consistently had the most positive perception of the safety culture (90.5% positive) and front-line providers were less positive: physicians (85.3%), advanced practice providers (88.1%), and nurses (80%). Teamwork was rated as a strength by patient care providers (physicians 88.3%, advanced practice providers 90.2%, and nurses 82.2%), but was perceived as weakest by administrators. Higher percentage of positive Safety Attitudes Questionnaire responses was significantly associated with lower risk of postoperative morbidity (p = 0.007) and death or serious morbidity (p = 0.04). No significant association between safety culture and the risk of mortality (p = 0.23) or readmissions (p = 0.52) was observed.
CONCLUSIONS:
Hospital safety culture can influence certain surgical patient outcomes. Improving the safety culture within a hospital can represent a previously unrecognized approach that can be leveraged to strengthen surgical quality improvement efforts at the hospital level.
The “safety culture” of the hospital has been defined as individual and institutional values, attitudes, and perceptions of health and safety management combined with the hospital’s ability to respond to identified patient safety problems.1 This safety culture within hospital systems is increasingly viewed as an important component in the delivery of high-quality care. Efforts to improve safety culture have demonstrated an ability to positively influence both staff perception and patient outcomes in specific areas. Teamwork training and checklist implementation in the operating room have resulted in improved staff perception of safety during operations in a number of studies.2-5 In the ICU setting, positive safety culture has been associated with lower rates of morbidity and mortality and decreased length of stay.6 Statewide quality improvement (QI) collaboratives have been identified as a vehicle that can be used to improve safety culture within hospitals,7 and have been successful in doing so in intensive care.8
The Illinois Surgical Quality Improvement Collaborative (ISQIC), which began with 49 hospitals in 2014, now includes 56 Illinois hospitals. The ISQIC members represent diverse care environments and include all major academic teaching hospitals in the state and 9 small rural hospitals. The collaborative’s hospitals perform 50% of the total surgical procedures performed in the state of Illinois and >80% of complex operations; approximately 550,000 surgical procedures are performed in ISQIC hospitals yearly. All hospitals in the collaborative participate in NSQIP and have defined surgeon champions. In addition, ISQIC supports the QI team at participating hospitals with formal QI education, external QI coaches, surgeon mentors, and hosts biannual collaborative meetings. Hospitals are also provided with de-identified, hospital-level reports, benchmarked to other ISQIC hospitals, assessing NSQIP outcomes and adherence to ISQIC process measures used in collaborative QI projects. The ISQIC periodically surveys all participating hospitals to assess QI resources, administrating engagement, and culture. As a component of the ongoing assessment of the collaborative, the Safety Attitudes Questionnaire (SAQ)9 was administered to surgeons, nurses, operating room staff, hospital administrators, and QI teams at all ISQIC hospitals in years 1 and 3 of the collaborative’s existence. The SAQ has been identified previously as a valid tool for the assessment of surgical safety culture among hospitals.10
Despite the development of tools to measure safety culture at the hospital level, very little is known about the influence of safety culture on patient-level outcomes after surgical procedures. Kaplan and colleagues11 hypothesized that interdependent and mutually reinforcing relationships between the care environment and QI infrastructure in hospitals helped to determine the degree to which QI interventions found success in healthcare. The authors formally developed a conceptual model to describe these relationships, the Model for Understanding Success in Quality (MUSIQ).11 This model was subsequently adapted by our group with a specific focus on surgical QI. The revised ISQIC model specifically focuses on the interrelated importance of the hospital environment, the perioperative microsystem, and the surgical QI team in surgical quality.12 We have used this conceptual model to guide the structure of interventions in ISQIC, hoping to influence the development of QI infrastructure and a paradigm for change in hospitals statewide. Based on this conceptual model, it would be anticipated that the safety culture of the institution could potentially influence patient-level outcomes. Therefore, we conducted a cross-sectional study to describe the perception of hospital safety culture surrounding surgical care at the diverse group of hospitals engaged in ISQIC in year 1 of the program. We also examined the association between this institutional safety culture and postoperative outcomes in surgical patients.
