Abstract
Background
Previous cross‐sectional studies have shown conflicting results regarding the effects of television viewing and occupational sitting on cardiovascular disease (CVD) risk factors. The purpose of this study was to compare the association of both television viewing and occupational sitting with CVD events and all‐cause mortality in blacks.
Methods and Results
Participants included 3592 individuals enrolled in the Jackson Heart Study, a community‐based study of blacks residing in Jackson, Mississippi. Television viewing (<2, 2–4, and >4 h/day) and occupational sitting (never/seldom, sometimes, often/always) were self‐reported. Over a median follow‐up of 8.4 years, there were 129 CVD events and 205 deaths. The highest category of television viewing (>4 h/day) was associated with a greater risk for a composite CVD events/all‐cause mortality end point compared with the lowest category (<2 h/day; hazard ratio, 1.49; 95% CI, 1.13–1.97). In contrast, the highest category of occupational sitting (often/always) was not associated with risk for a composite CVD events/all‐cause mortality end point compared with the lowest category (never/seldom; hazard ratio, 0.90; 95% CI, 0.69–1.18). Moderate‐to‐vigorous physical activity moderated the association of television viewing with CVD events/all‐cause mortality such that television viewing was not associated with greater risk among those with high moderate‐to‐vigorous physical activity levels.
Conclusions
Television viewing was associated with greater risk of CVD events and all‐cause mortality, while occupational sitting had no association with these outcomes. These findings suggest that minimizing television viewing may be more effective for reducing CVD and mortality risk in blacks compared with reducing occupational sedentary behavior.
Keywords: black, all‐cause mortality, cardiovascular disease, moderate‐to‐vigorous physical activity, occupational sedentary behavior, television viewing
Subject Categories: Cardiovascular Disease, Epidemiology, Lifestyle, Race and Ethnicity
Clinical Perspective
What Is New?
Television viewing, but not occupational sitting, was associated with an increased risk of cardiovascular disease and all‐cause mortality in blacks.
High levels of leisure‐time moderate‐to‐vigorous physical activity ameliorated the hazardous effects of television viewing in blacks.
What Are the Clinical Implications?
Minimalizing television viewing may be more effective in improving health outcomes, compared with reducing other sedentary behaviors, in blacks.
Participation in leisure‐time moderate‐to‐vigorous physical activity should be encouraged to offset hazardous outcomes attributable to high amounts of television viewing in blacks.
Introduction
An abundance of epidemiologic evidence has demonstrated that blacks are at greater risk of cardiovascular disease (CVD) and premature death relative to other race/ethnic groups in the United States.1, 2, 3 To combat the disproportionate CVD/mortality risk in blacks compared with whites, it is necessary to identify modifiable risk factors for directed behavioral interventions.4 Accumulating evidence has demonstrated that sedentary behavior is linked to several CVD risk factors, including metabolic syndrome, hypertension, and type 2 diabetes mellitus.5 Additionally, prospective studies have reported a significant association between sedentary behavior and incident CVD and all‐cause mortality, even when accounting for levels of moderate‐to‐vigorous physical activity (MVPA), suggesting that engagement in adequate levels of physical activity does not fully protect individuals from the deleterious effects of sedentary behavior.6, 7, 8, 9 Accordingly, sedentary behavior is now believed to represent a distinct health behavior that carries its own risk and is no longer considered as just the absence of physical activity.5
Emerging evidence indicates that certain types of sedentary behavior may lead to greater CVD risk than others, which has led some to speculate that “not all sedentary behavior is created equal.”10 Several studies have found that leisure‐time sedentary behavior, primarily television (TV) viewing, is more strongly associated with CVD risk factors (adiposity, C‐reactive protein, fibrinogen, blood lipids) compared with nonleisure forms of sedentary behavior (eg, occupational sedentary time), suggestive that TV viewing may be a more harmful form of sedentary behavior.11, 12, 13 These previous studies have been limited by their cross‐sectional rather than prospective design, and have rarely included diverse populations with high proportions of blacks. Furthermore, although population‐based studies have increasingly used accelerometers to objectively measure sedentary behavior to elucidate its role as a CVD risk factor, a limitation of accelerometry‐based studies is the difficulty in distinguishing between differing types of sedentary behavior. Epidemiologic evidence from prospective studies, therefore, is still needed to determine if the association of sedentary behavior with incident CVD and mortality varies by leisure versus nonleisure domains.
The purpose of this study was to determine the associations of TV viewing and occupational sitting with CVD events and all‐cause mortality in the large community‐based cohort of blacks enrolled in the JHS (Jackson Heart Study). As recent evidence suggests that the mortality risk conferred by prolonged sedentary behavior is dependent on one's physical activity levels, a secondary aim of the current study was to examine whether physical activity moderates the associations of TV viewing and occupational sitting with CVD events and all‐cause mortality.
Methods
Study Population
All data materials are publicly available14 and can be accessed pending completion and approval of a data use agreement. The JHS is a large, population‐based study of CVD among blacks. Details of study design, recruitment, and data collection have been previously described.15, 16, 17, 18 Briefly, the JHS enrolled 5306 black adults, aged ≥21 years, between 2000 and 2004. Participants included urban and rural residents from the Jackson, Mississippi, metropolitan tricounty region (Hinds, Madison, and Rankin counties) who were randomly contacted, volunteers, or family members. The baseline examination in 2000 to 2004 included an in‐home interview, conducted by trained black interviewers, and a clinical examination after an overnight fast. Information on sociodemographic characteristics, health behaviors, and medical history were collected during the in‐home interview. Follow‐up examinations were thereafter conducted from 2005 to 2008 (Exam 2) and 2009 to 2012 (Exam 3) to repeat collection of key variables. For the current analysis, only JHS participants who had data for TV viewing and occupational sitting time at the baseline examination were included (n=3592). The JHS was approved by the institutional review boards of participating institutions. All participants provided written informed consent.
