Abstract
Background and purpose
Self-monitoring of blood glucose (SMBG) is important to the management of diabetes mellitus, yet most patients with type 2 diabetes mellitus (T2DM) do not perform SMBG as recommended. The current status and influential factors of SMBG in China have not been well investigated. This study aimed to describe the present status of SMBG adherence in China and investigate the influential factors based on electronic questionnaires.
Patients and methods
A cross-sectional study was conducted from June to July of 2017 at hospitals in Changsha, China. Seven hundred and twenty-one patients with T2DM completed the information‑motivation‑behavioral (IMB) skills questionnaire and other electronic questionnaires composed of demographic and clinical characteristics as well as diabetes-related and psychological scales. Univariate comparisons and multivariate logistic regression were used to explore the relationships among SMBG adherence and related factors.
Results
Seven hundred and twenty-one patients with valid questionnaires were included. Only 27.5% (198/721) of the patients with T2DM were SMBG adherent based on the guideline of the Chinese Diabetes Society (CDS) in 2017. Among all groups of treatment regimens, the rate of SMBG adherence was highest at 36.6% (82/224) in patients on oral hypoglycaemic drugs (OHAs). In multivariable analysis, the treatment of OHAs (OR =3.731, CI 2.162–6.437) and diet/exercise (OR =3.534, CI 1.841–6.783), the patient having their own blood glucose meter (OR =6.916, CI 4.054–11.800) and a higher education level (OR =3.780, CI 1.688–8.466) were significantly associated with SMBG adherence.
Conclusion
Most Chinese patients with T2DM did not perform SMBG as recommended. The treatment of OHAs and diet/exercise, the patient having their own blood glucose meter, a higher education level and other factors were correlates of SMBG adherence. There is clearly a need for prospective, multicenter, large-scale studies to explore the reasons for patients’ failure to practice SMBG adherence.
Keywords: type 2 diabetes mellitus, self-monitoring of blood glucose, adherence, glycemic control, China
Introduction
Diabetes mellitus (DM) is one of the most common chronic diseases and has become a major health issue globally.1 According to the International Diabetes Federation, 1 in 11 adults in the world between the ages of 20 and 79 had suffered from diabetes by the year 2015, with the estimated number of patients with DM reaching 415 million people worldwide by the same year.2 The type 2 diabetes mellitus (T2DM) accounted for more than 90% of patients with diabetes and was the sixth leading cause of disability in the same year.3 The estimated number of patients with T2DM is expected to increase and would reach nearly 600 million by 2040.4 Like the rest of the world, the prevalence rate of DM keeps increasing in China, and the estimated prevalence of DM was 10.9% in 2013 due to rapid urbanization and the aging of the Chinese population,5,6 which was just below the unadjusted prevalence of total diabetes (12.3%) in the population of the United States from 2011 to 2012.7
As a disease of glucose metabolism dysfunction, T2DM poses a great threat to multi-organ systems and may lead to a series of related complications.8,9 The comprehensive treatment and control of T2DM in China are mainly composed of dietary restrictions, exercise, drugs and insulin therapy, diabetes education and blood glucose monitoring.6 The self-monitoring of blood glucose (SMBG) has become an effective tool in the management of diabetes as through this practice, patients can receive their real-time blood glucose level and then adjust their diet/exercise and treatment dose. Numerous studies have demonstrated that SMBG can improve glucose control and facilitate treatment promptly in patients with type 1 diabetes or T2DM.10,11 However, in both developed countries and developing countries, previous studies have indicated that the rate of SMBG adherence has not reached an optimal level, reporting the rate of adherence as 52% in America, 38.5% in Latin America, 49.8% in United Kingdom, 59% in Jordan, 22.6% in Cameroon and 18.98% in China.12–17 Several studies have shown that some factors were related to SMBG adherence, such as gender, age, education level, income, treatment regimen, the frequency of clinic visits, the duration of the diseases and the provision of glucose testing strips.12,13,18–21 Some studies have suggested that a higher level of education might lead to better SMBG adherence.22 And several psychological factors, such as self-efficacy, outcome expectations, physical influence, environmental barriers and social support, have also been included to explore their association with adherence to SMBG.17 High level of motivation was reported to enable patients with T2DM to maintain diet and perform SMBG.23 And the information of diabetes also attaches importance to the management of this chronic disease.24,25
As there are various differences in society and culture among China and other countries, it is uncertain whether influential factors from foreign countries apply to China. In addition, the current status and influential factors of SMBG in China have not been well investigated as SMBG has been introduced into China just in recent years. The number of relevant studies was limited,12 and there has been no study concerning the psychological factors of SMBG adherence. Understanding the current status and the association of factors with SMBG in China may help determine the solutions to achieving better glycemic control and decrease the burdens of chronic diseases in the future. Based on the Self- and Family Management Framework,26 the management of chronic diseases is related to many factors, including facilitators and barriers, processes, proximal outcomes and distal outcomes, which have instructive significance for the design and process of relevant studies. Electronic questionnaires are convenient and efficient with high response rates. Therefore, using electronic questionnaires, we aimed to explore the present status of SMBG adherence in China. Additionally, this study focused on the influential factors of SMBG based on demographic and clinical characteristics and psychological factors.
Materials and methods
Study design and patients
A cross-sectional study was carried out between June and July 2017 at secondary and tertiary hospitals in Changsha, China. Hospitals in Changsha were divided into 84 secondary hospitals and 20 tertiary hospitals according to the hospital scale. And 11 public tertiary hospitals and 4 public secondary hospitals own the independent endocrinology wards. Simple random sampling by random numbers was conducted using Statistical Package for the Social Sciences (SPSS).27 The starting point of random number were set at random via this software. Then the corresponding random numbers of 15 public hospitals were generated and then listed in an ascending sort order. The top two the random numbers were noted, and the corresponding hospitals including one secondary hospital and one tertiary hospital were selected. Three departments in each of these two hospitals were selected using the same sampling method. Patients within the three selected departments and one endocrinology ward of each of these two hospitals were included according to the following inclusive criteria: (1) the patients had been diagnosed with T2DM according to the standard World Health Organization (WHO) definition of the disease for over three months;28 (2) the patients were over the age of 18 and were capable of understanding and communicating; and (3) the patients had voluntarily joined this study with informed consent. The exclusion criteria included patients with some related complications, such as severe diabetic nephropathy, retinopathy and other diseases like low intelligence that prevented them from participating in this study.
The theoretical population of this study was calculated on the basis of local patient demographics and expert opinions, using the Krejcie and Morgan formula:29
As α is set to 0.05, u is equal to 1.96. P-value is the anticipated rate of patients with SMBG adherence (36.4% in this research), and d is admissible error (0.1P in this research). The theoretical population in this study totaled 671 based on the relevant parameters. Considering the possibility of dropouts during the survey, a larger sample size was designed to meet the aims of this study. Finally, 730 patients with T2DM were recruited to participate in this study and a total of 721 questionnaires were collected with a response rate of 98.8%.