METHODS
Survey administration
To assess baseline safety culture, we administered the SAQ at all 49 adult ISQIC hospitals between January and May 2015. Potential survey subjects were identified from personnel lists provided by the individual ISQIC hospitals. Hospitals were asked to specifically identify individuals directly involved in the care of surgical patients. Surveys were distributed via email to surgery and anesthesia physician staff; floor ICU and operating room nursing staff; hospital administration; and hospital QI and process improvement teams. The respondents were asked to consider their responses in terms of the patient care environment within their clinical unit. Respondents were provided with a unique link to REDCap to complete the survey securely. The validated SAQ was used to assess the culture of teamwork, communication, safety, and patient care at each hospital.9 The instrument is composed of 7 domains (Teamwork, Safety, Operating Room Safety, Unit Management, Hospital Management, Working Conditions, and Employee Engagement), each containing between 2 and 24 individual items (Table 1). An eighth domain was created to specifically interrogate the engagement of the surgeon champion at participating hospitals. This element was included specifically to assess the baseline function of the surgeon champion at ISQIC hospitals; engaging these individuals was a specific component of ISQIC implementation. Responses were collected using a 5-point Likert scale format (strongly disagree, disagree, neutral, agree, and strongly agree). The questionnaires from which the ISQIC SAQ was adapted have been validated and widely used in the measurement of hospital safety culture in earlier studies.13-17
Table 1.
Safety Attitudes Questionnaire Domains
| Domain | No. of items | Description |
|---|---|---|
| Teamwork | 6 | Support, coordination, ability to speak up/ask questions, disagreement resolution |
| Safety | 24 | Handling of clinical errors, perceptions of safety, incident and error reporting, adherence to guidelines for care, assessment of colleagues’ performance |
| Operating room safety | 2 | Briefing and information availability before operation |
| Working conditions | 4 | Training, supervision, provision of information |
| Unit management | 5 | Management support, handling of personnel issues, staffing levels |
| Hospital management | 5 | Management support, handling of personnel issues, staffing levels |
| Surgeon champion engagement | 5 | Surgeon champion leadership, motivation, effectiveness |
| Employee engagement | 6 | Employee participation, hospital leadership, and surgeon involvement in quality initiatives, employee voices being heard |
| Overall composite | 57 | All domains combined |
Patient outcomes data source
Postoperative patient outcomes were assessed using data from the American College of Surgeons (ACS) NSQIP for operations performed between July 1, 2014 and June 30, 2015. The ACS NSQIP database collects 30-day postoperative outcomes for a systematic sample of patients at participating hospitals. Patient-level data on patient characteristics, coexisting conditions, operative details, and surgical outcomes were obtained from ACS NSQIP. The program, which has been described in detail previously, provides a validated system for the collection of high-quality clinical data to measure surgical outcomes.18-20 Data on patients 18 years of age or older are collected in ACS NSQIP for most surgical specialties, excluding trauma and transplantation surgery, by trained, certified, and audited data abstractors at each site.18 The abstractors ascertain patient outcomes by examining the medical record, discussing with treating physicians, and contacting patients directly when needed. The end points of interest were the NSQIP-defined variables for morbidity, mortality, composite death or serious morbidity (DSM), and unplanned readmission. The morbidity measure captures a variety of postoperative complications, including cardiac arrest requiring resuscitation; MI; ventilator dependence for more than 48 hours; pneumonia; progressive renal insufficiency; acute renal failure; sepsis or septic shock, deep incisional, organ space, and superficial surgical site infections (SSI); stroke/CVA; unplanned intubation; urinary tract infection; and dehiscence. The DSM composite includes the complications in the morbidity measure except for ventilator dependence, superficial SSI, and stroke/CVA, and additionally includes venous thromboembolism.
Statistical analysis
The SAQ responses were examined both by domain and as an overall composite score. Descriptive statistics were calculated. Safety culture was measured as the percentage of positive responses (for each item, a response of agree or strongly agree, or in the case of negatively worded items, disagree or strongly disagree) out of all items answered across respondents at each hospital. Only respondents who answered 5 or more items from the survey were included.
Hospital-level risk-adjusted event rates were used for each NSQIP end point. These rates were computed from 2-level hierarchical logistic regression models with standard NSQIP patient-level risk adjustment, including CPT linear risk, which allowed for inclusion of all NSQIP-eligible procedure types.20 Risk-adjustment variables, such as patient characteristics, comorbidities, and preoperative laboratory values, were identified by forward selection logistic regression procedures run separately for morbidity, mortality, and readmission. The DSM model contained a smaller fixed set of patient risk-adjustment variables. From each of the hierarchical models, hospital-level predicted-to-expected event ratios were computed and multiplied by the overall outcomes rate in the data set to generate the risk-adjusted complication rates. The patient outcomes analysis was performed as part of ISQIC’s semiannual quality benchmarking report activities, based on NSQIP’s semiannual reports to hospitals. Finally, linear regression models with hospitals clustered by hospital system were used to assess the relationships between safety culture (percentage of positive responses on the 57-item SAQ composite rescaled to increments of 10% [range 0 to 10]) and patient outcomes (risk-adjusted complication rates), adjusting for Joint Commission accreditation, American Nurses Credentialing Center (ANCC) Magnet status, an ACGME-approved residency program, rural locale, hospital control (church-affiliated, other nonprofit, or government/for-profit), nurse-to-bed ratio, and annual surgical volume. Hospital covariates were taken from the 2013 American Hospital Association Annual Survey, except for ANCC Magnet status, which was identified from the ANCC website.21
The level of statistical significance was set at 0.05 and all tests were 2-sided. Statistical analyses were performed using SAS, version 9.3 (SAS Institute). The study was deemed non-human subjects research by the IRB at Northwestern University.