Sedentary Behavior and Physical Activity Measures
Sedentary behavior and physical activity were assessed using the JHS Physical Activity Cohort Survey consisting of 30 questions assessing physical activity over the past 12 months. This is a modified version of the Baecke physical activity survey, with the goal of improving the measurement of physical activity in blacks.19, 20 Television viewing was assessed by the single item, “During the past year, how often did you watch television?” Response options included the following: “<1 hour a week”, “At least 1 hour a week, but <7 hours a week”; “At least 1 hour a day, but <2 hours a day”; “At least 2 hours a day, but <4 hours a day”; and “4 or more hours a day.” This item has been validated against accelerometry (ρ=0.22) and has good reproducibility (r=0.75–0.78).21, 22 Occupational sitting was assessed using the single item, “When you are at work, how often do you sit?” Response options included the following: “Never,” “Seldom,” “Sometimes,” “Often,” and “Always.” This item question has been validated against accelerometry (ρ=0.63) and also has good reproducibility (intraclass correlation coefficient, 0.74).23
Leisure‐time MVPA was assessed by a series of interviewer‐administered questions inquiring about the yearly frequency and weekly duration of participation in exercise and sports over the past year. Responses were converted to “minutes per week” for each sport or exercise reported and incorporated the number of months a participant partook in the sport or exercise (min/week=[60×h/week]×[months in past year/12 months]) as previously described.24 Each sport/exercise was assigned a metabolic equivalent of task value using the Compendium of Physical Activities.25 Levels of leisure‐time MVPA were estimated by summing the minutes per week of participation in sports or exercise with a metabolic equivalent of task value ≥3.5. Participation in MVPA was expressed as a categorical variable, according to the American Heart Association's Life's Simple 7 criteria for minutes per week of leisure‐time MVPA: poor physical activity (0 minutes of MVPA per week), intermediate physical activity (>0 and <150 min/week of MVPA and <75 min/week of leisure‐time vigorous physical activity), and ideal physical activity (≥75 min/week of vigorous physical activity or ≥150 min/week of MVPA).26
Covariates
Age, sex, education, income level, alcohol consumption, smoking status, a healthful diet (defined according to the American Heart Association's Life's Simple 7 criteria), body mass index (BMI), hypertension, diabetes mellitus, history of myocardial infarction, and history of stroke were included as covariates. A detailed description of these measures is provided in Data S1.
Outcome Variables
The primary outcome was a composite end point of CVD events (coronary heart disease or stroke) and all‐cause mortality. Adjudication procedures for these outcomes have been described previously.27 Briefly, living participants or their proxies were contacted annually via telephone to assess potential CVD events and vital status. Hospital discharge lists with specific diagnostic criteria were also obtained from the Jackson, Mississippi, tricounty area hospitals. Death certificates were requested from the Mississippi State Department of Health for JHS participants as needed. When a CVD‐related hospitalization or a death was identified, medical records were retrieved and abstracted. Trained clinicians adjudicated events following published guidelines using the information available about the circumstances surrounding an event.27 For the present analysis, definite or probable CVD events (ie, coronary heart disease, nonfatal myocardial infarction, or acute coronary heart disease death or stroke defined as noncarotid embolic or thrombotic brain infarction, brain hemorrhage, or subarachnoid hemorrhage), and all‐cause mortality were available through December 31, 2010. The composite of CVD events or all‐cause mortality was the primary outcome, and each type of event was analyzed separately as secondary outcomes.
Statistical Analysis
Baseline characteristics of the sample were calculated stratified by TV viewing time (with groups defined as <2 hours per day, 2–4 hours per day, or >4 hours per day), and separately, occupational sitting time (with groups defined as never or seldom, sometimes, or often or always). Categories for television viewing/occupational sitting were consistent with previous work.28 Cox proportional hazards regression models were used to estimate the hazard ratio for the composite end point (CVD events and all‐cause mortality pooled) associated with each sedentary behavior. Crude hazard ratios were initially calculated modeling TV viewing (2–4 hours per day and >4 hours per day) and occupational sitting (“sometimes” and “often or always”) as indicator variables, with TV viewing time <2 hours per day and occupational sitting “never or seldom” serving as the respective reference groups. Subsequently, hazard ratios were calculated after adjustment for age and sex (Model 1); further adjustment for education, alcohol drinking, smoking status, healthy diet, BMI, hypertension, diabetes mellitus, history of myocardial infarction, and history of stroke (Model 2); and additional adjustment for leisure‐time MVPA (Model 3) and occupational sitting (Model 4 for TV viewing analyses) or TV viewing (Model 4 for occupational sitting analyses). Tests for linear trends (eg, P‐trend tests) were conducted by including the TV viewing and, separately, occupational sitting categories as ordinal variables in the regression models. This provided a test of significance for the hypothesis that as the amount of TV viewing (or occupational sitting) increases, the risk of CVD/mortality tends to increase. In secondary analyses, CVD events and all‐cause mortality were analyzed as separate outcomes.
To examine whether the association of television viewing/occupational sitting with the composite end point was moderated by level of leisure‐time MVPA, we added multiplicative interaction terms of MVPA (ideal MVPA levels versus inactive/intermediate MVPA levels) with the sedentary behavior indicator variables to the fully adjusted regression models. To explore the potential for reverse causality (ie, those with high levels of disability and illness, who thus have a high risk of death, are more sedentary), we conducted a sensitivity analysis wherein all of the above analyses were repeated after the exclusion of deaths in the first year of follow‐up. To account for the possibility that changes in selected covariates over follow‐up confounded our results, we also conducted a sensitivity analysis treating smoking status (assessed at Exams 1 and 3), BMI (assessed at Exams 1, 2, and 3), and leisure‐time MVPA (assessed at Exams 1 and 3) as time‐varying covariates in the Cox regression models. Data analyses were conducted using SPSS version 22 (SPSS Inc, Chicago, IL).
