Abstract
Introduction
Most mothers feel an immediate, strong emotional bond with their newborn. On a neurobiological level, this is accompanied with the activation of the brain reward systems, including the striatum. However, approximately 10% of all mothers report difficulties to bond emotionally with their infant and display impaired reward responses to the interaction with their infant which might have long-term negative effects for the child’s development. As previous studies suggest that activation of the striatal reward system can be regulated through functional MRI (fMRI)-based neurofeedback (NFB), we have designed and investigate fMRI-NFB training to treat maternal bonding difficulties.
Methods and analysis
In the planned trial, mothers will be presented pictures of their infant and real-time fMRI (rtfMRI), peripheral measures, neural, endocrine, psychophysiological and behavioural measures will be assessed. Mothers with bonding difficulties (n=68) will be randomised to one of two double-blind intervention groups at 4–6 months postpartum. They will participate in three repeated NFB training sessions with rtfMRI-NFB training to increase activation of (a) the ventral striatum or (b) the anterior cingulate. Interview data and real-time mother–infant interaction behaviour pre-intervention, post-intervention and at follow-up will serve as clinical outcome measures.
Ethics and dissemination
Study procedures are in line with the recommendations of the World Medical Association (revised Declaration of Helsinki) and were approved by the Ethics Committee of the Medical Faculty, s-450/2017, Heidelberg University. All participants will provide written informed consent after receiving a detailed oral and written explanation of all procedures and can withdraw their consent at any time without negative consequence. Results will be internationally published and disseminated, to further the discussion on non-pharmacological treatment options in complex mental disorders.
Trial registration number
DRKS00014570; Pre-results.
Keywords: mother–infant bonding, maternal bonding difficulties, ventral striatum, oxytocin, dopamine
Strengths and limitations of this study.
The novelty of used methods allows the investigation of the effect of real-time functional MRI (rtfMRI) neurofeedback (NFB) on maternal bonding.
The study investigates the ability of rtfMRI-NFB to upregulate brain activity in correlation with behavioural and biopsychological markers.
The simultaneous investigation of two brain regions as well as the presence of a control group proposed in the methods of this protocol enables a comparative analysis of the benefits of the rtfMRI training, as well as increasing clarity regarding the role of differential brain regions in social reward.
The proposed method, through its longitudinal design with follow-up measures, will help to evidence how NFB training brings about behavioural change, in turn allowing for better understanding of the potential applications, predictive neural signatures and participant criteria crucial for the success of rtfMRI.
Due to the statistical co-occurrence of maternal bonding difficulties and postpartum depression and the similar pattern of muted reward responses in both instances, the explanatory power of the results of the rtfMRI-NFB intervention may be confounded.
Introduction
Neurobiological, emotional and behavioural aspects of maternal bonding
The parental bond is the first social bond that infants experience in life. Usually, it is the mother who serves as the infant’s immediate and most central social interaction partner. Maternal bonding is reflective of the first emotional bond that a mother gradually develops with her infant, within the first weeks postpartum, and is characterised by positive feelings, emotional warmth and affection towards the infant.1 In the eyes of some researchers, maternal bonding represents one of the most important psychological processes that gradually enfold after birth2 and is a significant and central aspect of the emerging relationship between mother and infant.3
The initial period after birth is also known as the ‘Baby-Honeymoon’, a state of euphoria and happiness fuelled by the desire to constantly be near and to ‘fall in love’ with the infant, which allows the mother to take on the challenges of the adaptation to parenthood. In this way, maternal bonding also fulfils a biological function by ensuring the care for and subsequent survival of the newborn.4 On the behavioural level, maternal bonding emerges through touch, eye-contact, use of ‘motherese’ and the smiling at or caressing of the infant.5 Maternal bonding can therefore said to be expressed in the caregiving behaviours of the parent, in their focus on and high level of sensitivity to the needs of the infant.6 On the other hand, maternal bonding is also formed in the mother’s emotions and thoughts about the infant and in the mental representations of motherhood that the mother holds.7
The strength of maternal bonding can also be demonstrated on a neurobiological level.8 Central structures such as the striatum, ventral tegmental area, amygdala, septum and hypothalamus are involved in affiliative behaviour, together with a combination of neurotransmitters and modulators such as dopamine and oxytocin.9 10 For affiliative traits, it has been proposed that those are mediated by dopaminergic projections from the ventral tegmental area and endogenous opioids in the hypothalamus with projections to the septum, especially during physical contact11 that underlie rewarding feelings of affiliation.
One finding of central relevance to maternal bonding in particular is that mothers who report a good emotional bonding to their infant show increased reward-related activation in dopaminergic brain regions (the nucleus accumbens in the ventral striatum) in response to infant stimuli.12 These effects are particularly evident in the mother, in comparison to other caregivers, and have been assumed to be reinforced through the hormonal changes that accompany both birth and breastfeeding behaviours.13 14
However, the bonding process is not always successful15 16 and impaired maternal bonding can lead to avoidance or ambivalent emotions or behaviour in the mother. Impaired bonding can result not only in a lack of affection but also, in extreme cases, in the immediate rejection or neglect of the infant, as well as the possible presence of hostility or aggressive impulses.2 7 Although postpartum bonding difficulties also occur in psychologically healthy mothers, they are observed particularly in the context of postpartum depression.17 18 In a representative German sample, 6.4% of psychologically healthy mothers reported difficulties in establishing emotional bonding with their infant. In depressed mothers, the rate of prevalence is significantly higher at 17%–29%.19 Furthermore, it has been shown that even subclinical depressive symptoms may negatively affect the developing bonding during the first months postpartum.6
Depression during the postpartum period itself is generally characterised by loss of interest or joylessness, insomnia, feelings of guilt, difficulties concentrating and, in severe cases, suicidal tendencies. Intense feelings and self-blame about being a bad mother are also often reported.20 On a neurobiological level, postpartum depression relates to a reduced level of reactivity in the striatal reward system, for example in the putamen,21 but also the amygdala network22 together with endocrine changes in the serotonin and steroid systems.23 Studies show that in particular the mother–infant relationship,24 25 as well as the actual mother–infant interaction,26 both short term and long term can be impaired by peripartum and postpartum depression.24 27 Results of a recent study suggest that the link between maternal depressive symptoms at 2 months postpartum and maternal report about interaction with the infant at 6 months was mediated by maternal feelings of attachment.28 The present study focuses on bonding impairments, rather than postpartum depression, although there will be inevitable co-occurrence in the participant sample.
Research indicates that experiences and interaction in the ‘sensitive’ postpartum period have long-term consequences for the cognitive as well as socio-emotional development in children.24 29 Animal studies have also demonstrated that positive caring behaviours of the mother positively influence offspring brain development and long-term stress-coping behaviours even in the next generation via epigenetic changes.30 Conversely, in humans, decreased maternal bonding can result in higher rates of self-directed affect regulation strategies and increased stress reactivity31 of the infant, as well as variable self-comfort behaviours, moderated by the infant’s gender and age.31 Research also indicates that restrained (distant) maternal behaviour can have far-reaching negative consequences for self-regulation, social behaviour and stress management in the infant24 29 even into adulthood with potential influences on own parenting behaviour.32 Furthermore, the association between maternal depression, anxiety disorders and stress reactivity with changes in the hypothalamic–pituitary– adrenocortical axis (HPA axis) is well documented.33 Indeed, recent studies indicate that infant exposure to maternal mental disorders can increase infant baseline cortisol levels, as the main outcome of the HPA axis, in case of maternal depression and increase infant cortisol reactivity in cases of maternal anxiety.34 In a lower-income setting, exposure to variable intensities of maternal depression demonstrated a U-shaped response curve in infant cortisol reactivity levels in the context of immunisation. Those with exposure to moderate-maternal depression levels demonstrated the lowest cortisol reactivity during immunisation.35 The importance of the influence of maternal interaction behaviours themselves is also clear. One particular study demonstrates, for example, that maternal sensitivity during the interaction with their infant has a moderating influence between maternal mental health during pregnancy and infant salivary cortisol levels.36 Given data on the transgenerational transmission of maternal care via epigenetics,37 both in maternal bonding38–40 and caregiving behaviours,41 the importance of effective treatment and intervention plans is evident.
