Abstract
Introduction
Amyotrophic lateral sclerosis (ALS) is an intractable and incurable neurological disease. It is a progressive disease characterized by muscle atrophy and weakness caused by selective vulnerability of upper and lower motor neurons. In disease research, it has been common to use mouse models carrying mutations in responsible genes for familial ALS as pathological models of ALS. However, there is no model that has reproduced the actual conditions of human spinal cord pathology. Thus, we developed a method of producing human spinal motor neurons using human induced pluripotent stem cells (iPSCs) and an innovative experimental technique for drug screening. As a result, ropinirole hydrochloride was eventually discovered after considering such results as its preferable transitivity in the brain and tolerability, including possible adverse reactions. Therefore, we explore the safety, tolerability and efficacy of ropinirole hydrochloride as an ALS treatment in this clinical trial.
Methods
The ROPALS trial is a single-center double-blind randomized parallel group-controlled trial of the safety, tolerability, and efficacy of the ropinirole hydrochloride extended-release tablet (Requip CR) at 2- to 16-mg doses in patients with ALS. Twenty patients will be recruited for the active drug group (fifteen patients) and placebo group (five patients). All patients will be able to receive the standard ALS treatment of riluzole if not changed the dosage during this trial. The primary outcome will be safety and tolerability at 24 weeks, defined from the date of randomization. Secondary outcome will be the efficacy, including any change in the ALS Functional Rating Scale-Revised (ALSFRS-R), change in the Combined Assessment of Function and Survival (CAFS), and the composite endpoint as a sum of Z-transformed scores on various clinical items. Notably, we will perform an explorative search for a drug effect evaluation using the patient-derived iPSCs to prove this trial concept. Eligible patients will have El Escorial Possible, clinically possible and laboratory-supported, clinically probable, or clinically definite amyotrophic lateral sclerosis with disease duration less than 60 months (inclusive), an ALSFRS-R score ≥2 points on all items and age from 20 to 80 years.
Conclusion
Patient recruitment began in December 2018 and the last patient is expected to complete the trial protocol in November 2020.
Trial registration
Current controlled trials UMIN000034954 and JMA-IIA00397
Protocol version
version 1.6 (Date; 5/Apr/2019).
Keywords: Amyotrophic lateral sclerosis, Ropinirole hydrochloride, Requip CR, iPSC-drug discovery
Abbreviations: ADR, Adverse reaction; AE, Adverse effect; ALP, Alkaline phosphatase; ALS, Amyotrophic lateral sclerosis; ALT, Alanine aminotransferase; ALSFRS-R, ALS Functional Rating Scale-Revised; ALSAQ-40, Amyotrophic Lateral Sclerosis Assessment Questionnaire-40; APTT, Activated partial thromboplastin time; AST, Aspartate aminotransferase; BUN, Blood urea nitrogen; CAFS, Combined Assessment of Function and Survival; CK, Creatine kinase; CPK, Creatine phosphokinase; CRP, C-reactive protein; CTCAE, Common terminology Criteria for Adverse Events; EDC, Electronic data capture; FALS, Familial ALS; FAS, Full analysis set; %FVC, Forced vital capacity; GCP, Good clinical practice; HBs, Hepatitis B surface; HCG, Human chorionic gonadotropin; HCV, Hepatitis C virus; HDL, High-density lipoprotein; HIV, Human immunodeficiency virus; HTLV-1, Human T-cell leukemia virus type 1; IRB, Institutional review board; LDH, Lactate dehydrogenase; LDL, Low-density lipoprotein; MMT, Manual muscle testing; NfL, Neurofilament light chain; PPS, Per protocol set; PT, Prothrombin time; QOL, Quality of life; SAE, Severe adverse effect; SALS, sporadic ALS; SOD, Superoxide dismutase; TDP-43, Transactive response DNA-binding protein 43; TPHA, Treponema pallidum hemagglutination; 6-OHDA, 6-hydroxydopamine; 8-OHdG, 8-Hydroxydeoxyguanosine
Highlights
-
•
ALS is a progressive neurodegenerative disease caused by selective vulnerability of upper and lower motor neurons.
-
•
ALS patients have no radical treatment.
-
•
The ROPALS trial reveals the safety, tolerability, and efficacy of the ropinirole hydrochloride in patients with ALS.
-
•
This trial is the pioneering clinical trial for ALS based on iPSCs-drug discovery in Japan.
1. Introduction
Amyotrophic lateral sclerosis (ALS) is an intractable and incurable progressive neurological disease, which is characterized by muscle atrophy and weakness caused by selective vulnerability of upper and lower motor neurons. Patients with ALS develop symptoms such as gait difficulty, dysarthria, dysphagia, and respiratory disorder, which confound their freedom and ability to communicate. However, their consciousness and perception are completely normal, and this feature of the disease significantly reduces their quality of life (QOL) [1].
The annual crude prevalence and incidence rates per 100 000 people per year were 9.9 (95% CI 9.7–10.1) and 2.2 (95% CI 2.1–2.3), respectively, in Japan. The male–female ratio was approximately 1.5 and the age group with the highest prevalence as well as incidence was 70–79 years [2]. ALS develops mainly after middle-age, which impedes engaging in society. Therefore, the psychological and financial burdens of patients and their family are serious. While the clinical course varies among patients, the median time from onset to death or to the use of respiratory support has been reported to be 20–48 months.
Familial ALS (FALS) accounts for 5%–10% of all ALS cases, and the other 90% are classified as sporadic ALS (SALS), which has not been clearly elucidated for its genetic background or etiologic factors. More than 100 point mutations spanning the SOD1 sequence have been identified in patients with FALS (gain of function type). In addition, at least 25 responsible genes have also been reported [1]. Therefore, to develop treatment options for ALS, including SALS, which represents the majority of ALS cases, an approach to treating pathological conditions that are common to FALS and SALS is required. Specific loss and degeneration of upper and lower motor neurons and their nerve fibers are present in both FALS and SALS; thus, preventing motor neuron degeneration and death is key in developing treatment options that are common to both forms of ALS.
The pathological conditions of ALS have been studied, and the cellular process that follows after its onset—mitochondrial dysfunction, protein aggregation, oxidative stress, agitation toxicity, inflammatory response, and apoptosis—has been partly elucidated. Mitochondrial abnormalities can occur as an initial event of neurodegeneration or secondary to other cellular processes, and may also be the cause of oxidative stress, agitation toxicity, and apoptosis in some cases [1].
Riluzole, which is considered to exert neuroprotective effects by reducing glutamate toxicity, has been approved for the treatment of ALS. Riluzole was shown to potentially increase survival in some clinical trials and is therefore used widely in Japan [3], [4], [5], [6], [7], [8]. However, the effect of riluzole is not completely satisfactory for patients. Furthermore, edaravone injection solution was approved for the additional indication of inhibiting the progression of functional disorder in ALS. However, no study has been conducted to confirm the impact on survival, and the beneficial effect on survival has not yet been verified [9], [10]. Under these circumstances, development of treatment options to promote motor neuron survival is anticipated.
Ropinirole hydrochloride (trade name: Requip Tablets 0.25 mg, 1 mg, and 2 mg) is a dopamine receptor agonist with a non-ergot alkaloid chemical structure, which was synthesized and developed based on the structure of dopamine by GlaxoSmithKline Ltd. Co (UK). Ropinirole hydrochloride is selective for the D2 subtype of dopamine receptors. It was first approved for the indication of Parkinson's disease in the UK in July 1996 and was later approved worldwide. The drug in this trial (Requip Controlled-release (CR) Tablets 2 mg and CR Tablets 8 mg) is an extended-release formulation of ropinirole hydrochloride. This product was first approved in the Slovak Republic in 2006 and is now approved worldwide.
Ropinirole hydrochloride not only improves motor symptoms of Parkinson's disease by stimulating the dopamine receptors (particularly dopamine D2-like receptor), but also, exhibits the following neuroprotective properties in animal models: 1) preventing the decrease in 6-OHDA-induced striatal dopamine levels [11], 2) increasing glutathione, SOD, and catalase activities [11], [12], 3) promoting neurotrophic factor production in the ventral mesencephalon [13] and 4) promoting neural stem cell proliferation in the subventricular zone [14].
Pramipexole hydrochloride (PPX), with activity as a D2-like dopamine receptor agonist, which shares common function as dopamine agonist with ropinirole hydrochloride, has been demonstrated to have a protective effect on mitochondria and a free radical scavenging effect. Therefore, with hopes of improving the pathological conditions of ALS, a clinical study was conducted using dexpramipexole (RPPX), which is the R(+) enantiomer of PPX. RPPX does not have the dopamine receptor agonist activity, so has no adverse drug reactions [ADRs] by the dopamine receptor agonist activity). A phase I clinical study of RPPX was conducted as a randomized, double-blind, placebo-controlled study in 54 healthy volunteers. In that study, RPPX was well tolerated at doses up to 300 mg/data [15]. In the historical-controlled phase II study that followed, RPPX was administered to 30 ALS patients at a dose of 30 mg/day for 6 months. It was tolerated and improved the slope of decline on the ALS Functional Rating Scale-Revised (ALSFRS-R) score by 13% [16]. In a dose escalation study in 10 ALS patients, the dose of RPPX was increased to a maximum of 300 mg/day, which was confirmed to be safe and tolerable with no dopaminergic ADRs reported. This study was continued as an extension study, in which RPPX was administered at doses of 30 mg/day and 60 mg/day for 6 months for comparison. As a result, the decline (exacerbation) of the slope of the ALSFRS-R score was smaller at 60 mg/day than at 30 mg/day [16]. Next, a randomized, double-blind, placebo-controlled, phase II study was conducted, and the safety and tolerability of RPPX were evaluated in ALS patients. This study was divided into two parts: at Stage 1, 102 subjects were randomized to receive either RPPX 50 mg/day, 150 mg/day, 300 mg/day, or placebo for 12 weeks. At Stage 2, 92 subjects who underwent a 4-week washout were randomized to receive either 50 mg/day or 300 mg/day for 24 weeks. RPPX was generally safe and well tolerated. The slope of the ALSFRS-R score was markedly reduced in the higher dose group at both Stages 1 and 2, and the hazard ratio of mortality was reduced by 68% in the 300 mg/day group, compared with the 50 mg/day group at Stage 2 (p = 0.07, log-rank test). Treatment at 300 mg/day was significantly more beneficial in terms of the integrated outcome of the changes in ALSFRS-R and mortality (p = 0.046, joint-rank test) [17].
Based on these results, a phase III, multicenter, randomized, double-blind, placebo-controlled study of RPPX (EMPOWER) was conducted in ALS patients in the US, Canada, Australia, and Europe; however, regrettably, the results were clinically insignificant [18]. Nevertheless, there is still plenty of opportunities for improvement in clinical study design, including selection of patients, treatment method, and evaluation methods (especially methods other than the ALSFRS-R).
In ALS research, it is common to use mouse models carrying mutations in responsible genes for FALS as pathological models of ALS. However, the mutant SOD-1 transgenic mice model that has been most frequently used in previous pre-clinical studies do not show the aggregation of phosphorylated TDP-43, the most typical pathogenic feature of human ALS. While the recently reported TDP-43 or FUS transgenic/knock-in mice models showed some human ALS-like pathology [19], such as aggregation of TDP-43/FUS proteins, these model mice have not been used for the successful development of new drugs for ALS so far.
Thus, we developed a method of producing human spinal motor neurons using human iPSCs and an innovative experimental technique for drug screening [20]. Using this system, spinal motor neurons were produced from iPSCs from healthy individuals as well as patients of familial ALS (TDP-43 and FUS mutations) and/or SALS. Then, drug screening was carried out with existing drug libraries with improved ALS-related phenotypes using patient-derived spinal motor neurons in a dish. As a result, several candidate drugs came up, and ropinirole hydrochloride was eventually discovered after considering such results as blood–brain barrier permeability and tolerability. As mentioned above, the previous Phase III clinical trial for ALS (the EMPOWER study) used RPPX (R(+) enantiomer of PPX, with no D2R-agonist activity) [18]. Notably, by using an in vitro model, we showed that ropinirole hydrochloride had significantly superior anti-ALS therapeutic activity compared with the already-approved drugs for ALS (riluzole and edaravone), PPX or RPPX [20], suggesting the rationale to use ropinirole hydrochloride to conduct the present clinical trial. In the present clinical trial (the ROPALS trial), we explore the safety, tolerability and efficacy of ropinirole hydrochloride to ALS.
2. Methods
2.1. Study objectives
Primary Objective: To exploratively assess the safety (type, frequency, and severity of adverse events [AEs], and time course of laboratory test values) and tolerability of the ropinirole hydrochloride extended-release tablet in ALS patients.
Secondary Objective: To exploratively assess the efficacy of the ropinirole hydrochloride extended-release tablet, compared with placebo, in terms of delay in the progression of ALS.
2.2. Subject population
Patients affected by probable (clinically or laboratory supported) or definite ALS [21] must satisfy all the inclusion and exclusion criteria (Table 1) upon the interim registration during the 28-day screening period through clinical evaluation and laboratory and instrumental assessment. Screening assessments include general and neurological examinations, ALSFRS-R, blood sampling, biochemical and pregnancy evaluations (for fertile females), urinalysis, ECG, and spirometry. Moreover, patients also must meet all the inclusion and exclusion criteria (Table 1) upon the official registration after the 3-month run-in period.
Table 1.
Inclusion and exclusion criteria for the ROPALS trial.
| Inclusion criteria | Exclusion criteria |
|---|---|
[Interim Registration]
|
|
3. Explanation to subjects and caregivers and their informed consent
3.1. Subjects
3.1.1. Preparation of written information and informed consent form
The investigator will prepare written information for subjects and an informed consent form (hereinafter collectively referred to as the informed consent document). The informed consent document is an all-in-one document or a set of documents, and will be revised, as appropriate. The prepared informed consent document will be submitted to the head of the study site to obtain approval of the IRB prior to the start of the study.
3.1.2. Matters to be contained in the informed consent document
Items listed below must be at least contained in the written information for subjects.
