Abstract
Background
The uptake of proven stroke treatments varies widely. We aimed to determine the association of evidence‐based processes of care for acute ischemic stroke (AIS) and clinical outcome of patients who participated in the HEADPOST (Head Positioning in Acute Stroke Trial), a multicenter cluster crossover trial of lying flat versus sitting up, head positioning in acute stroke.
Methods and Results
Use of 8 AIS processes of care were considered: reperfusion therapy in eligible patients; acute stroke unit care; antihypertensive, antiplatelet, statin, and anticoagulation for atrial fibrillation; dysphagia assessment; and physiotherapist review. Hierarchical, mixed, logistic regression models were performed to determine associations with good outcome (modified Rankin Scale scores 0–2) at 90 days, adjusted for patient and hospital variables. Among 9485 patients with AIS, implementation of all processes of care in eligible patients, or “defect‐free” care, was associated with improved outcome (odds ratio, 1.40; 95% CI, 1.18–1.65) and better survival (odds ratio, 2.23; 95% CI, 1.62–3.09). Defect‐free stroke care was also significantly associated with excellent outcome (modified Rankin Scale score 0–1) (odds ratio, 1.22; 95% CI, 1.04–1.43). No hospital characteristic was independently predictive of outcome. Only 1445 (15%) of eligible patients with AIS received all processes of care, with significant regional variations in overall and individual rates.
Conclusions
Use of evidence‐based care is associated with improved clinical outcome in AIS. Strategies are required to address regional variation in the use of proven AIS treatments.
Clinical Trial Registration
URL: https://www.clinicaltrials.gov. Unique Identifier: NCT02162017.
Keywords: acute stroke care, multilevel analysis, outcome, quality
Subject Categories: Ischemic Stroke, Cerebrovascular Disease/Stroke, Quality and Outcomes, Clinical Studies
Clinical Perspective
What Is New?
Adherence to evidence‐based care was associated with improved outcomes in patients with ischemic stroke who participated in the large pragmatic trial HEADPOST (Head Positioning in Acute Stroke Trial).
However, there was significant variation in the amount of evidence‐based care across regions, and few patients received the entire range (optimal treatment) of such performance indicators.
What Are the Clinical Implications?
There is considerable opportunity to increase the uptake of evidence‐based care in ischemic stroke to improve clinical outcomes from this serious condition.
Introduction
Stroke is a major cause of death and disability, especially in low‐resource regions.1 Although considerable advances have been made in generating the evidence base that supports various treatments, particularly for acute ischemic stroke (AIS), their implementation is often limited by resource, organizational, and funding barriers in clinical practice.2 For example, acute stroke unit (ASU) care is one of the most cost‐effective treatments,3, 4, 5 but many hospitals around the world do not have such a service or only have it organized in a partial manner.6 Improvements in the delivery of stroke care can translate into better patient outcomes, but most “real‐life” quality‐of‐care evaluations are undertaken in well‐resourced hospitals located in high‐income countries and without necessarily considering both organizational and patient variables.7, 8 A better understanding of variations in the processes of care in relation to patient outcomes can help prioritize efforts toward improving the implementation of evidence, especially in low‐ and middle‐income countries.9, 10
In a previous report, we identified large variations in the organization of stroke care (ie, staffing, protocols, and discharge planning) across hospitals in different countries in establishing the network for the international, multicenter HEADPOST (Head Positioning in Acute Stroke Trial).11 More research is needed on the impact of gaps in evidence‐based care in low‐ and middle‐income countries, where access to ASU care, let alone other therapies, is often limited.12 We aimed to determine the association between the use of recommended evidence‐based processes of stroke care and clinical outcomes for patients with AIS who participated in HEADPOST using analyses to account for hospital and patient characteristics.
Methods
The data that support the findings of this study are available through a formal protocol request from researchers to the Research Office of The George Institute Australia via the corresponding author.
Design
HEADPOST was an international, multicenter, cluster‐randomized, crossover trial with centralized outcome assessment, the details of which are outlined elsewhere.13, 14 In brief, the trial used a pragmatic design with broad eligibility and assessment criteria, to facilitate the recruitment of 11 093 adult patients with a clinical diagnosis of acute stroke (AIS or intracerebral hemorrhage) to determine the effectiveness of lying flat (0°) compared with sitting up (≥30°) head positioning, applied within the first 24 hours of admission at 114 hospitals in 9 countries, during 2016 to 2017. Patients were eligible for inclusion in the trial if they were aged ≥18 years, presented to the emergency department or an inpatient service at a participating center, and received a clinical diagnosis of acute stroke. Patients were excluded if the local clinician‐investigator considered that the assigned head position could not be maintained consistently, if the confirmed diagnosis was a transient ischemic attack, or if the patient declined to participate in the trial. Patients were also excluded if there was a clear indication for, or contraindication to, either of the head positions.13 Local investigators were required to recruit a prespecified target (cluster) number of consecutive patients into an initial randomized head position that was implemented as a usual standard‐of‐care policy before the service was crossed over for the other randomized head position to be implemented as a similar standard‐of‐care policy. The protocol was approved by all regulatory authorities and ethics committees at participating hospitals. A senior executive officer at each hospital acted as a “guardian” (as part of the cluster‐randomized trial design) and provided consent at an institutional level for head positioning to be implemented as a “low‐risk intervention” to clusters of patients as part of routine care; written informed consent was subsequently obtained from patients (or their approved surrogates) for the collection of medical data and participation in follow‐up assessments. The corresponding author has full access to all the data in the study and takes responsibility for their integrity and the data analysis.
To assist the implementation of the intervention at each site, data were gathered on the organization of the hospital and in the wards involved in implementing the randomized interventions. After a baseline assessment that included collecting demographic, medical history, and clinical information on the severity of the neurological deficit, according to the National Institutes of Health Stroke Scale and vital signs, adherence to the allocated head position was monitored in patients over the subsequent 24 hours. Further follow‐up data were collected on the management of patients at the time of separation (day 7 or at hospital discharge, transfer, or death, if earlier) and all serious adverse events, including death, until 90 days. Appropriately trained outcome assessors in a central office, who were kept blind to the management of patients, used a script to conduct a telephone assessment of health and physical functioning at 90 days. The key clinical outcome was the degree of disability, according to the modified Rankin Scale (mRS) score.15 Main study results showed that disability outcomes after acute stroke did not differ significantly between patients assigned to a lying‐flat position for 24 hours and patients assigned to a sitting‐up position with the head elevated to at least 30° for 24 hours.13
Statistical Analysis
Only patients with AIS were included in these analyses. Comparisons of categorical and continuous variables were assessed with the χ2 and Wilcoxon Mann‐Whitney rank sum tests, respectively. Univariable analyses were used to evaluate associations between patient characteristics and process‐of‐care indicators with 90‐day clinical outcomes. Multilevel logistic regression models were used to examine the associations between processes of care implemented in the first week (by day 7 or at discharge, if earlier) on good outcome (mRS score 0–2). The following processes of care were considered independent variables: (1) use of intravenous recombinant tPA (tissue‐type plasminogen activator) or endovascular clot retrieval in patients who presented at the hospital within 4.5 hours of symptom onset; (2) admission to an ASU; use of (3) antihypertensive, (4) antiplatelet, (5) statin, and (6) anticoagulation therapy in those with evidence of atrial fibrillation/flutter (AF); (7) receipt of a dysphagia screen and/or assessment before feeding was commenced; and (8) assessment by a physiotherapist in patients with residual disability (mRS score 3–5 on day 7). A composite variable of early “defect‐free” care (including the aforementioned 8 independent processes of care) was constructed to identify the proportion of eligible patients who received all applicable processes of care. A hierarchical mixed logistic regression with fixed period, fixed head position effect, random cluster, and random cluster‐period effects, plus the variable for evidence‐based care, was used as the base model. Three sequential models were constructed to adjust for other patient‐ and hospital‐level characteristic associations with patient outcomes. Variables were treated as independent variables. Association between defect‐free care and excellent outcome (90‐day mRS score 0–1) was also evaluated.
Consistency of treatment effect across prespecified subgroups (defined by age, sex, major country/region groupings, baseline National Institutes of Health Stroke Scale score, and pathologic subtype of AIS) was assessed by means of tests for interaction. Sensitivity analyses included the use of multiple imputation because >10% of observations for mRS scores were missing at 90 days16 and exclusion of those who had died within the first 7 days after admission.
To analyze the association between patients’ outcome and hospital characteristics, univariable analyses were performed using hierarchical mixed logistic regression models, as previously described, taking account of the cluster crossover study design. Multivariable analyses included adjustment for patient characteristics that had the potential to influence recovery: age, sex, history of hypertension, stroke, heart disease or diabetes mellitus, premorbid estimated mRS score, baseline National Institutes of Health Stroke Scale score, time from symptom onset to commencement of the intervention, and country. Adjustment variables were selected for potential clinical significance as well as statistical significance on initial univariable analyses. Data are reported with 2‐sided P values, without adjustment for multiple comparisons, and as odds ratios with 95% CIs. All analyses were undertaken with SAS software, version 9.3 (SAS Institute).
Role of the Funding Source
The study sponsor was not involved in the study design or collection, analysis, and interpretation of data; and had no role in the writing of this report or in the decision to submit the manuscript for publication.
Results
There were 9485 patients with AIS included in analyses (Figure 1). Table 1 shows that patients with AIS who received defect‐free stroke care had more risk factors, lower levels of premorbid disability, and greater baseline neurological impairment, compared with those who did not receive defect‐free stroke care. Defect‐free care was more frequent in hospitals in Australia and the United Kingdom, in those with lower numbers of stroke admissions per annum, in nonacademic hospitals, and in those where specific protocols for stroke care were in place and where multidisciplinary teams were involved in usual care.
Figure 1.
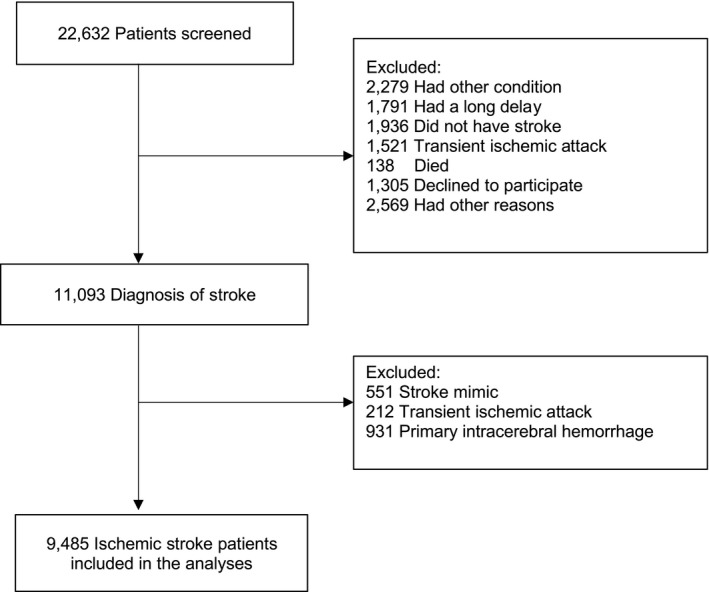
Patient flow diagram.
