Abstract
Objective
To describe changes in cardiovascular risk factors and in the estimated 10-year risk of acute myocardial infarction (AMI) or cerebral stroke (CS) between SAMINOR 1 (2003–2004) and SAMINOR 2 (2012–2014), and explore if these changes differed between Sami and non-Sami.
Design
Two cross-sectional surveys.
Setting
Inhabitants of rural Northern Norway.
Participants
Participants were aged 40–79 years and participated in SAMINOR 1 (n=6417) and/or SAMINOR 2 (n=5956).
Primary outcome measures
Generalised estimating equation regressions with an interaction term were used to estimate and compare changes in cardiovascular risk factors and 10-year risk of AMI or CS between the two surveys and by ethnicity.
Results
Mean cholesterol declined by 0.50, 0.43 and 0.60 mmol/L in women, Sami men and non-Sami men, respectively (all p<0.001). Sami men had a small decline in mean high-density lipoprotein (HDL) cholesterol and an increase in mean triglycerides (both p<0.001), whereas non-Sami showed no change in these variables. Non-Sami women had an increase in mean HDL cholesterol (p<0.001) whereas Sami women had no change. Triglycerides did not change in non-Sami and Sami women. Systolic and diastolic blood pressure declined by 3.6 and 1.0 mm Hg in women, and 3.1 and 0.7 in men, respectively (all p<0.01). Mean waist circumference increased by 6.7 and 5.9 cm in women and men, respectively (both p<0.001). The odds of being a smoker declined by 35% in women and 46% in men (both p<0.001). Estimated 10-year risk of AMI or CS decreased in all strata of sex and ethnicity (p<0.001), however, Sami women had a smaller decline than non-Sami did.
Conclusions
Independent of ethnicity, there was a decline in mean cholesterol, blood pressure, smoking, hypertension (women only) and 10-year risk of AMI or CS, but waist circumference increased. Relatively minor ethnic differences were found in changes of cardiovascular risk factors.
Keywords: epidemiology, preventive medicine, vascular medicine, ethnic groups, indigenous, health behaviour
Strengths and limitations of this study.
We used generalised estimating equation regression to account for overlapping samples.
We used self-reported measures to categorise participants into ethnic groups, including questions on self-perceived ethnicity, ethnic background and language use.
Due to lack of ethnic identifiers in national registries, we do not know if participation differs by ethnicity.
We have an acceptable participation rate in both surveys.
We lack information about the use of lipid-lowering drugs.
Introduction
Since the 1970s, a favourable decline in systolic blood pressure,1–4 total cholesterol5–7 and smoking8 has been reported for the adult population across different regions of Western Europe. This decline is probably due to changes in lifestyle and diet,7 9 10 in addition to use of medication.1 5 In Norway, this decline has coincided with a decrease in cardiovascular mortality and an increased prevalence of obesity and a sedentary lifestyle.11
The Sami is an indigenous people living in Sápmi, that is, the northern parts of Norway, Sweden, Finland and the Kola Peninsula in the Russian Federation. There are no official population records on the Sami population, but data from the 1970 national census roughly estimated that there were 40 000 Sami in Norway,12 whereas 55 000 is the population number that the Sami Parliament uses when considering subsidy schemes for business development.13 In 2017, approximately 17 000 Sami adults were enrolled in the electoral register to the Sami Parliament in Norway, which gives them the right to vote and be elected.14 The Sami people have unique cultures and languages, but these have partly vanished or at least declined in practice, due to structural assimilation that occurred from 1850 to 1960.15 The Norwegian part of Sápmi is also inhabited by Norwegians and Kvens, the latter of whom are descendants of Finnish-speaking people that came from Sweden and Finland to Northern Norway in the 1700s and 1800s.16
Surveys from Norway have concluded that there are no or only minor differences in cardiovascular risk factors and morbidity between the Sami and non-Sami in rural regions.17–21 However, knowledge is lacking on changes in conventional cardiovascular risk factors. Thus, this study aimed to describe changes in cardiovascular risk factors and in the estimated 10-year risk of acute myocardial infarction (AMI) or cerebral stroke (CS) between SAMINOR 1 (2003–2004) and SAMINOR 2 (2012–2014), and explore if these changes differed between Sami and non-Sami.
Methods
We used data from two cross-sectional surveys of the Population-based Study on Health and Living Conditions in Regions with Sami and Norwegian Populations (The SAMINOR Study): the SAMINOR 1 Survey carried out in 2003–2004 (SAMINOR 1) and the SAMINOR 2 Clinical Survey carried out in 2012–2014 (SAMINOR 2). SAMINOR 1 was a collaboration between the Centre for Sami Health Research at UiT The Arctic University of Norway and the Norwegian National Institute of Public Health,22 whereas SAMINOR 2 was performed by the former only.23 Participants were invited from 10 municipalities (figure 1) that, according to the population census from 1970,12 had high proportions of Sami inhabitants. Invitations were mailed to all who were aged 40–79 years and were registered as inhabitants in the 10 municipalities by the National Registry. In total, 11 518 and 12 455 received an invitation to SAMINOR 1 and SAMINOR 2, respectively. Participation was voluntarily and clinical examinations in each municipality were conducted within a period of 1–7 weeks, depending on the population size. Our analyses were restricted to those who attended clinical examinations, gave blood samples and answered the self-administered questionnaires.
Figure 1.
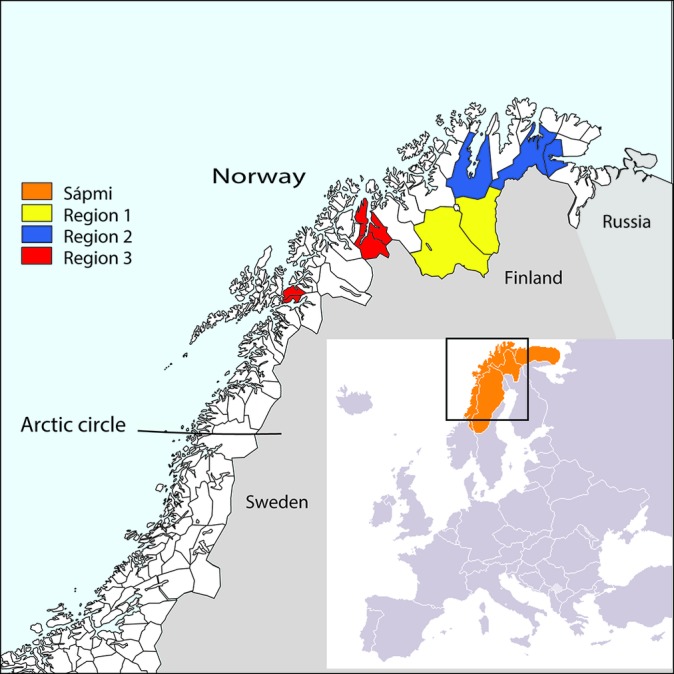
Inhabitants aged 40–79 years living in these 10 municipalities in the Norwegian part of Sápmi were invited to the SAMINOR 1 and SAMINOR 2 surveys. Region 1 includes Kautokeino and Karasjok, region 2 includes Nesseby, Tana and Porsanger, and region 3 includes Kåfjord, Lyngen, Storfjord, Skånland and Evenes. There are no copyrights attached to this figure. The figure is designed for this article by one of the co-authors, Marita Melhus, Centre for Sami Health Research at UiT The Arctic University of Norway. The figure is based on a raw map of Norway made by the Norwegian Mapping Authority, merged with a map of Europe that is available to the public domain at Wikipedia.
