Abstract
Background
Reports of postoperative pain treatment after uniportal video-assisted thoracoscopic surgery are limited. Thoracic paravertebral block and serratus anterior plane block have been described recently in pain management after thoracic surgery. A comparison between these two blocks for postoperative analgesia after uniportal video-assisted thoracoscopic surgery has not been previously reported. The aim of this study was to compare the analgesic benefits of serratus plane block and thoracic paravertebral block after uniportal video-assisted thoracoscopic surgery and examined the two block types for noninferiority.
Methods
From December 2015 to May 2018, a total of 636 relevant records of patients who underwent uniportal video-assisted thoracoscopic surgery under general anaesthesia alone or with the addition of serratus plane block or thoracic paravertebral block performed preoperatively were identified. A propensity-matched analysis incorporating preoperative variables was used to compare the efficacy of postoperative analgesia in three groups.
Results
Overall, 123 patients were identified for analysis. Propensity score matching resulted in 41 patients in each group. The visual analogue scale scores were significantly lower in the serratus plane block group and the thoracic paravertebral block group than in the control group at the 1st, 2nd, 4th, and 6th postoperative hours. Cumulative opioid consumption was significantly lower in the serratus plane and thoracic paravertebral block groups than in the control group at 6 hrs (18.3±3.1 mg, 18.7±3.9 mg vs 21.5±4.4 mg; P=0.001) and 24 hrs (43.4±7.3 mg, 42.5±7.7 mg vs 49.3±8.8 mg; P<0.001) postoperatively. The serratus plane block group was noninferior to the thoracic paravertebral block group on pain score and opioid consumption.
Conclusion
The addition of single-injection serratus plane or thoracic paravertebral block is associated with early analgesic benefits in patients undergoing uniportal video-assisted thoracoscopic surgery, including a reduction in the postoperative opioid consumption and pain scores. Serratus plane block is as effective as thoracic paravertebral block for reducing postoperative pain.
Keywords: regional anaesthesia, serratus anterior plane block, thoracic paravertebral block, postoperative pain, thoracoscopic surgery
Introduction
Since uniportal video-assisted thoracoscopic surgery (UVATS) was first introduced in 2004,1 it has become increasingly popular and gradually applied for major lung resection.2–4 Conventional video-assisted thoracic surgery (VATS) uses multiple incisions. Compared with conventional VATS, patients undergoing UVATS may have less postoperative pain and improved functional outcomes. However, UVATS may still result in moderate postoperative pain.4,5 Thoracic epidural analgesia (TEA) is considered the gold standard technique for pain management after thoracic surgery. Thoracic paravertebral (TPV) block is the second best method for post-thoracotomy pain relief. However, the optimal regional analgesic technique for UVATS procedures is unclear. TEA and TPV block are relatively invasive techniques accompanied by a risk of serious complications, including pneumothorax, spinal cord trauma, sympathetic block, and hypotension. Less invasive methods of analgesia may be needed for pain management after UVATS.
Serratus anterior plane (SAP) block is a new technique for providing surgical anaesthesia and postoperative analgesia. It was originally proposed for breast surgery and is now reported to be used in thoracic surgery.6–9 SAP block is an ultrasound-guided thoracic wall nerve block that covers the lateral cutaneous branch of the intercostal nerves from the T2 to the T9 level and provides prolonged anaesthesia of the hemithorax with numbness over the thoracic area.10 Ultrasound-guided SAP block is safe and easy to perform, as it is an easy-to-learn technique and uses distinct bony landmarks. Therefore, it could be an attractive regional analgesic technique for pain control after UVATS. The aim of this study was to compare the analgesic benefits of SAP and TPV block after UVATS.
Materials and methods
The retrospective study was approved by the Institutional Ethical Committee of Harbin Medical University Cancer Hospital (Chairperson, Prof Changhong Zhao). The requirement for written informed consent was waived because this study was limited to pre-existing data that had been collected as part of the standard of care. Patients with early-stage non-small lung cancer who underwent UVATS under general anaesthesia alone or with the addition of SAP or TPV block performed preoperatively between December 2015 and May 2018 were included. The demographic and clinical data of patients were retrieved from the institutional computer-based documentation system. Patient data confidentiality was maintained, in accordance with the Declaration of Helsinki. All of the data were analyzed anonymously.
