Abstract
This study integrates two important developments, the concept of health lifestyles (which has focused on adults and adolescents) and the increased attention to early childhood. We introduce the concept of children’s health lifestyles, identifying differences from adult health lifestyles and articulating intergenerational transmission and socialization processes shaping children’s health lifestyles. Using the nationally representative Early Childhood Longitudinal Study-Birth Cohort (2001 – 2007; N ≈ 6150), latent class analyses identify predominant health lifestyles among U.S. preschoolers. Five distinct empirical patterns representing health lifestyles emerge, two capturing low and medium levels of overall risk across domains and three capturing domain-specific risks. Social disadvantage predicts children’s health lifestyles, but lower household resources and social disadvantage often explain these relationships. Across kindergarten measures of cognition, behavior, and health, preschool health lifestyles predict children’s development even after controlling for social disadvantage and concurrent household resources. Further research on health lifestyles throughout childhood is warranted.
Keywords: Early childhood, health lifestyles, ECLS-B, latent class analysis, life course
Researchers and policy makers recognize that health behaviors are often resistant to change. Seeking to understand this problem, some have begun focusing on health lifestyles (Cockerham 2005). These are defined as groups of interrelated health behaviors, rooted in social identities related to understandings of health, responsibility, and risk, that are shaped by knowledge and resources and that have important consequences for health and other life outcomes. Significant gaps in knowledge about health lifestyles remain. The empirical operationalization of health lifestyles lags behind theoretical development, and we know very little about health lifestyles prior to adulthood.
A focus on health lifestyles in the early life course has the potential to turn the typical approach to health behavior policies on its head. Interventions targeting young people’s health behaviors most frequently focus on influencing single behaviors, often with disappointing results. In contrast, a lifestyle approach acknowledges that health behaviors do not happen in a vacuum; rather, they co-occur in sets and influence one another. A health lifestyle approach to crafting social policy suggests that targeting the underlying lifestyle and associated identities may be more effective than focusing on a single behavior. This approach must first be informed by research on what young people’s health lifestyles look like and what their predictors and implications are. We address this gap to provide an empirical and theoretical knowledge base on which future research can build.
In this study, we use the only available nationally representative longitudinal survey of early childhood in the United States, the Early Childhood Longitudinal Study-Birth Cohort (Snow et al. 2009, U.S. Department of Education 2007), to analyze children’s health lifestyles. We look specifically at health lifestyles in the prekindergarten period, when children’s health behaviors and risks are still strongly patterned by their families yet when they begin to exercise some agency in diet, safety, and sleep. To our knowledge, this is the first study to theorize about or empirically analyze young children’s health lifestyles. We focus on three unanswered research questions. (1) Are there predominant empirical patterns of health behaviors and risks that reflect health lifestyles among preschoolers in the United States? We use various measures of behaviors and risk or protective factors to operationalize health lifestyles. Latent class analyses allow the optimal number of distinct empirical patterns representing lifestyles to arise from indicators identified in the data. (2) What social disadvantage factors and household resources predict children’s health lifestyles? We include predictors representing family background and concurrent household resources to estimate children’s likelihood of having different predominant health lifestyles. (3) How are health lifestyles in preschool related to children’s health and development at the start of the school transition? Our analyses consider multiple outcomes across the cognitive, behavioral, and health domains at kindergarten start. We estimate associations between health lifestyles and child outcomes after controlling for background factors and concurrent household resources.
BACKGROUND
An important theoretical development in the study of health disparities is the concept of health lifestyles, or predominant configurations of health behaviors and health risks in the population (Cockerham 2005). Health lifestyles are shaped by social factors such as socioeconomic status (SES), race/ethnicity, and gender, which affect a person’s motivations and means to adopt a particular lifestyle (Pampel, Krueger and Denney 2010). People also engage in health lifestyles because of their links to social identities and the social statuses and networks associated with those identities (Cockerham 2005, Stets and Burke 2000). The literature on health lifestyles has used data from adults, with the exception of a few studies of adolescents (Dodd et al. 2010, Frech 2012, Sinha 1992, Stefansdottir and Vilhjalmsson 2007).
A second, equally important advance in understanding health disparities has been the attention the life course theoretical perspective has brought to the influence of early life conditions on later life outcomes (Elder 1994). Researchers have documented the role of the “long arm of childhood” in influencing health and socioeconomic status in later life (Haas 2008, Hayward and Gorman 2004). Policy analyses have particularly pinpointed early childhood as an important target for future research because improvements in early childhood conditions pay off throughout the rest of the life course (Duncan, Ludwig and Magnuson 2007). In particular, the period preceding the transition to school is important. Children’s school readiness in terms of cognitive and behavioral outcomes and health is compromised by school start in many marginalized populations, such as low-SES children, many racial/ethnic minority groups, and children of teen parents (Crosnoe and Wildsmith 2011, Entwisle, Alexander and Olson 2004). Because these outcomes at the school transition are highly correlated with academic performance in middle and high school (Butler et al. 1985, Weller, Schnittjer and Tuten 1992), it is an important policy goal to reduce disparities in school readiness before they can take root during the school transition. Our study integrates these theoretical strands by introducing the concept of children’s health lifestyles and focusing on early childhood.
Children’s Health Lifestyles
Health lifestyles can be defined as “collective patterns of health-related behavior based on choices from options available to people according to their life chances” (Cockerham 2007:460). The concept is rooted in Weber’s idea of lifestyles as the interaction of life choices (agency) and life chances (structure), and it has been further developed by scholars such as Sobel (1981), Abel (1991), and Cockerham (2005). In Weber’s conceptualization, lifestyles are not associated with individuals, but with status groups of people with similar backgrounds (Cockerham 2005), and choosing the lifestyle associated with a status group communicates one’s group identity. Some research has expanded the definition of health lifestyles to include factors such as understandings of what good health means, norms about health, and policy environments (Krueger, Bhaloo and Rosenau 2009). Individuals’ approaches towards health behaviors tend to cluster, with people who behave in one healthy or unhealthy way often behaving in others (Laaksonen, Prättälä and Lahelma 2002). Past research has found that people from higher social classes often have healthier lifestyles (e.g., Blaxter 1990, Snead and Cockerham 2002). Cockerham (2000) found that not only class, but other social characteristics such as gender and age are linked to health lifestyles.
The idea of health lifestyles among school-aged children (Kennedy and Floriani 2008, Sinha 1992) and adolescents (Nutbeam, Aaro and Catford 1989) has been raised in past research but not fully theoretically developed as separate from adult health lifestyles. Schuster and colleagues (2004) and Terre, Drabman, and Meydrech (1990) found that a variety of health behaviors varied by individual characteristics and were correlated in samples of preteens and teenagers, but they did not examine health lifestyles. Previous work has not studied or theorized about health lifestyles in early childhood. The life course perspective suggests the importance of theoretical attention to differences by life stage. Indeed, previous research on adolescents and adults has found that health behaviors and the composition of health lifestyles change over the life course (Backett and Davison 1995, Frech 2012). This insight is particularly important when thinking about health lifestyles in early childhood. Here, we develop the concept of health lifestyles as it applies to young children, articulating similarities and differences between adults’ health lifestyles and those of children. Some of the behaviors and risks considered when studying adults must be altered to be applicable for young children (e.g., smoking becomes exposure to secondhand smoke), others remain the same (e.g., a healthy diet), and still others only apply to one of these two age groups (e.g., using a car seat for children or drinking alcohol for adults).
There are some clear differences between conceptualizing health lifestyles for adults versus young children. Children’s health lifestyles are a mixture of parents’ and children’s agency, structural constraints, and identities, with parents’ influence waning and children’s influence growing with age. Thus, we can talk about children starting with a received health lifestyle and gradually transitioning to an achieved health lifestyle by adulthood. For these reasons, we assert that health lifestyles are part of the intergenerational transmission of social disadvantage from parents to children (Wickrama et al. 1999), and as such, they are a blend of parents’ behaviors (such as smoking, or ensuring automobile safety) and children’s behaviors (such as nutrition and sleep). Health theorists are interested in understanding how families shape children’s protective and risky health behaviors (e.g., Christensen 2004). Generally parents are making decisions for children, but four-year-olds have some power over what they eat, when they sleep, and what free time activities they engage in. DeGenna and colleagues (2006) emphasize that intergenerational links in health behaviors can occur through direct social learning from parents or from exposure to social environments that encourage similar behaviors as those of parents. Indeed, Abella and Heslin (1984) found that parents’ and children’s health behaviors were strongly linked, even though adult children did not consciously acknowledge that their parents had influenced them in this way. Wickrama and colleagues (1999) documented links between mothers’ and their teenage children’s health risk behaviors. Hardie and Landale (2013) found that latent classes representing maternal health and social disadvantage predicted children’s health. We suggest that health lifestyles are intergenerationally transmitted through the direct impacts of parents’ health lifestyles on children (e.g., smoking or family violence), through behaviors that affect children and parents alike (e.g., cooking nutritious dinners or having a smoke detector), and through behaviors that are unique to children but at least somewhat determined by parents (e.g., children’s sleep patterns or car seat use).
