Abstract
Introduction
Multiple rehabilitation therapies have been reported to be effective for poststroke balance impairment. However, the comparative effectiveness of these rehabilitation therapies is still unclear. Therefore, the aim of this study is to summarise evidence and identify the most effective rehabilitation therapy for poststroke balance impairment.
Methods and analysis
The following databases will be searched: China Biology Medicine, China National Knowledge Infrastructure, Wan Fang Data, the Chinese Science and Technology Periodical Database, Medline, Excerpt Medical Database (EMBASE), Web of Science, the Cochrane Library, from inception to June 2019. All randomised controlled trials that have used rehabilitation interventions to treat poststroke balance impairment will be included. The primary outcomes are the Berg Balance Scale, the Fugl-Meyer Assessment (balance), the Postural Assessment Scale for Stroke, as well as the function in sitting test, the Sitting Balance Scale, the Ottawa Sitting Scale, the Activities-specific Balance Confidence Scale, the Overall Balance Index and the Brunel Balance Assessment. The secondary outcomes include the Barthel Index, the Functional Ambulation Category Scale, fall rates, the Timed Up and Go test, the MOS 36-Item Short-Form Health Survey, and adverse events. To ensure that all relevant studies are included without personal bias, study selection, data extraction and quality assessment will be performed independently by two reviewers. Risk of bias will be assessed with the Cochrane risk of bias assessment tool. Review Manager V.5.3 software will be used to make bias risk diagram and pairwise meta-analysis, while network data synthesis will be performed using WinBUGS V.1.4.3 and R software.
Ethics and dissemination
Ethics approval is not required for systematic review and network meta-analysis. The results will be submitted to a peer review journal or at a conference.
Trial registration number
PROSPERO (CRD 42018107441).
Keywords: rehabilitation medicine, stroke medicine, therapeutics, complementary medicine
Strengths and limitations of this study.
This study will be the first network meta-analysis to compare the effectiveness and safety of different rehabilitation therapies for poststroke balance impairment.
The results of this study will provide evidence for the management of balance impairment and help the therapists and patients to choose suitable treatment.
To make sure that all relevant studies will be included without personal bias, two reviewers will perform the study selection, data extraction and quality assessment independently.
Although both electronic search and hand search will be performed in this study, potential unpublished trials are inevitable. To overcome this limitation, experts in this field will be consulted for unpublished trials.
Owing to the difficulty in locating all the effective rehabilitation therapies for poststroke balance impairment, we will review the guidelines and consult experts for recommended rehabilitation therapies.
Introduction
Stroke is a common clinical cerebrovascular disease, with high morbidity, mortality and disability rates, that bring a heavy economic burden to society and families.1–3 Balance is the ability to maintain the line of gravity within the base of support with minimal postural sway.4 The control of human balance is a comprehensive process relying on the integration of visual, vestibular and somatosensory inputs to the central nervous system. It is reported that about 83% of stroke survivors suffer from balance impairment. Balance impairment is characterised by short supporting time and differences between two sides of the body and slow walking speed, which may increase the risk of falls.5 Fear of falling can contribute to a sedentary lifestyle and increased disability, which means lower quality of life.6 Falling often leads to longer hospital stay, more medical and nursing costs, and economic losses directly or indirectly. In China, annual medical expenses caused by cerebrovascular falls exceed 5 billion yuan, resulting in a direct or indirect social cost of approximately 160 to 800 billion yuan.7 Therefore, management of balance impairment is challenging for patients who had a stroke.