Patient selection
Patients 20–70 years of age with a body mass index (BMI)<30 kg/m2 and an American Society of Anaesthesiologists physical status class of I or II undergoing UVATS were eligible. Patients with a significant psychiatric history (major depression or generalized anxiety disorder), pre-existing chronic pain (lasting for at least 3 months), or chronic opioid use (a mean daily use of more than 30 mg of oxycodone or equivalent per day) were excluded. Patients undergoing second surgery or urgent surgery were excluded.
Anaesthesia and pain management
Although intraoperative practices may vary slightly among anaesthesiologists within the same institution, all patients undergoing UVATS at Harbin Medical University Cancer Hospital routinely receive general anaesthesia using sevoflurane or propofol and remifentanil with a double-lumen endobronchial tube.
In this study, 3 analgesic modalities were considered. The choice of analgesic modality was based on one or more of patient-related, anaesthesiologist-related, and surgeon-related preferences. The first modality included the i.v. injection of hydromorphone 5 µg/kg 20 mins before the end of surgery, followed by i.v. patient-controlled analgesia (PCA). The PCA regimen consisted of hydromorphone 0.05 mg/ml mixed with normal saline to a total volume of 300 ml. The PCA device was set to deliver a 3 ml/h background infusion and 3 ml on-demand bolus, with a 10 min lockout time. If patients reported a visual analogue scale scores (VAS)>4 postoperatively, i.v. tramadol 50–100 mg or oral oxycodone 5–10 mg was administered as a supplement. The second modality included the same opioid-based analgesic regimen, in addition to ultrasound-guided TPV block performed preoperatively by the injection of 20–25 ml of ropivacaine 0.375% at T5 or T6. The third modality combined the same opioid-based analgesic regimen with ultrasound-guided SAP block performed preoperatively by the injection of 20–25 ml of ropivacaine 0.375% superficial to the serratus anterior muscle, as previously described.11 The level of SAP or TPV block was confirmed with the pinprick test. All patients were transferred to the PACU after surgery. The assessment of postoperative pain severity and the administration of postoperative analgesics were performed by the acute pain service team.
Propensity-matched design
Patients who received SAP block were matched to those who received TPV block and to control patients (no block) at a 1:1:1 ratio using propensity score matching. This matching was used to obtain groups of patients corresponding to the 3 analgesic modalities that were balanced with regard to potential confounding baseline variables (including age, sex, BMI, surgeon identity, surgical procedure type and surgical procedure duration).
Outcome measures
The set of matched patients was compared in terms of 2 kinds of primary outcomes: (1) the VAS pain scores at the 1st, 2nd, 4th, 6th, 24th and 48th postoperative hours; and (2) the amount of opioid consumption at the 6th and 24th postoperative hours. Consumption of the different types of postoperative opioids was converted to i.v. morphine equivalents using the ClinCalc morphine equivalence calculator assuming no cross-tolerance, accessed at http://clincalc.com/opioids/.
Secondary outcomes included (1) analgesia-related side effects evaluated by the acute pain service at least once a day, including nausea and vomiting, excessive sedation, urinary retention and hypotension; (2) the intraoperative opioid requirement; and (3) the PACU duration of stay, chest tube indwelling time, and hospital stay duration. The sedation level was evaluated using the Ramsey Sedation Scale (RSS). An RSS score ≥5 was considered oversedation, and the locking time of the PCA device was prolonged to 40 mins. Hypotension was defined as systolic blood pressure <90 mmHg.
Statistical analysis
Statistical analysis was performed using SPSS version 22.0 for Windows (IBM Corp., USA) and SAS software version 9.4 (SAS Institute, Cary, North Carolina, USA). Descriptive data are expressed as the frequency, percentage, mean and standard deviation, and min-max. The chi-squared test (χ2) was used to compare qualitative data. Fisher’s exact test was used for small sample sizes (expected frequencies <5). The normality of the data distribution was assessed with the Shapiro–Wilk test and P-P plots. For normally distributed data, groups were compared by analysis of variance (ANOVA). While for non-normally distributed data, groups were compared with the Kruskal–Wallis H test. A probability value less than 0.05 was considered to indicate a significant difference between the groups, while a value greater than 0.05 was considered to indicate no significant difference between the groups.