Current inpatient and outpatient mother–infant therapies, established in the context of postpartum mental disorders, focus not only on the disorder-specific treatment but also on specific elements for the promotion of the mother–infant relationship (eg, baby massage and video feedback methods). Video feedback interventions have been shown to have a positive influence on mother–infant interaction42 43 as well as the maternal self-efficacy in interacting and coping with the infant.44 45 To our knowledge, maternal bonding has thus far only been recorded as an outcome variable in one study using video feedback invention.46 This intervention demonstrated improvements in maternal bonding; however, the participant pool only included mentally healthy women without postpartum bonding problems. Thus, interventions focussing on maternal bonding in women experiencing difficulties forming an emotional bond to their infant are urgently needed. Presently, such interventions or findings, directly relating maternal bonding difficulties and their effects on the infant’s stress reactivity in either biological or behavioural domains, are still lacking and in particular non-pharmacological treatment concepts would substantially broaden the treatment options for affected mothers and their infants.
Reward learning in depression and its relation to maternal bonding difficulties
On a neural level, the dopamine-mediated reward system (specifically the ventral striatum and the nucleus accumbens) is crucial to the rewarding aspects of social interaction.47 48 The ventral striatum also appears to be specifically involved in learning rewarding stimuli, where high neural activation, correlated with the blood-oxygen-level-dependent '(BOLD) response’ in the functional MRI (fMRI), is accompanied by an increased dopaminergic response.47 As part of the learning process, this reward activation is first triggered by primary enhancers, such as glucose, and over the course of the learning process transfers to secondary enhancers, such as food or money. In humans, from early in life, repeated positive social experiences can be seen as very strong reward and provided the basis for the much discussed ‘social brain hypothesis’, in brain research.49 50
Images of happy children are generally perceived as positive by healthy individuals and activate the striatal areas of the brain.51 Psychologically healthy mothers also show a differential neural activation response to visual stimuli of happy children, as compared with stimuli of more ambiguous facial expressions of children. Expressions of joy activated the right limbic and paralimbic areas, compared to ambiguous expressions that correlated to activity in the left higher cognitive and motor areas that are often linked to cognitive effort.52 Consequently, positively reinforcing activities that lead to such activation, that is, positive social interaction, are likely to be subsequently performed more frequently. In the presence of depressive symptoms, however, such neural activation (ie, activation in striatal and limbic networks) seems to be diminished during positive social interactions, these activities are therefore perceived as less rewarding53 54 and diminish the motivation for social contact. Mothers with depressive symptoms demonstrated reduced activation in subcortical and cortical limbic regions (amygdala, cingulate) and cortical regions involved in emotion regulation (including the frontal cortex, insula, anterior cingulate), in line with symptomology of diminished capacities to experience joy and to downregulate anger, anxiety or worry.21 22 55 Notably, mothers with postpartum depression show a reduced activation in striatal reward areas in response to stimuli of their own children.21 22 55
On a neuroendocrine level, basic research suggests that in rodents social-interaction-related reward is associated with receptor activation for the neuropeptide oxytocin in the nucleus accumbens.56 Initial data in humans indicate that methylation of the oxytocin receptor gene is associated with attachment in different phases of the individual’s lifespan57 and higher methylation is associated with postpartum depression.58 Antidepressant treatment, in turn, is assumed to lower methylation.59 This may explain, on a neurobiological level, the correlation between postpartum depression and maternal bonding difficulties.60 However, no contemporary intervention has yet focused on the perception of the mother–infant interaction in terms of reward and involved oxytocin-related outcomes as possible evaluation criteria.
rtfMRI-NFB as a treatment method
Neurofeedback (NFB) is a novel method which, through the visualisation of real-time brain activation, allows an individual to consciously regulate one’s own brain activation. While it is well established that mental strategies modulate brain activation as measured by fMRI BOLD signal, NFB asks participants to modulate activation in prescribed regions or even networks of their brain by their own volition and in response to the immediate feedback/visualisation of the related brain activation patterns.61 Thus, volunteers can learn to regulate the activation of a previously defined brain region (see Sulzer et al 62 for a review). NFB interventions have previously often used electroencephalography and other electrophysiological methods to visualise and modulate activation in higher cortical areas. However, smaller and deeper areas of the limbic and reward system can be imaged primarily with high-resolution MRI. One previous study has proven that healthy volunteers can be trained to voluntarily increase their brain activation patterns that have been classified for affiliative emotions in the same individual subject using voxel pattern analyses.63 From a therapeutic point of view, the targeted modulation of specific brain areas and associated circuits via NFB should be associated with the improvement of mental symptoms.
In initial clinical pilot studies, for example, patients with borderline personality disorder, anxiety or obsessive-compulsive disorder have shown the ability to downregulate activation in the insula or the hyperactive amygdala in response to stress-related stimuli.64–66 Similarly, high-risk alcohol consumers learned to downregulate the reward-related activation of alcohol-related stimuli.67 In patients with post-traumatic stress disorder, the changes in brain connectivity after fMRI-NFB correlate with the reduction of symptoms.68 Based on the previously articulated and evidenced notion of the psychobiological mechanisms underlying attachment and bonding as goal oriented and reward drive,69 the proposed study looks to investigate whether specific activation of the ventral striatum can be voluntarily increased through training in the context of maternal bonding. Indeed, in previous research, patients with major depressive disorder or schizophrenia were successfully trained to increase the activation of the hypoactive amygdala and the anterior cingulum in conjunction with positive stimuli.70 71 Therefore, in line with the current understanding and treatment of mental illnesses, rtfMRI-NFB represents a promising new intervention method for complex mental processes. Particularly important for understanding the potential of rtfMRI interventions is the transfer of the modulation of the BOLD signal towards behavioural changes61 which allows the value of this intervention form in a clinical setting to be distilled.
The planned trial
In the planned double-blind randomised intervention trial (the ‘Neurofeedback for Mothers with Postpartum Bonding Difficulties Study’, ’NeMo-Study'), three central points will be addressed.
Women with postpartum bonding difficulties (including women with postpartum depression) will be compared with healthy unaffected women in terms of reward-related brain activation to pictures showing their own infant and control stimuli. It is hypothesised that women with bonding difficulties show less brain response in the reward-related areas (ventral striatum) compared with the control group.
The clinical group will then undergo a regiment of NFB training. Participants will learn to consciously increase the activation of reward-associated brain areas (specifically the ventral striatum), or a control region (anterior cingulate cortex, ACC), during the presentation of images of their own infant. For ethical reasons, an active control treatment was chosen rather than joke or non-feedback. The activation of the central nervous dopamine system via the striatum is hypothesised to improve bonding motivation and social interaction behaviour. The coupling of infant stimuli to the central nervous reward activation should make it easier for these women to feel more joy in the real interaction61 with their infant post-training and to be more attentive and more sensitive in their interactions. Training of the dorsal/rostral ACC with a rather unspecific role in emotion regulation, such as for example, in cognitive reappraisal72 or response inhibition73 may have general beneficial effects as shown in another NFB study70 but also indirectly influence parental affect regulation. However, the more specific striatal feedback based on the rewarding aspects of the mother–child interaction are assumed to have stronger effects.
Effects of the NFB training will be related to the changes in behaviourally coded mother–infant interaction, maternal bonding quality and diagnostics, and epigenetic oxytocin receptor alterations, as assessed from peripheral blood. It is hypothesised that following the ventral striatum intervention, interaction, maternal bonding and epigenetic markers will approximate the values of the healthy control group.
Thus, the study will address reward-related processes in impaired maternal bonding, observable changes on a behavioural and neuroendocrine level post-training—important steps in illustrating the validity of rtfMRI-NFB as an intervention method.61 The proposed study is therefore well placed to produce a wealth of valuable and informative data, regarding the potential scope of rtfMRI as a non-pharmacological intervention to young mothers.