Numerous rehabilitation therapies have been used to improve the ability to balance of patients who had a stroke including whole body vibration (WBV),8 virtual reality (VR),9 10 exercise,11 mirror therapy (MT),12–14 traditional Chinese medicine (TCM),15 traditional Chinese exercise (TCE),16–18 ankle-foot orthosis (AFO)19 and so on. WBV is able to improve results of the Functional Reach Test and the Timed Up and Go (TUG) test, which have a positive effect on the balance and gait function of patients who had a stroke.20 Results of an RCT concluded that VR is an effective rehabilitation therapy which can improve postural balance and upper extremity function in patients who had a stroke.21 Exercises such as bilateral upper extremity exercises,22 step climbing exercise23 and trampoline training24 are beneficial to the ability to balance and for fall prevention. Recent systematic reviews and meta-analyses showed that MT can improve balance, mobility, gait speed and motor function compared with control groups.12–14 AFO is capable of improving gait and balance in patients with balance impairment after a stroke.25 Acupuncture is an important part of TCM, which has been used to restore limb movement and balance disability in patients who had a stroke.15 Results from several meta-analyses showed that TCE including Tai Chi, Baduanjin, Yijinjing, Liuzijue and so on, can effectively enhance the ability to balance by increasing the Berg Balance Scale (BBS) Score and reducing the rate of falls.16
Based on these grounds, we raise an important clinical question: among these rehabilitation therapies, which is the most comparatively effective and safe therapy to enhance the ability to balance in patients who had a stroke. Different from traditional pairwise meta-analysis, network meta-analysis (NMA) is capable of summarising the direct and indirect evidence and evaluate the relative efficacy of multiple treatment comparisons. What is more, NMA is able to provide the ranking of treatment options based on their effectiveness. Therefore, to help physiotherapists and patients make a better choice for improving balance, a systematic review and NMA should be conducted to summarise the evidence of various rehabilitation therapies and to identify the most effective rehabilitation therapy for poststroke balance impairment.
Methods
The protocol of this systematic review will be reported in accordance with the Preferred Reporting Item for Systematic Review and Meta-analysis Protocols guidelines. The review process is shown in figure 1.
Figure 1.
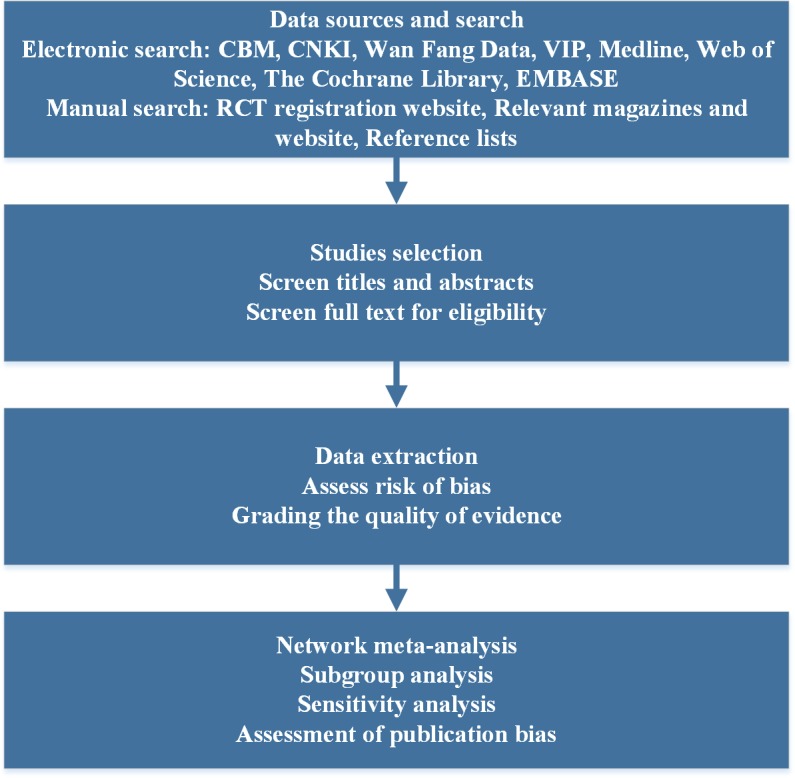
Flow chart of network meta-analysis for rehabilitation of balance impairment in patients who had a stroke. CBM, China Biology Medicine; CNKI, China National Knowledge Infrastructure; RCT, randomised controlled trial; VIP, the Chinese Science and Technology Periodical Database.