We compared SAP block with TPV block for noninferiority on the pain score and opioid consumption at 6 hrs after surgery. Noninferiority hypotheses were assessed against a 1-sided significance criterion of 0.05. Noninferiority was claimed if the upper limit of the 95% CI for the difference in means of pain score 6 hrs postoperatively was less than the noninferiority Δ of 1, and if difference in means of opioid consumption at 6 hrs after surgery was less than the noninferiority Δ of 2.0 mg. The predetermined ∆ for these outcomes based on our experience and the literature.12,13 We considered SAP block noninferior to TPV block if it was noninferior for both outcomes.
Results
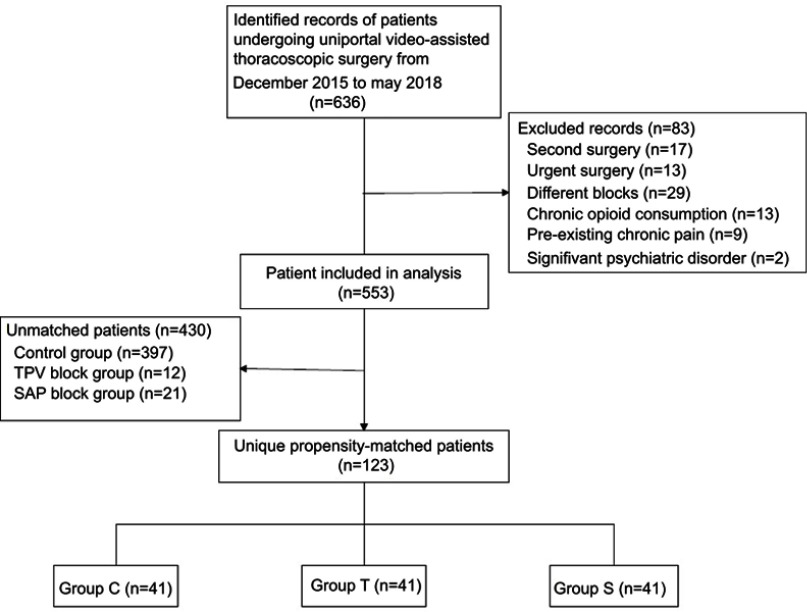
Our retrospective review identified 636 relevant records of patients who underwent UVATS between December 2015 and May 2018. Of these, 83 records were excluded (Figure 1), and 123 patients were successfully matched on a 1:1:1 basis based on predetermined confounders and baseline characteristics, including 41 patients in the SAP block, TPV block and control groups. This sample size provided 86% power for the noninferiority test of two block techniques. Matched patients were similar with respect to both matched and other baseline characteristics (Table 1).
Figure 1.
Flow diagram of case selection.
Table 1.