Participant and public involvement
Participants that had pathological findings from the clinical examination, were recommended to contact their primary physician. In emergency situations, participants were sent directly to the local health centre or the nearest hospital.
Before and after the surveys, the Centre for Sami Health Research had consultations with the Sami Parliament, Sami researchers and health workers in Sami core areas to identify the needs of the Sami community. Results from the surveys were reported to decision makers at the municipal and regional levels, and to the Sami Parliament and national health authorities. The population was informed through popular science forums, meetings and lectures.
Study sample
There were 6550 (56.9%) and 6004 (48.2%) individuals who attended the clinical examinations in SAMINOR 1 and SAMINOR 2, respectively. If information on ethnicity was lacking in one of the surveys, ethnicity information given in the other survey was used, as Sami ethnicity is found to be stable.24 This strategy was valuable for the SAMINOR 1 sample, as ethnicity information was lacking for some participants due to the study design.22 In SAMINOR 1, we categorised 69 out of 201 by using ethnicity information from SAMINOR 2: 7 non-Sami and 62 Sami. In SAMINOR 2, 96 had missing data on ethnicity and we categorised 58: 37 non-Sami and 21 Sami. Furthermore, we excluded those that did not hand in the main questionnaires (SAMINOR 1: n=1; SAMINOR 2: n=10). This left us with a final sample of 6417 and 5956 from SAMINOR 1 and SAMINOR 2, respectively, wherein 3249 participated in both surveys.
Information from questionnaires
Participants were categorised into ethnic groups based on information from the following 11 questions, which were identical in the two surveys: ‘What language(s) do/did you, your parents, and your grandparents use at home?’; ‘What is your, your father’s, and your mother’s ethnic background?’; ‘What do you consider yourself to be?’ The response options were ‘Norwegian’, ‘Sami’, ‘Kven’ and ‘other’ and multiple answers were allowed. Participants were defined as Sami if they (1) considered themselves to be Sami, or reported a Sami ethnic background for themselves, and (2) spoke a Sami language themselves or had at least one parent or grandparent that used it at home. All others were categorised as non-Sami. Sensitivity analyses were performed, in which different ethnic categorisations were used.
Smoking status was determined by the following questions, in SAMINOR 1: ‘Are you currently, or were you previously a daily smoker?’ (Yes, currently/Yes, previously/Never); in SAMINOR 2: ‘Have you ever smoked daily?’ (Yes/No), and ‘Are you currently a daily smoker?’ (Yes/No). Previous and never smokers were categorised as non-smokers.
Use of anti-hypertensive drugs was determined by the following question: ‘Do you take medication for high blood pressure?’ (Currently/Previously, but not now/Never used). Previous use, never-use and missing values were merged into non-use.
In both surveys, participates reported if they ever have had myocardial infarctions and age at first time. Positive responses to the former, or age reported for first time, were considered as having had a myocardial infarction.
Leisure time physical activity was measured in SAMINOR 1 by the ‘Saltin-Grimby’ questionnaire.25 Overall physical activity at current age was measured in SAMINOR 2 by a scale ranging from 1 to 10; an instrument validated in middle aged women living in Tromsø, Norway.26
Alcohol consumption was measured in SAMINOR 1 by asking: ‘How often during the last year have you consumed alcohol?’ (Never/Not during the last year/A few times during the last year/1 time per month/2–3 times per month/1 time per week/2–3 times per week/4–7 times per week). To approximate the question in SAMINOR 2, we created two categories: never consumed alcohol and consumers of alcohol. In SAMINOR 2, alcohol consumption was asked as follows: ‘Do you practice total alcohol abstinence?’ (Yes/no).
Education was measured similarly in both surveys by years of education. We categorised the item to match roughly primary and lower secondary school, upper secondary school and higher education: ≤9 years, 10–12 years and ≥13 years.
Clinical examination
Trained staff conducted the clinical examination. Waist circumference was measured at the umbilicus when the participant was standing. Blood pressure was measured with digital oscillometric devices (SAMINOR 1: DINAMAP-R, Criticon, Tampa, Florida, USA; SAMINOR 2: CARESCAPE V100 monitor, GE Healthcare, Milwaukee, Wisconsin, USA), with the participant in a seated position. Following a 2 min rest, three recordings were made at 1 min intervals, and the average of the last two measurements was used in the analysis. Participants were considered to have hypertension if their systolic blood pressure was ≥140 mm Hg, or their diastolic blood pressure was ≥90 mm Hg, or if they reported using anti-hypertensive drugs.
In both surveys, non-fasting blood samples were collected. The blood samples were left to coagulate for a minimum of 30 min, after which they were centrifuged and serum was separated within 2 hours. In SAMINOR 1, serum was sent by overnight post and analysed consecutively for lipids (total cholesterol, high-density lipoprotein (HDL) cholesterol and triglycerides) with an enzymatic method (Hitachi 917 auto analyser, Roche Diagnostics, Switzerland) at Ullevål University Hospital, Oslo, Norway. In SAMINOR 2, serum samples were kept at −20°C before they were sent to the biobank at UiT The Arctic University of Norway, for further storage at −70°C. The samples were analysed in batches during autumn 2014 at the University Hospital of North Norway, Tromsø, Norway. Lipids were measured with an enzymatic colorimetric method (Cobas 8000B, Roche Diagnostics GmbH, Mannheim, Germany).
The 10-year absolute risk of fatal or non-fatal AMI or CS was estimated by the NORRISK 2 model27 and determined separately in women and men based on age, total cholesterol, HDL cholesterol, smoking status, systolic blood pressure and use of anti-hypertensive drugs.
Statistical analyses
Statistical analyses were done using STATA V.15.0. Sample characteristics were given by sex for Sami and non-Sami in SAMINOR 1 and SAMINOR 2: means (SD) of continuous variables and proportions (numbers) of categorical variables. In order to account for the partly overlapping samples, changes in population average means and prevalences of risk factors between SAMINOR 1 and SAMINOR 2 were estimated by sex- and ethnicity-specific linear or logistic generalised estimating equation regression models. Assumptions of normality and homoscedasticity were assessed by a visual inspection of residual plots. Changes in triglycerides and in the estimated 10-year risk of AMI or CS were log-transformed due to skewed distributions. All regression models were adjusted for age, and linear models were additionally adjusted for age squared. We assessed if changes in outcomes differed by ethnicity by including an interaction term between survey and ethnicity in sex-specific models. If the p value for interaction was >0.05, the interaction term was excluded from the model and an overall sex-specific mean/prevalence was reported. In the opposite case, ethnicity-specific changes were reported. Marginal means/prevalences were estimated at age 57.5 years in women and at 58.2 years in men, that is, the sex-specific mean ages in the overall sample. Two-way graphs illustrate how cardiovascular risk factors varied by age, ethnicity and survey (online supplementary figures S1 and S2). Potential heterogeneity by age in the overall models was assessed by comparing two strata divided at sex-specific mean age. The terms for interaction between ethnicity and survey remained non-significant across age strata for both sexes. Hence, we concluded that age did not modify the overall estimates of change in cardiovascular risk factors. We considered a two-sided p<0.05 to be significant.