Measurements
Background information
A general information sheet was used to collect demographic and health-related information, including age, gender (female/male), weight, height, marital status, education levels, occupation, personal monthly income, health insurance, smoking and drinking status, the family history of diabetes, the treatment regimen, the complications or co-morbidities of diabetes and the frequency of hospitalization and physician consultation in the last year.
SMBG adherence
Adherence to SMBG was defined based on the frequency recommended in the official guideline on the prevention and control of T2DM in China, which was drafted by the Chinese Diabetes Society (CDS) in 2017.6 According to this guideline, patients with diabetes who are undergoing lifestyle intervention are supposed to perform SMBG at least once during a certain interval of time, so as to promote lifestyle modification. Patients taking oral hypoglycaemic drugs should perform SMBG at least twice a week. Patients with T2DM requiring insulin injection ought to perform SMBG at least once per day. Patients reported the actual number of times that they performed SMBG per day and per week on the electronic questionnaires accordingly. Based on the frequency recommendations referenced above and the actual frequency reflected on the questionnaires, the patients were divided into two groups: the adherence group and the non-adherence group.
Diabetes-related and psychological scales
IMB-SMBG questionnaire
The patients’ information-motivation-behavioral skills (IMB) were assessed in this study to evaluate SMBG.30,31 The Chinese version of the IMB-SMBG questionnaire was composed of three subscales concerning SMBG information, motivation and behavioral skills.32 This questionnaire covered a total of 76 items, including 30 items in the information part, 25 items in the motivation part and 21 items in the behavioral part. Each item was scored from 1 to 5. A higher score represented better diabetes self-management. In the initial test, the IMB-SMBG questionnaire proved to have good reliability over 0.8 in the whole scale (0.92), and the content validity suggested a strong correlation between the items (r>0.50 for 70% of the items, P<0.001) after retesting and examining the correlations.32 The Cronbach’s α of the total IMB‑SMBG questionnaire was 0.931 in this study and the Cronbach’s α of the information, motivation and behavioral parts were 0.859, 0.888 and 0.878, respectively.
The center for epidemiologic studies depression scale (CES-D)
Depressive symptoms were defined using the Center for Epidemiologic Studies Depression (CES-D) Scale.33 There were a total of 20 questions on the scale. Each question was scored from 0 to 3, and a score of 16 or above indicated the presence of depressive symptoms. A cut-off score ≥21 was set in this study based on the optimum balance between sensitivity and specificity for Chinese patients with T2DM.34 The Cronbach’s α of CES-D in this study was 0.892.
General self-efficacy scale
In assessing the self-efficacy of patients with T2DM, the General Self-Efficacy Scale (GSES) was used. This scale was developed by Schwarzer et al.35 There are 10 items on the GSES. The scale options were scored from 1 (totally wrong) to 4 (entirely correct). Higher scores demonstrated higher competence in dealing with the daily issues. The Cronbach’s α of GSES in this study was 0.932.
Simplified coping style questionnaire
The Simplified Coping Style Questionnaire (SCSQ) developed by Yaning Xie is composed of 20 questions.36 The questionnaire is divided into two parts, including 12 questions on the positive part and 8 questions on the negative part. Each item is rated on a 4-point scale, with the score level indicating the frequency of the related coping style. The Cronbach’s α of the positive parts of the SCSQ in this study was 0.918, while that of the negative parts of the SCSQ was 0.826. The Cronbach’s αs of these scales ranged from 0.826 to 0.932, which indicated the relatively high reliability of the scales used in this study.
Pain caused by SMBG and body mass index
In addition to the SMBG and body mass index (BMI), the level of pain the patients experienced in performing SMBG was evaluated by the numerical rating scale (NRS).37 The options provided on this scale were scored between 0 and 10, with the lowest score meaning no pain and the highest score signifying the greatest possible pain. The patients’ BMIs, defined as the body weight divided by the square of the body height, were calculated based on the body heights and weights given in the questionnaires. The CDS defined being overweight as having a BMI ≥24 and obesity as a BMI ≥28.38
Ethical consideration and data collection
This study was approved by the ethics committee of Xiangya Nursing School, Central South University (No. 2018012). The Declaration of Helsinki on medical protocol and ethics were followed. The investigators received grants from school administrators to collect data. The patients were aware of the objectives involved in this study and gave written informed consent before the survey. Permission to use the scales was obtained from the copyright holders by email if permission was required.
All study investigators and assistants were trained to follow the rules of the study, including for the objectives of the study, the ethical issues, the process used for the electronic questionnaires and the meaning of the items in the questionnaires. The questionnaire was uploaded to the online questionnaire website (wjx, https://www.wjx.cn/). After signing the informed consents, the patients filled out the electronic questionnaires via the online questionnaire website by using their mobile phones. During the questionnaire process, the patients were given detailed explanations by the study investigators and assistants, who were standing by the side of the room when the patients filled out the questionnaires.
Statistical analysis
The raw data collected via the online questionnaire website were first transformed into Excel files. Then the data in the Excel files were analyzed using the SPSS, version 24.0 for Windows (IBM, Armonk, New York, USA). The continuous variables were presented as the mean and standard deviation (SD), and the categorical variables were presented as the frequency and percentage. Three-phase analysis was conducted to analyze the relationship among SMBG adherence and the related factors. First, descriptive statistics on the background information and the scores on the scales were formulated to present demographic and other characteristics. Second, the univariate analyses were used to evaluate the associations between the two groups. The differences between the continuous variables were detected by an independent t-test or the Mann-Whitney U test. Comparisons of the categorical variables were analyzed by the Chi-squared test (for binomial variables) or the Cochran-Armitage trend test (for ordinal variables). Variables that were statistically significant (P<0.05) in the univariate comparisons were entered into the multivariate logistic regression. In order to decrease the probability of type I error, the Bonferroni method was introduced.39,40 Variables with P<0.05/n (n is the number of subgroups of this variable) in multiple comparison is considered statistically significant. Third, a multivariate logistic regression was conducted to analyze the effects of the potential variables on SMBG adherence. Logistic regression analyses were presented as odds ratios (ORs) and corresponding 95% confidence intervals (CIs). The receiver Operating Characteristic (ROC) curve was further developed to assess the potential of the final multivariable logistic regression model. Corresponding area under curve (AUC) and 95%CI were also calculated. 1,000 bootstrap samples of the whole cohort were performed to validate the final multivariable logistic regression model. Statistical significance was set at a P-value of <0.05.
Results
Characteristics of the samples
A total of 721 patients with valid questionnaires were included in this study. The process of filling out the questionnaire took up to 18.89 mins (range 3–77, SD =12.20) on average. The age of the patients ranged from 20 to 96 years (mean =56.94, SD =15.48). Female patients made up 54.6% of the total samples. The average BMI was 23.44 (SD =3.376) and 34.67% (250/721) of the patients were overweight (BMI ≥24), while 9.02% (65/721) of them were obese (BMI ≥28). The medical fee payment methods in this study were rendered through rural cooperative medical insurance (45.4%, 327/721), followed by urban medical insurance (32.9%, 237/721), government/business subsidies (15.0%, 108/721) and self-payments (6.8%, 49/721). More than half of the patients (55.3%, 399/721) reported at least one diabetes complication and 23.4% (169/721) of them visited community clinics more than twice a year.