Table 1.
Characteristics of Ischemic Stroke Patients and Hospitals, Stratified by Receipt of “Defect‐Free” Evidence‐Based Care
| Variable | Defect‐Free Care | |||
|---|---|---|---|---|
| Total (N=9485) | Yes (N=1445) | No (N=8040) | P Valuea | |
| Patients | ||||
| Age, y | 69 (59–79) | 72 (63–81) | 68 (59–78) | 0.999 |
| Men | 5759 (60.7) | 826 (57.2) | 4933 (61.4) | 0.914 |
| Hypertension | 6141 (64.9) | 1154 (80.0) | 4987 (62.2) | <0.001 |
| Prior stroke | 2258 (23.9) | 280 (19.4) | 1978 (24.7) | 0.826 |
| Coronary artery disease | 1339 (14.2) | 250 (17.4) | 1089 (13.6) | 0.002 |
| Atrial fibrillation | 1059 (11.2) | 106 (7.4) | 953 (11.9) | <0.001 |
| Heart failure | 358 (3.8) | 57 (4.0) | 301 (3.8) | 0.184 |
| Diabetes mellitus | 2354 (24.9) | 451 (31.3) | 1903 (23.7) | <0.001 |
| Tobacco use | 1924 (20.5) | 241 (16.8) | 1683 (21.2) | 0.917 |
| Aspirin or other antiplatelet use | 5182 (54.7) | 677 (46.9) | 4505 (56.1) | <0.001 |
| Anticoagulant use | 824 (8.7) | 86 (6.0) | 738 (9.2) | <0.001 |
| Premorbid function on the mRS | ||||
| 0 (No symptoms) | 5800 (61.3) | 968 (67.1) | 4832 (60.2) | 0.012 |
| 1 (No significant disability) | 1691 (17.9) | 214 (14.8) | 1477 (18.4) | … |
| 2 (Slight disability) | 998 (10.5) | 125 (8.7) | 873 (10.9) | … |
| 3 (Moderate disability) | 598 (6.3) | 93 (6.4) | 505 (6.3) | … |
| 4 (Moderate/severe disability) | 306 (3.2) | 32 (2.2) | 274 (3.4) | … |
| 5 (Severe disability) | 76 (0.8) | 11 (0.8) | 65 (0.8) | … |
| Admission NIHSS score | 4 (2–8) | 4 (2–8) | 4 (2–8) | <0.001 |
| Symptom onset to intervention, h | 14 (5–37) | 16 (7–33) | 14 (5–39) | <0.001 |
| Initial head position lying flat | 4532 (47.8) | 685 (47.4) | 3847 (47.8) | 0.770 |
| Region of recruitment | ||||
| Australia/United Kingdom | 3850 (40.6) | 1001 (69.3) | 2849 (35.4) | <0.001 |
| China, including Taiwan | 4178 (44.0) | 171 (11.8) | 4007 (49.8) | … |
| India and Sri Lanka | 658 (6.9) | 151 (10.4) | 507 (6.3) | … |
| South America | 799 (8.4) | 122 (8.4) | 677 (8.4) | … |
| Hospitals | ||||
| No. of stroke patients annually | ||||
| <500 | 2252 (24.1) | 442 (30.6) | 1810 (22.9) | 0.010 |
| 500–1000 | 3642 (39.0) | 673 (46.6) | 2969 (37.6) | … |
| >1000 | 3446 (36.9) | 330 (22.8) | 3116 (39.5) | … |
| Academic teaching hospital | 8094 (86.5) | 1112 (77.0) | 6982 (88.3) | 0.007 |
| Pathway for stroke care | 8491 (90.8) | 1416 (98.0) | 7075 (89.5) | <0.001 |
| Protocols for fever/blood glucose/swallow | 7043 (75.3) | 1088 (75.3) | 5955 (75.3) | 0.899 |
| ED protocols | 8847 (94.6) | 1309 (90.6) | 7538 (95.3) | 0.256 |
| Multidisciplinary teams | 5561 (59.5) | 1170 (81.0) | 4391 (55.5) | <0.001 |
| Endovascular clot retrieval | 5305 (57.4) | 685 (48.8) | 4620 (58.9) | 0.042 |
Data are given as number (percentage) or median (interquartile range). ED indicates emergency department; mRS modified Rankin Scale; NIHSS, National Institutes of Health Stroke Scale.
P values from unadjusted hierarchical mixed logistic regression model, with link function being logit with fixed period, fixed head position effect, random cluster, and random cluster‐period effects.
Table 2 shows the results of multilevel modeling: use of antiplatelets, use of statins, dysphagia screen, and physiotherapy assessment were associated with better clinical outcome. The use of standard reperfusion treatment (recombinant tPA or endovascular clot retrieval within the first 4.5 hours of symptoms onset) was also associated with better disability‐free survival after adjusting for patient and hospital characteristics. Early implementation of all stroke care eligible processes of care was associated with greater likelihood of good clinical outcome (odds ratio, 1.40; 95% CI, 1.18–1.65). When the outcome considered was mRS score 0 to 1, the association between early implementation of defect‐free care and greater likelihood of excellent outcome (mRS score 0–1) remained significant (odds ratio, 1.22; 95% CI, 1.04–1.43). These results were further confirmed in sensitivity analyses with multiple imputations for missing primary outcome data (Table S1) by excluding patients with early death (Table 2), and after excluding patients who received reperfusion therapy and anticoagulation for AF (Table 2). In terms of survival at 90 days, multilevel modeling showed that use of all processes of care was associated with better survival (odds ratio, 2.23; 95% CI, 1.62–3.09) (Table S2).
Table 2.
Evidence‐Based AIS Processes of Care and Good Outcome, in Various Models
| Variable | Good Outcome | Total | Unadjusted | Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| (N=5112) | (N=8383) | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Reperfusion therapy (n=3093) | 591 (34.2) | 1051 (34.0) | 1.06 (0.91–1.25) | 0.454 | 0.87 (0.73–1.04) | 0.129 | 1.39 (1.13–1.71) | 0.002 | 1.40 (1.14–1.73) | 0.001 |
| ASU admission | 2633 (51.5) | 4723 (56.3) | 0.77 (0.65–0.91) | 0.003 | 1.01 (0.82–1.25) | 0.932 | 1.01 (0.81–1.25) | 0.940 | 1.05 (0.84–1.32) | 0.669 |
| Antihypertensive therapy | 2771 (54.2) | 4725 (56.4) | 0.89 (0.81–0.98) | 0.023 | 1.06 (0.96–1.18) | 0.255 | 1.08 (0.95–1.24) | 0.221 | 1.09 (0.95–1.24) | 0.208 |
| Antiplatelet therapy | 4975 (97.3) | 8063 (96.2) | 1.98 (1.56–2.50) | <0.001 | 1.91 (1.49–2.47) | <0.001 | 1.50 (1.12–2.00) | 0.007 | 1.52 (1.13–2.03) | 0.006 |
| Statin therapy | 4390 (85.9) | 6960 (83.0) | 1.64 (1.45–1.87) | <0.001 | 1.47 (1.28–1.69) | <0.001 | 1.27 (1.09–1.48) | 0.003 | 1.26 (1.08–1.47) | 0.004 |
| Anticoagulation in AF (n=1203)a | 259 (49.7) | 574 (47.7) | 1.14 (0.89–1.45) | 0.293 | … | … | … | … | ||
| Swallow assessment | 3916 (76.6) | 6279 (74.9) | 1.47 (1.30–1.67) | <0.001 | 1.38 (1.20–1.58) | <0.001 | 1.26 (1.09–1.46) | 0.002 | 1.26 (1.08–1.47) | 0.003 |
| Physiotherapy in disabled patients (n=3073) | 645 (72.5) | 2194 (71.4) | 1.20 (0.96–1.50) | 0.102 | 1.53 (1.17–1.99) | 0.002 | 1.50 (1.14–1.97) | 0.004 | 1.47 (1.11–1.95) | 0.008 |
| “Defect‐free” stroke care | 770 (15.1) | 1229 (14.7) | 1.45 (1.26–1.67) | <0.001 | 1.48 (1.27–1.71) | <0.001 | 1.40 (1.19–1.65) | <0.001 | 1.40 (1.18–1.65) | <0.001 |
| Defect‐free stroke care (without reperfusion/anticoagulation) | 1146 (22.4) | 1941 (23.2) | 1.21 (1.07–1.37) | 0.002 | 1.36 (1.19–1.56) | <0.001 | 1.28 (1.10–1.49) | 0.002 | 1.28 (1.10–1.49) | 0.002 |
| Defect‐free stroke care (only survivors >7 d) (n=8265) | 770 (15.1) | 1224 (14.8) | 1.39 (1.21–1.60) | <0.001 | 1.42 (1.22–1.65) | <0.001 | 1.38 (1.17–1.63) | <0.001 | 1.38 (1.16–1.63) | <0.001 |
Analyses used multilevel logistic regression models with fixed period, fixed head position effect, random cluster, and random cluster‐period effects. Model 1: adjusted for country, prestroke modified Rankin Scale score, age, and sex. Model 2: further adjustment for baseline National Institutes of Health Stroke Scale score; history of stroke, heart disease, diabetes mellitus, and hypertension; and time from stroke onset to intervention. Model 3: further adjustment for number of patients with stroke admitted annually, availability of a multidisciplinary team, hospital status (academic or not), use of pathway or service organization for stroke care, and availability of endovascular treatment. Good outcome indicates modified Rankin Scale score 0 to 2. AF indicates atrial fibrillation; AIS, acute ischemic stroke; ASU, acute stroke unit; OR, odds ratio.
Result models not shown because of failure to converge caused by low numbers.
Overall, use of the AIS processes of care was low (1445/9485, 15.2%) and varied widely across regions, being highest in Australia/United Kingdom (1001/3850, 26.0%) and India/Sri Lanka (151/658, 22.9%), intermediate in South America (122/691, 15.2%), and lowest in China (171/4178, 4.1%) (P<0.001) (Table S3). Those components with the greatest regional differences were ASU admission, use of antihypertensive therapy, anticoagulation for AF, and physiotherapy assessment. There was consistency in the beneficial associations across patient subgroups (Figures 2 and 3), but no hospital characteristic was independently predictive of clinical outcome (Table S4).
Figure 2.
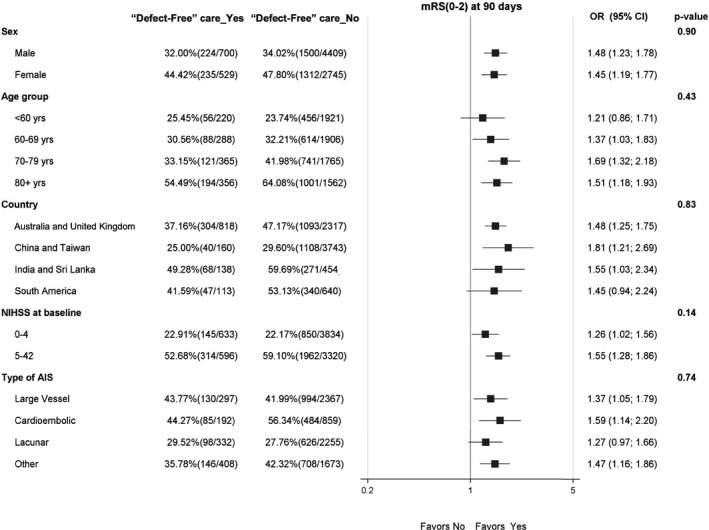
“Defect‐free” stroke care and good outcome (modified Rankin Scale [mRS] scores 0–2) at 90 days, by subgroups. AIS indicates acute ischemic stroke; NIHSS, National Institutes of Health Stroke Scale; OR, odds ratio.