Methods and analysis
Design overview
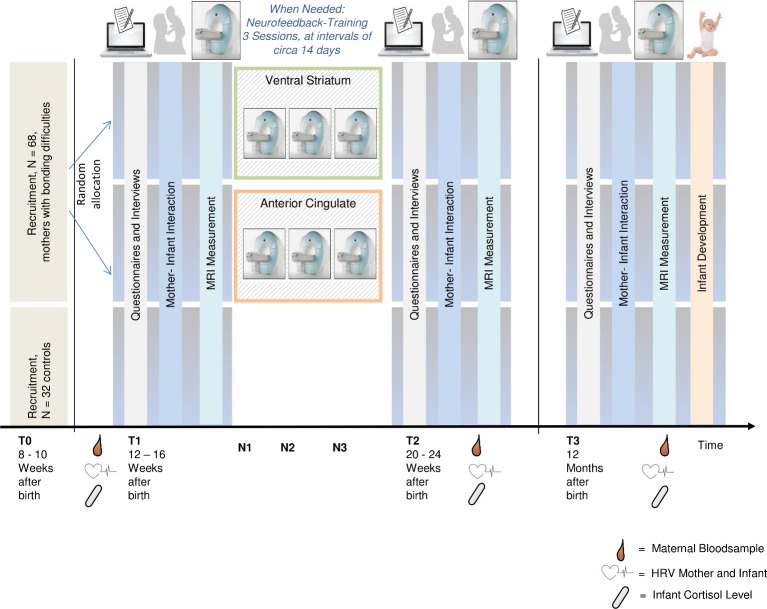
To investigate points (1)–(3) (above), a controlled longitudinal study with randomised allocation of the two intervention groups to one of two anatomically defined regionally targeted areas in the NFB training will be employed. The two intervention groups will consist of mothers with identified maternal bonding difficulties, whereas the control group will consist of psychologically healthy mothers without bonding difficulties. The intervention groups will receive three NFB training sessions at intervals of approximately 14 days. Changes in maternal behaviours during mother–infant interaction, measured using standardised coding of behavioural observations, will be assessed as the primary outcome measure. Possible alterations in oxytocin receptor methylation and gene expression will serve as secondary outcome measures. See figure 1 for overview of study design and timeline.
Figure 1.
Overview of study design. HRV, heart rate variability.
Participant eligibility and recruitment
Eligible participants
Intervention Group: Mothers, who report postpartum bonding difficulties, may present with a wide range of depressive symptoms.
Control Group: Psychologically healthy mothers with intact bonding to their infant.
Exclusion criteria for all groups
Mothers: acute suicidality, bipolar or schizophrenic disorders, diagnosed dementia or substance abuse or substance dependency. Necessarily fMRI exclusion criteria also apply.
Infants: multiple birth infants, preterm birth, confirmed physical or developmental disorders, which make participation impossible or unwise.
Participant recruitment
Participants will be recruited both online and by flyers disseminated through midwives, gynaecologists, paediatricians, in pharmacies and in maternity hospitals as well as mothering forums or self-help groups (eg, ‘Shadow and Light’) and registration offices. They receive thorough information about the study procedures both orally and in written form. The volunteer recruitment structure of the study makes it possible that given the intense feelings of self-blame symptomatology of the often co-occurring postpartum depression,18 those most severely affected may not volunteer for the study. This limitation will be addressed via carefully worded and emphatic recruitment materials and processes.
Patient and public involvement
Patients and the general public were not involved in the design or implementation of this study. However, the participants are asked to report on the cognitive strategies they adopted during their rtfMRI-NFB sessions and their subjective success with those strategies. These findings may inform future formulations of patient based NFB interventions.
The results of this study will not be disseminated to the participants directly but will be openly accessible online.
Screening assessment and group allocation
Screening assessment
For inclusion in the study, all potential participants will be screened (T0) prior to inclusion.
Random group assignment procedure
True random assignment to the two clinical intervention groups or the control group cannot occur due to the quasi-experimental nature of the design: The mothers are assigned to being clinical or control based on the quality of their postpartum bonding to their infant. Inclusion as part of the clinical intervention group is based on the categorical assessment of impaired maternal bonding using an in-depth interview based on the proposed criteria by Brockington et al 19 and asked during the clinical interview. Bonding assessment is further elaborated by the use of additional questionnaires exploring bonding impairment, such as the Postpartum Bonding Questionnaire 16, which holds an internal consistency of Cronbach’s α=0.085.5 This approach additionally allows for the dimensional assessment of maternal bonding impairments.
Within the intervention group, participants will be completely randomly and automatically assigned to one of the following two conditions: NFB of the right ventral striatum (clinical intervention group I) or NFB of the right ACC (clinical intervention group II). This randomisation is based on the order of inclusion into the study and pre-assigned lists that are double-blind in nature using non-public lists made by a colleague not involved in assessments and analyses. During all three intervention sessions, participants will be trained to modulate activation of the same pre-defined brain region (right ventral striatum or right ACC) based on the functional tasks during T1. Blinding of the treatment group will be revealed after the analyses at group level.
Power analysis and size estimation
The programme G-Power V.3.1.9.274 was used, in order to calculate the required sample size. To test the hypotheses mentioned above, a total of approximately n=100 cases is estimated.
To perform a simple group comparison of maternal sensitivity between two treatment groups with a middle to large effect size (d=0.78)43 with a power of 90% and an alpha-error threshold of p=0.05, a minimum group size of n=30 for each clinical intervention group is required (I, NFB of the ventral striatum, II, NFB of the ACC). Assuming a drop-out rate of approximately 10%, an experimental sample of n=100 will be aimed for in the projected study. With a repeated measures analyses and the T3 (follow-up) measurement, the power is improved, which makes it possible to observe even medium effects with this planned sample.
n=68 mothers with postpartum bonding difficulties will be included in the intervention (n=34 to NFB region I ventral striatum, n=34 to NFB region II ACC). Mental disorders, and especially postpartum depressive symptomatology, are measured in a multi-dimensional fashion through a structured clinical interview and a validated peripartum period questionnaire. Variability in depressive symptoms, ranging from none to moderate symptom load is sought, thus allowing for appropriate and adequate statistical analysis of this covariate factor. As a control group, n=32 psychologically healthy women with a good bond with their infant will be recruited.
Pre-intervention, post-intervention and follow-up assessments (T1, T2 and T3)
Before (T1) and after the training (T2), participants will perform an extensive battery of diagnostic assessments characterising the clinical aspects of bonding, including the instructed mother-infant–interaction in the Face-To-Face-Still-Face (FFSF) Paradigm.75 76 A baseline fMRI session will assess the sensitivity of both the reward system and the limbic system using established fMRI tasks and blood samples will be collected for analysing hormonal and (epi-)genetic markers. After the end of the last NFB training a post-intervention measurement (T2) and a 12 months a follow-up (T3) will be performed using the same methods as at T1. At T3, mothers and infants will be instructed to freely play77 and videotaped. Age-specific markers of the infant’s development will be coded using a standardised developmental test.78 (Refer to figure 1 for timeline clarification.)
This combination of assessments allows for a comprehensive understanding of maternal bonding and behaviour on a neural, neuroendocrine, epigenetic and behavioural level.
The primary behavioural outcome measures include the quality of maternal–infant interaction behaviour (composite scores of maternal and dyadic behaviour) while on the neuronal level, we assess the BOLD response to positive stimuli of the child as primary outcome measure. Physiological, endocrine and genetic markers serve as secondary outcomes.
See table 1 for further details on the assessments and scheduling of measure collection.
Table 1.