Results
Participant Characteristics
Among the 3592 participants included in the current analysis, 1174 (32.7%), 1306 (36.3%), and 1112 (31.0%) watched TV <2, 2 to 4, and >4 h/day, respectively. Participants who reported longer daily TV viewing were more likely to have the following characteristics: poor levels of leisure‐time MVPA, an annual family income <$50 000, heavy alcohol consumption, current smoker, unhealthy diet, and hypertension. They were also less likely to have graduated high school and had a higher BMI (Table 1).
Table 1.
Characteristics of Jackson Heart Study Participants (n=3592) by Category of Television Viewing
| Variable | Television Viewing | P Trend | ||
|---|---|---|---|---|
| <2 h/day (n=1174) | 2–4 h/day (n=1306) | >4 h/day (n=1112) | ||
| Age, y | 51.0±11.3 | 51.1±11.2 | 51.7±12.1 | 0.287 |
| Male sex, % | 36.7 | 40.8 | 39.8 | 0.120 |
| Education < HS, % | 9.6 | 9.9 | 16.1 | <0.001 |
| Income <$50 000, % | 56.9 | 62.6 | 70.9 | <0.001 |
| Heavy alcohol consumption, %a | 3.2 | 3.5 | 5.9 | 0.001 |
| Current smoking, % | 10.4 | 11.5 | 18.2 | 0.001 |
| Healthful diet, %b | ||||
| Poor | 59.2 | 62.4 | 67.3 | <0.001 |
| Intermediate | 39.9 | 36.9 | 32.3 | |
| Ideal | 0.9 | 0.7 | 0.4 | |
| BMI, kg/m2 | 31.0±6.6 | 32.1±7.5 | 32.0±7.8 | <0.001 |
| Hypertension, %c | 45.0 | 48.6 | 50.5 | 0.008 |
| Diabetes mellitus, %d | 15.2 | 16.6 | 17.9 | 0.089 |
| History of MI, %e | 2.9 | 2.8 | 3.3 | 0.551 |
| History of stroke, % | 2.4 | 1.7 | 3.0 | 0.370 |
| Leisure‐time MVPA, %f | <0.001 | |||
| Poor | 39.2 | 42.3 | 49.6 | |
| Intermediate | 36.6 | 34.3 | 34.2 | |
| Ideal | 24.2 | 23.4 | 16.3 | |
Data presented as mean±standard deviation or percentage. BMI indicates body mass index; HS, high school; MI, myocardial infarction; MVPA, moderate or vigorous physical activity.
Defined as >14 drinks/week for men; >7 drinks/week for women.
Defined according to American Heart Association's Life's Simple 7 criteria for the following components: fruits and vegetables ≥4.5 cups/day, fish >3.5 ounces twice/week, sodium <1500 mg/day, sugary beverages <450 kcal/week, whole grains ≥3 servings/day. Poor diet: 0 to 1 components; intermediate diet: 2 to 3 components; and ideal diet: 4 to 5 components.
Defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or use of antihypertension medication.
Defined as a serum glucose ≥126 mg⁄dL for participants who had fasted ≥8 hours before their blood draw, a serum glucose ≥200 mg⁄dL for those who had not fasted, or a self‐report of a prior diagnosis of diabetes mellitus with use of insulin or oral hypoglycemic medications.
History of myocardial infarction was defined as a self‐reported history of healthcare provider–diagnosed myocardial infarction.
Defined according to American Heart Association's Life's Simple 7 criteria for minutes/week of moderate or vigorous physical activity. Poor physical activity: 0 minutes/week of leisure‐time moderate or vigorous physical activity. Intermediate physical activity: >0 and <150 minutes/week of leisure‐time moderate physical activity.
For occupational sitting, 1007 (28.0%), 1033 (28.8%), and 1552 (43.2%) participants reported sitting at work “never or seldom,” “sometimes,” or “often or always,” respectively. Participants who reported spending more time sitting at work were more likely to be female, be of a younger age, and have a higher BMI. Additionally, they were more likely to have the following characteristics: high levels of leisure‐time MVPA, a high school graduate, an annual family income >$50 000, and a healthy diet. Furthermore, they were less likely to be current smokers or heavy alcohol consumers (Table S1).
Sedentary Behavior and CVD/All‐Cause Mortality
Over a median follow‐up of 8.4 years (range 0.1–11.2 years), there were 129 CVD events and 205 deaths (334 total events). In an unadjusted model, >4 h/day TV viewing was associated with a greater risk of the composite CVD event/mortality end point (Table 2, upper panel). This association remained statistically significant in all adjusted models (Models 1–4 in Table 2; Figure 1). For occupational sitting, longer time spent sitting at work was associated with a decreased risk of the composite CVD event/mortality end point in an unadjusted model (Table 2, lower panel); however, this association was not statistically significant in any of the adjusted models (Models 1–4 in Table 2; Figure 2). The pattern of results for TV viewing and occupational sitting were similar when CVD event and all‐cause mortality were examined as separate outcomes, albeit the smaller number of CVD events limited our power to detect statistical significance (Tables S2 and S3; Figures S1 and S2).
Table 2.