Figure 3.
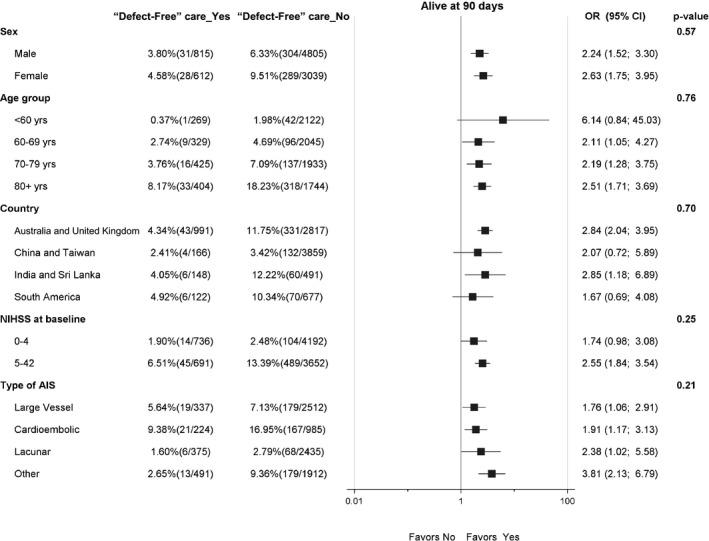
Impact in 90‐day mortality of “defect‐free” stroke care in different prespecified subgroups. AIS indicates acute ischemic stroke; NIHSS, National Institutes of Health Stroke Scale; OR, odds ratio.
Discussion
These secondary analyses of a large international clinical trial have 2 major findings. First, data show that the implementation of guideline‐recommended AIS processes of care is associated with clear beneficial clinical outcome, including a dramatic halving in the risk of death within 90 days, even after accounting for a range of confounding variables. Second, overall use of defect‐free stroke care was low, and there was considerable regional variation, especially across several components, including the use of ASU care. Although the organization of services is important for delivering efficient and effective stroke care, we were unable to identify a specific hospital characteristic that was independently associated with clinical outcome; patient‐level characteristics were the main driver of clinical outcome.
Various stroke quality assessment and improvement programs exist around the world. In the United States, for example, the Centers for Disease Control and Prevention monitors adherence to 10 quality‐of‐care measures in hospitals across 7 states through the Paul Coverdell National Acute Stroke Registry, where patients who received the best quality of care have been shown to have an increased chance of long‐term survival.8 Quality of care and process improvement have also been presented in numerous publications from the American Heart Association's Get With The Guidelines program.17 Similar initiatives have been developed in Australia and the United Kingdom,7, 18, 19 but there are few available in developing countries.20 In keeping with our findings of the cumulative benefit on outcomes from multiple processes of care, data from the Australian Stroke Clinical Registry have shown that patients who received 3 processes of care (stroke unit care, discharged on antihypertensive agents, and discharged with a care plan) had a 70% reduced hazard of death at 180 days.18
Within the various processes of care analyzed, reperfusion treatment and ASU care showed the greatest variations across the participating countries in our study, despite being recognized as those with the largest benefit. As a time‐critical treatment, use of intravenous thrombolysis is often restricted by local barriers, such as system networks and patient awareness of disease, resulting in early emergency consultation. For example, fewer patients receive recombinant tPA when arriving within 4 hours of symptom onset (39%),21 compared with those arriving within 2 hours (88%).22 Another consideration to be made is about stroke care performance and admission volume because our findings are opposed to the usual assumption that practice improves processes of care. This might have been related to overwhelming clinical volumes in larger hospitals, mostly from the Asian region.
We recognize that the definitions and timing of defect‐free stroke care treatments may vary,21, 22 as is the case for anticoagulation in those with AF and the initiation of antihypertensive treatment after AIS. Although current guidelines recommend initiation of anticoagulation within 2 weeks of a cardioembolic stroke, except for patients with large infarcts or other risk factors for hemorrhage,23 timing for treatment initiation after the onset of AIS presents high variability in practice. On the other hand, there is global consensus on the use of blood pressure–lowering treatment in patient candidates for acute reperfusion therapy and in patients not receiving reperfusion therapy but with severe hypertension.24 Early commencement of antihypertensive therapy in patients with milder hypertension is subjected to more debate, although it appears to be safe and reasonable to improve long‐term blood pressure control, unless contraindicated. Although we have shown that the initiation of anticoagulation and blood pressure lowering within 7 days was related to higher survival after AIS, there is the potential for this to reflect indication bias, whereby the treating clinician could have commenced the treatment earlier in those considered at low risk of complications and clinically stable.
Even after excluding the use of thrombolysis and thrombectomy, which can be more complex and dependent on specific time frames, and anticoagulation for AF, where early initiation is debatable, we have shown that defect‐free treatment was only applied in approximately one fifth of patients from this international cohort, revealing an alarming gap in guideline‐directed treatment. Direct comparison with other studies is limited by use of different criteria; however, an audit of UK hospitals revealed 46% of patients with AIS received good quality treatment in the first 72 hours.19 The latter considered different quality criteria, including brain scan; early evaluation by stroke consultant or associate specialist, nurse, and therapists; swallow evaluation; admission to stroke unit; antiplatelet use; and fluid/nutrition. When individual processes of care are compared, results are similar to our findings on swallow assessment, ASU, and antiplatelets use.19 In a recent report from INTERSTROKE (a case‐control study of the global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries), use of thrombolysis, antiplatelets, and statins was lower in comparison to our results, and higher for blood pressure lowering.12 Moreover, the authors showed that patients enrolled from hospitals in low‐ and middle‐income countries had poorer access to investigations, treatments, and services compared with those enrolled from hospitals in high‐income countries. In line with our results, these patients had worse clinical outcomes, which could only be partly explained by the inclusion of patients with more severe stroke. These findings highlight the importance of widespread implementation of stroke processes of care, particularly across low‐resource areas, where they are still scarce.
As stroke is a national priority in China, the central government has initiated a program of quality improvement strategies that include screening for high‐risk individuals in the community, process‐of‐care performance measures, and organizational development to improve stroke care.25 Multifaceted initiatives have been shown to improve adherence to performance measures in Chinese hospitals, but were not able to show significant change in the defect‐free stroke care.26 Accordingly, our data reemphasize the importance of quality improvement initiatives in China.
To our knowledge, this is the first study to assess the impact of using multiple evidence‐based stroke care processes on clinical outcomes in a large multinational cohort of patients. HEADPOST was a clinical trial with broad inclusion criteria, allowing the participation of a wide range of patients; and the analyses herein presented were strengthened by the use of multilevel modeling to account for patient‐ and hospital‐level variables. Inevitably, though, these secondary analyses of nonrandomized processes of care are limited by the potential for chance associations and residual confounding, as well as broad assumption of patient eligibility for different process of care. Interactions between different stroke care interventions were not explored, leading to possible risk of confounding by indication. Because the main study had 10% of missing primary outcome data in mRS score, the decision to use imputation for missing mRS scores is also to be acknowledged as a limitation of the study.
In summary, in this study, we have shown, among eligible patients with AIS, that those who received evidence‐based processes of care had better outcomes, but the overall uptake of the suite of therapies was low across a multinational population. Strategies to facilitate implementation of evidence‐based stroke care are needed, particularly in low‐resource regions.
Appendix
HEADPOST (Head Positioning in Acute Stroke Trial) Study Group and Trial Investigators
Steering Committee: Gillian Mead (Chair), Centre for Clinical Brain Sciences, University of Edinburgh, Edinburgh, United Kingdom; Maree Hackett (Principal Investigator), Craig S. Anderson (Co–Principal Investigator), and Laurent Billot, The George Institute for Global Health, Sydney, Australia; Pablo M. Lavados and Verónica V. Olavarría, Servicio de Neurología, Departamento de Neurología and Psiquiatría, Clínica Alemana de Santiago, Universidad del Desarrollo, Santiago, Chile; Sandy Middleton, St Vincent's Health Australia (Sydney) and Australian Catholic University, Sydney, Australia; Caroline L. Watkins, School of Health, Stroke Practice Research Unit, Lancashire Clinical Trials Unit, University of Central Lancashire, Preston, United Kingdom, and Australian Catholic University, Sydney, Australia; Thompson G. Robinson, Department of Cardiovascular Sciences, University of Leicester, British Heart Foundation Cardiovascular Research Centre, Leicester, United Kingdom; Hisatomi Arima (Co–Principal Investigator), Department of Preventive Medicine and Public Health, Faculty of Medicine, Fukuoka University, Fukuoka, Japan; H. Asita De Silva, Department of Pharmacology, Faculty of Medicine, University of Kelaniya, Colombo, Sri Lanka; Jeyaraj D. Pandian, Department of Neurology, Christian Medical College and Hospital, Ludhiana, India; Ruey‐Tay Lin, Department of Neurology, Kaohsiung Medical University and Hospital, Kaohsiung, Taiwan; Tsong‐Hai Lee, Department of Neurology, Linkou Chang Gung Memorial Hospital, Taipei, Taiwan; Liying Cui and Bin Peng, Peking Union Medical College Hospital, Beijing, China; and Octavio M. Pontes‐Neto, Ribeirao Preto School of Medicine University of São Paulo, Ribeirão Preto, Brazil.
Advisory Committee: Stephane Heritier, Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, Australia; Richard Lindley and Stephen Jan, The George Institute for Global Health, Sydney, Australia; Elizabeth Boaden, College of Health and Wellbeing, School of Health Sciences, University of Central Lancashire, Preston, United Kingdom; and Alejandro Brunser, Departamento de Neurología y Psiquiatría, Clínica Alemana de Santiago, Universidad del Desarrollo, Santiago, Chile.
Data Safety Monitoring Board: Robert Herbert (Chair), Neuroscience Research Australia, University of New South Wales, Sydney, Australia; Christopher P. L. H. Chen, Department of Pharmacology, National University of Singapore, Singapore; and Anne Forster, Bradford Institute for Health Research, Bradford Royal Infirmary, Leeds, United Kingdom.
Statisticians: Laurent Billot, Mark Woodward, Kris Rogers, and Anish Scaria, The George Institute for Global Health, Sydney, Australia.
