Abstract
Introduction
Patient and staff experiences are strongly influenced by attitudes and behaviours, and provide important insights into care quality. Patient and staff feedback could be used more effectively to enhance behaviours and improve care through systematic integration with techniques for reflective learning. We aim to develop a reflective learning framework and toolkit for healthcare staff to improve patient, family and staff experience.
Methods & analysis
Local project teams including staff and patients from the acute medical units (AMUs) and intensive care units (ICUs) of three National Health Service trusts will implement two experience surveys derived from existing instruments: a continuous patient and relative survey and an annual staff survey. Survey data will be supplemented by ethnographic interviews and observations in the workplace to evaluate barriers to and facilitators of reflective learning. Using facilitated iterative co-design, local project teams will supplement survey data with their experiences of healthcare to identify events, actions, activities and interventions which promote personal insight and empathy through reflective learning. Outputs will be collated by the central project team to develop a reflective learning framework and toolkit which will be fed back to the local groups for review, refinement and piloting. The development process will be mapped to a conceptual theory of reflective learning which combines psychological and pedagogical theories of learning, alongside theories of behaviour change based on capability, opportunity and motivation influencing behaviour. The output will be a locally-adaptable workplace-based toolkit providing guidance on using reflective learning to incorporate patient and staff experience in routine clinical activities.
Ethics & dissemination
The PEARL project has received ethics approval from the London Brent Research Ethics Committee (REC Ref 16/LO/224). We propose a national cluster randomised step-wedge trial of the toolkit developed for large-scale evaluation of impact on patient outcomes.
Keywords: behaviour change, empathy, medical care, patient experience, quality improvement, reflective learning, staff experience
Strengths and limitations of this study.
PEARL links together theories of reflection and learning with those of behaviour change (capability, opportunity and motivation influencing behaviour) in a novel framework.
Information from patient and staff surveys will provide insights into barriers to and facilitators of reflective and empathic behaviours.
Observations by ethnographers will provide information about the capability, opportunity and motivation of staff to reflect effectively.
Using co-design techniques, patients, relatives and clinical staff will develop workplace-based interventions for stimulating reflection.
To determine efficacy, the reflective learning toolkit will require testing subsequently in a prospective cluster-randomised clinical trial.
Introduction
Patient and staff experiences provide important insights into care quality, but health systems have difficulty using these experiences to improve care, particularly those related to attitudes, behaviours and culture.1–5 Reflective learning underpins approaches to improving non-technical skills, but the processes by which experiences are translated into reflection, and reflection into behavioural change are not well understood. We present a protocol for developing a toolkit to help frontline staff use patient and staff experiences to promote reflective learning, defined as an experiential process of personal insight development, in which one’s own and others’ experiences produce changes in behaviours.
Patient and staff experiences offer important insights into healthcare quality
Patient and staff experiences offer important insights into the quality of healthcare which complement organisational-level data on processes and outcomes.6–8 Patient experience is an explicit outcome measure in the UK National Health Service (NHS),9 10 and in the regulation of care quality.11 All NHS trusts are required to collect patient experience data through surveys.12 13 Complaints also provide an important data source.14 In the USA patients are surveyed through the Hospital Consumer Assessment of Healthcare Providers and Systems15 while in Australia health organisations are required to involve consumers in accreditation processes.16
Staff experience also provides insights into care quality: earlier action on staff concerns could have mitigated failings in care.17 18 The NHS staff survey has been conducted annually since 2003.19 Patients and staff appear to share complementary insights into care quality: patient satisfaction is higher in hospitals in which nurses also reported better care quality.20 21 Patient and staff perceptions appear to offer both overlapping and unique insights into safety in hospital.22
Patient and staff experience is strongly influenced by staff attitudes and behaviours
The NHS National Inpatient Survey asks respondents to rate their overall experience on a scale of 0 (‘very poor’) to 10 (‘very good’). In 2017, 50% of respondents rated their experience as 9 or above.12 This indicates that there are substantial opportunities within the health system for ‘learning from excellence’.23 However, ‘good’ ratings by patients (as opposed to ‘very good’) may also disguise important opportunities for improvement.24 A survey by Healthwatch England suggests that half of those experiencing substandard care do not report it.25 Patients who respond to surveys with perfect ratings but with negative free text frequently describe lapses in staff behaviours and attitudes,26 such as communication, empathy, courtesy, consideration, compassion and patient focus. A study of patient-reported safety incidents found that 22% were related to communication failures alone,27 while a systematic review of patient complaints28 judged that one-third were related to staff-patient relationships. This may be an underestimate: at the Queen Elizabeth Hospital in Birmingham local analysis shows that while non-technical aspects of patient care caused 37.7% of all issues raised, they were mentioned in 67.1% of all complaints (data on file). Non-technical issues are also likely drivers of staff dissatisfaction, as demonstrated by the 487 727 respondents to the NHS Staff survey in 2017.29 These data suggest that patient and staff experience, both positive and negative, provides an important opportunity for improvement through behaviour modification.
Patient and staff experience data are not used optimally to change behaviours
Using patient experience to improve care is not a trivial task.30 Lapses in care are usually multifactorial, the product of interactions between the individual and the ‘system’; but from the perspective of the patient, quality is largely about fiduciary relationships with specific individuals.31 Trust boards must contend with the competing priorities of hundreds of quality indicators each month, and may prioritise avoiding falling below a quality threshold rather than achieving higher values of a performance standard once met. A review in 2012 which examined how hospitals had used research from the UK’s national in-patient survey concluded that ‘simply providing hospitals with patient feedback does not automatically have a positive effect on quality standards’.32 Even trusts with a tradition of collecting and using patient survey data may struggle to convert these data into tangible improvements.33 In a study of 50 clinical and managerial staff in three English hospitals, Sheard et al 34 found that the collection of patient experience feedback was a ‘self-perpetuating industry’ conducted ‘at the expense of pan-organisational learning or improvements’; ward staff had difficulty using patient feedback. They concluded that ‘macro and micro prohibiting factors come together in a perfect storm which (prevent) improvements being made’. In a systematic review Gleeson reported that ‘Patient experience data were most commonly…used to identify small areas of incremental change to services that do not require a change to clinician behaviour’.35 Institutional commitment to using patient feedback may not be reflected at the front-line, where single individuals can adversely influence other members of staff.36 Conversely, frontline staff can struggle to get their voices heard at senior levels: one of the recommendations of the Mid Staffs enquiry17 has been to establish ‘Freedom To Speak Up Guardians’ in all NHS trusts to ensure that staff concerns are heard and acted on.37 These findings indicate that changing behaviours requires a change in underlying attitudes at individual, group and organisational levels. How is this best achieved?