RESULTS
Responses to the SAQ and patient outcomes data were available from 49 adult hospitals at the time of data collection and included diverse hospital types (Table 2). Most hospitals (n = 41; 83.7%) were Joint Commission-accredited and 21 (42.9%) had achieved ANCC Magnet status. The ACGME-accredited residency programs were present in 51% (n = 25) of hospitals. The majority of hospitals were in urban or suburban settings (88%; n = 43), with 6 rural hospitals (11%) also taking part in the collaborative during year 1. Most ISQIC hospitals were operated as not-for-profit institutions (57%; n = 28), 35% had a religious affiliation (n = 17), and 8% (n = 4) operated as either government or for-profit entities. The median annual surgical volume was 9,529 (interquartile range 5,993 to 13,017). With respect to postoperative hospital-level risk-adjusted complication rates, the median patient overall morbidity was 5.9%, mortality was 1.0%, DSM was 7.8%, and readmission was 5.0%.
Table 2.
Illinois Surgical Quality Improvement Collaborative Safety Attitudes Questionnaire and Hospital Characteristics
| Variable | Hospitals (n = 49) |
|---|---|
| Hospital characteristic | |
| Joint Commission accreditation, n (%) | 41 (83.7) |
| American Nurses Credentialing Center Magnet status, n (%) | 21 (42.9) |
| ACGME-approved residency program, n (%) | 25 (51.0) |
| Rural hospital, n (%) | 6 (12.2) |
| Hospital management, n (%) | |
| Religious affiliation | 17 (34.7) |
| Other non-profit | 28 (57.1) |
| For-profit or government | 4 (8.2) |
| Nurse-to-bed ratio, median (IQR) | 1.9 (1.5–2.3) |
| Total no. of operations annually, median (IQR) | 9,529 (5,993–13,017) |
| SAQ domains, overall % positive responses, median (IQR) | |
| Overall composite | 82.8 (80.1–86.6) |
| Teamwork | 84.4 (79.6–89.6) |
| Safety, median (IQR) | 84.9 (80.4–87.8) |
| Operating room safety | 97.7 (90.0–100) |
| Unit management | 85.7 (79.7–90.0) |
| Hospital management | 75.9 (70.7–80.4) |
| Working conditions | 82.2 (75.4–86.2) |
| Surgeon champion engagement | 85.7 (74.3–91.4) |
| Employee engagement | 81.6 (77.1–86.1) |
| Risk-adjusted postoperative complication rate, median (IQR) | |
| Morbidity | 5.9 (5.3–6.4) |
| Mortality | 1.0 (0.9–1.1) |
| Death/serious morbidity | 7.8 (7.0–8.1) |
| Readmission | 5.0 (4.4–5.6) |
IQR, interquartile range; SAQ Safety Attitudes Questionnaire.
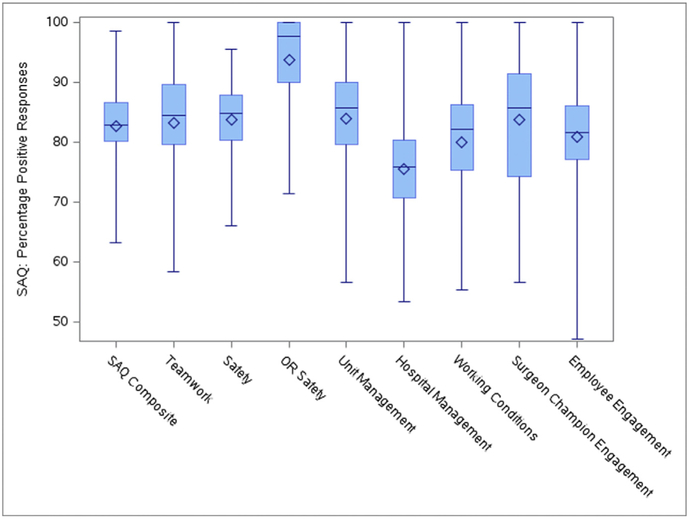
The total SAQ response rate was 47% (871 of 1,837 surveys, based on respondents who answered at least 5 items from the questionnaire). Hospital-specific response rates ranged from 15% to 84%. Individual hospitals had between 4 and 32 respondents. Additional analysis was performed to examine the relationship between response rate and hospital environment. The response rates ranged from 15.4% to 84.2% across hospitals. Individual hospitals had between 4 and 32 respondents. We ran t-tests for differences in the response rate by ACGME residency program, Joint Commission on Accreditation of Healthcare Organizations accreditation, rural hospital, magnet status, and ANOVA for hospital control. None were statistically significant at p < 0.05. The most positive perception of safety culture was observed when respondents were asked questions pertaining to operating room safety (97.7% positive responses) (Fig. 1). Conversely, respondents perceived the role of hospital administration in promoting a positive safety culture to be the least positive (75.5% positive responses).