International Coordinating Center, The George Institute for Global Health, Sydney, Australia: Project Management: Joyce Y. Lim (Project Manager), Natalie Espinosa, Lucy McEvoy, Lee Blackburn, Sarah S. Richtering, Shoujiang You, Simon Ladwig, Gabrielle P. Merritt, and Bryce Thomsen; Centralized Follow‐Up: Kerry Jenson, Penelope Gordon, Dennis Ryan Nguyen, Wei Wei Quan, Tessa Pei‐Yi Lo, Jonathan Lim, and Selena Goh; Data Management: Elizaveta Ivanova, Leibo Liu, Mirza Ahmad Baig, Ravider Singh, Paul Donnelly, and Manuela Armenis; Contracts and Quality Assurance: Marna Van Zyl, Helen Monaghan, Phillipa Smith, and Parisa Glass.
Regional Coordinating Centers: China (The George Institute China Incorporating George Clinical): Fanli Zhou, Yun Shen, Li Lei, Di Li, Ting Zhang; Centralized Follow‐Up: Lili Song, Xiaoyan Zhang, Yun Peng, Lingling Feng, Zhiping Ye, and Philip Gregory. India (Christian Medical College‐Ludhiana): Jeyaraj D. Pandain, and Deepti Arora. South America (Clinica Alemana de Santiago, Universidad del Desarrollo): Pablo M. Lavados, Paula Munoz‐Venturelli, Francisca Gonzalez, Bernardita Portales, Octavio Pontes‐Neto, Taiza Santos‐Pontelli, Brunna Rimoli, and Monica Braga; Centralized Follow‐Up: Lorena Hoffmeister, Carolina Vidal, Dafna Benadof, Rodrigo J. Rivas, Laura Carvallo, Pamela Carvallo, Rubia Miranda, and Brunna Pileggi. Sri Lanka (RemediumOne Pvt Ltd): H. Asita de Silva, Shalomi Weerawardena, Thanushanthan Jeevarajah, Devaki Dharmawardena, Dumindi Ranasinghe, and Matheesha Dharshana; Centralized Follow‐Up: M. M. M. Shafras, Nilesh Nandadeva, and Savithri Nawarathna. Taiwan (Kaohsiung Medical University Chung‐Ho Memorial Hospital): Ruey‐Tay Lin, Tsong‐Hai Lee, Jiu‐Haw Yin, Shoou‐Jeng Yeh, and Ruei‐Jen Ma. United Kingdom (Lancashire Clinical Trials Unit, University of Central Lancashire): Caroline L. Watkins, Gemma Whiteley, Denise Forshaw, Catherine Elizabeth Lightbody, Joanna Cox, Jane Fitzgerald, John F. Heney, Helen Byfield, Simone Finley, and Hayley E. Tyrer; Centralized Follow‐Up: Carole Bruce and Alison Gibbon.
Principal Investigators and Coordinators (according to country and center, with numbers of patients in parentheses): Australia (7 hospitals and 602 patients): Calvary Public Hospital Bruce (179): Brett Jones, Emma Siracusa, Koushik Gowda, Shahla Cowans, Briana Forman, Sherin Jacob, Kristine Caprecho, Roshan Khatri, Po Yi Wan, Maria Lopez, Sifiso Vanika, Wilhelmina Bleeker, and Marinka Ireland; Royal North Shore Hospital (121): Sheila Jala, Susan Day, Eric Ha, Martin Krause, Melissa Passer, and Sarah Giaccari; Royal Prince Alfred Hospital (133): Nadia Burkolter, Michael Braithwaite, and Kylie Tastula; Concord Repatriation General Hospital (95): Fiona Stanley Hospital (39): Darshan Ghia, Tapuwa Musuka, Anthony Alvaro, Gillian Edmonds, and Nicole O'Loughin, Rebecca Phair, and Joanne Kaoutal; Sir Charles Gairdner Hospital (20): David J. Blacker and Belinda L Saint; Port Macquarie Base Hospital (15): Kim Parrey, Michelle Coad, Matthew Kinchington, Nishantha Senanayake, Johanna Alaban, and Irma Kuehne. Brazil (4 hospitals and 264 patients): Hospital das Clinicas da Faculdade de Medicina de Ribeirao Preto, Universidade de Sao Paulo (147): Taiza Santos‐Pontelli, Monica Braga, Brunna Rimoli, Millene Camilo, and Milena Libardi; Clinicas de Porta Alegre (52): Sheila Martins, Batista Carlos, Magda Martins, Leonardo Carbonera, Andrea Almeida, and Martin Kelin; Hospital Governador Celso Ramos (33): Gladys Martins, Carla Pauli, Mariana Lunardi, Luciane Silveira, Olga Chagas, and Daily Souza; Hospital de Faculdade de Medicina de Botucatu, UNESP (São Paulo State University) (32): Rodrigo Bazan, Gabriel Braga, Priscila Ribeiro, Gustavo Luvizutto, Marcia Polin, and Fernanda Winckler. China (39 hospitals and 4479 patients): Yangquan Coalmine Group General Hospital (155): Jinfeng Liu, Zhenjiang Wang, Huibing Wang, Suying Lin, and Jing Dong; Nanjing First Hospital, Nanjing Medical University (150): Junshan Zhou, Suping Qin, and Hui Zhan; Dunhua City Hospital (144): Yongquan Xue, Dong Tian, Dan Yang, Yan Yin, and He Li; 85 Hospital of People's Liberation Army (142): Changming Geng, Jieyi Liu, Xiaolin Jiang, and Yujun Wu; Third People's Hospital of Dalian (142): Wei Sun; Zhucheng Traditional Chinese Medicine Hospital (141): Bingqi Yu, Yanmei Guan, Qin Wang, Bo Wei, Huirong Wang, and Yan Wang; Hospital of Hebei Medical University (141): Liwen Tai and Wenchao Zhang; Affiliated Hospital of Chifeng University (141): Weili Zhao, Xueying Wang, Guoli Li, Zhiming Ni, Fudong Guo, Lan Cen, Jun Lu, Zheng Chen, Guoming Yin, Yingchun Wang, Jiping Zheng, Zhimin Zhou, and Hongquan Wang; The Third Hospital of Wafangdian (140): Renlin Zou, Bin Xue, Airu Li, Jing Guo, Ying Guo, and Xingguo Jiang; Beijing Pinggu Hospital (140): Xiuge Tan and Chunpeng Zhang; The First Affiliated Hospital of Wenzhou Medical University (140): Bei Shao and Xiaoting Niu; The Second Affiliated Hospital of Soochow University (140): Chunfeng Liu, Dongqin Chen, Ping Liang, Xia Zhang, Chunqing Zhang, Wenjie Gong, Zhichao Huang, Huihui Liu, Shoujiang You, Junying Huang, and Rongfang Shi; Qilu Hospital of Shandong University (140): Cuilan Wang and Ying Liu; Yutian County Hospital (138): Jinchao Wang, Guojun Wu, and Zhihong Gao; The Yongjia County People's Hospital (138): Qunli Lin, Cong Xu, Huile Zheng, Xinghai Ye, and Xiaoqiong Jin; The Third Hospital of Hebei Medical University (133): Junyan Liu, Xiaoyun Cao, Yan Zhang, Jinyang Wang, Yuzhu Xu, and Yan Li; Xuanwu Hospital Capital Medical University (132): Xin Ma and Qi Kong; Affiliated Hospital of Jining Medical University (131): Yanlei Hao, Baojun Qiao, and Hui Yan; The Third People's Hospital of Huizhou (126): Zhiyong Huang, Baoqiang Chang, Jinjin Yan, Pinjun Liao, and Wei Zhang; The People's Hospital of Nanpi County (124): Ling Liu, Tingting Zhu, Xuehui Liu, and Yongping Li; The Second Cangzhou Central Hospital (121): Ruifang Dong; Hospital Affiliated to Shanghai Jiao Tong University School of Medicine (121): Miao Chen, Xiaoli Ge, Hairong Wang, Lihua Dai, and Jiafu Liu; Baogang Hospital (120): Shixia Wang, Jihui Du, and Aixiu Song; Hospital Central South University (120): Yunhai Li, Jie Feng, and Cheng Yu; The First Affiliated Hospital of Harbin Medical University (117): Honglin Feng, Xiaojia Sun, Ruihong Sun, Weisong Liu, and Jianfeng Liu; People's Hospital of Hejian City (117): Tong Ren Hospital Shanghai Jiao Tong University School (117): Xuesheng Lu and Enzhuo Chen; Peking University Shougang Hospital (112): Wei Gao, Hui Liu, and Heping Wang, Yanxia Wang, Juan Song, Dongqi Liu, Wenhui Du, Guixia Li, and Cuiling Li; The Third Affiliated Hospital of Guangzhou Medical University (109): Yanling Liang and Xuekun Cai; The Chinese PLA (People's Liberation Army) No. 263 Hospital (104): Jinli Zhang and Xiaowei Tao; Qinhuangdao Harbour Hospital (103): Pingshun An, Ranran Tang, Xu Qin, Yingling Wang, and Wenjun Zhang; Dongguan People's Hospital (101): Rong Ma, Xiaoqiong Huang, Yonglin Liu, and Yazhi Wang; The Second Hospital of Nanchang (97): Ping Fan and Hailan Yang; Bethune International Peace Hospital (85): Lianyuan Feng and Jianxia Zhi; XiangYa Xin Hua Henan Provincial People's Hospital (49): Jiewen Zhang and Yao Zhou; Shanghai Ninth People's Hospital, Shanghai Jiao Tong University School of Medicine (46): Danhong Wu and Haiyan He; The People's Hospital of Liaoning Province (42): Xiaohong Chen; Shijiazhuang Central Hospital (19): Yongge Hou and Xiaohui Su; Peking Union Medical College Hospital (1): Liying Cui, Bin Peng, and Siyuan Fan. Chile (7 hospitals and 608 patients): Hospital Base San José de Osorno (142): Luis Suárez, Juan de Dios Polanco, Patricio Sotomayor, Ricardo Urzúa, Daniela Urrutia, and Nathalie Conejan; Hospital de Iquique Dr Ernesto Torres Galdames (139): Arturo Escobar, Monica Gonzalez, Danisa Vargas, Angel Constante, Erika Vásquez, and Elizabeth Godoy; Complejo Asistencial Dr Victor Ríos Ruíz de Los Angeles (114): Christian Figueroa, Vanesa San Martin, Nataly Vidal, and Madeleyn Muñoz; Clínica Alemana de Santiago (71): Alejandro Brunser, María Spencer, Juan Almeida, and Ignacio Acosta; Hospital Santiago Oriente Dr Luis Tisné Brousse (64): Rodrigo Guerrero, Prudencio Lozano, Camila Aguayo, and Jimena Pizarro; Hospital Regional Temuco Doctor Hernán Henríquez Aravena (64): Alvaro Soto, Flor Bonilla, Pía García, Carolina Del Castillo, Marcela Grandjean, and Alexis Von Johnn; Hospital de Maipu El Carmen Dr Luis Valentin Ferrada (14): Ignacio Gutierrez, Francisca Rivero, and Ignacio López. Colombia (1 hospital and 38 patients): Fundación Cardiovascular de