Schedule of measures used the in study
| Measure | Citation | M. | F. | I. | T0 | T1 | N | T2 | T3 |
| Mother and infant: | |||||||||
| Mother–infant interaction (FFSF) | 75 76 | X | X | X | X | ||||
| Free-play situation and limit setting | 77 | X | X | X | |||||
| Interviews: | |||||||||
| Diagnostic interview for mental disorders | 92 | X | X | X | X | ||||
| Interview for postpartum bonding difficulties | X | X | X | X | |||||
| Attachment style interview | 93 | X | X | X | |||||
| Questionnaires: | |||||||||
| Postpartum Bonding Questionnaire 16 R | 5 | X | X | X | X | X | |||
| Edinburgh Postnatal Depression Scale | 94 | X | X | X | X | X | |||
| Agoraphobic Cognitions Questionnaire, Body Sensations Questionnaire, and Mobility Inventory | 95 | X | X | X | X | X | |||
| Maternal Self-Confidence Scale | 96 | X | X | X | X | X | |||
| Prenatal Emotional Stress Index | 17 | X | X | X | |||||
| Parental Bonding Instrument | 97 | X | X | X | |||||
| German version of the EMBU questionnaire regarding remembered parenting behaviour | 98 | X | X | X | |||||
| Experiences in Close Relationships-Revised | 99 | X | X | X | |||||
| Social Support Questionnaire | 100 | X | X | X | X | X | |||
| Personality Inventory-DSM 5 Short Form | 101 | X | X | X | |||||
| Childhood Trauma Questionnaire | 102 | X | X | X | |||||
| Partnership Questionnaire | 103 | X | X | X | X | X | |||
| Dyadic Coping Inventory | 104 | X | X | X | X | X | |||
| Parenting Stress Inventory | 105 | X | X | X | X | X | |||
| Vulnerable Attachment Style Questionnaire | 106 | X | X | X | |||||
| Edinburgh Handedness Questionnaire | 107 | X | X | ||||||
| Infant: | |||||||||
| Infant Behaviour Questionnaire | 108 | X | X | X | X | ||||
| Development Assessment: Infant | |||||||||
| Bayley’s Infant Development Scale III | 78 | X | X | ||||||
| Physiological measures | |||||||||
| Infant saliva sample | X | X | X | X | |||||
| Mother blood sample | X | X | X | X | |||||
| Neurofeedback training | X | X | |||||||
| Reward task | 83 | X | X | X | X | ||||
| Emotional go-no-go | 73 | X | X | X | X | ||||
| Passive viewing task | 84 | X | X | X | X |
M., mother response; F., father response; I., infant response; T0, screening assessment; T1, baseline assessment; N, neurofeedback sessions; T2, post-assessment; T3, follow-up.
DSM-5, Diagnostic and Statistical Manual of Mental Disorders, EMBU, Egna Minnen Beträffande Uppfostran (Own Memories of Child Rearing Experiences); Fifth Edition; FFSF, Face-to-Face-Still-Face.
Survey instruments and coding systems used in the study
Detailed description of measures, methods and instruments used
Initial assessments
Baseline assessment
For the baseline testing period (T1), the mothers will be invited to our video laboratory together with their infants. A structured clinical interview according to Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition as well as an interview regarding postpartum bonding difficulties will be carried out. Subsequently, mother–infant interaction will be assessed and videotaped during the FFSF paradigm, a widely used paradigm for evaluating the quality of early parent–infant interaction.75 To determine infant stress reactivity, cortisol and alpha-amylase will be extracted from infant saliva according to standard protocols,79 which is collected before (C1), immediately after (C2), 20 min (C3) and 30 min after the FFSF (C4).
Instructed mother–infant interaction
Mother–infant interaction pre–post-intervention (T1 and T3): The standardised mother–infant interaction before and after the intervention follows the established FFSF paradigm.75 76 It consists of three consecutive instructed 2 min episodes in which the mother, with the infant seated in the baby chair, interacts in accordance with a fixed pattern: First, an initial face-to-face interaction in which the mother is instructed to play with her infant as usual (without the aid of toys and pacifiers). Next, the still-face episode in which the mother has to turn her head aside while silently counting to 10 and then turn back to the infant but not engage in any gestures, facial expressions or vocalisations. Finally, the procedure ends with the reunion episode in which the mother is required to resume face-to-face play with her infant.
Mother–infant interaction follow-up (T4): As the Still-face paradigm can be conducted up to the age of 9 months, mother–infant interaction will be assessed at T4 during a 15 min free-play situation and a subsequent limit setting task. All interaction episodes will be videotaped and coded according to the Coding Interactive Behaviour (CIB) Scales.77 The CIB scales assess parental sensitivity and responsiveness as well as intrusiveness and withdrawal via composite scores.80
Psychobiological measurements
Epigenetic information on the oxytocin system and cortisol/alpha-amylase in saliva
Maternal blood samples are taken to examine the endogenous oxytocin level, gonadal hormones and epigenetic parameters of the oxytocin gene and oxytocin receptor gene. For the endocrine investigation of the stress hormone cortisol, painless saliva samples are taken from the infants directly before, immediately after, 20 and 30 min after the mother–infant interaction using a saliva probe. An elevation of infant stress reactivity is expected during the interaction, from these elevations the Peak and Recovery will be ascertained. The area under the curve is therefore analysed as a reactivity index81 as is standard practice.82
MRI tasks
Reward task
The task (adapted from Martin-Soelch et al 83) requires participants to perform a spatial working memory task with two levels of cognitive load, differentiated by the number of circles to be remembered. Subjects first see a cue informing them about the potential monetary reward value—high or low. After presentation of the fixation cross, an array of yellow circles (three or seven circles) is displayed followed by the target, a green circle, that is then presented at any position on the screen. The participants must decide whether this circle is in the same position as one of the circles presented previously. In the rewarded condition, a feedback about the win followed by the cumulated amount of earned money appears. Correct responses are reinforced by two different amounts of monetary reward that are counterbalanced with the levels of cognitive load. Incorrect responses on rewarded trials result in no monetary gain. While performing the task, participants rate their mood and stress levels a quarter of the trials.
Emotional go/nogo
The participants are presented with positive and negative expressions of unknown babies, unknown adults as well as un-social control stimuli (geometric figures; a circle, a cross, a diamond and a triangle) over three presentation blocks.
The following factors are systematically manipulated: child versus adult and emotionality of facial expression (positive vs negative). In two blocks, the participants receive instructions to respond by pressing a button as fast as possible to all facial expression except the negative (one block babies, one block adults). In two other blocks, they are instructed to respond as fast as possible to all except the positive (one block babies, one block adults). In the two non-social blocks, the participants should react as fast as possible to all shapes but not to a circle or a diamond.73
Passive viewing task
The participants view previously collected neutral-positive images of partners and their babies in positive and negative affect, with instructions to observe carefully. Unfamiliar men and babies will serve as control stimuli. Viewing images of partners and children leads to the activation of a broad socio-emotional neural network, that is involved with empathy and socio-emotional cognition.21 84
Coding systems used in the study
Coding interactive behaviour
For the evaluation of the mother-infant– interaction over all measurement points, the Coding Interactive Behaviour (CIB) System will be used77. The CIB is a widely used, global rating system for analysing mother–infant interaction. The system uses multiple codes for the infants, parents and dyadic codes that aggregate into meaningful theoretically based constructs (eg, sensitivity, intrusiveness, reciprocity, social engagement, withdrawal). The psychometric characteristics are all well described.85 The mother–infant interaction will be coded by blind and reliable coders who are independent of the current study, 10%–20% of the videos will be double coded for inter-rater reliability.
Infant development diagnostics used in the study
Bayley Scales of Infant and Toddler Development-III
The Bayley Scales of Infant and Toddler Development-III (Bayley-III86 87) assess the development of infants and toddlers between 1 and 42 months of age. The test battery covers the domains of cognition, language, motor, social-emotional and adaptive development using IQ-scaled composite scores. Whereas the first three aspects are assessed by behavioural observation, the latter two utilise questionnaires, with duration ranging between 50 and 90 min.88 The Cognitive Scale assesses sensorimotor development, exploration and manipulation, object relatedness, concept formation and memory. The Language Scale is composed of the two subscales (receptive and expressive communication), testing pre-verbal behaviour, vocabulary development, understanding of morphological markers, social referencing and verbal comprehension and pre-verbal communication, vocabulary development and morpho-syntactic development, respectively. In addition, the Bayley Scales include a Gross- and Fine-Motor Scale, a Social-Emotional Scale and an Adaptive Behaviour Scale. This study focuses on the language and cognitive composite scores due to the rather small proposed sample size.
The Bayley-III indices and subscales demonstrate good internal consistency and good split-half-consistency according to the Spearman-Brown formula.88 Regarding construct validity, a confirmatory factor analysis of the subtests of the Cognitive, Language and Motor Scales supported a three-factor model across all ages. The Bayley-III scales have been normed for German infants and children.89 This method is taken standard internationally, particularly in terms of reviewing developmental delays and planning targeted early interventions. The order of the subtests can be adapted to the needs of the child.
NFB setup
The mothers with bonding difficulties will be randomised to receive one of the two following interventions: (I) NFB for activation of the ventral striatum or (II) NFB for activation of the ACC.
