Abstract
Objectives
To report on women’s and families’ expectations and experiences of hospital postnatal care, and also to reflect on women’s satisfaction with hospital postnatal care and to relate their expectations to their actual care experiences.
Design
Systematic review.
Setting
UK.
Participants
Postnatal women.
Primary and secondary outcomes
Women’s and families’ expectations, experiences and satisfaction with hospital postnatal care.
Methods
Embase, MEDLINE, PsycINFO, Applied Social Sciences Index and Abstracts, Cumulative Index to Nursing and Allied Health (CINAHL Plus), Science Citation Index, and Social Sciences Citation Index were searched to identify relevant studies published since 1970. We incorporated findings from qualitative, quantitative and mixed-methods studies. Eligible studies were independently screened and quality-assessed using a modified version of the National Institutes of Health Quality Assessment Tool for quantitative studies and the Critical Appraisal Skills Programme for qualitative studies. Data were extracted on participants’ characteristics, study period, setting, study objective and study specified outcomes, in addition to the summary of results.
Results
Data were included from 53 studies, of which 28 were quantitative, 19 were qualitative and 6 were mixed-methods studies. The methodological quality of the included studies was mixed, and only three were completely free from bias. Women were generally satisfied with their hospital postnatal care but were critical of staff interaction, the ward environment and infant feeding support. Ethnic minority women were more critical of hospital postnatal care than white women. Although duration of postnatal stay has declined over time, women were generally happy with this aspect of their care. There was limited evidence regarding women’s expectations of postnatal care, families’ experience and social disadvantage.
Conclusion
Women were generally positive about their experiences of hospital postnatal care, but improvements could still be made. Individualised, flexible models of postnatal care should be evaluated and implemented.
PROSPERO registration number
CRD42017057913.
Keywords: postnatal care, women’s experience, systematic review
Strengths and limitations of this study.
We searched across 10 different databases.
Quality assessment and data extraction were performed by the authors independently of each other.
Although the aim was to focus on women and babies without complications, most studies did not differentiate by risk.
We initially planned to focus on hospital postnatal care, but some studies did not differentiate between hospital and community postnatal care. These were included for completeness.
Introduction
The key aspects of postnatal care include attention to the physical health of the mother, breastfeeding support, psychological well-being of parents, and education as to what the woman should expect after birth and regarding infant care. Over time there have been a number of changes in postnatal care in the UK, the most evident being a reduction in length of hospital stay.1 A hospital lying-in period of between 8 and 14 days was standard in the 1950s,2 whereas length of postnatal hospital stay for a woman with an uncomplicated vaginal birth in the UK is now often 1–2 days.3 4
A Cochrane review by Brown et al 5 on length of postnatal hospital stay for healthy mothers who gave birth to healthy term babies suggests that early discharge home does not have an adverse effect on maternal health or breastfeeding outcomes when accompanied by a policy of offering women at least one nurse-midwife home visit.5 Most trials included assessments of women’s satisfaction with postnatal care in hospital, and overall, while not statistically significant, women tended to favour a short postnatal stay. A trial by Waldenström et al 6 also reported that, following early discharge, fathers were more involved in early care of the infant. The Cochrane review has not been updated since 2002, and the current state of evidence regarding the impact of length of postnatal hospital stay is unclear, particularly regarding current UK postnatal care policy and practice.
More choices around place of birth means that women may have more variation in location for the immediate postnatal period, for example, a stand-alone birth centre (midwife-led units where the emphasis is on birth without medical intervention in a homely environment) in comparison with a hospital maternity unit. Content of care has also changed. Maternal health observations, feeding support and parental education all remain priorities, but there are limits to what can be achieved during a short stay. In addition, national guidance recommends that women are asked about their emotional well-being at every contact and that they have an initial assessment of needs and individualised plan of care, all of which require time.7 Better Births: Improving outcomes of maternity services in England8 acknowledges that postnatal care needs to be resourced appropriately and that women should have access to their midwife (and where appropriate obstetrician) as required after having had their baby. The Maternity Transformation Programme,9 which gives a structure to the implementation of Better Births, emphasises the importance of kind and personalised care, although postnatal care is not a specific work stream within this.
The need to invest in postnatal care arises from the knowledge that it is the most commonly criticised aspect of care by women, as evidenced in the National Maternity Survey reports and publications arising from secondary analysis of survey data.3 10 11 However, we do not know if this is related to unmet expectations, poor experience of birth or afterwards, or the emotional and physical well-being of the women reporting their experiences.
As hospital postnatal stay has been decreasing in duration and also changing its focus, identifying changes in maternal expectations, experiences and satisfaction may provide important insights as to what aspects of care need to be improved for future services.
Review objectives
This review was conducted to inform a series of policy research projects on postnatal care in the UK. The main aim of this review was to comprehensively report on women’s and families’ expectations and experiences of the immediate postnatal care received in hospitals (including both alongside and free-standing birth centres). The following were the objectives:
To report on women’s satisfaction with hospital/birth centre postnatal care.
To explore how this relates to expectations and experience of care.
To identify gaps in hospital postnatal service provision in the UK.
Methods
This review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2009 checklist12 and registered with PROSPERO (see Postnatal Care Protocol V.6 in online supplementary file).
bmjopen-2018-022212supp002.pdf (470KB, pdf)
Selection of studies and inclusion criteria
Studies were eligible for inclusion if they involved women with low-risk pregnancies as defined by the National Institute for Health and Care Excellence (NICE) 2017 guidelines13 and gave birth in hospitals or birth centres in the UK. If studies contained data relating to both low-risk and high-risk pregnancies, only information relevant to the low-risk group was sought for inclusion. Studies conducted on women with high-risk pregnancies as defined by the NICE 2017 guidelines on antenatal care13 were excluded. We initially planned to exclude studies involving women with various or unknown pregnancy risks, if it was not possible to separate data relating to low-risk women. Studies with findings relating to a woman’s partner were also sought for inclusion. Studies of women of all ages, parity, ethnic background and mode of delivery were eligible for inclusion. Data were also sought regarding contextual information relevant to women’s expectations, satisfaction and experiences of their immediate postnatal care in hospital or birth centre.
We incorporated findings from different research methods: qualitative, quantitative and mixed-method design studies. The quantitative studies of the following designs were eligible for inclusion: randomised controlled trials (RCTs), cross-sectional studies, retrospective or prospective survey-based studies, and observational cohort studies. As the aim was to provide an aggregative summary of what is known about women’s experiences of hospital care, it was important to include all possible data in the synthesis. Qualitative studies included were interview studies, observational studies, focus groups studies and open-ended text from surveys where thematic analysis had been conducted. Surveys where free-text quotes were provided purely for illustrative purposes were excluded.
Reviews, editorials, commentaries and reports were only used to identify additional studies that were not retrieved by the searches. This review focuses on hospital postnatal care; thus, studies on aspects of community postnatal care were not included unless it was impossible to differentiate between them in which case they were included.
Any outcomes relevant to women’s and families’ expectations, experiences and satisfaction with postnatal care received in hospital or birth centres were extracted and are reported in this review.
Search strategy and study selection
The methodological component of the SPIDER (Sample, Phenomenon of Interest, Design, Evaluation, Research type)14 search strategy was used. Sets of search terms were developed to cover the following concepts: expectations, experiences and satisfaction with postnatal care in hospital and birth centres in the UK. The MEDLINE search strategy is shown in online supplementary appendix 1.
bmjopen-2018-022212supp001.pdf (470KB, pdf)
The following databases were electronically searched: Embase, MEDLINE, PsycINFO, Applied Social Sciences Index and Abstracts, Cumulative Index to Nursing and Allied Health (CINAHL Plus), Science Citation Index, and Social Sciences Citation Index. We also searched the grey literature in the databanks of British Library EThOS, OpenGrey and ProQuest Dissertations & Theses Global. All retrieved references were stored in EndNote (V.X8) and screened independently by the review authors.
We restricted our search to English language only and limited by date from 1970. This date was chosen as many changes to postnatal care policies took place subsequently. Review searches were conducted in February 2017. An update search was carried out in February 2019. Authors were contacted as necessary to locate full-text papers.
Assessment of the included studies
For quantitative designs we applied a modified version of the National Institutes of Health Quality Assessment Tool for the observational cohort and cross-sectional studies.15 This tool was used to assess included studies for generalisability and risk of bias based on recruitment, exclusion criteria applied, description of the study population (demographic, location and time period), sample size, response rate and comparability with the wider population. The tool also assessed the adequacy of statistical techniques and adjustment for potential confounders and the reliability and validity of standardised measures. We rated the quality of evidence on each domain as ‘yes’ for low risk of bias, ‘no’ for high risk of bias and ‘unclear’ when no information was provided to support the judgement. The Critical Appraisal Skills Programme (CASP) risk of bias tool for RCTs16 was implemented to rate the quality of any RCTs identified for inclusion in this review.
For evaluating the risk of bias of qualitative studies, we used the CASP.16 This tool has a checklist of 10 questions which cover the study objectives and rationale, study methods, study design, recruitment strategies, method of data collection, information on ethical approval, and rigour of the method of analysing data and reporting of findings. Each domain is designated ‘yes’, ‘no’ or ‘unclear’ as above.
For mixed-methods studies, the quantitative and qualitative components were assessed and reported separately, and are thus included in both quantitative and qualitative tables.
All reviewers independently assessed the quality of the included studies, and any discrepancies in quality rating were resolved by discussion.
Data extraction and data analysis
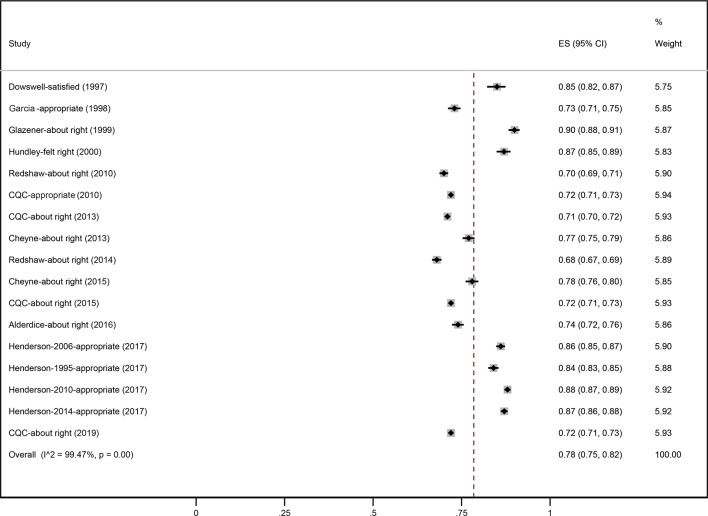
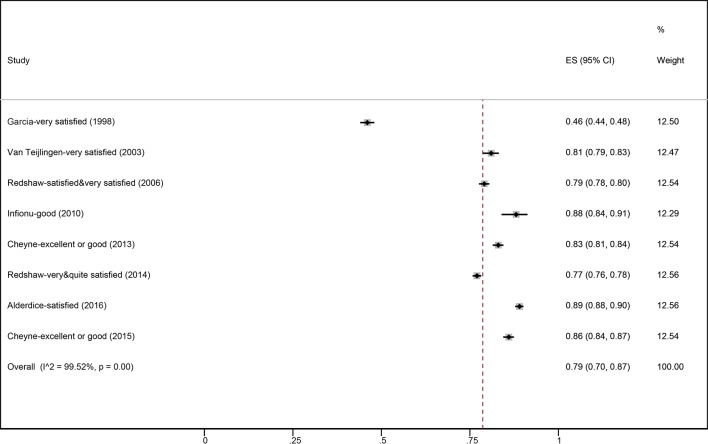
We designed two different data extraction forms, one for the quantitative studies and the second for the qualitative studies. We extracted information relevant to participants’ characteristics, study period, setting, study objective and study specified outcomes, in addition to the summary of results. Data from mixed-method studies were entered in both the qualitative and quantitative forms as appropriate. No authors were contacted to seek additional information. In this review we report findings from qualitative and quantitative studies separately. Meta-analyses were explored for quantitative data; however, heterogeneity was greater than 90% so this was not appropriate. Forest plots have been provided for outcomes where the variables were similar. An aggregative synthesis approach was used to summarise the qualitative data. With this approach the concepts are assumed to be largely well specified17 and the data pooled by providing a descriptive account of the pooled data.
We planned to perform the following subgroup analyses using both quantitative and qualitative data:
By parity.
By mode of delivery.
Ethnicity.
By the duration of postnatal stay: <24 hours, 24<48 hours, 48<72 hours, >72 hours.
Postnatal care received in hospitals in comparison with birth centres.
Comparisons over time: 1970–1989, 1990–2009 and 2010 to present.
Patient and public involvement
The need for a broad review of postnatal care was identified through discussion with our stakeholder groups, which included discussion with our parent, patient and public involvement (PPPI) stakeholders network. Dissemination of findings to stakeholders will be through plain language summaries developed with members of our PPPI stakeholders network.
Results
Results of the search
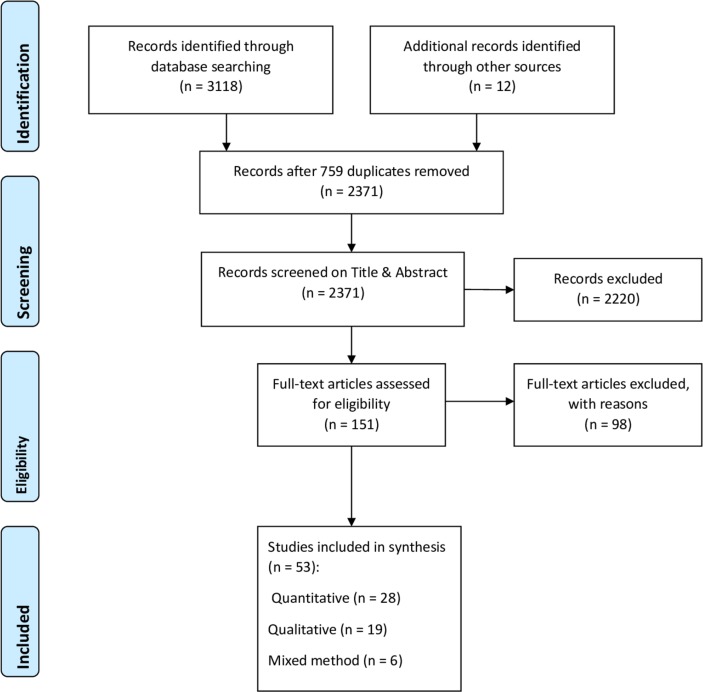
The search strategy retrieved 3118 references, of which 759 were duplicates and were removed. An additional 12 references were identified through hand searching of the reference list of full-text studies. Overall, 2371 titles and abstracts were independently screened by at least two reviewers, resulting in 151 full texts being retrieved. These were assessed for eligibility, and 53 studies are included in this review. Of these, 28 studies were purely quantitative, 19 purely qualitative and 6 used mixed methods (figure 1).
Figure 1.
PRISMA 2009 flow diagram. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Description of included studies
Summaries of the included studies are presented in tables 1 and 2 for quantitative and qualitative studies, respectively.
Table 1.