Influences on and Implications of Children’s Health Lifestyles
Besides identifying health lifestyles among young children, we investigate their predictors and implications. For the former, we focus on social disadvantage and concurrent resources. As the life course concept of “linked lives” suggests (Elder 1994), social disadvantage influences parents’ health lifestyles, cultural capital, and available resources (Bourdieu 1986, Snead and Cockerham 2002), leading to children’s health lifestyles. We expect family resources to be another key influence on children’s health lifestyles, and as suggested above, they may help explain why social disadvantage patterns lifestyles. Resources provide parents with the material means, knowledge, and social support to make positive changes in their children’s health lifestyles (Link and Phelan 1995).
We also expect young children’s health lifestyles to be linked to their early development. Our outcomes are measured at the start of kindergarten, which marks the beginning of the transition to school. This period affects children’s school trajectories for years afterward (Duncan et al. 2007). In particular, we examine outcomes in the cognitive, behavioral, and health domains because they have been shown to be interrelated and important both for a successful transition to school and for later outcomes (Crosnoe 2006, Entwisle, Alexander and Olson 2004, Halonen et al. 2006, Weller, Schnittjer and Tuten 1992). We expect health lifestyles characterized by consistent overall levels of risk across different health behaviors to influence each of these outcomes. In contrast, health lifestyles characterized by specific health risks may disproportionately predict different outcome domains. For example, witnessing violence may be most related to socioemotional behavior and secondhand smoke exposure to health.
Even more than adults’ health lifestyles, those of young children may also have important long-term consequences. Not only are they likely to shape future health and development for the rest of the life course, but they represent a process of socialization of children into some health behaviors and not others. For example, nutritious foods eaten regularly in early childhood may become “comfort foods” in adulthood, resulting in long-term health benefits. Cockerham (2005) views past socialization as key for understanding the health lifestyle choices people make from among available options.
Measuring Children’s Health Lifestyles
Researchers seeking to operationalize health lifestyles grapple with two major issues. The first is how to measure health lifestyles in a population empirically, rather than assuming that they exist or imposing preconceived behavior patterns. This has been acknowledged as a challenge (Abel 1991, Cockerham 2005), and analytic strategies have tended to lag behind theoretical developments. Some studies have used techniques such as cluster analysis, factor analysis, or others to allow patterns of lifestyle behaviors to emerge from the data, but have not tested hypotheses about their causes or consequences (e.g., Abel 1991, Burke et al. 1997, Dodd et al. 2010, Patterson, Haines and Popkin 1994). Others have focused on specific features of health lifestyles to test hypotheses but not examined how they covary or cluster in a population (e.g., Cockerham 2007, Reijneveld 1998). In contrast, latent class analysis allows researchers both to identify empirical patterns of lifestyle indicators that emerge from the data and test hypotheses about their causes and consequences. Krueger and colleagues (2009) and Laska and colleagues (2009) have used this method to examine health lifestyles among adults and college students, respectively, but neither used the latent classes to analyze causes and consequences of health lifestyles.
The second important empirical issue is deciding which indicators of health lifestyles to use. Researchers studying adult health lifestyles have often worked with limited behavioral indicators such as diet, exercise, and substance use, which has been identified as a concern (Stefansdottir and Vilhjalmsson 2007). With ECLS-B data we are able to incorporate a wide variety of indicators within the domains of diet, sleep, secondhand smoke exposure, safety, and exposure to violence. Some of these domains are direct measures of health behaviors, while others (such as safety) represent parents’ behavioral management of contextual risks in order to keep the child healthy. Each domain has been linked to children’s development and health (Butz et al. 2011, Cook et al. 2006, Dellinger and Kresnow 2010, Du et al. 2010, Durbin et al. 2005, Glewwe, Jacoby and King 2001, Hemenway 2011, King 2012, Koulouglioti, Cole and Kitzman 2008, Lin et al. 2011, Lucas 1998, Yount, DiGirolamo and Ramakrishnan 2011).
DATA AND METHODS
Data
Our data source is the Early Childhood Longitudinal Study-Birth Cohort (ECLS-B), which followed a nationally representative sample of about 10,600 children born in 2001 from infancy through the fall of kindergarten (U.S. Department of Education 2007).1 No other nationally representative U.S. study has tracked children through these first years of life using parent interviews and direct assessments. All 2001 births registered in National Center for Health Statistics vital statistics were eligible, and the sample was drawn using a clustered, list frame design. Children were sampled from 96 counties/county groups. Children with mothers below age 15 at their birth were excluded from data collection for confidentiality reasons.
This study used data from all waves of the survey, conducted when the children were about 11, 24, and 52 months old (typically the fall before the start of kindergarten), and in the fall of their kindergarten year at an average of 66 months old (thus, most children were interviewed in fall 2006 but some were interviewed in fall 2007). The primary parent, who was almost always the biological mother, was interviewed in person. Because of budgetary constraints, the kindergarten wave included a random subsample of about 85% of the children that had completed the parent interview of the preschool wave, though all American Indian children who completed either the 2-year or preschool wave were included (Snow et al. 2009). The weighted response rates for the parent interview were 74, 93, 91, 92, and 93 respectively for each wave. Since some covariates apply to biological mothers, we further restricted our sample those whose biological mothers completed the parent interview. The 8900 children eligible for latent class analysis (cases with missing data were retained) had valid wave 3 weights and clustering information. Because latent classes subsequently predicted kindergarten outcomes, all subsequent analyses restricted eligibility to children with valid wave K weights and clustering information whose biological mother completed the wave K parent interview. Multiple imputation was used to retain the approximately 6450 eligible cases.2 All analyses adjusted for complex survey design using probability weights, and accounting for clustering in SAS (for latent classes) and replication weights in Stata (for other analyses).
Measures
Health Lifestyle Indicators.
We used a variety of indicators that identified predominant health lifestyles among prekindergarten children in our latent class analyses, representing five domains of health behaviors and health risks. Variables included in the latent class analysis were all measured at wave 3 (52 months old). All measures are weighted equally because we are interested in identifying predominant profiles of health behaviors rather than comparing the relative influences of different indicators. The first domain was diet. Household food security was constructed by ECLS-B, comparing households with uncertain food provision to those without. The other nutrition indicators measured consumption of specific foods within the last week, some beneficial for children’s health and some detrimental. Children who drank milk at least once per day were coded as 1, with less coded as 0. Soda or sugary drinks (including sports drinks and fruit drinks that were less than 100% juice), fast food (meals or snack food from a fast food restaurant with no wait service), sweet snacks (such as cake, brownies, ice cream, candy, and cookies), and salty snacks (chips, popcorn, crackers, etc.) were all coded similarly to milk, with intake at least once per day coded as 1 for each separate variable, and less coded as 0. Per nutritional guidelines, fruit and vegetable intake per day was combined, with children consuming 5 or more servings per day coded as 1 and those eating fewer coded as 0.
The second domain was children’s average bedtime and average number of hours of sleep. Inadequate sleep was coded as 1 if the child slept less than 10 hours per night on average and 0 for 10 or more hours (NHLBI 2012). Late bedtime was coded as 1 if the child fell asleep after 10 p.m. on average and 0 for earlier (Simpkin et al. 2014). The third domain, secondhand smoke exposure, was coded 1 if the child had a family member who smoked inside the home and coded and 0 if there were no smokers in the home or smokers only smoked outside the house.
The fourth domain, safety, was represented by five indicators. A smoke detector measure was coded as 1 if there was a working smoke detector in the home all the time, and 0 if there was no smoke detector or it was not always in working order. Children were coded as 1 if they did not always wear a helmet when engaging in activities such as roller skating and biking and 0 if they always wore a helmet or did not ride a bike or have skates. Car seat use and riding in the back seat of cars were coded the same way. The presence of an unlocked gun in the child’s home was coded as 1, with no gun or a consistently locked gun coded as 0.
The final domain, violence, was represented by two indicators. Children who had witnessed any violent act in the home (such as physical fighting, destruction of property, or other violence) were coded as 1 and all others as 0. Finally, children whose mothers reported they were the victims of violence in the home in the last year were coded as 1 and all others as 0.
Outcomes.