Hazard Ratios for Pooled Outcomes (CVD Events and All‐Cause Mortality) Associated With Sedentary Behavior Domains in Jackson Heart Study Participants (n=3592)
| Sedentary Domain | No. of Events/No. at Risk | Hazard Ratio (95% CI) for Pooled Outcomes | ||||
|---|---|---|---|---|---|---|
| Unadjusted | Model 1 | Model 2 | Model 3 | Model 4 | ||
| TV viewing | ||||||
| <2 h/d | 87/1174 | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| 2–4 h/d | 104/1306 | 1.11 (0.83–1.49) | 1.08 (0.81–1.45) | 1.02 (0.76–1.37) | 1.02 (0.76–1.37) | 1.02 (0.76–1.36) |
| >4 h/d | 143/1112 | 1.80 (1.36–2.37) | 1.64 (1.25–2.17) | 1.50 (1.14–1.99) | 1.50 (1.14–1.98) | 1.49 (1.13–1.97) |
| P trend<0.001 | P trend<0.001 | P trend=0.003 | P trend=0.003 | P trend=0.003 | ||
| Occupational sitting | ||||||
| Never or seldom | 111/1007 | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Sometimes | 101/1033 | 0.91 (0.69–1.20) | 1.09 (0.82–1.44) | 1.06 (0.81–1.41) | 1.06 (0.80–1.40) | 1.06 (0.80–1.40) |
| Often or always | 122/1552 | 0.70 (0.54–0.91) | 0.89 (0.68–1.17) | 0.91 (0.69–1.19) | 0.91 (0.69–1.19) | 0.90 (0.69–1.18) |
| P trend=0.007 | P trend=0.380 | P trend=0.450 | P trend=0.459 | P trend=0.433 | ||
CVD indicates cardiovascular disease. Model 1: Adjusted for age and sex. Model 2: Adjusted for covariates in Model 1 plus education, heavy alcohol drinking, current smoking, healthful diet category, body mass index, hypertension, diabetes mellitus, history of myocardial infarction, and history of stroke. Model 3: Adjusted for covariates in Model 2 plus leisure‐time moderate or vigorous physical activity. Model 4: Adjusted for covariates in Model 3 plus occupational sitting (for television viewing analyses) or television viewing (for occupational sitting analyses).
Figure 1.
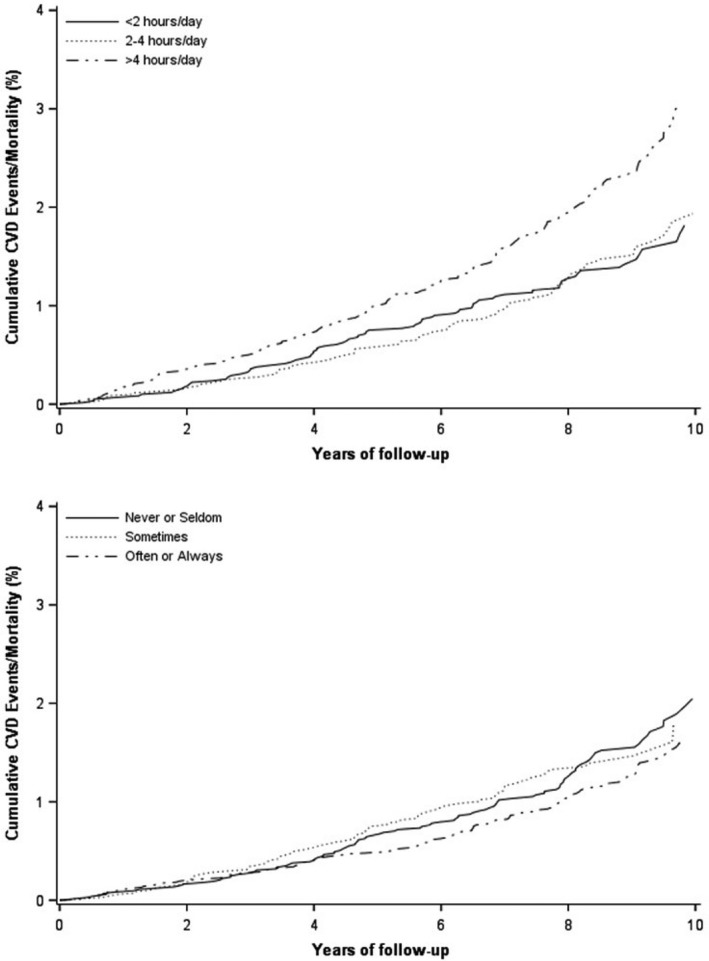
Adjusted cumulative CVD events/mortality by TV viewing (top) and occupational sitting (bottom) categories. Models adjusted for age, sex, education, heavy alcohol drinking, current smoking, healthful diet category, body mass index, hypertension, diabetes mellitus, history of myocardial infarction, history of stroke, leisure time moderate or vigorous physical activity, and occupational sitting (for television viewing analyses) or television viewing (for occupational sitting analyses). Cumulative CVD events/mortality=estimated failure function (1−S(t)) derived from Kaplan–Meier curves. CVD indicates cardiovascular disease.
Figure 2.
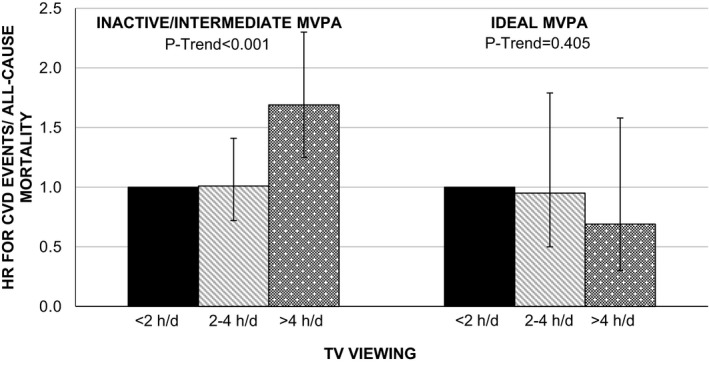
Hazard ratios for pooled outcomes (CVD events and all‐cause mortality) associated with TV viewing stratified by MVPA category (n=3592). Models adjusted for age, sex, education, heavy alcohol drinking, current smoking, healthful diet category, body mass index, hypertension, diabetes mellitus, history of myocardial infarction, history of stroke, and occupational sitting. Inactive/intermediate MVPA category defined as <150 minutes per week of moderate physical activity and <75 minutes per week of vigorous physical activity; ideal MVPA category defined as ≥150 minutes per week of moderate+vigorous physical activity. CVD indicates cardiovascular disease; HR, hazard ratio; MVPA, moderate‐to‐vigorous physical activity.