Colombia, Bucaramanga (38): Federico Silva, Marlen Pachón, José Mendoza, and Alexander Pabón. India (6 hospitals and 499 patients): Christian Medical College and Hospital, Ludhiana (147): Mahesh Kate, Naushad Akhtar, Gibbsdeep S. Narang, and Ashish Deepak; Mazumdar Shaw Medical Centre, a unit of Narayana Hrudayalaya Ltd, Bangalore (113): Vikram Huded, Romnesh De Sowza, Alben Sigamani, Karthikeyan Rajendran, Anisha Vishwanath and Anusha K; Dr Ramesh Cardiac and Multispeciality Hospital Pvt Ltd, Guntur (71): Somasundaram Kumaravelu, Syed Rahamath, and Sandeep Kannneganti; Post Graduate Institute of Medical Education and Research, Chandigarh (64): Dheeraj Khurana, Cheena Katoch, and Taranpreet Kaur; Baby Memorial Hospital Limited, Calicut (60): Ummer Karadan, Anu Kuriakose, Jaison John, and Mumthaz Basheer; Sree Chitra Tirunal Institute for Medical Sciences and Technology, Thiruvananthapuram (44): Sylaja Padmavathy N and Sapna Erat Sreedharan. Sri Lanka (4 hospitals and 271 patients): Sri Jayawardenepura General Hospital (100): Harsha Hemal Gunasekara, Gamlath Chandima Udeni De Silva, Peetagam Harshi Lakmali Ubeywickrama, Kavisha Chathumali Silva, and Eshani Anuradha De Silva; Colombo North Teaching Hospital (92): Udaya Ranawaka, Chamila Mettananda, Yamuna Nanayakkara, Tharini Mendis, Gayathri Fernando, Ahamed Imthikab, and Kandula Pieris; Colombo South Teaching Hospital (2 sites and 79 patients): Saman B. Gunatilake, Pamuditha M. W. Madanayake, Shiran A. Paranavitane, Bimsara Senanayake, Vaidhehi Vishwanathan, Maathury Sivapalan, Ruwangi U. Murage, and Uthpala Chandradeva. Taiwan (5 hospitals and 173 patients): Kaohsiung Medical University Chung‐Ho Memorial Hospital (33): Ruey‐Tay Lin, Yao‐Hua Liu, Chih‐Lung Lin, Hsiu‐Fen Lin, Kuan‐Ting Liu, Chien‐Fu Chen, Meng‐Ni Wu, Su‐Hua Tsai, Chi‐Ching Chen, and Lan‐Yi Chen; Linkou Chang Gung Memorial Hospital (94): Tsong‐Hai Lee, Chien‐Hung Chang, Yeu‐Jhy Chang, Kuo‐Lun Huang, Ting‐Yu Chang, Chi‐Hung Liu, Chen‐June Seak, Yu‐Li Lin, Jia‐Yi Luo, Hsiao‐Ying Yang, and Ching‐Yi Wang; Taipei Medical University Shuang Ho Hospital (20): Lung Chan, Chaur‐Jong Hu, Nai‐Fang Chi, Dean Wu, Yao‐Hsien Huang, Yi‐Chun Kuan, Chien‐Tai Hong, and Yi‐Chun Chen; En Chu Kong Hospital (18): Yu Sun, Cheng‐Huai Lin, Chien‐Jung Lu, Hai‐Jui Chu, Yi‐Chia Lo, Wen‐Hui Chang, and Wan‐Jung Lin; National Cheng Kung University Hospital (8): Hui‐Chen Su, Tien‐Yu Lin, Chi‐Hsuan Cho, Shu‐Lan Lu, Ya‐Fang Hsueh, and Ching‐Yi Lai. United Kingdom (41 hospitals and 4160 patients): Queen Alexandra Hospital, Portsmouth, Portsmouth Hospitals NHS (National Health Service) Trust (199): David Jarrett, Claire James, Stacey Valentine, Clare Whistler, and Rebecca Butler; University College London Hospitals NHS Foundation Trust (146): Simone Browning, Caroline Watchurst, Renuka Erande, Emma Elliott, Krishna Patel, Maria Brezitski, Caroline Hogan, Asra Banaras, Lucinda Crook, Rashidat Ahmed, Lindsay Potter, and Rosie Laird; St George's University Hospitals NHS (National Health Service) Foundation Trust (145): Natasha Clarke, Alison Loosemore, J. Godber, Sara Gawned, and K. A. Hamilton; Queen Elizabeth Hospital Birmingham, University Hospitals Birmingham NHS Foundation Trust (144): Rachael Jones; Southend University Hospital NHS Foundation Trust (143): Paul Guyler, Sharon Tysoe, Raji Prabakaran, Sweni Shah, and Joanne Calver; King's College Hospital (142): Laszlo K. Sztriha, Maria Fitzpatrick, Stephanie Drysdale, John Aeron‐Thomas, Emma McKenzie, and Belinda Chitando; York Teaching Hospitals NHS Foundation Trust (141): Paul Willcoxson, Elizabeth Iveson, Peter Wanklyn, Natasha Dyer, Michael Keeling, Romina Rodriguez, Kerry Elliott, Mia Porteous, and Mark O'Neill; Nottingham University Hospitals NHS Trust (141): Sheridan Orme, Carla Richardson, Janet Tomlinson, Suzanne Hawkins, and Delia Bester; Blackpool Teaching Hospitals NHS Foundation Trust (140): Carol Jeffs and Joanne Howard; Gloucestershire Royal Hospital, Gloucestershire Hospitals NHS Foundation Trust (140): Pauline Brown, Deborah Ward, Jennifer Turfrey, Leanne Raybould, Allison Bates, Sue O'Connell, Margaret O'Connor, and Samantha Williams; Teaching Hospitals NHS Foundation Trust (140): Hedley C. A. Emsley, Alison McLoughlin, Sonia Raj, Bindu Gregary, and Donna Doyle; Royal Cornwall Hospitals NHS Trust (140): G. M. Courtauld, C. Schofield, L. Lucas, A. Lydon, and A. James; The Royal London Hospital, Barts Health NHS Trust (139): Kari Saastamoinen, Laura Howaniec, and Premchand Daboo; Sheffield Teaching Hospitals NHS Foundation Trust (138): Ali N. Ali, Emma Richards, Joanne Howe, Christine Kamara, Kathy Stocks, and Ralf Lindert; Addenbrooke's Hospital, Cambridge University Hospitals NHS Foundation Trust (134): Diana J. Day, Sarah Finlay, Joanne McGee, Jennifer Mitchell, Elaine Amis, and Rosemary Macey; Royal Victoria Hospital, Belfast Health and Social Care Trust (132): Suzanne Tauro, Lauren Henry, Sarah Cuddy, Andrew Steele, Kerry Mullen, Sarah Kirker, and Murudappa Bhattad; Pinderfields General Hospital, Mid Yorkshire Hospitals NHS Trust (130): Michael Carpenter, Prabal Datta, Ann Needle, Linda Jackson, Julie Ball, and Rosie Beckitt; Royal Devon and Exeter NHS Foundation Trust (126): Nicola Chivers, Angela Bowring, Sara Eddy, Kevin Thorpe, Samantha Keenan, and Alison Griffin; Bradford Teaching Hospitals NHS Foundation Trust (108): Stuart Maguire, Chris Patterson, Hawraman Ramadan, Ruth Bellfield, Michaela Hooley, and Kelvin Stewart; Great Western Hospitals NHS Foundation Trust (97): Lucy Williams, Cara Gurney, Deborah Oliver, Maria Gardiner, and Sarah Grayland; Watford General Hospital (92): Mohit Bhandari, David M. Collas, Tolu Adesina, Saul Sundayi, Ruth Harvey, Emma Pope, Audrey Lam, Elaine Walker, and Colin Merrill; Imperial College Healthcare NHS Trust (91): Soma Banerjee, Kirsten Hannah Harvey, Sheila Mashate, and Peter Wilding; Lancashire Fairfield General Hospital, The Pennine Acute Hospitals NHS Trust (88): Linda Johnson, Robert Namushi, and Patricia Jacob; Queen's Hospital, Barking, Havering and Redbridge University Hospitals NHS Trust (87): Sreeman Andole, Karen Dunne, Naveen Gadapa, Sam King, Rabiya, Patel, and Sonata Siliuzaite; Whiston Hospital, St Helens and Knowsley Teaching Hospitals NHS Trust (87): Sharon Dealing and Karen Attwood; Medway NHS Foundation Trust (82): Samuel Sanmuganathan, Annette Woods, Banher Sandhu, Maam Mamun, Afzal Mahmood, June Jones, Abimbola Ojo, and Denise Carter‐Evans; Royal Liverpool and Broadgreen University NHS Trust (82): Paul Fitzsimmons, Aravind Manoj, Glyn Fletcher, and Paula Lopez; Calderdale and Huddersfield NHS Foundation Trust (81): Pretap Singh Rana, Jill Greig, and Matthew Robinson; Hywel Dda University Health Board (80): Phil Jones, Sarah Jones, Lorinda Jones, Claire West, and Helen Tench; Chesterfield Royal Hospital NHS Foundation Trust (76): Sue Potter, Rachel Gascoyne, Amanda Whileman, Emily Hall, Stephanie Wright, Julie Toms, and Janet Tomlinson; Luton and Dunstable University Hospital NHS Foundation Trust (75): Lakshmanan Sekaran, Duke Phiri, Sakthivel Sethuraman, Niaz Mohammed, Frances Justin, Margaret Louise Tate, and Meena Chauhan; Countess of Chester Hospital NHS Foundation Trust (63): Kausik Chatterjee, Syed I. Haider, Arumugam Nallasivan, Tim Webster, Sandra Leason, and Samantha Seagrave; Peterborough City Hospital, Peterborough and Stamford Hospitals NHS Foundation Trust (58): Santhosh Subramonian, Peter Owksu‐Agyei, Natalie Temple, Nicola Butterworth‐Cowin, and Frederick Magezi; Leicester Royal Infirmary, University Hospitals of Leicester NHS Trust (54): Eleanor Turner, Shagufta Khan, Claire Stephens, Amit Mistri, Aidan Murphy, Manda Lam, Paul Underwood, and Catherine Thompson; Yeovil District Hospital NHS Foundation Trust (51): Caroline Smith, Clare Buckley, Diane Wood, Sarah Board, and Linda Howard; Barnsley Hospital NHS Foundation Trust (51): Sharon Johnson, Ashraf Ahmed, and Bethany Oates; Dorset County Hospital NHS Foundation Trust (50): Damian F. Jenkinson and Sara Leonard; Royal Bournemouth Hospital, Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust (46): Becky J. Jupp, Kamy Thavanesan, Michelle Dharmasiri, Sathyabama Logianathan, Catherine Ovington, Gail Hann, and Chantel Cox; Craigavon Area Hospital, Southern Health and Social Care Trust, Northern Ireland (43): Michael T. McCormick, Catherine Douglas, Michael Goggin, Patricia Fearon, Sara Gilpin, and Margaret O'Hagan; Pilgrim Hospital, United Lincolnshire Hospitals NHS Trust (37): David M. Mangion, Anne Hardwick, and Kimberley Netherton; Bedford Hospital NHS Trust (21): H. Ni, Judith Quinn, Tulu Bozkaplan, and Josin Jose.