SMBG adherence
This study covered all standard treatment regimens: 34.5% of the patients (249/721) were on diet or exercise regimens, 31.1% (224/721) were on prescription oral hypoglycemic agents and 34.4% (248/721) were on insulin with/without hypoglycaemic drugs. The mean frequency of SMBG per week in patients on diet or exercise was 1.47 (range 0–30, SD =4.93) and that of patients treated with OHAs and insulin was 2.52 (range 0–40, SD =5.99) and 9.33 (range 0–94, SD =16.86), respectively (Table 2). Only 18.2% (131/721) of the patients performed SMBG more than once per day, while only 22.3% (161/721) of them performed it at least once a week. According to the frequency recommended by the CDS in 2017, the rate of SMBG adherence was the highest at 36.6% (82/224) in patients on OHAs, while the rate of SMBG adherence in patients on diet or exercise and insulin was 20.5% (51/249) and 26.2% (65/248), respectively. Only 27.5% (198/721) of all patients were SMBG adherent.
Table 2.
SMBG frequency by diabetic treatment regimen
| Treatment regimen | SMBG frequency per week (mean ± SD) | F-values | P-values |
|---|---|---|---|
| Diet/exercise (no drugs) | 1.47±4.93 | 38.117 | <0.0001 |
| Oral hypoglycemic agents (OHAs) | 2.52±5.99 | ||
| Insulin (with/without OHAs) | 9.33±16.86 |
Note: The frequency of SMBG per week in patients with different diabetic treatment regimen was presented as mean ± SD.
Abbreviations: SMBG, self-monitoring of blood glucose; SD, standard deviation.
Clinical and demographic characteristics based on SMBG adherence
In order to explore the factors associated with adherence to SMBG, a univariate analysis of clinical and demographic characteristics was conducted based on SMBG adherence. As shown in Table 1, demographic characteristics, including gender, occupation, medical payment method and drinking status, were significantly associated with SMBG adherence. In the subgroups of BMI, education level and per capita monthly income, multiple comparisons indicated that these three variables did not reach statistical significance. Disease-related factors, including a family history of T2DM, diabetes-related complications, the frequency of visits to community clinics per year, the frequency of hospitalization per year, the treatment regimen, whether the patient had his or her own blood glucose meter and knowledge of the recommendation on the frequency of SMBG, were also significantly associated with SMBG adherence.
Table 1.
Clinical and demographic data on the studied population
| Variable | Participants, n (%) | χ2 | Ρ-values | |
|---|---|---|---|---|
| SMBG adherence | SMBG non-adherence | |||
| Gender (F/M), n | 86/112 | 308/215 | 13.845 | <0.001 |
| Age (years) | 2.895 | 0.235 | ||
| Young adulthood (18–44) | 38 (24.4%) | 118 (75.6%) | ||
| Middle age (45–60) | 59 (25.2%) | 175 (74.8%) | ||
| Old age (>60) | 101 (30.5%) | 230 (69.5%) | ||
| Marital status | 2.917 | 0.233 | ||
| Single | 5 (14.7%) | 29 (85.3%) | ||
| Married | 176 (28.1%) | 451 (71.9%) | ||
| Divorced/widowed | 17 (28.3%) | 43 (71.7%) | ||
| Education level | 7.068 | 0.029 | ||
| Primary school and below | 53 (22.5%) | 183 (77.5%) | ||
| Secondary school | 94 (27.7%) | 245 (72.3%) | ||
| University and postgraduate | 51 (34.9%) | 95 (65.91%) | ||
| Occupation | 27.018 | <0.001 | ||
| Farmers | 39 (17.8%) | 180 (82.2%) | ||
| Workmen/clerks | 53 (43.8%) | 68 (56.2%) | ||
| Self-employed/freelancers | 28 (25.2%) | 83 (74.8%) | ||
| Retired/unemployed | 78 (28.9%) | 192 (71.1%) | ||
| Per capita monthly income (CNY) | 7.597 | 0.022 | ||
| ≤1500 | 60 (21.9%) | 214 (78.1%) | ||
| 1501–4500 | 86 (29.6%) | 205 (70.4%) | ||
| ≥4501 | 52 (33.3%) | 104 (66.7%) | ||
| Medical fee payment method | 14.537 | 0.002 | ||
| Rural cooperative medical insurance | 66 (27.8%) | 171 (72.2%) | ||
| Urban medical insurance | 75 (22.9%) | 252 (77.1%) | ||
| Self-payment | 12 (24.5%) | 37 (75.5%) | ||
| Government/business subsidy | 45 (41.7%) | 63 (58.5%) | ||
| Smoking status | 1.135 | 0.567 | ||
| Never smoked | 138 (26.4%) | 385 (73.6%) | ||
| Previous smoker | 21 (29.6%) | 50 (70.4%) | ||
| Current smoker | 39 (30.7%) | 88 (69.3%) | ||
| Drinking status | 8.908 | 0.012 | ||
| Never drinks | 147 (26.1%) | 417 (73.9%) | ||
| Previous drinker | 26 (44.1%) | 33 (55.9%) | ||
| Current drinker | 25 (25.5%) | 73 (74.5%) | ||
| BMI | 8.289 | 0.040 | ||
| BMI <18.5 | 12 (26.1%) | 34 (73.9%) | ||
| 18.5≤ BMI <24.0 | 111 (30.8%) | 249 (69.2%) | ||
| 24.0≤ BMI <28.0 | 66 (26.4%) | 184 (73.6%) | ||
| BMI ≥28.0 | 9 (13.8%) | 56 (86.2%) | ||
| Family history of T2DM | 12.669 | 0.002 | ||
| Yes | 67 (35.4%) | 122 (64.6%) | ||
| No | 107 (27.0%) | 289 (73.0%) | ||
| Unknown | 24 (17.6%) | 112 (82.4%) | ||
| Diabetes-related complications | 9.718 | 0.002 | ||
| Yes | 91 (22.8%) | 308 (77.2%) | ||
| No | 107 (33.2%) | 215 (66.8%) | ||
| Frequency of visiting to community clinics per year | 19.466 | <0.001 | ||
| ≤2 (including none) | 130 (23.6%) | 422 (76.4%) | ||
| ≥3 | 68 (40.2%) | 101 (59.8%) | ||
| Frequency of hospitalizations per year | 16.717 | <0.001 | ||
| ≤2 (including none) | 161 (25.1%) | 481 (74.9%) | ||
| ≥3 | 37 (46.8%) | 42 (53.2%) | ||
| Treatment regimen | 15.69 | <0.001 | ||
| Diet/exercise (no drugs) | 51 (20.5%) | 198 (79.5%) | ||
| Oral hypoglycemic agents (OHAs) | 82 (36.6%) | 142 (63.4%) | ||
| Insulin (with/without OHAs) | 65 (26.2%) | 183 (73.8%) | ||
| Having own blood glucose meter | 101.066 | <0.001 | ||
| Yes | 158 (44.4%) | 198 (55.6%) | ||
| No | 40 (11.0%) | 325 (89.0%) | ||
| Knowing the recommendation on frequency of SMBG | 111.688 | <0.001 | ||
| Yes | 184 (41.3%) | 262 (58.7%) | ||
| No | 14 (5.1%) | 261 (94.9%) | ||
Note: Clinical and demographic characteristics were listed and compared between population with and without SMBG adherence.