Changing attitudes and behaviours involves learning through reflection
Behavioural modification is a key societal preoccupation.38 A large number of techniques exist: a proposed behaviour change taxonomy has so far identified 93 different interventions.39 40 However, evidence supporting the primacy of one technique over another is not strong.41 42 Many interventions involve personal insight development through reflection, but few behaviour change theories express this explicitly. One which does is the capability, opportunity and motivation influencing behaviour (COM-B) model43 which assimilates 19 behaviour change theories into a single framework in which the behaviour of interest has three determinants, each with two subtypes: capability (physical and psychological), opportunity (physical and social) and motivation (reflective and automatic). The automatic subtype for motivation relies on heuristics, is engaged in conditions of complexity and stress and maps to Daniel Kahneman’s ‘System 1’ thinking.44 The reflective component is slower, more effortful and analytical (‘System 2’ thinking). These two subtypes of motivation map to the ‘peripheral’ and ‘central’ routes described in the elaboration likelihood model of persuasion.45 46 Factors influencing motivation (particularly the automatic subtype) are summarised in the acronym MINDSPACE: messenger, incentives, norms, defaults, salience, priming, affect, commitment and ego.47 As the behaviour of interest here is reflection itself, we need to consider both the automatic factors which influence the desire to reflect and the more effortful elements of ‘reflecting on the need for reflection’. We consider next how theories of reflection as a behaviour link to theories of reflective learning as a tool for personal insight development.
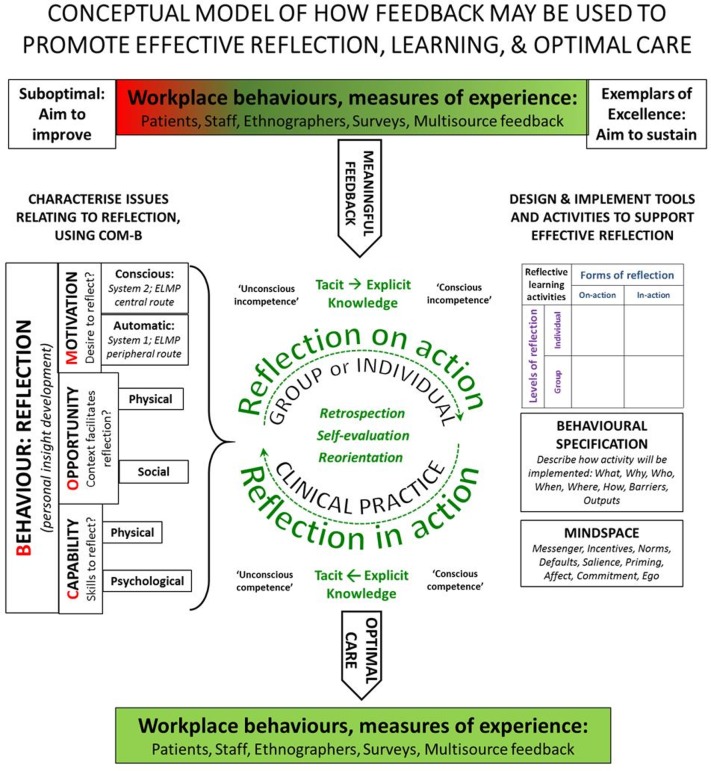
How does reflection stimulate learning? Kolb presented reflection as a four-stage model: experience, observation, analysis and recalibration.48 Schön described reflection ‘in-action’, and ‘on-action’.49 Others emphasise the importance of an emotional component to reflective learning,50 including the ‘disorientating dilemma’,51 the realisation that there is a gap between desired and actual behaviours. Sandars describes reflection as a metacognitive process that creates a greater understanding of self and situation to inform future actions52: looking back to look forward. This involves a transition from tacit to explicit knowledge,53 in which socially-acquired norms of behaviour54 are modified either through individual reflection or, more powerfully, through group activities.55 The process shares similarities with Broadwell’s four stages of competence56: unconscious incompetence (unaware of problem), conscious incompetence (data received, now being processed), conscious competence (using data to improve or disseminate excellence) and unconscious competence (effortless excellence). Effective reflection appears to involve making this transition, while recalibrating and reinterpreting experience in-action and on-action. We present a possible model linking theories of reflective learning to theories of behaviour change in figure 1.
Figure 1.
Conceptual model linking theories of behaviour change to those of reflective learning. COM-B, capability, opportunity and motivation influencing behaviour.
Reflective learning could be deployed more effectively to improve care quality
First described by Dewey in 1933,57 reflective learning is now a mandatory tool in the education of health professionals. In the UK, the General Medical Council and others define reflective practice as ‘the process whereby an individual thinks analytically about anything relating to their professional practice with the intention of gaining insight and using the lessons learnt to maintain good practice or make improvements where possible’. They state that ‘Reflecting on … experiences is vital to personal well-being and development, and to improving the quality of patient care’.58 Reflection is incorporated in all healthcare postgraduate training programmes in the UK, and evidence of reflecting on patient and colleague (‘multi-source’) feedback is required for physicians’ continuing professional development and revalidation.
However, despite the widespread acceptance of reflection as a tool for self-improvement, its utility in enhancing performance is uncertain,59 60 as is the efficacy of using patient experience surveys to promote reflection.61 People are biased towards favourable events and judgements,62 and doctors tend to reject the validity of adverse patient feedback.63 Undesirable information is processed as a threat with physiological correlates, which can impede learning.64 Effective reflection requires the emotional strength and capacity to take a critical view of one’s skills, attitudes and behaviours, which may be lacking among poor performers.65 In the UK, doctors are concerned that honest reflections documented in personal portfolios might incriminate them in a court of law.66
Communication skills training should provide an opportunity for reflection. However, a review of 243 studies of teaching communication skills to medical undergraduates identified only 16 interventional studies and only two of these reported behavioural outcomes,67 making it difficult to determine whether ‘communication skills’ are sufficient, or even if such courses are effective at all. At postgraduate level, the effects of communication skills training appear to be weak or evanescent,68–73 and in one randomised controlled trial were associated with worse depression among patients in the intervention group.74
By contrast, interventions focused on engaging staff in workplace-based activities which improve teamworking,75 insight, patient-centred care and empathy may be more effective and more durable.76–87 The Cleveland Clinic offers short videos on empathy,88 and similar internet-based resources demonstrate how emotion may be engaged to stimulate reflection and promote mutual understanding.89 90 For reflective learning to improve patient and staff experience, it must do so by changing ‘hearts and minds’. This is the focus of our research.
Aims & objectives
We aim to develop methods for using patient and staff experiences to promote effective reflection and patient-centred care.
Specific objectives include:
Developing a programme theory linking experiential feedback to reflective learning and behaviour change.
Establishing surveys for recording patient and staff experience.
Determining attitudes to, and uses of, patient and staff experience data.
Determining attitudes to, and techniques for, reflective learning.
Mapping factors which influence reflective learning to the COM-B model of behaviour change.
Developing and piloting methods for incorporating effective reflection in routine practice.
Outputs
The primary output will be guidance on effective reflective learning, in the form of a framework and toolkit.
Secondary outputs include data on patient and staff experience, how staff use these data to promote reflective learning and how staff propose to include reflective learning in routine activities in the workplace.
Study design
This is a 3 year mixed-methods observational study using patient and staff co-design techniques.
In subsequent research, we intend to evaluate the utility of the reflective learning toolkit in a cluster randomised step-wedge trial.
Participants and setting
Participants include clinical and managerial staff and patients and relatives from the three acute medical units (AMUs) and five intensive care units (ICUs) of three large urban hospital trusts: the Queen Elizabeth Hospital Birmingham, Heartlands Hospital Birmingham and Newcastle upon Tyne NHS Foundation Trust (Royal Victoria Infimary and Freeman Hospitals). This will provide access to at least 100 000 acute admissions over 2 years, from which we anticipate surveying around 25% with a response rate of 30%, providing around 7500 returned questionnaires for analysis.