Characteristics of included quantitative studies
| Study | Study objective(s) | Study period and setting | Study design | Participants’ characteristics | Postnatal expectations and experiences | ||||||
| Alderdice et al 18 | What is current practice in Northern Ireland, key areas of concern, do experiences of vulnerable groups differ from others, how do women’s experience compare with those in England? | October–December 2014, Northern Ireland. | Cross-sectional survey posted 3 months after birth to a random sample of women who delivered in the study period. Option of online completion. Eligibility: ages 16+ years, live baby, 2 reminders sent at 2 and 4 weeks. Response rate: 45%, n=2722. |
Mean age: 31 years. Primips: 43.2%. White: 97.9%. Mode of delivery: SVD: 54.6%. Instr: 15.3%. CS: 30.2%. |
LoS:
Mean LoS 2.1 days, primips 2.1, multips 1.9 days. 74% felt LoS about right (primips 71%, multips 74%), 14% too short, 8% too long. Women living alone more likely to stay in longer. No significant difference in LoS in women from deprived areas. Relationship with the staff: Always spoken so that they could understand: 85%. Always treated with respect: 83%. Always treated with kindness: 82%. Always treated as an individual: 79%. Always felt listened to: 77%. Overall satisfaction: 89% satisfied/very satisfied. |
||||||
| Bick et al 19 | To assess whether a quality improvement intervention was associated with improved bf, maternal health and enhanced women’s views of care. | January 2008–June 2009 for preintervention; April–September for postintervention, 1 hospital in England. | Before–after design using continuous quality improvement survey approach. Interventions included longer hospital stay, skin-to-skin contact and bf encouragement, preparation of PN discharge on the PN ward and a revision of PN information booklet. Questionnaire distributed by research MW on PN ward. Eligibility: 16 years or more, live baby, sufficient English. Response rates: preintervention 64% (n= 741); postintervention 63% (n=725). | Mean age: 30.5 years. Parity: 1.66. White European: 81%. Mode of delivery: SVD: 52.6%. Instr: 19.0%. CS: 28.2%. |
LoS:
Preintervention mean 2.2 days, postintervention 2.4 days. Expectations of hospital PN care: Care in hospital better than expected: preintervention 33.7%, postintervention 40.2%. Overall satisfaction with postnatal care: Preintervention 77.4%, postintervention 82.1%. Emotional support needs: No statistically significant differences between groups in women’s views of need for emotional support in hospital; of those women who reported that they did need emotional support in hospital, there was no difference in being able to speak to a midwife. Initiation of bf: Preintervention 86.1%, postintervention 87.4%. |
||||||
| Bowers and Cheyne20 | What is the impact on cost and quality of care of reducing PN stay? | 2013, 2014 Scottish and English National Maternity Surveys (2013). | Secondary analysis of surveys, Nursing and Midwifery Workforce and Workload Planning in Scotland in 2014, including 13 major hospitals with varying mean PN LoS (range 1.4–2.4 days), data from Scottish Government Information Services Division, routine NHS data. Simulation and financial modelling conducted. | Not reported. |
LoS:
Small correlation between LoS and mothers saying that LoS was too short. No correlation between mean LoS and overall satisfaction with PN care. Infant feeding: 40% did not get information needed. 60% did get active support and encouragement with feeding. Relationship with the staff: 30% not treated with kindness and respect. Parents’ education before discharge: 70% of general communication and feeding advice and assistance happened at the time of hospital admission and discharge, only 30% took place during the recovery phase. |
||||||
| Care Quality Commission21 | No objectives specified. | April–August 2010 births, England, 144 Trusts. | Cross-sectional survey posted 3 months after birth. Eligibility: age 16 years or more, live baby, no data about reminders. Response rate: 52%, n=25 229. |
Age:
<25 years: 14%. 25–34 years: 56%. 35+ years: 29%. Primips: 44%. White: 86%. Mode of delivery: SVD: 62%. Instr: 14%. CS: 25%. |
LoS:
<24 hours: 36%. 1–2 days: 35%. 3+ days: 29%. Views on duration of hospital stay: 72% ‘appropriate’. Kindness and understanding: 93% ‘always’. Information and explanations: 53% always given information/explanations, 89% received information needed when leaving hospital. Feeding advice (may include community): 79% ‘always or generally’ received consistent advice, 14% did not receive support. |
||||||
| Care Quality Commission22 (mixed methods) | No objectives specified. | February 2013 births, 137 Trusts, England. | Cross-sectional survey posted 3 months after birth to a random sample of women who delivered in the study period. Eligibility: excluded if woman or baby died, woman aged <16 years, concealed pregnancy, baby taken into care, private maternity care, woman resident outside UK. 2 reminders sent to non-responders. Response rate: 46%, n=>23 000 (exact number not reported). |
Mode of delivery:
SVD: 60%. Instr: 14%. CS: 26%. No other characteristics reported. |
Relationships with staff:
Always treated with kindness and understanding: 66%. Always received information/explanations needed after birth: all women 59%, primips 50%, multips 67%. Definitely given enough information about own recovery: all women 61%, primips 54%, multips 68%. Definitely received information about emotional changes: 56%. LoS: ≤12 hours: 17%. 1–2 days: 37%. 3–4 days: 18%. 5+ days: 9%. Views on LoS: About right: all women 72%, primips 69%, multips 75%. Infant feeding (may include community): Decision on feeding method always respected: 81%. Always consistent advice: 54%, primips 47%, multips 61%. Always active support/encouragement: all women 61%, primips 56%, multips 66%. |
||||||
| Care Quality Commission23 | No objectives specified. | February 2015 births, England, 133 Trusts. | Cross-sectional survey posted 3 months after birth. Eligibility: age 16 years or more, live baby, 2 reminders. Response rate: 40%, n=20 631. |
Age:
<25 years: 9%. 25–34 years: 59%. 35+ years: 32%. Primips: 51%. White: 77%. Mode of delivery: SVD: 59%. Instr: 51%. CS: 25%. |
LoS: 1–2 days 36%. View of LoS: about right 72%, too long primips 19%, multips 15%. Always treated with kindness and understanding: all women 71%, primips 66%, multips 75%. Always able to get help in reasonable time: 81%. Always took account of personal circumstances: 96%. Always given consistent feeding advice: 55% (may include community). |
||||||
| Care Quality Commission47 | No objectives specified. | February–January 2018 births, England, 129 Trusts. | Cross-sectional survey posted 3 months after birth. Eligibility: age 16 years or more, live baby, no data about reminders. Response rate: 37%, n=17 600. |
Age:
<24 years: 7.3%. 25–34 years: 58%. 35+ years: 35%. Primips: 42%. White: 86%. Mode of delivery: SVD: 58%. Instr: 14%. CS: 26%. |
LoS: within 2 days 70% of all women. View of LoS: about right 72%, 11% too short, 17% too long. Always treated with kindness and understanding: all women 77%. Always able to get help in reasonable time: 59%. Initiated bf: 80%. Always given information needed: 66%. Always given support and encouragement about feeding: 63%. Always given consistent feeding advice: 56%. Always respected their decision on feeding: 83%. Partners able to stay: 71%. Hospital room very clean: 70%. |
||||||
| Cheyne et al 25 | No objectives specified. | February–March 2013 birth, Scotland. | Cross-sectional survey posted 3 months after birth to a random sample of women who delivered in 2 weeks in the study period. Option of online completion. Eligibility: excluded if woman or baby died, woman aged <16 years, 2 reminders sent (not stated when). Response rate: 48%, n=2366. |
Age:
<25 years: 15%. 25–34 years: 57%. 35+ years: 28%. Primips: 42%. White: 92%. Mode of delivery: SVD: 56%. Instr: 14%. CS: 30%. |
Views on LoS: 77% ‘about right’, 14% ‘too long’, 10% ‘too short’. Always given explanations needed: 61%. Always treated with kindness and understanding: 67%. Overall quality of care: 83% excellent or good. Bf initiation: 49%. Feeding: consistent advice: always 57%. Feeding: active support and encouragement: always 63%. Feeding decisions respected by staff: always 82%. (Feeding may relate to community as well as hospital.) |
||||||
| Cheyne et al 24 (mixed methods) | No objectives specified. | February–March 2015, Scotland. | Cross-sectional survey posted 3 months after birth to a random sample of women who delivered in the study period. Online option for completion. Eligibility: excluded if woman or baby died, woman aged <16 years, 2 reminders sent (not stated when). Response rate: 41%, n=2036. |
Age:
<25 years: 10%. 25–34 years: 60%. 35+ years: 30%. Primips: 42%. White: 93%. Mode of delivery: SVD: 53%. Instr: 14%. CS: 33%. |
Views of LoS: about right 78%, too short 11%, too long 11%. Bf initiation: 52%. Always received information and explanations needed: 60%. Always treated with kindness and understanding: 70%. Partners accommodated on PN ward: 58%. Infant feeding decision always respected: 82%. Always consistent advice: 57%. Always active support and encouragement: 63%. Overall quality of care: excellent 54%, good 32%. (Feeding may relate to community as well as hospital.) |
||||||
| Cranfield26 | To assess women’s views of support received. | 1981, one centre in the North Herts Maternity Unit, England. | Cross-sectional postal survey sent 3 months after birth to 250 consecutive hospital admissions. Response rate: 76.4%, n=191. No eligibility criteria specified. No mention of reminders. |
Mean age: 26.8 years. Primips: 44%. Mode of delivery: SVD: 76%. Instr: 11%. CS: 13%. |
LoS: 1 day 3%, 2 days 28%, 3–4 days 9%, 5–6 days 9%, 7 days 30%, >7 days 22%. Received adequate help: 84%. Satisfaction with LoS: just right 75%, too long 18%. Bf initiation: 73%. |
||||||
| Dowswell et al 45 | To describe variation in the care process and to explore associations between care process, satisfaction and psychological well-being. | April 1994 births, 6 districts in Yorkshire, England. | Cross-sectional postal survey sent 4–8 weeks after birth to a random selection of women who delivered in the study period. Eligibility: live term births discharged home with mother, reminder sent 2 weeks after initial mailing. Response rate: 72%, n=720. |
No participant characteristics reported. Mode of delivery: SVD: 62.8%. Instr: 33.3%. CS: 3.8%. |
LoS (mean):
SVD: 2.6 days (range 2.0–3.0 days). Instr: 3.6 days. CS: 5.9 days. Women’s satisfaction with the LoS: 85% of women were satisfied with LoS.
|
||||||
| Farquhar et al 27 | To describe the views of women using a team MW scheme providing continuity of caregiver vs traditional care. | December 1994–June 1995, South East England. | Cross-sectional survey posted 1 week after birth to all women residents in health authority who delivered at 1 of 3 hospitals during study period. Women in study group received team MW. Comparison hospitals A and B provided traditional care. Eligibility: excluded women with concealed pregnancy, those with baby placed for adoption. Postal reminders sent after 2 weeks, then phone reminder. Response rates: team MW: 88%, n=1077. Comparison A: 88%, n=272; comparison B: 90% n=133. |
% | |||||||
| Age (years) | Team | Comparison A | Comparison B | % | Team MW | Comparison A | Comparison B | ||||
| <25 | 22 | 16 | 10 | Received fairly/very helpful advice | 94 | 93 | 94 | ||||
| 25–34 | 65 | 71 | 70 | Very satisfied with hospital PN care | 65 | 70 | 69 | ||||
| 35+ | 13 | 12 | 20 | ||||||||
| Primips | 38 | 35 | 27 | ||||||||
| White | 95 | 98 | 98 | ||||||||
| Mode of delivery not reported. | |||||||||||
| Garcia et al
28
(mixed methods) |
No objectives specified. | June–July 1995, England and Wales. | Cross-sectional survey posted 4 months after birth to a random sample of women who delivered in the study period. Eligibility: ages 16+ years, live baby. Response rate: 67%, n=2406. |
Age:
<25 years: 19.9%. 25–34 years: 65.6%. 35+ years: 14.5%. Primips: 42%. White: 92%. Mode of delivery: SVD: 71.9%. Instr: 11.7%. CS: 17.3%. |
LoS:
Had a say/choice in when they went home: 62%. Felt the duration was appropriate: 73%. Treated with respect, kindness and understanding: Always treated with respect: 54%. Always treated with kindness and understanding 51%. Well-supported, confidence and trust in staff: Always had confidence in staff: 59%. Overall satisfaction: 46% very satisfied. Discussion of delivery while on PN ward: Not wanted: 23%. Not been able to: 23%. Yes, at least in part: 53%. Bf: 72% put the baby to the breast at least once. Bf support: Always consistent advice: 31%. Always practical help: 34%. Always active support and encouragement: 38%. Always enough privacy to feed: 49%. |
||||||
| Glazener29 | To describe structures, processes and outcomes of PN care, characteristics, expectations and experiences of women, experience and roles of providers, factors associated with adverse outcome, and areas of unmet need. | May 1990 and May 1991, 2 hospitals in Scotland. | Postal questionnaires sent to a random sample of women immediately after discharge home. Eligibility: all women discharged from PN ward. Reminders sent at 2 and 6 weeks. Response rate: 89%, n=1412 (denominator was all women who initially agreed to take part). |
Mean age: 28.2 years. Primips: 46.7%. Ethnicity not reported. Mode of delivery: SVD: 72.6%. Instr: 13.6%. CS: 13.8%. |
Mean LoS: primips 5.8 days, multips 4.0 days. LoS considered: about right 90%, too short 2%, too long 8%. Considered room unsuitable (would have preferred smaller/single room): 13%. Visiting arrangements: Happy with visiting hours: 89%. Not enough: 9%. Too much: 2%. Staff adjective checklist: 1+ positive adjective: 97%. 1+ negative adjective: 36%. Bf initiation: 58%. Received enough advice about: Dressing baby: 62%. PN exercises: 84%. Own health: 68%. Bf problems at discharge: 16.8%. Received conflicting advice regarding bf: 31%. |
||||||
| Healthcare Commission30 | No objectives specified. | February 2007 births, England. | Cross-sectional survey posted 3 months after birth. Eligibility: age 16 years or more, live baby, no data about reminders. Response rate: 59%, n=26 325. |
Age:
<25 years: 17%. 25–34 years: 56%. 35+ years: 28%. Primips: 49%. White: 87%. Mode of delivery not reported. |
Information and kindness:
42% were not given information or explanations needed. 37% were not treated with kindness and understanding. Infant feeding (may include community): 23% did not receive consistent advice. 22% did not receive practical help. 22% did not receive active support or encouragement. Care after birth: 96% reported their baby had an examination or baby check before leaving hospital. Ward environment: Room/ward very clean: 40%. Toilets/bathroom very clean: 36%. Food: Always offered choice: 70%. Not enough: 28%. Poor overall: 19%. |
||||||
| Henderson and Redshaw1 | To explore change over time in women’s perceptions of maternity care. | 1995–2014, June–July 1995, 1 week March 2006, 2 weeks October–November 2009, 2 weeks January 2014, England. | Secondary analysis of 4 cross-sectional postal maternity surveys 1995, 2006, 2010 and 2014. Random samples selected, questionnaires sent 3 months after birth. Eligibility: aged 16 years or more, live baby. Reminders sent at 2, 4 (and 8 weeks for 2014); 1995 no reminders sent. Response rates: 1995: 67%, n=2406; 2006: 63%, n=2966; 2010: 55%, n=5333; 2014: 48%, n=4571. |
Age (years) | <25 (%) | 25–34 (%) | 35+ (%) | LoS | Women’s view of LoS | Confidence and trust in staff | |
| 1995 | 19.9 | 65.6 | 14.5 | 3 days or more (%) | Too short (%) | Always (%) | |||||
| 2006 | 19.3 | 56.6 | 24.1 | ||||||||
| 2010 | 17.1 | 58.4 | 24.5 | 1995 | 46.7 | 12.6 | 75.2 | ||||
| 2014 | 21.2 | 58.3 | 20.5 | 2006 | 34.8 | 13.1 | 68.9 | ||||
| 2010 | 30.6 | 12 | 68.6 | ||||||||
| Primips | White | 2014 | 28.7 | 12.2 | 68.7 | ||||||
| 1995 | 42.3 | 91.9 | |||||||||
| 2006 | 41 | 87.4 | |||||||||
| 2010 | 50.1 | 85.7 | |||||||||
| 2014 | 49.9 | 83.9 | |||||||||
| SVD | Instr | CS | |||||||||
| 1995 | 71.9 | 11.7 | 17.3 | ||||||||
| 2006 | 64.9 | 12.4 | 22.4 | ||||||||
| 2010 | 62.6 | 12.7 | 24.8 | ||||||||
| 2014 | 58.7 | 14.8 | 26.4 | ||||||||
| Henderson et al 31 | To examine use of services and perceptions of care of women from 7 specific ethnic minority groups. | April–August 2010 births, England, 144 Trusts. | Secondary analysis of Care Quality Commission 2010 data. Eligibility: age 16 years or more, live baby, no data about reminders. Response rate: 52%, n=25 229. |
Only ethnicity reported. White: 80.9%. Mixed: 1.2%. Indian: 2.3%. Pakistani: 2.3%. Bangladeshi: 0.6%. Caribbean: 0.6%. African: 2.6%. Chinese or other: 2.7%. |
LoS >2 days (%) | LoS too long/too short (%) | Information about recovery (%) | ||||
| White | 28.5 | 27.4 | 82 | ||||||||
| Mixed | 32.8 | 25.3 | 80.5 | ||||||||
| Indian | 36.6 | 32.7 | 83.4 | ||||||||
| Pakistani | 33.8 | 34.9 | 79.9 | ||||||||
| Bangladeshi | 32.5 | 29 | 81.3 | ||||||||
| Caribbean | 32.1 | 32 | 80.5 | ||||||||
| African | 38.5 | 28.6 | 87.5 | ||||||||
| Other | 33.1 | 28.7 | 85.4 | ||||||||