We used four outcome variables to capture different facets of children’s well-being. We looked at kindergarten indicators of reading, math, behavior, and health. Kindergarten information was taken from either wave 4 or wave 5, depending on when the survey indicated the child first enrolled in kindergarten. The two cognitive outcomes (early reading and math) came from one-on-one child assessments adapted from reputable assessment batteries developed for other child development studies or for the ECLS-B. See Nord and colleagues (2006) and Snow and colleagues (2009) for more information on these and other assessments. Interviewers administered early reading and math assessments adapted from several reputable assessment batteries developed for other large studies of preschoolers, such as the Peabody Picture Vocabulary Test, the Preschool Comprehensive Test of Phonological and Print Processing, the PreLAS® 2000, the Test of Early Mathematics Ability-3, and sister study Early Childhood Longitudinal Study-Kindergarten Cohort (ECLS-K).3 Early reading was assessed by a 35-item test covering age-appropriate areas such as phonological awareness, letter recognition and sound knowledge, print conventions, and word recognition (ECLS-B-reported reliability=0.84). Early math was assessed in two stages, routed after the first stage depending on the child’s score and evaluating counting, number sense, operations, geometry, pattern understanding, and measurement (ECLS-B-reported reliability=0.89). We standardized the scale scores for the cognitive, reading and math evaluations.
The socioemotional behavior measure was based on parent reports. Children’s behavior was captured by a standardized continuous variable, constructed from an index of 24 items in which the parent was asked how frequently the child acted in certain ways, using a 5-point scale ranging from “never” to “very often” (Cronbach’s alpha=0.86). The items were drawn from the Preschool and Kindergarten Behavior Scales—Second Edition, the Social Skills Rating System, and the Family and Child Experiences Study, as well as new questions developed for ECLS-B. The questions included items such as how often the child shares belongings or volunteers to help other children, how often the child is physically aggressive or acts impulsively, and how well the child pays attention. Negative behaviors were reverse coded so that higher behavior scores represented more positive behavior.
For a global indicator of health, we used the primary parent’s report of the child’s health status. Although there is less variation in responses to this measure than emerges later in life, subjective health ratings are meaningful and can capture aspects of health that are otherwise difficult to operationalize (Currie and Stabile 2003, Idler and Benyamini 1997). We coded those reporting very good or excellent health as 1, and those in good, fair, or poor health as 0.4
Independent Variables.
Analyses included several control variables, including the study child’s age at the kindergarten wave, which could affect scores on outcomes. An ECLS-B-constructed measure of child gender (with female as the reference category) was a second control. Other control variables measured prenatal conditions and birth outcomes. Prenatal care was represented in a dichotomous variable, with those either not receiving prenatal care in the first trimester or not receiving care at all coded 1 and those receiving care in the first trimester coded 0. Birth weight, constructed by ECLS-B, was coded as moderately low (<2500g and ≥1500g) or very low (<1500g) compared to normal (≥2500g). A measure indicated whether the biological mother ever drank at least one alcoholic drink per week during the third trimester of pregnancy. Finally, maternal depression symptoms at wave 1, measured by the Center for Epidemiologic Studies Depression (CES-D) scale, were included.
Several variables captured backgrounds of social disadvantage. Child race was represented by four mutually exclusive categories (non-Hispanic White, non-Hispanic Black, Hispanic, and other race which included Asian/Pacific Islander, Native American/Alaska Native, and multiracial children) constructed by the ECLS-B. A variable indicated whether or not the mother was foreign born. Teen parent status indicated whether or not the child’s biological mother and/or father was under the age of 20 at the time of birth. We used each parent’s own report when available.
We included wave 3 (concurrent with health lifestyle measurement) variables capturing a variety of financial, material, and social resources in the household, as well as activities that require or contribute resources. We measured three dimensions of socioeconomic status: income, education, and wealth. We used an income-to-needs ratio, which coded ECLS-B-constructed household income as a percentage of the federal poverty threshold for the appropriate household size. The mother’s educational attainment, constructed by the ECLS-B, was a continuous indicator reflecting total years of education, recoded from a categorical measure. A scale of household assets reflected the wealth of the household. The following dichotomous indicators were averaged to create a proportion of assets: whether or not the household owned a car, had stocks or investments, had a checking or savings account, owned their residence, and was not in subsidized housing (Cronbach’s alpha = 0.71).
A dichotomous variable indicated whether the household had received food stamps in the last year. The mother’s work status was reflected by three categories: working full-time (40 or more hours per week), working part-time (less than 40 hours), and not in the labor force. Similarly, the mother’s school enrollment was coded from her report as full-time, part-time, or none. An indicator of time spent in nonparental child care was coded as none, part-time (1–29 hours per week), or full-time (30 or more hours per week). The monthly cost of nonparental child care was a continuous measure. We also included measures of social resources. Other measures indicated the presence of specific categories of people in the household: a biological or social father, the number of other children in the home besides the study child, and any coresident grandparent. A dichotomous variable measured whether the mother received advice about parenting since the last wave.
Analyses
Latent classes.
Because we were interested in identifying prevalent health lifestyles in early childhood, we conducted latent class analyses using PROC LCA in SAS. Latent class analysis differs from factor analysis in that it uses dichotomous, not continuous, indicators and assumes that there are underlying discrete groups, or “classes,” of respondents. The underlying groups identified are a function of the indicators used in the latent class analysis, so they can be likened to an empirical “snapshot” of underlying patterns that may or may not reflect a more durable substantive phenomenon. To assess the robustness of our findings, we conducted latent class analyses with several variations in the indicators and the number of classes. Latent classes were created from the health lifestyle indicators described above, using the full eligible sample (N ≈ 8900). Each case was assigned a probability of membership in each class (similar to a factor loading), and population shares were calculated for each class. We chose the class with the highest probability of membership and assigned it to each child. See Table 1 for item response probabilities and population shares for the analysis sample.
Table 1.
Item response probabilities for health lifestyle indicators used in latent class analysis
| Variable | Consistently positive (40%; N ≈ 2950) | Middle of the road (30%; N ≈ 1650) | Food insecurity/ violence/ smoking (3%; N ≈ 150) | Nutrition/ sleep problems (23%; N ≈ 1350) | Safety problems (4%; N ≈ 300) |
|---|---|---|---|---|---|
| Health lifestyle indicators | |||||
| Household food insecurity | 0.04 | 0.33 | 0.51 | 0.35 | 0.25 |
| Milk one time per day | 0.89 | 0.80 | 0.90 | 0.85 | 0.84 |
| Sugary drink one time per day | 0.11 | 0.27 | 0.48 | 0.65 | 0.31 |
| Fruit/vegetables five per day | 0.94 | 0.86 | 0.92 | 0.95 | 0.92 |
| Fast food one time per day | 0.03 | 0.02 | 0.09 | 0.27 | 0.07 |
| Sweet snack one time per day | 0.44 | 0.20 | 0.53 | 0.86 | 0.37 |
| Salty snack one time per day | 0.20 | 0.06 | 0.34 | 0.79 | 0.28 |
| Inadequate sleep | 0.29 | 0.48 | 0.33 | 0.49 | 0.42 |
| Bedtime after 10 pm | 0.00 | 0.07 | 0.01 | 0.07 | 0.05 |
| Smoking in house | 0.01 | 0.18 | 0.36 | 0.22 | 0.23 |
| Smoke detector in house | 0.98 | 0.88 | 0.87 | 0.83 | 0.33 |
| Wears helmet when needed | 0.60 | 0.39 | 0.47 | 0.39 | 0.36 |
| Car seat used at all times | 0.97 | 0.82 | 0.74 | 0.74 | 0.03 |
| In back seat at all times | 0.99 | 0.96 | 0.92 | 0.90 | 0.03 |
| Unlocked gun in house | 0.07 | 0.07 | 0.04 | 0.06 | 0.09 |
| Witness of violent act | 0.02 | 0.04 | 0.99 | 0.04 | 0.12 |
| Victim of violent act | 0.00 | 0.01 | 0.49 | 0.00 | 0.02 |
Source: Early Childhood Longitudinal Study-Birth Cohort, 2001–2007. N ≈ 6450.
Notes: All variables are coded 1 = yes, 0 = no.
To determine the appropriate number of classes, we used several common fit measures, including G-squared, the Akaike Information Criterion (AIC), and the Bayesian Information Criterion (BIC, which rewards more parsimonious models), to make comparisons across solutions ranging from 1 to 10 classes. G-squared and AIC identified substantial fit improvements until 5 classes, then only marginal improvements until 10 classes. The BIC was lowest at 8 classes but showed little improvement starting at 5 classes. Thus, we chose the 5-class solution as the most parsimonious class with a good fit. It was also substantively sound with distinct, interpretable classes. Another approach is to calculate the average probability of respondents being assigned to the latent class for which they have the highest probability of membership. A mean closer to 1 indicates that class assignment is not ambiguous (a better fit). A mean closer to 0 lower average indicates that respondents might feasibly have been assigned to multiple classes (a poorer fit). The average probability for our 5-class solution was 0.77, suggesting quite distinctive classes and better fit.
Other analyses.