Each AMU and ICU will have a project group, and these will come together as site teams lead by a senior clinician. Meetings will be chaired by a non-executive director. Local project teams will be asked to ensure inclusion of at least two patient representatives. The research will be directed by the central project team which includes patient representatives, clinicians, social scientists, a behavioural psychologist, an educationalist and a co-design expert. Project governance will be overseen by an independent project steering committee.
The study is located in acute and emergency care settings for several reasons: acutely ill patients represent at least 50% of all hospitalised NHS patients, acute illness accentuates sensitivity to staff behaviours, emergency care creates particular demands on the non-technical skills of staff and both environments demand a high degree of multidisciplinary team working. Intensive care units offer a much higher ratio of nurses and doctors to patients than AMUs which provides an opportunity for comparison.
Definitions and programme theory
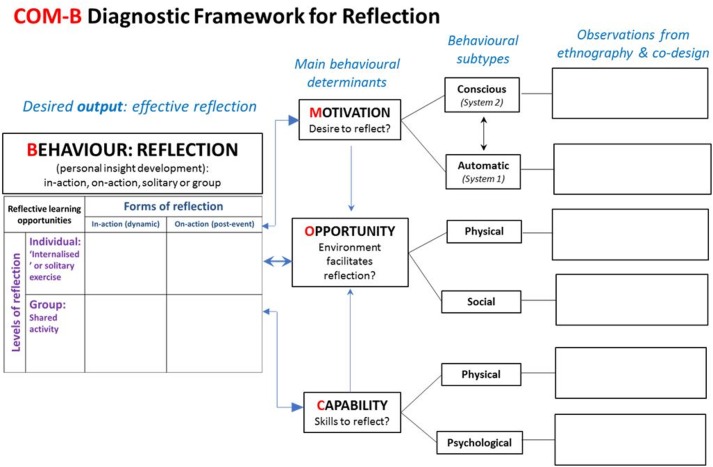
As stated above, we define reflective learning as an experiential process of personal insight development, in which one’s own and others’ experiences are used to produce a change in behaviours. The PEARL programme theory (figure 1) integrates theories of reflective learning with theories of behaviour change, as described in the introduction, using the approach recommended by the Medical Research Council for the development and evaluation of complex interventions.91 Our target behaviour is engagement in effective reflection, with consequential acquisition of insight, behavioural change and improvements to practice/standards of care. The COM-B model43 will be used to characterise capability, opportunity and motivation to engage in individual and group reflection, and this analysis will inform the development of tools to support the embedding of reflection in practice. This will be facilitated through the use of the PEARL-formatted COM-B diagram (figure 2) as a diagnostic tool. Diverse activities involving reflection in-action, on-action, solitary and group, can be documented in the box to the left of the diagram. The boxes on the right permit recording of facilitators or inhibitors of the three determinants of behaviour – motivation, opportunity and capability – and their subtypes. We will adapt the programme theory in the light of experience as the project proceeds.
Figure 2.
PEARL diagnostic framework using the COM-B model. COM-B, capability, opportunity and motivation influencing behaviour.
Methods and analysis
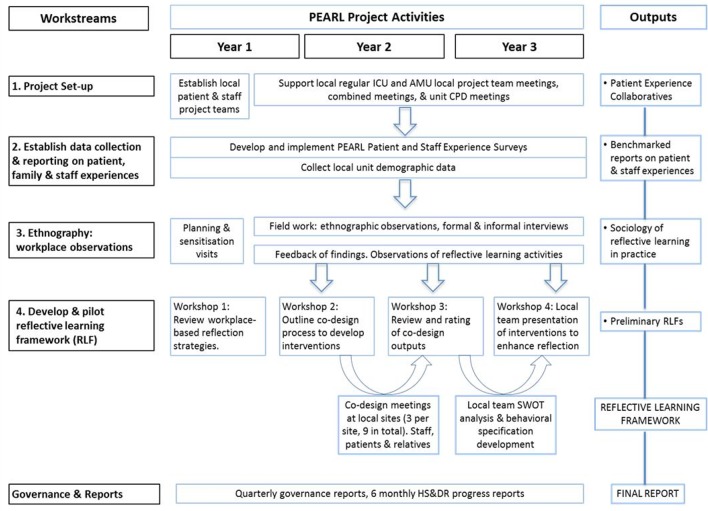
The PEARL project will run for a 3 year period from October 2016 to September 2019. Project workstreams and activities are displayed in figure 3.
Figure 3.
PEARL project gantt chart. AMU, acute medical unit; CPD, Continuing professional development; HS&DR, Health Services and Delivery Research; ICU, intensive care unit; SWOT, Strengths, weaknesses, opportunities, threats.
Workstream 1: project set-up
We will establish local site project groups as ‘communities of practice’,92 93 based on our earlier work showing that clinicians disengaged by multiple quality improvement policy initiatives are more motivated when they have professional ownership of the process and when performance feedback is linked to particular patients or events.94 95 Local project groups will include a non-executive trust director, patient representatives and AMU and ICU clinical and managerial staff. Opportunities for feedback and reflection will be identified and local arrangements for project delivery agreed. This includes the process for acquiring, analysing, reporting and benchmarking of data from surveys and local performance and quality data. Local project teams will be asked to hold meetings once every 2 months to review project outputs, encourage team reflection (for example through existing meetings, team briefs and formal reports) and consider methods for incorporating feedback in routine practice.
Workstream 2: experiential data collection
Patient and staff experience data collected routinely in the NHS do not enable responses to inform practice at unit level, and usually do not offer or report free-text responses. Duplication of questions between surveys is common; none simultaneously addresses issues of communication, clinical care, patient safety, satisfaction and response to feedback. We will therefore select previously validated questions across different questionnaires to create a single, parsimonious survey for patients and relatives, and a separate survey for staff. Both questionnaires will be anonymous, paper-based, permit optical character recognition, employ a 5-point scale for rating agreement and offer free-text for additional information. Questionnaires will be accompanied by a reply-paid envelope and covering letter. Survey forms will be returned to the central project team to be digitised, analysed and reported to each trust’s local project lead. Free-text responses will be transcribed and analysed using NVivo. Response rates will be determined from denominator data for each survey group.
Patient & Relative Experience Survey: the questionnaire will be developed from the Family Satisfaction Survey (FS-ICU),96–98 the Adult In-Patient Survey12 and the Friends and Family Test (F&FT).13 The questionnaire will be offered continuously throughout the project to patients and relatives who have spent >24 hours in the AMU, and to all relatives of patients in the ICU >48 hours. Different methods of distribution will be trialled by the individual teams before definitive implementation. Denominator data will be collected from trust admission databases to calculate response rates: a response rate of around 30% is anticipated (target 7500 responses). A covering letter will be provided with the questionnaire, suitably adapted for bereaved families. Performance-importance plots will be derived from the % ‘excellent’ ratings versus the correlation of each item with the overall weighted satisfaction score.
Staff Experience Survey: The aim of this survey is to gain insights into individual, contextual and organisational influences on staff behaviour, and attitudes to the use of patient experience for reflection and improvements in care. Questions will be derived from the following validated questionnaires: NHS Staff Core Survey,19 the Staff F&FT,99 Hospital Survey on Patient Safety Culture,100 Teamwork and Safety Climate Survey,101 General Medical Council Trainee Survey102 and the Self-Reflection and In-Sight Scale.103 Additional questions will be developed by the central project team to investigate attitudes towards the use of feedback for reflection and the potential for biases related to anxieties about transparency and honesty. Local project teams will be invited to participate in a modified Delphi method to prioritise questions for the final set.
