Abstract
Background. Cervical lymphadenopathy in children is common and its etiologies diverse. No systematic review of the differential diagnosis of pediatric cervical lymphadenopathy has been conducted. Objective. To determine the prevalence rate of specific etiologies of pediatric cervical lymphadenopathy. Data Sources. EMBASE, PubMed, and SCOPUS were searched electronically. Bibliographies of select studies were reviewed as well. Study Selection. (1) Any clinical trial, observational study, or cross-sectional case series with 10 or more subjects that included delineation of etiologies and/or associated conditions with lymphadenopathy; (2) subjects aged 0 to 21 years with enlarged lymphoid tissue on body; (3) lymphadenopathy was confirmed by clinical evaluation; and (4) no specific diagnoses were excluded. Data Extraction. Year and location of publication, definition of lymphadenopathy, percentage of lymphadenopathy that was cervical, total number of subjects, gender distribution of subjects, age range of patients, and specific etiologies. Results. Of the 1790 studies, 7 studies that were combined resulted in 2687 subjects that were selected. Nonspecific benign etiology was the most common diagnosis occurring at a rate of 67.8%. Epstein-Barr virus was the next most prevalent (8.86%), followed by malignancy (4.69%) and granulomatous disease (4.06%). The most common malignancy etiology was non-Hodgkin’s lymphoma (46.0%), and the most common granulomatous disease was tuberculosis (73.4%). Conclusions. This systematic review and meta-analysis provides a rate-based differential diagnosis of pediatric cervical lymphadenopathy. Although the most common causes of pediatric cervical lymphadenopathy are nonspecific, the etiologies are diverse. Rates and credible intervals are provided to enable a probability-based diagnostic approach to palpable cervical lymphadenopathy in this age group.
Keywords: cervical lymphadenopathy, pediatrics, differential diagnosis
Introduction
Cervical lymphadenopathy is a common complaint in the pediatric population. The prevalence rate of cervical lymphadenopathy, commonly defined as cervical nodal tissue measuring >1 cm in diameter, is estimated at 38% to 45% in otherwise healthy children.1 The differential diagnosis for cervical lymphadenopathy in children is broad, including both common benign etiologies and much more rare malignant causes.1,2 While myriad clinical trials, observational studies, and case series appear in the literature, a systematic review delineating the etiologies of pediatric cervical lymphadenopathy does not presently exist. The objectives of this study were to (1) identify the most common etiologies associated with pediatric cervical lymphadenopathy and (2) determine the relative prevalence of etiologies across a wide spectrum of patients.
Methods
Protocol
This study followed the guidelines of the Preferred Reporting Items in Systematic Reviews and Meta-Analyses.3
Eligibility
In order to be included in this review, the following criteria were developed a priori: (1) any clinical trial, observational study, or cross-sectional case series with 10 or more subjects that included delineation of etiologies and/or associated conditions with lymphadenopathy; (2) ages 0 to 21 years with enlarged lymphoid tissue and lymphadenopathy confirmed by clinical evaluation; and (3) no specific diagnoses were excluded. Case reports, review articles, and editorials were excluded. There were no restrictions regarding date of publication or language; however, abstracts were required to be in English.
Information Sources
EMBASE, PubMed, and SCOPUS were searched electronically. Bibliographies of selected studies were reviewed manually as well.
Search
The main search terms were “pediatric,” “lymphadenopathy,” and “children.” The following filters were used during the search: human, no language restriction, no publication status restriction, all dates, ages 0 to 24 years. The search was performed individually by authors AD and KD. The results of the searches were pooled and duplicates were eliminated.
Study Selection
Each article was evaluated by authors AD and KD. Any differences in judgment were resolved by consensus. All selected studies were reviewed by a third author MD.
Data Collection
For each selected article, the following information was recorded: year and location of study population, definition of lymphadenopathy, percentage of lymphadenopathy that was cervical, total number of subjects, gender distribution of subjects, age range of patients, and specific etiologies. Major categories for specific etiologies for pediatric cervical lymphadenopathy included malignancy, nonspecific changes, and granulomatous, infectious, and autoimmune diseases. Within each of these categories more specific etiologies were developed from the data. Data extraction was performed by authors AD and KD and reviewed by MD.