We analyzed descriptive information in Table 2, reporting all variables’ means overall and for each latent class, including significance tests comparing each class to the “consistently positive” class. Two sets of multivariate analyses were conducted. The first (not shown) predicted class membership on the basis of control variables, social disadvantage, and concurrent household resources. These analyses allowed us to understand how social factors are related to children’s health lifestyles. The second set predicted children’s four kindergarten outcomes on the basis of their health lifestyles. We included control variables, social disadvantage, and concurrent household resources to calculate the adjusted relationship between each health lifestyle indicator and each outcome. Predicted values/probabilities illustrated the relative strength of these relationships for an average child.
Table 2.
Weighted means of independent variables overall and by health lifestyle class
| Variable | Overall | Consistently positive (40%) | Middle of the road (30%) |
Food insecurity/ violence/smoking (3%) | Nutrition/sleep problems (23%) | Safety problems (4%) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Kindergarten outcomes (wave K) | ||||||||||
| Reading | −0.01 | 0.23 | ‒0.18 | *** | ‒0.36 | *** | ‒0.30 | *** | 0.01 | ** |
| Math | 0.03 | 0.29 | ‒0.13 | *** | ‒0.23 | *** | ‒0.31 | *** | ‒0.01 | *** |
| Positive behavior | 0.09 | 0.25 | ‒0.01 | *** | ‒0.27 | *** | ‒0.10 | *** | 0.05 | * |
| Very good/excellent health° | 0.87 | 0.92 | 0.82 | *** | 0.84 | * | 0.80 | *** | 0.91 | |
| Social Disadvantage and Controls | ||||||||||
| Child age in months | 68.13 | 68.08 | 68.29 | 68.32 | 67.98 | 68.40 | ||||
| Male° | 0.51 | 0.50 | 0.54 | + | 0.52 | 0.48 | 0.50 | |||
| Late/no prenatal care° | 0.08 | 0.04 | 0.10 | *** | 0.18 | *** | 0.12 | *** | 0.14 | *** |
| Birth weight (normal) | 0.93 | 0.94 | 0.91 | ** | 0.93 | 0.91 | ** | 0.93 | ||
| Low | 0.06 | 0.05 | 0.07 | ** | 0.05 | 0.07 | ** | 0.06 | ||
| Very low | 0.01 | 0.01 | 0.01 | 0.01 | 0.01 | 0.02 | ||||
| Drank during pregnancy° | 0.01 | 0.02 | 0.01 | * | 0.01 | 0.01 | * | 0.00 | ** | |
| Mother depression scale at Wave 1 | 1.33 | 1.26 | 1.41 | *** | 1.42 | * | 1.38 | *** | 1.44 | *** |
| Race/Ethnicity (White)° | 0.53 | 0.65 | 0.43 | *** | 0.43 | *** | 0.42 | *** | 0.50 | *** |
| Black | 0.14 | 0.07 | 0.18 | *** | 0.23 | *** | 0.21 | *** | 0.21 | *** |
| Hispanic | 0.25 | 0.21 | 0.31 | *** | 0.28 | 0.29 | *** | 0.16 | ||
| Other Race | 0.07 | 0.06 | 0.08 | * | 0.06 | 0.07 | 0.13 | *** | ||
| Biological mother foreign born | 0.20 | 0.19 | 0.22 | + | 0.17 | 0.23 | * | 0.11 | * | |
| Either parent a teen parent | 0.12 | 0.06 | 0.16 | *** | 0.19 | *** | 0.17 | *** | 0.14 | *** |
| Household Resources (Wave 3) | ||||||||||
| Income (proportion of poverty line) | 2.88 | 3.97 | 1.95 | *** | 1.42 | *** | 1.92 | *** | 2.47 | *** |
| Mother’s years of education | 13.44 | 14.47 | 12.77 | *** | 12.33 | *** | 12.25 | *** | 12.89 | *** |
| Asset scale | 0.71 | 0.82 | 0.63 | *** | 0.49 | *** | 0.59 | *** | 0.68 | *** |
| Household received food stamps | 0.25 | 0.09 | 0.36 | *** | 0.60 | *** | 0.41 | *** | 0.40 | *** |
| Mother’s paid work (none) | 0.40 | 0.37 | 0.40 | 0.48 | * | 0.47 | *** | 0.44 | + | |
| Part-time | 0.25 | 0.30 | 0.22 | ** | 0.28 | 0.20 | *** | 0.22 | * | |
| Full-time | 0.34 | 0.33 | 0.38 | * | 0.24 | 0.34 | 0.34 | |||
| Mother’s school enrollment (none) | 0.88 | 0.89 | 0.86 | 0.86 | 0.89 | 0.80 | ** | |||
| Part-time | 0.08 | 0.07 | 0.08 | + | 0.10 | 0.06 | 0.12 | + | ||
| Full-time | 0.05 | 0.04 | 0.05 | * | 0.03 | 0.05 | 0.09 | * | ||
| Cost of child care/month | 159.11 | 224.70 | 113.60 | *** | 59.61 | *** | 92.89 | *** | 115.92 | *** |
| Hours of child care (none) | 0.20 | 0.15 | 0.24 | *** | 0.26 | * | 0.25 | *** | 0.20 | + |
| Part-time (1–29) | 0.40 | 0.47 | 0.34 | *** | 0.29 | ** | 0.33 | *** | 0.37 | * |
| Full-time (≥30) | 0.40 | 0.38 | 0.42 | * | 0.45 | 0.42 | 0.42 | |||
| Residential father (biological) | 0.73 | 0.86 | 0.63 | *** | 0.41 | *** | 0.63 | *** | 0.69 | *** |
| None | 0.06 | 0.04 | 0.08 | *** | 0.06 | 0.07 | ** | 0.03 | ||
| Social father | 0.21 | 0.10 | 0.29 | *** | 0.54 | *** | 0.30 | *** | 0.27 | *** |
| # of household members under 18 | 2.45 | 2.31 | 2.49 | *** | 2.76 | ** | 2.63 | *** | 2.56 | ** |
| Grandparent in residence° | 0.21 | 0.15 | 0.24 | *** | 0.36 | *** | 0.27 | *** | 0.26 | ** |
| Mother received parenting help° | 0.09 | 0.09 | 0.08 | 0.15 | + | 0.08 | 0.12 | |||
Source: Early Childhood Longitudinal Study-Birth Cohort, 2001–2007. N ≈ 6450.
Notes: Analyses accounted for complex survey design. Reference categories are in parentheses. 1 = yes.
p<.10
p<.05
p<.01
p<.001 two-tailed design-based F tests comparing children in each latent class with those in the “consistently positive” group.
RESULTS
Question 1: What Are Young Children’s Predominant Health Lifestyles?
Table 1 presents the five predominant empirical patterns representing health lifestyles (latent classes), their share of the sample, and the mean levels of each health lifestyle indicator for each class. The first two classes were differentiated based on children’s average levels of risk across all domains. Class 1, labeled consistently positive, comprised 40% of the sample. Table 1 shows that children in this class experienced favorable conditions relative to most of their peers across nearly all indicators and domains, including nutrition, sleep, second-hand smoke, safety, and violence. Class 2, which we call middle of the road (30% of children), were neither the best nor the worst group for any health lifestyle indicator or domain except nutrition. In this domain their profile was inconsistent: They had average food insecurity levels, the lowest milk and produce consumption, and the lowest fast food and unhealthy snack consumption.
The last three classes were differentiated by a particular domain of high risk. Class 3, food insecurity/violence/smoking, at 3% of the sample, was the smallest class but had a distinct profile. More than half of these children lived in households that experienced food insecurity, 36% lived with a smoker, 49% had been a victim of violence in the last year, and 99% had witnessed violence in the household. In the other health lifestyle domains, they fell in the middle. Class 4, nutrition/sleep problems, comprised 23% of the sample. These children had fairly high levels of food insecurity in their households, as well as the highest unhealthy food consumption (each day, two thirds drank sugary drinks, 27% ate fast food, and the vast majority ate sweet and salty snacks). Children in this latent class also experienced the highest levels of inadequate nighttime sleep (49% of children) and late bedtimes (7%). In other domains they fell in the middle. Finally, we labeled class 5 safety problems (4% of the sample). These children were fairly typical in the other domains, but they were the most problematic in terms of physical safety. For example, just 33% had a smoke detector in their home, and 97% rode in cars without a car seat at times. Thus, these five classes have distinct profiles and may have different implications for children’s development and health.
Question 2: Are Social Disadvantage and Household Resources Related to Health Lifestyles?