Patient characteristics after propensity score matching
| Parameter | Group S (n=41) | Group T (n=41) | Control (n=41) |
|---|---|---|---|
| Age (y) | 55.9±8.6 | 56.1±8.7 | 54.7±9.1 |
| BMI (kg/m2) | 24.6±3.5 | 24.2±3.7 | 25.1±4.1 |
| ASA status (I/II) | 11/30 | 14/27 | 10/31 |
| Sex (M/F) | 17/24 | 13/28 | 16/25 |
| Duration of surgery (min) | 179±18 | 181±16 | 182±18 |
| Surgeon (A/B/C) | 22/13/6 | 26/9/6 | 25/11/5 |
| Surgical side (L/R) | 20/21 | 22/19 | 21/20 |
| Chest tube number (1/2) | 27/14 | 22/19 | 23/18 |
| Surgical procedures | |||
| Lobectomy | 29 | 28 | 31 |
| Lobectomy+wedge resection | 2 | 1 | 1 |
| Segmentectomy | 7 | 7 | 6 |
| Wedge resection | 3 | 5 | 3 |
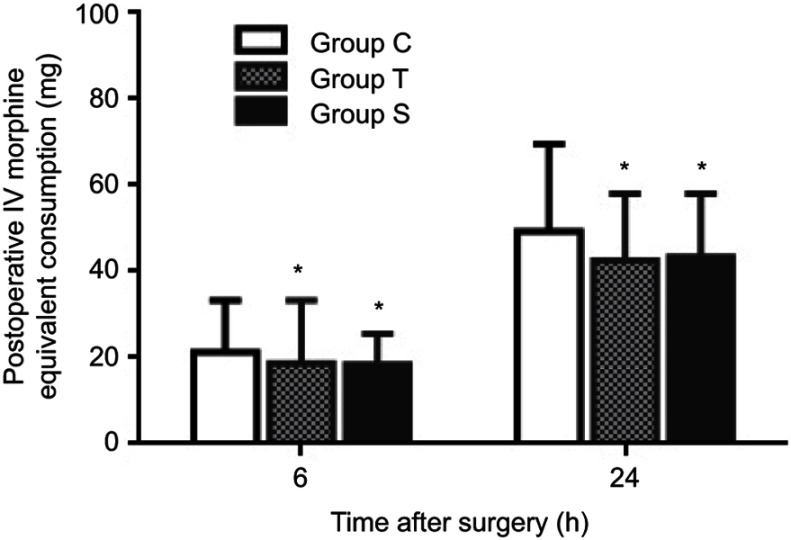
The VAS scores were significantly lower in both block groups than in the control group at the 1st, 2nd, 4th, and 6th postoperative hours (P<0.05) but were not significantly different among the three groups at 24 and 48 hrs after surgery (Table 2). Both blocks were associated with reduced postoperative opioid consumption, with cumulative opioid consumption being significantly lower in the SAP and TPV block groups than in the control group at 6 hrs (18.3±3.1 mg, 18.7±3.9 mg vs 21.5±4.4 mg; P=0.001) and 24 hrs (43.4±7.3 mg, 42.5±7.7 mg vs 49.3±8.8 mg; P<0.001) postoperatively (Figure 2). A noninferiority test was performed using both pain score and opioid consumption at 6 hrs after surgery. The SPB block group was noninferior to the TPV block group on pain score and opioid consumption. The upper confidence limits of pain score (difference 0.27, 95% CI, −0.55–1.09; P<0.001) and opioid consumption (difference −0.46, 95% CI, −2.50–1.58; P=0.024) were less than their respective deltas.(Table 3) There were no significant differences in the frequency of other analgesia-related side effects among the groups. The incidence of postoperative nausea and vomiting (PONV) was 36.6% in the control group, 19.5% in the SAP block group and 22.0% in the TPV block group. No significant differences were found in the intraoperative opioid requirement, PACU duration of stay, chest tube indwelling time, or hospital stay duration (Table 4).
Table 2.
Postoperative pain scores (visual analogue scale score)
| Time (h) | Group S (n=41) | Group T (n=41) | Group C (n=41) | P for overall group effecta | P for group S versus group Cb | P for group T versus group Cb | P for group S versus group Tb |
|---|---|---|---|---|---|---|---|
| 1 | 2.7 [2.2, 3.2] | 2.9 [2.5, 3.5] | 4.1 [3.7, 4.6] | <0.0001 | <0.0001 | 0.003 | 0.996 |
| 2 | 2.6 [2.2, 3.0] | 2.5 [2.0, 3.0] | 3.6 [3.2, 4.0] | <0.0001 | 0.001 | <0.0001 | 0.989 |
| 4 | 2.5 [2.2, 2.8] | 2.2 [1.8, 2.7] | 3.2 [2.7, 3.8] | 0.002 | 0.006 | 0.008 | 0.976 |
| 6 | 2.3 [1.9, 2.8] | 2.2 [1.7, 2.6] | 3.3 [2.8, 3.9] | 0.001 | 0.010 | 0.003 | 0.967 |
| 24 | 2.1 [1.7, 2.6] | 2.3 [1.9, 2.6] | 2.5 [2.0, 2.9] | 0.547 | 0.831 | 0.962 | 1.0 |
| 48 | 1.9 [1.6, 2.2] | 1.7 [1.4, 1.9] | 1.9 [1.6, 2.2] | 0.456 | 0.892 | 0.973 | 0.836 |
Notes: Values are expressed as the mean [95% confidence interval]. aThe P-value for the overall group effect is set at 0.05. bP-values less than 0.0167 were considered to indicate significant difference between three groups, according to the Bonferroni method.