The staff survey will be offered over a 2 month period during year 2 and year 3 of the project. A response rate of 50% is anticipated with a target of 600 staff responses during each round of the survey. Free-text will be transcribed and analysed using NVivo. Results will be collated in unit-specific reports benchmarked against aggregated data for the group as a whole, and where this is available, against national performance reports.
The results from both surveys will be presented to the AMUs and ICUs in the form of standardised reports showing the proportion of respondents selecting each level of strength of agreement with each statement. For the patient and relative satisfaction survey we will provide performance-importance plots which will show the relationship between the level of satisfaction with each item in the questionnaire, and how that particular item influences overall satisfaction. Free text will be encoded for thematic analysis using NVivo, and presented to the staff in each unit. As the main purpose of the surveys is to stimulate reflective learning by the local teams, all free text feedback will be returned to the local teams. If staff are named in this feedback the names will be redacted from the full reports, but made known to the project leads. If allegations relating to patient safety or staff probity were to be made, these will be reported unredacted to the non-executive director chairing the local project team.
Workstream 3: ethnography
This workstream has two phases. Phase 1 will employ site visits, interviews with around 40 front-line and managerial staff and workplace-based observations of up to 5 days per participating site, to describe the current use of patient experience data, to explore options for the feedback of data as part of the reflective learning process and to investigate barriers to and opportunities for workplace-based reflective learning. Phase 2 will focus on observations of co-design workshops, and of the implementation and piloting of components of the toolkit in practice. Findings from both phases will be used to inform the development of the reflective learning framework and toolkit in workstream 4.
Observations and interviews will be conducted by ethnographers (social scientists) experienced in making observations in the clinical environment. Publicly visible information sheets describing the project will be provided in clinical areas. Informed written consent will be obtained for formal interviews. No staff identifiers (other than professional status/occupational group) will be collected. We expect interviews to be approximately 1 hour in duration but appreciate this is likely to vary by individual.
Analysis of data will occur over the course of the fieldwork period. Interviews and field notes will be transcribed verbatim and coded using NVivo. Analysis will draw on elements of grounded theory, in particular, the constant comparative approach104 and will remain grounded in the data. We will use techniques developed through our experience of conducting large scale ethnographic studies to enable us to manage the large amounts of data generated, and to move quickly from data to interpretation. These include regular debriefs and the production of summaries of data by site and across sites, organised by research questions and emerging themes.
Workstream 4: co-design and piloting of the reflective learning framework & toolkit
‘Co-design’ or ‘co-production’ involves service users and providers working together using a structured approach to create improvements.105 Co-design has been used previously in exploring patient feedback.106 We will use an adapted version107 of the British Design Council’s ‘double diamond’ approach, of ‘Discover, Define, Develop and Deliver’ in which the initial problem (‘How to promote effective reflection’) is subject to two rounds of divergent and convergent thinking, first to refine the problem, and second to develop solutions. The co-design workshops will use creative co-production, which has collective making108 as its central approach to ensure meaningful engagement and creative responses from all participants.
Workstream 4 will therefore consist of 13 co-design meetings (table 1). The co-design meetings will consist of four plenary workshops for the whole collaboration over the period of the project; and three local meetings in year two for each local project team conducted on-site at each trust (nine local meetings in total). Attendees will include patients and relatives, clinical staff and the non-executive directors. The co-design elements will be developed in collaboration with the researchers from Lab4Living, the Art and Design Research Centre, Sheffield Hallam University. Co-design aims and outputs are shown in table 1. We anticipate that while the teams are becoming established, the process of reflection may be accompanied by release of emotions related to personal experiences. Project team members have expertise in managing emotionally challenging situations, and will ensure that individual experiences are channelled into creative outputs by the local teams. In this respect, reflection will have both therapeutical and educational value for the project as a whole.
Table 1.
Co-design meetings
| Event | Participants | Aims or activity |
| Workshop 1 | All project participants, central location | Discuss the background to the project and review or modify the proposed methodology |
| Workshop 2 | All project participants, central location | Co-design approach will be introduced to the local project teams |
| Site meetings 1 | Local project team, project core team, design team, meeting at each of the three sites | Describe ‘reflective moments’ – occasions when an event stimulated personal insight development |
| Site meetings 2 | Discuss attitudes to reflection and how habits and preferences shape response to events and the capacity for insight development | |
| Site meetings 3 | Discuss reflective opportunities – how reflection can be incorporated in routine activities in the workplace | |
| Workshop 3 | All project participants, central location | Structure and content of the toolkit will be provisionally outlined, and a set of candidate prototype interventions (tools and techniques for reflection). |
| Workshop 4 | All project participants, central location | Teams present experience of developing & piloting interventions. |
Following workshop 3, local project teams will be invited to develop behavioural specifications for embedding a maximum of three interventions into routine clinical activities. Teams will use COM-B as an analytical tool (figure 2) to identify gaps in reflective practice which can be addressed through these behavioural specifications. The teams will present their experiences of selecting, specifying and piloting interventions in the final plenary workshop 4.
Toolkit development: Outputs from each of the 13 co-design meetings will be documented by the ethnographers and members of the core project team and will feed into toolkit development. The members of the core project team will collate their findings from the co-design meetings and cross-reference them with ethnographic findings from site visits to produce short guidance notes and resource materials under the following headings: Aims of the toolkit, What is reflection?, Why reflect?, How to reflect effectively, Reflection in daily practice, Stimulating reflection in others, Evidencing reflection and Organisational support for reflection. The reflective learning framework and toolkit will be evaluated locally by the participating units. Staff will be asked to offer their views on the specific interventions. This feedback will be incorporated in the final version.
Patient & public involvement
The PEARL project puts patients and relatives at the centre of the research and they were involved at inception in the initial design, contributing as full collaborators. PEARL is a developmental project which uses co-design to develop the reflective learning framework. To develop the framework, patients and relatives from the acute medical units and intensive care units of four hospitals in three trusts will work together collaboratively in 12 facilitated workshops as well as being full members of each local project team. They are helping to design the patient and staff surveys, and have informed decisions about the extent to which patient and public involvements can contribute to this type of co-design process. They are co-authors in publications and will participate in dissemination activities.
Discussion
Patient experience data demonstrate important opportunities to improve the quality of healthcare, particularly those relating to attitudes, behaviours and staff-patient relationships. However, these data are not used optimally by organisations or frontline staff to make improvements. Reflective learning should hold the key to converting experience into action, but there is little evidence about how reflection can most effectively be incorporated in routine clinical practice for individuals and teams.
The PEARL project aims to develop a framework and toolkit to support effective reflection in the workplace. The apparent simplicity of this aim disguises the underlying complexity of the relationships linking the various theories of reflection, learning and behaviour change, as demonstrated in the introduction and in figure 1. These theories show that reflective learning – which has almost achieved the status of received wisdom in medical education – is itself a form of behaviour subject to multiple influences, summarised in the COM-B model. Individuals and groups vary in their capacity, opportunity and motivation to reflect, and to do so in a manner which promotes personal growth. And having reflected effectively, they must then use these insights to drive changes in behaviours at the ‘sharp end’ of medicine as well as at institutional level. It is perhaps not surprising that health systems have difficulty using patient and staff experience data to improve care quality.