Abbreviations: SMBG, self-monitoring of blood glucose; BMI, body mass index; T2DM, type 2 diabetes mellitus.
Associations among SMBG adherence and psychological scales
Table 3 provides descriptions of the diabetes-related and psychological scales, including the IMB-SMBG, CES-D, GSES, SCSQ and NRS, based on SMBG adherence. Among all the dimensions of the IMB-SMBG scale, the score of patients with SMBG adherence was much higher than that of patients with SMBG non-adherence and the results reached statistical significance, including the information part of the IMB-SMBG (t=−6.033, P<0.001), the motivation part of the IMB-SMBG (t=−6.252, P<0.001), the behavior part of the IMB-SMBG (t=−4.506, P<0.001) and the total score of the IMB-SMBG (t=−6.947, P<0.001). The average score on the CES-D was 21.55 (range 0–49, SD =7.76). According to the cut-off point mentioned above, nearly 51% (368/721) of the patients had depressive symptoms at different degrees. There was no statistical significance in the scores of the other scales.
Table 3.
The description of IMB-SMBG, CES-D, GSES, SCSQ and NRS
| Variable | Scores (mean ± SD) | χ2 | t-values | Ρ-values | |
|---|---|---|---|---|---|
| SMBG adherence | SMBG non-adherence | ||||
| IMB-SMBG scale (information part) | 109.72±12.35 | 103.42±12.56 | −6.033 | <0.001 | |
| IMB-SMBG scale (motivation part) | 85.16±11.89 | 78.97±11.86 | −6.252 | <0.001 | |
| IMB-SMBG scale (behavior part) | 70.46±11.14 | 66.42±10.60 | −4.506 | <0.001 | |
| IMB-SMBG scale (total) | 265.34±28.10 | 248.81±28.67 | −6.947 | <0.001 | |
| CES-D | 22.27±7.60 | 21.28±7.80 | −1.529 | 0.127 | |
| No depressive symptoms (≤21)* | 90 (25.5%) | 263 (74.5%) | 1.342 | 0.247 | |
| Depressive symptoms (>21)* | 108 (29.3%) | 260 (70.7%) | |||
| GSES | 2.37±0.58 | 2.40±0.60 | 0.738 | 0.461 | |
| SCSQ (positive part) | 1.54±0.56 | 1.60±0.58 | 1.379 | 0.168 | |
| SCSQ (negative part) | 1.23±0.49 | 1.25±0.58 | 0.538 | 0.591 | |
| Numerical Pain Rating Scale | 2.99±2.25 | 2.91±2.08 | −0.500 | 0.618 | |
Note: *The description of patients with and without depressive symptoms was presented with the number (%). The scores of diabetes-related and psychological scales were listed and compared between population with and without SMBG adherence.
Abbreviations: IMB, information-motivation-behavioral; SMBG, self-monitoring of blood glucose; CES-D, the center for epidemiologic studies depression scale; GSES, general self-efficacy scale; SCSQ, simplified coping style questionnaire; SD, standard deviation.
Multivariate logistic regression analysis of factors associated with SMBG adherence
Multivariate logistic regression was conducted to explore the factors associated with SMBG adherence. The covariates of the logistic regression were included based on the univariate comparisons and other variable including education level according to previous medical literature.22
After adjusting for the covariates, the following factors remained significantly associated with better SMBG adherence: male gender (OR =2.338, CI 1.367–3.998), patients with university and postgraduate education (OR =3.780, CI 1.688–8.466), urban medical insurance (OR =2.349, CI 1.237–4.461), government/business subsidies (OR =2.615, CI 1.243–5.502), patients visiting community clinics greater than or equal to 3 times per year (OR =1.804, CI 1.069–3.042) and patients hospitalized greater than or equal to 3 times per year (OR =2.185, CI 1.107–4.314) (Table 4). Patients with T2DM who were current drinkers (OR =0.412, CI 0.207–0.820) had poor SMBG adherence.
Table 4.
Final adjusted multivariable logistic regression with adherence to SMBG
| Variables | Number (%) | β | OR | 95% CI | P-values |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 327 (45.4%) | 0.849 | 2.338 | 1.367–3.998 | 0.002 |
| Education level | |||||
| Primary school and below | 236 (22.5%) | - | 1.000 | - | Reference |
| Secondary school | 339 (27.7%) | 0.410 | 1.507 | 0.865–2.628 | 0.148 |
| University and postgraduate | 146 (34.9%) | 1.330 | 3.780 | 1.688–8.466 | 0.001 |
| Medical fee payment method | |||||
| Rural cooperative medical insurance | 237 (27.8%) | - | 1.000 | - | Reference |
| Urban medical insurance | 327 (22.9%) | 0.854 | 2.349 | 1.237–4.461 | 0.009 |
| Self-payment | 49 (24.5%) | 0.835 | 2.305 | 0.873–6.081 | 0.092 |
| Government/business subsidy | 108 (41.7%) | 0.961 | 2.615 | 1.243–5.502 | 0.011 |
| Drinking status | |||||
| Never drinks | 564 (26.1%) | - | 1.000 | - | Reference |
| Previous drinker | 59 (44.1%) | 0.087 | 1.091 | 0.507–2.349 | 0.824 |
| Current drinker | 98 (25.5%) | −0.886 | 0.412 | 0.207–0.820 | 0.012 |
| Frequency of visiting community clinics per year | |||||
| ≥3 | 552/169 | 0.590 | 1.804 | 1.069–3.042 | 0.027 |
| Frequency of hospitalization per year | |||||
| ≥3 | 642/79 | 0.782 | 2.185 | 1.107–4.314 | 0.024 |
| Treatment regimen | |||||
| Diet/exercise (no drugs) | 249 (20.5%) | 1.262 | 3.534 | 1.841–6.783 | <0.001 |
| Oral hypoglycemic agents (OHAs) | 224 (36.6%) | 1.317 | 3.731 | 2.162–6.437 | <0.001 |
| Insulin (with/without OHAs) | 248 (26.2%) | - | 1.000 | - | Reference |
| Having own blood glucose meter | |||||
| Yes | 356/365 | 1.934 | 6.916 | 4.054–11.800 | <0.001 |
| Knowing the recommendation on frequency of SMBG | |||||
| Yes | 446/275 | 2.363 | 10.625 | 5.530–20.413 | <0.001 |
| IMB-SMBG scale (information part) | - | 0.067 | 1.069 | 1.028–1.113 | 0.001 |
| IMB-SMBG scale (motivation part) | - | 0.069 | 1.071 | 1.029–1.115 | 0.001 |
Note: Factors significantly associated with better SMBG adherence were listed in the final multivariable logistic regression model.