Synthesis of Results
A Bayesian methodology for point estimation was used as previously described.4 Posterior probabilities are reported as rates with the associated 95% credible intervals. All calculations were performed in the R environment.
Sources of Bias Across Studies
Potential sources of bias in this study include the following: inconsistency in individual studies regarding data in the text when compared with data presented in tables, inconsistencies in definition and terms across studies, and a percentage of patients with lymphadenopathy in areas other than cervical. To identify articles in which cervical lymphadenopathy was studied in conjunction with other regional lymphadenopathies, a broad search term of “lymphadenopathy” was used in the initial search terms. Once the source literature was pooled, eliminations were made to narrow the focus to cervical lymphadenopathy. Articles describing patients with peripheral lymphadenopathy in addition to cervical were accepted only if ≥90% of the subjects had cervical lymphadenopathy.
Ethical Approval and Informed Consent
This study did not involve any direct contact with patients. Public data sources were solely used thus not requiring the institutional review board approval or patient consent.
Results
Study Selection
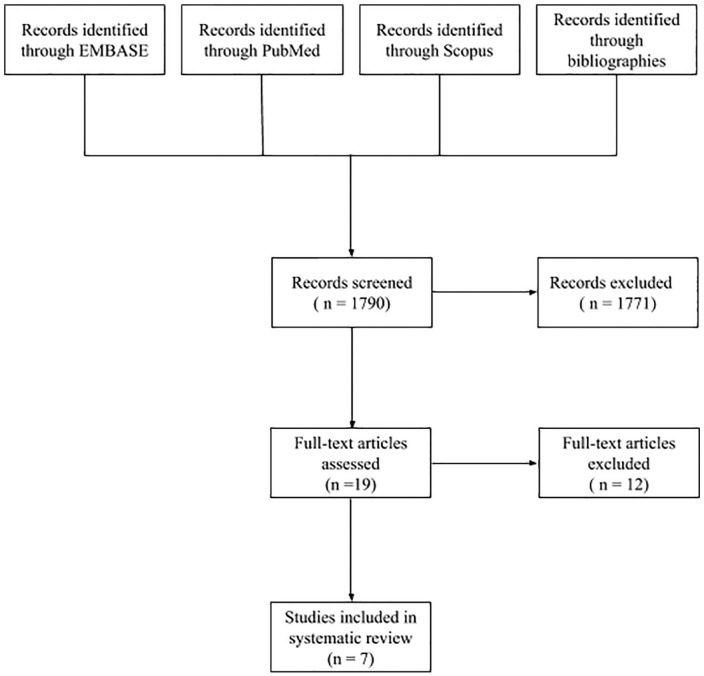
The results of the literature search are summarized in Figure 1. Searches of EMBASE, PubMed, and SCOPUS resulted in 1790 articles. Reviews of the bibliographies of selected articles and a search of the OVID Cochrane Reviews failed to yield any additional source references. A total of 1750 studies were excluded after review of the title. An additional 21 were excluded after review of the abstract. The full texts of the remaining 19 articles were assessed in detail; 12 were excluded. Three of the discarded studies were review articles and 5 had exclusion and inclusion criteria that eliminated certain etiologies of cervical lymphadenopathy from the study. Another study was excluded because it did not specify the age range of the patients. Attempts to contact the author were not successful. Three articles were excluded because the percentage of children with cervical lymphadenopathy was less than 90%. Attempts to contact these authors were also not successful. The remaining 7 articles were selected for review. Though the final articles selected for review were only 7 of the original 1790, this was after carefully eliminating articles that failed to meet inclusion and exclusion criteria, and had sufficient data to draw conclusions specifically about pediatric cervical lymphadenopathy. Though a prevalent presenting symptoms in pediatric patients globally, and articles were reviewed from countries across the world including the United States, only these 7 met our criteria.
Figure 1.
Flow diagram of literature search.
Study Characteristics and Outcomes
The 7 studies selected for this review are summarized in Table 1.5-11 These studies ranged in size from 49 to 1700 subjects and had a combined total of 2687 children. The subjects represent a global pediatric population from Nigeria, Turkey, Italy, India, and Egypt.
Table 1.