Inclusion criteria
Type of studies
Only randomised controlled trials (RCTs) will be included. Trials without a control group or those with quasi-random allocation will be excluded. There are no restrictions on language or publication date.
Types of participants
We will include RCTs that involved patients who had a stroke diagnosed according to the stroke diagnostic criteria formulated by The Fourth National Cerebrovascular Disease Conference in 1995,26 A Guide to the Prevention and Treatment of Chinese Cerebrovascular Disease developed by the Chinese Medical Association in 2005,27 and Standard for the Diagnosis and Evaluation of Stroke Difficulties formulated by the Encephalopathy Emergency Team of the State Administration of TCM in 1996.28 Diagnoses of stroke are summarised as following: clear stroke history and manifestations, supported by imaging examination such as cranial plain CT scan or MRI. There will be no restriction on age, sex and race.
Types of interventions
Experts were consulted for the recommended rehabilitation therapies. There are many kinds of rehabilitation therapies for poststroke balance impairment including TCM therapies (such as acupuncture, moxibustion, Tai Chi and so on) and modern rehabilitation therapies (which refer to physical therapies defined by the World Confederation for Physical Therapy (http://www.wcpt.org/policy/ps-descriptionPT)), typically including balance-specific activities (such as balance exercises, weight shift training and so on), more general activities (such as strengthening exercises, gait activities and so on), biofeedback, WBV, VR, MT, orthosis and so on.
Outcome measurements
Primary outcomes will focus on balance ability. Secondary outcomes will include functional ambulatory ability as well as quality of life.
Primary outcomes
The primary outcomes include BBS, the Postural Assessment Scale for Stroke (PASS) and the Fugl-Meyer Assessment (FMA(balance)),29 as well as the function in sitting test (FIST), the Sitting Balance Scale (SBS), the Ottawa Sitting Scale, the Activities-specific Balance Confidence (ABC) Scale, the Overall Balance Index (OBI) and the Brunel Balance Assessment (BBA).
The BBS assesses the functional postural abilities of patients in several conditions (lying on the back, sitting, standing, leaning forward, change of position and so on). This scale comprises 14 items. The maximal score, reflecting the best functional postural abilities, is 56 points.30–32 The FMA (balance) as a method for assessing the balance was developed from the Brunnstrom level 6 functional grading. This 3-level scale is composed of 7 items. The maximal score is 14 points. A lower score means more severe balance impairment.33 PASS was developed specifically for assessing balance in patients who had a stroke. PASS demonstrates high reliability,34 favourable individual item agreement35 and high test-retest reliability.36 37 Both FIST and SBS are scales related to sitting. FIST is a performance-based measure to examine deficits in seated postural control, which consists of 14 items,38 while SBS measures sitting balance for frail older adults.39 The ABC Scale is a balance confidence evaluation method, requiring participants to choose one percentage point on the scale from 0% to 100% for 16 items.40 The OBI is an index for evaluating the ability of balance control in all directions.41 The BBA is a measure of poststroke balance disability, which consists of 12 items in three areas (sitting balance, standing balance, walking function).42
Secondary outcomes
The secondary outcomes will include the Barthel Index (BI), The Functional Ambulation Category (FAC) Scale, fall rates, TUG, the medical outcomes study (MOS) 36-Item Short-Form Health Survey (SF-36), adverse events.
BI is used as standard measure for activities of daily living and motor function.43 FAC is an assessment tool designed to categorise functional ambulation ability. TUG is a simple test used to assess a person’s mobility and requires both static and dynamic balance.44 SF-36 is a health survey questionnaire, which consists of 36 items in areas of functional status, well-being, overall evaluation of health and health compared with 1 year ago.