Moderating Effect of Leisure‐Time MVPA
Analyses revealed that MVPA levels moderated the association of TV viewing with the composite CVD event/mortality end point (P interaction=0.006). For participants who were inactive or had intermediate MVPA levels, TV viewing was significantly associated with an increased risk of the composite CVD event/mortality end point (Figure 2; Table S4). In contrast, for participants with ideal levels of MVPA, TV viewing was not significantly associated with risk of the composite CVD event/mortality end point. However, the association between occupational sitting and the composite end point did not vary by leisure‐time MVPA (P interaction>0.10).
Sensitivity Analyses
A sensitivity analysis was conducted to evaluate the potential for reverse causality by excluding deaths occurring in the first year of follow‐up. HRs calculated for TV viewing and occupational sitting were similar after the exclusion of early deaths (Table S5). All results were also similar when smoking status, BMI, and leisure‐time MVPA were treated as time‐varying covariates (data not shown).
Discussion
The present study was conducted to determine the associations of leisure and nonleisure types of sedentary behavior (TV viewing and occupational sitting) with CVD events and all‐cause mortality in a community‐based sample of black adults. Among blacks, watching >4 hours of TV was associated with a 50% greater risk of pooled CVD events and all‐cause mortality compared with viewing <2 hours of TV daily. In contrast, a greater amount of occupational sitting was not associated with the composite outcome. These results suggest that the association between sedentary behavior and risk of CVD/all‐cause mortality in blacks differs for leisure and nonleisure types of sedentary behavior. Our results furthermore revealed that high levels of MVPA (≥150 min/week) eliminated the increased risk of CVD events and all‐cause mortality associated with high TV viewing time, underscoring the benefits of physical activity for blacks.
Blacks have a greater risk for CVD morbidity/mortality at all ages and a lower life expectancy by ≈5 years compared with their white counterparts.1 Much of the racial disparity in CVD is associated with modifiable risk factors, such as physical inactivity and obesity, leading some to suggest that cardiovascular health equity will require the successful implementation of lifestyle risk reduction interventions in clinical practice.1, 29 However, the adoption of healthy lifestyle behaviors is far from optimal in blacks, as a constellation of social, environmental, and systems factors serve as barriers to the attainment of healthy lifestyle behaviors, including ideal physical activity levels and a healthy diet.30 In this regard, there is a need to identify alternative lifestyle factors that may be more easily modified to reduce the CVD burden in blacks. Our finding that a high amount of TV viewing was associated with the risk of CVD events/all‐cause mortality in JHS participants suggests that TV viewing could be one such modifiable factor. These findings are consistent with previous results from the Southern Community Cohort Study and the National Institutes of Health–AARP study, which reported that prolonged TV viewing was associated with an increased risk for all‐cause mortality among blacks.4, 31 As TV viewing is the most prevalent sedentary behavior in the United States, and given that blacks report watching 20% to 30% more TV than whites, targeting reductions in this type of sedentary behavior could be a potential strategy to reduce CVD risk burden among the high‐risk population of blacks.4, 32
Our finding that occupational sitting was not associated with CVD events/mortality in blacks adds to a growing body of literature that has previously reported a lack of association between occupational sitting and health risk. A systematic review revealed that of 43 identified studies, 20 reported no association between occupational sitting and health outcomes/conditions.33 Among 6 studies that prospectively examined the association of occupational sitting with CVD outcomes specifically, 4 reported increased relative risks for the most sedentary group at work compared with the most active group.34, 35, 36, 37 However, 2 of these 4 studies included overlapping data, and another reported data from the 1960s and 1970s, when the shift toward more sedentary occupations because of technological advancement was just beginning. In contrast, 2 of the 6 studies showed no differences in CVD risk among groups based on occupational sitting.38, 39
The discrepant findings between leisure‐based and occupational‐based sedentary behavior has been reported in several cross‐sectional studies. Among 7660 middle‐aged adults in the 1958 British Birth Cohort, higher levels of TV viewing, but not occupational sitting, had an adverse association with CVD biomarkers including C‐reactive protein and fibrinogen.10 Similarly, a Danish population‐based study of 2544 adults reported no associations between occupational sitting and cardiometabolic risk factors, while leisure‐time sitting was associated with cardiometabolic risk factors such as low‐density lipoprotein cholesterol, cardiorespiratory fitness, and adiposity measures.40 Recent analysis of the JHS determined that TV viewing, but not occupational sitting, was adversely associated with subclinical atherosclerosis.28 Our findings extend previous cross‐sectional evidence by providing prospective evidence that the risk conferred by sedentary behavior varies by leisure and nonleisure types of sedentary activities. Only 1 other study to our knowledge has prospectively examined the association of TV viewing and occupational sitting with health outcomes.41 Consistent with our data, that study's analysis of the Multiethnic Cohort Study found that TV viewing, but not occupational sitting, was associated with all‐cause mortality among 134 596 middle‐ and older‐aged adults.
Reasons for the discrepancy between TV viewing and occupational sitting are unclear. Participants who reported spending more time sitting at work had higher levels of leisure‐time MVPA, a healthier diet, and were less likely to be current smokers or heavy alcohol consumers. Conversely, participants who reported longer daily TV viewing were more likely to smoke, be heavy alcohol consumers, have an unhealthy diet, and poor levels of leisure‐time MVPA; suggestive that the link between TV viewing and poorer health habits could be a contributing factor.42, 43 Additionally, prolonged, uninterrupted periods of sedentary behavior (eg, sitting for hours at a time) may be more adversely associated with cardiometabolic biomarkers compared with shorter bouts of sedentary behavior.43 This suggests that the discrepant risk conferred by TV viewing and occupational sitting could also be partly attributed to differences in the pattern of sedentary time accumulation (sitting on a couch for hours at a time versus frequent breaks in sedentary time to go to the copier, visit coworkers, etc). Future studies examining patterns of sedentary behavior and sedentary breaks during both leisure and occupational time may be needed to elucidate the differential risks conferred by various types of sedentary behavior.