| Hicks et al 32 | To compare a Changing Childbirth initiative, including continuity of care, with traditional care. | 2001, England. | RCT comparing intervention with traditional care. Validated questionnaires sent 4–6 weeks after birth, care elements scored out of 5. Eligibility and reminders not reported. Response rate: intervention group n=81 (81%); control group n=92 (92%). |
Mean age:
Intervention group: 28.9 years. Control group: 28.2 years. Mean number of previous births: Intervention group: 2.4. Control group: 2.1. Mode of delivery and ethnicity not reported. |
No significant difference between the two groups on PN ward regarding: Care and sensitivity (scores 2.2 vs 2.2). Explanation/consultation (scores 2.3 vs 2.3). Contact with obstetrician (scores 2.5 vs 2.6). Contact with GP (scores 2.5 vs 2.4). Contact with midwives (scores 2.0 vs 2.0). Not rushed/under pressure (scores 2.1 vs 2.2). Own views taken into account (scores 2.2 vs 2.2). Consistency of information (scores 2.2 vs 2.3). Willingness of MWs to attend to needs (scores 2.2 vs 2.2). |
||||||
| Hirst and Hewison33 (mixed methods) | To compare the quality of hospital PN care for Pakistani and indigenous white women. | July 1995–August 1996, 20 GP practices in 2 districts in Northern NHS region, England. | Prospective comparative survey between districts and between ethnic groups using purposive sampling. No data on reminders or eligibility. Response rate: 83%, n=187. |
No details of participant characteristics reported. White women who were having their first pregnancy were older than Pakistani women. Age range (15–20, 21–30 and 31–41) was similar for each district. |
Expected LoS (hours) | Pakistani | White | ||||
| District A | 60 | 36.5 | |||||||||
| District B | 61.4 | 36 | |||||||||
| LoS: | |||||||||||
| Mean duration 50.7 hours (SD 30.6) for all women. | |||||||||||
| Hundley et al 34 | To determine the extent to which recommendations from policy documents had been adopted. | 10-day period in September 1988, Scotland. | Cross-sectional postal survey distributed by MWs 10 days after birth with Freepost return to study team. Eligibility: all women delivering in Scotland during the study period except if insufficient English, MW considered inappropriate or no longer resident in Scotland. Reminders sent by post at 2 weeks. Response rate: 69%, n=1137 women. |
Mean age: 29.3 years. Primips: 45.4%. White: 98.2%. Mode of delivery not reported. |
LoS:
3–5 days: 48%. 1–2 days: 29%. Views on LoS: 87.2% felt it was right. 3.9% felt it was too long. 8.8% felt it was too short. Choice on when to go home: 77% had a choice. |
||||||
| Ifionu et al
35
(abstract only) |
To assess the quality of maternity care provided in a busy teaching maternity unit. | February–July 2009, Norfolk and Norwich University Hospitals. | Questionnaire distributed to women (no further details). Eligibility: live births, baby in ‘good condition’. Response rate: n=302, denominator not reported. |
Participant characteristics not reported. |
Overall postnatal hospital care: 11%–13% rated ‘poor’. Contraception postnatal advice: 65% did not receive any advice. |
||||||
| Ingram et al 36 | To determine whether specific ‘hands-off’ bf technique taught in hospital increases successful bf; to investigate factors associated with bf at 2 and 6 weeks. | October 1996–November 1998, Bristol, England. | Non-randomised, prospective cohort phased intervention study. Eligibility and reminders not reported. Response rate: 84%, n=1171. |
Mean age: 29.5 years. Primips: 58.4%. Mode of delivery and ethnicity not reported. |
Receiving enough support increased bf:
(OR 2.13, CI 1.28 to 3.53). Conflicting advice, enough advice and help, poor advice regarding problems not significantly associated with bf at 2 weeks. |
||||||
| McCourt et al 37 (mixed methods) | 1. Was 1:1 continuity of caregiver preferred by women? 2. Was it associated with any benefit to women? |
1994–1996, London, England. | Prospective study of all women receiving care in Trust over a 1-year period. Intervention and control groups from different areas. Questionnaires sent during pregnancy, and at 2 and 13 weeks postnatally. Eligibility: women resident in area over the period of study, delivered live, term baby. Analysis restricted to 1 hospital. Single reminder. Response rates at 2 weeks: 1:1 group, 59%, n=646; controls 60%, n=603. |
Age not reported. Primips: 35%. White: 42%. Mode of delivery not reported. |
Postnatal care experience comparing 1:1 care with routine care: very satisfied with care: 1:1 50%, routine care 54%. | ||||||
| National Childbirth Trust46 | To explore women’s experience of care and support during the first month after birth. | September 2008–September 2009, UK | Online survey on NCT website. Open to anyone accessing website. 95% NCT members. Response rate: unknown (no denominator), n=1321. |
Primips: 83%. Age (years), primips only: <25: 1%. 25–34: 65%. 35+: 34%. Primips: white 95%. Mode of delivery: Primips: SVD: 48%. Instr: 26%. CS: 26%. Multips: SVD: 81%. Instr/CS: 3%. |
LoS:
Primips (%), Multips (%) < 24 hours: 15, 40 1–2 days: 44, 32 3–4 days: 27, 19 5+ days: 14, 9 Emotional support 24 hours after birth: Primips: 41% received ‘all’, 41% ‘some’, 25% ‘little’ 17%, ‘none’ 17%. Physical support 24 hours after birth: ‘all’ 56%, ‘some’ 24%, ‘little’ 12%, ‘none’ 9%. Information received: 45% received ‘all’, 25% ‘little or none’. Babies’ health information and advice: Primips: ‘all’ 52%, ‘some’ 31%, ‘little’ 11%, ‘none’ 6%. (Data above refer to the first 24 hours. For 15% of primips and 40% of multips, some of this period was postdischarge.) |
||||||
| Raleigh et al 38 | To examine social and ethnic inequalities in women’s experience of maternity care. | February 2007 births, England. | Cross-sectional survey posted 3 months after birth. Eligibility: age 16 years or more, live baby, no data about reminders. Response rate: 59%, n=26 325. |
Age:
<25 years: 17%. 25–34 years: 56%. 35+ years: 28%. Primips: 49%. White: 87%. Mode of delivery not reported. |
Compared with white women, women from ethnic minority stayed in hospital longer after normal delivery, were more likely to initiate bf and for their babies to be checked predischarge. Women from ethnic minorities were more positive about receiving adequate information, being treated with respect and less positive about cleanliness and choice of food. (Numbers varied by ethnic group.) |
||||||
| Redshaw and Heikkila10 | What is current clinical practice, what are key areas of concern, have women’s experience of care changed over the years, are there regional differences in care? | October–November 2009 births, England. | Cross-sectional survey posted 3 months after birth to a random sample of women who delivered in 2 weeks in October–November 2009. Option of online completion. Eligibility: age 16 years or more, live baby. Reminders sent at 2, 4 and 8 weeks. Response rate: 54%, n=5333. |
Age:
<25 years: 17.1%. 25–34 years: 58.4%. 35+ years: 24.5%. Primips: 50.1%. White: 85.7%. Mode of delivery: SVD: 62.6%. Instr: 12.7%. CS: 24.8%. |
Mean LoS:
Primips 2.4 days, multips 1.6 days. Satisfaction with LoS: About right: 70%. Too short: 12%. Too long: 15%. Relationships with staff: Always treated as an individual: 57%. Treated with respect most of the time: 91%. Treated with kindness most of the time: 91%. Always had confidence in staff: 69%. Always spoken to so could understand: 94%. Treated with kindness most of the time: 94%. Infant feeding: Initiation of bf: 63%. |
||||||
| Always… (%) | All women | Primips | Multips | ||||||||
| Consistent advice | 37.5 | 35.2 | 39.8 | ||||||||
| Practical help | 35.6 | 35.2 | 35.7 | ||||||||
| Active support | 39.5 | 38.9 | 40 | ||||||||
| (may include community) | |||||||||||
| Redshaw and Henderson3 | To describe current practice, areas of concern to women, especially experience of vulnerable women, and change over time. | January 2014 births, England. | Cross-sectional survey posted 3 months after birth to a random sample of women who delivered in 2 weeks in the study period. Option of online completion. Eligibility: ages 16+ years, live baby, 3 reminders sent at 2, 4 and 8 weeks. Response rate: 47%, n=4571. |
Age:
<25 years: 21.2%. 25–34 years: 58.3%. 35+ years: 20.5%. Primps: 49.9%. White: 83.9%. Mode of delivery: SVD: 58.7%. Instr: 14.8%. CS: 26.4%. |
Mean LoS: primps 2.2 days, multips 1.8 days. Satisfaction with LoS: about right 68%, too short 12%, too long 15%. Primips 18% too long, multips 13% too long. Relationship with the staff: Always spoken to so could understand: 79%. Always treated with respect (76%) and kindness (75%). Always treated as an individual: 71%. Always felt listened to: 68%. Overall satisfaction: Very/quite satisfied: 77%. Dissatisfied: primips 14%, multips 10%. |
||||||
| Infant feeding: | |||||||||||
| Bf initiation: 87% | |||||||||||
| Always… (%) | All women | Primips | Multips | ||||||||
| Consistent advice | 42.7 | 40.1 | 45.6 | ||||||||
| Practical help | 42.2 | 41.6 | 43 | ||||||||
| Active support | 47.2 | 42.6 | 47.8 | ||||||||
| (may include community) | |||||||||||
| Redshaw et al 11 | From the perspective of women needing maternity care, what is current clinical practice, what are key areas of concern, have women’s experience of care changed over the years? | March 2006 births, England. | Cross-sectional survey posted 3 months after birth to a random sample of women who delivered in 1 week in March 2006. Eligibility: age 16 years or more, live baby, no data about reminders. Response rate: 63%, n=2966. |
Age:
<25 years: 19.3%. 25–34 years: 56.6%. 35+ years: 24.1%. Primips: 41.0%. White: 87.4%. Mode of delivery: SVD: 64.9%. Instr: 12.4%. CS: 22.4%. |
Mean LoS:
Primips SVD: 2.8 days. Multips SVD: 2.0 days. CS all women: 4.1 days. 63% stayed <3 days. Relationship with the staff: Always spoken to so could understand: 91.5%. Treated with respect most of the time: 89.2%. Always treated as individuals: all women 53.1%, primips 50.4%, multips 55.2%. Ward environment: Improvements needed: primips 77%, multips 72%. Critical of privacy 28%, space 22%, temperature 27%, cleanliness 19%, noise 23%. Overall satisfaction: Satisfied/very satisfied: 79.8%. Infant feeding: Bf initiation: 80%. |
||||||
| Always… (%) | All women | ||||||||||
| Consistent advice | 32.7 | ||||||||||
| Practical help | 30.9 | ||||||||||
| Active support | 35.8 | ||||||||||
| (may include community) | |||||||||||
| Scott et al 39 | To examine autonomy, privacy and informed consent in care of PN women. | Study period not reported Scotland (6 university and district hospitals). | Questionnaire packs left with ward staff. Care elements scored out of 5. Eligibility not reported. Response rate: 60%, n=404. |
Women’s characteristics not reported. |
Information women received about LoS: mean score 3.79. Infant feeding information: mean score 4.34. Supporting bowel and bladder function: mean score 3.48. Information related to personal hygiene: mean score 3.56. Breast care information: mean score 3.62. Privacy: mean score 4.33. Staff knocked before entering the room: mean score 4.32. Receiving help with their meals: mean score 4.17. Able to bf in private: mean score 4.63. Confidentiality of women’s treatment: mean score 4.73. Helped to use toilet: mean score 4.86. Helped with hygiene: mean score 4.81. Exposing woman’s body to others: mean score 4.85. |
||||||
| Shields et al 40 (mixed methods) | To compare women’s satisfaction with MW managed care vs shared care over 3 different time periods as part of RCT. | 1993–1994, Glasgow, Scotland. | RCT of MW managed vs shared care. Questionnaires sent during pregnancy and at 7 weeks and 7 months postnatally. Eligibility: booked within 16 weeks, normal, healthy pregnancy, live birth, resident in catchment area. No data on reminders. Response rate at 7 weeks: MW group: 71.9%, n=445; shared care: 63.1%, n=380. |
Mean age at booking*: MW group: 25.8 years. Shared care: 25.5 years. Primips: MW group: 54.7%. Shared care: 53.5%. Mode of delivery (%): MW group Shared care SVD: 73.5 73.7 Instr: 13.6 14.3 CS: 12.9 11.9 |
Satisfaction with staff interaction (mean score on 5-point Likert scale, −2 to +2). | ||||||
| MW group | Shared care | ||||||||||
| Relationships with staff | 1.31 | 0.84 | |||||||||
| Information transfer | 1.2 | 0.7 | |||||||||
| Choices and decisions | 1.13 | 0.07 | |||||||||
| Social support | 1.21 | 0.74 | |||||||||
| Spurgeon et al 41 | To investigate satisfaction with 2 pilot schemes based on Changing Childbirth compared with traditional care. | January 1997–June 1998, large Trust in central England. | Retrospective cohort between-group comparison, two received midwifery-led card (A and B), and the controls (C) received standard obstetric-led care. All delivered in the same hospital. Questionnaires sent 6 weeks after birth. Eligibility: excluded women at high obstetric risk. Reminders sent out until a minimum of 100 questionnaires had been received from each group. Response rates not specified: intervention group, n=215; control group, n=118. |
Mean age:
A. 27.9 years. B. 28.7 years. C. 28.7 years. Average number of previous births: A. 1.7 B. 1.9 C. 2.0 Mode of delivery and ethnicity not reported. |
LoS: no significant difference between the groups (actual LoS not stated). Information and advice: no significant difference between the groups for information, feeding methods, the baby’s health, handling, washing and changing the baby. |
||||||
| van Teijlingen et al 42 | To identify individual or specific concerns with maternity care provision. | September 1998, Scotland (Scottish Birth Study). | Cross-sectional survey distributed by MWs 10 days after birth to all women who delivered in a 10-day period. Eligibility: all women delivering in Scotland during the study period except if insufficient English, MW considered inappropriate or no longer resident in Scotland. Reminders sent by post at 2 weeks. Response rate: 69%, n=1137. |
Age:
15–24 years: 21.4%. 25–34 years: 64.2%. 35+ years: 14.5%. Primps: 45.4%. White: 98.2%. Mode of delivery not reported. |
Overall satisfaction with postnatal care (may include community): Very satisfied: 81%. Satisfied in some ways/dissatisfied: 19%. Primip women’s satisfaction with postnatal care: Very satisfied: 78%. Satisfied in some ways/dissatisfied: 22%. Multip women’s satisfaction with postnatal care: Very satisfied: 84%. Satisfied in some ways/dissatisfied: 16%. |
||||||
| Wardle43 | To examine women’s experience of maternity care. | April–May 1991 births, Staffordshire, England. | Cross-sectional postal survey sent 7–8 weeks after birth to all women who had a hospital birth in study period. No eligibility criteria specified. Reminders sent 2 and 4 weeks after initial mailing. Response rate: 80%, n=639. |
No participant characteristics reported. |
Infant feeding: 58% of babies given breast milk in hospital, >50% supplemented with formula. Women’s health and baby’s care: 30% received conflicting advice from HCPs. 45% wanted to talk more to HCPs about babies’ care and their own health. 21%–27% did not have enough advice about feeding, handling, settling the babies and problems with their own health. Relationship with HCPs: 53% reported midwives were too busy to talk to them. 259 women wrote comments: 81% reported HCPs were helpful and friendly, 29% not receiving enough help or advice, 15% staff too busy, 18% staff attitudes poor and not helpful. Information to women separated from their babies: Most given enough information about baby’s health and progress, 1/4 wanted more, 1/4 wanted to talk to HCP about worries. |
||||||
| Wray44 | To gain the views of women about PN care. | Study period not reported. North West England (2 neighbouring urban locations). | Cross-sectional survey distributed by community MWs on the 10th or 14th day after birth, not clear how survey was returned. Eligibility: women and babies discharged home together, birth weight >2 kg, care by MWs, both mother and baby well, not placed for adoption. No data about reminders. Response rate: 42%, n=452. |
Age:
< 25 years: 18.5%. 25–34 years: 60.9%. 35+ years: 19.7%. Primips: 44.5%. Mode of delivery: SVD: 66%. Instr and CS: 33%. Ethnicity not reported. |
Visiting arrangements: 81% felt visit durations were about right, 19% too short. Flexibility of visiting: 62% right, 38% not flexible Postnatal ward: 86% had enough opportunity to rest. LoS: < 24 hours: 32%. < 2 days: 59%. 3 or 4 days: 26%. 5–10 days: 12%. Infant feeding: 70% intended to bf and of those 75% did bf. Feeding support (may include community): During the day 86% of women felt they were given enough help vs 80% at night. Baby’s care (may include community): 66% shown how to bathe the baby, 34% of women shown how to change nappies and 34% shown top and tail clean, 69% care of cord, 70% had help with baby sleeping position. |
||||||
Bf/bf, breast feeding; CS, caesarean section; EPDS, Edinburgh Postnatal Depression Scale; GP, general practitioner; HCP, healthcare professional; Instr, instrumental delivery; LoS, length of stay; multip, multiparous; MW, midwife; NCT, National Childbirth Trust; NHS, National Health Service; PN, postnatal; primip, primiparous; RCT, randomised controlled trial; SVD, spontaneous vaginal delivery.