Sensitivity analyses were done with same sex-stratified generalised estimating equation models by
Dividing the study sample into three groups: (1) those who reported ‘Sami’ for all 11 questions, (2) who reported Sami in 1–10 questions and (3) those who did not report Sami on any of the questions (non-Sami) (online supplementary tables S1 and S2).
Using the original ethnic categorisation, we adjusted for geographical regions: (1) Kautokeino and Karasjok, (2) Nesseby, Tana and Porsanger, (3) Kåfjord, Lyngen, Storfjord, Skånland and Evenes (online supplementary table S3).
bmjopen-2019-028939supp003.pdf (138KB, pdf)
Results
Of the total sample, 53.5% were women. In women and men, 37.8% and 39.5% were Sami, respectively. The mean age was higher in both sexes in SAMINOR 2 than in SAMINOR 1. In both surveys, Sami women (table 1) and men (table 2) were less physically active, and Sami women reported more often to be non-consumers or abstainers of alcohol.
Table 1.
Unadjusted means (SD) and proportions (%) of sample characteristics in women aged 40–79 years participating in SAMINOR 1 (2003–2004) and SAMINOR 2 (2012–2014)
| Ethnicity | SAMINOR 1 (n=3390) | SAMINOR 2 (n=3234) | ||
| Non-Sami | Sami | Non-Sami | Sami | |
| Proportions, % (n) | 64.7 (2193) | 35.3 (1197) | 59.7 (1929) | 40.4 (1305) |
| Age, mean (SD) | 56.5 (10.1) | 55.5 (10.2) | 59.1 (10.3) | 58.6 (10.4) |
| Self-reported myocardial infarction, % (n)*† | 2.6 (58) | 1.9 (23) | 3.2 (62) | 1.8 (23) |
| Physical activity using ‘Saltin-Grimby’ questionnaire* | ‡ | ‡ | ||
| Reading, watching television or other sedentary activity, % (n) | 21.3 (415) | 27.7 (297) | – | – |
| Walking, bicycling or moving around in other ways at least 4 hours/week, % (n) | 68.1 (1330) | 61.9 (664) | – | – |
| Participation in recreational sports, heavy garden work, etc. Duration at least 4 hours/week, % (n) | 10.3 (200) | 9.6 (103) | – | – |
| Participation in hard training or athletic competitions regularly and several times/week, % (n) | 0.4 (7) | 0.8 (8) | – | – |
| Level of physical activity on a scale from 1 to 10, mean (SD)* | ‡ | ‡ | 5.6 (2.1) | 5.2 (2.2) |
| Never consumed alcohol, % (n)* | 14.8 (309) | 24.5 (279) | ‡ | ‡ |
| Alcohol abstinence, yes % (n)* | ‡ | ‡ | 18.4 (341) | 27.0 (337) |
| Years of education, mean (SD)* | 10.9 (3.8) | 10.7 (4.6) | 12.2 (4.0) | 12.4 (4.5) |
| 0–9 years education, % (n) | 41.7 (864) | 43.6 (497) | 28.0 (530) | 30.3 (385) |
| 10–12 years education, % (n) | 30.2 (626) | 23.2 (265) | 29.9 (565) | 23.2 (295) |
| ≥13 years of education, % (n) | 28.1 (584) | 33.1 (378) | 42.1 (797) | 46.5 (592) |
| Region 1: Kautokeino and Karasjok, % (n) | 3.8 (84) | 44.8 (537) | 5.2 (101) | 48.4 (631) |
| Region 2: Nesseby, Tana and Porsanger, % (n) | 27.5 (603) | 38.3 (458) | 30.1 (580) | 36.6 (478) |
| Region 3: Kåfjord, Lyngen, Storfjord, Skånland and Evenes, % (n) | 68.7 (1506) | 16.9 (202) | 64.7 (1248) | 15.0 (196) |
*Based on a lower number due to missing values.
†Measured differently in SAMINOR 1 and SAMINOR 2.
‡Question not posed.
Table 2.
Unadjusted means (SD) and proportions (%) of sample characteristics in men aged 40–79 years participating in SAMINOR 1 (2003–2004) and SAMINOR 2 (2012–2014)
| Ethnicity | SAMINOR 1 (n=3027) | SAMINOR 2 (n=2722) | ||
| Non-Sami | Sami | Non-Sami | Sami | |
| Proportions, % (n) | 62.1 (1881) | 37.9 (1146) | 58.7 (1597) | 41.3 (1125) |
| Age, mean (SD) | 56.5 (9.8) | 56.3 (10.1) | 60.4 (10.2) | 59.8 (10.3) |
| Self-reported myocardial infarction, % (n)*† | 6.9 (130) | 6.5 (75) | 8.8 (140) | 8.1 (91) |
| Physical activity using ‘Saltin-Grimby’ questionnaire* | ‡ | ‡ | ||
| Reading, watching television or other sedentary activity, % (n) | 20.2 (351) | 24.3 (254) | – | – |
| Walking, bicycling or moving around in other ways at least 4 hours/week, % (n) | 59.5 (1034) | 53.0 (555) | – | – |
| Participation in recreational sports, heavy garden work etc. Duration at least 4 hours/week, % (n) | 18.6 (324) | 20.2 (212) | – | – |
| Participation in hard training or athletic competitions regularly and several times/week, % (n) | 1.7 (29) | 2.5 (26) | – | – |
| Level of physical activity on a scale from 1 to 10, mean (SD)* | ‡ | ‡ | 5.2 (2.01) | 5.12 (2.16) |
| Never consumed alcohol, % (n)* | 5.4 (99) | 4.5 (50) | ‡ | ‡ |
| Alcohol abstinence, yes % (n)* | ‡ | ‡ | 10.6 (164) | 13.4 (150) |
| Years of education, mean (SD)* | 10.9 (3.7) | 10.2 (4.1) | 11.8 (3.6) | 11.4 (3.8) |
| 0–9 years education, % (n) | 39.6 (719) | 47.3 (519) | 29.7 (467) | 36.3 (400) |
| 10–12 years education, % (n) | 32.7 (594) | 27.6 (303) | 33.1 (520) | 30.3 (333) |
| ≥13 years of education, % (n) | 27.7 (502) | 25.1 (276) | 37.2 (584) | 33.4 (368) |
| Region 1: Kautokeino and Karasjok, % (n) | 3.3 (63) | 37.9 (434) | 4.6 (73) | 42.4 (477) |
| Region 2: Nesseby, Tana and Porsanger, % (n) | 28.9 (543) | 39.0 (447) | 32.9 (525) | 37.2 (419) |
| Region 3: Kåfjord, Lyngen, Storfjord, Skånland and Evenes, % (n) | 67.8 (1275) | 23.1 (265) | 62.6 (999) | 20.4 (229) |
*Based on a lower number due to missing values.
†Measured differently in SAMINOR 1 and SAMINOR 2.
‡Question not posed.
Both non-Sami and Sami women had a decline in total cholesterol between SAMINOR 1 and SAMINOR 2 (p<0.001, table 3). The overall change in total cholesterol in women was −0.50 mmol/L. Sami women had lower HDL cholesterol and higher triglycerides than non-Sami in both surveys (table 3). The change in triglycerides did not differ by ethnicity, but the change in HDL cholesterol did, with non-Sami showing a minor increase, and Sami showing no change.
Table 3.