Summary of Included Studies.
| Study | No. of Patients | No. of Females/Males | Age Range | Country |
|---|---|---|---|---|
| Ejeckam and Nwabueze (1984)8 | 100 | 32/68 | <20 years | Nigeria |
| Reddy et al (2002)10 | 100 | 21/79 | 1 month to 12 years | India |
| Citak et al (2011)6 | 282 | 124/158 | 6 months to 16 years | Turkey |
| De Corti et al (2014)7 | 238 | 91/126 | 3 months to 17 years | Italy |
| Gwili et al (2015)9 | 49 | 35/85 | 1 month to 18 years | Egypt |
| Bozlak et al (2016)5 | 218 | 75/143 | 13 months to 18 years | Turkey |
| Sarsu and Sahin (2016)11 | 1700 | 697/1003 | <18 years | Turkey |
Risk of Bias Within Studies
One study consisted of patients referred to an oncology clinic.6 In another study, multiple lymph node aspirates were taken from subjects and the etiologies were reported by the number of aspirates (n = 238) not by the number of subjects (n = 217).7 Another series reported both cervical and peripheral lymphadenopathy; the diagnoses specific to cervical lymphadenopathy were identifiable, but age and gender data specific to these patients were not.10
Synthesis of Results
Table 2 summarizes the prevalence rates and credible intervals for the major categories of disease associated with pediatric cervical lymphadenopathy. The majority of cases (67.8%; 95% confidence interval [CI] = 66.00-69.60) had no identifiable etiology. Epstein-Barr virus was the most prevalent cause of cervical lymphadenopathy (8.86%; 95% CI = 7.81-9.96), followed by malignancy (4.69%; 95% CI = 3.92-5.52) and granulomatous disease (4.06%; 95% CI = 3.34-4.83). Other less common etiologies included cytomegalovirus (4.02%; 95% CI = 3.31-4.79), group A/β hemolytic streptococcus (2.9%; 95% CI = 2.30-3.57), rubella virus (1.71%; 95% CI = 1.26-2.24), toxoplasmosis (1.19%; 95% CI = 0.82-1.63), and pyogenic abscess (1.04%; 95% CI = 0.69-1.46). Etiologies that occurred at a rate of less than 1% included systemic lupus erythematosus, cat scratch disease, Kawasaki’s disease, sarcoidosis, staphylococcal pharyngitis, streptococcal tonsillitis, phlegmon, Mycoplasma pneumoniae, parvovirus B19 virus, familial Mediterranean fever, AIDS, dermatomyositis, streptococcal pneumonia, Rosai-Dorfman disease, Kikuchi-Fujimoto disease, PFAPA syndrome, and lymphomatoid papillomatosis.
Table 2.
Summary by Disease Category.
| Etiology | No. of Patients | Prevalence Rate (% of Total) | 95% Confidence Interval |
|
|---|---|---|---|---|
| Lower (%) | Upper (%) | |||
| Nonspecific diagnosis | 1822 | 67.8 | 66 | 69.6 |
| Epstein-Barr virus | 238 | 8.86 | 7.81 | 9.96 |
| Malignant | 126 | 4.69 | 3.92 | 5.52 |
| Granulomatous | 109 | 4.06 | 3.34 | 4.83 |
| Cytomegalovirus | 108 | 4.02 | 3.31 | 4.79 |
| Group A/β Hemolytic Streptococcus | 78 | 2.9 | 2.3 | 3.57 |
| Rubella | 46 | 1.71 | 1.26 | 2.23 |
| Toxoplasmosis | 32 | 1.19 | 0.816 | 1.63 |
| Abscess | 28 | 1.04 | 0.694 | 1.46 |
| Systemic lupus erythematosus | 22 | 0.819 | 0.514 | 1.19 |
| Cat scratch disease | 17 | 0.633 | 0.369 | 0.966 |
| Kawasaki disease | 14 | 0.521 | 0.285 | 0.826 |