The current study is among the first to examine whether physical activity attenuates (or eliminates) the CVD/mortality risk conferred by sedentary behaviors among blacks, a population at heightened CVD risk. We observed a significant moderation effect of leisure‐time MVPA on the association between TV viewing and CVD events/mortality, suggesting that engagement in high levels of physical activity may ameliorate some of the adverse health effects of TV viewing in blacks. A recent meta‐analysis of over 1 million adults similarly reported that the increased mortality risk conferred by sitting was attenuated by higher levels of MVPA.44 However, it should be noted that attenuation of the increased risk of sedentary behavior on mortality by higher levels of MVPA was observed only for total sitting time. TV viewing was still associated with increased mortality risk even among the most physically active in this meta‐analysis. Further research is needed to determine the levels of physical activity needed to modify the deleterious health effects of TV viewing. Furthermore, as prolonged TV viewing is linked to adverse health characteristics (eg, JHS participants who reported >4 hours of TV viewing had a higher prevalence of hypertension and increased BMI), additional research is needed to elucidate whether the mitigation of risk by leisure‐time MVPA occurs though attenuation of these or other pathways.
The present study has several potential limitations. First, measurement of sedentary behavior was assessed by self‐report questionnaires, which are subject to measurement error and bias. However, unlike objective measures, questionnaires are able to differentiate among the various domains of sedentary behavior.45 Second, questions on TV viewing and occupational sitting had different response formats: for TV viewing, participants responded using predefined duration categories of hours/day or week (eg, 1–2 h/day); for occupational sitting, participants responded using predefined frequency categories (eg, “never,” “seldom”). Thus, the difference in measurement precision for assessing TV viewing and occupational sitting may have affected our findings. Third, there may be limited generalizability as the study was conducted in a single area in the Southeast United States, and the analytic sample was restricted to employed adults. Fourth, the CVD/mortality event rate was only ≈1.1% yearly in this all‐black sample. Because the present analyses were restricted to employed participants, we suspect that the analytic sample is younger and healthier and thus may have had fewer events than would be expected in the general black population. Finally, in sensitivity analyses, the observed association for TV viewing and CVD events alone (not pooling with all‐cause mortality) showed only a trend for statistical significance. The smaller number of CVD events likely limited our statistical power; nonetheless, the point estimates suggest that the risk incurred by TV viewing is consistent across CVD event and mortality outcomes. Notwithstanding these limitations, the JHS is one of the largest community‐based studies ever conducted among blacks. This landmark study provided a unique opportunity to characterize sedentary behavior in 2 separate domains and determine their associations with CVD events and all‐cause mortality. The present analyses represent some of the first prospective evidence that the risk conferred by sedentary behavior varies by leisure and nonleisure types of sedentary activities.
Implications
There are several implications that can be inferred from the current study. While it has been recommended that individuals limit the total time spent engaged in sedentary behaviors, it appears that, at least for blacks, minimizing TV viewing may be more effective for improving health outcomes compared with other sedentary behaviors. As many interventions have focused on workplace health behaviors, it is important to determine whether efforts to minimize sedentary behaviors should focus more on leisure‐time behaviors for improving health outcomes. Additionally, encouragement of leisure‐time physical activity may be especially important for blacks, as greater MVPA levels may ameliorate the hazardous effects of TV viewing. Our finding that that high levels of MVPA eliminated the increased risk of CVD events and all‐cause mortality associated with high TV viewing time importantly highlights that promoting leisure‐time MVPA should still remain a priority for health promotion among black populations.
Sources of Funding
The Jackson Heart Study is supported by contracts HHSN268201300046C, HHSN268201300047C, HHSN268201300048C, HHSN268201300049C, HHSN268201300050C from the National Heart, Lung, and Blood Institute and the National Institute on Minority Health and Health Disparities. This work was also supported by R01‐HL117323 and K24‐HL125704 from the National Heart, Lung, and Blood Institute/National Institutes of Health.
Disclosures
None.
Supporting information
Data S1. Supplemental methods.
Table S1. Characteristics of JHS Participants (n=3592) by Category of Occupational Sitting
Table S2. Hazard Ratios for CVD Events Associated With Sedentary Behavior Domains in Jackson Heart Study Participants
Table S3. Hazard Ratios for All‐Cause Mortality Associated With Sedentary Behavior Domains in Jackson Heart Study Participants
Figure S1. Adjusted cumulative CVD events by TV viewing (top) and occupational sitting (bottom) categories.
Figure S2. Adjusted cumulative mortality by TV viewing (top) and occupational sitting (bottom) categories.
Acknowledgments
This manuscript was reviewed by the JHS for scientific content and consistency of data interpretation with previous JHS publications. The authors thank the JHS participants, investigators, and staff for their valuable contributions and long‐term commitment to the study. The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; or the US Department of Health and Human Services.
(J Am Heart Assoc. 2019;8:e010406 DOI: 10.1161/JAHA.118.010406.)