Age-adjusted predicted changes in means and prevalences of cardiovascular risk factors between the SAMINOR 1 (2003–2004) and SAMINOR 2 (2012–2014) in non-Sami and Sami women (n=6624)
| Linear regression | Non-Sami (n=4122) | Sami (n=2502) | Interaction† | Overall (n=6624) | |||
| β (95% CI) | P value | β (95% CI) | P value | P value | β (95% CI) | P value | |
| Total cholesterol, mmol/L | −0.51 (−0.57 to –0.45) | <0.001 | −0.47 (−0.55 to –0.39) | <0.001 | 0.86 | −0.50 (−0.54 to–0.45) | <0.001 |
| SAMINOR 1, mean‡ | 6.24 (6.19 to 6.30) | 6.24 (6.16 to 6.32) | 6.25 (6.20 to 6.29) | ||||
| SAMINOR 2, mean‡ | 5.73 (5.67 to 5.79) | 5.77 (5.70 to 5.85) | 5.75 (5.70 to 5.79) | ||||
| HDL cholesterol, mmol/L | 0.05 (0.03 to 0.07) | <0.001 | −0.02 (-0.04 to 0.01) | 0.14 | <0.001 | * | |
| SAMINOR 1, mean‡ | 1.51 (1.49 to 1.53) | 1.47 (1.45 to 1.49) | |||||
| SAMINOR 2, mean‡ | 1.56 (1.54 to 1.58) | 1.45 (1.43 to 1.48) | |||||
| Triglycerides, mmol/L§ | −0.02 (−0.05 to 0.004) | 0.10 | 0.03 (0.004 to 0.07) | 0.03 | 0.07 | 0.002 (−0.02 to 0.02) | 0.87 |
| SAMINOR 1, meanঠ| 1.43 (1.40 to 1.47) | 1.48 (1.43 to 1.53) | 1.45 (1.43 to 1.48) | ||||
| SAMINOR 2, meanঠ| 1.40 (1.37 to 1.44) | 1.53 (1.49 to 1.58) | 1.46 (1.43 to 1.48) | ||||
| Systolic blood pressure, mm Hg | −3.9 (−4.86 to–2.98) | <0.001 | −3.0 (−4.23 to –1.81) | <0.001 | 0.10 | −3.6 (−4.36 to –2.88) | <0.001 |
| SAMINOR 1, mean‡ | 134.7 (133.8 to 135.6) | 132.4 (131.2 to 133.7) | 133.9 (133.2 to 134.6) | ||||
| SAMINOR 2, mean‡ | 130.8 (129.9 to 131.7) | 129.4 (128.3 to 130.6) | 130.3 (129.6 to 131.0) | ||||
| Diastolic blood pressure, mm Hg | −0.9 (−1.38 to –0.33) | 0.002 | −1.1 (−1.77 to–0.46) | 0.001 | 0.39 | −1.0 (−1.39 to,–0.57) | <0.001 |
| SAMINOR 1, mean‡ | 73.9 (73.4 to 74.4) | 73.4 (72.7 to 74.1) | 73.7 (73.3 to 74.1) | ||||
| SAMINOR 2, mean‡ | 73.0 (72.5 to 73.6) | 72.3 (71.6 to 72.9) | 72.7 (72.3 to 73.2) | ||||
| Waist circumference, cm | 7.0 (6.41 to 7.49) | <0.001 | 6.1 (5.44 to 6.76) | <0.001 | 0.26 | 6.7 (6.24 to 7.07) | <0.001 |
| SAMINOR 1, mean‡ | 86.4 (85.83 to 87.00) | 88.0 (87.29 to 88.78) | 87.0 (86.55 to 87.45) | ||||
| SAMINOR 2, mean‡ | 93.3 (92.75 to 93.94) | 94.1 (93.43 to 94.85) | 93.7 (93.20 to 94.11) | ||||
| 10-Year risk of AMI or CS, %§ | −0.19 (−0.22 to –0.17) | <0.001 | −0.13 (−0.16 to –0.09) | <0.001 | 0.011 | * | |
| SAMINOR 1, meanঠ| 4.16 (4.05 to 4.26) | 3.91 (3.77 to 4.05) | |||||
| SAMINOR 2, meanঠ| 3.43 (3.33 to 3.52) | 3.44 (3.32 to 3.56) | |||||
| Logistic regression | OR (95% CI) | P value | OR (95% CI) | P value | P value | OR (95% CI) | P value |
| Anti-hypertensive treatment | 0.96 (0.85 to 1.09) | 0.51 | 0.98 (0.83 to 1.16) | 0.82 | 0.77 | 0.96 (0.87 to 1.07) | 0.47 |
| SAMINOR 1, prevalence %‡ | 24.0 (22.10 to 25.80) | 22.9 (20.34 to 25.36) | 23.6 (22.11 to 25.10) | ||||
| SAMINOR 2, prevalence %‡ | 23.2 (21.17 to 25.24) | 22.5 (20.04 to 24.98) | 23.0 (21.38 to 24.53) | ||||
| Hypertension | 0.77 (0.68 to 0.86) | <0.001 | 0.79 (0.68 to 0.93) | 0.003 | 0.56 | 0.77 (0.70 to 0.85) | <0.001 |
| SAMINOR 1, prevalence %‡ | 47.4 (45.12 to 49.72) | 44.5 (41.37 to 47.68) | 46.3 (44.47 to 48.20) | ||||
| SAMINOR 2, prevalence %‡ | 40.8 (38.39 to 43.25) | 38.9 (35.90 to 41.79) | 40.1 (38.18 to 41.94) | ||||
| Current smokers | 0.59 (0.53 to 0.66) | <0.001 | 0.74 (0.64 to 0.85) | <0.001 | 0.10 | 0.65 (0.59 to 0.71) | <0.001 |
| SAMINOR 1, prevalence %‡ | 31.0 (29.07 to 32.90) | 27.9 (25.28 to 30.45) | 29.8 (28.26 to 31.34) | ||||
| SAMINOR 2, prevalence %‡ | 21.0 (19.26 to 22.76) | 22.3 (20.07 to 24.46) | 21.6 (20.21 to 22.94) |
*ß coefficients are estimated by linear generalised estimating equation regression models and adjusted for age and age2. ORs are estimated by logistic generalised estimating equation regression models and adjusted for age.
*P value for interaction <0.05, only ethnicity-specific estimations are reported.
†Test of interaction between survey and ethnicity in overall model. If p value for interaction >0.05, interaction term was excluded from the overall model.
‡Predicted means/prevalences at age 57.5 years, which is the mean age for women in the overall sample.
§Outcome variables are log-transformed.
¶Predicted geometric means at age 57.5 years.
Number of missing values: total and HDL cholesterol and triglycerides were missing in 18 subjects; systolic and diastolic blood pressure were missing in four subjects; hypertension in three subjects. NORRISK 2 score was missing for 193 subjects. Excluding missing values did not ange the results.
AMI, acute myocardial infarction; CS, cerebral stroke; HDL, high-density lipoprotein.
In both surveys, Sami women had somewhat lower blood pressure than non-Sami did (table 3). The overall decline in systolic and diastolic blood pressure was 3.6 and 1.0 mm Hg (both p<0.001), respectively; these changes did not differ by ethnicity. Roughly, 23% of women reported use of anti-hypertensive drugs, and this did not change over time. The prevalence of hypertension declined in a similar magnitude in Sami and non-Sami women: by 6.2 percentage points (p<0.001) (table 3).