Sources of Funding
The study was supported by a project grant (1066966) from the National Health and Medical Research Council of Australia.
Disclosures
Dr Muñoz Venturelli reports grant from Clínica Alemana de Santiago, during the conduct of the study; and a grant from CONICYT (Comisión Nacional de Investigación Científica y Tecnológica) Fondo Nacional de Desarrollo Científico y Tecnológico outside the submitted work. Dr Lavados reports grants from The George Institute for Global Health and Clínica Alemana de Santiago, during the conduct of the study; and nonfinancial support from Boehringer Ingelheim, grants and personal fees from Bayer and AstraZeneca, and grants from CONICYT, outside the submitted work. Dr Olavarría reports grants from Clínica Alemana de Santiago during the conduct of the study. Dr Hackett holds a National Health and Medical Research Council of Australia (NHMRC) Career Development Fellowship. Dr Pontes‐Neto received grants for the Brazilian Stroke Research Network by CNPQ (the National Council for Scientific and Technological Develop) (402388/2013‐5) for conduct of this study. Dr Robinson is a National Institutes of Health Research Senior Investigator. Dr Anderson holds an NHMRC Senior Principal Research Fellowship; and reports honoraria, travel reimbursement, and grant support from Takeda and Advisory Board fees from Amgen and Boehringer Ingelheim outside of this study. The remaining authors have no disclosures to report.
Supporting information
Table S1. Distribution of the Evidence‐Based Interventions and Model Analysis Results for Ischemic Stroke Treatment Based on mRS at 3 Months Including Multiple Imputation
Table S2. Distribution of the Evidence‐Based Interventions and Model Analysis Results for Ischemic Stroke Treatment Based on Mortality At 3 Months
Table S3. Evidence‐Based Interventions for Ischemic Stroke Treatment and Optimal Treatment Stratified By Region
Table S4. Patient Outcome by Hospital Characteristics: Uni and Multivariable Logistic Regression Adjusted for Patient Characteristics
Acknowledgements
We thank the participants and investigators of the HEADPOST (Head Positioning in Acute Stroke Trial).
(J Am Heart Assoc. 2019;8:e012640 DOI: 10.1161/JAHA.119.012640.)
Contributor Information
Craig S. Anderson, Email: canderson@georgeinstitute.org.au.
the HEADPOST (Head Positioning in Acute Stroke Trial) Investigators:
Gillian Mead, H. Asita De Silva, Jeyaraj D. Pandian, Ruey‐Tay Lin, Tsong‐Hai Lee, Liying Cui, Bin Peng, Stephane Heritier, Richard Lindley, Stephen Jan, Elizabeth Boaden, Christopher P. L. H. Chen, Anne Forster, Laurent Billot, Mark Woodward, Kris Rogers, Anish Scaria, Joyce Y. Lim, Natalie Espinosa, Lucy McEvoy, Lee Blackburn, Sarah S. Richtering, Shoujiang You, Simon Ladwig, Gabrielle P. Merritt, Bryce Thomsen, Kerry Jenson, Penelope Gordon, Dennis Ryan Nguyen, Wei Wei Quan, Tessa Pei‐Yi Lo, Jonathan Lim, Selena Goh, Leibo Liu, Mirza Ahmad Baig, Ravider Singh, Paul Donnelly, Manuela Armenis, Marna Van Zyl, Helen Monaghan, Phillipa Smith, Parisa Glass, Fanli Zhou, Yun Shen, Li Lei, Di Li, Ting Zhang, Xiaoyan Zhang, Yun Peng, Lingling Feng, Zhiping Ye, Philip Gregory, Jeyaraj D. Pandain, Deepti Arora, Pablo M. Lavados, Francisca Gonzalez, Bernardita Portales, Octavio Pontes‐Neto, Taiza Santos‐Pontelli, Brunna Rimoli, Monica Braga, Carolina Vidal, Dafna Benadof, Rodrigo J. Rivas, Laura Carvallo, Pamela Carvallo, Rubia Miranda, Brunna Pileggi, H. Asita de Silva, Shalomi Weerawardena, Thanushanthan Jeevarajah, Devaki Dharmawardena, Dumindi Ranasinghe, Matheesha Dharshana, Nilesh Nandadeva, Savithri Nawarathna, Ruey‐Tay Lin, Tsong‐Hai Lee, Jiu‐Haw Yin, Shoou‐Jeng Yeh, Ruei‐Jen Ma, Caroline L. Watkins, Gemma Whiteley, Denise Forshaw, Catherine Elizabeth Lightbody, Joanna Cox, Jane Fitzgerald, John F. Heney, Helen Byfield, Simone Finley, Hayley E. Tyrer, Carole Bruce, Alison Gibbon, Brett Jones, Emma Siracusa, Koushik Gowda, Shahla Cowans, Briana Forman, Sherin Jacob, Kristine Caprecho, Roshan Khatri, Po Yi Wan, Maria Lopez, Sifiso Vanika, Wilhelmina Bleeker, Marinka Ireland, Sheila Jala, Susan Day, Eric Ha, Martin Krause, Melissa Passer, Sarah Giaccari, Nadia Burkolter, Michael Braithwaite, Kylie Tastula, Darshan Ghia, Tapuwa Musuka, Anthony Alvaro, Gillian Edmonds, Nicole O'Loughin, Rebecca Phair, Joanne Kaoutal, David J. Blacker, Belinda L Saint, Kim Parrey, Michelle Coad, Matthew Kinchington, Nishantha Senanayake, Johanna Alaban, Irma Kuehne, Taiza Santos‐Pontelli, Monica Braga, Brunna Rimoli, Millene Camilo, Milena Libardi, Sheila Martins, Batista Carlos, Magda Martins, Leonardo Carbonera, Andrea Almeida, Martin Kelin, Carla Pauli, Mariana Lunardi, Luciane Silveira, Olga Chagas, Daily Souza, Gabriel Braga, Priscila Ribeiro, Gustavo Luvizutto, Marcia Polin, Fernanda Winckler, Jinfeng Liu, Zhenjiang Wang, Huibing Wang, Suying Lin, Jing Dong, Junshan Zhou, Suping Qin, Hui Zhan, Yongquan Xue, Dong Tian, Dan Yang, Yan Yin, He Li, Changming Geng, Jieyi Liu, Xiaolin Jiang, Yujun Wu, Wei Sun, Bingqi Yu, Yanmei Guan, Qin Wang, Bo Wei, Huirong Wang, Yan Wang, Liwen Tai, Wenchao Zhang, Weili Zhao, Xueying Wang, Guoli Li, Zhiming Ni, Fudong Guo, Lan Cen, Jun Lu, Zheng Chen, Guoming Yin, Yingchun Wang, Jiping Zheng, Zhimin Zhou, Hongquan Wang, Renlin Zou, Bin Xue, Airu Li, Jing Guo, Ying Guo, Xingguo Jiang, Xiuge Tan, Chunpeng Zhang, Bei Shao, Xiaoting Niu, Chunfeng Liu, Dongqin Chen, Ping Liang, Xia Zhang, Chunqing Zhang, Wenjie Gong, Zhichao Huang, Huihui Liu, Shoujiang You, Junying Huang, Rongfang Shi, Cuilan Wang, Ying Liu, Jinchao Wang, Guojun Wu, Zhihong Gao, Qunli Lin, Cong Xu, Huile Zheng, Xinghai Ye, Xiaoqiong Jin, Junyan Liu, Xiaoyun Cao, Yan Zhang, Jinyang Wang, Yuzhu Xu, Yan Li, Xin Ma, Qi Kong, Yanlei Hao, Baojun Qiao, Hui Yan, Zhiyong Huang, Baoqiang Chang, Jinjin Yan, Pinjun Liao, Wei Zhang, Ling Liu, Tingting Zhu, Xuehui Liu, Yongping Li, Ruifang Dong, Miao Chen, Xiaoli Ge, Hairong Wang, Lihua Dai, Jiafu Liu, Shixia Wang, Jihui Du, Aixiu Song, Yunhai Li, Jie Feng, Cheng Yu, Honglin Feng, Xiaojia Sun, Ruihong Sun, Weisong Liu, Jianfeng Liu, Xuesheng Lu, Enzhuo Chen, Wei Gao, Hui Liu, Heping Wang, Yanxia Wang, Juan Song, Dongqi Liu, Wenhui Du, Guixia Li, Cuiling Li, Yanling Liang, Xuekun Cai, Jinli Zhang, Xiaowei Tao, Pingshun An, Ranran Tang, Xu Qin, Yingling Wang, Wenjun Zhang, Rong Ma, Xiaoqiong Huang, Yonglin Liu, Yazhi Wang, Ping Fan, Hailan Yang, Lianyuan Feng, Jianxia Zhi, Jiewen Zhang, Yao Zhou, Danhong Wu, Haiyan He, Xiaohong Chen, Yongge Hou, Xiaohui Su, Liying Cui, Bin Peng, Siyuan Fan, Luis Suárez, Juan de Dios Polanco, Patricio Sotomayor, Ricardo Urzúa, Daniela Urrutia, Nathalie Conejan, Arturo Escobar, Monica Gonzalez, Danisa Vargas, Angel Constante, Erika Vásquez, Elizabeth Godoy, Christian Figueroa, Vanesa San Martin, Nataly Vidal, Madeleyn Muñoz, Alejandro Brunser, María Spencer, Juan Almeida, Ignacio Acosta, Rodrigo Guerrero, Prudencio Lozano, Camila Aguayo, Jimena Pizarro, Alvaro Soto, Flor Bonilla, Pía García, Carolina Del Castillo, Marcela Grandjean, Alexis Von Johnn, Ignacio Gutierrez, Francisca Rivero, Ignacio López, Federico Silva, Marlen Pachón, José Mendoza, Alexander Pabón, Mahesh Kate, Naushad Akhtar, Gibbsdeep S. Narang, Ashish Deepak, Vikram Huded, Romnesh De Sowza, Alben Sigamani, Karthikeyan Rajendran, Anisha Vishwanath, Anusha K, Somasundaram Kumaravelu, Syed Rahamath, Sandeep Kannneganti, Dheeraj Khurana, Cheena Katoch, Taranpreet Kaur, Ummer Karadan, Anu Kuriakose, Jaison John, Mumthaz Basheer, Harsha Hemal Gunasekara, Gamlath Chandima Udeni De Silva, Peetagam Harshi Lakmali Ubeywickrama, Kavisha Chathumali Silva, Eshani Anuradha De Silva, Udaya Ranawaka, Chamila Mettananda, Yamuna Nanayakkara, Tharini Mendis, Gayathri Fernando, Ahamed Imthikab, Kandula Pieris, Saman B. Gunatilake, Pamuditha M. W. Madanayake, Shiran A. Paranavitane, Bimsara Senanayake, Vaidhehi Vishwanathan, Maathury Sivapalan, Ruwangi U. Murage, Uthpala Chandradeva, Ruey‐Tay Lin, Yao‐Hua Liu, Chih‐Lung Lin, Hsiu‐Fen Lin, Kuan‐Ting Liu, Chien‐Fu Chen, Meng‐Ni Wu, Su‐Hua Tsai, Chi‐Ching Chen, Lan‐Yi Chen, Tsong‐Hai Lee, Chien‐Hung Chang, Yeu‐Jhy Chang, Kuo‐Lun Huang, Ting‐Yu Chang, Chi‐Hung Liu, Chen‐June Seak, Yu‐Li Lin, Jia‐Yi Luo, Hsiao‐Ying Yang, Ching‐Yi Wang, Lung Chan, Chaur‐Jong Hu, Nai‐Fang Chi, Dean Wu, Yao‐Hsien Huang, Yi‐Chun