The individual masks for extraction of the NFB value are built after the first level analyses of the reward task and the emotional go/nogo task submitting the peak voxel coordinates in the right ventral striatum and ACC based on the contrasts (reward >baseline) and (faces nogo >faces go) to build 12 mm sphere region of Interests (ROIs) for the striatum and ACC using the marsbar toolbox.90
Participants will partake in NFB training over three sessions at intervals of approximately 14 days (refer to figure 1). At baseline, a high-resolution structural MRI scan and the activation pattern based on the infant-like stimuli will be recorded (using a Tim Trio 3T MRI scanner, Siemens, Erlangen, Germany).
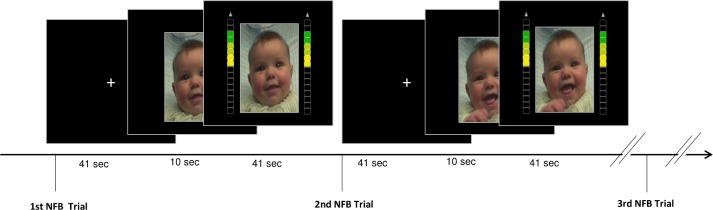
Each intervention session will last approximately 60 min and will begin with a 10 min preparatory structural MRI scan. A 6 min resting state fMRI scan is then conducted to allow a resting baseline to be established and to prepare the NFB setup. Afterwards, three rtfMRI-NFB runs of 9:29 min are conducted. During NFB training, positive and neutral pictures of the participants’ own infant taken from the recorded mother–infant interaction session will be presented together with an on-screen ‘thermometer’ which represents the current intensity of activation in the striatum or ACC and must be upregulated. In each run, six alternating phases of upregulation (~41 s, including a ~10 s initial period without thermometer display) and of rest (observation of a fixation cross, ~41 s) will be performed (see figure 2 for details). The women are instructed to try and explore different self-chosen strategies (of upregulation) and find the one that works best for them. Afterwards, they are asked to report which strategy they used and about their subjective success experience. The third and last run of each session is implemented as a ‘transfer’ block without the visible ‘thermometer’ display.65 67 71
Figure 2.
Two trials of the NFB intervention within a run. NFB, neurofeedback.
Functional images are acquired with a Siemens Tim Trio using a T2*weighted echoplanar sequence (TR=1.64 s, TE=30 ms, 30 slices, 3 mm slice thickness, FoV=192 mm, flip angle 73°, voxel size 3×3×3 mm, 343 volumes per trainings run, distance factor of 33% and GeneRalized Autocalibrating Partial Parallel Acquisition (GRAPPA) with iPat=2) and a 32 channel head coil. Control for cardiovascular parameters is conducted using the built-in pulse clip. In-house Matlab software based on statistical parametric mapping 12 (SPM12) functions is used to conduct rtfMRI-NFB and Presentation software (Neurobehavioral Systems, Albany, CA, USA) is used to present pictures and the feedback signal. At the beginning of each NFB training session, the anatomical image is segmented and normalised to Montreal Neurological Institute (MNI) standard space. The inverse deformations of the normalisation are then applied to warp the masks of the target regions into subject space.
To correct for movement, each acquired volume is realigned to the first image of the run. Then, volumes with more than 0.5 mm scan-to-scan movements are identified and marked in dummy regressors. Afterwards, the average intensity values from the target region and a cerebrospinal fluid (CSF) mask are extracted and the signal of the target region is corrected for the estimated motion parameters, high-motion dummy regressors and the CSF signal. For calculation of the feedback signal, the ROI intensity value of the last three volumes is averaged and compared with the average intensity of the baseline condition. For further technical details regarding the NFB setup, please refer to Gerchen et al 91 which uses an identical NFB procedure in the context of alcohol addiction.
Data analysis plan
Statistical analyses, namely the main comparison of the two groups (mothers with bonding difficulties vs the control group) and the longitudinal analysis of positive relationships changes after the NFB intervention (interaction behaviour, attachment data, as well as psychophysiological, neuroendocrine and epigenetic markers (see table 1) will be done using IBM SPSS Statics and R (r-project.org). The MRI data will be analysed with general linear models using statistical parametric mapping with SPM (https://www.fil.ion.ucl.ac.uk/spm/software/spm12/) implemented (Wellcome Department of Cognitive Neurology, London, UK) in MATLAB (MathWorks, Natick, MA).
For all MRI tasks, all events of the paradigms are modelled by means of general linear model. The relevant contrasts for the go/nogo task are (faces nogo >faces go), (infant faces nogo >adult faces nogo) and (negative faces nogo >positive faces nogo). The relevant contrasts for the reward task are (reward high >reward low), (reward high cognitive load >reward low cognitive load) and (anticipation of reward >baseline). The relevant contrasts for the passive viewing task are (own infant >unfamiliar infant), (positive infant >negative infant), (own partner >unfamiliar man) and (own infant >own partner).
To calculate pre-intervention, post-intervention and follow-up group differences between the intervention and control groups, repeated measures analyses of variance will be calculated while multi-level models will be used to model changes over the time course.
Supplementary Material
Acknowledgments
The authors wish to thank Britta Zipser, Ekaterina Schneider, Madgalena Vragovic, Elena Augenstein, Johanna Jübner, Antonia Huge, Corinna Abdaoui, Nora Nonnenmacher, Nina Schlegel, Josephine Parol, Lydia Oeljeklaus, Hanna Melles and Hanna-Sophie Lässig for their assistance with conducting the study.
Footnotes
ME and A-LZ contributed equally.
Contributors: BD, PK, A-LZ and ME designed the study; ME and A-LZ lead the study; SA-J collected data; PK, MFG and MMS established the experimental set up; SA-J, A-LZ and ME wrote the manuscript; all authors provided comments on the manuscript.
Funding: This work was supported by the Dietmar-Hopp Foundation (September 2017- March 2020). We acknowledge financial support by Deutsche Forschungsgemeinschaft within the funding programme Open Access Publishing, by the Baden-Württemberg Ministry of Science, Research and the Arts and by Ruprecht-Karls-Universität Heidelberg.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Parental/guardian consent obtained.