Abbreviations: Group C, intravenous patient-controlled analgesia; group S, intravenous patient-controlled analgesia + serratus anterior plane block; group T, intravenous patient-controlled analgesia + thoracic paravertebral block.
Figure 2.
Time course of opioid consumption (converted to mg of intravenous morphine equivalents). The bar chart displays the mean opioid consumption from 0–6 and 0–24 hrs after surgery. *P<0.05 versus control group (bar chart). Group C, intravenous patient-controlled analgesia; group T, intravenous patient-controlled analgesia + thoracic paravertebral block; group S, intravenous patient-controlled analgesia + serratus anterior plane block.
Table 3.
Effect of SAP block versus TPV block on pain score and opioid consumption at 6 h after surgery using one-sided noninferiority test
| Group S (n=41) | Group T (n=41) | Noninferiority 1-tailed test | |||
|---|---|---|---|---|---|
| Difference SPB—TPV (95% CI) | Δ | P-Value | |||
| Visual analogue scale score | 2.44±1.43 | 2.17±1.36 | 0.27 (−0.55 to 1.09) | 1 | <0.001 |
| Opioid consumption (mg) | 18.33±3.08 | 18.79±3.85 | −0.46 (−2.50 to 1.58) | 2 | 0.024 |
Table 4.
Secondary outcomes (intraoperative and postoperative data)
| Group S (n=41) | Group T (n=41) | Group C (n=41) | P-Value | |
|---|---|---|---|---|
| Intraoperative total dose of remifentanil (μg) | 963.6±302.7 | 989.3±310.6 | 977.2±313.7 | 0.63 |
| Duration of stay in PACU (min) | 48±12.3 | 50±13.1 | 46±12.6 | 0.51 |
| PONV | 8 (19.5%) | 9 (22.0%) | 15 (36.6%) | 0.163 |
| Excessive sedation | 0 (0%) | 1 (2.4%) | 1 (2.4%) | 1.0 |
| Urinary retention | 1 (2.4%) | 0 (0%) | 1 (2.4%) | 1.0 |
| Hypotension | 0 (0%) | 3 (7.3%) | 1 (2.4%) | 0.32 |
| Chest tube indwelling time (h) | 55.8 (42.1–79.6) | 50.6 (39.8–82.3) | 52.3 (41.3–87.6) | 0.26 |
| Length of hospital stay (d) | 6.07±1.86 | 6.65±2.3 | 6.92±2.2 | 0.16 |
Discussion
The results of this retrospective study suggest that both block techniques are similarly effective in reducing the severity of early postoperative pain. Compared with the control, each block was associated with decreased postoperative opioid consumption after UVATS.
Previous studies reported that compared with the control group, significantly lower pain scores were found in patients receiving a single-injection TPV block for VATS, which persisted for 48 hrs postoperatively.13 Hill et al found that compared with controls, patients undergoing preoperative multilevel single-dose TPV block consumed significantly less cumulative opioids and reported lower pain scores in the first 6 hrs after block placement.14 In the context of minimally invasive surgical approaches, TPV block is considered the first-line loco-regional technique instead of TEA for VATS.15,16 Similar to TEA, complications and side effects were also observed for TPV block. Although the ultrasound-guided TPV block is a reasonably accurate and safe approach, complications such as pneumothorax, haemodynamic compromise, or total spinal anaesthesia are still possible.17–19
Compared with the control, we found that similar to TPV block, single-injection ultrasound-guided SAP block could also provide superior pain relief in the early postoperative period, with significantly lower pain scores. In this study, SAP block was found to be noninferior to TPV block in terms of cumulative postoperative opioid consumption after UVATS. In a recently published study, SAP block was reported to be an effective adjuvant treatment option for thoracotomy analgesia that could potentiate PCA analgesia, reducing pain and morphine consumption.20 Do-Hyeong Kim8 also found that single-injection SAP block with ropivacaine enhanced the quality of recovery for 2 days postoperatively and improved postoperative analgesia during the early postoperative period in patients undergoing VATS. SAP block also provides more haemodynamic stability than TEA after thoracotomy.7 A previous prospective study and case series demonstrated the efficacy of SAP block for analgesia after minor VATS, VATS lobectomy, and thoracotomy.