| Sarcoidosis | 10 | 0.372 | 0.179 | 0.635 |
| Staphylococcal pharyngitis | 8 | 0.298 | 0.129 | 0.536 |
| Streptococcal tonsillitis | 7 | 0.261 | 0.105 | 0.486 |
| Phlegmons | 6 | 0.223 | 0.082 | 0.434 |
| Mycoplasma pneumonia | 3 | 0.112 | 0.023 | 0.269 |
| Parvovirus B19 | 2 | 0.0744 | 0.00902 | 0.207 |
| Familial Mediterranean fever | 2 | 0.0744 | 0.00902 | 0.207 |
| AIDS | 2 | 0.0744 | 0.00902 | 0.207 |
| Dermatomyositis | 2 | 0.0744 | 0.00902 | 0.207 |
| Streptococcal pneumoniae | 1 | 0.0372 | 0.000943 | 0.137 |
| Rosai-Dorfman disease | 1 | 0.0372 | 0.000943 | 0.137 |
| Kilkuchi-Fugimoto disease | 1 | 0.0372 | 0.000943 | 0.137 |
| PFAPA syndrome | 1 | 0.0372 | 0.000943 | 0.137 |
| Lymphomatoid papillomatosis | 1 | 0.0372 | 0.000943 | 0.137 |
Table 3 summarizes the prevalence rates and confidence intervals for malignant causes of cervical lymphadenopathy. Non-Hodgkin’s lymphoma was the most common (46%; 95% CI = 37.40-54.70) followed by Hodgkin’s lymphoma (27%; 95% CI = 14.70-29.00) and Langerhans cell histiocytosis (2.38%; 95% CI = 0.50, 5.66). Acute lymphocytic leukemia, hemophagocytic lymphohistiocytosis, neuroblastoma, and nonspecific leukemia occurred at rates below 1%.
Table 3.
Malignant Etiologies in 126 Patients With Cervical Lymphadenopathy.
| Etiology | No. of Patients | Prevalence Rate (% of Total) | 95% Confidence Interval |
|
|---|---|---|---|---|
| Lower (%) | Upper (%) | |||
| Unspecified malignant | 58 | 46 | 37.4 | 54.7 |
| Non-Hodgkin’s lymphoma | 34 | 27 | 19.6 | 35 |
| Hodgkin’s lymphoma | 27 | 21.4 | 14.7 | 29 |
| Langerhans cell histiocytosis | 3 | 2.38 | 0.498 | 5.66 |
| Acute lymphocytic leukemia | 1 | 0.794 | 0.0203 | 2.91 |
| Hemophagocytic lymphohistiocytosis | 1 | 0.794 | 0.0203 | 2.91 |
| Leukemia | 1 | 0.794 | 0.0203 | 2.91 |
| Neuroblastoma | 1 | 0.794 | 0.0203 | 2.91 |
The rates and confidence intervals for the granulomatous disease etiologies of cervical lymphadenopathy are shown in Table 4. Tuberculosis had the highest rate (73.4%; 95% CI = 64.80-81.20), followed by atypical mycobacteria (22.9%; 95% CI = 15.60-31.20) and nonspecific granulomatous disease (3.67%; 95% CI = 1.02-7.90).
Table 4.
Granulomatous Disease Etiologies in 109 Patients With Cervical Lymphadenopathy.
| Etiology | No. of Patients | Prevalence Rate (% of Total) | 95% Confidence Interval |
|
|---|---|---|---|---|
| Lower (%) | Upper (%) | |||
| Tuberculosis | 80 | 73.4 | 64.8 | 81.2 |
| Atypical mycobacteria | 25 | 22.9 | 15.6 | 31.2 |
| Nonspecific granulomatous disease | 4 | 3.67 | 1.02 | 7.9 |
Table 5 summarizes the prevalence rates and confidence intervals for the nonspecific disease etiologies of pediatric cervical lymphadenopathy. Nomenclature across studies for benign etiologies varied considerably. The different terms included nonspecific infectious, unknown, acute reactive lymphadenitis, no defined cause, reactive hyperplasia, nonspecific bacterial lymphadenitis, subchronic reactive lymphadenitis, chronic lymphadenitis, nonspecific noninfectious lymphadenitis, and normal.
Table 5.