Most interactions between patients and healthcare staff are associated with positive experiences. This is an asset in terms of reflection and behaviour modification, for two reasons. First, there are many excellent role models available, and a systematic approach for identifying and learning from them can help others to acquire similar skills. Second, it takes courage and resilience to cope with the discovery of imperfections, and this may be easier if the setting is one which prioritises learning from excellence.23
Emotional engagement is important in engaging people’s attention and in promoting empathy, but not at the price of preventing analytical thinking: the elaboration likelihood model of persuasion provides some evidence for the value of analysis over heuristics in sustained change in attitudes and beliefs.46 It may be easier to accept and improve deficiencies in technical skills than in attitudes and behaviours, because technical issues allow us to focus externally on the tool, while non-technical issues reflect on our inner character and personality, and evidence of deficiencies is therefore more threatening. Models of reflective learning may help to ‘externalise’ behaviours, providing enough distance to allow constructive analysis. The process of self-critiquing may also be made more palatable – that is, enhancing the recipient’s resilience - by focusing initially on positive aspects of feedback.
Potential limitations of the co-design process involve self-selection of participants naturally predisposed to favour reflection rather than sceptics. We will mitigate this by considering reflective personae when developing the interventions. A limitation of the patient survey is that respondents may have difficulty distinguishing locations (for example acute medical units vs ordinary wards). The accompanying patient information sheets will explain the the survey is focused on the initial period of care immediately following admission through the emergency department.
The PEARL project will gather important insights into the ‘black box’ of reflective learning. The framework and toolkit will use patient and staff experience to support workplace-based effective reflection and improvement during routine clinical practice for individuals and teams. Our intent in subsequent research is to evaluate the logic model (figure 1) and the toolkit in a mixed-methods step-wedge cluster randomised trial. The precise form this will take will become apparent in the final year of the project; it will be classed as a complex intervention, and the workstreams described above will test the methodologies to be deployed during larger scale roll-out.
Ethics & dissemination
Implied consent will apply to the return of completed questionnaires. Informed consent will be sought from participants of ethnographic interviews.
Research findings will be submitted for publication by scientific journals and presentation at conferences in the disciplines of patient safety, health services research, implementation science and intensive care medicine. We will also propose a national cluster randomised step-wedge trial of the toolkit for large-scale evaluation of impact on patient outcomes. We will offer this as a resource for national multidisciplinary training programmes through our partner organisations in acute and intensive care medicine, nursing and allied health professional programmes.
Supplementary Material
Acknowledgments
The PEARL project team are grateful to the study Steering Committee for their invaluable support; Professor Rebecca Lawton, Mr Harry Turner, Professor James Neuberger and Professor Stephen Brett. Dr Remi Bec and Cheryl Grindell were instrumental in the planning of the co-design workshops.
Footnotes
Contributors: OB as project manager and collaborator will manage the day-to-day running of the project under the CI, managing governance and study set-up, processing, analysis and presentation of study findings. CB has a strong academic background in pedagogical research at the University of Warwick, and is the lead for medical education and reflection in PEARL, workstream 4. She will contribute to our understanding of how reflection is used to achieve learning. CT is Associate Professor in Health Psychology and Joint Group Lead of the SAPPHIRE group at the University of Leicester. She is the lead for the ethnographic workstream (workstream 3), directing a group of ethnographers making original observations of practice. JA is Professor in Medical Education Research at the University of Plymouth. He is our expert on multisource feedback, advising on how to convert feedback into effective reflection. DB and LMB are patient and relative representatives with extensive experience of the totality of the emergency care pathway. They will provide insights into patient-staff interactions. IC is an intensive care consultant at Newcastle Upon Tyne NHS Trust. He will advise on practical aspects of reflective learning and will help co-design the reflection toolkit. FE is the statistician for the project and will oversee the quantitative analysis from the patient and staff survey instruments. FG Smith is the local lead for the intensive care unit at Heartlands Hospital. She will advise on practical aspects of reflective learning and will help co-design the reflection toolkit. CG is consultant in Acute Medicine at Newcastle Upon Tyne NHS Trust. He will advise on practical aspects of reflective learning and will help co-design the reflection toolkit. EH is the Acute Medicine lead at Heartlands Hospital. She will advise on practical aspects of reflective learning and will help co-design the reflection toolkit. JJ is the ethnography research fellow, organising and collating information from interviews and near-patient observations, and responsible for the analysis of qualitative data. RL is the PEARL methodologist advising on study design. RM is the local lead for the intensive care unit at the Queen Elizabeth Hospital. She will advise on practical aspects of reflective learning and will help co-design the reflection toolkit. GP is the trainee representative for the project, also part of the intensive care local team at Queen Elizabeth Hospital. He will analyse data from the GMC survey. GP is Professor of Intensive Care Medicine at the University of Warwick, and is the lead for debriefing and feedback in PEARL. JS is an intensive care consultant at Newcastle Upon Tyne NHS Trust. He will advise on practical aspects of reflective learning and will help co-design the reflection toolkit. CS is the Acute Medicine lead at the Queen Elizabeth Hospital. She will advise on practical aspects of reflective learning and will help co-design the reflection toolkit. PS represents the Society of Acute Medicine in PEARL, and provides expertise in quality improvement in acute medicine. IV is Professor of Behavioural Sciences at the University of Warwick. He advises the PEARL project on behaviour change theory and techniques, and will lead this aspect of the toolkit development. DW is the co-design facilitator who will lead the co-design workshops and help with the design of the toolkits. SEW is the senior intensive care consultant at Newcastle Upon Tyne NHS Trust. He will advise on practical aspects of reflective learning and will help co-design the reflection toolkit. He also advises the project on the family satisfaction survey. JB is the Chief Investigator responsible for the overall design, management and conduct of the study with extensive experience in health services research, pedagogical development and intensive care medicine.
Funding: This project is funded by the National Institute for Health Research (NIHR) Health Services and Delivery Research Programme (Ref 14/156/23). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Competing interests: None declared.
Ethics approval: The PEARL projecthas received ethics approval from the London Brent Research Ethics Committee(REC Ref 16/LO/224).
Provenance and peer review: Not commissioned; externally peer reviewed.
Collaborators: The PEARL Collaboration:J Willars; C Higenbottam; F Wyton; E Fellows; K Moss; L Cooper; L Flavell; J Flavell; J Raeside; M Hawkesford; H Laugher; T Jones; S Nevitt; K Naylor; J Sampson; J Mann; S Ballinger; T Melody; G Buggy; L Linhartova; J Thompson; S Majid; P Diviyesh; P Thorpe; A Shaha; R Carvell; A Joshi; K Kneller; H Halliday; C Iles; I O’Neil; G Yeoman; C Randell; H Korovesis; C Scott; H Doherty; K Protheroe; E Swann; L Dunn; K McCourt; S Perks; T Chakravorty; C Grindell; R Bec; L Duffy; E Tracey, C Nee; S Vince; I Barrow; N Alderson; C Straughan; K Cullen; I Spencer; M Thomas
Patient consent for publication: Not required.