Figure 1.
Box plots of the percentage of positive Safety Attitudes Questionnaire (SAQ) responses by domain among Illinois Surgical Quality Improvement Collaborative hospitals. OR, operating room.
Perceptions of hospital safety culture were also examined based on the role of the respondent within the healthcare institution (Table 3). Hospital administrators consistently had the most positive perception of the safety culture at their institutions, recording positive ratings for >90% of the items asked on the SAQ survey. However, front-line providers viewed safety culture less positively, with physicians recording positive responses on 85.3% of items and advanced practice providers on 88.1%. Nursing staff had the lowest perception of safety culture, with only 80% recording positive responses. Among both providers and administrators, culture was thought to be most positive with respect to the climate of safety in the operating room (percent positive responses: attending physicians 94.5%, advanced practice providers 91.7%, nurses 91.1%, and administrators 100%). Conversely, teamwork was believed to be a strong point by many respondents involved in direct patient care (attending physicians 88.3%, advanced practice providers 90.2%, and nurses 82.2%); but was perceived to be the weakest area by hospital administrators.
Table 3.
Mean Percentage Positive Responses by Safety Attitudes Questionnaire Domain and Position of Employment
| Variable | Hospital administrator (n = 103) |
Attending/staff physician (n = 131) |
Physician’s assistant/nurse practitioner (n = 17) |
Nurse (n = 460) | Quality improvement team member (n = 108) |
|---|---|---|---|---|---|
| SAQ composite | 90.5 (87.7–93.2) | 85.3 (82.1–88.6) | 88.1 (82.5–93.6) | 80.0 (77.9–82.1) | 82.2 (78.2–86.2) |
| Teamwork climate | 88.3 (84.4–92.2) | 88.3 (84.1–92.5) | 90.2 (83.0–97.4) | 82.2 (79.4–85.0) | 79.4 (72.9–86.0) |
| Safety climate | 88.3 (85.3–91.3) | 83.6 (80.1–87.1) | 92.5 (88.7–96.4) | 83.0 (81.0–85.0) | 81.6 (77.3–86.0) |
| Operating room safety climate | 100.00 | 94.5 (91.49–97.58) | 91.7 (80.55–102.78) | 91.1 (87.36–94.81) | 90.0 (77.1–102.9) |
| Working conditions | 92.6 (88.9–96.2) | 82.4 (78.0–86.8) | 77.9 (67.7–88.2) | 77.5 (73.7–81.2) | 74.1 (65.6–82.7) |
| Hospital management | 96.4 (93.4–99.5) | 82.3 (77.6–87.1) | 76.5 (60.5–92.4) | 67.4 (63.6–71.1) | 81.2 (74.8–87.6) |
| Unit management | 95.0 (91.4–98.6) | 86.5 (82.3–90.8) | 84.7 (73.2–96.3) | 80.9 (77.4–84.4) | 86.6 (81.9–91.3) |
| Surgeon champion | 92.6 (87.6–97.6) | 91.4 (87.3–95.6) | 83.8 (67.0–100.5) | 78.5 (74.2–82.9) | 88.6 (84.1–93.1) |
| Employee engagement | 97.1 (95.3–98.9) | 85.8 (81.7–89.9) | 88.8 (77.3–100.2) | 74.9 (71.6–78.1) | 82.3 (76.5–88.1) |
Values are mean (95% CI). Based on 819 respondents who fully completed at least 1 domain. The number of responses in each employment category varies by domain. The maximum number who responded to any domain is displayed.
SAQ, Safety Attitudes Questionnaire.