Kuan, Chien‐Tai Hong, Yi‐Chun Chen, Yu Sun, Cheng‐Huai Lin, Chien‐Jung Lu, Hai‐Jui Chu, Yi‐Chia Lo, Wen‐Hui Chang, Wan‐Jung Lin, Hui‐Chen Su, Tien‐Yu Lin, Chi‐Hsuan Cho, Shu‐Lan Lu, Ya‐Fang Hsueh, Ching‐Yi Lai, David Jarrett, Claire James, Stacey Valentine, Clare Whistler, Rebecca Butler, Simone Browning, Caroline Watchurst, Renuka Erande, Emma Elliott, Krishna Patel, Maria Brezitski, Caroline Hogan, Asra Banaras, Lucinda Crook, Rashidat Ahmed, Lindsay Potter, Rosie Laird, Natasha Clarke, Alison Loosemore, J. Godber, Sara Gawned, K. A. Hamilton, Rachael Jones, Paul Guyler, Sharon Tysoe, Raji Prabakaran, Sweni Shah, Joanne Calver, Laszlo K. Sztriha, Maria Fitzpatrick, Stephanie Drysdale, John Aeron‐Thomas, Emma McKenzie, Belinda Chitando, Paul Willcoxson, Elizabeth Iveson, Peter Wanklyn, Natasha Dyer, Michael Keeling, Romina Rodriguez, Kerry Elliott, Mia Porteous, Mark O'Neill, Sheridan Orme, Carla Richardson, Janet Tomlinson, Suzanne Hawkins, Delia Bester, Carol Jeffs, Joanne Howard, Pauline Brown, Deborah Ward, Jennifer Turfrey, Leanne Raybould, Allison Bates, Sue O'Connell, Margaret O'Connor, Samantha Williams, Hedley C. A. Emsley, Alison McLoughlin, Sonia Raj, Bindu Gregary, Donna Doyle, G. M. Courtauld, C. Schofield, L. Lucas, A. Lydon, A. James, Kari Saastamoinen, Laura Howaniec, Premchand Daboo, Ali N. Ali, Emma Richards, Joanne Howe, Christine Kamara, Kathy Stocks, Ralf Lindert, Diana J. Day, Sarah Finlay, Joanne McGee, Jennifer Mitchell, Elaine Amis, Rosemary Macey, Suzanne Tauro, Lauren Henry, Sarah Cuddy, Andrew Steele, Kerry Mullen, Sarah Kirker, Murudappa Bhattad, Michael Carpenter, Prabal Datta, Ann Needle, Linda Jackson, Julie Ball, Rosie Beckitt, Nicola Chivers, Angela Bowring, Sara Eddy, Kevin Thorpe, Samantha Keenan, Alison Griffin, Stuart Maguire, Chris Patterson, Hawraman Ramadan, Ruth Bellfield, Michaela Hooley, Kelvin Stewart, Lucy Williams, Cara Gurney, Deborah Oliver, Maria Gardiner, Sarah Grayland, Mohit Bhandari, David M. Collas, Tolu Adesina, Saul Sundayi, Ruth Harvey, Emma Pope, Audrey Lam, Elaine Walker, Colin Merrill, Soma Banerjee, Kirsten Hannah Harvey, Sheila Mashate, Peter Wilding, Linda Johnson, Robert Namushi, Patricia Jacob, Sreeman Andole, Karen Dunne, Naveen Gadapa, Sam King, Sonata Siliuzaite, Sharon Dealing, Karen Attwood, Annette Woods, Banher Sandhu, Maam Mamun, Afzal Mahmood, June Jones, Abimbola Ojo, Denise Carter‐Evans, Royal Liverpool, Aravind Manoj, Glyn Fletcher, Paula Lopez, Jill Greig, Matthew Robinson, Sarah Jones, Lorinda Jones, Claire West, Helen Tench, Rachel Gascoyne, Amanda Whileman, Emily Hall, Stephanie Wright, Julie Toms, Janet Tomlinson, Duke Phiri, Sakthivel Sethuraman, Niaz Mohammed, Frances Justin, Margaret Louise Tate, Meena Chauhan, Syed I. Haider, Arumugam Nallasivan, Tim Webster, Sandra Leason, Samantha Seagrave, Peterborough City Hospital, Peter Owksu‐Agyei, Natalie Temple, Nicola Butterworth‐Cowin, Frederick Magezi, Leicester Royal Infirmary, Shagufta Khan, Claire Stephens, Amit Mistri, Aidan Murphy, Manda Lam, Paul Underwood, Catherine Thompson, Clare Buckley, Diane Wood, Sarah Board, Linda Howard, Ashraf Ahmed, Bethany Oates, Sara Leonard, Royal Bournemouth Hospital, Royal Bournemouth, Kamy Thavanesan, Michelle Dharmasiri, Sathyabama Logianathan, Catherine Ovington, Gail Hann, Chantel Cox, Craigavon Area Hospital, Southern Health, Social Care Trust, Catherine Douglas, Michael Goggin, Patricia Fearon, Sara Gilpin, Margaret O'Hagan, Pilgrim Hospital, Anne Hardwick, Kimberley Netherton, Judith Quinn, Tulu Bozkaplan, and Josin Jose
References
- 1. GBD 2015 Neurological Disorders Collaborator Group . Global, regional, and national burden of neurological disorders during 1990‐2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol. 2017;16:877–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bray BD, Paley L, Hoffman A, James M, Gompertz P, Wolfe CDA, Hemingway H, Rudd AG; SSNAP Collaboration . Socioeconomic disparities in first stroke incidence, quality of care, and survival: a nationwide registry‐based cohort study of 44 million adults in England. Lancet Public Health. 2018;3:e185–e193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Glader EL, Stegmayr B, Johansson L, Hulter‐Åsberg K, Wester PO. Differences in long‐term outcome between patients treated in stroke units and in general wards: a 2‐year follow‐up of stroke patients in Sweden. Stroke 2001;32:2124–213. [DOI] [PubMed] [Google Scholar]
- 4. Stroke Unit Trialists’ Collaboration . Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev. 2013;9:CD000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Saposnik G, Kapral MK, Coutts SB, Fang J, Demchuk AM, Hill MD; the investigators of the Registry of the Canadian Stroke Network (RCSN) for the Stroke Outcome Research Canada (SORCan) Working Group . Do all age groups benefit from organized inpatient stroke care?. Stroke 2009;40:3321–3327. [DOI] [PubMed] [Google Scholar]
- 6. Pandian JD, William AG, Kate MP, Norrving B, Mensah GA, Davis S, Roth GA, Thrift AG, Kengne AP, Kissela BM, Yu C, Kim D, Rojas‐Rueda D, Tirschwell DL, Abd‐Allah F, Gankpe F, deVeber G, Hankey GJ, Jonas JB, Sheth KN, Dokova K, Mehndiratta MM, Geleijnse JM, Giroud M, Bejot Y, Sacco R, Sahathevan R, Hamadeh RR, Gillum R, Westerman R, Akinyemi RO, Barker‐Collo S, Truelsen T, Caso V, Rajagopalan V, Venketasubramanian N, Vlassovi VV, Feigin VL. Strategies to improve stroke care services in low‐ and middle‐income countries: a systematic review. Neuroepidemiology. 2017;49:45–61. [DOI] [PubMed] [Google Scholar]
- 7. Cadilhac DA, Kilkenny MF, Andrew NE, Ritchie E, Hill K, Lalor E; Stroke Foundation National Advisory Committee; and the National Stroke Audit Collaborative . Hospitals admitting at least 100 patients with stroke a year should have a stroke unit: a case study from Australia. BMC Heal Serv Res. 2017;17:212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ido MS, Frankel MR, Okosun IS, Rothenberg RB. Quality of care and its impact on one‐year mortality: the Georgia Coverdell acute stroke registry. Am J Med Qual. 2018;33:86–92. [DOI] [PubMed] [Google Scholar]
- 9. Ayis SA, Coker B, Bhalla A, Wellwood I, Rudd AG, Di Carlo A, Bejot Y, Ryglewicz D, Rastenyte D, Langhorne P, Dennis MS, McKevitt C, Wolfe CD. Variations in acute stroke care and the impact of organised care on survival from a European perspective: the European Registers of Stroke (EROS) investigators. J Neurol Neurosurg Psychiatry. 2013;84:604–612. [DOI] [PubMed] [Google Scholar]
- 10. Kaur P, Kwatra G, Kaur R, Pandian JD. Cost of stroke in low and middle income countries: a systematic review. Int J Stroke. 2014;9:678–682. [DOI] [PubMed] [Google Scholar]
- 11. Munoz Venturelli P, Robinson T, Lavados PM, Olavarria VV, Arima H, Billot L, Hackett ML, Lim JY, Middleton S, Pontes‐Neto O, Peng B, Cui L, Song L, Mead G, Watkins C, Lin RT, Lee TH, Pandian J, de Silva HA, Anderson CS, HeadPoST Investigators . Regional variation in acute stroke care organisation. J Neurol Sci. 2016;371:126–130. [DOI] [PubMed] [Google Scholar]
- 12. Langhorne P, O'Donnell MJ, Chin SL, Zhang H, Xavier D, Avezum A, Mathur N, Turner M, MacLeod MJ, Lopez‐Jaramillo P, Damasceno A, Hankey GJ, Dans AL, Elsayed A, Mondo C, Wasay M, Czlonkowska A, Weimar C, Yusufali AH, Hussain F Al, Lisheng L, Diener H‐C, Ryglewicz D, Pogosova N, Iqbal R, Diaz R, Yusoff K, Oguz A, Wang X, Penaherrera E, Lanas F, Ogah OS, Ogunniyi A, Iversen HK, Malaga G, Rumboldt Z, Magazi D, Nilanont Y, Rosengren A, Oveisgharan S, Yusuf S, O'Donnell M, Yusuf S, Rangarajan S, Rao‐Melacini P, Zhang XM, Islam S, Kabali C, Casanova A, Chin SL, DeJesus J, Dehghan M, Agapay S, McQueen M, Hall K, Keys J, Wang X, Devanath A, Gupta R, Prabhakaran D, Diaz R, Schygiel P, Garrote M, Rodriguez MA, Caccavo A, Duran RG, Sposato L, Molinos J, Valdez P, Cedrolla CM, Nofal PG, Huerta MF, Desmery PM, Zurru MC, Della Vedova B, Varigos J, Hankey G, Kraemer T, Gates P, Bladin C, Herkes G, Avezum A, Pereira MP, Minuzzo L, Oliveira L, Teixeira M, Reis H, Carvalho A, Ouriques Martins S, Carvalho JJ, Gebara O, Minelli C, Oliveira DC, Sobral Sousa AC, Ferraz de Almeida AC, Hernandez ME, Friedrich M, Mota DM, Ritt LE, Correa Vila Nova D, Teal P, Gladstone D, Shuaib A, Silver F, Dowlatshahi D, Lanas F, Carcamo D, Santibañez C, Garces E, Liu LS, Zhang HY, Fang