Abbreviations: IMB, information-motivation-behavioral; SMBG, self-monitoring of blood glucose; OR, odds ratio; CI, confidence interval.
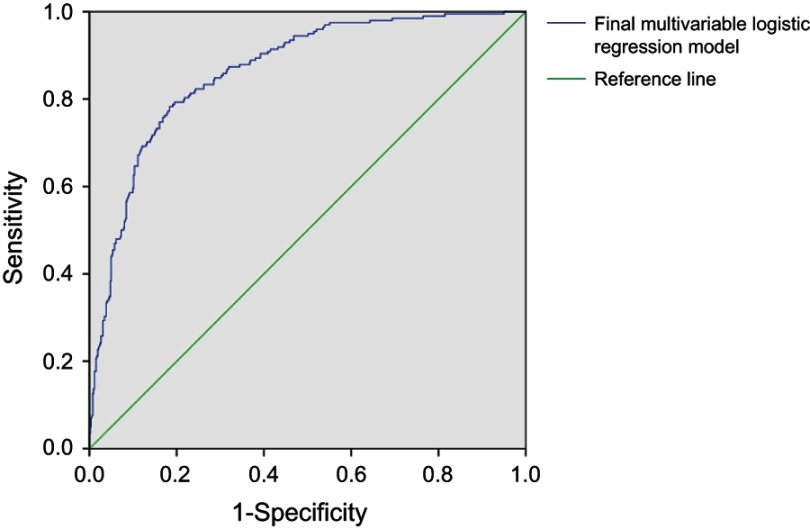
On the psychological scales, higher scores in the information part (OR =1.069, CI 1.028–1.113) and the motivation part (OR =1.071, CI 1.029–1.115) of the IMB-SMBG were associated with better SMBG adherence. As for the SMBG-related factors, patients who had own their blood glucose meter (OR =6.916, CI 4.054–11.800) and knew the recommendation on SMBG frequency from doctors (OR =10.625, CI 5.530–20.413) tended to have better SMBG adherence. Compared with insulin injection, SMBG adherence was easier to achieve if the patients were on diet or exercise regimens (OR =3.534, CI 1.841–6.783) and on OHA prescriptions (OR =3.731, CI 2.162–6.437). ROC curve was developed to assess the potential of the final multivariable logistic regression model (Figure 1). The ROC curve indicated optimal predictive capability (AUC =0.864, CI 0.836–0893). The final multivariable logistic model was validated via 1,000 bootstrap samples (Table S1).
Figure 1.
ROC curve of the final multivariable logistic regression model. The blue curve, the final multivariable logistic regression model including gender, education level, medical fee payment method, drinking status, frequency of visiting community clinics per year, frequency of hospitalization per year, treatment regimen, having own blood glucose meter, knowing the recommendation on frequency of SMBG and the score of information and motivation part in IMB-SMBG scale. AUC =0.864 (95% CI, 0.836–0893).
Table S1.
Bootstrap OR estimates versus initial OR estimates for the final model
| Variable at baseline | Initial estimates | Bootstrap estimates | ||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Male | 2.338 | 1.367–3.998 | 2.338 | 1.365–3.999 |
| University and postgraduate | 3.78 | 1.688–8.466 | 3.782 | 1.684–8.462 |
| Urban medical insurance | 2.349 | 1.237–4.461 | 2.351 | 1.234–4.468 |
| Government/business subsidy | 2.615 | 1.243–5.502 | 2.614 | 1.241–5.501 |
| Current drinker | 0.412 | 0.207–0.820 | 0.412 | 0.205–0.821 |
| Frequency of visiting community clinics per year ≥3 | 1.804 | 1.069–3.042 | 1.802 | 1.068–3.041 |
| Frequency of hospitalization per year ≥3 | 2.185 | 1.107–4.314 | 2.185 | 1.112–4.311 |
| Diet/exercise (no drugs) | 3.534 | 1.841–6.783 | 3.533 | 1.838–6.779 |
| Oral hypoglycemic agents (OHAs) | 3.731 | 2.162–6.437 | 3.731 | 2.162–6.437 |
| Having own blood glucose meter | 6.916 | 4.054–11.800 | 6.917 | 4.042–11.901 |
| Knowing the recommendation on frequency of SMBG | 10.625 | 5.530–20.413 | 10.625 | 5.535–20.407 |
| IMB-SMBG scale (information part) | 1.069 | 1.028–1.113 | 1.069 | 1.027–1.113 |
| IMB-SMBG scale (motivation part) | 1.071 | 1.029–1.115 | 1.071 | 1.025–1.118 |
Note: 1,000 bootstrap samples of the 721 patients with T2DM were performed to validate the final multivariable logistic regression model.
Abbreviations: IMB, information-motivation-behavioral; SMBG, self-monitoring of blood glucose; OR, odds ratio; CI, confidence interval.
Discussion
SMBG is critical for the systematic management of diabetes, though the proportion of patients with SMBG adherence was relatively low. In this cross-sectional analysis, the total proportion of SMBG adherence was 27.5% (198/721) and this proportion was consistent with the results of two previous Chinese studies.12,41 The rate of SMBG adherence in Western countries seems comparatively higher than that in China. The cross-sectional survey concerning SMBG in the United Kingdom in 2008 suggested that 49.8% (276/554) of patients followed the physician’s advice.15 And for a study on SMBG practice conducted in the United States in 2007,42 the daily SMBG rate was about 63.4% in the patients with diabetes and close to 86.7% for patients with T2DM on insulin treatment. The difference in rate may derive from the various definitions of SMBG adherence, but there is actually an obvious gap with the developed countries in terms of achieving the recommended frequency of SMBG.