Results from the linear regression models for the association between SAQ responses and risk-adjusted complication rates are displayed in Table 4. A 10% increase in the percentage of positive responses on the SAQ was associated with a statistically significantly lower risk-adjusted rate of both postoperative overall morbidity (−0.52%; p = 0.007) and of death or serious morbidity (−0.29%; p = 0.04). Each 10% incremental improvement in SAQ responses would reduce the risk-adjusted rate of perioperative complications by 0.52% and the rate of DSM by 0.29%. No significant association was observed between the SAQ composite score and either mortality (p = 0.23) or rates of readmission (p = 0.52). Model R2 values (all, <0.30) indicate that only a small proportion of the variation in risk-adjusted postoperative complications were accounted for in the models by safety culture and hospital characteristics, underscoring the multifactorial drivers of outcomes in surgical patients.
Table 4.
Association Between Safety Attitudes Questionnaire Survey Items and Postoperative Outcomes
| Variable | Morbidity | Mortality | Death or serious morbidity | Readmission |
|---|---|---|---|---|
| Percentage of positive responses on the SAQ composite (10% increments) | −0.519* (0.177) | −0.063 (0.051) | −0.292* (0.136) | −0.116 (1.422) |
| Joint Commission Accreditation | −0.185 (0.217) | −0.063 (0.039) | −0.009 (0.240) | −0.196 (0.223) |
| American Nurses Credentialing Center Magnet status | −0.056 (0.295) | −0.075* (0.033) | −0.025 (0.287) | −0.346 (0.354) |
| ACGME-approved residency program | −0.194 (0.215) | 0.009 (0.040) | −0.144 (0.279) | 0.234 (0.179) |
| Rural hospital | 0.642* (0.216) | 0.016 (0.045) | 0.261 (0.183) | 0.440† (0.235) |
| Hospital control | ||||
| Other non-profit organization | 0.144 (0.264) | −0.035 (0.043) | 0.016 (0.292) | 0.121 (0.196) |
| For-profit or government | −0.586 (0.415) | −0.021 (0.092) | −0.141 (0.433) | −0.466† (0.243) |
| Nurse-to-bed ratio | 0.461* (0.176) | 0.059† (0.033) | 0.299 (0.197) | 0.301 (0.210) |
| Total operations annually | −0.000 (0.000) | −0.000 (0.000) | −0.000 (0.00) | −0.000* (0.000) |
| Intercept | 9.56* (1.629) | 1.522* (0.396) | 9.538* (1.042) | 5.845* (1.422) |
| Model R2 | 0.251 | 0.202 | 0.068 | 0.235 |
Values are coefficient (SE). Results are from linear regression models of hospital risk-adjusted 30-day complication rates regressed on the percentage of positive responses on the SAQ scaled to 10% increments (range 1 to 10) and hospital characteristics from the American Hospital Association 2013 annual survey and the American Nurses Credentialing Center.
p < 0.05.
p < 0.01.
SAQ, Safety Attitudes Questionnaire.
DISCUSSION
The study is the first to examine the influence of safety culture across multiple surgical outcomes in a diverse patient population including a wide variety of operative interventions. Our findings support the potential importance of intrinsic institutional factors, such as the development of culture that promotes patient safety for improved outcomes at the patient level. We found positive safety culture to be associated with significantly lower risk-adjusted rates of morbidity in Illinois hospitals, and marginally significantly lower rates of DSM. Although the R2 values in this study were <0.30, these values are similar to if not higher than the R2 values reported in other published work examining the influence of factors such as hospital volume on outcomes.22-25 However, the exact manner and extent to which a positive hospital culture can influence patient-level outcomes remains somewhat unclear.
Hospital safety culture is generally described as the presence of a number of factors, including attitudes, beliefs, and perceptions of management and employees, which influence the overall environment of care and includes facets of teamwork, communication, and error recognition and reporting.3 Hospitals with a positive safety culture are typically characterized by high levels of both patient and provider satisfaction26 and by low rates of staff turnover.27 In addition, the importance of responsive and collegial management structures that encourage the discussion of potential safety concerns has also been recognized as an important component in the development of a positive hospital culture.26 Yet, the ability to accurately measure the cultural environment of a hospital remains somewhat difficult.28 The SAQ16 was designed for this purpose and has been widely used to quantify safety culture in the ICU setting,6,29-31 as well as in other aspects of acute hospital care, including in surgical specialties.2,4,10,32,33
Just as wide variation exists in the structure of hospitals in the US, safety culture also varies considerably from hospital to hospital.34,35 Safety culture does not appear to be simply a function of the hospital structure, but rather is related to the relationships built within the institution across roles, and involves both administrators and providers.34,35 This is an important concept, as safety culture can consequently be influenced without major structural change in the hospital infrastructure. This makes cultural improvement an attractive target for interventions aimed at care improvement. In our study, the most positive responses were seen with questions pertaining to operating room safety culture. The operating room environment represents a discrete clinical microsystem with a small number of providers relative to the hospital at large, and where a particular focus is placed on patient safety. The creation of a positive culture of safety in the operating room provides a discrete example of the ability of targeted interventions to improve safety culture within hospital systems.