Descriptive statistics reported in Table 2 (all significance test are design-based F tests to account for complex survey design and are compared to “consistently positive”) show that preschoolers’ predominant health lifestyles are strongly patterned by social disadvantage and household resources. Race/ethnicity was the most consistent predictor among the social disadvantage factors. Non-Hispanic White children were significantly overrepresented in the “consistently positive” class compared to all others, whereas Black children were significantly overrepresented in all other classes compared to “consistently positive” (proportions ranged from 7% in “consistently positive” to 23% in “food insecurity/violence/smoking”). Hispanic children were significantly overrepresented in the “nutrition/sleep problems” and “middle of the road” classes. Children from other racial groups were significantly overrepresented in the “safety problems” and “middle of the road” classes. Children of foreign-born mothers were underrepresented in the “safety problems” class and overrepresented in “nutrition/sleep problems.” Children with a teen parent were significantly overrepresented in all classes compared to “consistently positive.”
Resource patterns are associated as expected with children’s health lifestyles. For all measures of socioeconomic status (maternal educational attainment, household income as a proportion of the federal poverty line, and assets), children in the “consistently positive” class had the highest levels, followed by “safety problems,” with “middle of the road,” “food insecurity/violence/smoking,” and “nutrition/sleep problems” having the lowest levels. Socioeconomic differences were stark. For example, children in the “food insecurity/violence/smoking” class had 12.3 years of maternal education on average and a household income 1.4 times the poverty line, while those in the “consistently positive” class had 14.5 years of maternal educational attainment and income 4 times the poverty line. Similar patterns were found for food stamp receipt, the number of children and grandparents in the household, no maternal employment, and less money spent on child care. Children in the “food insecurity/violence/smoking” class were the least likely to be living with their biological father (41% compared to 86% for “consistently positive”) and the most likely to live with a social father.
Supplementary models (not shown) combined all Table 2 predictors of children’s health lifestyles in multinomial logistic regression models, comparing each class to “consistently positive.” We estimated two models, the first with background factors and control variables and the second introducing household resources. Thus, we could assess how much resource differences explained the relationships of social disadvantage factors with different health lifestyles. Findings generally echoed bivariate results from Table 2, but household income did not significantly predict the likelihood of belonging to any latent class compared to “consistently positive” except “middle of the road” (the coefficient was negative). Importantly, significant disparities by race/ethnicity and teen parent status were eliminated or substantially reduced by introducing household resources.
Question 3: Do Children’s Health Lifestyles Predict Their Development and Health?
Descriptive analyses presented in Table 2 show stark disparities in children’s outcomes across different health lifestyles. The lifestyle associated with the most favorable outcomes in all domains of development and health was the “consistently positive” class, followed by “safety problems” for all four outcomes. The most unfavorable outcomes were split evenly between the “nutrition/sleep problems” (lowest on early math and health) and “food insecurity/violence/smoking” (lowest on early reading and behavior) classes. The size of these differences was substantial, at between 0.5 and 0.6 standard deviations for reading, math, and behavior and a 12-percentage-point difference for child health. These descriptive findings suggest that health lifestyles may be important for children’s health and development, but multivariate analysis is needed to ascertain whether health lifestyles matter after accounting for controls, social disadvantage, and household resources.
Table 3 reports these results. We estimated ordinary least squares regression models for the continuous outcomes (reading, math, and behavior) and binary logistic regression models for parent-reported health status. The baseline model predicted outcomes based on child age and each health lifestyle class compared to “consistently positive,” the second model added control and social disadvantage variables, and the third model added concurrent household resources. All models’ fit was a significant improvement over the null model (design-based F tests). In model 1, all lifestyle classes were negatively related to all four child outcomes compared to the “consistently positive” class. The sole exception was the lack of a significant relationship between the “safety problems” class and child health. Household resources were an important explanation for all or part of the disparities experienced by children: Each of these significant relationships was at least partially explained either by the introduction of background factors, controls or by the addition of household resources. But most significant relationships between health lifestyles and child outcomes remained, all in the expected direction, after introducing these covariates.
Table 3.
Summary of coefficients from linear regression and binary logistic regression analyses predicting children’s kindergarten outcomes (compared to “consistently positive” class)
| Model 1: Baseline model | Model 2: Add disadvantage/ controls | Model 3: Add household resources | ||||
|---|---|---|---|---|---|---|
| Reading score | ||||||
| Middle of the road | −0.42 | *** | −0.33 | *** | −0.11 | ** |
| Food security/violence problems | −0.60 | *** | −0.49 | *** | −0.14 | |
| Nutrition/sleep problems | −0.52 | *** | −0.43 | *** | −0.15 | *** |
| Safety problems | −0.24 | ** | −0.20 | * | 0.02 | |
| Math score | ||||||
| Middle of the road | −0.44 | *** | −0.30 | *** | −0.08 | * |
| Food security/violence/smoking | −0.54 | *** | −0.38 | *** | −0.05 | |
| Nutrition/sleep problems | −0.60 | *** | −0.45 | *** | −0.19 | *** |
| Safety problems | −0.32 | *** | −0.25 | * | −0.02 | |
| Positive behavior | ||||||
| Middle of the road | −0.26 | *** | −0.23 | *** | −0.14 | ** |
| Food security/violence/smoking | −0.53 | *** | −0.52 | *** | −0.37 | ** |
| Nutrition/sleep problems | −0.35 | *** | −0.34 | *** | −0.24 | *** |
| Safety problems | −0.20 | ** | −0.21 | ** | −0.13 | + |
| Very good/excellent health | ||||||
| Middle of the road | −0.92 | *** | −0.76 | *** | −0.60 | *** |
| Food security/violence/smoking | −0.76 | * | −0.65 | * | −0.47 | |
| Nutrition/sleep problems | −1.05 | *** | −0.89 | *** | −0.67 | *** |
| Safety problems | −0.08 | 0.08 | 0.08 | |||
Source: Early Childhood Longitudinal Study-Birth Cohort, 2001–2007. N ≈ 6450.
Notes: Multivariate OLS regression (for reading, math, and behavior) and binary logistic regression (for health, chronic illness, and asthma) analyses accounted for complex survey design. Baseline adjusted for child age, each model builds on the previous one.
p<.10
p<.05
p<.01
p<.001; two-tailed tests.
In the final model of Table 3, the “middle of the road” and “nutrition/sleep problems” classes predicted significantly lower early reading and math scores compared to the “consistently positive” class. The largest of these relationships was for “nutrition/sleep problems,” with a difference of 0.2 standard deviations for math.5 Every class was significantly and negatively related to behavior scores compared to “consistently positive” (for “safety problems,” p<.10). The most negative relationship with behavior was for the “food insecurity/violence/smoking” group, with a difference of 0.37 standard deviations. Children in the “middle of the road” class were 45% less likely, and those in the “nutrition/sleep problems” class were 49% less likely, to be reported in very good or excellent health compared to those in the “consistently positive” group. For every outcome, then, children’s preschool health lifestyles predict their development and health at the start of the school transition after accounting for a variety of controls, social disadvantage measures, and household resources.6
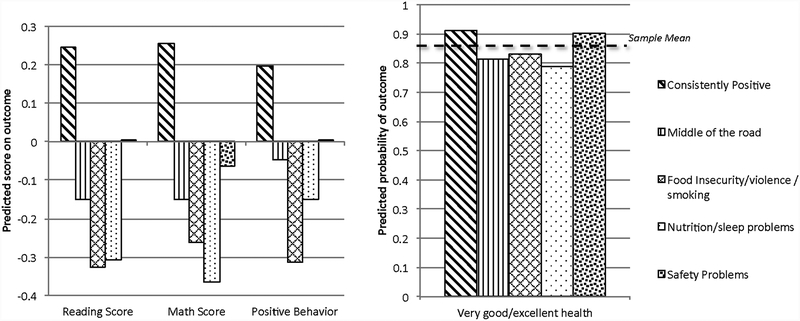
Figure 1 illustrates these significant relationships using predicted values/probabilities for each outcome. These predictions were estimated using the full model (Table 3, Model 3) for a hypothetical kindergartner who had the sample’s mean values for all variables except the health lifestyle indicators. The three continuous outcomes were standardized with a mean of 0, and the sample mean is indicated in the figure for the dichotomous outcome. We can see that typical kindergartners who were in the “consistently positive” group had considerably more favorable outcomes than the sample mean across all four outcomes. Although the “safety problems” class predicted lower behavior scores compared to “consistently positive” in Table 3 (p<.10), the figure shows that the hypothetical “safety problems” child was actually near or above the sample mean for all outcomes. This health lifestyle, while striking in its degree of compromised safety behaviors, does not appear to threaten children’s outcomes substantially. In contrast, the “middle of the road,” “nutrition/sleep problems,” and “food insecurity/violence/smoking” classes were compromised compared to both “consistently positive” and the sample mean across all outcomes, even though some relationships were not significant for the small “food insecurity/violence/smoking” class. “Middle of the road” children, though compromised, evidenced higher predicted values for cognition and behavior than children in the “nutrition/sleep problems” and “food insecurity/smoking/violence” classes.
