The area of demographic-specific medicine is currently a burgeoning area of research. The 2010 United States Census demonstrates that the United States is composed of an increasingly diverse population. For the digestive disease specialist, this diversity presents a number of diagnostic and therapeutic challenges because of differences in disease predisposition, presentation, and course, including response to therapy. An understanding of these differences will facilitate effective diagnosis and treatment specific to the unique needs of our increasingly culturally and linguistically diverse patients.
Hepatitis C: Racial and Ethnic Aspects of Its Management
One digestive disease with known racial variation in prevalence and treatment response is the hepatitis C virus (HCV). Currently, there are 170 million HCV-infected people worldwide, composing the largest portion of chronic liver disease patients and those with complications including cirrhosis and hepatocellular carcinoma. In the United States, HCV is twice as prevalent in African Americans compared with Caucasians. This discrepancy suggests that race might be an independent risk factor for chronic infection with hepatitis C. Hypotheses proposed to explain this difference in prevalence include racial differences in viral clearance, mode of transmission, viral kinetics, immune responsiveness, and socioeconomic status.
HCV genotype 1 comprises 75% of HCV infections in the Western world and is more resistant to therapy, requiring 12 months of treatment compared with 6 months of treatment for patients with genotypes 2 or 3. Even with longer treatment courses, attainment of sustained virologic response (SVR) is poor in persons infected with genotype 1.1 For unclear reasons, genotype 1 is more prevalent in African Americans, occurring in 91% of those infected compared with 65% of infected Caucasians.1 Furthermore, African Americans are less likely to respond to standard treatment for HCV. Chronicity is also associated with African American race. Chronic HCV occurs in 95% of African Americans but only in 33% of Caucasians.1
Latinos also have worse HCV outcomes than Caucasians. A nonrandomized prospective study of standard treatment with peginterferon alpha-2a and ribavirin for 48 weeks demonstrated that being of Latino descent was an independent predictor of decreased SVR, even when adjusted for body mass index (BMI), presence of cirrhosis, age, alanine aminotransferase, and HCV RNA viral load.2 Other factors such as the total amount of drug received, need for dose reduction, discontinuation of a study drug, and compliance with therapy did not explain the differences in SVR in Latinos versus non-Latinos. Histologic response to therapy was also 47% lower among Latinos. Although this study controlled for BMI (which has been shown previously to be associated with reduced SVRs), there was a greater proportion of Latinos who were obese and diabetic in this study, suggesting that residual confounding by these factors on the observed association between Latino ethnicity and reduced SVR might have been present. Alternatively, the authors propose that Latinos might be less sensitive to interferon, perhaps because of ethnic variation in the innate immune response to therapy, similar to African Americans. Thus, research highlights the importance of other underlying factors within the Latino and African-American populations that could lower response rates and could include factors such as immune differences in response rates to peginterferon, genetic variations, and other comorbidities.
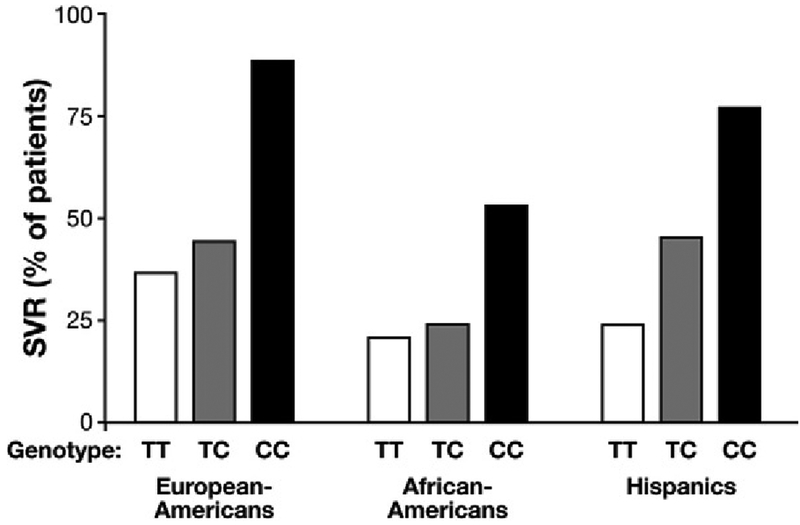
Genetic variations might underlie differences in treatment response. This issue has been further explored with identification of a genetic polymorphism associated with increased SVR in both Caucasians and African Americans.3 In patients of European ancestry, those homozygous for C allele of the IL28 B gene experienced a 2-fold greater rate of SVR than patients with the TT genotype. Interestingly, the African American population has a lower prevalence of the favorable CC genotype (Figure 1). This observation might explain the lower SVR rates in the African American population, lending credence to the claim that specific genetic factors cause an impaired immunologic response to hepatitis C seen in the African American population. Studies such as these pointing to racial differences in infection rates and treatment responses stress the importance for further research to improve treatment regimens in this population.