*Reported in original trial report.78
Table 2.
Characteristics of included qualitative studies
| Study identification, country | Study aim | Methods | Analysis | Sample characteristics | Themes, findings | |
| Baker et al,48 England | To explore women’s experience of childbirth and the post partum in the context of Changing Childbirth. | Semistructured interviews with 24 women (of 99 recruited for previous study of PN depression), 4–5 years post partum in women’s homes. Interviews recorded and transcribed. | Open and axial coding conducted independently by 3 researchers who then met to discuss interpretation. | Age range | 27–45 | Perception of control. |
| Primips | 9 | Staff attitudes and behaviour. | ||||
| Caucasian | All | Resources. | ||||
| Mode of delivery | Feeding. | |||||
| SVD | 16 | |||||
| Instr | 3 | |||||
| CS | 5 | |||||
| Length of stay | 1–3 days | |||||
| Beake et al,49 England | To explore women’s views and experiences on PN care in hospital and at home. | Indepth, semistructured interviews 8–12 months post partum in women’s homes conducted by researcher. Interviews recorded and transcribed. | Thematic approach similar to that adopted in grounded theory. 2 researchers independently read and coded transcripts. | 22 women, no demographics reported. ‘Diverse’ sample. Over one-third of the sample could not be contacted. | Support: unable to ask for help as women thought MWs too busy. Feeling neglected. Help with feeding the baby. Informational support. Poor facilities. Lack of privacy. Women wanted to go sooner. |
|
| Beake et al,50 England | To explore women’s experience and expectations of hospital PN care. | Semistructured interviews by research MW on PN ward within a few days of birth. | 2 researchers independently read transcripts to identify themes, analytic framework developed. Interviews continued until data saturation reached. | 20 women | Ward environment. | |
| Age range (years) | 23–39 | Attitudes of staff. | ||||
| White Europeans | 18 | Support for bf. | ||||
| Afro-Caribbean | 1 | Unmet information needs. | ||||
| Chinese | 1 | Women’s low expectations of care. | ||||
| Primips | 13 | |||||
| Mode of delivery | ||||||
| SVD | 2 | |||||
| Instr | 3 | |||||
| Emergency CS | 12 | |||||
| Elective CS | 3 | |||||
| Bowes and Domokos,51 Scotland | To explore Pakistani women’s own health concerns, including those related to maternity service provision. | Semistructured interviews, through an interpreter if required, in women’s home or community venue, time point not stated. | Interviews transcriptions indexed and sorted. | 19 Pakistani women and 1 Libyan, characteristics not reported. | Negative staff attitudes. Women reluctant to criticise service. Women appreciated having their babies taken away during night. Hospital food was criticised. |
|
| Care Quality Commission,22 England (mixed methods) | No objectives specified. | Free-text comments in postal questionnaires sent at 3 months post partum in 2013 to a random sample of women. Free-text from 10 007 women but only 8000 analysed. | Thematic analysis. | Whole sample: Mode of delivery |
Spoken to rudely and without consideration. Lack of discussion and explanation following complications. Being left unattended too long. Being neglected. Discharge too soon or held up. Partners not able to stay. Ward too noisy. Lack of privacy. Severely understaffed. MWs bossy and pushy. No support with bf. |
|
| SVD | 60% | |||||
| Instr | 14% | |||||
| CS | 26% | |||||
| No other characteristics reported. No characteristics reported specific to women who wrote free-text comments. | ||||||
| Cheyne et al,24 Scotland (mixed methods) | No objectives specified. | Free-text comments in postal questionnaires sent at 3 months post partum in 2015 to a random sample of women. Free-text from 1244 women. | Thematic analysis using detailed coding and constant comparison. | Whole sample: | Staff were excellent but too busy to have time to help with practical support. Some staff rude and unsupportive. Food was poor. Noisy environment. No proper aftercare or advice for specific conditions. Receiving conflicting advice. Need to build up women’s confidence. Women wanted partner involvement. Lengthy wait for discharge. |
|
| Age <25 years | 10% | |||||
| 25–34 years | 60% | |||||
| 35+ | 30% | |||||
| Primips | 42% | |||||
| White | 93% | |||||
| Mode of delivery | ||||||
| SVD | 53% | |||||
| Instr | 14% | |||||
| CS | 33% | |||||
| Condon et al,52 England | To explore teenagers’ experience of bf promotion and support by health professionals. | Semistructured interviews and focus groups involving 23 teenage mothers up to 2 years post partum, carried out in 2009. Snowball sampling. Interviews recorded and transcribed. Location for interviews not reported. | Inductive thematic analysis using NVivo. | 23 teen mothers aged <19 years, predominantly white (details not reported for PN sample). Mode of delivery and parity not reported. |
Experiences of bf promotion and support at birth. Experiences of continuing bf support. MWs helpful in showing how to position baby but insufficient help with subsequent feeds. |
|
| Cross-Sudworth et al,53 UK | To explore perspectives of first-generation and second-generation women of Pakistani origin and their experiences of maternity care. | Purposive sample. Semistructured interviews (n=8) and focus groups (n=7 in two groups), 3–18 months post partum in community setting, with interpreter as required. | Q methodology using −14 stage process to content analysis. Q set independently assessed by all team members. | UK-born | 10 | Empowerment and high confidence. Isolation and need for professional support. Poor maternity care. Caring maternity services and cultural traditions. Information and support. Importance of MW care. Wanted help bathing the baby. Wanted to stay longer. |
| UK-educated | 12 | |||||
| Age range | 15–21 years | |||||
| Parity | 1–4 | |||||
| Dykes,54 England | To explore the nature of interactions between MWs and bf women in PN ward, 2000–2002. | Participant observation of 97 encounters and 106 focused interviews with 61 women on PN ward in the first few days of birth. Excluded women unable to communicate in English or if baby was in NICU. | Ethnographic thematic analysis. Concurrent data collection and analysis. Basic, organising and global themes developed. Continued until theoretical saturation. | Age range (years) | 17–42 | MWs extremely busy, women aware of pressure on MWs. Bf support mechanical act and time-bound process. Limited continuity of carer. MWs constrained from developing ‘authentic presence’, not based on trusting relationship, led to labelling and stereotyping. Bf as a technically managed activity, teaching of specific techniques in reductionist way, invading body boundaries. Conflicting information received. |
| Primips | 40 | |||||
| White | 56 | |||||
| Asian | 5 | |||||
| Mode of delivery | ||||||
| SVD | 37 | |||||
| Instr | 11 | |||||
| CS | 13 | |||||
| Edwards,55 Scotland | To explore the expectations, knowledge and experiences regarding bf initiation in PN women. | 5 focus groups including 8 PN women within 6 months post partum held at PN clinics. Focus groups recorded and transcribed. | Inductive and deductive thematic analysis. | 8 PN women. All primips. All white. |
Women who had CS upset of not having skin-to-skin contact with the baby. MW taking over, attaching the baby to the breast. Distressing feeding experiences. Feeling of dependency bf, women expected the MW to attach baby to the breast. Lack of skill on the part of the MWs when baby does not attach. Reality better than what women expected. Busy MWs, some short-tempered, seemed uninterested. Feeling left alone. Receiving inconsistent help and support. Peers providing help in hospital with feeding. |
|
| Age 26–30 years | 3 | |||||
| 31–35 | 4 | |||||
| 36–40 | 1 | |||||
| No data on mode of delivery. | ||||||
| Fawcett,56 UK | To examine women’s experiences of hospital-based PN care. | Stories posted by women to the Patient Opinion website relating to hospital PN care, 2013–2015. | Thematic analysis. | 168 stories. No characteristics reported. |
Bf support: primips reported more negative experience. Inclusion of partners. Longer visiting hours. Contrast between good day care, poor night care. Ward environment. Not receiving pain relief. Fast discharge when women wished to be discharged early. Women happy to stay in hospital longer when staff intention was good. Positive comments when continuity of carer. Hospital staff stressed and overworked. Treating women as people not a number. |
|
| Fraser,57 England | To determine how competence in midwifery might be defined from the women’s perspective and aid curriculum development. | Opportunistic sample of 40 women. Semistructured to unstructured interviews at 3 times, including 6–48 hours after birth (n=28), in hospital in 1996 with an interpreter if required. | Thematic analysis using constant comparison aided by Textbase Alpha. | Whole sample: | Not specific to PN hospital care. | |
| Age <20 years | 4 | Characteristics and qualities of caregivers. | ||||
| 20–29 | 22 | Individualised care. | ||||
| 30+ | 15 | Clinical competence of the caregivers. | ||||
| White British | 28 | Developing a trusting relationship with a female MW was perceived as essential to promoting a positive childbirth experience. | ||||
| Primips | 14 | |||||
| Mode of delivery | ||||||
| SVD | 25 | |||||
| Instr | 7 | |||||
| CS | 7 | |||||
| Garcia et al,28 England and Wales (mixed methods) | No objectives specified. | Free-text comments in postal questionnaires sent at 4 months post partum in 1995 to a random sample of women. Free-text from 1042 women. | Thematic analysis. | Whole sample: | Wanting help on PN ward and not getting it. | |
| Age <25 years | 19.90% | Being patronised due to young age. | ||||
| 25–34 years | 65.60% | Poor clinical care and negligence. | ||||
| 35+ years | 14.50% | Feeling rushed and impersonal. | ||||
| Primips | 42% | Staff being rushed, understaffed wards. | ||||
| White | 92% | |||||
| Mode of delivery | ||||||
| SVD | 71.90% | |||||
| Instr | 11.70% | |||||
| CS | 17.30% | |||||
| Hirst and Hewison,33 England (mixed methods) | To compare the quality of hospital PN care for Pakistani and indigenous white women. | Indepth interviews with 139 women in their homes recorded using handwritten notes, 6–8 weeks post partum. Bilingual interviewer if required. | Content analysis. | No details of participant characteristics reported. White women who were having their first pregnancy were older than Pakistani women. Age range (15–20, 21–30 and 31–41) was similar for each district. |
Practical care and guidance. Staff support, sensitivity and communication. Rest. Length of stay. Catering. Socialisation. Psychological well-being. Ward environment. |
|
| Jomeen and Redshaw,58 England | To explore black and minority ethnic women’s experiences of maternity care. | Free-text comments in postal questionnaires sent at 3 months post partum in 2006 to a random sample of women. Free-text from 219 BME women. | Thematic analysis using NVivo. | Black | 25.50% | Feeling cared for. |
| Asian | 57.90% | Expectations of care and policies. | ||||
| Mixed | 11.40% | Rules and organisational pressures. | ||||
| Chinese | 2.70% | Staff attitudes and communication. | ||||
| Other ethnic group | 0.30% | Hospital as a safe place. | ||||
| Age range | 16–40+ | Choices denied. | ||||
| Primips | 39.30% | Sensitive and supportive care. | ||||
| Mode of delivery | Ethnicity and culture stereotyping. | |||||
| SVD | 66.70% | Improving the quality of care. | ||||
| Instr | 10.50% | |||||
| CS | 22.80% | |||||
| Lagan et al,59 Scotland | To report on women’s reflections on their infant feeding expectations and experiences. | Purposive sampling to ensure a range of infant feeding method. 40 semistructured interviews and 7 focus groups (38 women), 4–8 months post partum in non-hospital setting in 2010. | Framework analysis using NVivo. | Age range (years) | 19–41 | Mixed and missing messages. |
| Caucasian | 75 | Conflicting advice. | ||||
| Primips | 49 | Information gaps. | ||||
| Mode of delivery | Unrealistic expectations. | |||||
| SVD | 43 | Pressure to bf. | ||||
| Instr | 12 | Emotional costs. | ||||
| CS | 23 | |||||
| Not clear if themes relate to hospital or community care. | ||||||
| McCourt et al,37 England (mixed methods) | 1. Was 1:1 continuity of caregiver preferred by women? 2. Was it associated with any benefit to women? |
Free text from questionnaires (n not reported); interviews (n=24) either face-to-face or by phone; focus groups at drop-in centres (n and location not reported). | Interviews and focus groups recorded and transcribed. Key emergent themes developed through open coding. Analysis of open text corroborated by independent researcher. | Age not reported. Primips: 35%. White: 42%. Mode of delivery not reported. |
Insensitive responses to requests for support. Staff seeming unavailable, offhand, too busy. Inconsistent advice about bf. Staff undermining women’s self-esteem regarding baby care. Serious lack of morale and motivation among MWs. NB: no quotes presented. |
|
| McFadden et al,61
England |
To explore factors influencing women’s bf experiences following CS. | Semistructured interviews 2–52 days post partum, on ward or NICU, with 10 women who had delivered by CS; 5 had their babies with them on PN ward, 5 had babies in NICU. | Thematic analysis using MaxQda using constant comparison. | Age range: 27–38 years. 6 of 10 primips. 8 of 10 white British. All CS. Age range 21–40 years. Parity 1–6. UK-born: 4. No other characteristics reported. |
Maternal baby separation. Feeling isolated and left to cope alone. Lack of privacy. Underestimated the emotional and physical effects of CS. Lacking confidence in their abilities to bf. Highly dependent on ward staff to initiate bf. Receiving emotional support from staff and families. |
|
| McFadden et al,60
England |
