Abstract
Purpose of review:
This review aims to highlight the current knowledge about inflammatory mechanisms of neurodegeneration in glaucoma with emphasis on potential immunomodulation strategies.
Recent findings:
Glaucomatous retina and optic nerve present multiple evidences of inflammatory responses of astroglia, microglia, and blood-born immune cells. Although adaptive/protective responses of resident or systemic immune cells can support neurons and promote tissue repair mechanisms after injurious insults, prolonged inflammatory processes can also produce neurotoxic mediators. Treatments targeting these neurodestructive outcomes may restore immune homeostasis and protect neurons from inflammatory injury. Due to widespread and chronic nature of neuroinflammation in glaucoma, immunomodulation offers a treatment strategy to protect different neuronal compartments of RGCs during the chronic and asynchronous course of neurodegeneration. Uncovering of distinct molecular responses and interactions of different immune cells that determine the neuroinflammatory phenotype and participate in neurodegenerative outcomes will be critical to develop effective strategies for immunomodulation in glaucoma.
Summary:
Neuroinflammation has increasingly been recognized to play an important role in glaucomatous neurodegeneration, and its modulation appears to be a promising treatment strategy for neuroprotection.
Keywords: Glaucoma, immunoregulation, immunomodulation, neuroinflammation, neurodegeneration, neuroprotection
Introduction
Glaucoma, a leading cause of blindness in the world, is a chronic neurodegenerative disease characterized by degeneration of optic nerve axons and loss of retinal ganglion cell (RGC) somas and synapses. Although increased intraocular pressure and advanced age are the main risk factors for initiation and progression of neurodegeneration in glaucoma, genetic and epigenetic predispositions also take part. Advancement of neuron loss despite efficient control of increased intraocular pressure in many patients suggests that mechanisms other than intraocular pressure-related biomechanical and/or ischemic injury may enhance the neurodegenerative process. Among a number of mechanisms that have been linked to pathophysiology of neurodegeneration in glaucoma, emerging evidence supports an important role of inflammatory processes [1–3].
As reviewed herein, multiple studies focusing on the immunogenic aspects of glaucoma have revealed a prominent activation of resident and systemic immune responses at early stages of disease, and inhibition of some of these responses has provided protection against neuron injury. As summarized later below, findings of these studies have also provided a list of immune mediators/regulators that may serve as molecular targets for new treatments to restore immune homeostasis. Evidently, neurodestructive consequences of inflammatory responses may lead to injury of optic nerve axons, including proximal and distal axon degeneration, and loss of RGC somas, dendritic tree, and synapses. Immunomodulatory treatments may therefore provide widespread protection against inflammatory injury at different neuronal compartments. This review will provide an overview of the present evidence for immune system involvement in glaucomatous neurodegeneration and the potential of immunomodulation as a therapeutic approach for neuroprotection. Recent trends and advances in the field will be briefly highlighted, rather than including a comprehensive literature review.
Cell types involved in neuroinflammation in glaucoma
Similar to many other neurodegenerative diseases, chronic glial activation is recognized as a sufficient hallmark of neuroinflammation in glaucoma. This is mainly due to the immune privileged status of brain tissues, in which inflammatory responses are dampened to an intermediate state called parainflammation [4]. This intermediate state characterized by sustained low-grade inflammation relying on reactive glia may represent an adaptive response to primary stress stimuli and/or neuron injury in glaucoma as the body’s natural attempt to minimize injury and help tissue healing. However, prolonged inflammatory activation of the glia, along with a failure in the regulation of immune response pathways, may shift the initial beneficial state towards a neurodegenerative process and promote secondary injury to neurons. It seems quite possible that the danger signals arising from stressed and injured tissues over a chronic period (along with the aging-related, genetic, epigenetic, and/or other systemic vulnerabilities to develop autoimmunity) may compromise the immune homeostasis in glaucoma [1–3]. Thus, chronic tissue stress, neuron injury, glial and systemic immune responses, and sustained release of neurotoxic mediators may create a vicious cycle that may promote progressing neuron injury.
Both astroglia (retina and optic nerve astrocytes, and retinal Müller cells) and microglia resident in the retina and optic nerve (head) profoundly respond in glaucoma. Owing to the intimate relationship of these neurosupport cells with RGCs at different neuronal compartments, glial responses are evident through the entire projection of RGCs from the retina to upper brain centers. However, despite their widespread nature, inflammatory responses in glaucoma may vary between different compartments that present differences in populations of glial subtypes that exhibit morphological, molecular, and functional characteristics [5,6].
Astroglia normally preserve tissue homeostasis, maintain synapses, recycle neurotransmitters, deliver neurotrophic factors and metabolites, control blood flow and vascular barriers, and participate neurogenesis. These neurosupport cells quickly recognize and respond to stress and injury signals as a neuronal defense and recovery mechanism. Astroglial cells become highly reactive both in the retina [7] and optic nerve head [8] in glaucomatous human donor eyes, and animal models with glaucoma [9,10]. Even a short period of time with ocular hypertension may be sufficient to initiate astrocyte reactivity in experimental glaucoma [10]. The early activation response of astroglia to glaucoma-related insults is portrayed by morphological alterations [8,9,11–13], and molecular responses [5,14–16] that may be detectable even before the damage to RGCs and axons.
Reactive astrogliosis may insulate the injured tissue to protect uninjured neurons from damaging effects. However, as evident in the glaucomatous optic nerve head, astroglial responses leading to tissue remodeling and glial scarring [10] may also create biomechanical stress on optic nerve axons. In addition, reactive astrocytes execute a self-survival program that may result in inadequate mechanic, trophic, and bioenergetic support to RGCs [9]. Mac-2-expressing phagocytic astrocytes in the myelination transition zone which have tissue cleaning function also show reduced capacity in glaucoma [17]. Moreover, astrocytes after gaining the inflammatory phenotype that is characterized by increased production of pro-inflammatory and neurotoxic molecules may generate neurodestructive signals and induce the death of neurons and oligodendrocytes [18,19]. Besides driving innate inflammatory activity that can promote neuron injury, reactive glia, including astrocytes, may also function as antigen-presenting cells to prime T cells for activation [20,21]. Even more, glaucoma-related alterations may compromise astrocyte functions in controlling the blood-brain barrier [22] and may thereby play an additional role in increased access of systemic immune cells into retina and optic nerve.
Similar to astroglia, microglial cells demonstrate increased reactivity in the retina and optic nerve head in experimental models [5,16,23–25] and human donor eyes with glaucoma [7,26,27]. Microglia normally provide neurotrophic support, and their scavenger and phagoeytosing functions promote tissue cleaning and healing; however, inflammatory responses of microglial cells may also contribute to neuron injury [28–30].
As much as individual contribution of astroglial and microglial cells in neuroinflammation, their interplay is also critical for the inflammatory outcomes. There is an intricate inter-relationship between astroglia and microglia in induction of the inflammatory and neurotoxic phenotype. For example, activated microglia induce neurotoxic A1 astrocytes by secreting pro-inflammatory cytokines [19], while astroglial cytokines and chemokines chemoattract and activate microglia.
Based on studies of experimental models, widespread responses of glia may even include the contralateral eyes with normal intraocular pressure [31,32], and bilateral spread of inflammatory responses and activation of astrocytes and microglia in both ocular hypertensive and normotensive fellow eyes may be detectable through the RGC projection sites, including the superior colliculus [33].
Another group of resident immune regulatory cells includes dendritic cells [34–36]. These cells are known to be early responders of neuron injury; however, their roles in glaucomatous neurodegeneration are not well-studied.