Exclusion criteria
The following will be excluded: (1) Study types as following: reviews, cluster RCTs, cross-over designs, cohort or case-control studies. (2) Balance impairment not caused by stroke, for example, caused by Parkinson’s disease, paediatric cerebral palsy, knee surgery or other diseases. (3) Duplicate or unextracted data. (4) No access to obtain full text.
Data sources and search
The following databases will be searched from inception to June 2019: Medline, EMBASE, Web of Science, the Cochrane Library, China National Knowledge Infrastructure, China Biology Medicine, Wan Fang Data and the Chinese Science and Technology Periodical Database. RCT registration websites, including http://www.ClinicalTrials.gov and http://www.chictr.org.cn, will also be searched. Supplements like magazines, websites and reference lists of identified publications will also be searched for candidates. Experts in this field will be consulted for unpublished trials. The search strategy will be designed by a professional medical librarian (HZ); this can be seen in the online supplementary appendix.
bmjopen-2018-026844supp001.pdf (100.7KB, pdf)
Studies selection
All the retrieved studies will be imported into Endnote X8 and duplicate studies will be deleted. Two reviewers (DZ and JY) will screen the titles and abstracts independently in accordance with the inclusion and exclusion criteria and crosscheck. Two reviewers (DZ and JY) will download the full texts of all possibly relevant studies for further assessment independently and crosscheck. Disagreements will be resolved through team discussion or consulting a third reviewer (JL).
Data extraction
Two reviewers (DZ and JY) will independently extract information using an advance-designed standardised data extraction form. The extracted information includes study characteristics (author and year of publication), participants (sample size, sex, age, type of stroke, location of lesion, disease course, times of strokes and so on), interventions (frequency, duration, study period and so on), comparisons (frequency, duration, study period and so on), outcomes (BBS, FMA (balance), BI, SF-36 and so on) and adverse events of the included studies. Then two reviewers (DZ and JY) will crosscheck to make sure there is no mistake. Disagreements will be resolved by team discussion.
Risk of bias assessment
Risk of bias will be assessed in accordance with the Cochrane risk of bias tool (https://training.cochrane.org/handbook),45 which includes the following items (random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting and other bias). The assessment of each item can be rated as ‘low risk of bias’, ‘unclear risk of bias’ and ‘high risk of bias’. A ‘low risk of bias’ means the study meets all the criteria, ‘unclear risk of bias’ means the study provides insufficient information to judge and a ‘high risk of bias’ indicates the study meets none of the criteria. Two reviewers (XL and JL) will assess the risk of bias independently, then crosscheck to make sure there is no mistake. Disagreement will be settled by consulting a third reviewer (RJ). Review Manager V.5.3 will be used to make the risk of bias diagram.
Grading the quality of evidence
Two qualified reviewers (DZ and JL, who were certificated by the Chinese Grades of Recommendations, Assessment, Development and Evaluation (GRADE) centre in Lanzhou) will independently evaluate the quality of evidence for outcomes by using the GRADE system (http://www.gradeworkinggroup.org/society/index.htm). GRADE includes the following five aspects: limitations in study design, inconsistency, indirectness, imprecision and publication bias.46 The quality of evidence will be graded as ‘high’, ‘moderate’, ‘low’ or ‘very low’ in accordance with the GRADE rating standards.47 The results of GRADE including evidence profile and summary of finding table will be generated using the GRADE pro software.
Patient and public involvement
No patients were involved in writing this systematic review protocol and NMA. However, the results will be disseminated to patients suffering from poststroke balance impairment.
Statistical analysis
Pairwise meta-analysis
The characteristics of the included RCTs will be summarised. The clinical heterogeneity in the included RCTs will be checked through examination of patients’ baseline characteristics. For continuous data, standardised mean difference (SMD) will be calculated; for dichotomous data, ORs will be computed. Statistical heterogeneity across trials will also be assessed with the I2 statistics. If the p value is ≥0.1 and I2 ≤50%, we will synthesise SMD or OR with fixed -effects model (FEM). If the p value is <0.1 and I2 >50%, the random-effects model (REM) will be used.