To explore the extent to which cultural context makes a difference to experiences of bf support for Bangladeshi women and to consider the implications for the provision of culturally appropriate care. | Purposive sampling. Indepth interviews and focus groups in community setting with 23 Bangladeshi women in 2008 who had bf within the previous 5 years. Bilingual interviewer if required. | Initial coding was inductive, then codes reorganised into logical framework. | Bf support in hospital. Satisfaction with hospital care. Staff not always sympathetic to women’s need. Ineffective support with bf. Expectation of hands-on support with feeding. Women’s concerns about producing enough milk. Use of formula milk. |
||
| Proctor and Wright,63 England | To gain insights into aspects of maternity care among pregnant and recently delivered mothers. | Postal survey: 313 questionnaires returned, 155 from PN women (6–8 weeks), 117 commented in free text (‘anything in the service that had particularly impressed or bothered them’). | Framework analysis using NUD*IST. | Primips: 54%. No other characteristics reported. |
Continuity of carer. Environment of care. Information. Access. Care and treatment. Relationship with carer. Outcome. Attributes of staff. Choices. Control. |
|
| Proctor,62 England | To identify and compare perceptions of women and MWs concerning women’s beliefs about what constitutes quality in maternity services. | 7 focus groups and interviews, recorded and transcribed, 1994–1997, 2 units in Yorkshire. Interview numbers, PN time point and setting not reported. | Framework analysis using NUD*IST. | 19 PN women, 5 of whom gave birth 2–5 years previously. | Continuity of carer. | |
| Age range | 14–43 years | Environment of care. | ||||
| Parity | 0–3 | Information. | ||||
| Mode of delivery | Access. | |||||
| SVD | 7 | Care and treatment. | ||||
| Emergency CS | 3 | Relationship with carer. | ||||
| Elective CS | 2 | Outcome. | ||||
| Instr | 2 | Attributes of staff. | ||||
| Choices. | ||||||
| Control. | ||||||
| Puthussery et al,64 England | To explore the maternity care experiences and expectations in UK-born ethnic minority women. | Indepth, semistructured interviews with 34 UK-born ethnic minority women at mother’s home or convenient setting 3–12 months post partum. Interviews recorded and transcribed. | Grounded theory approach using NVivo. | Age <30 years | 14 | Sensitive care. |
| Women with adverse physical or mental health were excluded. | 30–39 | 18 | Mismatch between expectations and experiences. Women with additional needs less support than expected. Staff unfriendly and care impersonal. Care environment. PN wards perceived to be poorly equipped and furnished. Issues around privacy, noise, lack of cleanliness and hygiene. |
|||
| 40+ | 2 | |||||
| Primips | 22 | |||||
| Ethnicity | ||||||
| Indian | 11 | |||||
| Pakistani | 4 | |||||
| Bangladeshi | 2 | |||||
| Black African | 10 | |||||
| Black Caribbean | 2 | |||||
| Irish | 5 | |||||
| Ridger,65 England | To explore women’s views of ward PN care. | Purposive sample of 12 women. Non-participant observation and interviews at 2–4 weeks after birth at women’s home or a health facility. | Ethnographic analysis. | Primips | 6 | Busy wards and lack of staff. Task-initiated care. Wanting to have care needs acknowledged. Receiving support. |
| Mode of delivery | ||||||
| SVD | 5 | |||||
| Emergency CS | 2 | |||||
| Elective CS | 3 | |||||
| Instr | 2 | |||||
| Shields et al,40 Scotland (mixed methods) | To compare women’s satisfaction with MW managed care vs shared care over three different time periods as part of RCT. | Free-text comments in questionnaire about what they liked and disliked about their care, 825 women commented on hospital PN care. | Elements of satisfaction grouped and coded independently by 2 researchers. | Mean age at booking*: | Relationships with staff. | |
| MW group: 25.8 years | Information transfer. Social support. Environment. General satisfaction. |
|||||
| Shared care: 25.5 years | ||||||
| Primips: | ||||||
| MW group 54.7% | ||||||
| Shared care 53.5% | ||||||
| Mode of delivery (%): | ||||||
| MW group shared care | ||||||
| SVD: 73.5 73.7 | ||||||
| Instr: 13.6 14.3 | ||||||
| CS: 12.9 11.9 | ||||||
| Taylor,66 England | The experiences of PN ward cot type: side care crib and stand-alone cot in relation to breast feeding. | RCT substudy. Semistructured interviews in women’s home, mostly by phone. | Content analysis using NVivo. | Side care crib, n=29 | Stand-alone cot, n=35 | Birth experiences. Skin-to-skin contact. Delayed bf initiation. Mother–infant separation. Unrealistic bf expectation. Bf experiences on the PN ward. Ward environment. Introduction of formula milk on the PN ward. |
| Primips: 17 | Primips: 16 | |||||
| SVD: 15 | SVD: 10 | |||||
| CS: 2 | CS: 6 | |||||
| Multips: 12 | Multips: 19 | |||||
| SVD: 8 | SVD: 15 | |||||
| CS: 4 | CS: 4 | |||||
*Reported in the original trial report.78
Bf/bf, breast feeding; BME, Black and minority ethnic; CS, caesarean section; Instr, instrumental delivery; multips, multiparous; MW, midwife; NICU, neonatal intensive care unit; NUD*IST, Non-numberical Data Infomation Systems and Technology; PN, postnatal; primips, primiparous; RCT, randomised controlled trial; SVD, spontaneous vaginal delivery.
Quantitative studies
There were 34 quantitative studies included in the review,1 3 10 11 18–46 of which 6 were mixed methods.22 24 28 33 37 40
Of these studies, two were RCTs,32 40 one was a non-randomised controlled study,36 a further study was a before–after intervention study,19 and another three33 37 41 were cohort studies. The remaining 27 studies were cross-sectional surveys, 20 of which were national surveys with sample sizes ranging from 113734 to 26 325.30 Survey questions asked women their views on interpersonal and communication aspects of care, infant feeding advice and support received, physical and emotional well-being, length of stay and their view of their length of stay, and overall satisfaction.
The aim of the two included RCTs32 40 was ultimately to compare standard maternity care with midwife-led and managed care. Hicks et al 32 was a pilot study aiming to explore the compatibility of a new maternity care framework with maternity care as envisaged by the Changing Childbirth project. Women were randomised to either an experimental continuity of care group or a traditional care group. Women’s satisfaction with a variety of aspects of care was recorded. These included information received and interaction with healthcare professionals. In the second RCT,40 women were randomised to midwife-managed care or to standard care. However, looking at interventions to improve hospital postnatal care was not the intention of our review. Only data on women’s satisfaction ratings with the interaction with healthcare professionals, information transfer, choices and decisions, and social support were collected.
Of the included studies, 13 were conducted before 2000,26–29 33 34 36 37 40–43 45 and 21 were conducted since then. The majority of the studies were conducted in England, but one was conducted in Northern Ireland18 and seven in Scotland.24 25 29 34 39 40 42
Risk of bias of included studies
The methodological quality of the included studies was overall moderate to low (table 3). The study objectives were clearly prespecified in most of the included studies, but the research question was unclear in 11 studies.3 10 21–25 28 30 35 40 All the studies except one35 involved predefined populations. Of the 33 studies using surveys, 25 had response rates of at least 50%, and of those 8 studies had response rates over 70%,26 27 29 32 33 36 43 45 although in 1 study the denominator was women who had already agreed to participate.29 However, response rates were not reported and not possible to calculate in two studies.35 46 Sample selection was not clearly reported across the included studies, and in the majority of the studies the population had mixed risk status rather than low risk. The generalisability of the study results was also limited by differential response rates with significantly fewer responses from young, single women, those born outside the UK and those residents in deprived areas. Most of the studies reported methods to check the validity and reliability of the surveys. Overall, most of the included studies involved a sample size greater than 100 and used reliable and valid outcomes measures. However, few studies adjusted for potential confounding factors,3 19 31 32 38 46 or used statistical weighting to adjust for differential response rates.20–25 30
Table 3.
Risk of bias in quantitative studies
| Study identification | Was the research question clearly stated? | Was the study population clearly defined? | Was the participation rate of eligible persons at least 50%? | Were all the subjects recruited from the same or similar populations? | Was the sample of participants representative of low-risk women? | Are the measurements (questionnaires) likely to be valid and reliable? | Was the statistical significance assessed? | Are CIs given for the main result? | Was the sample size >100? | Were the exposure measures clearly defined, valid, reliable? | Were key potential confounding variables measured and adjusted for? | Was weighting used? | Can the results be generalised to low-risk women in the UK? |
| Alderdice et al 18 | Y | Y | N | Y | N | N | N | N | Y | Y | N | N | N |
| Bick et al 19 | Y | Y | Y | Y | U | U | Y | Y | Y | Y | Y | N | U |
| Bowers and Cheyne20 | Y | U | U | U | U | U | U | U | U | U | U | U | U |
| Care Quality Commission21 | U | Y | Y | U | Y | Y | N | N | Y | Y | N | Y | Y |
| Care Quality Commission22 (mixed methods) | U | Y | N | U | N | Y | N | N | Y | Y | N | Y | Y |
| Care Quality Commission23 | U | Y | N | U | N | Y | N | N | Y | Y | N | Y | Y |
| Care Quality Commission 201920 | Y | Y | N | U | Y | Y | Y | N | Y | Y | N | Y | Y |
| Cheyne et al 25 | U | Y | N | U | U | Y | Y | Y | Y | Y | U | Y | Y |
| Cheyne et al 24 (mixed methods) | U | Y | N | U | N | Y | Y | Y | Y | Y | N | Y | N |
| Cranfield26 | Y | Y | Y | N | U | N | Y | N | N | N | N | N | U |
| Dowswell et al 45 | Y | Y | Y | Y | Y | Y | Y | N | Y | N | N | N | Y |
| Farquhar et al 27 | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | N | N | Y |
| Garcia et al,28 first-class delivery (mixed methods) | U | Y | Y | U | Y | Y | N | N | Y | Y | N | N | Y |
| Glazener29 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | U | N | Y |
| Healthcare Commission30 | U | Y | Y | U | Y | Y | N | N | Y | Y | N | Y | Y |
| Henderson and Redshaw1 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | N | Y |
| Henderson et al 31 | Y | Y | Y | Y | Y | U | Y | Y | Y | Y | Y | Y | Y |
| Hicks et al 32 | |||||||||||||
| Hirst and Hewison33 (mixed methods) | Y | Y | Y | Y | Y | U | Y | Y | Y | Y | N | N | U |
| Hundley et al 34 | Y | Y | Y | N | Y | Y | N | N | Y | Y | N | N | N |
| Ifionu et al 35 | U | N | U | U | N | U | N | N | Y | N | N | N | U |
| Ingram et al 36 | Y | Y | Y | U | Y | U | Y | Y | Y | Y | U | N | Y |
| McCourt et al 37 (mixed methods) | Y | Y | Y | U | N | U | N | N | Y | Y | N | N | Y |
| National Childbirth Trust46 | Y | Y | Y | Y | Y | U | Y | N | Y | Y | Y | N | Y |
| Raleigh et al 38 | Y | Y | Y | Y | Y | U | Y | Y | N | Y | Y | N | Y |
| Redshaw and Heikkila10 | U | Y | Y | U | Y | Y | N | N | Y | Y | N | N | Y |
| Redshaw and Henderson3 | U | Y | N | U | Y | Y | Y | Y | Y | Y | Y | N | Y |
| Redshaw et al 11 | Y | Y | Y | Y | Y | Y | N | N | Y | Y | N | N | Y |
| Scott et al 39 | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | N | N | Y |
| Spurgeon et al 41 | Y | Y | Y | Y | U | U | Y | N | Y | Y | N | N | U |
| van Teijlingen et al 42 | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | N | N | Y |
| Wardle43 | Y | Y | Y | Y | Y | N | N | N | Y | N | N | N | Y |
| Wray44 | Y | Y | N | Y | N | N | N | N | Y | Y | N | N | N |
N, no; U, unclear; Y, yes.
We assessed the methodological quality of the two RCTs identified for inclusion using the CASP risk of bias tool for RCTs. Both RCTs32 40 clearly stated the focus of their research. Allocation to interventions was assigned randomly and the randomisation methods were reported in both trials. Information regarding whether women were aware or blinded to the intervention status is missing. Both trials reported no significant differences between groups at baseline. However, information relating to whether the groups were treated equally or differently during the study duration was unclear in both trials. Outcomes of interest were aspects of women’s satisfaction with the care they received, and as these were self-reported by the women themselves we are unable to discount the existence of bias in measuring outcomes. With regard to the intervention effect estimates, in Hicks et al,32 women reported a similar level of care satisfaction. In Shield et al,40 the estimated satisfaction with care was significantly higher in the midwife-managed care in comparison with the shared care group in relationships with staff, information transfer, choices and decisions and social support. Data on women’s emotional and physical support were not collected in either trial.
Quantitative results
Findings are reported by outcomes described across the included papers. Combining data for the following outcomes resulted in a significant heterogeneity across the study (I2 >90%) (meta-analyses not shown). Therefore, findings were tabulated and displayed in forest plots where possible.
Women’s expectations of hospital postnatal care
Women’s expectations of care were reported in one study only.19 This was a continuous quality improvement study with a before–after design. Prior to the intervention, 33.7% of women reported that care in hospital after birth was better than their expectations, and after the intervention this increased to 40.2%.
Interaction with healthcare professionals
Almost all the studies in this section of the review included some discussion of staff attitudes, communication and/or practical help received.1 3 10 11 18–32 35 38–41 43 44 46 47 However, different studies asked different questions in various different ways, making comparison problematic.