Contributor Information
On-behalf-of the PEARL Collaboration:
J Willars, C Higenbottam, F Wyton, E Fellows, K Moss, L Cooper, L Flavell, J Flavell, J Raeside, M Hawkesford, H Laugher, T Jones, S Nevitt, K Naylor, J Sampson, J Mann, S Ballinger, T Melody, G Buggy, L Linhartova, J Thompson, S Majid, P Diviyesh, P Thorpe, A Shaha, R Carvell, A Joshi, K Kneller, H Halliday, C Iles, I O’Neil, G Yeoman, C Randell, H Korovesis, C Scott, H Doherty, K Protheroe, E Swann, C Scott, L Dunn, K Mccourt, S Perks, T Chakravorty, C Grindell, and R Bec
Collaborators: On-behalf-of the PEARL Collaboration
References
- 1. Dixon-Woods M, Baker R, Charles K, et al. Culture and behaviour in the English National Health Service: overview of lessons from a large multimethod study. BMJ Qual Saf 2014;23:106–15. 10.1136/bmjqs-2013-001947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sheard L, Marsh C, O’Hara J, et al. The patient feedback response framework–understanding why UK hospital staff find it difficult to make improvements based on patient feedback: a qualitative study. Soc Sci Med 2017;178:19–27. 10.1016/j.socscimed.2017.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mannion R, Davies H. Understanding organisational culture for healthcare quality improvement. BMJ 2018;363:k4907 10.1136/bmj.k4907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Martin GP, Aveling EL, Campbell A, et al. Making soft intelligence hard: a multi-site qualitative study of challenges relating to voice about safety concerns. BMJ Qual Saf 2018;27:710–7. 10.1136/bmjqs-2017-007579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Armstrong N, Brewster L, Tarrant C, et al. Taking the heat or taking the temperature? A qualitative study of a large-scale exercise in seeking to measure for improvement, not blame. Soc Sci Med 2018;198:157–64. 10.1016/j.socscimed.2017.12.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization. The world health report 2000. Health systems: improving performance: WHO, 2000. [Google Scholar]
- 7. Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century: National Academy Press, 2001. [PubMed] [Google Scholar]
- 8. Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013;3:e001570 10.1136/bmjopen-2012-001570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Darzi A. High Quality Care For All. NHS Next Stage Review Final Report: Department of Health, 2008. [Google Scholar]
- 10. NHS Outcomes Framework. https://digital.nhs.uk/data-and-information/publications/ci-hub/nhs-outcomes-framework [Accessed Feb 2019].
- 11. Care Quality Commission. https://www.cqc.org.uk/file/151928 [Accessed Feb 2019].
- 12. Care Quality Commission, Adult In-Patient Survey. 2017. http://www.cqc.org.uk/publications/surveys/adult-inpatient-survey-2016 [Accessed Feb 2019].
- 13. NHS Friends and Family Test. https://www.england.nhs.uk/fft/ [Accessed Feb 2019].
- 14. NHS Digital, Data on Written Complaints in the NHS. https://digital.nhs.uk/data-and-information/publications/statistical/data-on-written-complaints-in-the-nhs [Accessed Feb 2019].
- 15. HCAHPS. https://www.hcahpsonline.org/ [Accessed Feb 2019].
- 16. Australian Commission on Safety and Quality in Health Care. National safety and quality health service (NSQHS) standards. Sydney: ACSQHC, 2012. [Google Scholar]
- 17. Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office., 2013. [Google Scholar]
- 18. Gosport Enquiry. 2018. https://www.gosportpanel.independent.gov.uk/panel-report/ [Accessed Feb 2019].
- 19. NHS Staff Survey. http://www.nhsstaffsurveys.com/Page/1056/Home/NHS-Staff-Survey-2018/ [Accessed Feb 2019].
- 20. Aiken LH, Sermeus W, Van den Heede K, et al. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ 2012;344:e1717 10.1136/bmj.e1717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Flott K, Darzi A, Mayer E. Care pathway and organisational features driving patient experience: statistical analysis of large NHS datasets. BMJ Open 2018;8:e020411 10.1136/bmjopen-2017-020411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lawton R, O’Hara JK, Sheard L, et al. Can staff and patient perspectives on hospital safety predict harm-free care? An analysis of staff and patient survey data and routinely collected outcomes. BMJ Qual Saf 2015;24:369–76. 10.1136/bmjqs-2014-003691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Learning from Excellence. https://learningfromexcellence.com/ [Accessed Feb 2019].
- 24. Burt J, Newbould J, Abel G, et al. Investigating the meaning of ’good' or ’very good' patient evaluations of care in English general practice: a mixed methods study. BMJ Open 2017;7:e014718 10.1136/bmjopen-2016-014718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Healthwatch. Suffering in silence: Listening to consumer experiences of the health and social care complaints system: Healthwatch, 2014. [Google Scholar]
- 26. Gallan AS, Girju M, Girju R. Perfect ratings with negative comments: Learning from contradictory patient survey responses. Patient Exp J 2017;4:15–28. 10.35680/2372-0247.1234 [DOI] [Google Scholar]
- 27. O’Hara JK, Reynolds C, Moore S, et al. What can patients tell us about the quality and safety of hospital care? Findings from a UK multicentre survey study. BMJ Qual Saf 2018;27:673–82. 10.1136/bmjqs-2017-006974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Reader TW, Gillespie A, Roberts J. Patient complaints in healthcare systems: a systematic review and coding taxonomy. BMJ Qual Saf 2014;23:678–89. 10.1136/bmjqs-2013-002437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. NHS Staff survey. 2017. http://www.nhsstaffsurveys.com/Page/1064/Latest-Results/2017-Results/ [Accessed Feb 2019].
- 30. Flott KM, Graham C, Darzi A, et al. Can we use patient-reported feedback to drive change? The challenges of using patient-reported feedback and how they might be addressed. BMJ Qual Saf 2017;26:502–7. 10.1136/bmjqs-2016-005223 [DOI] [PubMed] [Google Scholar]
- 31. Scott DAH, Grant SM. A meta-ethnography of the facilitators and barriers to successful implementation of patient complaints processes in health-care settings. Health Expect 2018;21:508–17. 10.1111/hex.12645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. DeCourcy A, West E, Barron D. The National Adult Inpatient Survey conducted in the English National Health Service from 2002 to 2009: how have the data been used and what do we know as a result? BMC Health Serv Res 2012;12:71 10.1186/1472-6963-12-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lee R, Baeza JI, Fulop NJ. The use of patient feedback by hospital boards of directors: a qualitative study of two NHS hospitals in England. BMJ Qual Saf 2018;27:103–9. 10.1136/bmjqs-2016-006312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sheard L, Peacock R, Marsh C, et al. What’s the problem with patient experience feedback? A macro and micro understanding, based on findings from a three-site UK qualitative study. Health Expect 2019;22:46–53. 10.1111/hex.12829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gleeson H, Calderon A, Swami V, et al. Systematic review of approaches to using patient experience data for quality improvement in healthcare settings. BMJ Open 2016;6:e011907 10.1136/bmjopen-2016-011907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sheard L, Marsh C, O’Hara J, et al. Exploring how ward staff engage with the implementation of a patient safety intervention: a UK-based qualitative process evaluation. BMJ Open 2017;7:e014558 10.1136/bmjopen-2016-014558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Freedom To Speak Up Guardians. https://www.cqc.org.uk/national-guardians-office/content/national-guardians-office [Accessed Feb 2019]
- 38. The Behavioural Insights Team. Cabinet Office. https://www.behaviouralinsights.co.uk/ [Accessed Feb 2019].