Non-Sami and Sami women had a similar increase of 6.7 cm in mean waist circumference. The prevalence of smoking in non-Sami and Sami women declined by 10.0 and 5.6 percentage points, respectively (both p<0.001); this change did not differ by ethnicity. Overall, the odds of current smoking declined by 35% (table 3).
The estimated 10-year risk of AMI or CS declined between SAMINOR 1 and SAMINOR 2 in both Sami and non-Sami women (both p<0.001, table 3), but more so in non-Sami.
Between SAMINOR 1 and SAMINOR 2, total cholesterol declined more in non-Sami than in Sami men (0.60 vs 0.43 mmol/L; both p<0.001, table 4), and this change varied by ethnicity. Between the surveys, Sami men had a slight decline in HDL cholesterol (p<0.001) and a slight increase in triglycerides (p<0.001); whereas non-Sami men had no changes, hence, changes in HDL cholesterol and triglyceride differed for Sami and non-Sami (table 4).
Table 4.
Age-adjusted predicted changes in means and in prevalences of cardiovascular risk factors between the SAMINOR 1 (2003–2004) and SAMINOR 2 (2012–2014) in non-Sami and Sami men (n=5749)
| Linear regression | Non-Sami (n=3478) | Sami (n=2271) | Interaction† | Overall (n=5749) | |||
| β (95% CI) | P value | β (95% CI) | P value | P value | β (95% CI) | P value | |
| Total cholesterol, mmol/L | −0.60 (–0.66 to –0.53) | <0.001 | −0.43 (–0.51 to –0.35) | <0.001 | 0.03 | * | |
| SAMINOR 1, mean‡ | 6.00 (5.95 to 6.07) | 6.00 (5.92 to 6.08) | |||||
| SAMINOR 2, mean‡ | 5.41 (5.35 to 5.48) | 5.58 (5.50 to 5.65) | |||||
| HDL cholesterol, mmol/L | −0.01 (-0.03 to 0.01) | 0.18 | −0.06 (-0.08 to –0.04) | <0.001 | 0.005 | * | |
| SAMINOR 1 mean‡ | 1.30 (1.28 to 1.31) | 1.28 (1.26 to 1.31) | |||||
| SAMINOR 2, mean‡ | 1.28 (1.26 to 1.30) | 1.22 (1.20 to 1.25) | |||||
| Triglycerides, mmol/L§ | 0.001 (-0.03 to 0.03) | 0.96 | 0.09 (0.05 to 0.13) | <0.001 | 0.001 | * | |
| SAMINOR 1, meanঠ| 1.61 (1.56 to 1.65) | 1.58 (1.53 to 1.64) | |||||
| SAMINOR 2, meanঠ| 1.61 (1.56 to 1.66) | 1.73 (1.67 to 1.79) | |||||
| Systolic blood pressure, mm Hg | −3.2 (–4.19 to –2.18) | <0.001 | −2.8 (–4.11 to –1.44) | <0.001 | 0.38 | −3.1 (–3.87 to –2.27) | <0.001 |
| SAMINOR 1 mean‡ | 137.0 (136.1 to 137.9) | 136.8 (135.5 to 138.1) | 136.9 (136.2 to 137.7) | ||||
| SAMINOR 2, mean‡ | 133.8 (132.8 to 134.8) | 134.0 (132.7 to 135.3) | 133.9 (133.1 to 134.6) | ||||
| Diastolic blood pressure, mm Hg | −0.5 (−1.08 to 0.11) | 0.11 | −1.1 (−1.82 to –0.33) | 0.004 | 0.08 | −0.7 (−1.20 to –0.28) | 0.002 |
| SAMINOR 1, mean‡ | 79.7 (79.2 to 80.2) | 79.9 (79.2 to 80.6) | 79.8 (79.4 to 80.2) | ||||
| SAMINOR 2, mean‡ | 79.2 (78.6 to 79.8) | 78.9 (78.2 to 79.5) | 79.1 (78.6 to 79.5) | ||||
| Waist circumference, cm | 6.0 (5.45 to 6.56) | <0.001 | 5.9 (5.22 to 6.48) | <0.001 | 0.37 | 5.9 (5.50 to 6.31) | <0.001 |
| SAMINOR 1, mean‡ | 94.4 (93.82 to 94.90) | 93.1 (92.45 to 93.79) | 93.9 (94.48 to 94.32) | ||||
| SAMINOR 2, mean‡ | 100.4 (99.78 to 100.95) | 99.0 (98.29 to 99.64) | 99.8 (99.36 to 100.24) | ||||
| 10-year risk of AMI or CS, %§ | −0.19 (–0.22 to –0.17) | <0.001 | −0.16 (–0.19 to –0.12) | <0.001 | 0.23 | −0.18 (–0.20 to –0.16) | <0.001 |
| SAMINOR 1, meanঠ| 8.73 (8.52 to 8.95) | 8.75 (8.45 to 9.04) | 8.74 (8.57 to 8.92) | ||||
| SAMINOR 2, meanঠ| 7.20 (7.00 to 7.40) | 7.48 (7.23 to 7.73) | 7.32 (7.17 to 7.48) | ||||
| Logistic regression | OR (95% CI) | P value | OR (95% CI) | P value | P value | OR (95% CI) | P value |
| Anti-hypertensive treatment | 1.19 (1.03 to 1.36) | 0.02 | 1.15 (0.97 to 1.37) | 0.11 | 0.37 | 1.17 (1.06 to 1.31) | 0.003 |
| SAMINOR 1, prevalence %‡ | 21.4 (19.48 to 23.28) | 20.7 (18.34 to 23.11) | 21.1 (19.60 to 22.56) | ||||
| SAMINOR 2, prevalence %‡ | 24.4 (22.15 to 26.67) | 23.1 (20.53 to 25.74) | 23.9 (22.18 to 25.60) | ||||
| Hypertension | 0.94 (0.83 to 1.06) | 0.32 | 0.89 (0.77 to 1.04) | 0.13 | 0.39 | 0.92 (0.83 to 1.01) | 0.08 |
| SAMINOR 1, prevalence %‡ | 51.0 (48.62 to 53.42) | 50.4 (47.43 to 53.43) | 50.7 (48.84 to 52.63) | ||||
| SAMINOR 2, prevalence %‡ | 49.4 (46.83 to 52.01) | 47.5 (44.39 to 50.51) | 48.6 (46.61 to 50.57) | ||||
| Current smokers | 0.51 (0.44 to 0.58) | <0.001 | 0.59 (0.51 to 0.69) | <0.001 | 0.27 | 0.54 (0.49 to 0.60) | <0.001 |
| SAMINOR 1, prevalence %‡ | 30.4 (28.35 to 32.50) | 30.8 (28.16 to 33.45) | 30.7 (29.06 to 32.35) | ||||
| SAMINOR 2, prevalence %‡ | 18.1 (16.30 to 19.97) | 20.8 (18.55 to 23.12) | 19.4 (17.94 to 20.81) |
β coefficients are estimated by linear generalised estimating equation regression models and adjusted for age and age2. ORs are estimated by logistic generalised estimating equation regression models and adjusted for age.
*P value for interaction <0.05, only ethnicity-specific estimations are reported.
†Test of interaction between survey and ethnicity in overall model. If p value for interaction >0.05, interaction term is excluded from the overall model.
‡Predicted means/prevalences at age 58.2 years, which is the mean age for men in the overall sample.