Adequate practical help was reportedly received by 84% of women in one study,26 and 59% always received help in a reasonable time.47 In another study, 56% of primiparous women reported receiving all necessary physical support.46 Between 79%3 and 94%10 of women were always spoken to so that they could understand, but only 47% of women reported that they had enough time to talk to midwives.43 Between 54% and 83%3 18 28 were always treated with respect, and 91%–92% were mostly treated with respect.10 11 Two surveys reported that 68% and 77% of women felt listened to.3 18 Four surveys also reported women’s perceptions of always being treated as an individual on the postnatal ward at between 53% and 79%.3 10 11 18
Kindness, understanding and sensitivity were reported more widely.3 10 11 18 21–25 28 30 32 47 Between 51% and 93% of women reported always being treated with kindness, but in a further survey only 41% of primiparous women received all necessary emotional support.46 Care and sensitivity were also reported as a score, 2.2 out of 5,32 and on a scale of −2 to +2 social support scored between 0.7 and 1.2.40 Always having confidence and trust in staff on the postnatal ward was reported in two studies at 59% and 69%.10 28
Information
Another vital aspect of postnatal care is for women to receive clear and adequate information. This was reported in 11 studies.21 22 24 25 27 30 32 40 43 46 47 Adequate information and explanations were always received by 53%, 58% and 65% of women in three surveys21 30 47 compared with 93%–94% who received fairly or very helpful advice in another study.27 The two studies which used the scoring systems referred to above reported explanations at 2.3 out of 532 and information transfer at between 0.7 and 1.2 on a −2 to +2 scale.40 Information about specific elements of care such as the woman’s recovery, postnatal exercises, emotional changes and advice about baby care was reported more patchily. Between 61%22 and 88%31 of women were given information about their recovery, 84% about postnatal exercises,29 53%–56% about emotional changes,22 27 and between one-third and three-quarters of women reported receiving information about elements of baby care.29 43 44 46
Postnatal hospital stay
More than half of the studies reported on the duration of hospital stay and/or women’s views about their length of stay.1 3 10 11 18 19 21–26 28 29 31 33 34 44–46 The mean length of stay was stated in seven studies10 11 18 19 29 33 45 and ranged from 1.8 days in multiparous women in 199029 to 5.9 days in women following a caesarean delivery in 1994.45 The proportion of women with longer lengths of stay declined over the years, and this is described below under the Subgroup analyses section.
About three-quarters of women felt that their duration of stay was about right.1 10 18 19 21 22 24–26 28 29 31 34 45 The proportion of women who felt satisfied with the length of hospital postnatal stay is visually presented in forest plots (see figure 2). The proportion of women who considered their length of stay too short remained remarkably constant over time at 12%–13%.1 Two studies reported that 62% and 77% of women, respectively, had some choice in their duration of stay.28 34 Another study reported that there was an association between women considering their length of stay too short and scoring high on the Edinburgh Postnatal Depression Scale.45 However, no correlation was found between length of stay and overall satisfaction with postnatal care.20
Figure 2.
Proportion of women who were satisfied with length of postnatal hospital stay. CQC, Care Quality Commission; ES, effect size.
Infant feeding
Data relating to infant feeding were reported in more than half of the studies.3 10 11 18–26 28–30 36 38 39 43 44 47 The proportion of women who reported initiating breast feeding ranged from 49% in Scotland in 201325 to 87% in England in 2015.3 Infant feeding support was also reported in 15 studies.3 10 11 18 20–26 28–30 39 Consistent advice in relation to infant feeding was always received by between 31%28 and 77% of women,30 although most estimates were between 40% and 60%. Women were also asked in most of the national surveys if they received practical help with infant feeding. Between 31%11 28 and 46%18 of women reported that they always received practical help. Similarly, always receiving support and encouragement ranged from 38%28 to 78%.30 Three studies reported that infant feeding decisions were always respected in 81%–82% of cases,21 24 25 but always having privacy to breast feed was reported by only 49% of women in one study.28
Apart from problems of definition and timing, many of these studies did not differentiate between feeding support in hospital and at home. However, a study which focused specifically on breastfeeding support in hospital36 reported that receiving enough support was associated with an adjusted OR of 2.13 (95% CI 1.28 to 3.53) for successful breast feeding.
Ward environment
Six studies reported women’s views of the ward environment,11 29 30 39 44 47 including aspects of visiting, partner being able to stay and ward hygiene. Three studies reported women’s views of visiting: 81%–89% of women were happy with the visiting arrangement, but 9%–19% thought visiting was too short, 2% thought too much visiting was allowed, and 38% thought it insufficiently flexible.29 44 In the most recent study,47 22% felt restricted by visiting hours. However, 71% said their partners were able to stay with them. One study reported partners’ experience of postnatal care and the impact of partners’ presence on women’s experience.24 In that study 58% of partners were accommodated on the postnatal ward; however, their experience in this regard was not reported.
Ward hygiene, particularly in the toilets and bathrooms, was a concern for many women, being reported as very clean by only 46% in one study29 30 and 19% in another.11 However, this may have improved: in the most recent Care Quality Commission survey, 70% of women reported wards as being ‘very clean’. Women were also critical of food,30 privacy, space, temperature and noise levels.11
Overall satisfaction with hospital postnatal care
Eight studies reported women’s overall satisfaction with hospital postnatal care,3 10 11 19 27 28 37 42 and three others reported overall quality of postnatal care.24 25 35 About three-quarters of women reported being satisfied or very satisfied with care,3 10 11 19 and between 46% and 81% reported being very satisfied with care27 28 37 42; however, the figure of 81%42 was from a survey distributed by midwives at 10 days post partum so may be biased. Good or excellent quality postnatal care was reported by 83%–86% of women in two Scottish surveys,24 25 and as poor by 11%–13% of women in another study.35 Forest plots of the proportion of women who were satisfied with overall postnatal hospital care are presented in figure 3.
Figure 3.
Proportion of women who were satisfied with overall postnatal hospital care. ES, effect size.
Qualitative studies
The literature search and screening resulted in 19 purely qualitative studies and 6 mixed-methods studies that included qualitative data relating to hospital postnatal care.22 24 28 33 37 40 48–66 Of these 25, 17 were based on interviews,28 33 37 48–54 57–78 7 on focus groups37 52 53 55 59 60 62 and 7 on free-text comments in questionnaires22 24 28 37 40 58 63; 6 used a mixture of different methods. The majority (18) were conducted in England (or England and Wales),28 33 37 48–54 57–78 5 were based in Scotland24 40 51 55 59 and 2 across the whole of the UK.53 56 Some questionnaire-based studies which included free-text quotes for illustrative purposes only have not been included here as they were not analysed using qualitative methods.
Most of the studies focused on women’s views of maternity care in general rather than their views of hospital postnatal care specifically. Six studies did focus specifically on hospital postnatal care,33 49 50 54 56 65 six others focused on infant feeding,52 55 59–61 66 and six focused on exploring the experience of ethnic minority women.33 51 53 58 60 64
Risk of bias in qualitative studies
Only three of the qualitative studies48 54 66 appeared to be entirely free from bias (table 4). Although a qualitative method was appropriate throughout, the aims generally specified and the study design was generally appropriate, the recruitment strategy and methods for data collection were sometimes unclear.33 37 50 51 53 55–57 60–64 67 The relationship between the researcher(s) and participants was only considered in nine studies,48 51 53–55 57 61 65 66 and it was often unclear how rigorous an analysis was carried out. The population was not described in eight studies,22 33 37 50–52 56 63 limiting transferability. In addition, in one study,50 interviews were conducted by a research midwife in hospital within a few days of birth, which may have resulted in biased responses. In six studies the analysis was based on free-text comments in postal surveys,22 24 28 40 58 63 in which comments tend to be brief and superficial. However, there was generally a clear statement of the findings and most of the studies could be considered valuable.
Table 4.
Quality assessment of qualitative studies
| Study identification | Was there a clear statement of the aims of the research? | Was a qualitative methodology appropriate? | Was the research design appropriate to address the aims of the research? | Was the recruitment strategy appropriate to the aims of the research? | Were the data collected in a way that addressed the research issue? | Has the relationship between researcher and participants been adequately considered? | Have ethical issues been taken into consideration? | Was the data analysis sufficiently rigorous? | Is there a clear statement of findings? | Is the research valuable? |
| Baker et al 48 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Beake et al 49 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Beake et al 50 | Y | Y | Y | U | Y | N | Y | Y | Y | Y |
| Bowes and Domokos51 | U | Y | Y | U | Y | Y | U | U | N | N |
| Cheyne et al 24 (mixed methods) | U | Y | Y | Y | Y | N | N | U | U | Y |
| Condon et al 52 | Y | Y | Y | Y | Y | N | Y | U | Y | N |
| Care Quality Commission22 (mixed methods) | U | Y | Y | Y | Y | N | N | U | Y | Y |
| Cross-Sudworth et al 53 | Y | Y | Y | U | Y | Y | Y | U | Y | U |
| Dykes54 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Edwards55 | Y | Y | Y | Y | U | Y | Y | Y | Y | Y |
| Fawcett56 | N | Y | N | N | Y | N | N | U | Y | N |
| Fraser57 | Y | Y | Y | Y | U | Y | N | N | Y | Y |
| Garcia et al 28 (mixed methods) | U | Y | Y | Y | Y | N | N | U | Y | Y |
| Hirst and Hewison33 (mixed methods) | Y | Y | Y | Y | U | N | Y | N | Y | Y |
| Jomeen and Redshaw58 | Y | Y | U | Y | N | N | Y | Y | Y | Y |
| Lagan et al 59 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| McCourt et al 37 (mixed methods) | Y | Y | Y | U | Y | N | Y | Y | Y | Y |
| McFadden et al 61 | Y | Y | Y | Y | N | Y | Y | Y | Y | Y |
| McFadden et al 60 | Y | Y | Y | Y | U | N | Y | Y | Y | Y |
| Proctor62 | Y | Y | Y | Y | N | N | N | N | Y | U |
| Proctor and Wright63 | Y | Y | Y | U | U | N | U | N | N | U |
| Puthussery et al 64 | Y | Y | Y | U | U | U | Y | Y | Y | U |
| Ridgers65 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Shields et al 40 (mixed methods) | Y | Y | Y | Y | Y | N | Y | N | Y | Y |
| Taylor66 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
N, no; U, unclear; Y, yes.
Themes from qualitative studies
Women’s expectations
Seven studies referred to women’s expectations of hospital postnatal care.50 55 58–60 64 66 None of these studies was prospective, so expectations were asked about or inferred retrospectively. These studies indicated that women often had low expectations of hospital postnatal care, which were sometimes met and sometimes exceeded.50 55 Ethnic minority women generally expected more support from staff, particularly with breast feeding, and were disappointed.60 64 Some women reported a lack of balance and honesty regarding antenatal preparation for breast feeding, leading to unrealistic expectations.59 66
Staff attitudes and behaviour
This theme, in various forms, emerged in almost all of the qualitative research in this area. Although staff were generally viewed positively, as friendly, helpful and polite,50 63 other women reported feeling neglected, feeling unable to ask for help as the midwives were perceived as too busy.22 24 28 37 49 54 55 65 Some midwives were reportedly rude or abrupt in their manner,22 24 50 and ethnic minority women in particular encountered negative staff attitudes and stereotyping.51 58 64 Some women who had a particular problem or who had a previous baby felt neglected.49
One study focused on interactions between breastfeeding women and midwives on the postnatal ward and used participant observation and focused interviews.54 They found that, due in part to time pressures on midwives, they were constrained from developing an ‘authentic presence’, which led to labelling and stereotyping. Another study reported ‘task orientated care’ focusing on routine clinical observation.65 Emotional relationships with women were often precluded by the organisation of care.
Women were aware that midwives were under pressure and often short-staffed and generally forgiving when this led to delays, even feeling guilty themselves for bothering them.24 49 54 56 Delayed discharge was commented on in several studies,22 24 48 women feeling low priority and neglected at this time.
Support
Emotional support
Twenty papers22 24 33 37 40 49 50 53–65 highlighted the need for emotional support in hospital. After birth women reported that being left alone, continuously needing to ask for help, feeling neglected and being told that the midwife would be back shortly eroded their confidence.22 24 49 65 Women reported on the difficulty experienced in having their voices heard and their choices respected. In this theme, the importance of perceived control and related elements such as trust, continuity of care, supportive care and influence over decision making came to the fore.48 53 63 Emotional support, not just practical or informational support, was also highlighted in relation to breast feeding.50 54 59–61
Women valued reassurance that they were doing well,37 and this gave them confidence in looking after themselves and their baby.10 Women wanted ‘sensitive’ care which met their individual needs. They also highlighted the need for practical support in looking after themselves and their baby, particularly those who felt vulnerable, for example after caesarean section.40 62 64
Informational support
Eleven studies reported on aspects of informational support, including inconsistent advice especially in relation to breast feeding.22 37 40 49 50 53–55 59 62 63 Women appreciated receiving information about what was happening and about practical aspects of baby care, especially primiparous women, but when this was absent it caused anxiety.49 50 Some women reported a lack of discussion and explanation following complications,22 and stressed the importance of being offered information rather than having to probe for it.62 The need for specific, detailed information so that women could be involved in decision making and to help them make choices was mentioned in three studies.58 62 63
The difficulty in conveying information about breast feeding on wards where midwives are working under pressure was noted. Some midwives felt compelled to achieve information transfer as efficiently as possible, sometimes without assessing comprehension.54
Infant feeding
Although length of hospital stay is now so short as to preclude breast feeding becoming established in hospital, it was nevertheless an important theme in many studies.22 37 48–50 52 54–56 59–61 66 There was significant overlap with several of the previous themes, such as staff attitudes and conflicting information. Some women felt harassed and pressurised to breast feed, and made to feel guilty if they could not or chose to formula feed.48 59 While some mothers said that midwives were helpful during the initial feed, they said that there was insufficient help during subsequent feeds.52 Breast feeding was also sometimes taught in a reductionist way, as a technically managed activity; some midwives physically attached the baby to the breast in a ‘hands-on’ manner, undermining the woman’s confidence in her ability to manage independently.54 55
Conversely, women who were formula feeding sometimes felt neglected and perceived that information about formula feeding was restricted, leading them to feel alienated.59 However, in some hospital postnatal wards, formula feeding was normalised, convenience being prioritised over established health benefits.66
Ward environment
This theme relates to a variety of factors in the postnatal ward, including visitors, noise levels, bright lights, temperature, lack of privacy and cleanliness, poor facilities and poor food. Reported comments were almost entirely negative.22 24 33 49–51 56 61–64 66
Some women commented on the general lack of orientation regarding the ward environment and routines, not knowing where the showers were, insufficient number of showers49 and the lack of cleanliness of the facilities that were available.22 63
The issue of visitors was criticised both ways: some women were critical of unrestricted visiting as being too noisy and preventing women from resting. It also created problems with privacy, particularly for women who were breast feeding.49 50 56 61 Conversely, other women would have preferred more open visiting, especially for their partner, to provide practical and emotional support when the midwives were too busy to provide this (see below).
Hospital food was criticised by many women, in terms of both quantity and quality.22 24 33 In particular, women who requested vegetarian or halal food fared poorly, had a lack of choice and had to ask their families to bring food with them when visiting.50 51 64
Many of the issues associated with the ward environment were perceived as being for the benefit of staff rather than the women.