The rate of SMBG adherence varied under different treatment methods. The rate of patients on diet or exercise regimens who performed SMBG according to the recommendation was the lowest in this study, compared with patients receiving other types of treatment. Patients treated by diet or exercise were usually at an early stage of diabetes and these patients just needed to perform SMBG at least once during a certain interval of time, so as to promote lifestyle modification.6 There is relatively less attention devoted to the diabetic condition of these patients,43 thus accounting for the low rates of adherence in these patients. In this study, the rate of SMBG adherence in patients on OHAs was much higher than that of patients on insulin injection. However, the association between OHAs and SMBG adherence seems to be opposite in one Chinese study, in which patients under OHAs tended to be poor SMBG adherence.18 One reason between the difference might be the different definitions of SMBG adherence. In the previous study, SMBG adherence was defined as the mean SMBG frequency in one week over 3-month period according to one guideline released in 2015,44 while there was notable difference of the exact recommended SMBG frequency between this guideline and the latest one. Besides, the SMBG frequency was collect via a portable glucose monitoring device. The use of this device might be hard for older patients with low level education, thus leading to possible selection bias at the beginning of the previous study. The frequency of SMBG of patients with T2DM in this study, by contrast, was significantly higher in the patients treated with insulin. Previous studies have indicated the frequency of SMBG was significantly correlated with treatment regimen and the purposes of performing it, and the frequency of SMBG was much higher in patients using insulin.13,15,41 Plenty of patients on insulin need to inject insulin repeatedly each day, so performing SMBG daily or before each meal could help them determine their blood-glucose level and then adjust the insulin dose accordingly. The paradox between the frequency of SMBG and the rate of SMBG adherence could be explained by the official guidelines on the prevention and control of T2DM in China provided by the CDS in 2017.6 The high frequency of SMBG recommended by the CDS underlines the importance of SMBG for patients on insulin injection.
The suboptimal adherence of SMBG also reflected low awareness of self-management in patients with T2DM. In our study, the patients who were familiar with the recommendation on SMBG frequency showed better compliance, and patients with T2DM on insulin injection are supposed to perform more SMBG to meet the frequency criterion and their medical workers need to conduct health education on SMBG. In addition, previous studies showed that after obtaining their results, most patients with T2DM tended to take no action because of a lack of health education.45 It is the responsibility of health workers in clinics and hospitals to help patients with DM improve their ability to interpret the results after SMBG. We also found that the patients who owned a blood glucose meter tended to be SMBG adherent because owning a blood-testing device may allow patients to perform SMBG easily.
Our study indicated that better adherence to SMBG was associated with the male gender, a higher education level, urban medical insurance, government/business subsidies and the frequency of clinic visits and hospitalization. Current drinkers were associated with poor SMBG adherence. The relationship between gender and SMBG adherence is contrast to one previous study.12 The ratio of female versus male was 1.2 in this study while that was 0.84 in that study. Besides, the ratio of gender in this study is much closer to that in one authoritative research.5 Therefore, the difference may partly come from the selection bias. Further researches concerning the gender effect on SMBG adherence are needed to confirm this result. A previous study confirmed that education level was associated with the self-management of patients with diabetes.46 Patients with a higher education level are more receptive to a doctor’s recommendation and good health behavior, thus leading them to perform SMBG regularly. A study including 798 patients with T2DM conducted in Southeast China revealed that higher education was related to better glycemic control,22 which suggested a possible correlation between SMBG and glucose control. Moreover, better adherence to SMBG was related to a higher frequency of clinic visits and hospitalization. Patients who often visited clinics paid more attention to their health issues and they could obtain the latest recommendations from the physicians that could be used in self-management later, which created a virtuous cycle. As for the patients who were often hospitalized, frequent hospitalization may push them to perform SMBG more frequently. Previous studies have indicated that occupation was significantly related to diabetes and changing psychological work conditions could decrease the risk factors of diabetes.47,48 Drinking alcohol was a risk factor for diabetes based on the studies conducted in Asian populations,49,50 and there was a negative correlation between self-efficacy and drinking behavior.51 Current drinkers usually have a low level of self-efficacy,52 and they tend to perform less SMBG than previous drinkers and patients who never drink. In addition, the empirical evidence has shown a positive correlation between alcohol consumption and BMI,53 and an increased BMI may lead to worse glycemic control.
In this study, the IMB-SMBG questionnaire for patients with T2DM was proven to present the current status of SMBG based on the scores. Patients with SMBG adherence tended to have higher scores in the parts on information, motivation and behavior, which suggested that this questionnaire could be applied to a comprehensive assessment of SMBG in future studies. The information and motivation part play important roles in SMBG adherence, as SMBG adherence may improve significantly with the increase of scores on these two parts. Thus, health workers should probably focus on how to increase the awareness of diabetes-related information in the population with DM and enhance their motivation.
In this analysis, the CES-D was introduced to evaluate the depressive symptoms of patients with T2DM and the cut-off point was set to 21 due to achieve a better balance.34 Nearly 51% of patients had depressive symptoms at different degrees in our study, while merely 34% of patients had similar symptoms within a study undertaken in Germany.54 In another study conducted among elderly patients with DM in Vietnam,55 almost 79.4% of patients had depressive symptoms as assessed by the scales. Patients with diabetes are at greater risk of diabetes-related complications compared with people without diabetes,8,9 thus it’s more likely for them to develop depressive symptoms. The clinical definition of depression and the assessment tools vary from country to country, and patients’ depressive symptoms don’t mean that they have actually developed clinical depression. However, the relationship between SMBG adherence and depressive symptoms is still largely unclear. While the GSES and SCSQ have been proven to evaluate self-efficacy and coping style concerning the management of chronic diseases,56,57 the scores on the GSES and SCSQ didn’t suggest a significant difference between patients with SMBG adherence and SMBG non-adherence. The long-term and repeated process of treatment and monitoring may pose negative effects upon the whole state of psychology, thus impairing self-efficacy and coping style, but the correlation between self-efficacy and the progression of diabetes remains unknown. Further study could delve deeper into the states of self-efficacy and coping styles in different stages of diabetes.
Medical questionnaires have been widely used in various fields and studies in medicine. For the self-management of chronic diseases, special medical questionnaires could assess the demographic and clinical characteristics, treatment outcome, quality of life and other aspects of diseases, which would provide further guidance on future self-management. With the rapid development of information and software technology, the use of smart phones and other portable mobile devices has increased dramatically in recent years. Electronic questionnaires, based on portable mobile devices and mobile applications accessed via the internet, have been proven to improve the response rate, clinical efficiency and doctor-patient communication.58,59 In our study, the self-designed questionnaire was uploaded to the online questionnaire website and could be filled out on smart phones via the internet. The background workstation of the website recorded and stored the questionnaire results, and then automatically calculated the scores of some items, which significantly improved their efficiency and accuracy. The range of time of filling out electronic questionnaires was relatively wide in this study. Some elders may have low-level ability of understanding, thus leading to relatively long time of filling out questionnaires. But with the help of assistants nearby, the questionnaires could be filled out truthfully. Therefore, the electronic questionnaires have extensive prospects in the assessment of chronic diseases.
Strengths and limitations
To the best of our knowledge, this is the first study conducted with electronic questionnaires concerning the current status and influential factors of SMBG adherence in Chinese patients with T2DM. This study provided up-to-date and accurate data on the present status of SMBG adherence in China and identified important influential factors that could be applied and explored for further study.