References
- 1. Klaus M, Kennell J, Klaus P. Bonding. New York: Addison-Wesley, 1995. [Google Scholar]
- 2. Brockington I. Postpartum psychiatric disorders. Lancet 2004;363:303–10. 10.1016/S0140-6736(03)15390-1 [DOI] [PubMed] [Google Scholar]
- 3. Klaus MH, Kennell JH. Parent-infant bonding. 2nd edn St. Louis, Mo [u.a.]: Mosby, 1982:313. [Google Scholar]
- 4. Maestripieri D. Is There Mother–Infant Bonding in Primates? Dev Rev 2001;21:93–120. 10.1006/drev.2000.0522 [DOI] [Google Scholar]
- 5. Reck C, Klier CM, Pabst K, et al. The German version of the Postpartum Bonding Instrument: psychometric properties and association with postpartum depression. Arch Womens Ment Health 2006;9:265–71. 10.1007/s00737-006-0144-x [DOI] [PubMed] [Google Scholar]
- 6. Tietz A, Zietlow A-L, Reck C. Maternal bonding in mothers with postpartum anxiety disorder: the crucial role of subclinical depressive symptoms and maternal avoidance behaviour. Arch Womens Ment Health 2014;17:433–42. 10.1007/s00737-014-0423-x [DOI] [PubMed] [Google Scholar]
- 7. Hornstein C, Hohm E, Trautmann-Villalba P. Die postpartale Bindungsstörung: Eine Risikokonstellation für den Infantizid? Forensische Psychiatrie Psychologie Kriminologie 2009;1:1–8. [Google Scholar]
- 8. Feldman R. The adaptive human parental brain: implications for children’s social development. Trends Neurosci 2015;38:387–99. 10.1016/j.tins.2015.04.004 [DOI] [PubMed] [Google Scholar]
- 9. Moll J, Schulkin J. Social attachment and aversion in human moral cognition. Neurosci Biobehav Rev 2009;33:456–65. 10.1016/j.neubiorev.2008.12.001 [DOI] [PubMed] [Google Scholar]
- 10. Moll J, Bado P, de Oliveira-Souza R, et al. A neural signature of affiliative emotion in the human septohypothalamic area. J Neurosci 2012;32:12499–505. 10.1523/JNEUROSCI.6508-11.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Depue RA, Morrone-Strupinsky JV. A neurobehavioral model of affiliative bonding: implications for conceptualizing a human trait of affiliation. Behav Brain Sci 2005;28:313–50. discussion 350-95 10.1017/S0140525X05000063 [DOI] [PubMed] [Google Scholar]
- 12. Strathearn L, Li J, Fonagy P, et al. What’s in a smile? Maternal brain responses to infant facial cues. Pediatrics 2008;122:40–51. 10.1542/peds.2007-1566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bakermans-Kranenburg MJ, van IJzendoorn MH. Oxytocin receptor (OXTR) and serotonin transporter (5-HTT) genes associated with observed parenting. Soc Cogn Affect Neurosci 2008;3:128–34. 10.1093/scan/nsn004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Feldman R, Weller A, Zagoory-Sharon O, et al. Evidence for a neuroendocrinological foundation of human affiliation: plasma oxytocin levels across pregnancy and the postpartum period predict mother-infant bonding. Psychol Sci 2007;18:965–70. 10.1111/j.1467-9280.2007.02010.x [DOI] [PubMed] [Google Scholar]
- 15. Reck C, Klier CM, Pabst K, et al. The German version of the Postpartum Bonding Instrument: Psychometric properties and association with postpartum depression. Arch Womens Ment Health 2006;9:265–71. 10.1007/s00737-006-0144-x [DOI] [PubMed] [Google Scholar]
- 16. Brockington IF, Aucamp HM, Fraser C. Severe disorders of the mother–infant relationship: definitions and frequency. Arch Womens Ment Health 2006;9:243–51. 10.1007/s00737-006-0133-0 [DOI] [PubMed] [Google Scholar]
- 17. Moehler E, Brunner R, Wiebel A, et al. Maternal depressive symptoms in the postnatal period are associated with long-term impairment of mother–child bonding. Arch Womens Ment Health 2006;9:273–8. 10.1007/s00737-006-0149-5 [DOI] [PubMed] [Google Scholar]
- 18. Reck C, Zietlow A-L, Müller M, et al. Perceived parenting stress in the course of postpartum depression: the buffering effect of maternal bonding. Arch Womens Ment Health 2016;19:473–82. 10.1007/s00737-015-0590-4 [DOI] [PubMed] [Google Scholar]
- 19. Brockington IF, Oates J, George S, et al. A screening questionnaire for mother-infant bonding disorders. Arch Womens Ment Health 2001;3:133–40. 10.1007/s007370170010 [DOI] [Google Scholar]
- 20. Hofecker-Fallahpour M, Riecher-Rössler A. Depression in der frühen Mutterschaft. Neurotransmitter Sonderheft 2003;2:35–9. [DOI] [PubMed] [Google Scholar]
- 21. Laurent HK, Ablow JC. A face a mother could love: depression-related maternal neural responses to infant emotion faces. Soc Neurosci 2013;8:228–39. 10.1080/17470919.2012.762039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wonch KE, de Medeiros CB, Barrett JA, et al. Postpartum depression and brain response to infants: Differential amygdala response and connectivity. Soc Neurosci 2016;11:600–17. 10.1080/17470919.2015.1131193 [DOI] [PubMed] [Google Scholar]
- 23. Pawluski JL, Lonstein JS, Fleming AS. The Neurobiology of Postpartum Anxiety and Depression. Trends Neurosci 2017;40:106–20. 10.1016/j.tins.2016.11.009 [DOI] [PubMed] [Google Scholar]
- 24. Reck C, Nonnenmacher N, Zietlow A-L. Intergenerational Transmission of Internalizing Behavior: The Role of Maternal Psychopathology, Child Responsiveness and Maternal Attachment Style Insecurity. Psychopathology 2016;49:277–84. 10.1159/000446846 [DOI] [PubMed] [Google Scholar]
- 25. Zietlow A-L, Schlüter MK, Nonnenmacher N, et al. Maternal Self-confidence Postpartum and at Pre-school Age: The Role of Depression, Anxiety Disorders, Maternal Attachment Insecurity. Matern Child Health J 2014;18:1873–80. 10.1007/s10995-014-1431-1 [DOI] [PubMed] [Google Scholar]
- 26. Reck C, Noe D, Stefenelli U, et al. Interactive coordination of currently depressed inpatient mothers and their infants during the postpartum period. Infant Ment Health J 2011;32:542–62. 10.1002/imhj.20312 [DOI] [PubMed] [Google Scholar]
- 27. Licata M, Zietlow A-L, Träuble B, et al. Maternal Emotional Availability and Its Association with Maternal Psychopathology, Attachment Style Insecurity and Theory of Mind. Psychopathology 2016;49:334–40. 10.1159/000447781 [DOI] [PubMed] [Google Scholar]
- 28. Mason ZS, Briggs RD, Silver EJ. Maternal attachment feelings mediate between maternal reports of depression, infant social–emotional development, and parenting stress. J Reprod Infant Psychol 2011;29:382–94. 10.1080/02646838.2011.629994 [DOI] [Google Scholar]
- 29. Hay DF, Pawlby S, Sharp D, et al. Intellectual problems shown by 11-year-old children whose mothers had postnatal depression. J Child Psychol Psychiatry 2001;42:871–89. 10.1111/1469-7610.00784 [DOI] [PubMed] [Google Scholar]
- 30. Meaney MJ. Maternal care, gene expression, and the transmission of individual differences in stress reactivity across generations. Annu Rev Neurosci 2001;24:1161–92. 10.1146/annurev.neuro.24.1.1161 [DOI] [PubMed] [Google Scholar]
- 31. Müller M, Tronick E, Zietlow A-L, et al. Effects of Maternal Anxiety Disorders on Infant Self-Comforting Behaviors: The Role of Maternal Bonding, Infant Gender and Age. Psychopathology 2016;49:295–304. 10.1159/000448404 [DOI] [PubMed] [Google Scholar]
- 32. Dalsant A, Truzzi A, Setoh P, et al. Maternal bonding in childhood moderates autonomic responses to distress stimuli in adult males. Behav Brain Res 2015;292:428–31. 10.1016/j.bbr.2015.06.026 [DOI] [PubMed] [Google Scholar]
- 33. Hellhammer D, Hellhammer J. Stress: the brain-body connection: Karger Medical and Scientific Publishers, 2008. [Google Scholar]
- 34. Brennan PA, Pargas R, Walker EF, et al. Maternal depression and infant cortisol: influences of timing, comorbidity and treatment. J Child Psychol Psychiatry 2008;49:1099–107. 10.1111/j.1469-7610.2008.01914.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Fernandes M, Stein A, Srinivasan K, et al. Foetal exposure to maternal depression predicts cortisol responses in infants: findings from rural South India. Child Care Health Dev 2015;41:677–86. 10.1111/cch.12186 [DOI] [PubMed] [Google Scholar]
- 36. Kaplan LA, Evans L, Monk C. Effects of mothers' prenatal psychiatric status and postnatal caregiving on infant biobehavioral regulation: Can prenatal programming be modified? Early Hum Dev 2008;84:249–56. 10.1016/j.earlhumdev.2007.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Champagne FA. Epigenetic mechanisms and the transgenerational effects of maternal care. Front Neuroendocrinol 2008;29:386–97. 10.1016/j.yfrne.2008.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Benoit D, Parker KCH. Stability and transmission of attachment across three generations. Child Dev 1994;65:1444–56. 10.2307/1131510 [DOI] [PubMed] [Google Scholar]
- 39. Main M, Hesse E. Parents' unresolved traumatic experiences are related to infant disorganized attachment status: Is frightened and/or frightening parental behavior the linking mechanism? 1990.