Nonspecific Disease Etiologies in 1822 Patients With Cervical Lymphadenopathy.
| Etiology | No. of Patients | Prevalence Rate (% of Total) | 95% Confidence Interval |
|
|---|---|---|---|---|
| Lower (%) | Upper (%) | |||
| Nonspecific infectious | 1212 | 66.5 | 64.3 | 68.7 |
| Unknown origin | 219 | 12 | 10.6 | 13.6 |
| Acute reactive lymphadenitis | 154 | 8.45 | 7.22 | 9.77 |
| No defined cause | 128 | 7.03 | 5.9 | 8.24 |
| Reactive hyperplasia | 29 | 1.59 | 1.07 | 2.21 |
| Nonspecific bacterial lymphadenitis | 25 | 1.37 | 0.89 | 1.95 |
| Subchronic reactive lymphadenitis | 20 | 1.1 | 0.672 | 1.62 |
| Lymphadenitis | 14 | 0.768 | 0.421 | 1.22 |
| Chronic lymphadenitis | 12 | 0.659 | 0.341 | 1.08 |
| Nonspecific non-infectious lymphadenitis | 7 | 0.384 | 0.155 | 0.716 |
| Normal | 2 | 0.11 | 0.0133 | 0.306 |
Discussion
Pediatric cervical lymphadenopathy is a common problem with a broad differential diagnosis. Synthesized data obtained from 7 studies representing 5 countries and including 2687 patients demonstrates that two thirds of cases have no identifiable etiology. Of the patients who received a definitive diagnosis, Epstein-Barr virus, malignancy, and granulomatous disease accounted for 8.86%, 4.69%, and 4.06% of cases, respectively. Non-Hodgkin’s lymphoma was the most common malignant etiology (46.0% of malignancies), while tuberculosis was the most common granulomatous disease (73.4% of cases of granulomatous origin).
While every article selected for this study did provide an age rage of their subjects, age range of each specific etiology was not always indicated. In the articles with specific malignant etiology identified, subjects were under the age of 18 years, and the youngest subject was between 1 month and 13 months.5,9,10 Also common to all these articles was the presenting symptom of cervical lymphadenopathy. Then depending on other presenting symptoms and examinations, there was further workup of laboratory tests, diagnostic imaging such as ultrasound, fine-needle aspiration, and/or biopsy, which established the malignant etiology.
Common signs found in history included cough, fever, changes in weight, or sore throat.10 In Citak et al,6 3 of the patients with Hodgkin’s or non-Hodgkin’s lymphoma had weight loss and night sweats; common to all of the patients with lymphoma was the physical examination finding of rubbery and fixed lymph nodes. Other physical examination findings common to lymph nodes of malignant etiology were bilateral, multiple, non-tender nodes that did not present with any skin changes.9 These findings in the history and physical led to further workup, and some of these predicative factors for malignancy included enlargement of lymph node in follow-up, elevated serum C-reactive protein, lactate dehydrogenase, and uric acid, and leucopenia.5 Ultrasound findings showed no hilum and undetectable cortical and medullary contours.5,11
Regarding the specific etiologies of malignancy found across the articles, unspecified was the most common followed by non-Hodgkin’s lymphoma at 27% and Hodgkin’s lymphoma at 21%. This is not to say necessarily that non-Hodgkin’s is the more common malignant etiology when presenting with cervical lymphadenopathy. Had the other articles specified beyond malignant versus nonmalignant, another malignant etiology may have been made more prevalent. Common to all the articles is a careful history paired with the above physical examination findings and laboratory/diagnostics that then led to a procedure confirming the malignant etiology. These findings help practitioners differentiate between benign and malignant etiology of cervical lymphadenopathy, as the vast majority of the time the etiology will be nonmalignant in nature. Reassuring to both the clinical provider and the pediatric patient and their family is that in the vast majority of cases, the etiology of cervical lymphadenopathy is benign and nonspecific, rather than malignant.
Risk of Bias
The largest study in this review contributed 63.3% of the total number of subjects.11 This article was included after analysis of its data showed consistency with the smaller studies. There were many variances in nomenclature to define nonspecific, benign disease. The breakdown of these terms can be seen in Table 5. The large number of tuberculosis cases reflects the countries of origin included in this study; no large studies from the United States were included in this study.
Limitations
The main limitations of this study are variations in terminology and diagnostic evaluation across studies illustrated in Table 5. However, all articles included were required to demonstrate a thorough diagnostic evaluation.