Myelin-producing oligodendrocytes constitute another important cell type that joins astrocytes and microglia behind the optic nerve head. Immune regulatory functions of oligodendrocytes are not fully understood; however, they can provide a physical barrier for immune cell infiltration into the optic nerve, and their loss may result the breakdown of this barrier [37,38].
In addition to resident glia, blood-born immune cells, such as monocytes, that can invade the optic nerve tissue may also be related to neuroinflammation in glaucoma. For example, in hereditary DBA-2J glaucoma with strong inflammatory component, transendothelial monocyte migration has been linked to the inflammatory component of neurodegeneration [29].
Thus, the complex process of neuro inflammation involves several cell types, and its outcomes may affect neuron survival at different compartments of RGCs, including dendritic tree, soma, axon, and synapses. Ongoing studies are expected to improve the molecular and mechanistic understanding of inflammatory responses and interactions of different cell types at different sites and different stages of neurodegeneration to enable immunomodulation as a neuroprotection strategy in glaucoma. The next section summarizes the current knowledge on molecular regulation of neuroinflammation in glaucoma, which founds the basis for further work and provides new directions for progress.
Molecular pathways of neuroinflanunation
Multiple studies using transcriptional [14–16,39–41] orproteomics profiling [42–45] have identified early upregulation of numerous molecules linked to inflammation pathways in the retina and optic nerve head of human donor eyes or animal models with glaucoma. Identified molecules have included a number of sensors/inducers, transducers, and effectors of neuro inflammatory processes leading to the production of neurotoxic mediators.
Glial cells can recognize stress or damage-associated molecular patterns (DAMPs) released from stressed or dying cells [46]. Among various DAMPS, heat shock proteins (HSPs) are a major group of stress proteins upregulated in the glaucomatous retina and optic nerve head [47], and these highly antigenic molecules have been associated with the immune responses in glaucoma [48,49]. An important class of pattern recognition receptors (PRRs) that can sense DAMPs is toll-like receptors (TLRs) [50]. Different TLRs display increased expression on astroglia and microglia in human glaucoma [43], experimental animals with induced ocular hypertension [45], and DBA-2J mice with hereditary glaucoma [16]. Based on in vitro experiments, components of the glaucomatous tissue stress, including upregulated HSPs and oxidative stress end-products, may function as intrinsic ligands for glial TLRs. Recognition of these endogenous stress-associated molecular patterns by TLRs initiates MyD88-dependent signaling that leads to nuclear factor-kappaB (NF-κB) activation, cytokine production, and stimulation of co-cultured T cells [43]. Tenascin C, another intrinsic ligand for TLRs, is also upregulated in the glaucomatous optic nerve head [51]. In addition, TLRs can recognize mitochondrial DAMPS, including the mitochondrial DNA released from cell debris [52]. The TLR signaling initiated by endogenous danger signals has been linked to innate and adaptive immune responses in various diseases with autoimmune origin [53].
As a matter of fact, recent observations suggest that not only intrinsic stimuli, but also conventional ligands for TLRs, namely pathogen-associated molecular patterns, may signal for TLR activation in glaucoma. This is because increased loads in microbiome have been linked to immune responses and neurodegeneration in human glaucoma and animal models [54,55]. As microbial and human proteins share significant homologies, the cross-reactivity between microbial and human antigens may also influence immune responses through TLR signaling in glaucoma [56,57], similar to many autoimmune diseases.
Nucleotide-binding oligomerization domain-like (NOD-like) receptors, another class of PRRs, are components of the multiprotein complex, named inflammasome. Inflammasome formation, an early innate response to cell stress, activates an inflammatory cascade that promotes proteolytic activation and secretion of cytokines. Gial NOD-like receptors, and inflammasome components are also among the molecules upregulated in the retina of human donors [44] and experimental animals with glaucoma [45].
While glial cells are equipped to sense stressed or injured neurons to initiate inflammatory signaling through DAMPs/PRRs, these cells may also directly respond to increased intraocular pressure and mechanical strain by sensing through mechanosensitive ion channels, such as purinergic receptors (P2X7R), transient receptor potential vanilloid (TRPV), and pannexin channels (PANX) [58–60]. However, inflammation-promoting mechanosensitive receptor signaling may also be activated by the ATP released from damaged RGCs. A principal role of nerve injury in stimulation of glial responses is supported by the attenuation of retinal glial responses after optic nerve crush when RGC death was blocked by deletion of the Bax gene [61].
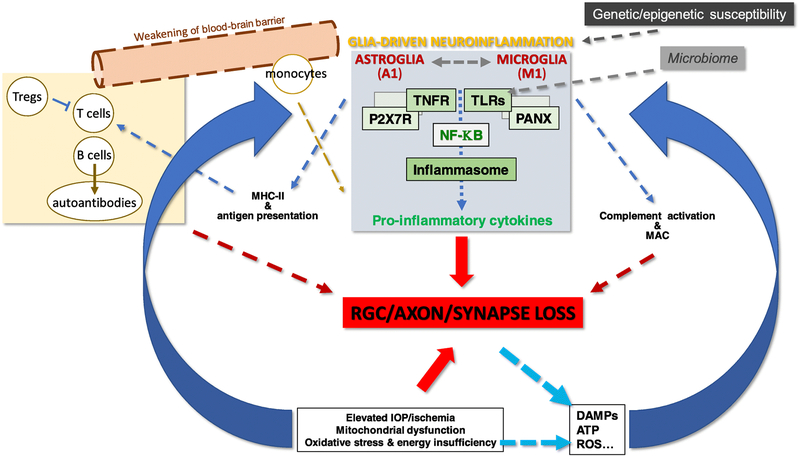
Thus, as schematized in Figure 1, glial inflammatory responses may be triggered by neuron stress/injury (by DAMPs through PRRs, by ATP through mechanosensitive ion channels), as well as directly by glaucoma-related insults, such as increased intraocular pressure (through mechanosensitive ion channels). Additionally, it is important to note that the neuron damage in glaucoma is asynchronous over a prolonged period, and the chronic disease process may also generate recurring waves of inflammatory stimulation.
Figure 1.
Glia-driven neuroinflammation may be initiated by both neuron injury (by DAMPs and ROS through PRRs, by ATP through mechanosensitive ion channels) and glaucoma-related insults, such as elevated intraocular pressure (through mechanosensitive ion channels). Thus, chronic tissue stress, neuron injury, glial and systemic immune responses, and sustained release of neurotoxic mediators create a vicious cycle that promotes further injury to retinal ganglion cells at different neuronal compartments.
After sensing the tissue stress and/or neuron injury, cooperative actions of different pathways initiate cascades of events that involve NF-κB, the key transcriptional activator of inflammatory mediators. This master regulator of the transcriptional program for inflammation [62] is activated in human glaucoma and animal models [44,45]. Various inflammation pathways that are activated in the glaucomatous glia, including TNFR and TLR signaling and inflammasome formation [43–45], are commonly linked to NF-κB.
In addition to stress/damage sensors (such as PRRs, TLRs), and inflammatory transducers (such as NF-κB, MyD88), upregulated molecules in glaucoma also include effectors and amplifiers of inflammation with neurotoxic outcomes, such as pro-inflammatory cytokines and chemokines. In glaucoma, reactive glia usually gain the pro-inflammatory phenotype characterized by increased production of pro-inflammatory cytokines, such as TNF-α, IL-1, IL-12 [16,44], as opposed to anti-inflammatory cytokines. The glial pro-inflammatory cytokine imbalance in glaucomatous tissues is most prominent by increased production of TNF-α [63,64], which is also linked to RGC death [18,21,63–65]. Evidently, TNFα/TNFRl signaling can induce RGC death through proteolytic caspase cascade, mitochondrial dysfunction, oxidative stress [18,44,66], and calcium-permeable AMPA receptor activation [67]. Besides direct neurotoxicity of TNF-α produced by reactive glia [18,68], downstream NF-κB activation leads to transcriptional activation of more cytokines and other immune mediators, further activate glial responses, and thereby amplify the vicious cycle of inflammation. Additionally, TNF-α may weaken the blood-brain barrier and directly facilitate glia-T cell interactions to stimulate differentiation of T cells into effector cells of systemic immune responses [21].