-
(1)
That the study involves research
-
(2)
The purpose of the study
-
(3)
The name, title, and contact information of the investigator
-
(4)
The study procedure(s) (including experimental aspects of the study, subject inclusion criteria, and probability for random assignment to each treatment)
-
(5)
Reasonably expected benefits, and foreseeable risks or inconveniences to subjects (When there is no intended clinical benefit to subjects, the subjects should be made aware of this.)
-
(6)
Presence/absence of alternative courses of treatment, and if present, their expected notable benefits and risks in a study in patients
-
(7)
The expected duration of subject's participation in the study
-
(8)
That the subject's participation in the study is voluntary and that the subject can withdraw from or refuse participation in the study or his/her legal representative can withdraw the subject from or refuse his/her participation in the study at any time, without penalty or loss of benefits to which the subject is otherwise entitled
-
(9)
That individuals involved in the study, including monitors, auditors, IRB, etc. and regulatory authorities, may request direct access to source documents, without violating the subject's confidentiality, and that, by signing or sealing the informed consent form, the subject or his/her legal representative authorizes such access
-
(10)
That the subject's identity remains confidential even when the study results are published
-
(11)
The person(s) to contact at the study site for further information about the study and subject's rights or in the event of a study-related health injury
-
(12)
Compensation and/or treatment available to the subject in the event of a study-related health injury
-
(13)
The type of the IRB that reviews the appropriateness etc. of the study, items to be reviewed at each IRB meeting, and other IRB-related matters in the study
-
(14)
The planned number of subjects involved in the study
-
(15)
That the subject or his/her legal representative will be informed immediately when information is obtained that may affect the subject's or his/her legal representative's willingness to continue participation in the study
-
(16)
Conditions or reasons for withdrawing the subject from his/her participation in the study
-
(17)
The anticipated financial burden, if any, on the subject for participation in the study
-
(18)
The anticipated prorated payment, if any, to the subject for participation in the study (e.g., agreement on payment estimation)
-
(19)
Matters to be adhered to by the subjects.
3.1.3. Method of obtaining informed consent
-
(1)
Prior to the start of the study, the investigator will distribute the informed consent document approved by the IRB to patients as prospective study subjects and provide them with an adequate explanation of the contents of the study. A study collaborator may provide a supplementary explanation. Explanations should be provided in as plain language as possible so that patients can understand them, based on the informed consent document for the study, and patient's questions must be adequately answered. After confirming that the patients have fully understood the contents of the explanation, the investigator will obtain their voluntary written informed consent for participation in the study. Interim registration will take place within 28 days of informed consent obtainment. The presence of cognitive impairment is not listed in the exclusion criteria (Table 1) because as many ALS patients as possible are to be recruited for the evaluation of safety profiles of ropinirole hydrochloride. However, we will be very careful in obtaining the informed consent from the ALS patients with possible cognitive impairment. First, when the cognitive impairment is too severe for them to perform “writing” or “using chopsticks”, they are to be excluded by the ALSFRS-R criteria (Table 1). Second, when the patients do not fully understand the protocol, informed consent can be obtained from their close proxies. Importantly, however, these patients can also be excluded based on investigator's judgement (Table 1).
-
(2)
The investigator who provides the explanation and the patient will affix their names/seals or signatures to the informed consent form, with the date. The study collaborator who provides a supplementary explanation will also affix his/her name/seal or signature to the informed consent form, with the date.
-
(3)
If the patient is unable to sign the informed consent document due to a loss of upper limb function caused by ALS symptoms, the investigator will provide an adequate explanation in the presence of a fair witness, and obtain voluntary written informed consent to participate in the study from the patient. The witness will also affix his/her name/seal or signature to the informed consent form, with the date, and provide the relationship with the patient. If the patient is physically unable to sign, his/her witness will write the reason for his/her inability to give an authentic signature to the informed consent form.
-
(4)
The investigator will issue the signed and dated informed consent document to the subjects before their participation in the study. The original informed consent form will be appropriately retained in accordance with the regulations of the study site.
3.1.4. Revision of the informed consent document
-
(1)
If new important information that could be relevant to the subject's willingness to continue is obtained, the investigator will immediately decide whether or not to revise the informed consent document based on the obtained information.
-
(2)
If it is deemed necessary to revise the informed consent document, the investigator must revise the document and forward it to the IRB to reobtain its approval.
-
(3)
In the case of the above (2), the investigator will immediately notify the subjects already participating in the study of the matter verbally, confirm their willingness to continue participation in the study, and record the result in the medical record.
-
(4)
The investigator will provide subjects already participating in the study with an explanation using the informed consent document reapproved by the IRB, and obtain voluntary written informed consent for continued participation in the study from the subjects.
-
(5)
As in the case of obtaining the initial informed consent, the investigator who provides the information and the subject will affix their names/seals or signatures to the informed consent form, with the date. The study collaborator who provides a supplementary explanation will also affix his/her name/seal or signature to the informed consent form, with the date.
-
(6)
The investigator will issue the signed and dated informed consent document to the subjects. The original informed consent form will be appropriately retained in accordance with the regulations of the study site.
3.2. Caregivers
The Zarit Caregiver Burden Interview is set as an endpoint in this study. Because this assessment will be conducted by caregivers of the subjects, written informed consent must also be obtained from caregivers. Caregiver's assessment will be made wherever possible, and subjects are able to participate in the study even if their caregivers do not provide informed consent. Subjects will designate their caregivers involved in the assessment. Subjects are allowed to designate two or more caregivers or change the caregivers during the study. If the study for the subject is discontinued, the caregiver's assessment will be ended upon completion of the assessment at the time of discontinuation (wherever possible).
3.2.1. Preparation of written information and informed consent form
The investigator will prepare the informed consent document for caregivers. The informed consent document is an all-in-one document or a set of documents, and will be revised, as appropriate. The prepared informed consent document will be submitted to the head of the study site to obtain IRB's approval prior to the start of the study.
3.2.2. Matters to be contained in the informed consent document
Items listed below must be at least contained in the informed consent document.
-
(1)
Qualification required for caregivers involved in the assessment
-
(2)
Roles of caregivers
-
(3)
That caregiver's participation in the study is voluntary and that the caregiver can withdraw from or refuse participation in the study at any time, without penalty or loss of benefits to which the subject is otherwise entitled
-
(4)
Information collected
-
(5)
Use of study data and protection of privacy
-
(6)
The name, title, and contact information of the investigator
3.2.3. Method of obtaining informed consent
-
(1)
Prior to the start of the study, the investigator will distribute the informed consent document approved by the IRB to caregivers of prospective study subjects, and provide them with an adequate explanation of the contents of the study. A study collaborator may provide a supplementary explanation. Explanations should be provided in as plain language as possible so that patients can understand them, based on the informed consent document for the study, and caregiver's questions must be adequately answered. After confirming that the caregivers have fully understood the contents of the explanation, the investigator will obtain their voluntary written informed consent for participation in the study.
-
(2)
The investigator who provides the explanation and the caregiver will affix their names/seals or signatures to the informed consent form, with the date. The study collaborator who provides a supplementary explanation will also affix his/her name/seal or signature to the informed consent form, with the date.
-
(3)
The investigator will issue the signed and dated informed consent document to the caregivers before their participation in the study. The original informed consent form will be appropriately retained in accordance with the regulations of the study site.
4. Study design
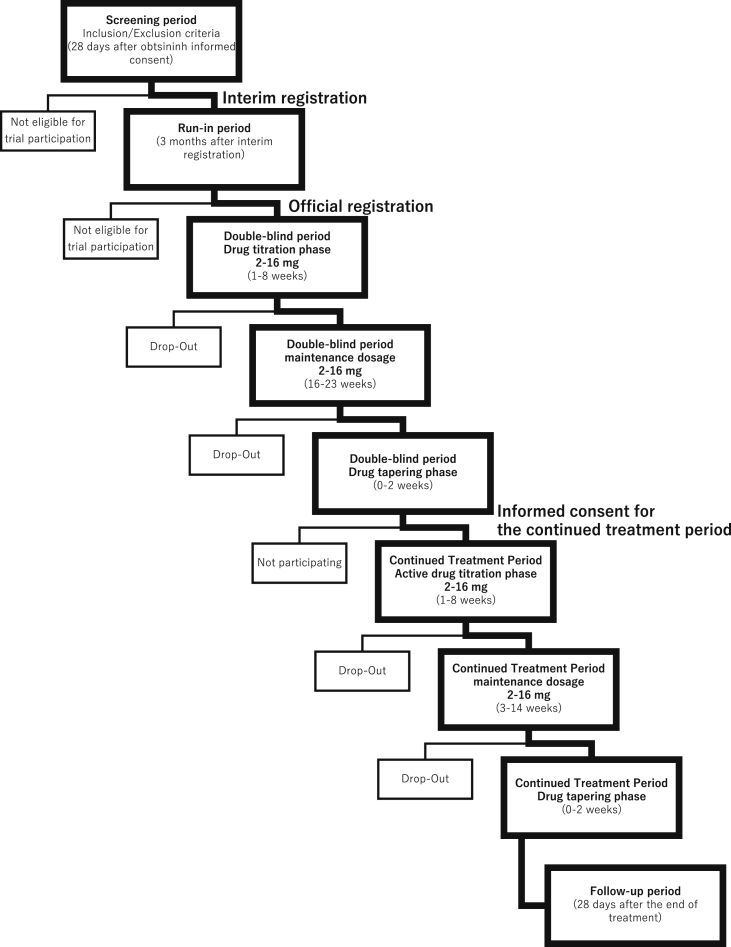
The flow of this study is shown Table 2a, Table 2ba,b.
Table 2a.
The flow of this study.
| Informed consent | Screening period | Interim registration | Run-in period | Official registration | Double-blind period *1 | Informed consent for the continued treatment period | Continued treatment period *1 | Follow-up period |
| 28 days after obtaining informed consent | 3 months after interim registration | 24 weeks | 4–22 weeks | 28 days after the end of treatment | ||||
| Eligibility confirmation for interim registration | Eligibility confirmation for official registration | Oral administration of the active drug or placebo | Oral administration of the active drug | Follow-up assessment | ||||
| *2 |
*1: When the study proceeds to the continued treatment period or when the treatment is completed, the dose of the study drug should be tapered in accordance with the Study Drug Tapering Protocol (Table 4).
*2: When the study does not proceed to the continued treatment period, the procedure during the follow-up period should be performed.
Table 2b.
The flow chart of this study.
4.1. Phase and type of the study
Study phase: Phase I/IIa, Study type: Exploratory study
4.2. Study design
-
•
Double-blind period: Single center (Keio University Hospital), randomized, double-blind, placebo-controlled design
-
•
Continued treatment period: Single center (Keio University Hospital), open-label, uncontrolled, active drug continued treatment design
This study consists of the following periods.
-
(1)
Screening period (from informed consent to interim registration)
-
(2)
Run-in period: 12 weeks (from interim registration to official registration)
-
(3)
Double-blind period: 24 weeks
-
(4)
Tapering treatment period: 0–2 weeks
-
(5)
Continued treatment period (open-label) (only for subjects willing to receive continued treatment): 4–22 weeks
-
(6)
Tapering treatment period (after the continued treatment period): 0–2 weeks
-
(7)
Follow-up period (after the double-blind period, the continued treatment period, or the time of discontinuation): within 28 days
[Screening period]
After obtaining informed consent, necessary tests/observations will be performed. Eligibility assessment will then be conducted, and interim registration will take place. Interim registration will be performed within 28 days of informed consent obtainment.
[Run-in period]
After interim registration, eligibility will be reconfirmed during the run-in period (12 weeks ± 7 days), and official registration will take place. In addition to the criteria for interim registration, subjects must have the change in ALSFRS-R score within the range between −2 and −5 points during the 12-week run-in period to be eligible for official registration. This criterion will be confirmed to complete official registration.
[Double-blind period]
After the first dose of the study drug, the dose will be increased once weekly. Treatment with the study drug (study treatment) will be started at a first dose of 2 mg, followed by increases in the dose to a maximum of 16 mg, and subjects will be monitored until Week 24. Study treatment will be started within 15 days after official registration. The last dose of study treatment during the double-blind period will be administered on the preceding day of Week 25. If the study proceeds to the continued treatment period, the double-blind period is defined as the period before study drug administration at Week-25. In principle, subjects will be monitored under hospitalization for approximately 1 week from the preceding day of the first dose of the study treatment (subjects are allowed to be temporarily discharged during the specified test period if their hospital discharge is considered valid by the investigator). Subsequently, a once-weekly dose increase (allowable range: ±3 days), treatment, and monitoring will be conducted in outpatient settings.
[Tapering treatment period]
After the double-blind period, the dose of the study drug will be tapered in accordance with the Study Drug Tapering Protocol (Table 4). If the study does not proceed to the continued treatment period, the study treatment will be completed.
[Continued treatment period]
Table 4.
Study drug tapering protocol for proceeding to the continued treatment period.
| Final target dose | Week 0 | Week 1 | Week 2 |
|---|---|---|---|
| ●◯ 2 mg | ● 2 mg (1st week of the continued treatment period) | – | – |
| ●◯ 4 mg | ● 2 mg (1st week of the continued treatment period) | – | – |
| ●◯ 6 mg | ●◯ 4 mg (two 2-mg tablets) | ● 2 mg (1st week of the continued treatment period) | – |
| ●◯ 8 mg | ●◯ 6 mg (three 2-mg tablets) | ●◯ 4 mg (two 2-mg tablets) | ● 2 mg (1st week of the continued treatment period) |
| ●◯ 10 mg | ●◯ 8 mg (one 8-mg tablet) | ●◯ 4 mg (two 2-mg tablets) | ● 2 mg (1st week of the continued treatment period) |
| ●◯ 12 mg | ●◯ 8 mg (one 8-mg tablet) | ●◯ 4 mg (two 2-mg tablets) | ● 2 mg (1st week of the continued treatment period) |
| ●◯ 14 mg | ●◯ 10 mg (one 8-mg tablet + one 2-mg tablets) | ●◯ 6 mg (three 2-mg tablets) | ● 2 mg (1st week of the continued treatment period) |
| ●◯ 16 mg | ●◯ 12 mg (one 8-mg tablet + two 2-mg tablets) | ●◯ 6 mg (three 2-mg tablets) | ● 2 mg (1st week of the continued treatment period) |
●: Active drug.