Figure 1.
Likelihood of clearance of hepatitis C (SVR) as determined by IL28B genotype and race or ethnicity. Genotype CC is associated with the highest likelihood of SVR. Because African Americans and Hispanics who are homozygotes for CC have lower SVRs than European Americans who are homozygotes for CC, there are other aspects associated with race or ethnicity that influence likelihood of an SVR. Figure adapted from Ge D et al. Nature 2009;461:399 – 401, by permission from Macmillian Publishers, Ltd.
Colorectal Cancer Among African Americans: Unique Clinical Presentation and Potential Need for Targeted Management
Colorectal Cancer Risk Is Higher Among African Americans
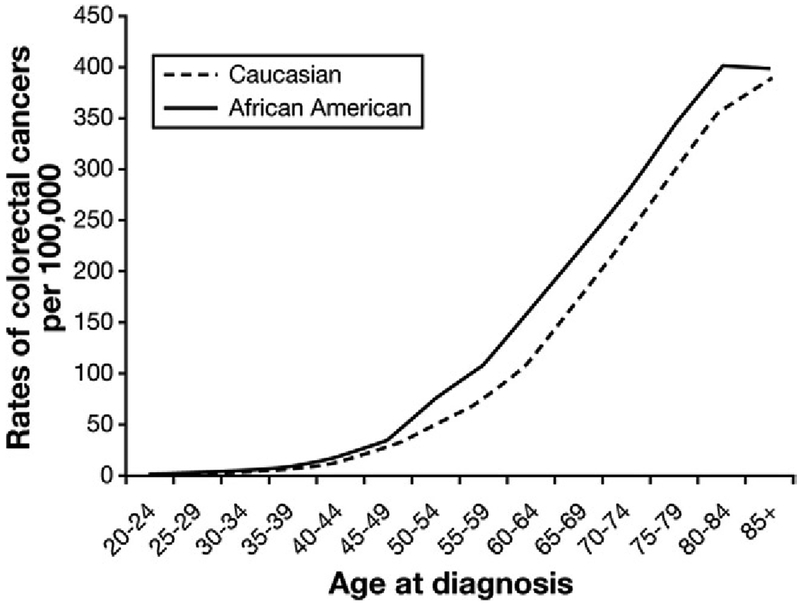
Colorectal cancer (CRC) is the second leading cause of cancer death in the United States, and the burden of disease presents a particularly formidable challenge for African Americans and their physicians.4 African Americans have the highest CRC incidence (Figure 2), youngest age of onset, and most advanced stage at presentation, leading to the highest CRC mortality rates of any population.4 Social, economic, biological, and environmental factors have been postulated as causes for the high rate of CRC among African Americans, although the causes of these disparities remain largely unexplained.
Figure 2.
Age-specific CRC incidence for Caucasian and African American men and women. Beginning after age 45, African Americans have higher rates of CRC incidence at all ages. The absolute highest excess in CRC incidence is seen after age 50. Data source: Surveillance Epidemiology End Results Incidence Rates, http://seer.cancer.gov/faststats, accessed 10/5/2010.
Screening Rates Are Lower Among African Americans, but Promising Strategies for Boosting Screening Exist
Screening rates for African Americans have lagged behind Caucasians and, at 59%, are clearly suboptimal for such a high-risk population. Lower rates of physician recommendation for screening as well as access to health insurance are commonly cited but addressable barriers to screening completion. Beyond screening recommendation and access, studies suggest interventions targeted to African Americans might be of value. For example, one randomized trial has shown that patient navigation substantially improved CRC screening in a low-income, diverse population, including African Americans.5 In this study, navigation consisted of use of trained lay out-reach workers to educate patients about screening, aid in scheduling appointments, and address personal, cultural, or systemic barriers to screening and resulted in doubling the screening rate compared with usual care.