References
- 1. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, De Ferranti S, Despres JP, Fullerton HJ, Howard VJ. Executive summary: heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133:447–454. [DOI] [PubMed] [Google Scholar]
- 2. Fuchs FD. Why do black Americans have higher prevalence of hypertension? An enigma still unsolved. Hypertension. 2011;57:379–380. [DOI] [PubMed] [Google Scholar]
- 3. Gorelick PB. Cerebrovascular disease in African Americans. Stroke. 1998;29:2656–2664. [DOI] [PubMed] [Google Scholar]
- 4. Matthews CE, Cohen SS, Fowke JH, Han X, Xiao Q, Buchowski MS, Hargreaves MK, Signorello LB, Blot WJ. Physical activity, sedentary behavior, and cause‐specific mortality in black and white adults in the Southern Community Cohort Study. Am J Epidemiol. 2014;180:394–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ford ES, Caspersen CJ. Sedentary behavior and cardiovascular disease: a review of prospective studies. Int J Epidemiol. 2012;41:1338–1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Diaz KM, Howard VJ, Hutto B, Colabianchi N, Vena JE, Safford MM, Blair SN, Hooker SP. Patterns of sedentary behavior and mortality in U.S. middle‐aged and older adults: a national cohort study. Ann Intern Med. 2017;167:465–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Winjidaele K, Brage S, Besson H, Khaw KT, Sharp SJ, Luben R, Wareham NJ, Ekelund U. Television viewing time independently predicts all‐cause and cardiovascular mortality: the EPIC Norfolk study. Int J Epidemiol. 2011;40:150–159. [DOI] [PubMed] [Google Scholar]
- 8. Patel AV, Berstein L, Deka A, Feigelson HS, Campbell PT, Gapstur SM, Colditz GA, Thun MJ. Leisure time spent sitting in relation to total mortality in a prospective cohort of US adults. Am J Epidemiol. 2010;172:419–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Warren TY, Vaughn B, Hooker S, Sui X, Church TS, Blair S. Sedentary behaviors increase risk of cardiovascular disease mortality in men. Med Sci Sports Exerc. 2010;42:879–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pinto Pereira SM, Ki M, Fower C. Sedentary behavior and biomarkers for cardiovascular disease and diabetes in mid‐life: the role of television‐viewing and sitting at work. PLoS One. 2012;7:e31132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Howard BJ, Balkau B, Thorp AA, Magliano DJ, Shaw JE, Owen N, Dunstan DW. Associations of overall sitting time and TV viewing time with fibrinogen and C reactive protein: the AusDiab study. Br J Sports Med. 2015;49:255–258. [DOI] [PubMed] [Google Scholar]
- 12. Wiseman AJ, Lynch BM, Cameron AJ, Dunstan DW. Associations of change in television viewing time with biomarkers of postmenopausal breast cancer risk. Cancer Causes Control. 2014;25:1309–1319. [DOI] [PubMed] [Google Scholar]
- 13. Dunstan DW, Howard B, Healy GN, Owen N. Too much sitting—a health hazard. Diabetes Res Clin Pract. 2012;97:368–376. [DOI] [PubMed] [Google Scholar]
- 14. Carpenter MA, Crow R, Stettes M, Rock W, Heilbraun J, Evans G, Jensen R, Sarpong D. Laboratory, reading center, and coordinating center data management methods in the Jackson Heart Study. Am J Med Sci. 2004;328:131–144. [DOI] [PubMed] [Google Scholar]
- 15. Fuqua SR, Wyatt SB, Andrew ME, Sarpong DR, Hendersson FR, Cunningham MK, Taylor HA. Recruiting African‐American research participation in the Jackson Heart Study: methods, response rates, and sample description. Ethn Dis. 2005;15:S6‐18–S6‐29. [PubMed] [Google Scholar]
- 16. Payne TJ, Wyatt SB, Mosley TH, Dubbert PM, Guiterrez‐Mohammed ML, Calvin RL, Taylor HA, Williams DR. Sociocultural methods in the Jackson Heart Study: conceptual and descriptive overview. Ethn Dis. 2005;15:S6‐38–S6‐48. [PubMed] [Google Scholar]
- 17. Taylor HA, Wilson JG, Jones DW, Sarpong DK, Srinivasan A, Garrison RJ, Nelson C, Wyatt SB. Toward resolution of cardiovascular health disparities in African Americans: design and methods of the Jackson Heart Study. Ethn Dis. 2005;15:S6‐4–S6‐17. [PubMed] [Google Scholar]
- 18. Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36:936–942. [DOI] [PubMed] [Google Scholar]
- 19. Dubbert PM, Carithers T, Ainsworth BE, Taylor HA Jr, Wilson G, Wyatt SB. Physical activity assessment methods in the Jackson Heart Study. Ethn Dis. 2005;15:S6‐56–S6‐61. [PubMed] [Google Scholar]
- 20. Clark BK, Healy GN, Winkler EA, Gardiner PA, Sugiyama T, Dunstan DW, Matthews CE, Owen N. Relationship of television time with accelerometer‐derived sedentary time: NHANES. Med Sci Sports Exerc. 2011;43:822–828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wareham NJ, Jakes RW, Rennie KL, Mitchell J, Hennings S, Day NE. Validity and repeatability of the EPIC–Norfolk Physical Activity Questionnaire. Int J Epidemiol. 2002;31:168–174. [DOI] [PubMed] [Google Scholar]
- 22. Wijndale K, De Bourdeaudhuij I, Godino JG, Lynch BM, Griffin SJ, Westgate K, Brage S. Reliability and validity of a domain‐specific last 7‐d sedentary time questionnaire. Med Sci Sports Exerc. 2014;46:1248–1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bell JA, Hamer M, Batty GD, Singh‐Manoux A, Sabia S, Kivimaki M. Combined effect of physical activity and leisure time sitting on long‐term risk of incident obesity and metabolic risk factor clustering. Diabetologia. 2014;57:2048–2056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ainsworth BE, Haskell WL, Hermann SD, Meckes N, Bassett DR Jr, Tudor‐Locke C, Greer JL, Vezina J, Whitt‐Glover MC, Leon AS. Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–1581. [DOI] [PubMed] [Google Scholar]
- 25. Lloyd‐Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. [DOI] [PubMed] [Google Scholar]
- 26. Keku E, Rosamind W, Taylor HA, Garrison R, Wyatt SR, Richard M, Jenkins B, Reeves K, Sarpong D. Cardiovascular disease event classification in the Jackson Heart Study: methods and procedures. Ethn Dis. 2005;15:S6‐62–S6‐70. [PubMed] [Google Scholar]
- 27. Diaz KM, Booth JN, Seals SR, Hooker SP, Sims M, Dubbert PM, Muntner P, Shimbo D. Sedentary behavior and subclinical atherosclerosis in African Americans: cross‐sectional analysis of the Jackson Heart Study. Int J Behav Nutr Phys Act. 2016;13:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Stuart‐Shor EM, Berra K, Kamou MW, Kumanyika S. Behavioral strategies for cardiovascular risk reduction in diverse and underserved racial/ethnic groups. Circulation. 2013;125:171–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Djousse L, Petrone AB, Blackshear C, Griswold M, Harman JL, Clark CR, Talegawkar S, Hickson DA, Gaziano JM, Dubbert PM, Correa A. Prevalence and changes over time of ideal cardiovascular health metrics among African‐Americans: the Jackson Heart Study. Prev Med. 2015;74:111–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Matthews CE, George SM, Moore SC, Bowles HR, Blair A, Park Y, Troiano RP, Hollenbeck A, Schatzkin A. Amount of time spent in sedentary behaviors and cause‐specific mortality in U.S. adults. Am J Clin Nutr. 2012;95:437–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bureau of Labor Statistics, US Department of Labor . American Time Use Survey: Table A1, 2011. Published June 22, 2012. Available at: http://www.bls.gov/tus/tables/a1_2011.pdf. Accessed December 21, 2018.