◯: Placebo.
Upon completion of the double-blind period, the subjects can choose whether to complete the study or continue treatment with the active drug under an open-label design (continued treatment period). The continued treatment period is 4–22 weeks; if any of the criteria listed in “12.1 Discontinuation Criteria for Subjects” are met, the study for the relevant subject should be discontinued even before the 22-week period is attained. For subjects who are unable to stay in the study for at least 4 weeks after proceeding to the continued treatment period, the study will be discontinued at the end of the double-blind period without proceeding to the continued treatment period.
When proceeding to the continued treatment period, the dose of the study drug will be tapered (it will take 2 weeks in the case of reducing the dose from the maximum of 16 mg) for both the active drug and placebo groups in accordance with the Study Drug Tapering Protocol (Table 4) to maintain the blindness. Subsequently, treatment with the active drug will be started at a dose of 2 mg, followed by increases in the dose to a maximum of 16 mg in accordance with the Study Drug Titration Protocol (Table 3).
[Tapering treatment period (after the continued treatment period)]
Table 3.
Study drug titration protocol.
| After the start of treatment | Week 1 | Week 2 | Week 3 | Week 4 | Week 5 | Week 6 | Week 7 | Week 8 | From Week 9 |
|---|---|---|---|---|---|---|---|---|---|
| Active drug/placebo at a dose of 2 mg | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | 0 |
| Active drug/placebo at a dose of 8 mg | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 2 |
| Total number of tablets taken | 1 | 2 | 3 | 4 | 2 | 3 | 4 | 5 | 2 |
| Total dose | 2 mg | 4 mg | 6 mg | 8 mg | 10 mg | 12 mg | 14 mg | 16 mg | 16 mg |
After the end of the continued treatment period, the dose of the study drug will be tapered in accordance with the Study Drug Tapering Protocol (Table 4), and the study treatment will be completed.
[Follow-up period]
The final observation will be performed within 28 days after the end of the tapering treatment period.
4.3. Methods procedures such as blinding and randomization
4.3.1. Method of blinding
The study drug randomization manager will confirm the indistinguishability in appearance and packaging form among the ropinirole hydrochloride extended-release 2 mg tablet, the ropinirole hydrochloride extended-release 8 mg tablet, and placebo before drug assignment.
The study drug randomization manager will prepare the treatment code and emergency code in accordance with the procedural document separately prepared.
4.3.2. Methods of randomization and assignment
The investigator will enter the information required for registration in an electronic data capture (EDC) system. Subjects who are eligible for the study will be randomized to either the active drug or placebo group on the EDC system. The result of treatment assignment and the registration number will be transmitted automatically via e-mail to the unblinded pharmacist of the study site.
Subjects will be randomly assigned to either the active drug or placebo at a 3:1 ratio by dynamic allocation incorporating probabilistic elements with the following variables as allocation adjustment factors.
-
(1)
Number of months after onset (“≥30 months” and “<30 months”)
-
(2)
Age (“≥65 years” and “<65 years”)
-
(3)
Total ALSFRS-R score (“≤36 points” and “≥37 points”)
4.4. Endpoints
4.4.1. Primary endpoints
Type, frequency, and severity of AEs, and time course of laboratory test values, and intergroup difference in the proportion of discontinued subjects during the 24-week double-blind period (from official registration to the final observation at Week 24 of the double-blind period).
4.4.2. Secondary endpoints
-
(1)
Ratio of change in the ALSFRS-R score every 4 weeks between pre-treatment and post-treatment assessments
The change in the ALSFRS-R score every 4 weeks during the run-in period and the change in the ALSFRS-R score every 4 weeks during the 24-week double-blind period will be calculated, and the latter-to-former ratio will be determined as the delta (Δ) ALSFRS-R ratio. The change in the ALSFRS-R score every 4 weeks during the 24-week double-blind period will be calculated using a simple linear regression model with the measured ALSFRS-R score as a response variable and the number of days from the treatment start day at each measurement time point as an explanatory variable.
The ratio between the treatment groups will be tested for comparison.
-
(2)
Intergroup difference in the change in the ALSFRS-R score (ΔALSFRS-R) during the 24-week double-blind period (from Day 1 to Week 24 of the double-blind period)
The ALSFRS-R score will be assessed according to the specified schedule. The difference (ΔALSFRS-R) in the change from the day of the first dose of the study treatment in the ALSFRS-R score at Week 24 of the double-blind period between the treatment groups will be tested for comparison.
-
(3)
Change in the ALSFRS-R score during the continued treatment period (from the assessment at the start to the final assessment of the continued treatment period) and during the overall treatment period (from Day 1 of the double-blind period to the final assessment of the continued treatment period) (ΔALSFRS-R).
-
(4)
Combined Assessment of Function and Survival (CAFS) score [22] during the 24-week double-blind period (from Day 1 to Week 24 of the double-blind period), during the continued treatment period (from the assessment at the start to the final assessment of the continued treatment period), and during the overall treatment period (from Day 1 of the double-blind period to the final assessment of the continued treatment period).
-
(5)Composite endpoint as a sum of Z-transformed scores on the following items [23].
-
•ALSFRS-R sub-score of each domain (bulbar function, limb function, and respiratory function)
-
•ALS severity classification
-
•Simple respiratory function test (FEV1, FEV6)
-
•Detailed respiratory function test (VC, %FVC, FEV1%)
-
•Manual muscle testing (MMT) score (limb and trunk muscles)
-
1)Quantitative muscle strength (The same muscle as for the MMT assessment should be used.)
-
2)Grip strength and pinch strength
-
3)Modified Norris Scale (Bulbar Symptom Score)
-
4)Tongue pressure
-
5)Body weight
-
6)Amount of physical activity and number of steps
-
7)Objective muscle mass determined using computed tomography (CT) for skeletal muscle
-
8)Amyotrophic Lateral Sclerosis Assessment Questionnaire-40 (ALSAQ-40) score (QOL assessment)
-
•
-
(6)
Time to death or time to a specified state of disease progression
The time to onset of any of the following events from the day of the first dose of treatment will be assessed.
Death, inability of independent ambulation, loss of unilateral upper limb function, a) tracheostomy, respiratory support, b) tube feeding, c) loss of vocal conversation, d) and inability of oral administration. e)
-
a)
Loss of unilateral upper limb function: a condition where the subject is unable to grip a pen in one hand, as a guide.
-
b)
Respiratory support: Noninvasive respiratory support during all-day hours (generally, at least 22 h except for meal hours) or invasive respiratory support.
-
c)
A condition where “Swallowing” on the ALSFRS-R is scored 0 points: “nothing by mouth (NPO); exclusively parenteral or enteral feeding.”
-
d)
Loss of vocal conversation: barely able to speak to express emotions or unable to speak.
-
e)
Inability to take oral medications: the disease progresses for reasons other than the above a) to c), which renders the subject incapable of orally taking the medication.
-
(7)
Time to %FVC of ≤50%
The length of time until %FVC decreases to ≤50% from the day of the first dose of the study treatment will be assessed.
-
(8)
Time to decrease of at least 6 points in the ALSFRS-R score (at least a 6-point decrease in the ALSFRS-R score [ΔALSFRS-R] from Day 1 of the double-blind period].
The time to decrease of at least 6 points in ALSFRS-R score (at least a 6-points decrease in the ALSFRS-R score [ΔALSFRS-R] from the day of the first dose of the study treatment) from the ALSFRS-R score measurement on the day of the first dose of the study treatment will be assessed.
-
(9)
Proportion of patients who discontinued the treatment (discontinuation rate) during the period from Day 1 of the double-blind period to the final assessment of the continued treatment period.
4.4.3. Exploratory endpoints
-
(1)
Comparison of the in vitro drug effect evaluation and clinical effect using patient iPSC-derived motor neurons
Blood samples will be collected from subjects who have provided separate informed consent and iPSCs will be established at the Department of Physiology, Keio University School of Medicine. These iPSCs will be directed to differentiate into motor neurons to reproduce the pathological conditions of ALS. The cells will then be treated with ropinirole hydrochloride and will be assessed for a delay in the progression of ALS. The correlation between the results and the change in phenotype of subjects treated with medication will be examined.
-
(2)
Explorative search of new biomarkers for diagnosis, pathology, and drug effect evaluation
-
9)
Measurement of biomarkers related to the ALS pathology, including TDP-43 and NfL in blood and spinal fluid
Proteins such as TDP-43 and NfL, which are biomarkers related to ALS pathology, in blood and spinal fluid collected from subjects will be measured using single molecule arrays (Simoa™) or immunomagnetic reduction (IMR) assay.
-
10)
RNA expression analysis before and after treatment with ropinirole hydrochloride
Total and micro RNAs will be extracted from exosomes in blood and spinal fluid collected from subjects and analyzed using microarrays or RNA-seq. RNA extracts will be used for network analysis etc. to identify variable factors associated with disease progression and Hub genes that may contribute to the therapeutic effect of ropinirole hydrochloride.
-
(3)
Search of known familial ALS genes
Blood samples collected from subjects who have provided informed consent will be transported to the Department of Neurology, Tohoku University School of Medicine, and mutations in known FALS-related genes will be searched using a targeted resequencing panel for screening of ALS.
This assessment will be conducted for subjects who can be assessed by caregivers. Subjects will designate a caregiver involved in the assessment. Subjects are allowed to designate several caregivers but it is preferable to conduct the assessment by the same caregiver as much as possible. Caregivers who are designated as the rater will fill in the Zarit Caregiver Burden Interview (Assessment of Caregivers' Burden), and place it in an envelope to keep it out of the subject's sight, and submit it to the investigator.
5. Target sample size and study period
5.1. Target sample size and sample size calculation
Twenty subjects for official registration (15 subjects for the active drug group and 5 subjects for the placebo group). Up to 24 subjects (18 subjects for the active drug group and 6 subjects for the placebo group) can be registered. The target number of subjects enrolled in this study was set at 20, taking feasibility into consideration. Considering the seriousness of the disease, the ratio of subjects treated with the active drug and placebo is 3:1 (15 subjects:5 subjects). A summary of biostatistical considerations related to the safety assessment for the design of this study is shown below. In this study, the sample size of the placebo group is limited because of ethical considerations, and a comparison between the active drug group and the control group will therefore be made in an explorative manner, and statistical assessment will be conducted mainly for each treatment group. As for the safety assessment, the primary objective of this study, if any clinically significant AEs occur with an incidence of approximately 10% in the active drug group, the scale of this study is enough to detect such an AE with an 80% probability. In other words, clinically significant AEs with relatively low incidences can be detected with a certain probability in this study. As for the efficacy assessment, the secondary objective of this study, the change from Day 1 in the ALSFRS-R score during the 24-week double-blind period (exacerbation of symptoms) will be assessed as the primary endpoint. In two past confirmatory studies of edaravone in ALS patients [10], [26], the weighted mean change in the ALSFRS-R score at Week 24 in the placebo group (n = 99 and n = 66) was −6.8 points. Assuming that the true value of the change in ALSFRS-R score and its standard deviation (SD) in the active drug group are −5.5 points, which is similar to the value in the edaravone group, and 6 points, respectively, the probability that the point estimate of the mean change in the active drug group does not exceed the threshold (−6.8 points) is 80% with a sample size of 15 subjects in the active drug group. The efficacy will be exploratively assessed using the point estimate of the mean score and information to plan a next-phase clinical study will be collected.
5.2. Study period
November 2018 to March 2021
6. Study drug
6.1. Name of study drug
-
(1)Test Drug
- Name: SK & F101468-A
- Generic name: Ropinirole hydrochloride
- Dosage form and strength:
- SK & F101468-A 2 mg: Each tablet contains 2 mg of ropinirole.
- SK & F101468-A 8 mg: Each tablet contains 8 mg of ropinirole.
-
(2)Comparator
- Name: SK & F101468-A placebo
- Dosage form and strength:
- SK & F101468-A 2 mg placebo:
- Tablets do not contain ropinirole and are indistinguishable from the SK & F101468-A 2 mg tablet.
- SK & F101468-A 8 mg placebo:
- Tablets do not contain ropinirole and are indistinguishable from the SK & F101468-A 8 mg tablet.
6.2. Packaging and labeling of the study drug
-
(1)
Packaging
Seven tablets of the study drug will be packaged in a press-through package (PTP) sheet, and 20 PTP sheets will then be packed in a small box.
-
(2)
Labeling
The study drug labeling contains information including a statement of “For clinical study use,” study drug code, manufacturing number, storage method, expiratory date, and name, affiliation, title, and address of the sponsor-investigator.
6.3. Storage method
The study drug should be stored at room temperature.
6.4. Methods of study drug handling, storage, and management
The study drug manager will store and manage the study drug in accordance with the “Procedure for Study Drug Management” prepared by the sponsor-investigator. The study drug manager will dispose of unused study drugs after the end of the study.
Use the study drug is not allowed for purposes other than this study (another clinical study, animal studies, basic experiments, etc.).
6.5. Emergency code breaking
If it becomes necessary to urgently identify the study drug for a subject for his/her treatment and safety assurance, the investigator may request the study drug randomization manager to break the emergency code. The detailed procedure for emergency code breaking will be specified in the procedural document separately prepared.
7. Treatments administered to subjects
7.1. Preparation of the subject screening list
The investigator will prepare a subject screening list, list all subjects who have received an explanation for informed consent, and assign subject identification (ID) codes to subjects who have provided informed consent.
The investigator will manage the registration numbers and other information pertaining to the registered subjects (including those who discontinue or suspend treatment).
7.2. Registration of subjects
-
(1)
Informed consent to interim registration
The investigator will perform the tests/examinations that are required to assess the eligibility of subjects during the screening period after obtaining informed consent. The investigator will confirm that the subjects satisfy the inclusion and exclusion criteria upon interim registration, and fill in the items that are required for interim registration in the EDC system. Interim registration will take place within 28 days of obtaining informed consent.
-
(2)
Official registration
The investigator will perform the tests/examinations and observations for the run-in period that are required for official registration, confirm that the subjects satisfy the inclusion and exclusion criteria upon official registration, and fill in the items that are required for official registration in the EDC system. After official registration, the registration number will be automatically assigned by the EDC system. The investigator will confirm that official registration has been completed, then prescribe the study drug. Study treatment will be started within 15 days after official registration.