Discharge
Six studies highlighted the importance of the transition to home care, and there was again a recognition of the importance of identifying the needs of individual women and vulnerable groups who may not have good family support following discharge.22 24 33 53 56 58 Women who left earlier than they wanted reported that they felt anxious about going home before they were ready. Delayed discharge caused dissatisfaction and frustration with an inefficient service.24 50 56 Other women commented positively on being able to choose how long they stayed in hospital, not feeling under pressure to leave before they were ready.24
Partners
Only three studies22 24 56 explicitly referred to partners not being able to stay on the postnatal ward as a theme, although others mentioned it in the context of support and visiting. If there were facilities for a woman’s partner to stay, and if she had her own room, this resulted in a more positive experience.56 Similarly, if the partner did not have unrestricted visiting, particularly if the woman had experienced a complicated or operative delivery, this was associated with a less positive experience.22 56 Some women reported feeling anxious when their partner had to leave, feeling relatively unsupported on the ward.24 56
Subgroup analyses
Subgroup by parity
Nine quantitative studies3 10 11 18 22 23 29 42 46 and one qualitative study55 included some data on women’s experiences of postnatal care by parity. The majority of these studies looked at length of stay by parity and reported that primiparous women had longer stays than multiparous women. The shortest mean lengths of stay were 2.1 days in primiparous women compared with 1.9 days in multiparous women (Northern Ireland in 2014),18 and the longest were 5.8 in primiparous compared with 4.0 in multiparous women (Scotland in 1990–1991).29 Women’s views of length of stay were also compared in five quantitative studies.3 10 18 22 23 These all reported that multiparous women were more likely to be happy with their length of stay. The biggest disparity was 69% compared with 75% of primiparous and multiparous women, respectively, who considered their length of stay about right.22 Infant feeding support was examined by parity in four quantitative studies,3 10 18 22 and all found that multiparous women reported more consistent advice, support and encouragement, but primiparous women reported more practical help. Multiparous women also reported receiving more information and explanations generally, and specifically about their own recovery,22 that staff were kind and treated them as individuals,11 23 were happier with the ward environment and overall were more satisfied with their postnatal stay.42 One qualitative study included eight primiparous women and explored their experience of breast feeding, but there was no comparison with multiparous women.55
Subgroup by mode of delivery
Two quantitative studies reported the mean length of stay by mode of delivery.11 45 Unsurprisingly length of stay was longer following instrumental and operative delivery. A qualitative study examined women’s breastfeeding experience following caesarean section.61 The results indicate that women underestimated the emotional and physical effects of a caesarean delivery and were reliant on staff to help them breast feed.
Subgroup by length of stay
One quantitative study included data on satisfaction by length of stay.45 The mean length of stay for women who considered their length of stay too long, about right and too short was 3.1 days, 2.6 days and 1.6 days, respectively. Six qualitative studies included length of postnatal stay as a theme or subtheme,22 24 33 49 53 56 but data were not disaggregated by length of stay.
Subgroup by hospital versus birth centre
There were no studies reporting expectations or experience of postnatal care in birth centres.
Subgroup by time period
The time periods to be compared were 1970–1989, 1990–2009 and 2010 to the present. There was only one study conducted prior to 199026 so this has been combined with the 1990–2009 period in which there were 23 quantitative studies. Between 2010 and 2017 there were 10 quantitative studies. The decline in mean length of stay is apparent, for example 5.8 days in 199029 to 2.1 days in 2014,18 and also the increase in caesarean sections from 13% in 1990 to 33% in 2015 in Scotland24 29 and 13% in 1981 to 26% in 2014 in England.3 26 One study explicitly examined change over time in women’s experience of maternity care using data from four surveys dating from 1995 to 2014.1 The proportion of women who considered their length of stay too short remained constant at 12%–13%, but always having confidence and trust in postnatal staff fell between 1995 and 2006 from 75% to 69%. However, support for infant feeding improved considerably over this period, particularly always receiving consistent advice which improved from 31% in 1995 to 43% in 2014.1 Staff interaction also generally improved. Women reporting that they were always treated as an individual increased from 53% in 200611 to 79% in 2014,18 and perceived respect increased from 54% in 199528 to 92% in 200611 before tailing off again to 76% in 2014.3
Thirteen of the qualitative studies were published prior to 2010 and 12 since 2010. However, the themes described did not differ substantively over the time period.
Ethnicity
Two studies explicitly focused on the perceptions of women from minority ethnic groups.31 33 These both reported variations in length of postnatal stay and women’s views of this. Women from all non-white ethnic groups had longer lengths of stay than white women, but they expected to stay even longer and, except for women of mixed ethnicity, were less likely to consider their length of stay about right.31 33
Six qualitative studies focused on the experiences of ethnic minority women on postnatal wards.33 51 53 58 60 64 All except one58 which used free-text from a survey were based on interviews with ethnic minority women. Bilingual interviews or interpreters were used as necessary except for one study64 which focused on UK-born ethnic minority women. Three main themes emerged in relation to ethnicity:
Negative staff attitudes and stereotyping were a dominant theme related to ethnicity.51 Women reported being treated without kindness, not being listened to or treated as an individual. However, in one study which compared the experiences of Pakistani women with those of white indigenous women, it was the white women who made the most complaints.33 Related to this were difficulties with communication due to language or unfamiliarity with the National Health Service (NHS) systems and rules.33 51 53 Women were particularly critical of rules forbidding them having their partner stay, leaving them feeling isolated from friends and family. Women also reported a lack of practical support, for example, wanting (and failing) to be shown how to bathe their baby.33 53 However, women were reluctant to criticise midwives, recognising that they were busy and not feeling that they have the right to complain.51 Running counter to this subtheme, one study reported some more highly educated women feeling empowered and confident.53
Cultural traditions, rest and duration of hospital stay.53 In many cultures it is considered appropriate for women to stay in bed and rest for a significant amount of time following childbirth.68 However, currently in the NHS women generally stay only 1 or 2 days following a normal delivery,4 which women of Asian ethnicity often feel is too short.33 Women complained about not getting rest in hospital due to the noise, lights and other babies.33 Many women think of hospital as a safe place should anything go wrong with either the mother or the baby, so women felt anxious if they were discharged early, particularly if they did not have family nearby.58 However, some women also reported feeling that the length of stay was too long and that they were bored, particularly if they lacked the social interaction with their partner, friends and family. A further cultural norm in many ethnic minority families is for the baby to be taken away at night to allow the mother to sleep. While this was viewed positively when it occurred,51 it is not recommended by the Baby Friendly Initiative, which recommends rooming in69 and is now unusual.
Food and privacy. As noted previously, women who requested vegetarian or halal food were particularly poorly served.51 Similarly, while many white women also criticised the wards for a lack of privacy, for ethnic minority women it was a major concern.
Discussion
Summary of findings
The main aims of this review were to report on women’s satisfaction with hospital/birth centre postnatal care, to explore how this relates to expectations and experience of care, and to identify gaps in hospital postnatal service provision in the UK. We included 53 studies of weak to moderate methodological quality.
The duration of hospital stay after delivery was one of the most commonly discussed outcomes across the included studies. While the length of stay decreased over time, this was not reflected in changes in the level of satisfaction with maternity care. More importance was placed on women having some choice in their duration of stay and the discharge itself not being unduly delayed. This is in keeping with a policy initiative in Canada which offered an increase in postnatal stay up to 60 hours. This showed an increase in satisfaction with postnatal length of stay irrespective of whether or not women chose to stay 60 hours.70 While study design limitations necessitate caution in interpretation, Watt et al 70 also found that there was not a large increase in duration of stay as women appeared to leave hospital when they felt ready and there were no changes in maternal or infant health outcomes. Not surprisingly, the ability to exercise some degree of control over care continues to be an important issue in women’s satisfaction, and Watt et al’s70 studies suggest that it is probably a factor in a woman’s decision about how long to stay in hospital.
Staff interaction was generally viewed favourably in both quantitative and qualitative studies. Overall women’s perceptions of care, being spoken to so they could understand, feeling listened to and treated as an individual appeared to improve over time. However, many studies reported that midwives did not have enough time to talk to, or otherwise support, women leading to ‘task oriented care’65 and a lack of ‘authentic presence’.54 A number of recommendations in the NICE guidelines7 highlight the need for good communication, for example, asking the woman about her health and well-being and that of her baby, offering consistent information and clear explanations to empower the woman to take care of her own health and that of her baby, and to recognise symptoms that may require discussion, encourage the woman and her family to report any concerns in relation to their physical, social, mental or emotional health, discuss issues, and ask questions. While establishing good communication is a perennial problem in all aspects of care, the lack of time and resources in the face of many tasks would appear to be particularly problematic in achieving these NICE postnatal care recommendations.
Communication and support were also raised in many of the included studies in relation to infant feeding. Women reported receiving conflicting advice, sometimes feeling pressurised to breast feed, and there was also a lack of support and information for women who were formula feeding. Breast feeding was sometimes taught in a reductionist way, and there was a lack of privacy for breast feeding. However, while the data could not be meta-analysed, the quantitative studies suggested an improving picture with regard to consistent advice, practical help and active support, which all increased over time. Interestingly, these problems highlight the focus on informational and practice support on breast feeding in the NICE guidelines and reflect the lack of guidance on providing emotional support related to infant feeding. An international meta-synthesis by Schmied et al 71 emphasised the importance of person-centred communication skills and of relationships in supporting a woman to breast feed, in keeping with the findings of this review. Schmied et al 71 also concluded that organisational systems and services that facilitate continuity of caregiver, for example, continuity of midwifery care or peer support models, are more likely to facilitate supportive care and a trusting relationship with professionals.
Gaps in the literature included the relationship between expectations and experiences, the experiences of minority and vulnerable groups, and the experiences of partners and the wider family. There was only one quantitative study which explicitly explored women’s expectations of hospital postnatal care, although seven qualitative studies included some reference to this. Wider maternity care literature suggests that expectations impact on our experience of care.72 However, from the current review, it is unclear if the lower satisfaction with postnatal care, in comparison with antenatal or intrapartum care, is related to unmet expectations, poor experience of birth or after giving birth, or the emotional or physical well-being of the women reporting their experiences.
Over 20 years ago, the WHO recommended that care after childbirth should include all family members73; however, partners’ experience of postpartum care has received little attention. The Royal College of Midwives in collaboration with the Royal College of Obstetricians and Gynaecologists, the Department of Health and the Fatherhood Institute produced a paper highlighting the importance of making opportunities to explore and discuss both the mother’s and father’s experiences of childbirth and early parenting.74 The paper also identified the need to provide health education and support to both parents, covering general health and well-being advice such as nutrition, exercise, rest and relaxation, healthy lifestyle habits, and contraception. From this review it is clear that, in the UK, early postnatal care is not designed to involve partners despite being noted as a priority by the NICE guidelines.
Strengths and limitations
This is an up-to-date systematic review reflecting on women’s experiences of postnatal care in hospitals in the UK. The search strategy was broad and covered 10 different databases. The methods were rigorous, and quality assessment and data extraction were performed by authors independently of each other.
Although we set out to review the literature relating to postnatal care for women at low risk of complications to explore routine practice, this was not always possible. Most of the studies reported results undifferentiated by risk and without excluding those women at high risk. Similarly, this review has focused on postnatal care in hospital, but for some outcomes, particularly those relating to infant feeding, it was not possible to separate hospital from community care. These studies were included for completeness.
The breadth of the review was a strength in terms of a comprehensive assessment of existing literature, but this also limited the ability to meta-analyse the data in a meaningful way due to heterogeneity.
Implications for research
The review identified a number of gaps in the literature that would benefit from additional research. Although several large surveys included women who delivered in birth centres, no studies were found which specifically explored women’s experience of postnatal care in these settings. This would be a topic worth exploring, particularly as there has been an increase in the number of birth centres in the UK over time. Further research is also required to explore the experiences of women with more complex needs. For example, there was some evidence that women were more critical of their care following an operative delivery or following complications in childbirth, when they expected that physical help and support would be more forthcoming.
Priority should be given to developing a stronger evidence base to guide postnatal hospital care in areas such as length of hospital stay, the use of clinical pathways, involvement of partners, and the nature and timing of routine observations of the mother and the baby to enhance the provision of individualised care. Schmied and Bick75 highlighted a number of potential strategies that might improve care, including planning for the postnatal period during pregnancy, development of consumer-written information, introduction of new handheld records to prompt individualised care, and offering daily ‘One to One’ time in which a midwife listens to a woman’s needs and discusses issues related to their health and that of their baby. Such initiatives are promising but require rigorous evaluation.
Also when conducting evaluations we need to rethink how to measure the main outcomes of postnatal care. The so-called ‘hard outcomes’ such as maternal morbidity and breastfeeding initiation remain important but, building on our review findings, we need to detect other aspects that are important to women, including discharge readiness, parenting confidence and psychological well-being (both positive and negative aspects).
Policy implications
The review suggests that current approaches, such as fixed length of stay, may inhibit rather than support individualised care for women after childbirth and that a move towards greater flexibility in the organisation and provision of care would be valued by women. Hospital care was widely perceived by women to be complex, busy and under-resourced, which allowed for limited investment in effective psychosocial support to women and their families at this key time just after birth. Studies of women’s views of maternity care have consistently found that hospital postnatal care is poorly rated compared with other areas of maternity care. In line with the recommendations from Better Births8 and the Maternity Transformation Programme,9 strategies are needed to optimise women’s experiences, including improving communication and information giving, involving women in decisions regarding their length of stay, and continuing to improve feeding support. NICE postnatal care guidelines are currently being reviewed and updated, which provides an important opportunity to reflect on our current model of care and its limitations.
The review also highlights that more needs to be done to integrate partners into postnatal hospital care policy. Partners are important as supporters and a resource for the mother76 and as a recipient of care.77 A number of other groups were also identified who would benefit from additional research and policy attention, for example, primiparous women, those with complex needs, those from ethnic minorities and other vulnerable groups.
Much of the research in this review suggests that staff shortages have placed midwives under too great a pressure to provide a good service. This clearly has resource implications, but this must be considered for realistic strategic future planning. If we want to see further reductions in maternal and perinatal mortality and improved experiences of care, much more needs to be done to establish effective care particularly in the early days after birth.
Conclusions
This review suggests that the majority of women in the UK were generally happy with their hospital postnatal care. The results of this review suggest that there are areas of hospital postnatal care that could be improved to ensure that the first days after birth establish good maternal and infant health and well-being.
Supplementary Material
Acknowledgments
Our thanks to Maggie Redshaw and Merryl Harvey for commenting on a draft manuscript and Charles Opondo for his assistance with the meta-analyses and forest plots. Thank you also to our PPPI stakeholder network for their ongoing contribution to dissemination of findings.
Footnotes
Contributors: FA conceived the idea and planned the project. FA, JH and RM developed the protocol, and RM developed the search strategy. RM, JH and FA screened the search results and full papers, assessed the quality of included papers, extracted the data and synthesised the results. RM, JH and FA drafted the manuscript, and all authors agreed on the final manuscript. RM conducted the search update. RM and FA screened and extracted the updated results, and RM, JH and FA agreed on the revised manuscript.
Funding: This paper reports on an independent study whichwas funded by the Policy Research Programme in the Department of Health. The views expressed are not necessarily those of the Department. The Department of Health was not involved in any aspect of the study.
Disclaimer: The views expressed are not necessarily those of the Department.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: All the data included in this systematic review are in the public domain.
Patient consent for publication: Not required.