A positive hospital safety culture was associated with reduced rates of serious morbidity in our study across the wide range of surgical procedures captured in the NSQIP database. Although this is the first study to look at the influence of culture on surgical outcomes globally within hospitals, authors have demonstrated similar findings in specific surgical disciplines previously. Fan and colleagues36 assessed the culture of surgical units at 7 hospitals using the Hospital Survey on Patient Safety Culture and the rates of SSI after colon procedures in these hospitals. After adjustment for surgical volume and patient comorbidities, they found an association between hospital safety culture and reduced SSI in 9 of the 12 measured domains of hospital culture.
Although a positive safety culture does appear to be associated with certain more favorable outcomes, it remains unclear whether efforts to improve hospital safety culture will result in concomitant improvements in outcomes for patients. However, an emerging body of literature indicates that this might be the case. In a study of clinical performance of staff in pediatric cardiac surgery units, the recognition and reporting of errors was identified as a significant psychological burden that negatively impacted patient care, but was improved with interventions to create a positive unit safety culture.37 Similar efforts to promote a culture of safety in the operating room environment have also been shown to directly impact patient outcomes. Haynes and colleagues32 demonstrated that the institution of an operative checklist routine resulted in improved operating room SAQ scores and a concomitant reduction in postoperative complication rate (r = 0.7143; p = 0.0381). These results have since been replicated by a number of authors.2-4,33 Hospital-level interventions aimed at improving safety culture have also demonstrated some efficacy. A study performed in the Mayo Clinic care network used a learning collaborative approach to building a positive safety culture through enhanced leadership engagement resulted in increased process measure compliance and a reduction in risk-stratified mortality after acute MI.38-40 These studies provide support for the concept that interventions aimed at improving culture might be able to directly impact patient outcomes as well. Although additional data are needed to validate this relationship, the theoretical construct has important implications for QI and patient safety efforts in healthcare systems.
It is important to acknowledge the presence of some specific limitations of the current analysis. First, the assessment of safety culture was performed using a survey tool that, although validated, provides only a subjective assessment of the institutional culture. In ongoing work, our group is performing site visits at collaborative hospitals that can provide a correlative, qualitative assessment of hospital culture. In addition, not all individuals working at each institution were surveyed, and not all of those to whom a survey was distributed ultimately responded. Although a 45% response rate is reasonable in large-scale survey research, it is difficult to know what impact response bias might have on the measurement of safety culture, as demographic information is not available for nonrespondents. Finally, we chose to use risk-adjusted outcomes variables for the analysis, given the difficulty in accounting for the variety contextual features that can influence the outcomes for an individual patient. This risk adjustment might, in fact, also adjust for some of the contextual features that are components of safety culture, functionally blunting the observed effect of safety culture on the tested outcomes. This approach was chosen to provide the highest standard for any positive finding of an association between safety culture and outcomes. It is possible that differential effects might be seen if specific subsets of patients, or specific surgical procedures, were examined independently.
CONCLUSIONS
This study demonstrates positive hospital safety culture can influence certain outcomes in surgical patients, with the greatest effect seen in the form of lower postoperative morbidity. This protective influence of safety culture could be independent of the operation or individual provider, and rather an effect of the environment of care. The full nature of this interaction is likely to involve a number of factors, and additional investigation is needed to determine the precise mechanisms by which the culture of a hospital can impact patient outcomes and how these might be optimized to improve care. However, efforts to improve hospital safety culture might represent a previously unrecognized approach that can be leveraged to strengthen surgical QI programs.
Acknowledgments
Support: Illinois Surgical Quality Improvement Collaborative receives support from the Edward Mallinckrodt, Jr Foundation. Dr Odell receives support from the National Cancer Institute under Award Number K07CA216330. Dr Yang receives support from the National Heart, Lung, and Blood Institute under Award Number K08HL145139. Dr Bilimoria receives support from the Agency for Healthcare Research and Quality under Award Number R01HS024516.