7.3. Dose and dosage regimen
-
(1)
Criteria for administration
[At the time of the first dose]
The study drug will be administered if all of the following conditions are satisfied.
-
1)
Events corresponding to Grade ≥3 of the “Criteria for Seriousness Classification of ADRs, etc. [Notification No. 80 of the Safety Division, Pharmaceutical Affairs Bureau (PAB), dated June 29, 1992]” are not observed in the assessment of the test/examination and observation items, general conditions, and vital signs on the day of administration.
-
2)
There is no concern about administration in the assessment of the test/examination and observation items, general conditions, and vital signs on the day of administration.
-
(2)
Criteria for dose adjustment of the study drug
Study treatment will be started at a dose of 2 mg once daily, followed by increases in weekly increments of 2 mg (to a maximum of 16 mg) (Table 3). If side effects (drowsiness, vertigo, dizziness, etc.) that can be objectively tolerated but interfere with ADL appear, the same dose will be maintained at the discretion of the investigator, or will be reduced every week until the side effects disappear, with maintenance doses being administered in an amount without the side effects. If the dosage is reduced to 2 mg and the side effects that are objectively acceptable but impair ADL are not alleviated, the drug will be discontinued.
7.4. Proceeding to the continued treatment period
7.4.1. Criteria for continued treatment
Subjects who have completed the double-blind period and are willing to receive continued treatment can proceed to the open-label continued active drug treatment period after the double-blind period.
Subjects who satisfy all of the following criteria are eligible for proceeding to the continued treatment period.
-
(1)
Subjects are voluntarily willing to receive continued treatment.
-
(2)
Subjects do not meet any of the criteria listed in “12.1 Discontinuation Criteria for Subjects.”
-
(3)
Subjects can receive study treatment for at least 4 weeks after proceeding to the continued treatment period.
-
(4)
Subjects can proceed to the continued treatment period in the judgment of the investigator.
7.4.2. Method of proceeding to the continued treatment period
-
(1)
The investigator will explain the details of the continued treatment period to subjects who satisfy “7.4.1 Criteria for Continued Treatment” by Week 24 of the double-blind period, confirm their willingness, and obtain their written informed consent.
-
(2)
When proceeding to the continued treatment period, the dose of the study drug will be tapered to 2 mg (it will take 3 weeks in the case of reducing the dose from the maximum of 16 mg) for both the active drug and placebo groups in accordance with the Study Drug Tapering Protocol (Table 4) to maintain the blindness. Subsequently, treatment will be started, followed by increases in the dose to a maximum of 16 mg in accordance with the Study Drug Titration Protocol (Table 3). The period of open-label treatment with the active drug will be extended within the range of a maximum of 48 weeks from the first dose of study treatment. In the continued treatment period, subjects who have been assigned to receive placebo in the double-blind period will be exposed to the active drug and may thus be at a risk for developing AEs. The subjects should therefore be adequately explained this matter before the start of treatment.
7.5. Duration of treatment
24–50 weeks (including the tapering period)
-
•
Double-blind period: 24 weeks
-
•
Tapering treatment period: 0–2 weeks
-
•
Continued treatment period (for subjects willing to receive continued treatment): 4–22 weeks
-
•
Tapering treatment period (for subjects proceeding to the continued treatment period): 0–2 weeks
7.6. Prohibited and restricted concomitant drugs
7.6.1. Prohibited concomitant drugs
Concomitant use of CYP1A2 inhibitors (cimetidine, fluvoxamine, etc.), edaravone, and high-dose methylcobalamin (25 mg or 50 mg) is prohibited, regardless of dose and treatment regimen, during the period from interim registration to the end of the study (to the end of continued treatment for subjects who receive continued treatment) or to the time of discontinuation. Although edaravone is an important therapeutic choice for ALS patients, daily administration of edaravone in Keio University Hospital is practically difficult because visiting our hospital every day will be a big burden on the subjects who are living in distant regions of Japan. Edaravone can be administered in local clinics or hospitals, however we think that 1) the efficacy of ropinirole hydrochloride (the secondary outcome of this trial) might be obscured by edaravone because it works as a ROS scavenger, which is one of the possible underlying mechanisms of ropinirole hydrochloride as well, 2) management of participants is by a single institution, Keio University Hospital, is preferable. Thus, we explain these reasons very carefully and obtain informed consent from only patients who are not receiving edaravone, excluding patients who want to continue edaravone treatment.
7.6.2. Restricted concomitant drugs
Concomitant use of riluzole (brand name: Rilutek Tablets 50 mg or Riluzole Tablets 50 mg “AA”) is allowed during the period from obtaining informed consent to the end of the study (to the end of continued treatment for subjects who receive continued treatment) or to the time of discontinuation. Subjects who are not receiving riluzole before providing informed consent are not allowed to start treatment with riluzole after providing informed consent. Use of riluzole is not a requirement.
7.6.3. Descriptions of concomitant drugs and therapies
The investigator or the study collaborator will enter the following information on concomitant drugs and therapies used during the period from obtaining informed consent to the end of the follow-up period or the time of discontinuation into the concomitant drug and therapy pages of the EDC system.
-
(1)
Concomitant drugs: name of drug, daily dose, delivery route, duration of treatment, and purpose of use
-
(2)
Concomitant therapies: name/content of therapy, duration of use, and purpose of use
7.7. Management of subjects
-
(1)
Instructions for administration
The investigator, the study collaborator, or the study drug manager (or the person in charge) will provide subjects with instructions for administration, keeping the following in mind.
-
1)
Subjects must take the drug as instructed by the physician.
-
2)
Subjects must bring unused drugs (including spare drugs) and empty PTP sheets at the subsequent visit.
-
(2)
Instructions for lifestyle
The investigator or the study collaborator will provide subjects with instructions for lifestyle, keeping the following in mind.
-
1)
Subjects must undergo the medical examination and other tests/examinations on the designated days. When the subject cannot make a visit on the scheduled day, he/she must contact the investigator and seek his/her instructions.
-
2)
Subjects must bring the Clinical Study Participation Card with them and present it when receiving a medical attention at another hospital or at other departments of this hospital. Subjects who are using drugs prescribed by doctors other than the investigator of this study or drugs purchased at pharmacies are required to inform the investigator or the study collaborator. Subjects who start using an additional drug during the study are also required to contact the investigator or the study collaborator before beginning use.
-
3)
Subjects must try not to modify their lifestyle (daily exercise, meals, etc.) as much as possible.
-
4)
Subjects must contact study staff if they have an abnormal condition in their body.
-
5)
Subjects must use an effective form of birth control (e.g., condom, pill, diaphragm, intrauterine devices (IUD), implantable contraceptives, spermicide) during the study period if they are sexually active.
-
6)
Subjects must not engage in potentially hazardous activities, including car driving, machine operation, or working in a high place.
-
(3)
Instructions on how to fill in the dosing diary
The investigator or the study collaborator will distribute a rainy weather information form at the start of the run-in period and a dosing diary at the start of study treatment to the subjects. At this time, the investigator will explain how to fill in the diary and instruct them to fill in the diary every day during the run-in period and the study drug treatment period. The investigator will also instruct them to describe rainy weather information.
In addition, if the upper limb function of the subjects deteriorates and the description becomes difficult, substitutes can write for the subjects. In the case of an allograph, the investigator or the study collaborator will instruct the subjects to identify the where the entry was written and write the name of substitutes and relationship with the subjects in the margin of the dosing diary.
-
(4)
Contacting another attending doctor by subjects
The investigator will check whether the subject is receiving medical attention other than that in this study. If the subject is receiving medical attention from another physician, the investigator will contact the relevant physician, with the subject's consent, to inform the physician that the subject is participating in the study. In addition, the investigator or the study collaborator will issue the Clinical Study Participation Card etc. to the subjects and instruct them to present it at another hospital or at other departments of this hospital to inform other physicians that he/she is participating in the study.
8. Tests/examinations and observations
8.1. Test/examination and observation items and time points
8.1.1. Subject characteristics
The following subject characteristics will be investigated during the screening period.
Age (date of birth), date of informed consent, gender, race, and presence or absence of allergies (drug, food, and others)
8.1.2. Medical history and concomitant diseases
Medical history of diseases (previous diseases, including history of surgery, in the past 5 years, in principle; a definite time frame will not be established for the history of cancers and other diseases that may affect the assessment in this study in the judgment of the investigator etc.) and concomitant diseases will be investigated at 12 weeks after interim registration.
Events that occur during the investigation, at 12 weeks after interim registration to the day preceding the first dose of study treatment, will be handled as follows:
-
11)
Events that have resolved before the day of the first dose of study treatment: handled as previous diseases
-
12)
Events that persist on the day of the first dose of study treatment: handled as concomitant diseases
8.1.3. Investigations of concomitant drugs and therapies
Concomitant drugs and therapies that are used during the period from obtaining informed consent to the end or discontinuation of observation will be investigated for the following items.
-
(1)
Concomitant drugs: name of drug, dose, delivery route, start date, end date, and reason for use
-
(2)
Concomitant therapies: name/content of therapy, start date, end date, and reason for use
8.1.4. Investigation of the primary disease
The primary disease will be investigated for the following items during the screening period.
Classification of ALS (sporadic, familial), previous treatment, time of onset, criteria for the diagnosis of ALS (El Escorial revised, World Congress of Neurosurgery), ALS Severity Classification (Specific Disease Research Survey, Ministry of Health, Labour and Welfare, January 1, 2007), family history (second-degree relatives), and initial symptoms (bulbar paralysis, upper limb symptoms, lower limb symptoms, respiratory muscle paralysis)
8.1.5. Height
Height will be measured during the screening period.
8.1.6. Body weight
Body weight will be measured during the screening period, at 12 weeks after interim registration, before the start of the first dose of the study treatment (from 3 days before to the day of the first dose), before study drug administration at Weeks 5, 9, 13, 17, 21, and 24 after the start of study treatment, and at the time of discontinuation (when possible).
For subjects who proceed to the continued treatment period, body weight will be measured before study drug administration at each of the following time points, in addition to the above time points. Measurement will also be conducted, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Weeks 27, 31, 35, 39, 43, and 46 after the start of study treatment, or the time of termination
- [Dose at the end of the double-blind period: 6 mg]
- Weeks 26, 28, 32, 36, 40, 44, and 47 after the start of study treatment, or the time of termination
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Weeks 27, 29, 33, 37, 41, 45, and 48 after the start of study treatment, or the time of termination
8.1.7. Study treatment compliance
Study treatment compliance will be investigated for the following items by checking the dosing dairy filled out by the subjects during the treatment period.
Date of administration, dose, and time of the final administration before each visit day
8.1.8. General conditions
General conditions (physical findings) will be examined during the period from the start of the screening period to the end or discontinuation of observation.
8.1.9. Vital signs
-
(1)
Blood pressure, body temperature, and pulse rate
Measurement will be performed under the same conditions throughout the study period.
Blood pressure, body temperature, and pulse rate will be measured during the screening period, at 12 weeks after interim registration, before the start of the first dose of the study treatment (3 days before to the day of the first dose), the day following the first dose of the study treatment, before study drug administration at Weeks 2, 3, 5, 9, 13, 17, 21, and 24 after the start of study treatment, during the follow-up period, and at the time of discontinuation (when possible).
For subjects who proceed to the continued treatment period, blood pressure, body temperature, and pulse rate will be measured before study drug administration at each of the following time points, in addition to the above time points and during the follow-up period. Measurement will also be conducted, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Weeks 26, 27, 31, 35, 39, 43, and 46 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 6 mg]
- Weeks 26, 27, 28, 32, 36, 40, 44, and 47 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Weeks 27, 28, 29, 33, 37, 41, 45, and 48 after the start of the study treatment, or the time of termination
-
(2)
Respiratory rate
Measurement will be performed under the same conditions throughout the study period.
Respiratory rate will be measured during the screening period, at 12 weeks after interim registration, before the start of the first dose of the study treatment (3 days before to the day of the first dose), the day following the first dose of the study treatment, before study drug administration at Weeks 5, 9, 13, 17, 21, and 24 after the start of study treatment, during the follow-up period, and at the time of discontinuation (when possible).
For subjects who proceed to the continued treatment period, respiratory rate will be measured before the study drug administration at each of the following time points, in addition to the above time points and during the follow-up period. Measurement will also be conducted, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Weeks 26, 27, 31, 35, 39, 43, and 46 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 6 mg]
- Weeks 26, 27, 28, 32, 36, 40, 44, and 47 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Weeks 27, 28, 29, 33, 37, 41, 45, and 48 after the start of the study treatment, or the time of termination
8.1.10. Twelve-lead electrocardiography
Twelve-lead electrocardiography (ECG) will be performed during the screening period, at 12 weeks after interim registration, before study drug administration at Week 24 after the start of the study treatment, and at the time of discontinuation (when possible).
For subjects who proceed to the continued treatment period, 12-lead ECG will be performed before study drug administration at each of the following time points, in addition to the above time points. Measurement will also be conducted, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Week 46 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 6 mg]
- Weeks 26 and 47 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Weeks 27 and 48 after the start of the study treatment, or the time of termination
8.1.11. Screening for infections
Screening for infections will be performed using serum samples during the screening period and at 12 weeks after interim registration.
HTLV-1 antibody test, HIV antibody test, HBs antigen test, HCV antibody test, and TPHA (only during the screening period)
8.1.12. Conventional laboratory tests
Blood and urine samples will be collected during the screening period, at 12 weeks after interim registration, the day following the first dose of the study treatment, before study drug administration at Weeks 5, 9, 13, 17, 21, and 24 after the start of study treatment, at the follow-up period and at the time of discontinuation (when possible).