Network meta-analysis
Bayesian network analysis will be conducted to compare the effects of different rehabilitation therapies. The Markov Chain Monte Carlo algorithm will be performed. A total of 5000 simulations for each chain will be defined as the ‘burn-in’ period. Then, posterior summaries will be based on 200 000 subsequent simulations. The Brooks-Gelman-Rubin plots method will be used to assess model convergence. Node splitting will be performed to check inconsistency between direct and indirect evidence. We will adopt the deviance information criterion to explore the model fitness, in which the FEM and REM will be compared.
Since primary outcomes are continuous data, the effect size of the rehabilitation therapies will be calculated with SMD with 95% CIs, while dichotomous outcomes will be presented as OR with 95% CIs. The 95% CIs of each SMD will also be calculated.
For each outcome, the rankogram plots and the surface under the cumulative ranking (SUCRA) curves will be used to estimate the hierarchy of the different rehabilitation therapies. The rankogram plots will show the probabilities of rehabilitation therapies assuming any of the possible ranks. SUCRA curves will be presented as percentages, 100% for the best treatment while 0% for the worst. Data analysis will be performed using WinBUGS V.1.4.3 and R software. We will perform a narrative review and summarise the evidences, if the available data are not suitable for synthesis.
Dealing with missing data
The original authors will be contacted for more information on the missing data. In the absence of a reply, we will try to calculate the data through the available coefficients. The potential impact of these missing data on the results of the NMA will be tested in sensitivity analysis.
Subgroup analysis
Subgroup analysis will be performed to address the potential heterogeneity and inconsistency. Subgroup analysis will be performed based on age, gender, type of stroke, disease course of stroke (within 6 months or after 6 months), location of lesion, times of stroke, the severity of balance impairment (BBS will be taken to define the severity of balance impairment. 0~20: poor balance ability; 20~40: fair balance ability; 41~56: good balance ability) and the duration of treatment. Meanwhile, network meta regression will be conducted to explore the possible sources of heterogeneity.
Sensitivity analysis
To verify the robustness of the study conclusions, sensitivity analysis of primary outcomes will be carried out, assessing the impact of methodological quality, study quality, sample size and the effect of missing data as well as the analysis methods on the result of this review.
Assessment of publication bias
Each included study will be assessed according to the Consolidated Standards of Reporting Trials criteria. Egger’s test and funnel plots will be used to assess the publication bias of the included studies for primary outcomes. If the funnel plots are found to be asymmetrical, we will try to interpret funnel plot asymmetry.48
Discussion
Balance impairment is one of the common impairments in patients after stroke, which is related to worse physical impairments, disability and low quality of life. Moreover, balance impairment often leads to high fall rates, which brings a great burden to patients who had a stroke, their families and the society. In addition, good balance is a prerequisite for regaining the ability to walk independently and activities of daily living.
Currently, rehabilitation therapies including WBV, VR, exercise, MT, AFO, TCM, TCE have been used to improve balance in patients who had a stroke. Several meta-analyses of head-to-head comparisons have investigated the comparative efficacy and safety of these rehabilitation therapies. So far, no NMA has been conducted to assess the comparative efficacy and acceptability of all the available rehabilitation therapies. Therefore, NMA is needed to determine the comparative effects of these rehabilitation therapies.
To our knowledge, this is the first systematic review and NMA to investigate rehabilitation therapies for balance impairment in patients after stroke. On the basis of comparative effectiveness evidence and safety, this NMA is expected to provide a ranking of these therapies for balance impairment in patients who had a stroke. The results of this NMA could help patients and therapists choose the best treatment for balance impairment. Moreover, we also hope that the results of this study may provide evidence for recommendations of guidelines.
Supplementary Material
Acknowledgments
The authors thank Yu Hu from Cardiff University for language copyediting.