Optimal Age of Initiation and Screening Modality for Screening African Americans Requires Further Study
Although the US Preventive Services Task Force, the American Cancer Society, and the American Gastroenterological Association have not offered any race-specific screening recommendations, the American College of Gastroenterology and the American Society for Gastrointestinal Endoscopy have recommended that African Americans begin screening for CRC at age 45 rather than 50, specifically with colonoscopy. Although the efforts of the American College of Gastroenterology and American Society for Gastrointestinal Endoscopy to bring attention to the risks African Americans face are to be commended, many questions regarding this strategy remain. The earlier screening recommendations are based on the observation that African Americans have higher age-specific incidence of CRC than other groups, beginning in the fifth decade of life. Indeed, national cancer registry data report that African Americans have 5.1 more cases of CRC per 100,000 people compared with Caucasians from age 40 – 49 and 10.7 more cases per 100,000 from age 45– 49.4 Nonetheless, these same epidemiologic data suggest that 90% of CRCs occur among African Americans older than age 50 (more than 57% older than age 64).4 Thus, although African Americans certainly have higher rates of CRC beginning in the fifth decade, one can question whether lowering the screening age is as beneficial as optimizing screening in patients over age 50 who are currently eligible for screening. Furthermore, it is unknown whether a universal recommendation for early screening will expand the number of African Americans who undergo screening or simply shift the onset of screening for those who would have participated in screening 5 years earlier; the latter scenario might not have a substantial public health benefit. Thus, early age of screening, although an attractive approach because of higher rates of early onset disease among African Americans, requires further study as a public health strategy for reducing the burden of CRC on African Americans. In addition to earlier screening, more frequent screening (such as every 5-year colonoscopy) might also need to be formally studied.
Another key question is whether a colonoscopy only recommendation is the best public health approach to improving CRC outcomes for African Americans. Proponents cite higher relative proportion of right-sided CRC and adenomas and higher rates of adenomas overall among African Americans compared with Caucasians as a rationale to support colonoscopy only based screening.6 However, the rate of left-sided CRC is still predominant among African Americans, and some studies have reported no increase in total or right-sided adenomas in this group.7 Given that access to health insurance and colonoscopy is lower among African Americans compared with Caucasians, a colonoscopy only policy might in some cases result in recommendation for a screening test that will be effectively unavailable and not ultimately completed. In addition, because screening tests tend to be more sensitive in high-risk populations than in lower-risk populations, the higher burden of disease in African Americans might make less invasive, potentially more widely available tests such as the fecal immunochemical test (FIT) more effective than they are for the general population. Moreover, survey research reports conflicting results regarding the preference of screening modalities in the African American population, with some studies showing a plurality prefer colonoscopy over fecal occult blood testing, others showing the opposite, and none reporting dominant preference for one test over the other.8,9 Until it is clear that all African Americans have access to and are ready to complete colonoscopy, a “best test is the one that gets done” philosophy might be prudent.
Overall, research on how to optimize screening rates, improve cancer treatment after diagnosis, and lower risk factors for African Americans is vital. In the meantime, gastroenterologists must focus on counseling African Americans regarding risk for CRC and optimizing uptake of screening.
Novel Potential Future Screening Programs
The Dallas-Fort Worth metroplex is a multicultural region enriched by patients speaking a variety of languages. Consequently, language barriers and cultural beliefs are a relevant aspect of care of patients in our local community. An ongoing clinical trial at University of Texas Southwestern by one of the authors (S.G.) might provide novel insights into strategies to improve participation of diverse patient populations in screening programs for CRC.
The program, funded by the Cancer Prevention and Research Institute of Texas, will randomly invite several thousand uninsured, unscreened patients served by the safety net health system for Tarrant County, TX to complete CRC screening. The target population is diverse: 29% African American and 23% Hispanic. Key features of the program include a study of whether mailed outreach accompanied by reminder phone calls (with Spanish language availability) improves screening rates over standard care. To determine whether test-specific participation varies among those selected for a mailed invitation, patients will be randomly selected to receive a mailed invitation to complete a free FIT or a free colonoscopy. Thus, the study will not only seek to improve screening for communities at high risk for poor CRC screening outcomes but also to determine whether response to interventions differs by ethnicity. For example, the study might show that Hispanics are more likely to complete FIT and less likely to complete colonoscopies (as has been suggested by prior survey research),8 or that when access to colonoscopy is enabled, this modality is acceptable on a large scale to populations at high risk for screening non-completion.