For subjects who proceed to the continued treatment period, blood and urine samples will be collected before study drug administration at each of the following time points and at the follow-up period, in addition to the above time points. Blood and urine samples will also be collected, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Weeks 27, 31, 35, 39, 43, and 46 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 6 mg]
- Weeks 28, 32, 36, 40, 44, and 47 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Weeks 29, 33, 37, 41, 45, and 48 after the start of the study treatment, or the time of termination
[Tests]
-
(1)
Blood biochemistry (under fasting conditions)
Total protein, albumin, BUN, uric acid, total cholesterol, triglyceride, HDL cholesterol, LDL cholesterol, creatinine, total bilirubin, direct bilirubin, AST (GOT), ALT (GPT), alkaline phosphatase (ALP), LDH, amylase, CPK (CK), Na, K, Cl, Ca, Mg, CRP, blood glucose, hemoglobin Alc (only during the screening period)
-
(2)
Hematology
White blood cell (WBC) count, red blood cell (RBC) count, hemoglobin, hematocrit, platelet count, morphology, international normalized ratio of prothrombin time (PT-INR), activated partial thromboplastin time (APTT), and fibrinogen
-
(3)
Urinalysis
pH, specific gravity, protein, glucose, ketone body, occult blood, urobilinogen
8.1.13. Specific laboratory tests
Blood samples will be collected before the start of the first dose of the study treatment (3 days before to the day of the first dose), before study drug administration at Week 24 after the start of study treatment, and at the time of discontinuation (when possible).
For subjects who proceed to the continued treatment period, blood samples will be collected before study drug administration at the following time points, in addition to the above time points. Blood samples will also be collected, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Week 46 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 6 mg]
- Week 47 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Week 48 after the start of the study treatment, or the time of termination
[Tests]
-
(1)
Blood biochemistry: four fractions of fatty acids
-
(2)
Urinalysis: 8-OHdG (CRE-corrected)
8.1.14. Blood ropinirole concentrations
Blood samples will be collected at 12 weeks after interim registration, Week 2 after the start of the study treatment, visits in the week following a dose increase, before study drug administration at Weeks 13 and 24, and the time of discontinuation (when possible).
For subjects who proceed to the continued treatment period, blood samples will be collected before study drug administration in the week following a dose increase after the start of study treatment and at each of the following time points, in addition to the above time points. Blood samples will also be collected, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Weeks 26, 35, and 46 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 6 mg]
- Weeks 27, 36, and 47 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Weeks 28, 37, and 48 after the start of the study treatment, or the time of termination
8.1.15. Pregnancy test (only for subjects of childbearing potential)
Subjects of childbearing potential will be tested for pregnancy by the urine human chorionic gonadotropin (HCG) test during the screening period. The presence of pregnancy will also be confirmed by the serum HCG test at 12 weeks after interim registration. The presence of pregnancy will be further confirmed by the urine HCG test at the time of discontinuation (when possible).
For subjects of childbearing potential who do not proceed to the continued treatment period, the urine HCG test will be performed at Week 24, in addition to the above time points.
For subjects of childbearing potential who proceed to the continued treatment period, the urine HCG test will be performed at the following time points, in addition to the above time points. The test will also be performed, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Week 46 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 6 mg]
- Week 47 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Week 48 after the start of the study treatment, or the time of termination
Both urine and serum HCG tests that are specific for the beta subunit (HCG-β) will be used in this study. A pregnancy test is not required for men, surgically sterile women, hysterectomized or bilaterally ovariectomized women, and women with at least 1 year elapsing after their last menstruation because the possibility of pregnancy can be ruled out in these subjects.
8.1.16. Cerebrospinal fluid (CSF) test
The CSF test will be performed using lumbar puncture before the start of the first dose of the study treatment (3 days before to the day of the first dose), before study drug administration at Week 24 after the start of the study treatment, and at the time of discontinuation (when possible).
For subjects who proceed to the continued treatment period, the CSF test will be performed before study drug administration at each of the following time points, in addition to the above time points. The test will also be performed, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Week 46 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 6 mg]
- Week 47 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Week 48 after the start of the study treatment, or the time of termination
[Tests]
CSF pressure, appearance, cell count, quantitative protein, albumin, quantitative glucose, LDH, Cl, IgG, CRP, hypersensitive CRP and 8-OHdG
8.1.17. Ropinirole concentration in CSF
CSF samples will be collected using lumbar puncture before the start of the first dose of study treatment (3 days before to the day of the first dose), before study drug administration at Week 24 after the start of the study treatment, and at the time of discontinuation (when possible).
For subjects who proceed to the continued treatment period, spinal fluid samples will be collected before study drug administration at each of the following time points, in addition to the above time points. CSF samples will also be collected, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Week 46 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 6 mg]
- Week 47 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Week 48 after the start of the study treatment, or the time of termination
8.1.18. ALS Functional Rating Scale-Revised
Assessment by ALSFRS-R will be conducted during the screening period (within 7 days before interim registration), at 4, 8, and 12 weeks after interim registration, before the start of the first dose of study treatment (3 days before to the day of the first dose), before study drug administration at Weeks 5, 9, 13, 17, 21, and 24 after the start of treatment, and at the time of discontinuation (when possible).
For subjects who proceed to the continued treatment period, the assessment by ALSFRS-R will be conducted before study drug administration at each of the following time points, in addition to the above time points. The assessment will also be conducted, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Weeks 27, 31, 35, 39, 43, and 46 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 6 mg]
- Weeks 26, 28, 32 36, 40, 44, and 47 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Weeks 27, 29, 33, 37, 41, 45, and 48 after the start of the study treatment, or the time of termination
8.1.19. Amyotrophic lateral sclerosis severity classification
Assessment by ALS severity classification (by the Research Committee for CNS Degenerative Diseases, Ministry of Health, Labour and Welfare, Japan) will be conducted during the screening period, at 12 weeks after interim registration, before the start of the first dose of study treatment (3 days before to the day of the first dose), before study drug administration at Weeks 5, 9, 13, 17, 21, and 24 after the start of treatment, and at the time of discontinuation (when possible).
For subjects who proceed to the continued treatment period, the assessment by ALS severity classification will be conducted before study drug administration at each of the following time points, in addition to the above time points. The assessment will also be conducted, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Weeks 27, 31, 35, 39, 43, and 46 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 6 mg]
- Weeks 26, 28, 32 36, 40, 44, and 47 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Weeks 27, 29, 33, 37, 41, 45, and 48 after the start of the study treatment, or the time of termination
8.1.20. Simple respiratory function test (FEV1, FEV6)
The simple respiratory function test will be performed during the screening period, at 12 weeks after interim registration, before the start of the first dose of study treatment (3 days before to the day of the first dose), before study drug administration at Weeks 5, 9, 13, 17, 21, and 24 after the start of treatment, and at the time of discontinuation (when possible).
For subjects who proceed to the continued treatment period, the simple respiratory function test will be performed before study drug administration at each of the following time points, in addition to the above time points. The test will also be performed, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Weeks 27, 31, 35, 39, 43, and 46 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 6 mg]
- Weeks 26, 28, 32 36, 40, 44, and 47 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Weeks 27, 29, 33, 37, 41, 45, and 48 after the start of the study treatment, or the time of termination
8.1.21. Detailed respiratory function test (VC, %FVC, FEV1%)
The detailed respiratory function test will be conducted during the screening period, at 12 weeks after interim registration, before study drug administration at Weeks 13 and 24 after the start of treatment, and at the time of discontinuation (when possible).
For subjects who proceed to the continued treatment period, the detailed respiratory function test will be performed before study drug administration at each of the following time points, in addition to the above time points. The test will also be performed, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Weeks 35 and 46 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 6 mg]
- Weeks 26, 36, and 47 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Weeks 27, 37, and 48 after the start of the study treatment, or the time of termination
Blood gas analysis (PaCO2, PaO2, pH, and HCO3-) will be performed if %FVC is 50% or less after the start of the run-in period.
In addition, the following formula will be used for the "forced vital capacity prediction value" for calculating % FVC.
-
-
Male: forced vital capacity prediction value (mL) = (0.042 × height (cm)-0.024 × age (as of day of implementation)−1.785) × 1000
-
-
Female: forced vital capacity prediction value (mL) = (0.031 × height (cm)-0.019 × age (as of day of implementation)−1.105) × 1000
(Reference: Respiration 33, No. 10 (2014) "Spirometry・flow volume curve")
8.1.22. Amyotrophic Lateral Sclerosis Assessment Questionnaire-40
Assessment by ALSAQ0 [10], [27], [28] will be conducted at 12 weeks after interim registration, before the start of the first dose of study treatment (3 days before to the day of the first dose), before study drug administration at Weeks 5, 9, 13, 17, 21, and 24 after the start of treatment, and at the time of discontinuation (when possible).
For subjects who proceed to the continued treatment period, the assessment by ALSAQ-40 will be conducted before study drug administration at each of the following time points, in addition to the above time points. The assessment will also be conducted, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Weeks 27, 31, 35, 39, 43, and 46 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 6 mg]
- Weeks 26, 28, 32, 36, 40, 44, and 47 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Weeks 27, 29, 33, 37, 41, 45, and 48 after the start of the study treatment, or the time of termination
8.1.23. Neurological assessment and quantitative muscle strength measurement
Muscle strength will be quantitatively determined using an instrument for measuring muscle strength [29]. Neurological assessment will be conducted at 12 weeks after interim registration, before study drug administration at Weeks 5, 9, 13, 17, 21, and 24 after the start of the study treatment, and at the time of discontinuation (when possible).
For subjects who proceed to the continued treatment period, the neurological assessment will be conducted before study drug administration at each of the following time points, in addition to the above time points. The assessment will also be conducted, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Weeks 27, 31, 35, 39, 43, and 46 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 6 mg]
- Weeks 26, 28, 32, 36, 40, 44, and 47 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Weeks 27, 29, 33, 37, 41, 45, and 48 after the start of the study treatment, or the time of termination
8.1.24. Modified Norris Scale (Bulbar symptom score)/tongue pressure measurement
Tongue pressure will be quantitatively determined using an instrument for measuring tongue pressure in addition to the Modified Norris Scale (bulbar symptom score) [30], [31]. Assessment by the Modified Norris Scale (bulbar symptom score) will be conducted during the screening period, at 12 weeks after interim registration, before study drug administration at Weeks 5, 9, 13, 17, 21, and 24 after the start of treatment, and at the time of discontinuation (when possible).
For subjects who proceed to the continued treatment period, the assessment by the Modified Norris Scale (bulbar symptom score) will be conducted before study drug administration at each of the following time points, in addition to the above time points. The assessment will also be conducted, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Weeks 27, 31, 35, 39, 43, and 46 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 6 mg]
- Weeks 26, 28, 32, 36, 40, 44, and 47 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Weeks 27, 29, 33, 37, 41, 45, and 48 after the start of the study treatment, or the time of termination
8.1.25. Amount of physical activity and number of steps
The amount of physical activity and the number of steps in daily living will be quantitatively determined using the Active style Pro manufactured and distributed by OMRON Corporation [32]. Prior to the assessment, the rater will check the rainy weather information form and the dosing diary filled out by subjects. The data will be confirmed at 4, 8, and 12 weeks after interim registration, before study drug administration at Weeks 5, 9, 13, 17, 21, and 24 after the start of study treatment, during the follow-up period, and at the time of discontinuation (when possible).
For subjects who proceed to the continued treatment period, the data will be confirmed before study drug administration at each of the following time points and during the follow-up period, in addition to the above time points. The data will also be confirmed, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Weeks 27, 31, 35, 39, 43, and 46 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 6 mg]
- Weeks 26, 28, 32, 36, 40, 44, and 47 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Weeks 27, 29, 33, 37, 41, 45, and 48 after the start of the study treatment, or the time of termination
8.1.26. Confirmation of death, inability of independent ambulation, loss of unilateral upper limb function, tracheostomy, respiratory support, tube feeding, and loss of vocal conversation, inability to take oral medications
Whether any of the defined events are present will be confirmed before the start of the first dose of study treatment (3 days before to the day of the first dose), and during the period from the day of the first dose to the end of observation or the time of discontinuation.
Loss of unilateral upper limb function, respiratory support, tube feeding, loss of vocal conversation and inability to take oral medications are defined as the conditions shown below.
-
(1)
Loss of unilateral upper limb function: a condition where the subject is unable to grip a pen in one hand, as a guide.
-
(2)
Respiratory support: noninvasive respiratory support during all-day hours (generally, at least 22 h except for meal hours) or invasive respiratory support.
-
(3)
A condition where “Swallowing” on ALSFRS-R is scored 0 points: “nothing by mouth (NPO); exclusively parenteral or enteral feeding.”
-
(4)
Loss of vocal conversation: barely able to speak to express emotions or unable to speak.
-
(5)
Inability to take oral medications: the subject's condition deteriorates for reasons other than (1) to (3) and oral administration becomes impossible.
8.1.27. Skeletal muscle computed tomography
Skeletal muscle CT scanning will be performed during the screening period, at Week 1 after the start of study treatment (3 days before the first dose to Day 7 after the start of treatment), before study drug administration at Week 24, and at the time of discontinuation (when possible).
8.1.28. Exploratory endpoints
-
(1)
Comparison of the in vitro drug effect evaluation and clinical effect using subjects' iPSC-derived neurons
Blood samples will be collected from subjects who have provided informed consent for iPSC production during the period from after interim registration to before the start of the first dose of study treatment (3 days before to the day of the first dose). Motor neurons will be induced in iPSCs produced from peripheral blood cells. The motor neurons will be analyzed for (1) confirmation that the ALS pathology has been represented; (2) assessment of disease improvement after treatment with ropinirole hydrochloride; (3) exploration of the action mechanism of ropinirole hydrochloride; and (4) comparison with clinical outcomes [19].
-
(2)Explorative search of new biomarkers for diagnosis, pathology, and drug effect evaluation
-
(6)Testing of TDP-43, NfL, etc. in blood and CSF
-
(6)
Blood samples will be collected before the start of the first dose of the investigational drug (3 days before the day of administration of the first dose) from 12 weeks after interim registration and at Weeks 13 and 24 after the start of the study treatment. CSF samples will also be collected before the start of the first dose of the investigational drug (3 days before the day of administration of the first dose) from 12 weeks after interim registration and at Week 24 after the start of the study treatment. Blood and CSF samples will be collected, when possible, at the time of discontinuation.