Footnotes
Contributors: JL, DZ and JY contributed equally to the work as first authors. Study concept and design: RJ and S-lZ. Acquisition of data: JL, DZ, MH, HZ and XL. Drafting of the manuscript: JL, DZ and JY. Critical revision of the manuscript for important intellectual content: all authors. Supervision: RJ. All authors approved the publication of this protocol.
Funding: National Natural Science Foundation of China (grant numbers 81674047 and 81704137).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not required.
References
- 1. GBD 2017 Mortality Collaborators. Global, regional, and national age-sex-specific mortality and life expectancy, 1950-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1684–735. 10.1016/S0140-6736(18)31891-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1736–88. 10.1016/S0140-6736(18)32203-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1789–858. 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shumway-Cook A, Anson D, Haller S. Postural sway biofeedback: its effect on reestablishing stance stability in hemiplegic patients. Arch Phys Med Rehabil 1988;69:395–400. [PubMed] [Google Scholar]
- 5. Forster A, Young J. Incidence and consequences of falls due to stroke: a systematic inquiry. BMJ 1995;311:83–6. 10.1136/bmj.311.6997.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schmid AA, Van Puymbroeck M, Altenburger PA, et al. Balance is associated with quality of life in chronic stroke. Top Stroke Rehabil 2013;20:340–6. 10.1310/tsr2004-340 [DOI] [PubMed] [Google Scholar]
- 7. S Z. The Risk Factors and Nursing of Elderly Cerebrovascular Inpatient Falls. Inner Mongolia Traditional Chinese Medicine 2013;32:157–8. [Google Scholar]
- 8. Yang X, Wang P, Liu C, et al. The effect of whole body vibration on balance, gait performance and mobility in people with stroke: a systematic review and meta-analysis. Clin Rehabil 2015;29:627–38. 10.1177/0269215514552829 [DOI] [PubMed] [Google Scholar]
- 9. Corbetta D, Imeri F, Gatti R. Rehabilitation that incorporates virtual reality is more effective than standard rehabilitation for improving walking speed, balance and mobility after stroke: a systematic review. J Physiother 2015;61:117–24. 10.1016/j.jphys.2015.05.017 [DOI] [PubMed] [Google Scholar]
- 10. Li Z, Han XG, Sheng J, et al. Virtual reality for improving balance in patients after stroke: A systematic review and meta-analysis. Clin Rehabil 2016;30:432–40. 10.1177/0269215515593611 [DOI] [PubMed] [Google Scholar]
- 11. Schmid AA, Van Puymbroeck M, Altenburger PA, et al. Poststroke balance improves with yoga: a pilot study. Stroke 2012;43:2402–7. 10.1161/STROKEAHA.112.658211 [DOI] [PubMed] [Google Scholar]
- 12. Broderick P, Horgan F, Blake C, et al. Mirror therapy for improving lower limb motor function and mobility after stroke: A systematic review and meta-analysis. Gait Posture 2018;63:208–20. 10.1016/j.gaitpost.2018.05.017 [DOI] [PubMed] [Google Scholar]
- 13. Li Y, Wei Q, Gou W, et al. Effects of mirror therapy on walking ability, balance and lower limb motor recovery after stroke: a systematic review and meta-analysis of randomized controlled trials. Clin Rehabil 2018;32:1007–21. 10.1177/0269215518766642 [DOI] [PubMed] [Google Scholar]
- 14. Louie DR, Lim SB, Eng JJ. The Efficacy of Lower Extremity Mirror Therapy for Improving Balance, Gait, and Motor Function Poststroke: A Systematic Review and Meta-Analysis. J Stroke Cerebrovasc Dis 2019;28:107–20. 10.1016/j.jstrokecerebrovasdis.2018.09.017 [DOI] [PubMed] [Google Scholar]