Parallel to increased expression of pro-inflammatory cytokines in the glaucomatous retina and optic nerve, analysis of glaucomatous aqueous humor and blood samples has also detected increased levels of these cytokines [69–72]. Furthermore, proteins encoded by the current collection of glaucoma-related genes include those linked to cytokine signaling [73]. It is evident that not only genetic predispositions, but epigenetic susceptibility factors may also affect the glia-driven neuroinflammation in glaucoma. For example, individual variations detected in the retinal expression pattern of TNF-α-induced protein-3 (TNFAIP3, a regulator of the inflammatory outcomes of TNFα/TNFRl signaling) among glaucomatous human donors have been found correlated with increased methylation of the TNFAIP3 promoter [44].
Another important immunostimulatory stimulus in glaucoma includes oxidative stress. As well as the age-dependence of glaucoma and key roles of oxidative stress in aging-related deterioration, the glaucoma-related amplification of oxidative stress (through mitochondrial dysfunction or other pathogenic processes) has been implicated in neurodegeneration [74]. Apparently, many consequences of oxidative stress may also be immunostimulatory in glaucoma [1,75]. For example, oxidative stress stimulates glial cytokine production [21], activates glial TLR signaling [43], and induces complement dysregulation [42]. In addition to co-stimulatory role of reactive oxygen species in antigen presentation of glial cells to T lymphocytes [21], protein oxidation [76] may modify the antigenic features of retina and optic nerve proteins [77]. Moreover, advanced glycation end-products (AGEs) that accumulate through oxidative stress-dependent processes in glaucomatous tissues [78] may act as a persistent antigenic stimulus and activate immunostimulatory signaling through specific receptors (such as RAGE, another sensor receptor of tissue stress). It is also noteworthy that the NF-κB-regulated transcriptional program for inflammation is redox-sensitive. In support of these immunostimulatory roles of oxidative stress in glaucoma, antioxidant treatment has been found immunomodulatory. Parallel to neuroprotective outcomes, antioxidant treatment has decreased the production of pro-inflammatory cytokines and activation of NF-κB in experimental glaucoma [79].
Complement activation has also been associated to glaucomatous neurodegeneration. Various components of the complement activation cascade, including the cytolytic membrane attack complex, have been detected in glaucomatous eyes [16,42,80–82]. This critical mechanism for immune surveillance and clearance has been linked to synapse elimination and dendrite remodeling in glaucoma [82]. In addition, transgenic or pharmacologic treatments inhibiting complement components have provided protection against RGC loss in animal models [83–85]. Although many evidences support neurodestructive consequences of uncontrolled complement activation in mouse glaucoma, inflammatory outcomes through complement anaphylatoxins, C3a, C5a, remain poorly defined.
Systemic immune responses
Besides innate immune responses, glial cells (together with other resident immune cells) also have the ability to stimulate systemic immune responses. The neuroinflammatory environment enriched with pro-inflammatory cytokines appears to favor the interaction of glia with T lymphocytes to elicit expanded immune responses. Additionally, increased expression of highly antigenic and immunostimulatory stress proteins [47,48], increased antigenicity due to protein modifications [76,77], and increased exposure of antigens due to neuron injury may help create a proper setting for autoimmunity. Growing data from gene or protein expression studies of glaucoma also support a marked upregulation of various chemotaxis and adhesion molecules needed for the glia-T cell interaction [14–16,39–41,44,45]. Furthermore, major histocompatibility complex II molecules are increased on reactive glia in human glaucoma [20] and animal models [23,86], and stress-associated costimulatory molecules in glaucomatous tissues, including reactive oxygen species [21], may enhance the ability of glial cells for antigen presentation to T lymphocytes. As supported by animal models, activated T cells may be recruited to the eye, infiltrate the site of injury [55,87,88], and produce inflammatory outcomes that are neurotoxic to RGCs [49,55,88,89].
Indeed, studies of experimental models have provided data supportive of stimulated T cell responses with neurodegenerative potential [49,55,88,89]. Likewise, studies of blood samples from patient groups with glaucoma have detected a shift in T cell subset distribution towards the pro-inflammatory Th1 cytokine phenotype [90,91]. Recent studies have also pointed to an imbalance of the regulatory subset of T cells (Treg), indicating the lack of efficient T cell suppression in some patients with glaucoma (presented at the Annual Meeting of the Association for Research in Vision and Ophthalmology, 2018, Abstract # 3733). These observations are consistent with increased titers of pro-inflammatory cytokines in the glaucomatous human blood [71].
Numerous studies have also documented a complex repertoire of circulating autoantibodies that react to a variety of retina and optic nerve proteins, and the accompanying deposition of immunoglobulins in glaucomatous retinas [89,92]. Whether these antibody responses are an outcome or a pathogenic mechanism of neurodegeneration is the subject of ongoing debate. Based on experimental studies, HSP antibodies, when exogenously applied at concentrations similar to that detected in the glaucomatous blood, may be internalized by retinal neurons and facilitate their death in the human retina, ex vivo [93]. Although antibody-mediated processes may not produce inflammatory outcomes, which is the focus of this review, autoantibody production and ocular entrance may be the consequence of glia-driven inflammatory responses that prepare the conditions for antigen presentation (leads to autoantibody production) and blood-brain barrier permeability (facilitates the access of autoantibodies).
While reactive T lymphocytes may be able to invade through the intact blood-brain barrier [55,94], glaucoma-related alterations in astrocyte functions may also weaken the perivascular barriers [22]. It seems quite possible that a breach in the blood-retina barrier as evident in small optic disc hemorrhages [95] or parapapillary chorioretinal atrophy areas [96], both of which are commonly detectable in glaucomatous eyes in association with disease progression, may also allow increased access of circulating immune cells, or non-cellular components (like auto antibodies) into the retina and optic nerve. Interestingly, activated microglia have been found strategically positioned within the regions of parapapillary chorioretinal atrophy in glaucomatous eyes [26,27]. A longitudinal study of serum autoantibody reactivity has also showed an increase over time in glaucoma patients with optic disc hemorrhages, but no change has been detected in patients without optic disc hemorrhages [97]. Consistent with these observations, transfer of the mononuclear cells obtained from glaucoma patients with optic disc hemorrhages into immune deficient mice has resulted in a marked decrease in RGC density (presented at the Annual Meeting of the Association for Research in Vision and Ophthalmology, 2018, Abstract # 3731).
Potential treatments for immunomodulation
With respect to neurodegenerative potential of neuroinflammation, its efficient control can protect neurons from inflammatory neurotoxicity and enhance endogenous recovery processes. Due to widespread nature of neuroinflammation through different neuronal compartments, immunomodulation may offer a treatment strategy to protect RGC somas, axons, and synapses during the course of neurodegeneration in glaucoma. As being major players of neuroinflammation, glial cells appear to be excellent candidates for targeting to restore immune homeostasis and improve the outcome of glaucoma. Chronic nature of the astroglial response, as opposed to temporary responses of microglia, during glaucomatous neurodegeneration makes them particularly important as treatment target. As also noted above, ongoing tissue stress and asynchronicity of neuron injury over the chronic disease period may re-amplify glial inflammatory responses in glaucomatous eyes. Therefore, lowering of elevated intraocular pressure, or other neuroprotective treatments, may also have anti-inflammatory outcomes.