References
- 1. Henderson J, Redshaw M. Change over time in women’s views and experiences of maternity care in England, 1995-2014: A comparison using survey data. Midwifery 2017;44:35–40. 10.1016/j.midw.2016.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rush JCI, Enkin M. Care of the new mother and baby : Chalmers IEM, Keirse M, Effective care in pregnancy and childbirth. Oxford: Oxford University Press, 1989:1341–4. [Google Scholar]
- 3. Redshaw M, Henderson J. Safely delivered: a national survey of women’s experience of maternity care 2014. Oxford 2015. [Google Scholar]
- 4. NHS Digital. Hospital Maternity Activity, 2015-16 London: NHS Digital. 2016. http://digital.nhs.uk/catalogue/PUB22384
- 5. Brown S, Small R, Faber B, et al. Early postnatal discharge from hospital for healthy mothers and term infants. Cochrane Database Syst Rev 2002;3:CD002958 10.1002/14651858.CD002958 [DOI] [PubMed] [Google Scholar]
- 6. Waldenström U, Sundelin C, Lindmark G. Early and late discharge after hospital birth: breastfeeding. Acta Paediatr Scand 1987;76:727–32. [DOI] [PubMed] [Google Scholar]
- 7. National Institute for Health and Care Excellence. Postnatal care up to 8 weeks after birth. London: NICE, 2006. [PubMed] [Google Scholar]
- 8. NHS England. National Maternity Review. Better Births. Improving outcomes of maternity services in England. London, 2016. [Google Scholar]
- 9. NHS England. Maternity Transformation Programme London: NHS England. 2017. https://www.england.nhs.uk/mat-transformation/
- 10. Redshaw M, Heikkila K. Delivered with care: a national survey of women’s experiences of maternity care 2010. Oxford: NPEU, 2010. [Google Scholar]
- 11. Redshaw M, Rowe R, Hockley C, et al. Recorded delivery: a national survey of women’s experiences of maternity care 2006. Oxford: NPEU, 2006. [Google Scholar]
- 12. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. National Institute of Health and Care Excellence. Antenatal care for uncomplicated pregnancies. 2017. https://www.nice.org.uk/guidance/cg62 [PubMed]
- 14. Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res 2012;22:1435–43. 10.1177/1049732312452938 [DOI] [PubMed] [Google Scholar]
- 15. National Institute for Health. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort2017
- 16. Critical Appraisal Skills Programme. CASP Qualitative Checklist. 2017. http://www.casp-uk.net/casp-tools-checklists;
- 17. Dixon-Woods M, Bonas S, Booth A, et al. How can systematic reviews incorporate qualitative research? A critical perspective. Qualitative Research 2006;6:27–44. [Google Scholar]
- 18. Alderdice F, Hamilton K, McNeill J, et al. Birth NI: a survey of women’s experience of maternity care in Northern Ireland. Belfast: Queen’s University Belfast, 2016. [Google Scholar]
- 19. Bick D, Murrells T, Weavers A, et al. Revising acute care systems and processes to improve breastfeeding and maternal postnatal health: a pre and post intervention study in one English maternity unit. BMC Pregnancy Childbirth 2012;12:41 10.1186/1471-2393-12-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bowers J, Cheyne H. Reducing the length of postnatal hospital stay: implications for cost and quality of care. BMC Health Serv Res 2016;16:16:16 10.1186/s12913-015-1214-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Care Quality Commission. Women’s experiences of maternity care in England: key findings from the 2010 NHS trust survey. 2010. www.cqc.org.uk/sites/default/files/media/documents/20101201_mat10_briefing_final_for_publication_201101072550.pdf
- 22. Care Quality Commission. National findings from the 2013 survey of women’s experiences of maternity care. London: CQC, 2013. [Google Scholar]
- 23. Care Quality Commission. 2015 survey of women’s experience of maternity care. Statistical release. London: CQC, 2015. [Google Scholar]
- 24. Cheyne H, Critchley A, Elders A, et al. Having a baby in Scotland 2015: listening to mothers. National report. Edinburgh: NHS Scotland, 2015. [Google Scholar]
- 25. Cheyne H, Skår S, Paterson A, et al. Having a baby in Scotland 2013: women’s experiences of maternity care. National report. Edinburgh: NHS Scotland, 2013. [Google Scholar]
- 26. Cranfield FM. Survey of postnatal care. J R Soc Med 1983;76:41–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Farquhar M, Camilleri-Ferrante C, Todd C. Continuity of care in maternity services: women’s views of one team midwifery scheme. Midwifery 2000;16:35–47. 10.1054/midw.1999.0189 [DOI] [PubMed] [Google Scholar]
- 28. Garcia J, Redshaw M, Fitzsimons B, et al. First class delivery: a national survey of women’s views of maternity care. Audit Commission, NPEU: Oxford, 1998. [Google Scholar]
- 29. Glazener C. Investigation of postnatal experience and care in Grampian: University of Aberdeen, 1999. [Google Scholar]
- 30. Healthcare Commission. Women’s experiences of maternity care in the NHS in England. London: Commission for Healthcare Audit and Inspection, 2007. [Google Scholar]
- 31. Henderson J, Gao H, Redshaw M. Experiencing maternity care: the care received and perceptions of women from different ethnic groups. BMC Pregnancy Childbirth 2013;13:196 10.1186/1471-2393-13-196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hicks C, Spurgeon P, Barwell F. Changing Childbirth: a pilot project. J Adv Nurs 2003;42:617–28. [DOI] [PubMed] [Google Scholar]
- 33. Hirst J, Hewison J. Hospital postnatal care: obtaining the views of Pakistani and indigenous ‘white’ women. Clinical Effectiveness in Nursing 2002;6:10–18. 10.1054/cein.2002.0250 [DOI] [Google Scholar]
- 34. Hundley V, Rennie AM, Fitzmaurice A, et al. A national survey of women’s views of their maternity care in Scotland. Midwifery 2000;16:303–13. 10.1054/midw.2000.0231 [DOI] [PubMed] [Google Scholar]
- 35. Ifionu J, Hamouda T, Saleh M. A survey of the quality of maternity care at the Norfolk & Norwich University Hospital NHS Foundation Trust. Arch Dis Child Fetal Neonatal Ed 2010;95:Fa99 10.1136/adc.2010.189761.34 [DOI] [Google Scholar]
- 36. Ingram J, Johnson D, Greenwood R. Breastfeeding in Bristol: teaching good positioning, and support from fathers and families. Midwifery 2002;18:87–101. [DOI] [PubMed] [Google Scholar]
- 37. McCourt C, Page L, Hewison J, et al. Evaluation of one-to-one midwifery: women’s responses to care. Birth 1998;25:73–80. [DOI] [PubMed] [Google Scholar]
- 38. Raleigh VS, Hussey D, Seccombe I, et al. Ethnic and social inequalities in women’s experience of maternity care in England: results of a national survey. J R Soc Med 2010;103:188–98. 10.1258/jrsm.2010.090460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Scott PA, Taylor A, Välimäki M, et al. Autonomy, privacy and informed consent 2: postnatal perspective. Br J Nurs 2003;12:117–27. 10.12968/bjon.2003.12.2.11051 [DOI] [PubMed] [Google Scholar]
- 40. Shields N, Turnbull D, Reid M, et al. Satisfaction with midwife-managed care in different time periods: a randomised controlled trial of 1299 women. Midwifery 1998;14:85–93. [DOI] [PubMed] [Google Scholar]
- 41. Spurgeon P, Hicks C, Barwell F. Antenatal, delivery and postnatal comparisons of maternal satisfaction with two pilot Changing Childbirth schemes compared with a traditional model of care. Midwifery 2001;17:123–32. 10.1054/midw.2001.0255 [DOI] [PubMed] [Google Scholar]
- 42. van Teijlingen ER, Hundley V, Rennie AM, et al. Maternity satisfaction studies and their limitations: "What is, must still be best". Birth 2003;30:75–82. [DOI] [PubMed] [Google Scholar]
- 43. Wardle S. Getting consumers' views of maternity services. Professional Care of Mother & Child 1994;4:170–4. [PubMed] [Google Scholar]
- 44. Wray J. Seeking to explore what matters to women about postnatal care. British Journal of Midwifery 2006;14:246–54. 10.12968/bjom.2006.14.5.21041 [DOI] [Google Scholar]
- 45. Dowswell T, Piercy J, Hirst J, et al. Short postnatal hospital stay: implications for women and service providers. J Public Health Med 1997;19:132–6. [DOI] [PubMed] [Google Scholar]
- 46. National Childburth Trust. Left to your own devices: the postnatal care experiences of 1260 first-time mothers. London: NCT, 2010. [Google Scholar]
- 47. Care Quality Commission. 2018 survey of women’s experiences of maternity care. 2019. https://wwwcqcorguk/publications/surveys/maternity-services-survey-2018
- 48. Baker SR, Choi PYL, Henshaw CA, et al. ‘I Felt as though I’d been in Jail’: Women’s Experiences of Maternity Care during Labour, Delivery and the Immediate Postpartum. Fem Psychol 2005;15:315–42. 10.1177/0959-353505054718 [DOI] [Google Scholar]
- 49. Beake S, McCourt C, Bick D. Women’s views of hospital and community-based postnatal care: the good, the bad and the indifferent. Evidence Based Midwifery 2005;3:80–6. [Google Scholar]
- 50. Beake S, Rose V, Bick D, et al. A qualitative study of the experiences and expectations of women receiving in-patient postnatal care in one English maternity unit. BMC Pregnancy Childbirth 2010;10:70 10.1186/1471-2393-10-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Bowes AM, Domokos TM. Pakistani women and maternity care: raising muted voices. Sociology of Health & Illness 1996;18:45–65. [Google Scholar]
- 52. Condon L, Rhodes C, Warren S, et al. ‘But is it a normal thing?’ Teenage mothers’ experiences of breastfeeding promotion and support. Health Education Journal 2013;72:156–62. 10.1177/0017896912437295 [DOI] [Google Scholar]
- 53. Cross-Sudworth F, Williams A, Herron-Marx S. Maternity services in multi-cultural Britain: using Q methodology to explore the views of first- and second-generation women of Pakistani origin. Midwifery 2011;27:458–68. 10.1016/j.midw.2010.03.001 [DOI] [PubMed] [Google Scholar]
- 54. Dykes F. A critical ethnographic study of encounters between midwives and breast-feeding women in postnatal wards in England. Midwifery 2005;21:241–52. 10.1016/j.midw.2004.12.006 [DOI] [PubMed] [Google Scholar]
- 55. Edwards ME. Confidence in initiation of breastfeeding: University of Stirling, 2013. [Google Scholar]
- 56. Fawcett J. The impact of postnatal care on a woman’s overall maternity experience: an analysis of stories from Patient Opinion. Sheffiel: Sheffield Medical School, 2016. [Google Scholar]
- 57. Fraser DM. Women’s perceptions of midwifery care: a longitudinal study to shape curriculum development. Birth 1999;26:99–107. [DOI] [PubMed] [Google Scholar]
- 58. Jomeen J, Redshaw M. Ethnic minority women’s experience of maternity services in England. Ethn Health 2013;18:280–96. 10.1080/13557858.2012.730608 [DOI] [PubMed] [Google Scholar]
- 59. Lagan BM, Symon A, Dalzell J, et al. ’The midwives aren’t allowed to tell you': perceived infant feeding policy restrictions in a formula feeding culture - the Feeding Your Baby Study. Midwifery 2014;30:e49–55. 10.1016/j.midw.2013.10.017 [DOI] [PubMed] [Google Scholar]
- 60. McFadden A, Renfrew MJ, Atkin K. Does cultural context make a difference to women’s experiences of maternity care? A qualitative study comparing the perspectives of breast-feeding women of Bangladeshi origin and health practitioners. Health Expect 2013;16:e124–35. 10.1111/j.1369-7625.2012.00770.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. McFadden C, Baker L, Lavender T. Exploration of factors influencing women’s breastfeeding experiences following a caesarean section. Evidence Based Midwifery 2009;7:64–70. [Google Scholar]
- 62. Proctor S. What determines quality in maternity care? Comparing the perceptions of childbearing women and midwives. Birth 1998;25:85–93. [DOI] [PubMed] [Google Scholar]
- 63. Proctor S, Wright G. Consumer responses to health care: women and maternity services. Int J Health Care Qual Assur Inc Leadersh Health Serv 1998;11:147–55. 10.1108/09526869810230803 [DOI] [PubMed] [Google Scholar]
- 64. Puthussery S, Twamley K, Macfarlane A, et al. ’You need that loving tender care': maternity care experiences and expectations of ethnic minority women born in the United Kingdom. J Health Serv Res Policy 2010;15:156–62. 10.1258/jhsrp.2009.009067 [DOI] [PubMed] [Google Scholar]
- 65. Ridgers MI. ’Passing through but needing to be heard' an ethnographic study of women’s perspectives of their care on the postnatal ward: Bournemouth University, 2007. [Google Scholar]
- 66. Taylor CA. Post-natal care and breastfeeding experiences: a qualitative investigation following a randomised trial of side-car crib use (NECOT Trial: Durham University, 2014. [Google Scholar]
- 67. Jomeen J, Redshaw M. Black and minority ethnic women’s experiences of contemporary maternity care in England. J Reprod Infant Psychol 2011;29:e9. [Google Scholar]
- 68. Katbamna S. ’Race' and childbirth. Buckingham: Open University Press, 2000. [Google Scholar]
- 69. Baby Friendly Hospital Initiative. Ten steps to successful breastfeeding. 2013. http://www.tensteps.org/ten-steps-successful-breastfeeding.shtml [DOI] [PMC free article] [PubMed]
- 70. Watt S, Sword W, Krueger P. Longer postpartum hospitalization options--who stays, who leaves, what changes? BMC Pregnancy Childbirth 2005;5:13 10.1186/1471-2393-5-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Schmied V, Beake S, Sheehan A, et al. Women’s perceptions and experiences of breastfeeding support: a metasynthesis. Birth 2011;38:49–60. 10.1111/j.1523-536X.2010.00446.x [DOI] [PubMed] [Google Scholar]
- 72. Green JM, Coupland VA, Kitzinger JV. Great expectations (2nd edn): Books for Midwives Press, 1998. [Google Scholar]
- 73. World Health Organisation (WHO). Postpartum care of the mother and newborn: a practical guide. 1998. https://wwwwhoint/maternal_child_adolescent/documents/who_rht_msm_983/en/ [PubMed]
- 74. Royal College of Midwives. Reaching out: Involving fathers in maternity care. 2011. https://wwwrcmorguk/sites/default/files/Father’s%20Guides%20A4_3_0pdf
- 75. Schmied V, Bick D. Postnatal care - current issues and future challenges. Midwifery 2014;30:571–4. 10.1016/j.midw.2014.05.001 [DOI] [PubMed] [Google Scholar]
- 76. Persson EK, Dykes AK. Parents' experience of early discharge from hospital after birth in Sweden. Midwifery 2002;18:53–60. 10.1054/midw.2002.0291 [DOI] [PubMed] [Google Scholar]
- 77. Ellberg L, Högberg U, Lindh V. ’We feel like one, they see us as two': new parents' discontent with postnatal care. Midwifery 2010;26:463–8. 10.1016/j.midw.2008.10.006 [DOI] [PubMed] [Google Scholar]
- 78. Turnbull D, Holmes A, Shields N, et al. Randomised, controlled trial of efficacy of midwife-managed care. Lancet 1996;348:213–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-022212supp002.pdf (470KB, pdf)
bmjopen-2018-022212supp001.pdf (470KB, pdf)