Despite the advantages and analgesic efficacy of SAP block, TPV block seems to be superior according to previous studies13,21 and has been preferred by anaesthesiologists.15,16 There is no research comparing SAP and TPV blocks for postoperative analgesia after UVATS. In UVATS, the incision is limited to one intercostal space, and the length and number of incisions are less than those in conventional VATS. The trauma to muscles, nerves, and blood vessels is reduced, with less postoperative pain and chest paraesthesia.2,4,22,23 SAP block can provide analgesia between the T2 and T9 levels by blocking the cutaneous branches of intercostal muscles.11,24 The duration of the sensory blockade produced by superficial and deep SAP is 730–780 mins and 380–400 mins, respectively.25–27 Compared with TPV block, SAP block produces only a somatic blockade. However, in our study, SAP block was noninferior to TPV block in terms of pain scores and cumulative postoperative opioid consumption after UVATS.
Chest tube-related pain is often reported after thoracic surgery and is not blocked sufficiently by TPV block, TEA, or selective intercostal nerve blocks. This might be partly due to unblocked nociceptive signals from the long thoracic nerve (LTN), the phrenic nerve, the thoracodorsal nerve, and the vagus nerve, as well as incompletely blocked intercostal nerves.10,28 It has been reported that SAP block can be used to provide analgesia for chest tube site pain inadequately relieved by TPV block.29 The long thoracic nerve and thoracodorsal nerve lie on the surface of the serratus anterior muscle. Because of their origin and trajectory, they are not blocked by TPV block, TEA, or any selective intercostal nerve blocks. Although these nerves have classically been considered motor nerves, recent thinking has challenged the premise that only sensory nerve blockade is necessary for analgesia. However, the extent to which these nerves contribute to postoperative analgesia is unclear.
In UVATS, the single-incision approach could minimize intercostal injury such that SAP block could be as effective as TVP block for postoperative analgesia. The SAP block technique has limited invasiveness and could be an attractive alternative for pain control after UVATS.
There are several limitations to this retrospective study. As an observational study, our conclusions may have been limited by potential errors in data collection and documentation. A randomized trial of TPV block and SAP block for postoperative analgesia after UVATS could not be performed. Although using propensity score matching may have reduced the risk of bias and improved the validity of our analysis, selection bias was not eliminated. We did not assess the dermatomal distribution of blockade after surgery in addition to the presurgical assessment. In addition, the population examined was limited to ASA I and II patients who underwent UVATS in a single center, which may not be representative of the general population.
Conclusion
Our results suggest that in patients undergoing UVATS, the addition of single-injection SAP block or TPV block is associated with early analgesic benefits, including a reduction in postoperative opioid consumption and VAS score. SAP block is as effective as TPV block in reducing postoperative pain. Compared to TPV block, SAP block is advantageous due to its relative ease of application. Although SAP block can be an effective treatment option for postoperative UVATS analgesia, further large-scale prospective randomized controlled trials are required to investigate the efficacy of and indications for SAP block.
Acknowledgments
This study was supported by Postdoctoral Office of Heilongjiang Province (Hei Long Jiang Postdoctoral Foundation Grant #LBH-Z17181).
Availability of data and material
All data generated or analyzed during this study are included in this published article.