However, this study had some limitations that must be mentioned. First, because of the cross-sectional design, we could not draw absolute conclusions about the causal relationships of the demographic and clinical characteristics of SMBG adherence. But the results of this study do provide some evidence and suggestions for the future study of the influential factors of SMBG. Second, most patients included in this study lived in the provincial capital, so patients in the remote areas may not have been adequately considered. Third, the data collection was self-reported, thus the data might be influenced by potential recall bias. In addition, regarding intimate issues in daily life, like income, some patients might not have answered truthfully. The sample size of this study was relatively limited and further subgroup analysis based on the treatment type need to be conducted. This study did not include an index of blood sugar, like fasting blood glucose or glycosylated hemoglobin (HbA1c), to assess glycemic control, and a future study could focus on the association between SMBG adherence and glycemic control.
Conclusions and recommendations
In summary, most of the Chinese patients with T2DM did not adhere to the SMBG frequency recommended by the CDS. In addition, this study suggested that several factors, including gender, medical fee payment methods, drinking status, the frequency of clinic visits and hospitalization, the treatment regimen, owning a blood glucose meter and knowing the recommended frequency of SMBG were associated with SMBG adherence. Our study also highlights the importance of health education, especially for patients on insulin, who often need to know their blood-glucose level and adjust their insulin dose accordingly. Based on the practical factors, patients with T2DM are encouraged to learn the recommended frequency of SMBG and use own blood glucose meter to perform SMBG. Manufacturers producing the blood glucose meter should make the device more portable and the man-machine interface friendlier. Furthermore, some applications and programs of the device need to be developed to record and analyze the blood glucose level, which is helpful to assess the history and adjust the dose of insulin.
There is clearly a need for prospective, multicenter, large-scale trials to explore the reasons for patients’ failure to meet the recommended frequency of SMBG. Further studies should establish a scientific and standardized system to train investigators, collect data and analyze the results, so as to increase the efficacy and accuracy of the program.
Acknowledgments
We thank Sinocare Diabetes Foundation for improving public cognition of diabetes mellitus.
Disclosure
The authors report no conflicts of interest in this work.
Supplementary material
References
- 1.Collaboration ERF. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med. 2011;364(9):829–841. doi: 10.1056/NEJMoa1008862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogurtsova K, Da Rocha Fernandes JD, Huang Y, et al. IDF Diabetes Atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017;128:40–50. doi: 10.1016/j.diabres.2017.03.024 [DOI] [PubMed] [Google Scholar]
- 3.Chatterjee S, Khunti K, Davies MJ. Type 2 diabetes. Lancet. 2017;389(10085):2239–2251. doi: 10.1016/S0140-6736(17)30058-2 [DOI] [PubMed] [Google Scholar]
- 4.Atlas D. International diabetes federation. IDF Diabetes Atlas. 7th ed. Brussels (Belgium): International Diabetes Federation; 2015. [Google Scholar]
- 5.Wang L, Gao P, Zhang M, et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA. 2017;317(24):2515–2523. doi: 10.1001/jama.2017.7596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Society. CD. Guidelines for the prevention and control of type 2 diabetes in China (2017 Edition). ChiN J Pract Internal Med. 2018;38(4):292–344. [Google Scholar]
- 7.Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA. 2015;314(10):1021–1029. doi: 10.1001/jama.2015.10029 [DOI] [PubMed] [Google Scholar]
- 8.Bragg F, Holmes MV, Iona A, et al. Association Between Diabetes and Cause-Specific Mortality in Rural and Urban Areas of China. JAMA. 2017;317(3):280–289. doi: 10.1001/jama.2016.19720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stratton IM, Adler AI, Neil HAW, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–412. doi: 10.1136/bmj.321.7258.405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Polonsky WH, Fisher L, Schikman CH, et al. Structured self-monitoring of blood glucose significantly reduces A1C levels in poorly controlled, noninsulin-treated type 2 diabetes: results from the Structured Testing Program study. Diabetes Care. 2011;34(2):262–267. doi: 10.2337/dc10-1732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miller KM, Beck RW, Bergenstal RM, et al. Evidence of a strong association between frequency of self-monitoring of blood glucose and hemoglobin A1c levels in T1D exchange clinic registry participants. Diabetes Care. 2013;36(7):2009–2014. doi: 10.2337/dc12-1770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yuan L, Guo X, Xiong Z, et al. Self-monitoring of blood glucose in type 2 diabetic patients in China: current status and influential factors. Chin Med J (Engl). 2014;127(2):201–207. [PubMed] [Google Scholar]
- 13.Al-Keilani MS, Almomani BA, Al-Sawalha NA, Shhabat BA. Self-monitoring of blood glucose among patients with diabetes in Jordan: perception, adherence, and influential factors. Diabetes Res Clin Pract. 2017;126:79–85. doi: 10.1016/j.diabres.2017.01.005 [DOI] [PubMed] [Google Scholar]
- 14.Claude Mbanya J, Aschner P, Chan JCN, Jose Gagliardino J, Saji J. Self-monitoring of blood glucose (SMBG) and glycaemic control in Cameroon: results of the International Diabetes Management Practices Study (IDMPS). Diabetes Res Clin Pract. 2017;126:198–201. doi: 10.1016/j.diabres.2016.11.029 [DOI] [PubMed] [Google Scholar]
- 15.Farmer A, Balman E, Gadsby R, et al. Frequency of self-monitoring of blood glucose in patients with type 2 diabetes: association with hypoglycaemic events. Curr Med Res Opin. 2008;24(11):3097–3104. doi: 10.1185/03007990802473062 [DOI] [PubMed] [Google Scholar]
- 16.Chan JC, Gagliardino JJ, Baik SH, et al. Multifaceted determinants for achieving glycemic control: the International Diabetes Management Practice Study (IDMPS). Diabetes Care. 2009;32(2):227–233. doi: 10.2337/dc08-0435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vincze G, Barner JC, Lopez D. Factors associated with adherence to self-monitoring of blood glucose among persons with diabetes. Diabetes Educ. 2004;30(1):112–125. doi: 10.1177/014572170403000119 [DOI] [PubMed] [Google Scholar]