- 32. Van Uffelen JGZ, Wong J, Chau JY, van der Ploeg HP, Riphagen I, Gilson ND, Burton NW, Healy GN, Thorp AA, Clark BK, Gardiner PA. Occupational sitting and health risks: a systematic review. Am J Prev Med. 2010;39:379–388. [DOI] [PubMed] [Google Scholar]
- 33. Sjol A, Thomsen KK, Schroll M, Andersen LB. Secular trends in acute myocardial infarction in relation to physical activity in the general Danish population. Scand J Med Sci Sports. 2013;13:224–230. [DOI] [PubMed] [Google Scholar]
- 34. Hu G, Tuomilehto J, Borodulin K, Jousilahti P. The joint associations of occupational, commuting, and leisure‐time physical activity, and the Framingham risk score on the 10‐year risk of coronary heart disease. Eur Heart J. 2007;28:492–498. [DOI] [PubMed] [Google Scholar]
- 35. Hu G, Jousilahti P, Borodulin K, Barengo NC, Lakka TA, Nissinen A, Tuomilehto J. Occupational, commuting and leisure‐time physical activity in relation to coronary heart disease among middle‐aged Finnish men and women. Atherosclerosis. 2007;194:490–497. [DOI] [PubMed] [Google Scholar]
- 36. Hu G, Sarti C, Jousilahti P, Silventoinen K, Barengo NC, Tuomilehto J. Leisure time, occupational, and commuting physical activity and the risk of stroke. Stroke. 2005;36:1994–1999. [DOI] [PubMed] [Google Scholar]
- 37. Rosenman RH, Bawol RD, Oscherwitz M. A 4‐year prospective study of the relationship of different habitual vocational physical activity to risk and incidence of ischemic heart disease in volunteer male federal employees. Ann N Y Acad Sci. 1977;301:627–641. [DOI] [PubMed] [Google Scholar]
- 38. Johanssen S, Rosengren A, Tsipogianni A, Ulvenstam G, Wiklund I, Wilhelmsen L. Physical inactivity as a risk factor for primary and secondary coronary events in Goteborg, Sweden. Eur Heart J. 1988;9:8–19. [DOI] [PubMed] [Google Scholar]
- 39. Saidj M, Jorgensen T, Jacobsen RK, Linneberg A, Aadahl M. Differential cross‐sectional associations of work‐ and leisure‐time sitting, with cardiorespiratory and muscular fitness among working adults. Scand J Work Environ Health. 2014;40:531–538. [DOI] [PubMed] [Google Scholar]
- 40. Kim Y, Wilkens LR, Park S, Goodman MT, Monroe KR, Kolonel LN. Association between various sedentary behaviors and all‐cause cardiovascular disease and cancer mortality: the Multiethnic Cohort Study. Int J Epidemiol. 2013;42:1040–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ciccone J, Woodruff SJ, Fryer K, Campbell T, Cole M. Associations among evening snacking, screen time, weight status, and overall diet quality in young adolescents. Appl Physiol Nutr Metab. 2013;38:789–794. [DOI] [PubMed] [Google Scholar]
- 42. Vereecken CA, Todd J, Roberts C, Mulvihill C, Maes L. Television viewing behaviour and associations with food habits in different countries. Public Health Nutr. 2006;9:244–250. [DOI] [PubMed] [Google Scholar]
- 43. Dunstan DW, Thorp AA, Healy GN. Prolonged sitting: is it a distinct coronary heart disease risk factor? Curr Opin Cardiol. 2011;26:412–419. [DOI] [PubMed] [Google Scholar]
- 44. Ekelund U, Steene‐Johannessen J, Brown WJ, Fagerland MW, Owen N, Powell KE, Bauman A, Lee IM. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonized meta‐analysis of data from more than 1 million men and women. Lancet. 2016;388:1302–1310. [DOI] [PubMed] [Google Scholar]
- 45. Boone JE, Gordon‐Larsen P, Adair LS, Popkin BM. Screen time and physical activity during adolescence: longitudinal effects on obesity in young adulthood. Int J Behav Nutr Phys Act. 2007;4:26–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supplemental methods.
Table S1. Characteristics of JHS Participants (n=3592) by Category of Occupational Sitting
Table S2. Hazard Ratios for CVD Events Associated With Sedentary Behavior Domains in Jackson Heart Study Participants
Table S3. Hazard Ratios for All‐Cause Mortality Associated With Sedentary Behavior Domains in Jackson Heart Study Participants
Figure S1. Adjusted cumulative CVD events by TV viewing (top) and occupational sitting (bottom) categories.
Figure S2. Adjusted cumulative mortality by TV viewing (top) and occupational sitting (bottom) categories.