Abbreviations and Acronyms
- ACS
American College of Surgeons
- ANCC
American Nurses Credentialing Center
- DSM
death or serious morbidity
- ISQIC
Illinois Surgical Quality Improvement Collaborative
- QI
quality improvement
- SAQ
Safety Attitudes Questionnaire
- SSI
surgical site infection
Footnotes
Disclosure Information: Illinois Surgical Quality Improvement Collaborative receives support from Blue Cross/Blue Shield of Illinois. All authors have nothing additional to disclose.
Presented at the Annual American College of Surgeons NSQIP meeting, San Diego, CA, July 2016. The work was recognized as the “Best Clinical Abstract.”
REFERENCES
- 1.Sorra J, Nieva VF. Hospital Survey on Patient Safety Culture (Prepared by Westat under contract no. 290-96-0004). AHRQ Publication No. 04-0041. Rockville, MD: Agency for Healthcare Research and Quality; 2004. [Google Scholar]
- 2.Makary MA, Mukherjee A, Sexton JB, et al. Operating room briefings and wrong-site surgery. J Am Coll Surg 2007;204: 236–243. [DOI] [PubMed] [Google Scholar]
- 3.Makary MA, Sexton JB, Freischlag JA, et al. Operating room teamwork among physicians and nurses: teamwork in the eye of the beholder. J Am Coll Surg 2006;202:746–752. [DOI] [PubMed] [Google Scholar]
- 4.Hill MR, Roberts MJ, Alderson ML, Gale TC. Safety culture and the 5 steps to safer surgery: an intervention study. Br J Anaesthesia 2015;114:958–962. [DOI] [PubMed] [Google Scholar]
- 5.Sexton JB, Makary MA, Tersigni AR, et al. Teamwork in the operating room: frontline perspectives among hospitals and operating room personnel. Anesthesiology 2006;105: 877–884. [DOI] [PubMed] [Google Scholar]
- 6.Huang DT, Clermont G, Kong L, et al. Intensive care unit safety culture and outcomes: a US multicenter study. Int J Qual Health Care 2010;22:151–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pronovost PJ, Berenholtz SM, Goeschel C, et al. Improving patient safety in intensive care units in Michigan. J Crit Care 2008;23:207–221. [DOI] [PubMed] [Google Scholar]
- 8.Sexton JB, Berenholtz SM, Goeschel CA, et al. Assessing and improving safety climate in a large cohort of intensive care units. Crit Care Med 2011;39:934–939. [DOI] [PubMed] [Google Scholar]
- 9.Cohen AB, Restuccia JD, Shwartz M, et al. A survey of hospital quality improvement activities. Med Care Res Rev 2008;65: 571–595. [DOI] [PubMed] [Google Scholar]
- 10.Makary MA, Sexton JB, Freischlag JA, et al. Patient safety in surgery. Ann Surg 2006;243:628–632; discussion 632–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaplan HC, Provost LP, Froehle CM, Margolis PA. The Model for Understanding Success in Quality (MUSIQ): building a theory of context in healthcare quality improvement. BMJ Qual Saf 2012;21:13–20. [DOI] [PubMed] [Google Scholar]
- 12.Wandling MW, Minami CA, Johnson JK, et al. Development of a conceptual model for surgical quality improvement collaboratives. JAMA Surg 2016;151:1181–1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Etchegaray JM, Thomas EJ. Comparing two safety culture surveys: safety attitudes questionnaire and hospital survey on patient safety. BMJ Qual Saf 2012;21:490–498. [DOI] [PubMed] [Google Scholar]
- 14.Nguyen G, Gambashidze N, Ilyas SA, Pascu D. Validation of the safety Attitudes Questionnaire (short form 2006) in Italian in hospitals in the northeast of Italy. BMC Health Serv Res 2015;15:284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Profit J, Lee HC, Sharek PJ, et al. Comparing NICU teamwork and safety climate across two commonly used survey instruments. BMJ Qual Saf 2016;25:954–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sexton JB, Helmreich RL, Neilands TB, et al. The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res 2006;6:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Watts BV, Percarpio K, West P, Mills PD. Use of the Safety Attitudes Questionnaire as a measure in patient safety improvement. J Patient Saf 2010;6:206–209. [DOI] [PubMed] [Google Scholar]
- 18.Shiloach M, Frencher SK Jr, Steeger JE, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 2010;210:6–16. [DOI] [PubMed] [Google Scholar]
- 19.Merkow RP, Hall BL, Cohen ME, et al. Validity and feasibility of the American College of Surgeons colectomy composite outcome quality measure. Ann Surg 2013;257:483–489. [DOI] [PubMed] [Google Scholar]