For subjects who proceed to the continued treatment period, blood and CSF samples will be collected at each of the following time points, in addition to the above time points. Blood and CSF samples will also be collected, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Weeks 35 (blood) and 46 after the start of the study treatment, or the time of termination (blood and CSF)
- [Dose at the end of the double-blind period: 6 mg]
- Weeks 36 (blood) and 47 after the start of the study treatment, or the time of termination (blood and CSF)
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Weeks 37 (blood) and 48 after the start of the study treatment, or the time of termination (blood and CSF)
-
(7)RNA expression analysis in blood and CSF
Blood samples will be collected from subjects who have provided informed consent for RNA expression analysis before the start of the first dose of the investigational drug (3 days before the day of administration of the first dose) from 12 weeks after interim registration and at Weeks 13 and 24 after the start of the study treatment. CSF samples will be collected before the start of the first dose of the investigational drug (3 days before the day of administration of first dose) from 12 weeks after interim registration and at Week 24 after the start of the study treatment. Blood and CSF samples will be collected, when possible, at the time of discontinuation.
For subjects who proceed to the continued treatment period, blood and CSF samples will be collected at each of the following time points, in addition to the above time points. Blood and CSF samples will also be collected, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Weeks 35 (blood) and 46 after the start of the study treatment, or the time of termination (blood and CSF)
- [Dose at the end of the double-blind period: 6 mg]
- Weeks 36 (blood) and 47 after the start of the study treatment, or the time of termination (blood and CSF)
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Weeks 37 (blood) and 48 after the start of the study treatment, or the time of termination (blood and CSF)
-
(3)
Examination of known familial ALS genes
Blood samples will be collected from subjects who have provided informed consent for the gene test at 12 weeks after interim registration.
-
(4)
Zarit Caregiver Burden Interview
Assessment by the Zarit Caregiver Burden Interview [24], [25] will be conducted for subjects who can be assessed by caregivers who have provided informed consent for the assessment at 12 weeks after interim registration, before the start of the first dose of the study treatment (3 days before to the day of the first dose), at Weeks 5, 9, 13, 17, 21, and 24 after the start of the study treatment, and at the time of discontinuation (when possible).
For subjects who proceed to the continued treatment period, the assessment by the Zarit Caregiver Burden Interview will be conducted at each of the following time points, in addition to the above time points. The assessment will be also conducted, when possible, at the time of discontinuation, even after the continued treatment period.
- [Dose at the end of the double-blind period: 2 mg–4 mg]
- Weeks 27, 31, 35, 39, 43, and 46 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 6 mg]
- Weeks 26, 28, 32, 36, 40, 44, and 47 after the start of the study treatment, or the time of termination
- [Dose at the end of the double-blind period: 8 mg–16 mg]
- Weeks 27, 29, 33, 37, 41, 45, and 48 after the start of the study treatment, or the time of termination
8.2. Adverse events
An AE is any unfavorable and unintended sign (including a laboratory abnormality), symptom, disease or disorder in a subject administered a study drug, whether it is related to the study drug or not. Over dosage and improper use of the study drug are also handed as AEs. Events that occur during the period from the day of the first dose of study treatment to the end of the follow-up period (within 28 days after the end of treatment) are handled as AEs.
The following events are not handled as AEs.
-
•
Weight loss, muscular weakness, arthralgia, myalgia, motor disorder, dyslalia, respiratory disorder, dysphagia, cognitive dysfunction, anxiety disorder, and depression symptoms, which are considered to be symptoms resulting from an exacerbation of the primary disease in the judgment of the investigator
-
•
Procedures performed only for the purpose of testing (e.g., endoscopy)
-
•
Modification of concomitant diseases that is considered to be within the predictable/foreseeable range by the investigator
-
•
Progression of the primary disease that is considered to be within the predictable/foreseeable range
-
•
Absence of any unfavorable medical occurrence (e.g., protocol-specified hospitalization, hospitalization already scheduled at the time of obtaining informed consent, hospitalization for non-medical but social reasons, hospitalization to enhance the convenience of visits for treatment/testing, etc.)
Changes in laboratory test values that meet any of the following are handled as AEs.
-
(1)
If any action for study treatment (cessation, discontinuation) becomes necessary owing to a change in laboratory test values
-
(2)
If use of any drug or procedure for treatment becomes necessary owing to a change in laboratory test values
-
(3)
If any surgical intervention has been introduced owing to a change in laboratory test values
-
(4)
If none of the above applies but the change in laboratory test values is an event of medical concern in the judgment of the investigator, etc.
8.2.1. Action taken for adverse events
If an AE occurs, the investigator should perform appropriate action(s) or treatment. Reported AEs should be followed until the following conditions are attained. AEs that are persisting at the scheduled end day of observation will be followed in the same manner.
-
•
The AE has resolved or is resolving (or stable)
-
•
In the case of sequela(e), the symptom has become fixed
-
•
The AE has been followed adequately and further follow-up is no longer necessary in the judgement of the investigator
The investigator etc. will enter the details of all the AEs reported, including the date of onset, severity, causal relationship with the study drug, presence/absence of treatment and, if any, the content, and outcome, in the EDC system.
The investigator may seek the opinion of the Independent Data Monitoring Committee about these AEs.
8.2.2. Definition of serious adverse events
A serious adverse event (SAE) is any of the reported AEs that: 1) results in death or is life-threatening, 2) requires inpatient hospitalization or prolongation of the existing hospitalization (except for protocol-specified hospitalization, hospitalization already scheduled at the time of obtaining informed consent, hospitalization for non-medical but social reasons, hospitalization to enhance the convenience of visits for treatment/testing, etc.), 3) results in disability/incapacity, 4) may result in disability/incapacity, 5) is serious according to the above (1) to (4), and 6) is a congenital anomaly/birth defect in the next generation.
8.2.3. Reporting of serious adverse events
If the information of an SAE that occurs during the period from the day of informed consent to the end of the follow-up period (within 28 days after the end of treatment) is obtained, the investigator will immediately report to the head of the study site and the study drug supplier. Upon receiving a request for provision of further necessary information from the study drug supplier, the head of the study site, or the IRB, the investigator should respond to this. If it becomes necessary to break the emergency code, the investigator will carry out code breaking in accordance with the procedural document. The investigator will report all SAEs to the Independent Data Monitoring Committee. If the relevant SAE needs to be reported immediately to the regulatory authorities, the investigator will report it within the timeframe specified by the regulatory authorities according to the content of the SAE.
8.2.4. Assessment of severity of adverse events
The investigator will assess the severity of all AEs as mild, moderate, or severe using a 3-grade rating scale based on the grades specified in the “Criteria for Seriousness Classification of ADRs, etc. [Notification No. 80 of the Safety Division, Pharmaceutical Affairs Bureau (PAB), dated June 29, 1992].”
For events that are not listed in the “Criteria for Seriousness Classification of ADRs, etc. [Notification No. 80 of the Safety Division, Pharmaceutical Affairs Bureau (PAB), dated June 29, 1992],” the investigator will determine the severity by referring to the following criteria.
1) Mild: easily tolerable without intervention, 2) Moderate: requires intervention but does not preclude post-treatment tests/examinations or observations, or 3) Severe: severely interferes with the activities of daily living (ADL).
If the severity of an AE changes during the study period, the highest grade observed during the period will be entered in the EDC system.
8.2.5. Assessment of causal relationship
The investigator will assess the causal relationship with the study drug for all AEs in accordance with the following categories.
-
•
Related: The AE resolves after discontinuation of treatment, the AE recurs after resumption of treatment, a statement that the AE could be related to the study drug is provided in the investigator's brochure, there is no confounding risk factor, the AE is consistent with the amount and/or duration of exposure, the potential relationship with concomitant disease(s), etc. is ruled out, etc.
-
•
Unrelated: The reasonable causal relationship between the study drug and the AE is unlikely.
8.2.6. Assessment of outcome
The outcome of AEs will be assessed on the following 6-grade rating scale.
1) Recovered, 2) Recovering, 3) Not recovered, 4) Recovered with sequelae, 5) Fatal, and 6) Unknown
8.2.7. Significant adverse events
Non-specific significant AEs are not defined in this study.
8.2.8. Action taken in the case of pregnancy
Investigators will explain at the start of the study that subjects should immediately inform the investigator if any sign of pregnancy is found due to a failure of birth control, e.g., delay in the period for female subjects or male subjects' partners. If a female subject or a male subject's partner is suspected of being pregnant, the investigator should not provide the study treatment until the potential pregnancy is ruled out based on a pregnancy test result. If a female subject or a male subject's partner is found to be pregnant, the investigator will discontinue the study for the relevant subject and identify the type of study drug by breaking the code of the study drug. If the drug administered to the subject is the active drug, the investigator will immediately report the matter in writing to the head of the study site and the study drug supplier. The investigator will follow the relevant subject until the completion of delivery or pregnancy. Pregnancy-related SAEs (miscarriage, abortion, birth defect/congenital anomaly) will be handled in accordance with the same procedures as those in “8.3.3 Reporting of Serious Adverse Events.”
9. Independent Data Monitoring Committee
The investigator may seek the opinion of the Independent Data Monitoring Committee about the study progress, and evaluation of safety data, as well as efficacy data, if necessary. Even in this case, the sponsor/investigator is responsible for the final decision-making. The responsibilities of the Independent Data Monitoring Committee are shown below.
9.1. Safety monitoring
-
(1)
The Committee will examine the details of SAEs reported in this study and conduct risk assessment for the study. The Committee will recommend whether to further continue the study and protocol revisions, including a change in the inclusion criteria to reduce the risk of AEs, as appropriate.
-
(2)
For SAEs that are difficult to differentiate from exacerbation of the primary disease among those related to the events defined as “death or a specified state of disease progression” assessed as a secondary endpoint, the risk of these events having been caused by the active drug will be assessed.
9.2. Monitoring of the implementation status of the study
Data related to the implementation status of the study will be monitored to guarantee the quality of this study. The data include the status of subject registration, validity of study subjects, status of withdrawals/dropouts, and protocol compliance status.
10. Risks and benefits for subjects
10.1. Risks
-
(1)
As with other dopamine receptor agonists, sudden onset of sleep and somnolence occurring in the ADL, e.g., when driving, have been reported in patients receiving this product or the ropinirole hydrochloride tablet. Some of these events were associated with accidents. In addition, some patients who experienced sudden onset of sleep had no warning symptoms, such as somnolence, beforehand or experienced such events for the first time after 1 or more years had elapsed from the start of treatment with this product.
-
(2)
Psychiatric symptoms such as hallucinations and delusions are considered to be associated with excessive dopamine receptor stimulation [33]. Treatment with dopamine receptor agonists, including this product, may potentially exacerbate these psychiatric symptoms.
-
(3)
Dopamine D2 receptor agonists, including this product, may cause a decrease in heart rate through inhibition of norepinephrine release from peripheral nerve endings [34].
-
(4)
In a study in UK, the pharmacokinetics of this product was compared in patients with Parkinson's disease who were divided into three age groups: <65 years, 65–75 years, and >75 years. Oral clearance (CL/F) decreased with increasing age, with a prolonged elimination half-life (T1/2) observed [35]. In a Japanese clinical study, the incidence of psychiatric symptoms, including hallucination, was reported to be higher in older adult patients (≥65 years) than in younger patients (<65 years).
10.2. Benefits
The therapeutic effect of this product for ALS has been confirmed in in vitro models. However, whether this product is effective in human patients with ALS will be exploratively assessed for the first time in this study. This study therefore does not guarantee the therapeutic effect of this product in treating ALS patients. Nevertheless, when considering that there is no truly effective established approach to the treatment of ALS at present, it is deemed quite meaningful to assess the safety, tolerability, and efficacy of this product.
11. Discontinuation criteria for subjects and the procedure
11.1. Discontinuation criteria for subjects
If any of the following apply, the study will be discontinued.
-
(1)
Subject's request for discontinuation of the study
-
(2)
Subject's withdrawal of consent
Subjects who withdraw informed consent for participation in the study while participating in the study will be handled as discontinued subjects.
-
(3)
Unable to start the first dose of the study drug.
-
(4)
Marked decrease in respiratory function
If any of the following apply, the study will be discontinued.
-
•
%FVC is ≤50% and PaCO2 in blood is ≥50 mmHg.
-
•
Tracheostomy is performed.
-
•
Noninvasive respiratory support is required during all-day hours (generally, at least 22 h except for meal hours) or invasive respiratory support becomes necessary.
-
(5)
Oral administration of the study drug becomes difficult owing to progression of dysphagia.
-
(6)
Unable to visit the hospital owing to progression of ALS.
This refers to the subject being unable to visit the hospital to receive the study drug and/or undergo observations due to his/her death or significant progression of disease.
-
(7)
Unable to visit the hospital twice in a row during the double-blind period or a total five times during the study.
These subjects are deemed inappropriate for efficacy assessment and are therefore handled as discontinued subjects.
If a similar situation occurs during the continued treatment period, the study for the subject should not be discontinued immediately; if the subject continues to be unable to visit the hospital, the investigator should then determine whether to continue the study for the subject.
-
(8)
If the study drug assigned to a subject is identified by emergency code breaking, the subsequent treatment of the subject should be discontinued.
-
(9)
Discontinuation based on the decision of the investigator etc.
If any of the following apply, the investigator etc. may discontinue the study.
-
1)
The investigator etc. determine that continued study is inappropriate as a result of safety assessment of the study drug based on subject's clinical symptoms, laboratory test values, vital signs, ECGs, etc.
-
2)
The investigator etc. determine that the subject is unable to comply with the protocol.
-
3)
The investigator determines that the subject is ineligible for the study because he/she is found not to satisfy the inclusion or exclusion criteria after interim or official registration, or for other reasons.
-
4)
Other circumstances in which the study should be discontinued in the judgment of the investigator etc.
Upon decision of discontinuation of the study, the investigator will provide the subject with an explanation about the discontinuation, reason for discontinuation, and required tests/examinations and treatment, etc. The investigator will then proceed with these tests/examinations, treatment, etc. This does not apply to cases where the subject withdraws consent for these tests/examinations etc.