Figure 1. Predicted values from linear regression and probabilities from binary logistic regression models.
Source: Early Childhood Longitudinal Study-Birth Cohort, 2001–2005. N ≈ 6450.
Notes: Predicted values and probabilities are drawn from Table 3, Model 3’s multivariate OLS regression analyses (for reading, math, and behavior) and binary logistic regression analyses (for health) and accounted for complex survey design. Predicted values and probabilities are for a hypothetical child who has average (for continuous variables), median (for ordinal variables) or modal (for other categorical variables) values for all variables except health lifestyle class.
DISCUSSION
Our first research question asked whether there were predominant empirical patterns representing health lifestyles among U.S. preschool-aged children. We found that there are. Five predominant lifestyles emerged from the data in our latent class analysis, each with a distinct sociodemographic profile and unique consequences for children’s health and development. None was characterized by a single health risk, but rather, by risks from multiple domains. Thus, empirical approaches isolating a single health behavior or risk may miss the single factor’s contextualization within a landscape of diverse but sometimes closely related behaviors and risks that comprise an individual’s health lifestyle. We have followed prior literature in characterizing health lifestyles as patterns of behavior and encourage future research that also incorporates identity and other components of health lifestyles. Our combination of overall risky and specific domain-focused latent classes echoes Krueger and colleagues’ (2009) seven state- and province-level latent classes in U.S. and Canadian adults and Laska and colleagues (2009) four gender-specific latent classes in Minnesota college students. This similarity arose even though these two studies used very different behavioral indicators in different age groups from ours. Our latent class analysis results would likely differ depending on the indicators used. Here, we combined parents’ behavioral management of children’s health risks with children’s own health behaviors, but boundaries are blurry for indicators such as experiences of violence.
The second research question asked whether social disadvantage and household resources were related to health lifestyles. Children’s health lifestyles were strongly patterned by both factors. For many measures, compromised household resources partly or completely explained the relationship between social disadvantage and health lifestyles. These findings suggest an intergenerational process in which parents’ disadvantaged backgrounds and limited resources are reflected in young children’s health lifestyles. Future quantitative and qualitative research should articulate how this occurs.
The third research question asked if preschool-aged children’s health lifestyles predict their development and health at the start of kindergarten. Our findings show that health lifestyles have a complex and multidimensional relationship with child outcomes, and we highlight some overarching patterns here. First, disparities by lifestyle were surprisingly consistent across the cognitive, behavioral, and health domains. Two classes characterized by specific health risks, “food insecurity/violence/smoking” and “nutrition/sleep problems,” tended to have the most compromised predicted outcomes (though not all relationships were significant for the former, small class likely because of statistical power). Although the latter class was similar to the “middle of the road” class in terms of social disadvantage, it was more strongly related to most child outcomes compared to the “consistently positive” class. The predictive power of both generalized levels of moderate health lifestyle risk, and pronounced health lifestyle risks in a small number of domains, suggests that this approach of contextualizing health behaviors within a cohesive lifestyle may be fruitful for understanding health and development.
Second, the associations of health lifestyles with cognitive outcomes were explained to a substantial extent by household resources, but relationships with behavior and health were more robust. In particular, the risk of having a worse health status than “very good” nearly doubled when comparing either the “nutrition/sleep problems” or “middle of the road” classes to “consistently positive.” Future research should both acknowledge that health lifestyle implications are often consistent across outcome domains and consider focusing in particular on implications for health and socioemotional behavior.
Third, health lifestyles predicted child outcomes in ways that made substantive sense. The overall risk represented by “middle of the road” translated into disparities across all outcomes in full models, as did the increased “junk food” consumption and suboptimal sleep patterns of the “nutrition/sleep problems” class. Children’s risks in this latter class are suggestive of permissive parenting or less monitoring by adults. Developmental implications of the “safety problems” class were limited to a marginally significant relationship with behavior, perhaps because injury incidents associated with the safety risks experienced by these children are rare. The main implications of these safety risks may have been for children’s overall sense of security in their homes, manifesting in the behavioral domain. Thus, the lack of significant associations for the “safety problems” class in other domains suggests that we may have adequately controlled for confounders related to health lifestyles. Risks associated with food insecurity, secondhand smoke exposure, and violence exposure were most concentrated in the behavior domain but were also substantial (though not significant likely because of low sample size) for child health and reading. Perhaps more than other indicators and domains, the three major risks in this latent class implied that the children’s most basic needs, such as consistent access to food and freedom from physical violence, were not being met.
Taken together, these findings show that specific health risks co-occur in predominant health lifestyles, and some sets of risks have more pronounced implications than others for children’s development and health. Therefore, children may be struggling in one area of development for reasons we can best understand by considering a broad range of interconnected health behaviors. Further studies of children’s health lifestyles should improve upon the limitations of this one. We examined a snapshot of empirical patterns of behaviors representing health lifestyles in prekindergarten, when children likely have little agency in crafting their own health lifestyles. But even at this age, agency is beginning to come into play: Many children begin to request some foods and refuse others, lobby for a later bedtime, or start biking without a helmet. Earlier and later in childhood, changing developmental stages could result in different degrees of parental influence, different influences from adults such as teachers, and different types of health lifestyles being predominant. Future research should think developmentally about health lifestyles. Qualitative research is needed to complement initial work that has been done in documenting the socialization of children into health lifestyles (e.g., Lareau 2003).
Although this study’s data cannot capture longer-term outcomes, we expect that children’s preschool health lifestyles shape their health lifestyles and outcomes throughout adulthood. This may occur through at least two pathways. First, as articulated above, early health lifestyles may socialize children to adopt similar health behaviors in adulthood. Second, the developmental and health impacts of early health lifestyles may affect later socioeconomic and other characteristics, which in turn are linked to adult health lifestyles. Understanding the roles parents’ and children’s identities play in these emerging health lifestyles begs a qualitative approach. Processes linking social disadvantage and resources to children’s health lifestyles, the health lifestyles of parents to those of their children, and children’s health lifestyles to their subsequent development may also be best identified using a mixed-methods approach. Additional research linking macrolevel influences such as social structures and cultural norms to health lifestyles is needed. Finally, more attention should be paid to the bidirectional relationship between socioeconomic status and health lifestyles, both in childhood and linking childhood to the remaining life course. Theoretical progress in this area has been rich when thinking about adults, and childhood is important terrain for expanding these ideas.
Our articulation of childhood health lifestyles and our empirical findings have theoretical implications. The literature on health lifestyles has articulated complicated interrelationships among health behaviors, socioeconomic status, and identities in adulthood. Life course researchers have shown that both socioeconomic status and health behaviors are dynamic processes rooted in family background and childhood that cross generations. Incorporating the idea of childhood health lifestyles into research on intergenerational inequalities can help us understand these processes. Continued consideration of the dimensions that constitute health lifestyles in childhood and the roles of agency and identity will benefit theoretical development.
Although observational findings cannot substitute for randomized controlled trials, they suggest three primary directions for shaping future research and social policy. First, specific health risks in early childhood do not occur in a vacuum. Children with low or high risks in one domain are likely to have risks in others as well. Thus, policies intended to fix a specific health risk, such as secondhand smoke exposure, miss a set of interrelated risks that, when analyzed together, have implications for children’s development and health. Targeting a specific behavior without understanding the health lifestyle and related identities it is embedded in may lead to less effective policy interventions. Second, we found that household resources were important predictors of class membership. In many cases, these resources explained why children from disadvantaged social disadvantages were more likely to be members of these classes. Although these results are only suggestive, they imply that interventions helping families with low levels of resources might nudge families toward improved health lifestyles for their young children, reducing intergroup disparities in these health lifestyles and improving early development and health. Third, children’s health lifestyles predict cognition, behavior, and health in early childhood. Thus, policy interventions to improve children’s health lifestyles in early childhood might pay off in the short term. Our findings argue against a one-size-fits-all approach to encouraging school readiness in favor of tailored approaches acknowledging overall health lifestyles. Because improvements to children’s development and health by the start of school are particularly important for later life outcomes, expanded research on children’s health lifestyles is warranted.
BIOSKETCHES
Stefanie Mollborn is an associate professor in the Institute of Behavioral Science and the Department of Sociology, University of Colorado Boulder. Her past work has focused on teen parenthood and early childhood. She is beginning a research program on health lifestyles among children and youth. Her research has been published in Social Forces, Demography, Social Psychology Quarterly, and Journal of Marriage and Family.
Laurie James-Hawkins is a Ph.D. candidate in the Department of Sociology and the Institute of Behavioral Science, University of Colorado Boulder. She is interested in the social psychology of contraceptive use, unintended pregnancy, partner and family dynamics, and child health. Her dissertation examines reasons for non-use of contraceptives when one does not desire pregnancy, and social influences on contraceptive use and unintended pregnancy in emerging adulthood.