- 40. Pederson DR, Gleason KE, Moran G, et al. Maternal attachment representations, maternal sensitivity, and the infant–mother attachment relationship. Dev Psychol 1998;34:925–33. 10.1037/0012-1649.34.5.925 [DOI] [PubMed] [Google Scholar]
- 41. Miller L, Kramer R, Warner V, et al. Intergenerational transmission of parental bonding among women. J Am Acad Child Adolesc Psychiatry 1997;36:1134–5. 10.1097/00004583-199708000-00022 [DOI] [PubMed] [Google Scholar]
- 42. Bakermans-Kranenburg MJ, van IJzendoorn MH, Juffer F. Less is more: Meta-analyses of sensitivity and attachment interventions in early childhood. Psychol Bull 2003;129:195–215. 10.1037/0033-2909.129.2.195 [DOI] [PubMed] [Google Scholar]
- 43. Kalinauskiene L, Cekuoliene D, Van Ijzendoorn MH, et al. Supporting insensitive mothers: the Vilnius randomized control trial of video-feedback intervention to promote maternal sensitivity and infant attachment security. Child Care Health Dev 2009;35:613–23. 10.1111/j.1365-2214.2009.00962.x [DOI] [PubMed] [Google Scholar]
- 44. Bilszta JLC, Buist AE, Wang F, et al. Use of video feedback intervention in an inpatient perinatal psychiatric setting to improve maternal parenting. Arch Womens Ment Health 2012;15:249–57. 10.1007/s00737-012-0283-1 [DOI] [PubMed] [Google Scholar]
- 45. Teti DM, Black Maureen M, Rose V. Intervention with African American premature infants: Four-month results of an early intervention program. J Early Interv 2009;31:146–66. [Google Scholar]
- 46. Hoffenkamp HN, Tooten A, Hall RAS, et al. Effectiveness of hospital-based video interaction guidance on parental interactive behavior, bonding, and stress after preterm birth: A randomized controlled trial. J Consult Clin Psychol 2015;83:416–29. 10.1037/a0038401 [DOI] [PubMed] [Google Scholar]
- 47. Daniel R, Pollmann S. A universal role of the ventral striatum in reward-based learning: Evidence from human studies. Neurobiol Learn Mem 2014;114:90–100. 10.1016/j.nlm.2014.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Flagel SB, Watson SJ, Robinson TE, et al. Individual differences in the propensity to approach signals vs goals promote different adaptations in the dopamine system of rats. Psychopharmacology 2007;191:599–607. 10.1007/s00213-006-0535-8 [DOI] [PubMed] [Google Scholar]
- 49. Adolphs R. The Social Brain: Neural Basis of Social Knowledge. Annu Rev Psychol 2009;60:693–716. 10.1146/annurev.psych.60.110707.163514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Bhanji JP, Delgado MR. The social brain and reward: social information processing in the human striatum. Wiley Interdiscip Rev Cogn Sci 2014;5:61–73. 10.1002/wcs.1266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Montoya JL, Landi N, Kober H, et al. Regional brain responses in nulliparous women to emotional infant Stimuli. PLoS One 2012;7:e36270 10.1371/journal.pone.0036270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lenzi D, Trentini C, Pantano P, et al. Neural basis of maternal communication and emotional expression processing during infant preverbal stage. Cereb Cortex 2009;19:1124–33. 10.1093/cercor/bhn153 [DOI] [PubMed] [Google Scholar]
- 53. DelDonno SR, Weldon AL, Crane NA, et al. Affective personality predictors of disrupted reward learning and pursuit in major depressive disorder. Psychiatry Res 2015;230:56–64. 10.1016/j.psychres.2015.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Zhang W-N, Chang S-H, Guo L-Y, et al. The neural correlates of reward-related processing in major depressive disorder: A meta-analysis of functional magnetic resonance imaging studies. J Affect Disord 2013;151:531–9. 10.1016/j.jad.2013.06.039 [DOI] [PubMed] [Google Scholar]
- 55. Laurent HK, Ablow JC. A cry in the dark: depressed mothers show reduced neural activation to their own infant’s cry. Soc Cogn Affect Neurosci 2012;7:125–34. 10.1093/scan/nsq091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Dölen G, Darvishzadeh A, Huang KW, et al. Social reward requires coordinated activity of nucleus accumbens oxytocin and serotonin. Nature 2013;501:179–184. 10.1038/nature12518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ebner NC, Lin T, Muradoglu M, et al. Associations between oxytocin receptor gene (OXTR) methylation, plasma oxytocin, and attachment across adulthood. Int J Psychophysiol 2019;136:22–32. 10.1016/j.ijpsycho.2018.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. King L, Robins S, Chen G, et al. Perinatal depression and DNA methylation of oxytocin-related genes: a study of mothers and their children. Horm Behav. 2017;96:84–94. 10.1016/j.yhbeh.2017.09.006 [DOI] [PubMed] [Google Scholar]
- 59. Galbally M, Ryan J, van IJzendoorn M, et al. Maternal depression, antidepressant use and placental oxytocin receptor DNA methylation: Findings from the MPEWS study. Psychoneuroendocrinology 2018;90:1–8. 10.1016/j.psyneuen.2018.01.004 [DOI] [PubMed] [Google Scholar]
- 60. Feldman R. Oxytocin and social affiliation in humans. Horm Behav 2012;61:380–91. 10.1016/j.yhbeh.2012.01.008 [DOI] [PubMed] [Google Scholar]
- 61. Thibault RT, MacPherson A, Lifshitz M, et al. Neurofeedback with fMRI: A critical systematic review. Neuroimage 2018;172 10.1016/j.neuroimage.2017.12.071 [DOI] [PubMed] [Google Scholar]
- 62. Sulzer J, Haller S, Scharnowski F, et al. Real-time fMRI neurofeedback: progress and challenges. Neuroimage 2013;76:386–99. 10.1016/j.neuroimage.2013.03.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Moll J, Weingartner JH, Bado P, et al. Voluntary enhancement of neural signatures of affiliative emotion using FMRI neurofeedback. PLoS One 2014;9:e97343 10.1371/journal.pone.0097343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Buyukturkoglu K, Roettgers H, Sommer J, et al. Self-regulation of anterior insula with real-time fMRI and its behavioral effects in obsessive-compulsive disorder: a feasibility study. PLoS One 2015;10:e0135872 10.1371/journal.pone.0135872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Paret C, Kluetsch R, Zaehringer J, et al. Alterations of amygdala-prefrontal connectivity with real-time fMRI neurofeedback in BPD patients. Soc Cogn Affect Neurosci 2016;11:952–60. 10.1093/scan/nsw016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Zilverstand A, Sorger B, Sarkheil P, et al. fMRI neurofeedback facilitates anxiety regulation in females with spider phobia. Front Behav Neurosci 2015;9 10.3389/fnbeh.2015.00148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Kirsch M, Gruber I, Ruf M, et al. Real-time functional magnetic resonance imaging neurofeedback can reduce striatal cue-reactivity to alcohol stimuli. Addict Biol 2016;21 10.1111/adb.12278 [DOI] [PubMed] [Google Scholar]
- 68. Misaki M, Phillips R, Zotev V, et al. Real-time fMRI amygdala neurofeedback positive emotional training normalized resting-state functional connectivity in combat veterans with and without PTSD: a connectome-wide investigation. Neuroimage 2018;20:543–55. 10.1016/j.nicl.2018.08.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Ditzen B, Heinrichs M. Psychobiology of social support: the social dimension of stress buffering. Restor Neurol Neurosci 2014;32:149–62. [DOI] [PubMed] [Google Scholar]
- 70. Cordes JS, Mathiak KA, Dyck M, et al. Cognitive and neural strategies during control of the anterior cingulate cortex by fMRI neurofeedback in patients with schizophrenia. Front Behav Neurosci 2015;9 10.3389/fnbeh.2015.00169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Young KD, Zotev V, Phillips R, et al. Real-time fMRI neurofeedback training of amygdala activity in patients with major depressive disorder. PLoS One 2014;9:e88785 10.1371/journal.pone.0088785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Etkin A, Egner T, Kalisch R. Emotional processing in anterior cingulate and medial prefrontal cortex. Trends Cogn Sci 2011;15:85–93. 10.1016/j.tics.2010.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Wessa M, Houenou J, Paillère-Martinot M-L, et al. Fronto-striatal overactivation in euthymic bipolar patients during an emotional Go/NoGo task. Am J Psychiatry 2007;164:638–46. 10.1176/ajp.2007.164.4.638 [DOI] [PubMed] [Google Scholar]