- 20.Cohen ME, Ko CY, Bilimoria KY, et al. Optimizing ACS NSQIP modeling for evaluation of surgical quality and risk: patient risk adjustment, procedure mix adjustment, shrinkage adjustment, and surgical focus. J Am Coll Surg 2013;217:336–346.e1. [DOI] [PubMed] [Google Scholar]
- 21.Kester BS, Wayne JD, Ross MI, et al. An opportunity to ensure high-quality melanoma care through the use of a preoperative treatment algorithm. Ann Surg Oncol 2013;20: 3976–3983. [DOI] [PubMed] [Google Scholar]
- 22.Birkmeyer JD, Dimick JB, Staiger DO. Operative mortality and procedure volume as predictors of subsequent hospital performance. Ann Surg 2006;243:411–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med 2002;346:1128–1137. [DOI] [PubMed] [Google Scholar]
- 24.Hollenbeck BK, Wei Y, Birkmeyer JD. Volume, process of care, and operative mortality for cystectomy for bladder cancer. Urology 2007;69:871–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reames BN, Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital volume and operative mortality in the modern era. Ann Surg 2014;260:244–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lingard L, Espin S, Whyte S, et al. Communication failures in the operating room: an observational classification of recurrent types and effects. Qual Saf Health Care 2004;13:330–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oliveira RM, Leitao IM, Aguiar LL, et al. Evaluating the intervening factors in patient safety: focusing on hospital nursing staff. Rev Esc Enferm USP 2015;49:104–113. [DOI] [PubMed] [Google Scholar]
- 28.Jackson J, Sarac C, Flin R. Hospital safety climate surveys: measurement issues. Curr Opin Crit Care 2010;16:632–638. [DOI] [PubMed] [Google Scholar]
- 29.Huang DT, Clermont G, Sexton JB, et al. Perceptions of safety culture vary across the intensive care units of a single institution. Crit Care Med 2007;35:165–176. [DOI] [PubMed] [Google Scholar]
- 30.Profit J, Etchegaray J, Petersen LA, et al. The Safety Attitudes Questionnaire as a tool for benchmarking safety culture in the NICU. Arch Dis Child Fetal Neonatal Ed 2012;97: F127–F132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.France DJ, Greevy RA Jr, Liu X, et al. Measuring and comparing safety climate in intensive care units. Med Care 2010;48:279–284. [DOI] [PubMed] [Google Scholar]
- 32.Haynes AB, Weiser TG, Berry WR, et al. Changes in safety attitude and relationship to decreased postoperative morbidity and mortality following implementation of a checklist-based surgical safety intervention. BMJ Qual Saf 2011;20:102–107. [DOI] [PubMed] [Google Scholar]
- 33.Olsson C, Forsberg A, Bjersa K. Safety climate and readiness for implementation of evidence and person centered practice—a national study of registered nurses in general surgical care at Swedish university hospitals. BMC Nurs 2016;15:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Singer SJ, Gaba DM, Geppert JJ, et al. The culture of safety: results of an organization-wide survey in 15 California hospitals. Qual Saf Health Care 2003;12:112–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Speroff T, Nwosu S, Greevy R, et al. Organisational culture: variation across hospitals and connection to patient safety climate. Qual Saf Health Care 2010;19:592–596. [DOI] [PubMed] [Google Scholar]
- 36.Fan CJ, Pawlik TM, Daniels T, et al. Association of safety culture with surgical site infection outcomes. J Am Coll Surg 2016;222:122–128. [DOI] [PubMed] [Google Scholar]
- 37.Bognar A, Barach P, Johnson JK, et al. Errors and the burden of errors: attitudes, perceptions, and the culture of safety in pediatric cardiac surgical teams. Ann Thorac Surg 2008;85: 1374–1381. [DOI] [PubMed] [Google Scholar]
- 38.Bradley EH, Brewster AL, McNatt Z, et al. How guiding coalitions promote positive culture change in hospitals: a longitudinal mixed methods interventional study. BMJ Qual Saf 2018;27:218–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Curry LA, Brault MA, Linnander EL, et al. Influencing organisational culture to improve hospital performance in care of patients with acute myocardial infarction: a mixed-methods intervention study. BMJ Qual Saf 2018;27:207–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Curry LA, Linnander EL, Brewster AL, et al. Organizational culture change in U.S. hospitals: a mixed methods longitudinal intervention study. Implement Sci 2015;10:29. [DOI] [PMC free article] [PubMed] [Google Scholar]