Recent experimental studies of therapeutic approaches have targeted different molecules to modulate neuro inflammation in glaucoma. Genetic or pharmaceutical inhibition of TNF-α, a major pro-inflammatory and pro-apoptotic cytokine, has provided protection against RGC and axon degeneration in experimental models of glaucoma [68,98]. However, it should be clarified that TNF-α signaling may lead to protective or destructive outcomes depending on the type of receptor preferentially used, and the cross-talk between multiple signalling pathways. In addition, soluble TNF-a more than its membrane-bound form is required to generate neuroinflammation, which is the principal ligand for TNFR1, the primary receptor for majority of inflammatory responses [65]. Different effects of TNF-α on neuron survival or glia-driven inflammatory outcomes may also be time-dependent [99,100], as well as depending on interactions between different molecular pathways [44].
As a treatment approach towards sensing and inducing of inflammation, selective inhibition of TLR4 signaling with TAK-242 (resatorvid) has also reduced astrocyte activation and RGC death after optic nerve crush injury in mice [101].
Regarding the transduction of inflammation signaling, inactivation of astroglial NF-κB, the key transcriptional activator of inflammatory mediators downstream of TNF-α/TNFR and TLR signaling pathways, has reduced pro-inflammatory genes and promoted RGC survival after retinal ischemia [102]. Recent experimental findings from the cre/lox-based deletion of IκKβ (the main activating kinase for NF-κB in the canonical pathway with inflammatory outcomes) in experimental mouse glaucoma have also supported immunomodulatory and neuroprotective outcomes of astroglial NF-κB inhibition in the glaucomatous retina and optic nerve head (presented at the Annual Meeting of the Association for Research in Vision and Ophthalmology, 2018, Abstract # 6140). Although NF-κB appears to be a promising target for immunomodulation, it should be emphasized that besides inflammatory mediators, NF-kB also activates critical anti-apoptotic genes and regulates a broad range of processes essential for neuron survival [62,103]. These opposing aspects of NF-κB point to the need for glia-targeting transgenic strategies, because the lack of cell-specifieity of NF-κB-inhibiting pharmacological treatments would potentially cause adverse effects on neuron survival. This is also supported by NF-κB 1 knockouts that develop optic neuropathy and progressive RGC loss [104].
Consistent with various roles of oxidative stress in induction of glia-driven inflammatory responses in glaucoma [74], antioxidant treatment has lowered pro-inflammatory cytokine production and NF-κB activation in the ocular hypertensive rat retina and optic nerve [79].
Various studies have also targeted different cellular components of neuroinflammation in experimental models. Decreasing the astroglial and microglial reactivity with intraocular administration of a cAMP phosphodiesterase inhibitor (ibudilast) has resulted in decreased production of pro-inflammatory mediators and increased survival of neurons in ocular hypertensive rat eyes [105]. Other studies testing different treatments to deactivate retina or optic nerve head microglia at early stages of experimental glaucoma have also reported to reduce neurodegeneration [28,106,107]. Additionally, inhibition of monocyte entry into optic nerve head by irradiation has provided protection against neuron injury in DBA/2J mice [29]. Treatments targeting endothelin-2, a damaging mediator produced by monocytes (bosentan) combined with anti-complement treatment (C1qa mutation) have also been found protective [84]. Furthermore, findings of a more recent study have indicated that the extensive neuroinflammation in DBA/2J glaucoma, but not in induced microbead occlusion model of glaucoma that lacks pre-existing inflammation, may contribute to Ranvier node pathology and neurophysiological deficits, and immunosuppressive treatment with fingolimod can provide some protection [108].
Treatments towards systemic immune responses may also be considered to restore immune homeostasis in glaucoma. The neurodegenerative potential of reactive T cells, along with the altered T cell profile with inefficient Treg suppression in patients’ blood, may promise for T cell-based immunotherapies. Antigenic vaccination has been suggested to boost protective T cell responses for neuroprotection in glaucoma models but not been pursued further [109]. Similar to many autoimmune neurodegenerative diseases, boosting of the endogenous Treg response, or adoptive cell therapy by transferring purified induced Treg [110], may be further tested as an immunomodulation strategy for glaucoma.
Moreover, stem cell-based strategies may be useful to modulate inflammatory responses. For example, mesenchymal stem cell-derived exosomes have been reported to deliver trophic and immunomodulatory factors, suppress the migration of inflammatory cells, attenuate pro-inflammatory cytokine secretion, and promote RGC survival [111,112].
Despite favorable results of recent experimental studies, development of immunomodulatory treatments is highly challenging when respecting the dynamic nature of inflammatory responses and the complexity of cellular and molecular components of neuroinflammation. Since beneficial and detrimental outcomes of inflammatory processes involve shared molecules (as noted above for TNF-α signaling, or NF-κB activation), protective versus destructive pathways of glial responses should be carefully outweighed. Various potential treatments may also require the development of glia-targeting strategies. Further elucidation of the molecular components and time course of specific responses of glial subtypes and interactions of different immune cells in governing the final outcome will be crucial to develop effective treatment modalities.