§Outcome variables are log-transformed.
¶Predicted geometric means at age 58.2 years.
Number of missing values: total and HDL cholesterol were missing in 12 subjects; triglycerides were missing in 13 subjects, systolic and diastolic blood pressure and hypertension was missing in one subject. NORRISK 2 score was missing for 173 subjects. Excluding missing values did not change the results.
AMI, acute myocardial infarction; CS, cerebral stroke; HDL, high-density lipoprotein.
In men, the decline in systolic and diastolic blood pressure did not differ by ethnicity (table 4). The overall decline in systolic and diastolic blood pressure in men were 3.1 and 0.7 mm Hg (both p<0.05), respectively. Overall, we found an increase in the prevalence of anti-hypertensive drug use, from 21.1% to 23.9% in men, which did not differ by ethnicity. The prevalence of hypertension remained similar in SAMINOR 1 and SAMINOR 2, with roughly half of men being considered hypertensive (table 4).
Waist circumference increased similarly in Sami and non-Sami men, with an overall increase of 5.9 cm (p<0.001). The prevalence of smoking declined similarly in non-Sami and Sami men, by 12.3 and 10.0 percentage points (both p<0.001), respectively. The overall decline in the odds of being a smoker was 46%.
The estimated 10-year risk of AMI or CS declined in non-Sami and Sami men (both p<0.001, table 4), but not differently in the two ethnic groups.
Sensitivity analyses
Overall, the sensitivity analyses were consistent with the main findings when using a different ethnic categorisation (online supplementary tables S1 and S2) and when adjusting for region (online supplementary table S3).
Discussion
From SAMINOR 1 (2003–2004) to SAMINOR 2 (2012–2014), participants from the selected 10 municipalities in Northern Norway had a favourable decline in total cholesterol, blood pressure, proportion of smokers and the estimated 10-year risk of AMI or CS, whereas waist circumference increased. The changes in total cholesterol (men only), HDL cholesterol (both sexes), triglycerides (men only) and the estimated 10-year risk of AMS or CS (women only), were statistically significantly different between Sami and non-Sami. The odds of anti-hypertensive drug use increased only in men, whereas the prevalence of hypertension decreased only in women. To our knowledge, there are no other studies in Sápmi that explore whether changes in cardiovascular risk factors differ between Sami and non-Sami over time.
In both SAMINOR 1 and SAMINOR 2, the participation rate was lowest among the youngest participants, especially young men. In both surveys, less than half of those invited participated, hence, selection bias might be an issue. Also, as there is no official registry on ethnicity, we do not know if non-participation differed by ethnicity. It might be expected that Sami would be less willing to participate, given the history of assimilation15 and unethical research.28 On the other hand, as the surveys were carried out by a Sami research centre, invitees with Sami affiliations might have been more motivated to participate. If that is the case, the slightly adverse pattern in Sami, might be partly due to a different selection of Sami compared with non-Sami participants.
Further, due to design issues of SAMINOR 1,22 the study sample included a lower proportion of participants from Sami-dominated municipalities in Finnmark, while the same municipalities had an overall high response rate in SAMINOR 2. This influences the ethnic and regional compositions of the two samples, and makes comparisons between the surveys challenging. However, when using a different categorisation of ethnicity or adjusting for region, the results remained consistent with the main results. Moreover, generalisation to the entire Sami and non-Sami populations in Northern Norway is not advised, as only 10 municipalities were included. However, assuming a similar response rate in Sami and non-Sami participants, we believe the findings are applicable to Sami and non-Sami women and men over 50 years of age living in the given geographical regions.
The use of antihypertensive drugs increases with age2 and during 1975–2010, the prevalence of treatment for hypertension increased by a factor of four in Norway.29 In our study, the use of anti-hypertensive drugs in women remained similar in the surveys, whereas the prevalence of hypertension in women declined, which corresponds to a decline that is independent of treatment with anti-hypertensive drugs.2 In men, we observed an increase in the use of anti-hypertensive drugs, whereas the prevalence of hypertension remained the same, which may indicate that treatment with anti-hypertensive drugs could have contributed to a decline in blood pressure.
The observed decreases in cholesterol, systolic blood pressure and proportion of smokers, and the increase in waist circumference, corresponds well with studies in Western Europe3 4 6 7 and with national trends.1 2 5 8 11 30 Possible explanations are changes in lifestyle and diet—in line with what is observed nationally11—decreases in smoking, less occupational physical activity, more frequent use of vehicles for transportation, higher consumption of fruits and vegetables, lower consumption of saturated fats and an assumed lower consumption of salt.31 The decrease in systolic blood pressure may have been halted due to the increase in obesity over the last decades.32
In a cohort study in Finnmark (1987–2003), based on a follow-up of those participating in both the Finnmark 3 and SAMINOR 1 surveys, Hermansen et al 33 observed—using the same ethnicity definition as in our study—that changes in cardiovascular risk factors according to change in physical activity level occurred independently of ethnicity. Similarly, we observed that changes in cardiovascular risk factors did not differ substantially by ethnicity, only small and probably negligible differences were observed in total cholesterol and triglycerides in men, and in HDL cholesterol in both sexes, which suggests that Sami and non-Sami populations overall have undergone similar lifestyle changes. This might be considered unexpected, as Sami may be perceived as distinct from non-Sami in terms of diet34 35 and physical activity.33 A recent study from SAMINOR 2 found that participants who defined themselves solely as Sami had a lower consumption of vegetables, and a higher consumption of moose meat, reindeer meat and fat spread on bread than non-Sami and those who regard themselves as both Sami and non-Sami.34 In SAMINOR 1 (24 municipalities included), a higher consumption of unfiltered coffee was observed in Sami participants compared with non-Sami and Sami of mixed ethnic descent.35 Furthermore, unpublished results from SAMINOR 2 (Borch, personal communication, 2018), show that, in women, Sami ethnicity was associated with lower total physical activity. In the cohort study by Hermansen et al, the proportion of leisure-time sedentary individuals in Finnmark decreased between 1987 and 2003; however, the proportions who were sedentary was higher in Sami than in non-Sami, both at baseline and at the end of follow-up.33 Nonetheless, evidence of relevant ethnic differences in changes in cardiovascular risk factors and estimated 10-year risk of AMI and CS, was not found in our study.
The observed decline in cardiovascular risk factors is likely to have a beneficial impact on the incidence of coronary heart diseases36 and ischaemic stroke37 in this population, which is also reflected by a decrease in the estimated 10-year risk of AMI or CS. The decrease in risk was smaller in Sami than non-Sami women, which might be due to the increase in HDL cholesterol in non-Sami women. However, the causal effect of low levels of HDL cholesterol on cardiovascular disease is debated.38 39
Inuit populations are characterised by a rapid increase in obesity, diabetes and hypertension in parallel with decreasing physical activity and deterioration of the lipid profile.40 On the other hand, decline in smoking and alcohol use have been observed.40 But still, there are disparities in cardiovascular health between Indigenous peoples and their benchmark populations in high-income countries.40 41 Our study indicated that such disparities in cardiovascular risk factors are not present in the 10 rural municipalities in Northern Norway. Previous studies have also shown similar burdens of cardiovascular risk factors and morbidity among Sami and non-Sami in Norway.17–21 This might be due to the fact that the non-Sami reference population in these studies17–21 lives side by side with the Sami in the same rural regions. This is a stark contrast to, for instance, the Inuit and reference Danish population, who live on different continents. If we had compared the Sami in this study to the general Norwegian population, we might have found larger differences in cardiovascular risk factors, as there are disparities in health issues across regions.11 Second, the small or non-existent disparities in health between Sami and non-Sami are suggested to be due to similar access to healthcare and education,42 whereas the lack of similar access has been put forward as a reason for health disparities between the Inuit and their reference population.40 In summary, differences in settlement patterns and in the social determinants of health challenge our ability to compare our results with international data.