- 74. Faul F, Erdfelder E, Buchner A, et al. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods 2009;41:1149–60. 10.3758/BRM.41.4.1149 [DOI] [PubMed] [Google Scholar]
- 75. Tronick E, Als H, Adamson L, et al. The infant’s response to entrapment between contradictory messages in face-to-face interaction. J Am Acad Child Psychiatry 1978;17:1–13. 10.1016/S0002-7138(09)62273-1 [DOI] [PubMed] [Google Scholar]
- 76. Tronick EZ, Cohn JF. Infant-mother face-to-face interaction: age and gender differences in coordination and the occurrence of miscoordination. Child Dev 1989;60:85–92. 10.2307/1131074 [DOI] [PubMed] [Google Scholar]
- 77. Feldman R. Coding interactive behavior manual. Israel: Unpublished manual, Bar-Ilan University, 1998. [Google Scholar]
- 78. Reuner G, Rosenkranz J. Bayley-III - Bayley Scales of Infant & Toddler Development III. Deutsche Version. Frankfurt: Pearson Assessment & Information GmbH, 2015. [Google Scholar]
- 79. Schwartz EB, Granger DA, Susman EJ, et al. Assessing salivary cortisol in studies of child development. Child Dev 1998;69:1503–13. 10.1111/j.1467-8624.1998.tb06173.x [DOI] [PubMed] [Google Scholar]
- 80. Feldman R, Masalha S, Nadam R. Cultural perspective on work and family: Dual-earner Israeli Jewish and Arab families at the transition to parenthood. Journal of Family Psychology 2001;15:492–509. 10.1037/0893-3200.15.3.492 [DOI] [PubMed] [Google Scholar]
- 81. Pruessner JC, Kirschbaum C, Meinlschmid G, et al. Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology 2003;28:916–31. 10.1016/S0306-4530(02)00108-7 [DOI] [PubMed] [Google Scholar]
- 82. Stalder T, Kirschbaum C, Kudielka B, et al. Assessment of the cortisol awakening response: Summary of the ISPNE expert consensus guidelines. Psychoneuroendocrinology 2016;71:44 10.1016/j.psyneuen.2016.07.116 [DOI] [PubMed] [Google Scholar]
- 83. Martin-Soelch C, Kobel M, Stoecklin M, et al. Reduced Response to Reward in Smokers and Cannabis Users. Neuropsychobiology 2009;60:94–103. 10.1159/000239685 [DOI] [PubMed] [Google Scholar]
- 84. Scheele D, Wille A, Kendrick KM, et al. Oxytocin enhances brain reward system responses in men viewing the face of their female partner. Proc Natl Acad Sci U S A 2013;110:20308–13. 10.1073/pnas.1314190110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Feldman R, Masalha S. Parent–child and triadic antecedents of children’s social competence: Cultural specificity, shared process. Dev Psychol 2010;46:455–67. 10.1037/a0017415 [DOI] [PubMed] [Google Scholar]
- 86. Bayley N. Bayley Scales of Infant and Toddler Development–Third Edition: Administration Manual. San Antonio: TX: Harcourt Assessment Google Scholar, 2006. [Google Scholar]
- 87. Bayley N. Bayley Scales of Infant and Toddler Development–Third Edition: Technical Manual. San Antonio: TX: Harcourt Assessment Google Scholar, 2006. [Google Scholar]
- 88. Albers CA, Grieve AJ. Test Review: Bayley, N. (2006). Bayley Scales of Infant and Toddler Development– Third Edition. San Antonio, TX: Harcourt Assessment. J Psychoeduc Assess 2007;25:180–90. 10.1177/0734282906297199 [DOI] [Google Scholar]
- 89. Reck C, Van Den Bergh B, Tietz A, et al. Maternal avoidance, anxiety cognitions and interactive behaviour predicts infant development at 12 months in the context of anxiety disorders in the postpartum period. Infant Behavior and Development 2018;50:116–31. 10.1016/j.infbeh.2017.11.007 [DOI] [PubMed] [Google Scholar]
- 90. Brett M, Anton JL, Valabrgue R, et al. Region of interest analysis using an SPM toolbox. in 8th international conference on functional mapping of the human brain. Sendai, 2002. [Google Scholar]
- 91. Gerchen MF, Kirsch M, Bahs N, et al. The SyBil-AA real-time fMRI neurofeedback study: protocol of a single-blind randomized controlled trial in alcohol use disorder. BMC Psychiatry 2018;18:12 10.1186/s12888-018-1604-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Margraf J, Cwik JC, Suppiger A, et al. DIPS Open Access: Diagnostic Interview for Mental Disorders. [DIPS Open Access: Diagnostisches Interview bei psychischen Störungen.]. Bochum: Mental Health Research and Treament Center, Ruhr-Universität Bochum, 2017. [Google Scholar]
- 93. Bifulco A, Moran PM, Ball C, et al. Adult attachment style. I: Its relationship to clinical depression. Soc Psychiatry Psychiatr Epidemiol 2002;37:50–9. 10.1007/s127-002-8215-0 [DOI] [PubMed] [Google Scholar]
- 94. Bergant AM, Nguyen T, Heim K, et al. Deutschsprachige Fassung und Validierung der »Edinburgh postnatal depression scale«. DMW - Deutsche Medizinische Wochenschrift 1998;123:35–40. 10.1055/s-2007-1023895 [DOI] [PubMed] [Google Scholar]
- 95. Ehlers A, Margraf J, Chambless D. Fragebogen zu körperbezogenen Ängsten, Kognitionen und Vermeidung (AKV). Göttingen: Beltz Test, 2001. [Google Scholar]
- 96. Lips HM, Bloom K. Psychometric Evaluation of a New Scale to Measure Maternal Self-Confidence: Radford, 1993. [Google Scholar]
- 97. Parker G, Tupling H, Brown LB. A Parental Bonding Instrument. Br J Med Psychol 1979;52:1–10. 10.1111/j.2044-8341.1979.tb02487.x [DOI] [Google Scholar]
- 98. Schumacher J, Eisemann M, Brähler E. Fragebogen zum erinnerten elterlichen Erziehungsverhalten: Huber, 2000. [Google Scholar]
- 99. Ehrenthal J, Dinger U, Lamla A, et al. Evaluation der deutschsprachigen Version des Bindungsfragebogens „Experiences in Close Relationships – Revised” (ECR-RD). PPmP - Psychotherapie · Psychosomatik · Medizinische Psychologie 2009;59:215–23. 10.1055/s-2008-1067425 [DOI] [PubMed] [Google Scholar]
- 100. Fydrich T, Sommer G, Brähler E. Fragebogen zur Sozialen Unterstützung (F-SozU). Manual. Göttingen: Hogrefe. [Google Scholar]
- 101. Zimmermann J, Altenstein D, Krieger T, et al. The Structure and Correlates of Self-Reported DSM-5 Maladaptive Personality Traits: Findings From Two German-Speaking Samples. J Pers Disord 2014;28:518–40. 10.1521/pedi_2014_28_130 [DOI] [PubMed] [Google Scholar]
- 102. Klinitzke G, Romppel M, Häuser W, et al. [The German Version of the Childhood Trauma Questionnaire (CTQ): psychometric characteristics in a representative sample of the general population]. Psychother Psychosom Med Psychol 2012;62:47–51. 10.1055/s-0031-1295495 [DOI] [PubMed] [Google Scholar]
- 103. Hahlweg K. Fragebogen zur Partnerschaftsdiagnostik. Göttingen: Hogrefe, 1996. [Google Scholar]
- 104. Bodenmann G. Dyadisches coping inventar: Testmanual [Dyadic coping inventory: Test manual]. Bern, Switzerland: Huber, 2008. [Google Scholar]
- 105. Tröster H. Eltern-Belastungs-Inventar (EBI). Deutsche Version des Parenting Stress Index (PSI) von R. R. Abidin. Manual Göttingen: Hogrefe, 2010. [Google Scholar]
- 106. Bifulco A, Mahon J, Kwon J-H, et al. The Vulnerable Attachment Style Questionnaire (VASQ): an interview-based measure of attachment styles that predict depressive disorder. Psychol Med 2003;33:1099–110. 10.1017/S0033291703008237 [DOI] [PubMed] [Google Scholar]
- 107. Oldfield RC. The assessment and analysis of handedness: The Edinburgh inventory. Neuropsychologia 1971;9:97–113. 10.1016/0028-3932(71)90067-4 [DOI] [PubMed] [Google Scholar]
- 108. Pauli-Pott U, Mertesacker B, Beckmann D. Ein Fragebogen zur Erfassung des «frühkindlichen Temperaments» im Elternurteil. Zeitschrift für Kinder- und Jugendpsychiatrie und Psychotherapie 2003;31:99–110. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.