11.2. Procedure for discontinuation
If the study for a subject is discontinued after the start of study treatment, the investigator will take appropriate measures for the relevant subject. The investigator will perform the tests/examinations and observations scheduled at the time of discontinuation, when possible. The assessment at the time of discontinuation will be performed within 12 weeks of discontinuation. Rapid dose reduction or discontinuation of this drug can cause malignant syndrome, such as high-grade fever, consciousness disturbance, hypermyotonia, dyskinesia, and shock. Therefore, the investigator should consider the condition of the subject at the time of discontinuation and determine the need for gradually tapering the dose. If the investigator performs gradual tapering, the “Drug Tapering Protocol (Table 4)” will be followed.
The investigator will enter information relevant to the discontinuation, including the date, reason, details, background information and action taken in the EDC system. If the study is discontinued because of AEs, the name of the AE leading to discontinuation will be entered in the discontinuation page of the EDC system. The date of discontinuation is defined as the day when assessment of discontinuation is performed; however, if the assessment of discontinuation cannot be conducted, the day of discontinuation is determined to be the date of discontinuation.
Subjects who have not undergone observations and tests/examinations scheduled at the time of discontinuation, or who have no visit scheduled after discontinuation, will be followed by letter (mailed) or phone to collect information on the reason, subsequent course, etc. The collected information will be entered in the discontinuation page of the EDC system.
The investigator or the study collaborator will make every effort to collect the dosing record of subjects who have no visit scheduled after discontinuation, by mail and other means.
12. Statistical analysis
Details of statistical analysis will be documented in the Statistical Analysis Plan prepared separately. The Statistical Analysis Plan will be finalized by the time of code breaking.
12.1. Analysis sets
12.1.1. Case handling
-
(1)
Efficacy
The following two analysis sets are defined in this study, and analysis will be performed in each analysis set.
-
1)
Full Analysis Set (FAS)
The full analysis set (FAS) is based on the intention-to-treat (ITT) principle. The FAS is a subset of all subjects enrolled in the study but excludes the subjects listed below.
-
•
Subjects in violation of the eligibility criteria (subjects who failed to satisfy major registration criteria for this study)
-
•
Subjects who have not received any dose of the study drug
-
•
Subjects who have no data at baseline or during the treatment period
-
•
Subjects who withdrew informed consent in the course of the study and refused the use of all of their data
-
2)
Per Protocol Set (PPS)
The per protocol set (PPS) is a subset of subjects who are included in the efficacy assessment according to the criteria for case handling prepared before data lock. For endpoints that are measured over time, the case and data inclusion/exclusion criteria will be prepared for each time point.
The FAS is the primary analysis set of efficacy assessment in this study. Statistical analysis in the PPS will be performed only on the change from baseline in ALSFRS-R score at Week 24, which is an important secondary endpoint.
-
(2)
Safety
The safety analysis set is the subset excluding the following subjects from all subjects included in this study.
-
-
Subjects who have not received any investigational drug
-
-
Subjects who have withdrawn consent during this study and refused the use of all of their data
12.1.2. Data handling
-
(1)
Imputation of missing data
Imputation of missing data will be performed for efficacy endpoints.
Details of the imputation method and items for imputation will be documented in the Statistical Analysis Plan separately prepared.
-
(2)
Case handling criteria
The case handling criteria will be determined before data lock.
12.2. Baseline patient characteristics
Summary statistics of patient characteristics (age, sex, body weight, etc.) and baseline characteristics will be calculated by treatment group.
12.3. Statistical analysis of efficacy
The change from baseline (Day 1) in ALSFRS-R score at Week 24 will be analyzed as an important secondary efficacy endpoint. Summary statistics of the measured value and the change from baseline, and the two-sided 95% confidence interval (CI) will be calculated by treatment group. A null hypothesis, that the change from baseline at each time point is 0, will be tested by treatment group using a one-sample t-test. The least squares mean will be compared between the treatment groups using contrasts by an analysis of covariance (ANCOVA) model with the baseline value as a covariate. The least squares mean difference and the two-sided 95% CI will be calculated.
For the secondary endpoints listed below, continuous data will be analyzed in the same manner as for the change in ALSFRS-R score. If a significant deviation is found in the distribution of dependent variables, a non-parametric approach will be used. For binary data, the point estimate of the ratio will be calculated by treatment group and the two-sided 95% CI for the ratio will be calculated using the Clopper Pearson method. The two-sided 95% CI for the difference in the ratio between the treatment groups will also be calculated using the normal approximation method. For survival time data, Kaplan–Meier plots will be generated and survival function will then be estimated.
The number and proportion of subjects for each maintenance dose (a maximum of 16 mg) will be summarized by treatment group.
Secondary endpoints
-
(1)
Ratio of change in ALSFRS-R score every 4 weeks between pre-treatment and post-treatment assessments.
-
(2)
Change in ALSFRS-R score during the 24-week double-blind period (from Day 1 to Week 24 of the double-blind period) (ΔALSFRS-R).
-
(3)
Change in ALSFRS-R score during the continued treatment period (from the assessment at the start to the final assessment of the continued treatment period) and during the overall treatment period (from Day 1 of the double-blind period to the final assessment of the continued treatment period) (ΔALSFRS-R).
-
(4)
CAFS score during the 24-week double-blind period (from Day 1 to Week 24 of the double-blind period), during the continued treatment period (from the assessment at the start to the final assessment of the continued treatment period), and during the overall treatment period (from Day 1 of the double-blind period to the final assessment of the continued treatment period).
-
(5)Composite endpoint as a sum of Z-transformed scores on the following items.
-
•ALSFRS-R subscore of each domain (bulbar function, limb function, and respiratory function)
-
•ALS severity classification
-
•Simple respiratory function test (FEV1, FEV6)
-
•Detailed respiratory function test (VC, %FVC, FEV1%)
-
•MMT score (limb and trunk muscles) and quantitative muscle strength
-
•Grip strength and pinch strength
-
•Modified Norris Scale (bulbar symptom score)
-
•Tongue pressure
-
•Body weight
-
•Amount of physical activity and number of steps
-
•Objective muscle mass determined using CT for skeletal muscle
-
•ALSAQ-40 score
-
•
-
(6)
Time to death or time to a specified state of disease progression (defined as any of death, inability to perform independent ambulation, loss of unilateral upper limb function, tracheostomy, respiratory support, tube feeding, loss of vocal conversation, and inability to take oral medications).
-
(7)
Time to %FVC of ≤50% (length of time until %FVC decreases to ≤50%).
-
(8)
Time to decrease of at least 6 points in ALSFRS-R score (change of at least a 6-point decrease in ALSFRS-R score [ΔALSFRS-R] from Day 1 of the double-blind period].
-
(9)
Proportion of patients who discontinue the treatment (discontinuation rate) during the period from Day 1 of the double-blind period to the final assessment of the continued treatment period.
Furthermore, analysis will be performed on the following exploratory endpoints: (1) comparison of the drug effect using motor neurons derived from patient's iPSCs and clinical effect, (2) explorative search of new biomarkers (changes in TDP-43 and NfL levels in blood and spinal fluid [change in RNA expression in blood and spinal fluid]) for diagnosis, pathology, and evaluation of drug effect, and (3) search of known FALS-related genes.
12.4. Statistical analysis of safety
12.4.1. Adverse events
The number of AEs and ADRs and the number of subjects with AEs and ADRs will be tabulated by treatment group and the two-sided 95% CI for the incidence will be calculated using the Clopper Pearson method.
12.4.2. Laboratory test values and vital signs
For continuous safety variables, summary statistics of the measured value at each time point and change from baseline, and two-sided 95% CI will be calculated by treatment group. For discrete variables, a cross table of data at baseline and each time point will be prepared.
12.5. Level of significance and multiplicity
All the analyses in this study will be performed at a two-sided 5% significance level and two-sided 95% confidence level. Efficacy analysis is the secondary objective, and adjustment for multiplicity of tests among the endpoints or time points will not be performed. For safety analysis, statistical power will be prioritized, and adjustment for multiplicity among the endpoints or time points will not be performed.
12.6. Primary analysis
Data will be locked after the end of the double-blind period of all the subjects but before the end of the continued treatment period of all the subjects, and will then be analyzed.
12.7. Deviations from originally planned statistical analyses
If any analysis is performed using a different method from that originally specified in the protocol, all changes should be reported in the clinical study report.
13. Quality control and assurance of the study
The sponsor-investigator must conduct “quality control of the study” and “quality assurance of the study” in accordance with the procedural document prepared separately to maintain the quality and reliability of the study. The study site must cooperate with the quality control and assurance of the study by the sponsor-investigator.
In the conduct of quality control of the study, the monitor will confirm that the study is conducted in accordance with the operating procedure for clinical studies prepared by the study site, the latest protocol, and GCP through direct access, as appropriate. The monitor will also confirm that descriptions in the CRF reported by the investigator are accurate and complete and that they are verifiable against study-related records including source documents.
To guarantee that the study is conducted in accordance with the protocol and GCP, an auditor will conduct audits in accordance with the procedural document and confirm that quality control is conducted appropriately.
The CROs for this trial are CTD Inc. and DOT WORLD Co., Ltd.
14. Ethics
14.1. Ethical conduct of the study
This study must be conducted in consideration of the ethical principles based on the Declaration of Helsinki, and in adherence to the Pharmaceutical and Medical Device Act (PMD Act), GCP, and standard protocols.
14.2. Institutional review board
The IRB of Keio University Hospital reviewed whether to conduct and continue the study from the standpoints of its ethical, scientific, and medical validity based on the descriptions in the investigator's brochure, protocol, informed consent document, and sample CRF, and approved this trial.
14.3. Confidentiality of subjects
The subject identification code will be used for subject registration and subject identification in the CRF. Personnel involved in this study must protect the confidentiality of subjects at times of direct access to source documents for study procedures, publication in medical journals, submission of materials to regulatory authorities, etc.
15. Retention of records etc.
-
(1)
Records etc. will be retained at the study site
The archiving manager designated by the head of the study site will retain those study-related documents and records that should be retained at the study site until the date defined in 1) or 2) below, whichever comes later. However, if the sponsor-investigator deems it necessary to retain them for a longer period, the study site will discuss the specific period and method of retention with the sponsor-investigator.
If it is decided that data related to the clinical study results collected in the study are not included in the application dossier, the study drug supplier should notify the head of the study site of the matter and the reason in writing.
-
1)
Date of marketing approval for the study drug (date of approval for partial changes in the approved items in the case of additional indications) (or the date when 3 years have passed since the notification that development of the drug is discontinued or if the clinical study results are not included in the application dossier)
-
2)
Date when 3 years have passed since discontinuation or completion of the study
If marketing approval for the study drug is obtained or discontinuation of development is decided due to a failure to obtain approval, the study drug supplier will notify the head of the study site of the matter in writing.
-
(2)
Records etc. retained by the sponsor-investigator (investigator)
The sponsor-investigator (investigator) will retain study-related documents and records that should be retained by the sponsor-investigator until the date defined in 1) or 2) below, whichever comes later. The sponsor-investigator (investigator) will discuss the response after the end of the retention period with the study drug supplier.
-
1)
Date of marketing approval for the study drug (or the date of approval for partial changes in the approved items in the case of additional indications) (date when 3 years have passed since the notification that development of the drug is discontinued or if the clinical study results are not included in the application dossier)
-
2)
Date when 3 years have passed since discontinuation or completion of the study
If marketing approval for the study drug is obtained or discontinuation of development is decided due to a failure to obtain approval, the study drug supplier will notify the head of the study site of the matter in writing.
16. Cost bearing for the study
16.1. Financial source and conflicts of interest
This study will be conducted under the sponsorship of the Japan Agency for Medical Research and Development (AMED) (JP 18ek0109329h0001) and K Pharma, Inc. As for the study drug, all test drugs and part of the comparator will be supplied free-of-charge by GlaxoSmithKline K.K. It will be determined at the Conflicts of Interest Management Committee of Keio University that these do not fall under the conflicts of interest acts.
17. Compensation for study-related health injuries
If a subject suffers any study-related health injury, the study site will provide the relevant subject with treatment and other necessary measures.
17.1. Medical care provision system
The investigator and the study site will organize sufficient systems that allow for provision of medical care for the treatment of ADRs of the study drug etc. and make every effort to provide the best possible treatment for relevant health injuries.
17.2. Purchase of insurance
The investigator shall purchase insurance to guarantee the execution of compensation for subject's health injuries and is responsible for compensation according to the regulations on clinical study insurance. The investigator (or subinvestigator) or the study collaborator will distribute written information for compensation to subjects when providing explanations about informed consent for participation in the study.
18. Study registration
This study was registered to the two databases listed below.
-
(1)
Database established by the National University Hospital Council of Japan (University hospital Medical Information Network [UMIN])
UMIN trial ID: UMIN000034954
-
(2)
Database established by The Japan Medical Association Center for Clinical Trials [JMACCT]
JMACCT-ID: JMA-IIA00397
19. Protocol compliance, deviation, or change
19.1. Protocol compliance
The investigator must comply with this protocol.
19.2. Protocol deviation or modification
The investigator must not deviate from the protocol or modify the protocol without written approval based on the IRB's prior review. However, the investigator is allowed to do this in unavoidable medical situations, including the case where such an action is required to avoid an urgent risk to the subject, without prior approval of the IRB.
In such a case, the investigator confirms that the content of and reason for deviation or modification and subsequent protocol revision are appropriate, and submit the draft to the head of the study site and the IRB as soon as possible to gain its approval. The agreement of the head of the study site is also required.
The investigator must record all protocol deviations. Only for protocol deviations that arise in unavoidable medical situations, including the case where such an action is required to avoid an urgent risk to subjects, the investigator will prepare a written document to explain the deviation and the reason, and immediately submit it to the head of the study site. The investigator (or sub-investigator) will retain a copy of the document.
The investigator will immediately submit the report on all changes in the study procedures that may significantly affect the conduct of the study or increase the risk to subjects to the head of the study site and the IRB.
20. Protocol revision
If it is deemed necessary to modify the protocol in the course of the study, the sponsor-investigator will revise the protocol. The sponsor-investigator will immediately notify the head of the study site of the content of the revision in writing, and obtain the IRB's approval through the head of the study site. If a revision of the protocol is announced from the head of the study site based on the IRB's opinion, the sponsor-investigator will decide whether the changes are valid and revise the protocol, if necessary. The sponsor-investigator will immediately notify the head of the study site of the content of the revision in writing, and obtain the IRB's approval through the head of the study site.