- 39. Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81–95. 10.1007/s12160-013-9486-6 [DOI] [PubMed] [Google Scholar]
- 40. Michie S, West R, Sheals K, et al. Evaluating the effectiveness of behavior change techniques in health-related behavior: a scoping review of methods used. Transl Behav Med 2018;8:212–24. 10.1093/tbm/ibx019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Johnson MJ, May CR. Promoting professional behaviour change in healthcare: what interventions work, and why? A theory-led overview of systematic reviews. BMJ Open 2015;5:e008592 10.1136/bmjopen-2015-008592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Chauhan BF, Jeyaraman MM, Mann AS, et al. Behavior change interventions and policies influencing primary healthcare professionals' practice-an overview of reviews. Implement Sci 2017;12:3 10.1186/s13012-016-0538-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6:42 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kahneman D. Thinking, fast and slow. Penguin 2012. [Google Scholar]
- 45. Petty RE, Cacioppo JT. The effects of involvement on responses to argument quantity and quality: Central and peripheral routes to persuasion. J Pers Soc Psychol 1984;46:69–81. 10.1037/0022-3514.46.1.69 [DOI] [Google Scholar]
- 46. O’Keefe D. The Elaboration Likelihood Model : Dillard JP, Shen L, The SAGE Handbook of Persuasion: Developments in Theory and Practice: SAGE publications, 2012. [Google Scholar]
- 47. Dolan P, Hallsworth M, Halpern D, et al. Influencing behaviour: The mindspace way. J Econ Psychol 2012;33:264–77. 10.1016/j.joep.2011.10.009 [DOI] [Google Scholar]
- 48. Kolb DA, Fry R. Toward an applied theory of experiential learning : Cooper C, Theories of Group Process. London: John Wiley, 1975. [Google Scholar]
- 49. Schön DA. The reflective practitioner: How professionals think in action. New York: Basic Books, 1983. [Google Scholar]
- 50. Pedler M, Burgoyne J, Boydell T. The Learning Company. A strategy for sustainable development. London: McGraw-Hill, 1996. [Google Scholar]
- 51. Mezirow J. A critical theory of adult learning and education. Adult Educ 1981;32:3–24. 10.1177/074171368103200101 [DOI] [Google Scholar]
- 52. Sandars J. The use of reflection in medical education: AMEE Guide No. 44. Med Teach 2009;31:685–95. 10.1080/01421590903050374 [DOI] [PubMed] [Google Scholar]
- 53. Nonaka I, von Krogh G. Perspective—Tacit Knowledge and Knowledge Conversion: Controversy and Advancement in Organizational Knowledge Creation Theory. Organization Science 2009;20:635–52. 10.1287/orsc.1080.0412 [DOI] [Google Scholar]
- 54. Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84:191–215. 10.1037/0033-295X.84.2.191 [DOI] [PubMed] [Google Scholar]
- 55. Aronson L. Twelve tips for teaching reflection at all levels of medical education. Med Teach 2011;33:200–5. 10.3109/0142159X.2010.507714 [DOI] [PubMed] [Google Scholar]
- 56. Broadwell MM. Teaching for learning (XVI). The Gospel Guardian. 1969;20 http://www.wordsfitlyspoken.org/gospel_guardian/v20/v20n41p1-3a.html [Google Scholar]
- 57. Dewey J. How we think: A restatement of the relation of reflective thinking to the educative process. Boston: D.C. Heath and Company, 1933. [Google Scholar]
- 58. General Medical Council. The Reflective Practitioner. Guidance for doctors and medical students. London: Academy of Medical Royal Colleges, the UK Conference of Postgraduate Medical Deans, the General Medical Council, and the Medical Schools Council. GMC, 2018. https://www.gmc-uk.org/education/standards-guidance-and-curricula/guidance/the-reflective-practitioner-guidance-for-doctors-and-medical-students. [Google Scholar]
- 59. Winkel AF, Yingling S, Jones AA, et al. Reflection as a Learning Tool in Graduate Medical Education: A Systematic Review. J Grad Med Educ 2017;9:430–9. 10.4300/JGME-D-16-00500.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ferguson J, Wakeling J, Bowie P. Factors influencing the effectiveness of multisource feedback in improving the professional practice of medical doctors: a systematic review. BMC Med Educ 2014;14:76 10.1186/1472-6920-14-76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Boiko O, Campbell JL, Elmore N, et al. The role of patient experience surveys in quality assurance and improvement: a focus group study in English general practice. Health Expect 2015;18:1982–94. 10.1111/hex.12298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kappes A, Faber NS, Kahane G, et al. Concern for Others Leads to Vicarious Optimism. Psychol Sci 2018;29:379–89. 10.1177/0956797617737129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Farrington C, Burt J, Boiko O, et al. Doctors' engagements with patient experience surveys in primary and secondary care: a qualitative study. Health Expect 2017;20:385–94. 10.1111/hex.12465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Garrett N, González-Garzón AM, Foulkes L, et al. Updating Beliefs under Perceived Threat. J Neurosci 2018;38:7901–11. 10.1523/JNEUROSCI.0716-18.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Ehrlinger J, Johnson K, Banner M, et al. Why the Unskilled Are Unaware: Further Explorations of (Absent) Self-Insight Among the Incompetent. Organ Behav Hum Decis Process 2008;105:98–121. 10.1016/j.obhdp.2007.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. The Bawa-Garba case. BMJ https://www.bmj.com/bawa-garba [Accessed Feb 2019]. [Google Scholar]
- 67. Sanson-Fisher R, Hobden B, Waller A, et al. Methodological quality of teaching communication skills to undergraduate medical students: a mapping review. BMC Med Educ 2018;18:151 10.1186/s12909-018-1265-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Papageorgiou A, Loke YK, Fromage M. Communication skills training for mental health professionals working with people with severe mental illness. Cochrane Database Syst Rev 2017;6:CD010006 10.1002/14651858.CD010006.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Ditton-Phare P, Loughland C, Duvivier R, et al. Communication skills in the training of psychiatrists: A systematic review of current approaches. Aust N Z J Psychiatry 2017;51:675–92. 10.1177/0004867417707820 [DOI] [PubMed] [Google Scholar]
- 70. Moore PM, Rivera Mercado S, Grez Artigues M, et al. Communication skills training for healthcare professionals working with people who have cancer. Cochrane Database Syst Rev 2013;3:CD003751 10.1002/14651858.CD003751.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Brighton LJ, Koffman J, Hawkins A, et al. A Systematic Review of End-of-Life Care Communication Skills Training for Generalist Palliative Care Providers: Research Quality and Reporting Guidance. J Pain Symptom Manage 2017;54:417–25. 10.1016/j.jpainsymman.2017.04.008 [DOI] [PubMed] [Google Scholar]
- 72. Oladeru OA, Hamadu M, Cleary PD, et al. House staff communication training and patient experience scores. J Patient Exp 2017;4:28–36. 10.1177/2374373517694533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Chung HO, Oczkowski SJ, Hanvey L, et al. Educational interventions to train healthcare professionals in end-of-life communication: a systematic review and meta-analysis. BMC Med Educ 2016;16:131 10.1186/s12909-016-0653-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Curtis JR, Back AL, Ford DW, et al. Effect of communication skills training for residents and nurse practitioners on quality of communication with patients with serious illness: a randomized trial. JAMA 2013;310:2271–81. 10.1001/jama.2013.282081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Haynes AB, Edmondson L, Lipsitz SR, et al. Mortality Trends After a Voluntary Checklist-based Surgical Safety Collaborative. Ann Surg 2017;266:923–9. 10.1097/SLA.0000000000002249 [DOI] [PubMed] [Google Scholar]