Elizabeth Lawrence is a Ph.D. candidate in the Sociology department and Population Program at the University of Colorado Boulder. Her research focuses on how social background shapes educational attainment and how background and education in turn influence adult health outcomes. She is currently working on her dissertation, which examines the effects of college degrees on health behaviors.
Paula Fomby is an associate research scientist at the Institute for Social Research, University of Michigan. She investigates how family structure change is associated with child well-being in the context of high social inequality. Her research has been published in outlets such as Journal of Marriage and Family, American Sociological Review, Sociology of Education, and Social Science Research.
NOTES
1 Because of ECLS-B confidentiality requirements, all Ns are rounded to the nearest 50.
2 About 7,000 children participated in the kindergarten data collection. We omitted ~150 cases with missing weights and another ~400 whose biological mother was not the respondent.
3 The frequently copyrighted items from assessments were not available to users of the data, so we relied on scores constructed by ECLS-B staff using item response theory (IRT) modeling.
4 The high proportion of reports of favorable child health necessitated this particular dichotomy; only 3% of child health reports at Wave 3 fell into the “fair” or “poor” categories.
5 The small “food security/violence/smoking” class had substantial but nonsignificant negative coefficients for early reading and child health, which would likely have been significant if there had been greater statistical power.
6 Supplementary models found that F statistics, which reward more parsimonious models, were consistently higher in the models using latent classes compared to equivalent models using the health risk indicators instead, revealing a preference for the simpler models. These analyses suggest that the operationalization of health lifestyles using latent classes may be statistically preferable to using the individual indicators.
Acknowledgments
This study was supported by National Science Foundation grants SES 1061058 and SES 1423524. Research funds were also provided by the NIH/NICHD funded CU Population Center grant R24HD066613. The authors thank Richard Jessor, Joshua Goode, Aakriti Shrestha, and Jeff Dennis for their contributions to this project.
Contributor Information
Stefanie Mollborn, University of Colorado Boulder.
Laurie James-Hawkins, University of Colorado Boulder.
Elizabeth Lawrence, University of Colorado Boulder.
Paula Fomby, University of Michigan.
REFERENCES
- Abel Thomas. 1991. “Measuring Health Lifestyles in a Comparative Analysis: Theoretical Issues and Empirical Findings.” Social Science & Medicine 32(8):899–908. [DOI] [PubMed] [Google Scholar]
- Abella Rodolfo and Heslin Richard. 1984. “Health, Locus of Control, Values, and the Behavior of Family and Friends: An Integrated Approach to Understanding Preventive Health Behavior.” Basic and Applied Social Psychology 5(4):283–94. [Google Scholar]
- Backett Kathryn C. and Davison Charlie. 1995. “Lifecourse and Lifestyle: The Social and Cultural Location of Health Behaviours.” Social Science & Medicine 40(5):629–38. [DOI] [PubMed] [Google Scholar]
- Blaxter Mildred. 1990. Health and Lifestyles. London: Routledge. [Google Scholar]
- Bourdieu Pierre. 1986. Distinction: A Social Critique of the Judgement of Taste. London: Routledge & Kegan Paul. [Google Scholar]
- Burke V, Milligan RAK, Beilin LJ, Dunbar D, Spencer M, Balde E and Gracey MP. 1997. “Clustering of Health-Related Behaviors among 18-Year-Old Australians.” Preventive Medicine 26(5):724–33. [DOI] [PubMed] [Google Scholar]
- Butler Susan R., Marsh Herbert W., Sheppard Marlene J. and Sheppard John L.. 1985. “Seven-Year Longitudinal Study of the Early Prediction of Reading Achievement.” Journal of Educational Psychology 77(3):349–61. [Google Scholar]
- Butz Arlene M., Breysse Patrick, Rand Cynthia, Curtin-Brosnan Jean, Eggleston Peyton, Diette GB, Williams D, Bernert JT and Matsui EC. 2011. “Household Smoking Behavior: Effects on Indoor Air Quality and Health of Urban Children with Asthma.” Maternal and Child Health Journal 15(4):460–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen Pia. 2004. “The Health-Promoting Family: A Conceptual Framework for Future Research.” Social Science & Medicine 59(2):377–87. [DOI] [PubMed] [Google Scholar]
- Cockerham William C. 2000. “The Sociology of Health Behavior and Health Lifestyles” In Handbook of Medical Sociology, edited by Bird C, Conrad P and Fremont AM. Upper Saddle River, NJ: Prentice-Hall. [Google Scholar]
- Cockerham William C. 2005. “Health Lifestyle Theory and the Convergence of Agency and Structure.” Journal of Health and Social Behavior 46(1):51–67. [DOI] [PubMed] [Google Scholar]
- Cockerham William C. 2007. “Health Lifestyles and the Absence of the Russian Middle Class.” Sociology of Health & Illness 29(3):457–73. [DOI] [PubMed] [Google Scholar]
- Cook John T., Frank Deborah A., Levenson Suzette M., Neault Nicole B., Heeren TC, Black MM, Berkowitz C, Casey PH, Meyers AF, Cutts DB and Chilton M. 2006. “Child Food Insecurity Increases Risks Posed by Household Food Insecurity to Young Children’s Health.” Journal of Nutrition 136(4):1073–76. [DOI] [PubMed] [Google Scholar]
- Crosnoe Robert. 2006. “Health and the Education of Children from Racial/Ethnic Minority and Immigrant Families.” Journal of Health and Social Behavior 47(1):77–93. [DOI] [PubMed] [Google Scholar]
- Crosnoe Robert and Wildsmith Elizabeth. 2011. “Nonmarital Fertility, Family Structure, and the Early School Achievement of Young Children from Different Race/Ethnic and Immigration Groups.” Applied Developmental Science 15(3):156–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie Janet and Stabile Mark. 2003. “Socioeconomic Status and Child Health: Why Is the Relationship Stronger for Older Children?” American Economic Review 93:1812–23. [DOI] [PubMed] [Google Scholar]
- De Genna Natacha M., Stack Dale M., Serbin Lisa A., Ledingham Jane E. and Schwartzman Alex E.. 2006. “From Risky Behavior to Health Risk: Continuity across Two Generations.” Journal of Developmental and Behavioral Pediatrics 27(4):297–309. [DOI] [PubMed] [Google Scholar]
- Dellinger Ann M. and Kresnow Marcie-jo. 2010. “Bicycle Helmet Use among Children in the United States: The Effects of Legislation, Personal and Household Factors.” Journal of Safety Research 41(4):375–80. [DOI] [PubMed] [Google Scholar]
- Dodd Lorna J., Yahya Al-Nakeeb Alan Nevill and Forshaw Mark J.. 2010. “Lifestyle Risk Factors of Students: A Cluster Analytical Approach.” Preventive Medicine 51(1):73–77. [DOI] [PubMed] [Google Scholar]
- Du Wei, Finch Caroline F., Hayen Andrew, Bilston Lynne, Brown Julie and Hatfield Julie. 2010. “Relative Benefits of Population-Level Interventions Targeting Restraint-Use in Child Car Passengers.” Pediatrics 125(2):304–12. [DOI] [PubMed] [Google Scholar]
- Duncan Greg J., Dowsett Chantelle J., Claessens Amy, Magnuson Katherine, Huston Aletha C., Klebanov Pamela, Pagani Linda S., Feinstein Leon, Engel Mimi, Jeanne Brooks-Gunn Holly Sexton, Duckworth Kathryn and Japel Crista. 2007. “School Readiness and Later Achievement.” Developmental Psychology 43(6):1428–46. [DOI] [PubMed] [Google Scholar]
- Duncan Greg J., Ludwig Jens and Magnuson Katherine A.. 2007. “Reducing Poverty through Preschool Interventions.” Future of Children 17(2):143–60. [DOI] [PubMed] [Google Scholar]
- Durbin Dennis R., Chen Irene, Smith Rebecca, Elliott Michael R. and Winston Flaura K.. 2005. “Effects of Seating Position and Appropriate Restraint Use on the Risk of Injury to Children in Motor Vehicle Crashes.” Pediatrics 115(3):E305–E09. [DOI] [PubMed] [Google Scholar]
- Elder Glen H. Jr. 1994. “Time, Human Agency, and Social Change: Perspectives on the Life Course.” Social Psychology Quarterly 57(1):4–15. [Google Scholar]
- Entwisle Doris R., Alexander Karl L. and Olson Linda Steffel. 2004. “The First-Grade Transition in Life Course Perspective” In Handbook of the Life Course, edited by Mortimer JT and Shanahan MJ. New York: Springer. [Google Scholar]