- 15. Xu L, Dong Y, Wang M, et al. Acupuncture for balance dysfunction in patients with stroke: A systematic review protocol. Medicine 2018;97:e11681 10.1097/MD.0000000000011681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chen BL, Guo JB, Liu MS, et al. Effect of Traditional Chinese Exercise on Gait and Balance for Stroke: A Systematic Review and Meta-Analysis. PLoS One 2015;10:e0135932 10.1371/journal.pone.0135932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Li GY, Wang W, Liu GL, et al. Effects of Tai Chi on balance and gait in stroke survivors: A systematic meta-analysis of randomized controlled trials. J Rehabil Med 2018;50:582–8. 10.2340/16501977-2346 [DOI] [PubMed] [Google Scholar]
- 18. Wu S, Chen J, Wang S, et al. Effect of Tai Chi Exercise on Balance Function of Stroke Patients: A Meta-Analysis. Med Sci Monit Basic Res 2018;24:210–5. 10.12659/MSMBR.911951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tyson SF, Kent RM. Effects of an ankle-foot orthosis on balance and walking after stroke: a systematic review and pooled meta-analysis. Arch Phys Med Rehabil 2013;94:1377–85. 10.1016/j.apmr.2012.12.025 [DOI] [PubMed] [Google Scholar]
- 20. Choi ET, Kim YN, Cho WS, et al. The effects of visual control whole body vibration exercise on balance and gait function of stroke patients. J Phys Ther Sci 2016;28:3149–52. 10.1589/jpts.28.3149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lee MM, Lee KJ, Song CH. Game-Based Virtual Reality Canoe Paddling Training to Improve Postural Balance and Upper Extremity Function: A Preliminary Randomized Controlled Study of 30 Patients with Subacute Stroke. Med Sci Monit 2018;24:2590–8. 10.12659/MSM.906451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Shin JW, Don Kim K. The effect of enhanced trunk control on balance and falls through bilateral upper extremity exercises among chronic stroke patients in a standing position. J Phys Ther Sci 2016;28:194–7. 10.1589/jpts.28.194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Park KH, Kim DY, Kim TH. The effect of step climbing exercise on balance and step length in chronic stroke patients. J Phys Ther Sci 2015;27:3515–8. 10.1589/jpts.27.3515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hahn J, Shin S, Lee W. The effect of modified trampoline training on balance, gait, and falls efficacy of stroke patients. J Phys Ther Sci 2015;27:3351–4. 10.1589/jpts.27.3351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shin YJ, Lee DH, Kim MK. The effect of newly designed multi joint ankle foot orthosis on the gait and dynamic balance of stroke patients with foot drop. J Phys Ther Sci 2017;29:1899–902. 10.1589/jpts.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Association TtCDCotCM. Various types of diagnosis of cerebrovascular diseases. Chinese Journal of Neurology 1996;29:379–81. [Google Scholar]
- 27. Department of Disease Control MoH, Division of Neurology, Chinese Medical Association. Guidelines for the Prevention and Treatment of Cerebrovascular Diseases in China. Chinese Journal of Modern Nervous Diseases 2007;7:200–8. [Google Scholar]
- 28. Group SAoEec. Stroke Diagnosis and Curative Effect Evaluation Standard (Trial). Journal of Beijing University of Traditional Chinese Medicine 1996;19:55–6. [Google Scholar]
- 29. Fugl-Meyer AR, Jääskö L, Leyman I, et al. The post-stroke hemiplegic patient. 1. a method for evaluation of physical performance. Scand J Rehabil Med 1975;7:13–31. [PubMed] [Google Scholar]
- 30. Tyson SF, DeSouza LH. Reliability and validity of functional balance tests post stroke. Clin Rehabil 2004;18:916–23. 10.1191/0269215504cr821oa [DOI] [PubMed] [Google Scholar]