Conclusion
Accumulating evidence from studies of human donor eyes and animal models supports prolonged roles of resident and systemic immune responses in glaucomatous neurodegeneration and points to immunomodulation as a neuroprotective treatment strategy for glaucoma. Since neurodestructive outcomes of glia-driven neuroinflammation may affect RGC survival at different neuronal compartments, glia-targeting strategies are likely to provide widespread protection against inflammatory injury to RGC somas, dendrites, axons, and synapses during the chronic and asynchronous course of glaucomatous neurodegeneration. Ongoing efforts are expected to further enhance the molecular understanding of specific responses and interactions of different immune cells at different sites and different stages of neurodegeneration so that improved strategies can be developed for immunomodulation in glaucoma.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of Interest
Gülgün Tezel reports grants from National Eye Institute, during the conduct of her studies. Mine Bariş declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance, •• Of major importance
- 1.Tezel G. Immune regulation toward immunomodulation for neuroprotection in glaucoma. Curr Opin Pharmacol. 2013;13:23–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soto I, Howell GR. The complex role of neuroinflammation in glaucoma. Cold Spring Harb Perspect Med. 2014;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mac Nair CE, Nickells RW. Neuroinflammation in glaucoma and optic nerve damage. Prog Mol Biol Transi Sci. 2015;134:343–363. [DOI] [PubMed] [Google Scholar]
- 4.Medzhitov R. Origin and physiological roles of inflammation. Nature. 2008;454:428–435. [DOI] [PubMed] [Google Scholar]
- 5.Qu J, Jakobs TC. The time course of gene expression during reactive gliosis in the optic nerve. PLoS One. 2013;8:e67094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seitz R, Ohlmann A, Tamm ER. The role of Muller glia and microglia in glaucoma. Cell Tissue Res. 2013;353:339–345. [DOI] [PubMed] [Google Scholar]
- 7.Tezel G, Chauhan BC, LeBlanc RP, Wax MB. Immunohistochemical assessment of the glial mitogen-activated protein kinase activation in glaucoma. Invest Ophthalmol Vis Sci. 2003;44:3025–3033. [DOI] [PubMed] [Google Scholar]
- 8.Hernandez MR, Miao H, Lukas T. Astrocytes in glaucomatous optic neuropathy. Prog Brain Res. 2008;173:353–373. [DOI] [PubMed] [Google Scholar]
- 9.Dai C, Khaw PT, Yin ZQ, Li D, Raisman G, Li Y. Structural basis of glaucoma: the fortified astrocytes of the optic nerve head are the target of raised intraocular pressure. Glia. 2012;60:13–28. [DOI] [PubMed] [Google Scholar]
- 10.Sun D, Qu J, Jakobs TC. Reversible reactivity by optic nerve astrocytes. Glia. 2013;61:1218–1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang L, Ciofïl GA, Cull G, Dong J, Fortune B. Immunohistologie evidence for retinal glial cell changes in human glaucoma. Invest Ophthalmol Vis Sci. 2002;43:1088–1094. [PubMed] [Google Scholar]
- 12.Inman DM, Homer PJ. Reactive nonproliferative gliosis predominates in a chronic mouse model of glaucoma. Glia. 2007;55:942–953. [DOI] [PubMed] [Google Scholar]
- 13.Lye-Barthel M, Sun D, Jakobs TC. Morphology of astrocytes in a glaucomatous optic nerve. Invest Ophthalmol Vis Sci. 2013;54:909–917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nikolskaya T, Nikolsky Y, Serebryiskaya T, Zvereva S, Sviridov E, Dezso Z, Rahkmatulin E, Brennan RJ, Yankovsky N, Bhattacharya SK, Agapova O, Hernandez MR, Shestopalov VI. Network analysis of human glaucomatous optic nerve head astrocytes. BMC Med Genomics. 2009;2:24, [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson EC, Jia L, Cepuma WO, Doser TA, Morrison JC. Global changes in optic nerve head gene expression after exposure to elevated intraocular pressure in a rat glaucoma model. Invest Ophthalmol Vis Sci. 2007;48:3161–3177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Howell GR, Macalinao DG, Sousa GL, Walden M, Soto I, Kneeland SC, Barbay JM, King BL, Marchant JK, Hibbs M, Stevens B, Barres BA, Clark AF, Libby RT, John SW. Molecular clustering identifies complement and endothelin induction as early events in a mouse model of glaucoma. J Clin Invest. 2011;121:1429–1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nguyen JV, Soto I, Kim KY, Bushong EA, Oglesby E, Valiente-Soriano FJ, Yang Z, Davis CH, Bedont JL, Son JL, Wei JO, Buchman VL, Zack DJ, Vidal-Sanz M, Ellisman MH, Marsh-Armstrong N. Myelination transition zone astrocytes are constitutively phagocytic and have synuclein dependent reactivity in glaucoma. Proc Natl Acad Sci U S A. 2011;108:1176–1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tezel G, Wax MB. Increased production of tumor necrosis factor-alpha by glial cells exposed to simulated ischemia or elevated hydrostatic pressure induces apoptosis in cocultured retinal ganglion cells. J Neurosci. 2000;20:8693–8700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. **.Liddelow SA, Guttenplan KA, Clarke LE, Bennett FC, Bohlen CJ, Schirmer L, Bennett ML, Munch AE, Chung WS, Peterson TC, Wilton DK, Frouin A, Napier BA, Panicker N, Kumar M, Buckwalter MS, Rowitch DH, Dawson VL, Dawson TM, Stevens B, Barres BA. Neurotoxic reactive astrocytes are induced by activated microglia. Nature. 2017;541:481–487. [DOI] [PMC free article] [PubMed] [Google Scholar]; This paper presents evidence for microglia-astrocyte interactions in neuroinflammation that activated microglia induce neurotoxic A1 astrocytes by secreting cytokines.
- 20.Yang J, Yang P, Tezel G, Patil RV, Hernandez MR, Wax MB. Induction of HLA-DR expression in human lamina cribrosa astrocytes by cytokines and simulated ischemia. Invest Ophthalmol Vis Sci. 2001;42:365–371. [PubMed] [Google Scholar]
- 21.Tezel G, Yang X, Luo C, Peng Y, Sun SL, Sun D. Mechanisms of immune system activation in glaucoma: oxidative stress-stimulated antigen presentation by the retina and optic nerve head glia. Invest Ophthalmol Vis Sci. 2007;48:705–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Flammer J, Mozaffarieh M. What is the present pathogenetic concept of glaucomatous optic neuropathy? Surv Ophthalmol. 2007;52 Suppl 2:S162–173. [DOI] [PubMed] [Google Scholar]
- 23.Ebneter A, Casson RJ, Wood JP, Chidlow G. Microglial activation in the visual pathway in experimental glaucoma: spatiotemporal characterization and correlation with axonal injury. Invest Ophthalmol Vis Sci. 2010;51:6448–6460. [DOI] [PubMed] [Google Scholar]
- 24.Bosco A, Steele MR, Vetter ML. Early microglia activation in a mouse model of chronic glaucoma. J Comp Neurol. 2011;519:599–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taylor S, Calder CJ, Albon J, Erichsen JT, Boulton ME, Morgan JE. Involvement of the CD200 receptor complex in microglia activation in experimental glaucoma. Exp Eye Res. 2011;92:338–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Neufeld AH. Microglia in the optic nerve head and the region of parapapillary chorioretinal atrophy in glaucoma. Arch Ophthalmol. 1999; 117:1050–1056. [DOI] [PubMed] [Google Scholar]
- 27.Yuan L, Neufeld AH. Activated microglia in the human glaucomatous optic nerve head. J Neurosci Res. 2001;64:523–532. [DOI] [PubMed] [Google Scholar]
- 28.Bosco A, Inman DM, Steele MR, Wu G, Soto I, Marsh-Armstrong N, Hubbard WC, Calkins DJ, Homer PJ, Vetter ML. Reduced retina microglial activation and improved optic nerve integrity with minocycline treatment in the DBA/2J mouse model of glaucoma. Invest Ophthalmol Vis Sci. 2008;49:1437–1446. [DOI] [PubMed] [Google Scholar]
- 29.Howell GR, Soto I, Zhu X, Ryan M, Macalinao DG, Sousa GL, Caddie LB, MacNicoll KH, Barbay JM, Porciatti V, Anderson MG, Smith RS, Clark AF, Libby RT, John SW. Radiation treatment inhibits monocyte entry into the optic nerve head and prevents neuronal damage in a mouse model of glaucoma. J Clin Invest. 2012;122:1246–1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bosco A, Romero CO, Breen KT, Chagovetz AA, Steele MR, Ambati BK, Vetter ML. Neurodegeneration severity can be predicted from early microglia alterations monitored in vivo in a mouse model of chronic glaucoma. Dis Model Mech. 2015;8:443–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ramirez AI, Salazar JJ, de Hoz R, Rojas B, Gallego BI, Salinas-Navarro M, Alarcon-Martinez L, Ortin-Martinez A, Aviles-Trigueros M, Vidal-Sanz M, Trivino A, Ramirez JM. Quantification of the effect of different levels of IOP in the astroglia of the rat retina ipsilateral and contralateral to experimental glaucoma. Invest Ophthalmol Vis Sci. 2010;51:5690–5696. [DOI] [PubMed] [Google Scholar]
- 32.Gallego BI, Salazar JJ, de Hoz R, Rojas B, Ramirez AI, Salinas-Navarro M, Ortin-Martinez A, Valiente-Soriano FJ, Aviles-Trigueros M, Villegas-Perez MP, Vidal-Sanz M, Trivino A, Ramirez JM. IOP induces upregulation of GFAP and MHC-II and microglia reactivity in mice retina contralateral to experimental glaucoma. J Neuroinflammation. 2012;9:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. *.Sapienza A, Raveu AL, Reboussin E, Roubeix C, Boucher C, Degardin J, Godefroy D, Rostene W, Reaux-Le Goazigo A, Baudouin C, Melik Parsadaniantz S. Bilateral neuroinflammatory processes in visual pathways induced by unilateral ocular hypertension in the rat. J Neuroinflammation. 2016; 13:44. [DOI] [PMC free article] [PubMed] [Google Scholar]; * This study demonstrates bilateral spread of inflammatory responses in visual pathways after unilateral induction of intraocular pressure elevation in rats.