- Frech Adrianne. 2012. “Healthy Behavior Trajectories between Adolescence and Young Adulthood.” Advances in Life Course Research 17(2):59–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glewwe Paul, Jacoby Hanan G. and King Elizabeth M.. 2001. “Early Childhood Nutrition and Academic Achievement: A Longitudinal Analysis.” Journal of Public Economics 81(3):345–68. [Google Scholar]
- Haas Steven. 2008. “Trajectories of Functional Health: The ‘Long Arm’ of Childhood Health and Socioeconomic Factors.” Social Science & Medicine 66(4):849–61. [DOI] [PubMed] [Google Scholar]
- Halonen Anne, Aunola Kaisa, Ahonen Timo and Nurmi Jari-Erik. 2006. “The Role of Learning to Read in the Development of Problem Behaviour: A Cross-Lagged Longitudinal Study.” British Journal of Educational Psychology 76(3):517–34. [DOI] [PubMed] [Google Scholar]
- Hardie Jessica Halliday and Landale Nancy S.. 2013. “Profiles of Risk: Maternal Health, Socioeconomic Status, and Child Health.” Journal of Marriage and Family 75(3):651–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward Mark D. and Gorman Bridget K.. 2004. “The Long Arm of Childhood: The Influence of Early-Life Social Conditions on Men’s Mortality.” Demography 41(1):87–107. [DOI] [PubMed] [Google Scholar]
- Hemenway David. 2011. “Risks and Benefits of a Gun in the Home.” American Journal of Lifestyle Medicine 5(6):502–11. [Google Scholar]
- Idler Ellen L. and Benyamini Yael. 1997. “Self-Rated Health and Mortality: A Review of Twenty-Seven Community Studies.” Journal of Health and Social Behavior 38(1):21–37. [PubMed] [Google Scholar]
- Kennedy Christine and Floriani Victoria. 2008. “Translating Research on Healthy Lifestyles for Children: Meeting the Needs of Diverse Populations.” Nursing Clinics of North America 43(3):397–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King W. James. 2012. “Installation of Safety Devices Reduces the Risk of Home Injury in Children.” Evidence-Based Nursing 15(1):13–14. [DOI] [PubMed] [Google Scholar]
- Koulouglioti Christina, Cole Robert and Kitzman Harriet. 2008. “Inadequate Sleep and Unintentional Injuries in Young Children.” Public Health Nursing 25(2):106–14. [DOI] [PubMed] [Google Scholar]
- Krueger Patrick M., Bhaloo Tajudaullah, and Rosenau Pauline Vaillancourt. 2009. “Health Lifestyles in the United States and Canada: Are We Really So Different?” Social Science Quarterly 90(5):1380–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laaksonen Mikko, Prättälä Ritva and Lahelma Eero. 2002. “Sociodemographic Determinants of Multiple Unhealthy Behaviors.” Scandinavian Journal of Public Health 30:1–7. [DOI] [PubMed] [Google Scholar]
- Lareau Annette. 2003. Unequal Childhoods: Class, Race, and Family Life. Berkeley: University of California Press. [Google Scholar]
- Laska Melissa, Pasch Keryn, Lust Katherine, Story Mary and Ehlinger Ed. 2009. “Latent Class Analysis of Lifestyle Characteristics and Health Risks Behaviors among College Youth.” Prevention Science 10(4):376–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Jin-Ding, Tung Ho-Jui, Hsieh Yu-Hsin and Lin Fu-Gong. 2011. “Interactive Effects of Delayed Bedtime and Family-Associated Factors on Depression in Elementary School Children.” Research in Developmental Disabilities 32(6):2036–44. [DOI] [PubMed] [Google Scholar]
- Link Bruce G. and Phelan Jo. 1995. “Social Conditions as Fundamental Causes of Disease.” Journal of Health and Social Behavior 35:80–94. [PubMed] [Google Scholar]
- Lucas Alan. 1998. “Programming by Early Nutrition: An Experimental Approach.” Journal of Nutrition 128(2):401S–06S. [DOI] [PubMed] [Google Scholar]
- National Heart, Lung, and Blood Institute. 2012. “How Much Sleep Is Enough?” Retrieved September 1, 2014 (http://www.nhlbi.nih.gov/health/health-topics/topics/sdd/howmuch.html).
- Nord C, Edwards B, Andreassen C, Green JL and Wallner-Allen K. 2006. “Early Childhood Longitudinal Study, Birth Cohort (ECLS-B), User’s Manual for the ECLS-B Longitudinal 9-Month-2-Year Data File and Electronic Codebook (Nces 2006–046).” Washington, D.C.: U.S. Department of Education, National Center for Education Statistics. [Google Scholar]
- Nutbeam Don, Aaro Leif and Catford John. 1989. “Understanding Children’s Health Behaviour: The Implications for Health Promotion for Young People.” Social Science & Medicine 29(3):317–25. [DOI] [PubMed] [Google Scholar]
- Pampel Fred C., Krueger Patrick M. and Denney Justin T.. 2010. “Socioeconomic Disparities in Health Behaviors.” Annual Review of Sociology 36:349–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson Ruth E., Haines Pamela S. and Popkin Barry M.. 1994. “Health Lifestyle Patterns of U.S. Adults.” Preventive Medicine 23(4):453–60. [DOI] [PubMed] [Google Scholar]
- Reijneveld Sijmen A. 1998. “Reported Health, Lifestyles, and Use of Health Care of First Generation Immigrants in the Netherlands: Do Socioeconomic Factors Explain Their Adverse Position?” Journal of Epidemiology and Community Health 52(5):298–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuster Tonya L., Dobson Marnie, Jauregui Maritza and Blanks Robert H. I.. 2004. “Wellness Lifestyles I: A Theoretical Framework Linking Wellness, Health Lifestyles, and Complementary and Alternative Medicine.” Journal of Alternative and Complementary Medicine 10(2):349–56. [DOI] [PubMed] [Google Scholar]
- Simpkin Charles T., et al. 2014. “Chronotype Is Associated with the Timing of the Circadian Clock and Sleep in Toddlers.” Journal of Sleep Research 23(4):397–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha Dinesh P. 1992. “Project Lifestyle: Developing Positive Health Lifestyles for Schoolchildren in Antigua.” Journal of School Health 62(10):449–53. [DOI] [PubMed] [Google Scholar]
- Snead M. Christine and Cockerham William C.. 2002. “Health Lifestyles and Social Class in the Deep South.” Social Inequalities, Health and Health Care Delivery 20:107–22. [Google Scholar]
- Snow K, Derecho A, Wheeless S, Lennon J, Rosen J, Rogers J, Kinsey S, Morgan K and Einaudi P. 2009. “Early Childhood Longitudinal Study, Birth Cohort (ECLS-B), Kindergarten 2006 and 2007 Data File User’s Manual.” NCES 2010–010. Washington, D.C.: National Center for Education Statistics. [Google Scholar]
- Sobel Michael E. 1981. Lifestyle and Social Structure: Concept, Definitions, Analyses. New York: Academic Press. [Google Scholar]
- Stefansdottir Ingibjorg Katrin and Vilhjalmsson Runar. 2007. “Dimensions of Health-Related Lifestyle in Young Adulthood: Results from a National Population Survey.” Scandinavian Journal of Caring Sciences 21(3):321–28. [DOI] [PubMed] [Google Scholar]
- Stets Jan E. and Burke Peter J.. 2000. “Identity Theory and Social Identity Theory.” Social Psychology Quarterly 63(3):224–37. [Google Scholar]
- Terre Lisa, Drabman Ronald S. and Meydrech Edward F.. 1990. “Relationships among Children’s Health-Related Behaviors: A Multivariate, Developmental Perspective.” Preventive Medicine 19(2):134–46. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Education, National Center for Education Statistics. 2007. “Early Childhood Longitudinal Study, Birth Cohort (ECLS-B), Longitudinal 9-Month/Preschool Restricted-Use Data File.” NCES 2008–024. U.S. Department of Education, National Center for Education Statistics. [Google Scholar]
- Weller LD, Schnittjer CJ and Tuten BA. 1992. “Predicting Achievement in Grades Three through Ten Using the Metropolitan Readiness Test.” Journal of Research in Childhood Education 6(2):121–29. [Google Scholar]
- Wickrama KAS, Rand D. Conger, Wallace Lora Ebert and Elder Glen H. Jr. 1999. “The Intergenerational Transmission of Health-Risk Behaviors: Adolescent Lifestyles and Gender Moderating Effects.” Journal of Health and Social Behavior 40(3):258–72. [PubMed] [Google Scholar]
- Yount Kathryn M., DiGirolamo Ann M. and Ramakrishnan Usha. 2011. “Impacts of Domestic Violence on Child Growth and Nutrition: A Conceptual Review of the Pathways of Influence.” Social Science & Medicine 72(9):1534–54. [DOI] [PubMed] [Google Scholar]