Author contributions
L.W. and G.W. designed the study; Y.W., X. Zhang and X. Zhu collected the data; Y.W. and X. Zhu analysed the data; L.W. wrote the manuscript. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg. 2004;77:726–728. doi: 10.1016/S0003-4975(03)01219-0 [DOI] [PubMed] [Google Scholar]
- 2.Wang BY, Liu CY, Hsu PK, Shih CS, Liu CC. Single-incision versus multiple-incision thoracoscopic lobectomy and segmentectomy: a propensity-matched analysis. Ann Surg. 2015;261:793–799. doi: 10.1097/SLA.0000000000000712 [DOI] [PubMed] [Google Scholar]
- 3.Piccioni F, Segat M, Falini S, et al. Enhanced recovery pathways in thoracic surgery from Italian VATS group: perioperative analgesia protocols. J Thorac Dis. 2018;10:S555–S63. doi: 10.21037/jtd.2017.12.86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McElnay PJ, Molyneux M, Krishnadas R, Batchelor TJ, West D, Casali G. Pain and recovery are comparable after either uniportal or multiport video-assisted thoracoscopic lobectomy: an observation study. Eur J Cardiothorac Surg. 2015;47:912–915. doi: 10.1093/ejcts/ezu324 [DOI] [PubMed] [Google Scholar]
- 5.Tam JK, Lim KS. Total muscle-sparing uniportal video-assisted thoracoscopic surgery lobectomy. Ann Thorac Surg. 2013;96:1982–1986. doi: 10.1016/j.athoracsur.2013.07.002 [DOI] [PubMed] [Google Scholar]
- 6.Park MH, Kim JA, Ahn HJ, Yang MK, Son HJ, Seong BG. A randomised trial of serratus anterior plane block for analgesia after thoracoscopic surgery. Anaesthesia. 2018;73:1260–1264. doi: 10.1111/anae.14424 [DOI] [PubMed] [Google Scholar]
- 7.Khalil AE, Abdallah NM, Bashandy GM, Kaddah TA. Ultrasound-guided serratus anterior plane block versus thoracic epidural analgesia for thoracotomy pain. J Cardiothorac Vasc Anesth. 2017;31:152–158. doi: 10.1053/j.jvca.2016.08.023 [DOI] [PubMed] [Google Scholar]
- 8.Kim DH, Oh YJ, Lee JG, Ha D, Chang YJ, Kwak HJ. Efficacy of ultrasound-guided serratus plane block on postoperative quality of recovery and analgesia after video-assisted thoracic surgery: a randomized, triple-blind, placebo-controlled study. Anesth Analg. 2018;126:1353–1361. doi: 10.1213/ANE.0000000000002779 [DOI] [PubMed] [Google Scholar]
- 9.Barbera C, Milito P, Punturieri M, Asti E, Bonavina L. Serratus anterior plane block for hybrid transthoracic esophagectomy: a pilot study. J Pain Res. 2017;10:73–77. doi: 10.2147/JPR.S121441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mayes J, Davison E, Panahi P, et al. An anatomical evaluation of the serratus anterior plane block. Anaesthesia. 2016;71:1064–1069. doi: 10.1111/anae.13549 [DOI] [PubMed] [Google Scholar]
- 11.Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013;68:1107–1113. doi: 10.1111/anae.12344 [DOI] [PubMed] [Google Scholar]
- 12.Myles PS, Myles DB, Galagher W, et al. Measuring acute postoperative pain using the visual analog scale: the minimal clinically important difference and patient acceptable symptom state. Br J Anaesth. 2017;118:424–429. doi: 10.1093/bja/aew466 [DOI] [PubMed] [Google Scholar]
- 13.Vogt A, Stieger DS, Theurillat C, Curatolo M. Single-injection thoracic paravertebral block for postoperative pain treatment after thoracoscopic surgery. Br J Anaesth. 2005;95:816–821. doi: 10.1093/bja/aei250 [DOI] [PubMed] [Google Scholar]
- 14.Hill SE, Keller RA, Stafford-Smith M, et al. Efficacy of single-dose, multilevel paravertebral nerve blockade for analgesia after thoracoscopic procedures. Anesthesiology. 2006;104:1047–1053. doi: 10.1097/00000542-200605000-00022 [DOI] [PubMed] [Google Scholar]