- 34.Lehmann U, Heuss ND, McPherson SW, Roehrich H, Gregerson DS. Dendritic cells are early responders to retinal injury. Neurobiol Dis. 2010;40:177–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Heuss ND, Pierson MJ, Montaniel KR, McPherson SW, Lehmann U, Hussong SA, Ferrington DA, Low WC, Gregerson DS. Retinal dendritic cell recruitment, but not function, was inhibited in MyD88 and TRIF deficient mice. J Neuroinflammation. 2014; 11:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schlereth SL, Kremers S, Schrodl F, Cursiefen C, Heindl LM. Characterization of antigen-presenting macrophages and dendritic cells in the healthy human sclera. Invest Ophthalmol Vis Sci. 2016;57:4878–4885. [DOI] [PubMed] [Google Scholar]
- 37.Dewar D, Underhill SM, Goldberg MP. Oligodendrocytes and ischemic brain injury. J Cereb Blood Flow Metab. 2003;23:263–274. [DOI] [PubMed] [Google Scholar]
- 38.Fitzgerald M, Bartlett CA, Harvey AR, Dunlop SA. Early events of secondary degeneration after partial optic nerve transection: an immunohistochemical study. J Neurotrauma. 2010;27:439–452. [DOI] [PubMed] [Google Scholar]
- 39.Steele MR, Inman DM, Calkins DJ, Homer PJ, Vetter ML. Microarray analysis of retinal gene expression in the DBA/2J model of glaucoma. Invest Ophthalmol Vis Sci. 2006;47:977–985. [DOI] [PubMed] [Google Scholar]
- 40.Yang Z, Quigley HA, Pease ME, Yang Y, Qian J, Valenta D, Zack DJ. Changes in gene expression in experimental glaucoma and optic nerve transection: the equilibrium between protective and detrimental mechanisms. Invest Ophthalmol Vis Sci. 2007;48:5539–5548. [DOI] [PubMed] [Google Scholar]
- 41.Panagis L, Zhao X, Ge Y, Ren L, Mittag TW, Danias J. Gene expression changes in areas of focal loss of retinal ganglion cells in the retina of DBA/2J mice. Invest Ophthalmol Vis Sci. 2010;51:2024–2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tezel G, Yang X, Luo C, Kain AD, Powell DW, Kuehn MH, Kaplan HJ. Oxidative stress and the regulation of complement activation in human glaucoma. Invest Ophthalmol Vis Sei. 2010;51:5071–5082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Luo C, Yang X, Kain AD, Powell DW, Kuehn MH, Tezel G. Glaucomatous tissue stress and the regulation of immune response through glial toll-like receptor signaling. Invest Ophthalmol Vis Sei. 2010;51:5697–5707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yang X, Luo C, Cai J, Powell DW, Yu D, Kuehn MH, Tezel G. Neurodegenerative and inflammatory pathway components linked to TNF-alpha/TNFRl signaling in the glaucomatous human retina. Invest Ophthalmol Vis Sei. 2011;52:8442–8454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tezel G, Yang X, Luo C, Cai J, Powell DW. An astrocyte-specific proteomic approach to inflammatory responses in experimental rat glaucoma. Invest Ophthalmol Vis Sei. 2012;53:4220–4233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kono H, Rock KL. How dying cells alert the immune system to danger. Nat Rev Immunol. 2008;8:279–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tezel G, Hernandez MR, Wax MB. Immunostaining of heat shock proteins in the retina and optic nerve head of normal and glaucomatous eyes. Arch Ophthalmol. 2000;118:511–518. [DOI] [PubMed] [Google Scholar]
- 48.Tezel G, Yang J, Wax MB. Heat shock proteins, immunity and glaucoma. Brain Res Bull. 2004;62:473–480. [DOI] [PubMed] [Google Scholar]
- 49.Wax MB, Tezel G, Yang J, Peng G, Patil RV, Agarwal N, Sappington RM, Calkins DJ. Induced autoimmunity to heat shock proteins elicits glaucomatous loss of retinal ganglion cell neurons via activated T-cell-derived fas-ligand. J Neurosci. 2008;28:12085–12096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lehnardt S. Innate immunity and neuro inflammation in the CNS: the role of microglia in Toll-like receptor-mediated neuronal injury. Glia. 2010;58:253–263. [DOI] [PubMed] [Google Scholar]
- 51.Pena JD, Varela HJ, Ricard CS, Hernandez MR. Enhanced tenascin expression associated with reactive astrocytes in human optic nerve heads with primary open angle glaucoma. Exp Eye Res. 1999;68:29–40. [DOI] [PubMed] [Google Scholar]
- 52.Zhang Q, Raoof M, Chen Y, Sumi Y, Sursal T, Junger W, Brohi K, Itagaki K, Hauser CJ. Circulating mitochondrial DAMPs cause inflammatory responses to injury. Nature. 2010;464:104–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rifkin IR, Leadbetter EA, Busconi L, Viglianti G, Marshak-Rothstein A. Toll-like receptors, endogenous ligands, and systemic autoimmune disease. Immunol Rev. 2005;204:27–42. [DOI] [PubMed] [Google Scholar]
- 54.Astafurov K, Elhawy E, Ren L, Dong CQ, Igboin C, Hyman L, Griffen A, Mittag T, Danias J. Oral microbiome link to neurodegeneration in glaucoma. PLoS One. 2014;9:el04416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. **.Chen H, Cho KS, Vu THK, Shen CH, Kaur M, Chen G, Mathew R, McHam ML, Fazelat A, Lashkari K, Au NPB, Tse JKY, Li Y, Yu H, Yang L, Stein-Streilein J, Ma CHE, Woolf CJ, Whary MT, Jager MJ, Fox JG, Chen J, Chen DF. Commensal mieroflora-induced T cell responses mediate progressive neurodegeneration in glaucoma. NatCommun. 2018;9:3209. [DOI] [PMC free article] [PubMed] [Google Scholar]; Findings of this study support T cell-mediated component of glaucomatous neurodegeneration, which may initiate after pre-sensitization of T cells by exposure to commensal microflora, as wel as elevation of intraocular pressure.
- 56.Wax MB. Anti-Ro/SS-A positivity and heat shock protein antibodies in patients with normal-pressure glaucoma. J Glaucoma. 1998;125:145–157. [DOI] [PubMed] [Google Scholar]
- 57.Romano C, Li Z, Arendt A, Hargrave PA, Wax MB. Epitope mapping of anti-rhodopsin antibodies from patients with normal pressure glaucoma. Invest Ophthalmol Vis Sei. 1999;40:1275–1280. [PubMed] [Google Scholar]
- 58.Reigada D, Lu W, Zhang M, Mitchell CH. Elevated pressure triggers a physiological release of ATP from the retina: Possible role for pannexin hemichannels. Neuroscience. 2008;157:396–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Krizaj D, Ryskamp DA, Tian N, Tezel G, Mitchell CH, Slepak VZ, Shestopalov VI. From mechanosensitivity to inflammatory responses: new players in the pathology of glaucoma. Curr Eye Res. 2014;39:105–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. **.Albalawi F, Lu W, Beckel JM, Lim JC, McCaughey SA, Mitchell CH. The P2X7 receptor primes IL-lbeta and the NLRP3 inflammasome in astrocytes exposed to mechanical strain. Front Cell Neurosci. 2017;11:227. [DOI] [PMC free article] [PubMed] [Google Scholar]; Presented findings provide links between mechanical strain and neuroinflammation through purinergic receptor signaling.