We were not able to adjust for lipid-lowering drugs, physical activity, coffee and alcohol consumption, affiliation with reindeer herding, or diet in our study, as questions relating to these items in the two surveys were not comparable. Lipid-lowering drugs are estimated to account for approximately 20%–30% of the decline in total cholesterol over time,5 6 and therefore it is likely that some of the decline in cholesterol is due to the use of these drugs. The public health relevance of this study is that preventive measures aimed to reduce cardiovascular risk seem to have worked independent of ethnicity. Nevertheless, further surveillance of cardiovascular risk factors is advisable due to the adverse pattern—although minor—in Sami compared with non-Sami.
Conclusion
From SAMINOR 1 (2003–2004) to SAMINOR 2 (2012–2014), the population in rural Northern Norway had a favourable decline in total cholesterol, blood pressure, hypertension (women only), smoking and the estimated 10-year risk of AMI or CS; however, they had an increase in waist circumference. We found only minor differences between Sami and non-Sami subjects regarding change in cardiovascular risk factors during this period, which suggests that the population of Northern Norway have had similar changes in lifestyle and diet.
bmjopen-2019-028939supp001.pdf (134.3KB, pdf)
bmjopen-2019-028939supp002.pdf (138KB, pdf)
Supplementary Material
Acknowledgments
The authors thank the participants of the SAMINOR 1 and SAMINOR 2.
Footnotes
Contributors: The study was conceived by BME and TB. SRAS performed all the data analyses, produced the tables and drafted the manuscript. MM produced the figure. TB guided and assisted with statistical analyses. BME, BKJ, MM, ARB, VLM and TB helped with the interpretation of the results, and contributed to the revision of the manuscript and approved the final version.
Funding: SAMINOR 1 and SAMINOR 2 were financed by the Norwegian Ministry of Health and Care Services. SAMINOR 2 was also financially supported by the Northern Norway Regional Health Authority; the Regional Research Fund of Northern Norway; the Sami Parliament; the Sami Norwegian National Advisory Unit on Mental Health and Substance Use; Finnmark, Troms, and Nordland county councils.
Competing interests: None declared.
Ethics approval: The Norwegian Data Inspectorate and the Regional Committee for Medical and Health Research Ethics for region North (REC North) have approved The SAMINOR Study which SAMINOR 1 survey and SAMINOR 2 surveys are part of. The REC North (2015/2204–11) have approved this study. All participants included in this study gave written informed consent and consented to linkage between the surveys.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data are available upon reasonable request.
Patient consent for publication: Not required.
Map disclaimer: The depiction of boundaries on the map(s) in this article do not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. The map(s) are provided without any warranty of any kind, either express or implied.
References
- 1. Holmen J, Holmen TL, Tverdal A, et al. . Blood pressure changes during 22-year of follow-up in large general population - the HUNT Study, Norway. BMC Cardiovasc Disord 2016;16:94 10.1186/s12872-016-0257-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hopstock LA, Bønaa KH, Eggen AE, et al. . Longitudinal and secular trends in blood pressure among women and men in birth cohorts born between 1905 and 1977: The Tromsø Study 1979 to 2008. Hypertension 2015;66:496–501. 10.1161/HYPERTENSIONAHA.115.05925 [DOI] [PubMed] [Google Scholar]
- 3. Danaei G, Finucane MM, Lin JK, et al. . National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5·4 million participants. Lancet 2011;377:568–77. 10.1016/S0140-6736(10)62036-3 [DOI] [PubMed] [Google Scholar]
- 4. Zhou B, Bentham J, Di Cesare M, et al. . Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet 2017;389:37–55. 10.1016/S0140-6736(16)31919-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hopstock LA, Bønaa KH, Eggen AE, et al. . Longitudinal and secular trends in total cholesterol levels and impact of lipid-lowering drug use among Norwegian women and men born in 1905-1977 in the population-based Tromsø Study 1979-2016. BMJ Open 2017;7:e015001 10.1136/bmjopen-2016-015001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Eriksson M, Forslund AS, Jansson JH, et al. . Greater decreases in cholesterol levels among individuals with high cardiovascular risk than among the general population: the northern Sweden MONICA study 1994 to 2014. Eur Heart J 2016;37:1985–92. 10.1093/eurheartj/ehw052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Farzadfar F, Finucane MM, Danaei G, et al. . National, regional, and global trends in serum total cholesterol since 1980: systematic analysis of health examination surveys and epidemiological studies with 321 country-years and 3·0 million participants. Lancet 2011;377:578–86. 10.1016/S0140-6736(10)62038-7 [DOI] [PubMed] [Google Scholar]
- 8. Jenum A, Graff-Iversen S, Selmer R, et al. . Risikofaktorer for hjerte- og karsykdom og diabetes gjennom 30 år [Risk factors for cardiovascular diseases and diabetes through 30 years]. Tidsskr Nor Laegeforen 2007;127:2532–6. [PubMed] [Google Scholar]
- 9. Capewell S, Ford ES. Why have total cholesterol levels declined in most developed countries? BMC Public Health 2011;11:641 10.1186/1471-2458-11-641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Aburto NJ, Ziolkovska A, Hooper L, et al. . Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ 2013;346:f1326 10.1136/bmj.f1326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Folkehelserapporten. Helsetilstanden i Norge [Public health report 2014, the health in Norway]. Oslo: Norwegian Institute of Public Health; 2014 [Norwegian], 2014. [Google Scholar]
- 12. Aubert V. Artikler fra Statistisk sentralbyrå. Den samiske befolkning i Nord-Norge [The Sami population in Northern Norway]. Oslo: Statistics Norway, 1978. Report No.: 107 [Norwegian]. [Google Scholar]
- 13. Statistics Norway. Samiske forhold [Conditions for the Sami] Oslo: Statistics Norway [Norwegian]. https://www.ssb.no/befolkning/statistikker/samisk (cited 2018.05.05).
- 14. Sametingets valgmanntall. 2017 per 30.06.2017 [The Sami parliament census for 2017 per 2017.06.30]: The Sami Parliament [Norwegian]; 2017 [updated 2017.09.25. https://www.sametinget.no/Valg/Valgmanntall/Sametingets-valgmanntall-2017 (cited 2018.08.05).