Another limitation of this study was the need to extrapolate data specific to the cervical lymph node region from articles in which etiology and workup of peripheral sites of lymphadenopathy were included. In some articles it was possible to extract the diagnoses pertinent to cervical lymphadenopathy from the included tables. In others, it was not possible to differentiate between the cases of cervical and peripheral lymphadenopathy. In the last instance, only articles in which more than 90% of cases were identified as cervical lymphadenopathy were included.
Finally, given that many of the leading specific etiologies identified in this study are of infectious origin, the locations where the included studies were performed may have influenced the prevalence of certain infectious diseases, primarily tuberculosis. Of the 7 studies included in this meta-analysis, 2 were in tuberculosis endemic regions (Nigeria and India), while the remaining 5 studies took place in regions not endemic for tuberculosis. However, while the tuberculosis rates differed based on study location, the rates of other infections etiologies remained consistent among studies.
Conclusions
Cervical lymphadenopathy in the pediatric population is a common presenting complaint with myriad possible etiologies. The 3 most common etiologies identified include nonspecific diagnosis, Epstein-Barr virus, and malignancy. As with any systematic review, limitations and potential sources of bias exist. By combining these data with the patient’s clinical picture, the treating physician can estimate the probability of a specific diagnosis and more accurately evaluate the need for further diagnostic evaluation.
Footnotes
Author Contributions: A.D helped concieve the topic for study, performed the original search, aided in data collection and writing the manuscript;
K.D helped concieve the topic for studey, performed original searches, aided in data collection and in writing the manuscript;
S.A aided in conception of the topic, performed the statistical analysis and aided in final manusript perparation;
M.D.V conceived the topic of study, directed the search methods and aided in final manuscript prepartion.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Katherine Donches  https://orcid.org/0000-0001-7766-8007
https://orcid.org/0000-0001-7766-8007
References
- 1. Larsson L, Bentzon M, Kelly KB, et al. Palpable lymph nodes of the neck in Swedish schoolchildren. Acta Paediatr. 1994;83:1091-1094. [DOI] [PubMed] [Google Scholar]
- 2. Leung AK, Robson WL. Childhood cervical lymphadenopathy. J Pediatr Health Care. 2004;18:3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Liberati A, Altman D, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Garcia-Pierce JI, Aronoff SC, Del Vecchio MT. Systematic review and meta-analysis of seizure recurrence after a first unprovoked seizure in 815 neurologically and developmentally normal children. J Child Neurol. 2017;32:1035-1039. doi: 10.1177/0883073817726461 [DOI] [PubMed] [Google Scholar]
- 5. Bozlak S, Varkal MA, Yildiz I, et al. Cervical lymphadenopathies in children: a prospective clinical cohort study. Int J Pediatr Otorhinolaryngol. 2016;82:81-87. [DOI] [PubMed] [Google Scholar]
- 6. Citak EC, Koku N, Demirci M, Tanyeri B, Deniz H. A retrospective chart review of evaluation of the cervical lymphadenopathies in children. Auris Nasus Larynx. 2011;38:618-621. [DOI] [PubMed] [Google Scholar]
- 7. De Corti F, Cecchetto G, Vendraminelli R, Mognato G. Fine-needle aspiration cytology in children with superficial lymphadenopathy. Pediatr Med Chir. 2014;36:80-82. [DOI] [PubMed] [Google Scholar]
- 8. Ejeckam GC, Nwabueze ED. Pathology of superficial lymph node in children and young adults in Enugu, Nigeria. J Trop Pediatr. 1984;30:307-309. [DOI] [PubMed] [Google Scholar]
- 9. Gwili N, Abdel-Hadi M, Nour-Eldin A, et al. Lymphadenop-athy in a series of Egyptian pediatric patients and the role of pathology in the diagnostic workup. Pediatr Dev Pathol. 2015;05-1480-OA.1. [DOI] [PubMed] [Google Scholar]
- 10. Reddy MP, Moorchung N, Chaudhary A. Clinico-pathological profile of pediatric lymphadenopathy. Indian J Pediatr. 2002;69:1047-1051. [DOI] [PubMed] [Google Scholar]
- 11. Sarsu SB, Sahin BK. A retrospective evaluation of lymphadenopathy in children in a single center’s experience. J Pak Med Assoc. 2016;66:654-657. [PubMed] [Google Scholar]