- 61. **.Mac Nair CE, Schlamp CL, Montgomery AD, Shestopalov VI, Nickells RW. Retinal glial responses to optic nerve crush are attenuated in Bax-deficient mice and modulated by purinergic signaling pathways. J Neuroinflammation. 2016; 13:93. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study of mouse optic nerve crush model presents evidence for a principal role of nerve injury in stimulation of retinal glial responses.
- 62.Harari OA, Liao JK. NF-kappaB and innate immunity in ischemic stroke. Ann N Y Acad Sei. 2010;1207:32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yan X, Tezel G, Wax MB, Edward DP. Matrix metalloproteinases and tumor necrosis factor alpha in glaucomatous optic nerve head. Arch Ophthalmol. 2000;118:666–673. [DOI] [PubMed] [Google Scholar]
- 64.Tezel G, Li LY, Patil RV, Wax MB. Tumor necrosis factor-alpha and its receptor-1 in the retina of normal and glaucomatous eyes. Invest Ophthalmol Vis Sci. 2001;42:1787–1794. [PubMed] [Google Scholar]
- 65.Tezel G. TNF-alpha signaling in glaucomatous neurodegeneration. Prog Brain Res. 2008;173:409–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tezel G, Yang X. Caspase-independent component of retinal ganglion cell death, in vitro. Invest Ophthalmol Vis Sci. 2004;45:4049–4059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cueva Vargas JL, Osswald IK, Unsain N, Aurousseau MR, Barker PA, Bowie D, Di Polo A. Soluble tumor necrosis factor alpha promotes retinal ganglion cell death in glaucoma via calcium-permeable AMP A receptor activation. J Neurosci. 2015;35:12088–12102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Nakazawa T, Nakazawa C, Matsubara A, Noda K, Hisatomi T, She H, Michaud N, Hafezi-Moghadam A, Miller JW, Benowitz LI. Tumor necrosis factor-alpha mediates oligodendrocyte death and delayed retinal ganglion cell loss in a mouse model of glaucoma. J Neurosci. 2006;26:12633–12641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kuchtey J, Rezaei KA, Jaru-Ampompan P, Sternberg P Jr., Kuchtey RW. Multiplex cytokine analysis reveals elevated concentration of interleukin-8 in glaucomatous aqueous humor. Invest Ophthalmol Vis Sci. 2010;51:6441–6447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sawada H, Fukuchi T, Tanaka T, Abe H. Tumor necrosis factor-alpha concentrations in the aqueous humor of patients with glaucoma. Invest Ophthalmol Vis Sci. 2010;51:903–906. [DOI] [PubMed] [Google Scholar]
- 71.Huang P, Qi Y, Xu YS, Liu J, Liao D, Zhang SS, Zhang C. Serum cytokine alteration is associated with optic neuropathy in human primary open angle glaucoma. J Glaucoma. 2010;19:324–330. [DOI] [PubMed] [Google Scholar]
- 72.Chua J, Vania M, Cheung CM, Ang M, Chee SP, Yang H, Li J, Wong TT. Expression profile of inflammatory cytokines in aqueous from glaucomatous eyes. Mol Vis. 2012;18:431–438. [PMC free article] [PubMed] [Google Scholar]
- 73.Wiggs JL. Glaucoma genes and mechanisms. Prog Mol Biol Transl Sci. 2015; 134:315–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tezel G. Oxidative stress in glaucomatous neurodegeneration: Mechanisms and consequences. Prog Retin Eye Res. 2006;25:490–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tezel G. The immune response in glaucoma: a perspective on the roles of oxidative stress. Exp Eye Res. 2011;93:178–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tezel G, Yang X, Cai J. Proteomic identification of oxidatively modified retinal proteins in a chronic pressure-induced rat model of glaucoma. Invest Ophthalmol Vis Sci. 2005;46:3177–3187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tezel G, Thornton IL, Tong MG, Luo C, Yang X, Cai J, Powell DW, Soltau JB, Liebmann JM, Ritch R. Immunoproteomic analysis of potential serum biomarker candidates inhuman glaucoma. Invest Ophthalmol Vis Sci. 2012;53:8222–8231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Tezel G, Luo C, Yang X. Accelerated aging in glaucoma: immunohistochemical assessment of advanced glycation end products in the human retina and optic nerve head. Invest Ophthalmol Vis Sci. 2007;48:1201–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. *.Yang X, Hondur G, Tezel G. Antioxidant treatment limits neuroinflammation in experimental glaucoma. Invest Ophthalmol Vis Sci. 2016;57:2344–2354. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study of experimental mouse glaucoma supports the potential of antioxidant treatment as an immunomodulation strategy for neuroprotection in glaucoma.
- 80.Stasi K, Nagel D, Yang X, Wang RF, Ren L, Podos SM, Mittag T, Danias J. Complement component IQ upregulation in retina of murine, primate, and human glaucomatous eyes. Invest Ophthalmol Vis Sci. 2006;47:1024–1029. [DOI] [PubMed] [Google Scholar]
- 81.Kuehn MH, Kim CY, Ostojic J, Beilin M, Alward WL, Stone EM, Sakaguchi DS, Grozdanic SD, Kwon YH. Retinal synthesis and deposition of complement components induced by ocular hypertension. Exp Eye Res. 2006;83:620–628. [DOI] [PubMed] [Google Scholar]
- 82.Stevens B, Allen NJ, Vazquez LE, Howell GR, Christopherson KS, Nouri N, Micheva KD, Mehalow AK, Huberman AD, Stafford B, Sher A, Litke AM, Lambris JD, Smith SJ, John SW, Barres BA. The classical complement cascade mediates CNS synapse elimination. Cell. 2007;131:1164–1178. [DOI] [PubMed] [Google Scholar]
- 83.Howell GR, Soto I, Ryan M, Graham LC, Smith RS, John SW. Deficiency of complement component 5 ameliorates glaucoma in DBA/2J mice. J Neuroinflammation. 2013; 10:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Howell GR, MacNicoll KH, Braine CE, Soto I, Macalinao DG, Sousa GL, John SW. Combinatorial targeting of early pathways profoundly inhibits neurodegeneration in a mouse model of glaucoma. Neurobiol Dis. 2014;71:44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. **.Bosco A, Anderson SR, Breen KT, Romero CO, Steele MR, Chiodo VA, Boye SL, Hauswirth WW, Tomlinson S, Vetter ML. Complement C3-targeted gene therapy restricts onset and progression of neurodegeneration in chronic mouse glaucoma. Mol Ther. 2018;26:2379–2396. [DOI] [PMC free article] [PubMed] [Google Scholar]; Findings of this study support that transgenic inhibition of complement C3 activation restricts neurodegeneration in DBA-2J glaucoma.