- 15.Kotemane NC, Gopinath N, Vaja R. Analgesic techniques following thoracic surgery: a survey of United Kingdom practice. Eur J Anaesthesiol. 2010;27:897–899. doi: 10.1097/EJA.0b013e32833d1259 [DOI] [PubMed] [Google Scholar]
- 16.Shanthanna H, Moisuik P, O’Hare T, et al. Survey of postoperative regional analgesia for thoracoscopic surgeries in Canada. J Cardiothorac Vasc Anesth. 2018;32:1750–1755. doi: 10.1053/j.jvca.2018.01.003 [DOI] [PubMed] [Google Scholar]
- 17.Naja Z, Lonnqvist PA. Somatic paravertebral nerve blockade. Incidence of failed block and complications. Anaesthesia. 2001;56:1184–1188. [DOI] [PubMed] [Google Scholar]
- 18.Pace MM, Sharma B, Anderson-Dam J, Fleischmann K, Warren L, Stefanovich P. Ultrasound-guided thoracic paravertebral blockade: a retrospective study of the incidence of complications. Anesth Analg. 2016;122:1186–1191. doi: 10.1213/ANE.0000000000001117 [DOI] [PubMed] [Google Scholar]
- 19.Kelly ME, Mc Nicholas D, Killen J, Coyne J, Sweeney KJ, McDonnell J. Thoracic paravertebral blockade in breast surgery: is pneumothorax an appreciable concern? A review of over 1000 cases. Breast J. 2018;24:23–27. doi: 10.1111/tbj.12831 [DOI] [PubMed] [Google Scholar]
- 20.Okmen K, Okmen BM. The efficacy of serratus anterior plane block in analgesia for thoracotomy: a retrospective study. J Anesth. 2017;31:579–585. doi: 10.1007/s00540-017-2364-9 [DOI] [PubMed] [Google Scholar]
- 21.Kaya FN, Turker G, Mogol EB, Bayraktar S. Thoracic paravertebral block for video-assisted thoracoscopic surgery: single injection versus multiple injections. J Cardiothorac Vasc Anesth. 2012;26:90–94. doi: 10.1053/j.jvca.2011.09.008 [DOI] [PubMed] [Google Scholar]
- 22.Martin LW, Sarosiek BM, Harrison MA, et al. Implementing a thoracic enhanced recovery program: lessons learned in the first year. Ann Thorac Surg. 2018;105:1597–1604. doi: 10.1016/j.athoracsur.2018.01.080 [DOI] [PubMed] [Google Scholar]
- 23.Kim JA, Kim TH, Yang M, et al. Is intravenous patient controlled analgesia enough for pain control in patients who underwent thoracoscopy? J Korean Med Sci. 2009;24:930–935. doi: 10.3346/jkms.2009.24.5.930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Piracha MM, Thorp SL, Puttanniah V, Gulati A. “A tale of two planes”: deep Versus superficial serratus plane block for postmastectomy pain syndrome. Reg Anesth Pain Med. 2017;42:259–262. doi: 10.1097/AAP.0000000000000555 [DOI] [PubMed] [Google Scholar]
- 25.Bhoi D, Pushparajan HK, Talawar P, Kumar A, Baidya DK. Serratus anterior plane block for breast surgery in a morbidly obese patient. J Clin Anesth. 2016;33:500–501. doi: 10.1016/j.jclinane.2015.09.004 [DOI] [PubMed] [Google Scholar]
- 26.Lopez-Matamala B, Fajardo M, Estebanez-Montiel B, Blancas R, Alfaro P, Chana M. A new thoracic interfascial plane block as anesthesia for difficult weaning due to ribcage pain in critically ill patients. Medicina Intensiva. 2014;38:463–465. doi: 10.1016/j.medin.2013.10.005 [DOI] [PubMed] [Google Scholar]
- 27.Madabushi R, Tewari S, Gautam SK, Agarwal A, Agarwal A. Serratus anterior plane block: a new analgesic technique for post-thoracotomy pain. Pain Physician. 2015;18:E421–4. [PubMed] [Google Scholar]
- 28.Piraccini E, Pretto EA Jr., Corso RM, Gambale G. Analgesia for thoracic surgery: the role of paravertebral block. HSR Proc Intensive Care Cardiovasc Anesth. 2011;3:157–160. [PMC free article] [PubMed] [Google Scholar]
- 29.Chu GM, Jarvis GC. Serratus anterior plane block to address postthoracotomy and chest tube-related pain: a report on 3 cases. A A Case Rep. 2017;8:322–325. doi: 10.1213/XAA.0000000000000502 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.