- 15. Minde H. Assimilation of the Sami – Implementation and Consequences1. Acta Borealia 2003;20:121–46. 10.1080/08003830310002877 [DOI] [Google Scholar]
- 16. Niemi E. The Finns in Northern Scandinavia and minority policy Tägil S, Ethnicity and nation building in the Nordic world. London: Hurst, 1995:145–78. [Google Scholar]
- 17. Eliassen B-M, Graff-Iversen S, Braaten T, et al. . Prevalence of self-reported myocardial infarction in Sami and non-Sami populations: the SAMINOR study. Int J Circumpolar Health 2015;74:24424 10.3402/ijch.v74.24424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Eliassen B-M, Graff-Iversen S, Melhus M, et al. . Ethnic difference in the prevalence of angina pectoris in Sami and non-Sami populations: the SAMINOR study. Int J Circumpolar Health 2014;73:21310 10.3402/ijch.v73.21310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Njølstad I, Arnesen E, Lund-Larsen PG. Cardiovascular diseases and diabetes mellitus in different ethnic groups: the Finnmark study. Epidemiology 1998;9:550–6. 10.1097/00001648-199809000-00014 [DOI] [PubMed] [Google Scholar]
- 20. Nystad T, Utsi E, Selmer R, et al. . Distribution of apoB/apoA-1 ratio and blood lipids in Sami, Kven and Norwegian populations: the SAMINOR study. Int J Circumpolar Health 2008;67:69–83. 10.3402/ijch.v67i1.18238 [DOI] [PubMed] [Google Scholar]
- 21. Njølstad I, Arnesen E, Lund-Larsen PG. Body height, cardiovascular risk factors, and risk of stroke in middle-aged men and women. A 14-year follow-up of the Finnmark study. Circulation 1996;94:2877–82. [DOI] [PubMed] [Google Scholar]
- 22. Lund E, Melhus M, Hansen KL, et al. . Population based study of health and living conditions in areas with both Sámi and Norwegian populations--the SAMINOR study. Int J Circumpolar Health 2007;66:113–28. 10.3402/ijch.v66i2.18241 [DOI] [PubMed] [Google Scholar]
- 23. Broderstad AR, Hansen S, Melhus M. The second clinical survey of the population-based study on health and living conditions in regions with Sami and Norwegian populations - the SAMINOR 2 Clinical Survey: Performing indigenous health research in a multiethnic landscape. Scand J Public Health 2019:140349481984557 10.1177/1403494819845574 [DOI] [PubMed] [Google Scholar]
- 24. Pettersen T, Brustad M. Same Sámi? A comparison of self-reported Sámi ethnicity measures in 1970 and 2003 in selected rural areas in northern Norway. Ethn Racial Stud 2015;38:2071–89. 10.1080/01419870.2015.1031262 [DOI] [Google Scholar]
- 25. Grimby G, Börjesson M, Jonsdottir IH, et al. . The "Saltin-Grimby Physical Activity Level Scale" and its application to health research. Scand J Med Sci Sports 2015;25(Suppl.):119–25. 10.1111/sms.12611 [DOI] [PubMed] [Google Scholar]
- 26. Borch KB, Ekelund U, Brage S, et al. . Criterion validity of a 10-category scale for ranking physical activity in Norwegian women. Int J Behav Nutr Phys Act 2012;9:2 10.1186/1479-5868-9-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Selmer R, Igland J, Ariansen I, et al. . NORRISK 2: A Norwegian risk model for acute cerebral stroke and myocardial infarction. Eur J Prev Cardiol 2017;24:773–82. 10.1177/2047487317693949 [DOI] [PubMed] [Google Scholar]
- 28. Kyllingstad JR. Norwegian Physical Anthropology and the Idea of a Nordic Master Race. Curr Anthropol 2012;53(S5):S46–56. 10.1086/662332 [DOI] [Google Scholar]
- 29. Blix HS, Landmark K, Selmer R, et al. . [Patterns in the prescription of antihypertensive drugs in Norway, 1975-2010]. Tidsskr Nor Laegeforen 2012;132:1224–8. 10.4045/tidsskr.11.0984 [DOI] [PubMed] [Google Scholar]
- 30. Jacobsen BK, Aars NA. Changes in waist circumference and the prevalence of abdominal obesity during 1994-2008 - cross-sectional and longitudinal results from two surveys: the Tromsø Study. BMC Obes 2016;3:41 10.1186/s40608-016-0121-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Directory of Health. Utvikling av norsk kosthold 2014. [Development in Norwegian nutrion 2014]. Report No. IS-2680 [Norwegian]. 2017. https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/802/Utviklingen-i-norsk-kosthold-2014-IS-2255.pdf (cited 2018.09.20).
- 32. Goff DC, Gillespie C, Howard G, et al. . Is the obesity epidemic reversing favorable trends in blood pressure? Evidence from cohorts born between 1890 and 1990 in the United States. Ann Epidemiol 2012;22:554–61. 10.1016/j.annepidem.2012.04.021 [DOI] [PubMed] [Google Scholar]
- 33. Hermansen R, Broderstad AR, Jacobsen BK, et al. . The impact of changes in leisure time physical activity on changes in cardiovascular risk factors: results from The Finnmark 3 Study and SAMINOR 1, 1987-2003. Int J Circumpolar Health 2018;77:1459145 10.1080/22423982.2018.1459145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Petrenya N, Skeie G, Melhus M, et al. . Food in rural northern Norway in relation to Sami ethnicity: the SAMINOR 2 Clinical Survey. Public Health Nutr 2018;21:2665–77. 10.1017/S1368980018001374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Nystad T, Melhus M, Brustad M, et al. . The effect of coffee consumption on serum total cholesterol in the Sami and Norwegian populations. Public Health Nutr 2010;13:1818–25. 10.1017/S1368980010000376 [DOI] [PubMed] [Google Scholar]
- 36. Mannsverk J, Wilsgaard T, Mathiesen EB, et al. . Trends in modifiable risk factors are associated with declining incidence of hospitalized and nonhospitalized acute coronary heart disease in a population. Circulation 2016;133:74–81. 10.1161/CIRCULATIONAHA.115.016960 [DOI] [PubMed] [Google Scholar]
- 37. Vangen-Lønne AM, Wilsgaard T, Johnsen SH, et al. . Declining incidence of ischemic stroke: what is the impact of changing risk factors? the Tromsø Study 1995 to 2012. Stroke 2017;48:544–50. [DOI] [PubMed] [Google Scholar]
- 38. Rader DJ, Hovingh GK. HDL and cardiovascular disease. Lancet 2014;384:618–25. 10.1016/S0140-6736(14)61217-4 [DOI] [PubMed] [Google Scholar]
- 39. Wu Z, Lou Y, Qiu X, et al. . Association of cholesteryl ester transfer protein (CETP) gene polymorphism, high density lipoprotein cholesterol and risk of coronary artery disease: a meta-analysis using a Mendelian randomization approach. BMC Med Genet 2014;15:118 10.1186/s12881-014-0118-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tvermosegaard M, Dahl-Petersen IK, Nielsen NO, et al. . Cardiovascular disease susceptibility and resistance in circumpolar inuit populations. Can J Cardiol 2015;31:1116–23. 10.1016/j.cjca.2015.06.002 [DOI] [PubMed] [Google Scholar]
- 41. Cameron VA, Faatoese AF, Gillies MW, et al. . A cohort study comparing cardiovascular risk factors in rural Māori, urban Māori and non-Māori communities in New Zealand. BMJ Open 2012;2:e000799 10.1136/bmjopen-2011-000799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Brustad M. The Health of the Sámi - A knowledge summary of published findings from population studies in Norway : Broderstad EG, Brustad M, Kalstad JA, Sámi Figures Reveal 2 - Annotated Sámi statistics 2009. Guovdageaidnu, 2009. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-028939supp003.pdf (138KB, pdf)
bmjopen-2019-028939supp001.pdf (134.3KB, pdf)
bmjopen-2019-028939supp002.pdf (138KB, pdf)