21. Ownership and publication of results
Intellectual property rights etc. arising from this study shall belong to the researchers. The researchers and drug suppliers shall use part or all of clinical study results for the purpose of application for marketing approval of the study drug. In doing this, the clinical study results are partially disclosed in accordance with applicable laws and regulations; however, each subject's personal information remains protected.
22. Conclusion
We believe that this study will be proof of concept for iPSC-drug discovery if ropinirole hydrochloride is effective in ALS patients. Patient recruitment began in Dec 2018 and the last patient is expected to complete the trial protocol in November 2020.
Declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of Keio University based on the Declaration of Helsinki. Written informed consent was obtained from the all participants of this trial.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Competing interests
K.F. is a President of K Pharma Inc. H.O. is a Scientific Advisory Board member of K Pharma Inc. All authors have no COIs with GlaxoSmithKline.
Funding
The basic study on the anti-ALS action of ropinirole hydrochloride was performed under the support of the Japan Agency for Medical Research and Development (AMED) (The Acceleration Program for Intractable Disease Research Utilizing Disease-specific iPS Cells to H.O. (Grant No. 19bm0804003h0003) and the Research on Practical Application of Innovative Pharmaceutical and Medical Devices for Rare and Intractable Diseases to H.O. (Grant No. JP 18ek0109395h0001, 19ek0109395h0002)). This clinical trial will be conducted under the sponsorship of AMED (Research on practical application of innovative pharmaceutical and medical devices for rare and intractable diseases to H.O. (Grant No. JP 18ek0109329h0001, 19ek0109329h0002)) and K Pharma, Inc. As for the study drug, all test drugs and part of the comparator will be supplied free-of-charge by GlaxoSmithKline K.K.
Authors' contributions
S.M. and S.T. were the Subinvestigators and wrote the protocol.
J.N. is the Principal Investigators for the trial.
K.F., H.S., N.S., M.A. contributed to the protocol.
H.O. contributed to the protocol and supervised the trial management.
All authors sit on the Trial Management Group.
All authors contributed to the manuscript.
All authors read and approved the final manuscript.
Acknowledgements
We gratefully thank Kentaro Higashi (Keio University Hospital, Clinical and Translational Research Center; primary project manager), Yuto Fujiki (Keio University Hospital, Clinical and Translational Research Center; secondary project manager), Takashi Kasama (Keio University Hospital, Clinical and Translational Research Center; translational research adviser), Yukiko Matsushima (Keio University Hospital, Clinical and Translational Research Center; data monitoring), Kazuo Watanabe (contract research organization), Yasunori Sato (Keio University Hospital, Clinical and Translational Research Center; statistical analysis), Takayuki Abe (Keio University Hospital, Clinical and Translational Research Center; statistical analysis), Masahiro Jinzaki (Keio University Hospital, Department of Radiology), and Akihisa Yamazaki (Keio University Hospital, Department of Radiology).
Footnotes
Peer review under responsibility of the Japanese Society for Regenerative Medicine.
Contributor Information
Satoru Morimoto, Email: s.morimoto.tmgh@gmail.com.
Shinichi Takahashi, Email: takashin@tka.att.ne.jp.
Komei Fukushima, Email: komeifukushima@z2.keio.jp.
Hideyuki Saya, Email: hsaya@a5.keio.jp.
Norihiro Suzuki, Email: nrsuzuki@keio.jp.
Masashi Aoki, Email: aokim@med.tohoku.ac.jp.
Hideyuki Okano, Email: hidokano@a2.keio.jp.
Jin Nakahara, Email: nakahara@a6.keio.jp.
References
- 1.Brown R.H., Al-Chalabi A. Amyotrophic lateral sclerosis. N Engl J Med. 2017, 13;377:162–172. doi: 10.1056/NEJMra1603471. [DOI] [PubMed] [Google Scholar]
- 2.Doi Y., Atsuta N., Sobue G., Morita M., Nakano I., for Research Committee of CNS Degenerative Diseases of Japan Prevalence and incidence of amyotrophic lateral sclerosis in Japan. J Epidemiol. 2014;24:494–499. doi: 10.2188/jea.JE20140059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bensimon G., Lacomblez L., Meininger V., the ALS/Riluzole Study Group A controlled trial of riluzole in amyotrophic lateral sclerosis. N Engl J Med. 1994;330:585–591. doi: 10.1056/NEJM199403033300901. [DOI] [PubMed] [Google Scholar]
- 4.Lacomblez L., Bensimon G., Leigh P.N., Guillet P., Meininger V. Doseranging study of riluzole in amyotrophic lateral sclerosis. Lancet. 1996;347:1425–1431. doi: 10.1016/s0140-6736(96)91680-3. [DOI] [PubMed] [Google Scholar]
- 5.Lacomblez L., Bensimon G., Leigh P.N., Guillet P., Powe L., Durrleman S. A confirmatory dose-ranging study of riluzole in ALS. ALS/Riluzole Study Group-II. Neurology. 1996;47(6 Suppl 4):S242–S250. doi: 10.1212/wnl.47.6_suppl_4.242s. [DOI] [PubMed] [Google Scholar]
- 6.Pongratz D., Neundörfer B., Fischer W. German open label trial of riluzole 50 mg b.i.d. in treatment of amyotrophic lateral sclerosis (ALS) J Neurol Sci. 2000;180:82–85. doi: 10.1016/s0022-510x(00)00426-3. [DOI] [PubMed] [Google Scholar]
- 7.Riviere M., Meininger V., Zeisser P., Munsat T. An analysis of extended survival in patients with amyotrophic lateral sclerosis treated with riluzole. Arch Neurol. 1998;55:526–528. doi: 10.1001/archneur.55.4.526. [DOI] [PubMed] [Google Scholar]
- 8.Yanagisawa N., Tashiro K., Tohgi H., Mizuno Y., Kowa H., Kimura J. Efficacy and safety of riluzole in patients with amyotrophic lateral sclerosis: double-blind placebo-controlled study in Japan. Igakuno Ayumi. 1997;182:851–866. [Google Scholar]
- 9.Yoshino H., Kimura A. Investigation of the therapeutic effects of edaravone, a free radical scavenger, on amyotrophic lateral sclerosis (Phase II study) Amyotroph Lateral Scler. 2006;7:241–245. doi: 10.1080/17482960600881870. [DOI] [PubMed] [Google Scholar]
- 10.Abe K., Itoyama Y., Sobue G., Tsuji S., Aoki M., Doyu M., Edaravone ALS Study Group Confirmatory double-blind, parallel-group, placebo-controlled study of efficacy and safety of edaravone (MCI-186) in amyotrophic lateral sclerosis patients. Amyotroph Lateral Scler Frontotemporal Degener. 2014;15:610–617. doi: 10.3109/21678421.2014.959024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iida M., Miyazaki I., Tanaka K., Kabuto H., Iwata-Ichikawa E., Ogawa N. Dopamine D2 receptor-mediated antioxidant and neuroprotective effects of ropinirole, a dopamine agonist. Brain Res. 1999;838:51–59. doi: 10.1016/s0006-8993(99)01688-1. [DOI] [PubMed] [Google Scholar]
- 12.Tanaka K., Miyazaki I., Fujita N., Haque M.E., Asanuma M., Ogawa N. Molecular mechanism in activation of glutathione system by ropinirole, a selective dopamine D2 agonist. Neurochem Res. 2001;26:31–36. doi: 10.1023/a:1007672414239. [DOI] [PubMed] [Google Scholar]
- 13.Du F., Li R., Huang Y., Li X., Le W. Dopamine D3 receptor-preferring agonists induce neurotrophic effects on mesencephalic dopamine neurons. Eur J Neurosci. 2005;22:2422–2430. doi: 10.1111/j.1460-9568.2005.04438.x. [DOI] [PubMed] [Google Scholar]
- 14.Höglinger G.U., Rizk P., Muriel M.P., Duyckaerts C., Oertel W.H., Caille I. Dopamine depletion impairs precursor cell proliferation in Parkinson disease. Nat Neurosci. 2004;7:726–735. doi: 10.1038/nn1265. [DOI] [PubMed] [Google Scholar]
- 15.Bozik M.E., Mather J.L., Kramer W.G., Gribkoff V.K., Ingersoll E.W. Safety, tolerability, and pharmacokinetics of KNS-760704 (dexpramipexole) in healthy adult subjects. J Clin Pharmacol. 2011;51:1177–1185. doi: 10.1177/0091270010379412. [DOI] [PubMed] [Google Scholar]
- 16.Wang H., Larriviere K.S., Keller K.E., Ware K.A., Burns T.M., Conaway M.A. R+ pramipexole as a mitochondrially focused neuroprotectant: initial early phase studies in ALS. Amyotroph Lateral Scler. 2008;9:50–58. doi: 10.1080/17482960701791234. [DOI] [PubMed] [Google Scholar]
- 17.Cudkowicz M., Bozik M.E., Ingersoll E.W., Miller R., Mitsumoto H., Shefner J. The effects of dexpramipexole (KNS-760704) in individuals with amyotrophic lateral sclerosis. Nat Med. 2011;17:1652–1656. doi: 10.1038/nm.2579. [DOI] [PubMed] [Google Scholar]
- 18.Cudkowicz M.E., van den Berg L.H., Shefner J.M., Mitsumoto H., Mora J.S., Ludolph A., EMPOWER investigators Dexpramipexole versus placebo for patients with amyotrophic lateral sclerosis (EMPOWER): a randomised, double-blind, phase 3 trial. Lancet Neurol. 2013;12:1059–1067. doi: 10.1016/S1474-4422(13)70221-7. [DOI] [PubMed] [Google Scholar]
- 19.De Giorgio F., Maduro C., Fisher E.M.C., Acevedo-Arozena A. Transgenic and physiological mouse models give insights into different aspects of amyotrophic lateral sclerosis. Dis Model Mech. 2019;12 doi: 10.1242/dmm.037424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fujimori K., Ishikawa M., Otomo A., Atsuta N., Nakamura R., Akiyama T. Modeling sporadic ALS in iPSC-derived motor neurons identifies a potential therapeutic agent. Nat Med. 2018;24:1579–1589. doi: 10.1038/s41591-018-0140-5. [DOI] [PubMed] [Google Scholar]
- 21.Brooks B.R., Miller R.G., Swash M., Munsat T.L., World Federation of Neurology Research Group on Motor Neuron Diseases El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord. 2000;1:293–299. doi: 10.1080/146608200300079536. [DOI] [PubMed] [Google Scholar]
- 22.Berry J.D., Miller R., Moore D.H., Cudkowicz M.E., van den Berg L.H., Kerr D.A. The Combined Assessment of Function and Survival (CAFS): a new endpoint for ALS clinical trials. Amyotroph Lateral Scler Frontotemporal Degener. 2013;14:162–168. doi: 10.3109/21678421.2012.762930. [DOI] [PubMed] [Google Scholar]
- 23.Freemantle N., Calvert M., Wood J., Eastaugh J., Griffin C. Composite outcomes in randomized trials: greater precision but with greater uncertainty? J Am Med Assoc. 2003;289:2554–2559. doi: 10.1001/jama.289.19.2554. [DOI] [PubMed] [Google Scholar]
- 24.Zarit S.H., Reever K.E., Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontol. 1980;20:649–655. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]
- 25.Zarit S.H., Zarit J.M. Pennsylvania State University Gerontology Center; University Park, PA: 1990. The memory and behaviour problems checklist 1987R and the burden Interview. [Google Scholar]
- 26.Mitsubishi Tanabe Pharma Co., Ltd: second confirmatory test (in-house material).
- 27.Jenkinson C., Levvy G., Fitzpatrick R., Garratt A. The amyotrophic lateral sclerosis assessment questionnaire (ALSAQ-40): tests of data quality, score reliability and response rate in a survey of patients. J Neurol Sci. 2000;180:94–100. doi: 10.1016/s0022-510x(00)00420-2. [DOI] [PubMed] [Google Scholar]
- 28.Jenkinson C., Fitzpatrick R., Brennan C., Swash M. Evidence for the validity and reliability of the ALS assessment questionnaire: the ALSAQ-40. Amyotrophic Lateral Scler Other Motor Neuron Disord. 1999;1:33–40. doi: 10.1080/146608299300080022. [DOI] [PubMed] [Google Scholar]
- 29.Shefner J.M., Liu D., Leitner M.L., Schoenfeld D., Johns D.R., Ferguson T. Quantitative strength testing in ALS clinical trials. Neurology. 2016;87:617–624. doi: 10.1212/WNL.0000000000002941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Norris F.H., Jr., Calanchini P.R., Fallat R.J., Panchari S., Jewett B. The administration of guanidine in amyotrophic lateral sclerosis. Neurology. 1974;24:721–728. doi: 10.1212/wnl.24.8.721. [DOI] [PubMed] [Google Scholar]
- 31.Hiraoka A., Yoshikawa M., Nakamori M., Hosomi N., Nagasaki T., Mori T. Maximum tongue pressure is associated with swallowing dysfunction in ALS patients. Dysphagia. 2017;32:542–547. doi: 10.1007/s00455-017-9797-z. [DOI] [PubMed] [Google Scholar]
- 32.Miyamoto S., Minakata Y., Azuma Y., Kawabe K., Ono H., Yanagimoto R. Verification of a motion sensor for evaluating physical activity in COPD patients. Can Respir J. 2018;2018:8343705. doi: 10.1155/2018/8343705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wolters E.C. Intrinsic and extrinsic psychosis in Parkinson's disease. J Neurol. 2001;248(suppl):22–27. doi: 10.1007/pl00007822. [DOI] [PubMed] [Google Scholar]
- 34.Acton G., Broom C. A dose rising study of the safety and effects on serum prolactin of SK&F 101468, a novel dopamine D2-receptor agonist. Br J Clin Pharmacol. 1989;28:435–441. doi: 10.1111/j.1365-2125.1989.tb03524.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kaye C.M., Nicholls B. Clinical pharmacokinetics of ropinirole. Clin Pharmacokinet. 2000;39:243–254. doi: 10.2165/00003088-200039040-00001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.