Conclusions
The unique characteristics of the courses of digestive diseases in our culturally diverse patients generate discussion points regarding patient management in these patients. The fact that difficult to treat patient populations, such as African Americans and Latinos, have a lower response rate to HCV treatments might indicate that such populations might require longer treatment courses or might be candidates for combination therapies with protease inhibitors or polymerase inhibitors. It is also possible that treatments might be individualized on the basis of an in-depth evaluation of genetic variation rather than more limited assessment of racial or ethnic phenotypes. For example, ILB28 genotype is better than race in predicting HCV treatment response and viral clearance.
In addition, the central role of gastroenterologists in the promotion and delivery of CRC screening requires that we consider these issues and work together to identify the best approach to reducing the public health burden of CRC on African Americans and Latinos. Promising approaches include use of early screening and patient navigators, although generalizability and costs of these approaches require further study. Demographic-based guidelines require a comprehensive approach that takes into account cultural, financial, and system barriers to screening to address obvious disparities in CRC outcomes.
The cardiology and primary care medical communities appear to be several steps ahead of us in digestive diseases in their incorporation of race and ethnicity into their management guidelines in cardiovascular diseases such as hypertension and congestive heart failure. For those of us who focus our practices in digestive diseases, it appears as if we too have sufficient evidence to incorporate specific management plans for our culturally and linguistically diverse patients and to support critical research to optimize care for these groups.
Funding
This work was supported in part by Cancer Prevention and Research Institute of Texas Grant PP100039 (S.G., PI).
Abbreviations used in this paper:
- BMI
body mass index
- CRC
colorectal cancer
- FIT
fecal immunochemical test
- HCV
hepatitis C virus
- SVR
sustained virologic response
Footnotes
Conflicts of interest
The authors disclose no conflicts.
References
- 1.Jeffers LJ. Treating hepatitis C in African Americans. Liver Int 2007;27:313–322. [DOI] [PubMed] [Google Scholar]
- 2.Rodriguez-Torres M, Jeffers LJ, Sheikh MY, et al. Peginterferon alfa-2a and ribavirin in Latino and non-Latino whites with hepatitis C. N Engl J Med 2009;360:257–267. [DOI] [PubMed] [Google Scholar]
- 3.Ge D, Fellay J, Thompson AJ, et al. Genetic variation in IL28B predicts hepatitis C treatment-induced viral clearance. Nature 2009;461:399 – 401. [DOI] [PubMed] [Google Scholar]
- 4.Rim SH, Seeff L, Ahmed F, et al. Colorectal cancer incidence in the United States, 19992004: an updated analysis of data from the National Program of Cancer Registries and the Surveillance, Epidemiology and End Results Program. Cancer 2009;115:1967–1976. [DOI] [PubMed] [Google Scholar]
- 5.Percac-Lima S, Grant RW, Green AR, et al. A culturally tailored navigator program for colorectal cancer screening in a community health center: a randomized, controlled trial. J Gen Intern Med 2009;24:211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lieberman DA, Holub JL, Moravec MD, et al. Prevalence of colon polyps detected by colonoscopy screening in asymptomatic black and white patients. JAMA 2008;300:1417–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Penn E, Garrow D, Romagnuolo J. Influence of race and sex on prevalence and recurrence of colon polyps. Arch Intern Med 2010; 170:1127–1132. [DOI] [PubMed] [Google Scholar]
- 8.DeBourcy AC, Lichtenberger S, Felton S, et al. Community-based preferences for stool cards versus colonoscopy in colorectal cancer screening. J Gen Intern Med 2008;23:169 –174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Palmer RC, Midgette LA, Mullan ID. Colorectal cancer screening preferences among African Americans: which screening test is preferred? J Cancer Educ 2010;25:577–581. [DOI] [PubMed] [Google Scholar]