- 31. Yelnik A, Bonan I. Clinical tools for assessing balance disorders. Neurophysiol Clin 2008;38:439–45. 10.1016/j.neucli.2008.09.008 [DOI] [PubMed] [Google Scholar]
- 32. Blum L, Korner-Bitensky N. Usefulness of the Berg Balance Scale in stroke rehabilitation: a systematic review. Phys Ther 2008;88:559–66. 10.2522/ptj.20070205 [DOI] [PubMed] [Google Scholar]
- 33. F-m AR. Post strok heimplgia assessment of physical properties. Scand J Rehab Med 1980;7:85. [PubMed] [Google Scholar]
- 34. Benaim C, Pérennou DA, Villy J, et al. Validation of a standardized assessment of postural control in stroke patients: the Postural Assessment Scale for Stroke Patients (PASS). Stroke 1999;30:1862–8. [DOI] [PubMed] [Google Scholar]
- 35. Mao HF, Hsueh IP, Tang PF, et al. Analysis and comparison of the psychometric properties of three balance measures for stroke patients. Stroke 2002;33:1022–7. 10.1161/01.STR.0000012516.63191.C5 [DOI] [PubMed] [Google Scholar]
- 36. Chien CW, Hu MH, Tang PF, et al. A comparison of psychometric properties of the smart balance master system and the postural assessment scale for stroke in people who have had mild stroke. Arch Phys Med Rehabil 2007;88:374–80. 10.1016/j.apmr.2006.11.019 [DOI] [PubMed] [Google Scholar]
- 37. Liaw LJ, Hsieh CL, Lo SK, et al. The relative and absolute reliability of two balance performance measures in chronic stroke patients. Disabil Rehabil 2008;30:656–61. 10.1080/09638280701400698 [DOI] [PubMed] [Google Scholar]
- 38. Gorman SL, Rivera M, McCarthy L. Reliability of the Function in Sitting Test (FIST). Rehabil Res Pract 2014;2014:1–6. 10.1155/2014/593280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Medley A, Thompson M. Development, reliability, and validity of the Sitting Balance Scale. Physiother Theory Pract 2011;27:471–81. 10.3109/09593985.2010.531077 [DOI] [PubMed] [Google Scholar]
- 40. Guan Q, Han H, Li Y, et al. Activities-specific Balance Confidence (ABC) Scale adapted for the mainland population of China. Clin Rehabil 2012;26:648–55. 10.1177/0269215511427748 [DOI] [PubMed] [Google Scholar]
- 41. Mohan G, Pal PK, Sendhil KR, et al. Quantitative evaluation of balance in patients with spinocerebellar ataxia type 1: a case control study. Parkinsonism Relat Disord 2009;15:435–9. 10.1016/j.parkreldis.2008.10.003 [DOI] [PubMed] [Google Scholar]
- 42. Tyson SF, Hanley M, Chillala J, et al. The relationship between balance, disability, and recovery after stroke: predictive validity of the Brunel Balance Assessment. Neurorehabil Neural Repair 2007;21:341–6. 10.1177/1545968306296966 [DOI] [PubMed] [Google Scholar]
- 43. Mudaliar MR, Yiragamreddy SR, Tejashwani PP, et al. Quality of Life in Stroke Patients Using SSQoL Scale and Barthel Index. Indian Journal of Pharmacy Practice 2018;11:44–50. 10.5530/ijopp.11.1.8 [DOI] [Google Scholar]
- 44. Weng C STZ, Min L. The value of the timed “up and go” test at the evaluation of functional mobility in stroke patients. Chinese Journal of Rehabilitation Theory & Practice 2004. [Google Scholar]
- 45. Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ 2004;328:1490 10.1136/bmj.328.7454.1490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Zeng Xiantao LW, Sheng L, et al. How to understand and use the GRADE system correctly. Chinese Journal of Evidence-based Medicine 2011;11:985–90. [Google Scholar]
- 48. Sterne JA, Sutton AJ, Ioannidis JP, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011;343:d4002 10.1136/bmj.d4002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-026844supp001.pdf (100.7KB, pdf)