- 76. Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract 2013;63:e76–84. 10.3399/bjgp13X660814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Kelm Z, Womer J, Walter JK, et al. Interventions to cultivate physician empathy: a systematic review. BMC Med Educ 2014;14:219 10.1186/1472-6920-14-219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Dwamena F, Holmes-Rovner M, Gaulden CM, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev 2012;12:CD003267 10.1002/14651858.CD003267.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Mazzi MA, Rimondini M, Deveugele M, et al. What do people appreciate in physicians' communication? An international study with focus groups using videotaped medical consultations. Health Expect 2015;18:1215–26. 10.1111/hex.12097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Agledahl KM, Gulbrandsen P, Førde R, et al. Courteous but not curious: how doctors' politeness masks their existential neglect. A qualitative study of video-recorded patient consultations. J Med Ethics 2011;37:650–4. 10.1136/jme.2010.041988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Beach MC, Sugarman J, Johnson RL, et al. Do patients treated with dignity report higher satisfaction, adherence, and receipt of preventive care? Ann Fam Med 2005;3:331–8. 10.1370/afm.328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Laganá L, Gavrilova L, Carter DB, et al. A Randomized Controlled Study on the Effects of a Documentary on Students' Empathy and Attitudes towards Older Adults. Psychol Cogn Sci 2017;3:79–88. 10.17140/PCSOJ-3-127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Nelson SW, Germann CA, MacVane CZ, et al. Intern as Patient: A Patient Experience Simulation to Cultivate Empathy in Emergency Medicine Residents. West J Emerg Med 2018;19:41–8. 10.5811/westjem.2017.11.35198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Pollak KI, Alexander SC, Tulsky JA, et al. Physician empathy and listening: associations with patient satisfaction and autonomy. J Am Board Fam Med 2011;24:665–72. 10.3122/jabfm.2011.06.110025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Buckman R, Tulsky JA, Rodin G. Empathic responses in clinical practice: intuition or tuition? CMAJ 2011;183:569–71. 10.1503/cmaj.090113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Amutio-Kareaga A, García-Campayo J, Delgado LC, et al. Improving Communication between Physicians and Their Patients through Mindfulness and Compassion-Based Strategies: A Narrative Review. J Clin Med 2017;6:33 10.3390/jcm6030033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Kiosses VN, Karathanos VT, Tatsioni A. Empathy promoting interventions for health professionals: a systematic review of RCTs. J Compassionate Health Care 2016;3:7 10.1186/s40639-016-0024-9 [DOI] [Google Scholar]
- 88. Empathy: The Human Connection to Patient Care. https://www.youtube.com/watch?v=cDDWvj_q-o8 [Accessed Feb 2019].
- 89. TEDxMaastricht - Fred Lee - "Patient Satisfaction or Patient Experience?". https://www.youtube.com/watch?v=tylvc9dY400 [Accessed Feb 2019].
- 90. Say This, Not That: Patient Experience Video. Eastern Idaho Regional Medical Center. https://www.youtube.com/watch?v=r842Ylpa-nQ [Accessed Feb 2019].
- 91. Moore GF, Audrey S, Barker M, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350:h1258 10.1136/bmj.h1258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Wenger E. Communities of Practice: A brief introduction: STEP Leadership Workshop, University of Oregon, 2011. https://scholarsbank.uoregon.edu/xmlui/handle/1794/11736 [Google Scholar]
- 93. Li LC, Grimshaw JM, Nielsen C, et al. Evolution of Wenger’s concept of community of practice. Implement Sci 2009;4:11 10.1186/1748-5908-4-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Dixon-Woods M, Leslie M, Bion J, et al. What counts? An ethnographic study of infection data reported to a patient safety program. Milbank Q 2012;90:548–91. 10.1111/j.1468-0009.2012.00674.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Dixon-Woods M, Leslie M, Tarrant C, et al. Explaining Matching Michigan: an ethnographic study of a patient safety program. Implement Sci 2013;8:70 10.1186/1748-5908-8-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Wall RJ, Engelberg RA, Downey L, et al. Refinement, scoring, and validation of the Family Satisfaction in the Intensive Care Unit (FS-ICU) survey. Crit Care Med 2007;35:271–9. 10.1097/01.CCM.0000251122.15053.50 [DOI] [PubMed] [Google Scholar]
- 97. Wright SE, Walmsley E, Harvey SE, et al. Family-Reported Experiences Evaluation (FREE) study: a mixed-methods study to evaluate families’ satisfaction with adult critical care services in the NHS. Health Services and Delivery Research 2015;3:1–250. 10.3310/hsdr03450 [DOI] [PubMed] [Google Scholar]
- 98. Harrison DA, Ferrando-Vivas P, Wright SE, et al. Psychometric assessment of the Family Satisfaction in the Intensive Care Unit questionnaire in the United Kingdom. J Crit Care 2017;38:346–50. 10.1016/j.jcrc.2016.10.023 [DOI] [PubMed] [Google Scholar]
- 99. NHS Staff Friends & Family Test. https://www.england.nhs.uk/fft/staff-fft/ [Accessed Feb 2019].
- 100. Hospital Survey on Patient Safety Culture. https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/patientsafetyculture/hospital/resources/hospscanform.pdf [Accessed Feb 2019].
- 101. Teamwork and Safety Climate Survey. https://med.uth.edu/chqs/files/2012/05/Survey-SAQ-Teamwork-Safety-Climate-.pdf [Accessed Feb 2019].
- 102. General Medical Council Trainee Survey. https://www.gmc-uk.org/education/how-we-quality-assure/national-training-surveys/national-training-surveys-doctors-in-training [Accessed Feb 2019].
- 103. Grant AM, Franklin J, Langford P. The self-reflection and insight scale: a new measure of private self-consciousness. Soc Behav Pers 2002;30:821–35. 10.2224/sbp.2002.30.8.821 [DOI] [Google Scholar]
- 104. Glaser B, Strauss A. The discovery of grounded theory. Hawthorne, NY: Aldine Publishing Company, 1967. [Google Scholar]
- 105. Batalden M, Batalden P, Margolis P, et al. Coproduction of healthcare service. BMJ Qual Saf 2016;25:509–17. 10.1136/bmjqs-2015-004315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Scott J, Heavey E, Waring J, et al. Healthcare professional and patient codesign and validation of a mechanism for service users to feedback patient safety experiences following a care transfer: a qualitative study. BMJ Open 2016;6:e011222 10.1136/bmjopen-2016-011222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Better Services by Design. http://www.bsbd.org.uk/double-diamond-design-process/ [Accessed Feb 2019].
- 108. Langley J, Wolstenholme D, Cooke J. ’Collective making' as knowledge mobilisation: the contribution of participatory design in the co-creation of knowledge in healthcare. BMC Health Serv Res 2018;18:585 10.1186/s12913-018-3397-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.