- 86.Chidlow G, Ebneter A, Wood JP, Casson RJ. Evidence supporting an association between expression of major histocompatibility complex II by microglia and optic nerve degeneration during experimental glaucoma. J Glaucoma. 2016;25:681–691. [DOI] [PubMed] [Google Scholar]
- 87.Moalem G, Leibowitz-Amit R, Yoles E, Mor F, Cohen IR, Schwartz M. Autoimmune T cells protect neurons from secondary degeneration after central nervous system axotomy. Nat Med. 1999;5:49–55. [DOI] [PubMed] [Google Scholar]
- 88.Gramlich OW, Ding QJ, Zhu W, Cook A, Anderson MG, Kuehn MH. Adoptive transfer of immune cells from glaucomatous mice provokes retinal ganglion cell loss in recipients. Acta Neuropathol Commun. 2015;3:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Joachim SC, Gramlich OW, Laspas P, Schmid H, Beck S, von Pein HD, Dick HB, Pfeiffer N, Grus FH. Retinal ganglion cell loss is accompanied by antibody depositions and increased levels of microglia after immunization with retinal antigens. PLoS One. 2012;7:e40616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Yang J, Patil RV, Yu H, Gordon M, Wax MB. T cell subsets and sIL-2R/IL-2 levels in patients with glaucoma. Am J Ophthalmol. 2001;131:421–426. [DOI] [PubMed] [Google Scholar]
- 91. *.Guo C, Wu N, Niu X, Wu Y, Chen D, Guo W. Comparison of T helper cell patterns in primary open-angle glaucoma and normal-pressure glaucoma. Med Sci Monit. 2018;24:1988–1996. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study documents different pattern of T helper cells in blood samples of patients with glaucoma.
- 92.Wax MB, Tezel G, Edward PD. Clinical and ocular histopathological findings in a patient with normal-pressure glaucoma. Arch Ophthalmol. 1998;116:993–1001. [DOI] [PubMed] [Google Scholar]
- 93.Tezel G, Wax MB. The mechanisms of hsp27 antibody-mediated apoptosis in retinal neuronal cells. JNeurosci. 2000;20:3552–3562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hu P, Pollard JD, Chan-Ling T. Breakdown of the blood-retinal barrier induced by activated T cells of nonneural specificity. Am J Pathol. 2000; 156:1139–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Uhler TA, Piltz-Seymour J. Optic disc hemorrhages in glaucoma and ocular hypertension: implications and recommendations. Curr Opin Ophthalmol. 2008;19:89–94. [DOI] [PubMed] [Google Scholar]
- 96.Tezel G, Siegmund KD, Trinkaus K, Wax MB, Kass MA, Kolker AE. Clinical factors associated with progression of glaucomatous optic disc damage in treated patients. Arch Ophthalmol. 2001;813–818. [DOI] [PubMed] [Google Scholar]
- 97. *.Lorenz K, Beck S, Keilani MM, Wasielica-Poslednik J, Pfeiffer N, Gras FH. Longitudinal analysis of serum autoantibody-reactivities in patients with primary open angle glaucoma and optic disc hemorrhage. PLoS One. 2016; 11 :e0166813. [DOI] [PMC free article] [PubMed] [Google Scholar]; This longitudinal stud) of serum autoantibody reactivity shows an increase over time in glaucoma patients with optic disc hemorrhage.
- 98.Roh M, Zhang Y, Murakami Y, Thanos A, Lee SC, Vavvas DG, Benowitz LI, Miller JW. Etanercept, a widely used inhibitor of tumor necrosis factor-alpha (TNF-alpha), prevents retinal ganglion cell loss in a rat model of glaucoma. PLoS One. 2012;7:e40065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Tezel G, Yang X, Yang J, Wax MB. Role of tumor necrosis factor receptor-1 in the death of retinal ganglion cells following optic nerve crash injury in mice. Brain Res. 2004;996:202–212. [DOI] [PubMed] [Google Scholar]
- 100.Mac Nair CE, Fernandes KA, Schlamp CL, Libby RT, Niekells RW. Tumor necrosis factor alpha has an early protective effect on retinal ganglion cells after optic nerve crash. J Neuroinflammation. 2014; 11:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. *.Nakano Y, Shimazawa M, Ojino K, Izawa H, Takeuchi H, Inoue Y, Tsurama K, Hara H. Toll-like receptor 4 inhibitor protects against retinal ganglion cell damage induced by optic nerve crash in mice. J Pharmacol Sci. 2017;133:176–183. [DOI] [PubMed] [Google Scholar]; This study presents that resatorvid, an inhibitor of TLR4 signaling, is effective to inhibit inflammatory activation of retinal astrocytes after optic nerve crush injury.
- 102.Dvoriantchikova G, Barakat D, Brambilla R, Agudelo C, Hernandez E, Bethea JR, Shestopalov VI, Ivanov D. Inactivation of astroglial NF-kappa B promotes survival of retinal neurons following ischemic injury. Eur J Neurosci. 2009;30:175–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Karin M, Lin A. NF-kappaB at the crossroads of life and death. Nat Immunol. 2002;3:221–227. [DOI] [PubMed] [Google Scholar]
- 104.Takahashi Y, Katai N, Murata T, Taniguchi SI, Hayashi T. Development of spontaneous optic neuropathy in NF-kappaBetap50-deficient mice: requirement for NF-kappaBetap50 in ganglion cell survival. Neuropathol Appl Neurobiol. 2007;33:692–705. [DOI] [PubMed] [Google Scholar]
- 105. *.Cueva Vargas JL, Belforte N, Di Polo A. The glial cell modulator ibudilast attenuates neuroinflammation and enhances retinal ganglion cell viability in glaucoma through protein kinase A signaling. Neurobiol Dis. 2016;93:156–171. [DOI] [PubMed] [Google Scholar]; Findings of this study suggest that attenuation of gliosis by ibudilast, a eAMP phosphodiesterase inhibitor, decreases the production of pro-inflammatory mediators and increases the survival of neurons in ocular hypertensive rat eyes.
- 106.Bosco A, Crish SD, Steele MR, Romero CO, Inman DM, Homer PJ, Calkins DJ, Vetter ML. Early reduction of microglia activation by irradiation in a model of chronic glaucoma. PLoS One. 2012;7:e43602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Su W, Li Z, Jia Y, Zhuo Y. Rapamyein is neuroprotective in a rat chronic hypertensive glaucoma model. PLoS One. 2014;9:e99719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. **.Smith MA, Plyler ES, Dengler-Crish CM, Meier J, Crish SD. Nodes of Ranvier in glaucoma. Neuroscience. 2018;390:104–118. [DOI] [PubMed] [Google Scholar]; This paper points to Ranvier node pathology in DBA-2J glaucoma, which may reduce after immunosuppressive treatment with fingolimod.
- 109.Schwartz M. Harnessing the immune system for neuroprotection: therapeutic vaccines for acute and chronic neurodegenerative disorders. Cell Mol Neurobiol. 2001;21:617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. *.Kanamori M, Nakatsukasa H, Okada M, Lu Q, Yoshimura A. Induced regulatory T cells: their development, stability, and applications. Trends Immunol. 2016;37:803–811. [DOI] [PubMed] [Google Scholar]; This paper provides a review of work to devolop immunotherapies with induced Tregs.
- 111.Mead B, Tomarev S. Bone marrow-derived mesenchymal stem cells-derived exosomes promote survival of retinal ganglion cells through miRNA-dependent mechanisms. Stem Cells Transl Med. 2017;6:1273–1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. *.Harrell CR, Simovic Markovie B, Fellabaum C, Arsenijevic A, Djonov V, Arsenijevic N, Volarevic V. Therapeutic potential of mesenchymal stem cell-derived exosomes in the treatment of eye diseases. Adv Exp Med Biol. 2018. [DOI] [PubMed] [Google Scholar]; This review article discusses the therapeutic potential of mesenchymal stem cell-derived exosomes in degenerative and inflammatory ocular diseases.