HP, Lian MF, Shen F, Luo FX, Wen XX, Xu ZQ, Liu ZZ, Yan W, Yu JF, Wang WK, Liu LH, Sun YH, Zhou LC, Zhang ZF, Lv J, Zhang CS, Chen G, Wang HL, Chen Y, Zheng H, Huang JJ, Li WZ, Wang LJ, Shi JX, Hu CY, Song HF, Ji RY, Wang DL, Meng LH, Meng QW, Duan LJ, Liu HF, Luo YC, Zhang QY, Wu YB, Wang CR, Zhao JG, Liu SG, Shi CL, Wang XY, Lopez‐Jaramillo P, Martinez A, Sanchez‐Vallejo G, Molina DI, Espinosa T, Garcia Lozada H, Gomez‐Arbelaez D, Camacho PA, Rumboldt Z, Lusic I, Iversen HK, Truelsen T, Back C, Pedersen MM, Peñaherrera E, Duarte YC, Cevallos S, Tettamanti D, Caceres S, Diener HC, Weimar C, Grau A, Rother J, Ritter M, Back T, Winter Y, Pais P, Xavier D, Sigamani A, Mathur N, Rahul P, Murali A, Roy AK, Sarma GRK, Matthew T, Kusumkar G, Salam KA, Karadan U, Achambat L, Singh Y, Pandian JD, Verma R, Atam V, Agarwal A, Chidambaram N, Umarani R, Ghanta S, Babu GK, Sathyanarayana G, Sarada G, Navya Vani S, Sundararajan R, Sivakumar SS, Wadia RS, Bandishti S, Gupta R, Agarwal RR, Mohan I, Joshi S, Kulkarni S, Partha Saradhi S, Joshi P, Pandharipande M, Badnerkar N, Joshi R, Kalantri SP, Somkumar S, Chauhan S, Singh H, Varma S, Singh H, Sidhu GK, Singh R, Bansal KL, Bharani A, Pagare S, Chouhan A, Mahanta BN, Mahanta TG, Rajkonwar G, Diwan SK, Mahajan SN, Shaikh P, Devendrappa HR, Agrawal BK, Agrawal A, Khurana D, Thakur S, Jain V, Oveisgharan S, Bahonar A, Kelishadi R, Hossienzadeh A, Raeisidehkordi M, Akhavan H, Walsh T, Albaker O, Yusoff K, Chandramouli A, Shahadan S, Ibrahim Z, Husin A, Damasceno A, Lobo V, Loureiro S, Govo VA, Ogah OS, Ogunniyi A, Akinyemi RO, Owolabi MO, Sani MU, Owolabi LF, Iqbal R, Wasay M, Raza A, Malaga GG, Lazo‐Porras M, Loza‐Herrera JD, Acuña‐Villaorduña A, Cardenas‐Montero D, Dans A, Collantes E, Morales D, Roxas A, Villarruz‐Sulit MVC, Czlonkowska A, Ryglewicz D, Skowronska M, Restel M, Bochynska A, Chwojnicki K, Kubach M, Stowik A, Wnuk M, Pogosova N, Ausheva A, Karpova A, Pshenichnikova V, Vertkin A, Kursakov A, Boytsov S, Al‐Hussain F, DeVilliers L, Magazi D, Mayosi B, Elsayed ASA, Bikhari A, Sawaraldahab Z, Hamad H, ElTaher M, Abdelhameed A, Alawad M, Alkabashi D, Alsir H, Rosengren A, Andreasson M, Kembro Johansson J, Cederin B, Schander C, Elgasen AC, Bertholds E, Boström Bengtsson K, Nilanont Y, Nidhinandana S, Tatsanavivat P, Paryoonwiwat N, Poungvarin N, Suwanwela NC, Tiamkao S, Tulyapornchote R, Boonyakarnkul S, Hanchaiphiboolkul S, Muengtaweepongsa S, Watcharasaksilp K, Sathirapanya P, Pleumpanupat P, Oguz A, Akalin AA, Caklili OT, Isik N, Caliskan B, Sanlisoy B, Balkuv E, Tireli H, Yayla V, Cabalar M, Culha A, Senadim S, Arpaci B, Dayan C, Argun T, Yilmaz S, Celiker S, Kocer A, Asil T, Eryigit G, Mondo C, Kayima J, Nakisige M, Kitoleeko S, Yusufali AM, Zuberi BJ, Mirza HZ, Saleh AA, BinAdi JM, Hussain F, Langhorne P, Muir K, Walters M, McAlpine C, Ghosh S, Doney A, Johnston S, Mudd P, Black T, Murphy P, Jenkinson D, Kelly D, Whiting R, Dutta D, Shaw L, McFarlane C, Ronald E, McBurnie K. Practice patterns and outcomes after stroke across countries at different economic levels (INTERSTROKE): an international observational study. Lancet. 2018;391:2019–2027. [DOI] [PubMed] [Google Scholar]
- 13. Anderson CS, Arima H, Lavados P, Billot L, Hackett ML, Olavarria VV, Munoz Venturelli P, Brunser A, Peng B, Cui L, Song L, Rogers K, Middleton S, Lim JY, Forshaw D, Lightbody CE, Woodward M, Pontes‐Neto O, De Silva HA, Lin R‐T, Lee T‐H, Pandian JD, Mead GE, Robinson T, Watkins C; HeadPoST Investigators and Coordinators . Cluster‐randomized, crossover trial of head positioning in acute stroke. N Engl J Med. 2017;376:2437‐2447. [DOI] [PubMed] [Google Scholar]
- 14. Muñoz‐Venturelli P, Arima H, Lavados P, Brunser A, Peng B, Cui L, Song L, Billot L, Boaden E, Hackett ML, Heritier S, Jan S, Middleton S, Olavarría VV, Lim JY, Lindley RI, Heeley E, Robinson T, Pontes‐Neto O, Natsagdorj L, Lin R‐T, Watkins C, Anderson CS. Head Position in Stroke Trial (HeadPoST)—sitting‐up vs lying‐flat positioning of patients with acute stroke: study protocol for a cluster randomised controlled trial. Trials. 2015;16:256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Savio K, Pietra GL, Oddone E, Reggiani M, Leone MA. Reliability of the modified Rankin Scale applied by telephone. Neurol Int. 2013;5:e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. van Buuren S. Multiple imputation of discrete and continuous data by fully conditional specification. Stat Methods Med Res. 2007;16:219–242. [DOI] [PubMed] [Google Scholar]
- 17. Smith EE, Shobha N, Dai D, Olson DM, Reeves MJ, Saver JL, Hernandez AF, Peterson ED, Fonarow GC, Schwamm LH. Risk score for in‐hospital ischemic stroke mortality derived and validated within the Get With The Guidelines‐Stroke Program. Circulation. 2010;122:1496–1504. [DOI] [PubMed] [Google Scholar]
- 18. Cadilhac DA, Andrew NE, Lannin NA, Middleton S, Levi CR, Dewey HM, Grabsch B, Faux S, Hill K, Grimley R, Wong A, Sabet A, Butler E, Bladin CF, Bates TR, Groot P, Castley H, Donnan GA, Anderson CS; Australian Stroke Clinical Registry Consortium . Quality of acute care and long‐term quality of life and survival. Stroke. 2017;48:1026–1032. [DOI] [PubMed] [Google Scholar]
- 19. Bray BD, Ayis S, Campbell J, Hoffman A, Roughton M, Tyrrell PJ, Wolfe CD, Rudd AG. Associations between the organisation of stroke services, process of care, and mortality in England: prospective cohort study. BMJ. 2013;346:f2827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Urimubenshi G, Langhorne P, Cadilhac DA, Kagwiza JN, Wu O. Association between patient outcomes and key performance indicators of stroke care quality: a systematic review and meta‐analysis. Eur J Stroke. 2017;2:287–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dirks M, Niessen LW, van Wijngaarden JD, Koudstaal PJ, Franke CL, van Oostenbrugge RJ, Huijsman R, Lingsma HF, Minkman MM, Dippel DW; PRomoting ACute Thrombolysis in Ischemic StrokE (PRACTISE) Investigators . Promoting thrombolysis in acute ischemic stroke. Stroke. 2011;42:1325–1330. [DOI] [PubMed] [Google Scholar]
- 22. Asdaghi N, Romano JG, Wang K, Ciliberti‐Vargas MA, Koch S, Gardener H, Dong C, Rose DZ, Waddy SP, Robichaux M, Garcia EJ, Gonzalez‐Sanchez JA, Burgin WS, Sacco RL, Rundek T. Sex disparities in ischemic stroke care: FL‐PR CReSD Study (Florida‐Puerto Rico Collaboration to Reduce Stroke Disparities). Stroke. 2016;47:2618–2626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, Fang MC, Fisher M, Furie KL, Heck DV, Johnston SC, Kasner SE, Kittner SJ, Mitchell PH, Rich MW, Richardson D, Schwamm LH, Wilson JA; American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Peripheral Vascular Disease . Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:2160–2236. [DOI] [PubMed] [Google Scholar]
- 24. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, Jauch EC, Kidwell CS, Leslie‐Mazwi TM, Ovbiagele B, Scott PA, Sheth KN, Southerland AM, Summers D V, Tirschwell DL; American Heart Association Stroke Council . 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018;49:e46–e110. [DOI] [PubMed] [Google Scholar]
- 25. Wang Y, Li Z, Zhao X, Wang D, Li H, Xian Y, Liu L, Wang Y. Stroke care quality in China: substantial improvement, and a huge challenge and opportunity. Int J Stroke. 2017;12:229–235. [DOI] [PubMed] [Google Scholar]
- 26. Wang Y, Li Z, Zhao X, Wang C, Wang X, Wang D, Liang L, Liu L, Wang C, Li H, Shen H, Bettger J, Pan Y, Jiang Y, Yang X, Zhang C, Han X, Meng X, Yang X, Kang H, Yuan W, Fonarow GC, Peterson ED, Schwamm LH, Xian Y, Wang Y. Effect of a multifaceted quality improvement intervention on hospital personnel adherence to performance measures in patients with acute ischemic stroke in China. JAMA. 2018;320:245. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Distribution of the Evidence‐Based Interventions and Model Analysis Results for Ischemic Stroke Treatment Based on mRS at 3 Months Including Multiple Imputation
Table S2. Distribution of the Evidence‐Based Interventions and Model Analysis Results for Ischemic Stroke Treatment Based on Mortality At 3 Months
Table S3. Evidence‐Based Interventions for Ischemic Stroke Treatment and Optimal Treatment Stratified By Region
Table S4. Patient Outcome by Hospital Characteristics: Uni and Multivariable Logistic Regression Adjusted for Patient Characteristics