- 18.Hu ZD, Zhang KP, Huang Y, Zhu S. Compliance to self-monitoring of blood glucose among patients with type 2 diabetes mellitus and its influential factors: a real-world cross-sectional study based on the Tencent TDF-I blood glucose monitoring platform. Mhealth. 2017;3:25. doi: 10.21037/mhealth.2017.06.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wambui Charity K, Kumar AMV, Hinderaker SG, Chinnakali P, Pastakia SD, Kamano J. Do diabetes mellitus patients adhere to self-monitoring of blood glucose (SMBG) and is this associated with glycemic control? Experiences from a SMBG program in western Kenya. Diabetes Res Clin Pract. 2016;112:37–43. doi: 10.1016/j.diabres.2015.11.006 [DOI] [PubMed] [Google Scholar]
- 20.Martin S, Schneider B, Heinemann L, et al. Self-monitoring of blood glucose in type 2 diabetes and long-term outcome: an epidemiological cohort study. Diabetologia. 2006;49(2):271–278. doi: 10.1007/s00125-005-0083-5 [DOI] [PubMed] [Google Scholar]
- 21.Fujisawa T, Ikegami H, Kasayama S, et al. Age-dependent difference in factors affecting choice of system for self-monitoring of blood glucose. Diabetes Res Clin Pract. 2008;79(1):103–107. doi: 10.1016/j.diabres.2007.08.012 [DOI] [PubMed] [Google Scholar]
- 22.Zeng Y, Wu J, Han Y, et al. Educational disparities in the associations between self-monitoring of blood glucose and glycemic control in type 2 diabetes patients in Xiamen, China. J Diabetes. 2018;10(9):715–723. doi: 10.1111/1753-0407.12651 [DOI] [PubMed] [Google Scholar]
- 23.Shigaki C, Kruse RL, Mehr D, et al. Motivation and diabetes self-management. Chronic Illn. 2010;6(3):202–214. doi: 10.1177/1742395310375630 [DOI] [PubMed] [Google Scholar]
- 24.Beeney LJ, Bakry AA, Dunn SM. Patient psychological and information needs when the diagnosis is diabetes. Patient Educ Couns. 1996;29(1):109–116. [DOI] [PubMed] [Google Scholar]
- 25.Osborn CY, Egede LE. Validation of an Information-Motivation-Behavioral Skills model of diabetes self-care (IMB-DSC). Patient Educ Couns. 2010;79(1):49–54. doi: 10.1016/j.pec.2009.07.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grey M, Schulman-Green D, Knafl K, Reynolds NR. A revised self- and family management framework. Nurs Outlook. 2015;63(2):162–170. doi: 10.1016/j.outlook.2014.10.003 [DOI] [PubMed] [Google Scholar]
- 27.Arifin WN. Random sampling and allocation using SPSS. Educ Med J. 2012;4(1). doi: 10.5959/eimj.v4i1.4 [DOI] [Google Scholar]
- 28.World Health Organization. Definition, Diagnosis and Classification of Diabetes Mellitus and Its Complications: Report of a WHO Consultation. Part 1, Diagnosis and Classification of Diabetes Mellitus. Geneva: World Health Organization; 1999. [Google Scholar]
- 29.Krejcie RV, Morgan DW. Determining sample size for research activities. Educ Psychol Meas. 1970;30(3):607–610. doi: 10.1177/001316447003000308 [DOI] [Google Scholar]
- 30.Gao J, Wang J, Zhu Y, Yu J. Validation of an information-motivation-behavioral skills model of self-care among Chinese adults with type 2 diabetes. BMC Public Health. 2013;13:100. doi: 10.1186/1471-2458-13-100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mayberry LS, Osborn CY. Empirical validation of the information-motivation-behavioral skills model of diabetes medication adherence: a framework for intervention. Diabetes Care. 2014;37(5):1246–1253. doi: 10.2337/dc13-1828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Qin Z-Y, Yan J-H, Yang D-Z, Deng H-R, Yao B, Weng J-P. Behavioral analysis of Chinese adult patients with type 1 diabetes on self-monitoring of blood glucose. Chin Med J. 2017;130(1):39–44. doi: 10.4103/0366-6999.196574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- 34.Zhang Y, Ting RZ, Lam MH, et al. Measuring depression with CES-D in Chinese patients with type 2 diabetes: the validity and its comparison to PHQ-9. BMC Psychiatry. 2015;15:198. doi: 10.1186/s12888-015-0580-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schwarzer R, Bäßler J, Kwiatek P, Schröder K, Zhang JX. The assessment of optimistic self‐beliefs: comparison of the German, Spanish, and Chinese versions of the general self‐efficacy scale. Appl Psychol. 1997;46(1):69–88. doi: 10.1111/apps.1997.46.issue-1 [DOI] [Google Scholar]
- 36.Xie Y. Reliability and validity of the simplified Coping Style Questionnaire. Chin J Clin Psychol. 1998;6(2):114–115. [Google Scholar]
- 37.Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. [DOI] [PubMed] [Google Scholar]
- 38.Chen C, Lu F. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci. 2004;17:1. [PubMed] [Google Scholar]
- 39.Bland JM, Altman DG. Multiple significance tests: the Bonferroni method. BMJ. 1995;310(6973):170. doi: 10.1136/bmj.310.6973.170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hochberg J, AC T. Multiple Comparison Procedures. John Wiley & Sons; Hoboken, NJ: 1987. [Google Scholar]
- 41.Ji L, Su Q, Feng B, et al. Glycemic control and self-monitoring of blood glucose in Chinese patients with type 2 diabetes on insulin: baseline results from the COMPASS study. Diabetes Res Clin Pract. 2016;112:82–87. doi: 10.1016/j.diabres.2015.08.005 [DOI] [PubMed] [Google Scholar]
- 42.Control CfD, Prevention. Self-monitoring of blood glucose among adults with diabetes–United States, 1997–2006. MMWR Morb Mortal Wkly Rep. 2007;56(43):1133. [PubMed] [Google Scholar]
- 43.Maclean HM. Patterns of diet related self-care in diabetes. Soc Sci Med. 1991;32(6):689–696. doi: 10.1016/0277-9536(91)90148-6 [DOI] [PubMed] [Google Scholar]
- 44.Society CD. Clinical application guideline of blood glucose monitoring in China (2015). Chin J Diabetes Mellitus. 2015;7:603–613. [Google Scholar]
- 45.Evans JM, Mackison D, Swanson V, Donnan PT, Emslie-Smith A, Lawton J. Self-monitoring among non-insulin treated patients with type 2 diabetes mellitus: patients’ behavioural responses to readings and associations with glycaemic control. Diabetes Res Clin Pract. 2013;100(2):235–242. doi: 10.1016/j.diabres.2013.03.005 [DOI] [PubMed] [Google Scholar]
- 46.Walker RJ, Smalls BL, Campbell JA, Williams JLS, Egede LE. Impact of social determinants of health on outcomes for type 2 diabetes: a systematic review. Endocrine. 2014;47(1):29–48. doi: 10.1007/s12020-014-0195-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Adekanmbi VT, Uthman OA, Erqou S, Echouffo-Tcheugui JB, Harhay MN, Harhay MO. Epidemiology of prediabetes and diabetes in Namibia, Africa: a multilevel analysis. J Diabetes. 2019;11(2):161–172. doi: 10.1111/1753-0407.12829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lian Y, Sun Q, Guan S, et al. Effect of changing work stressors and coping resources on the risk of type 2 diabetes: the OHSPIW Cohort Study. Diabetes Care. 2018;41(3):453–460. doi: 10.2337/dc17-0749 [DOI] [PubMed] [Google Scholar]
- 49.Liang Z, Qiu QY, Wu JH, et al. Alcohol drinking, dyslipidemia, and diabetes: a population-based prospective cohort study among inner mongolians in China. Biomed Environ Sci. 2016;29(8):555–562. doi: 10.3967/bes2016.074 [DOI] [PubMed] [Google Scholar]
- 50.Hong SW, Linton JA, Shim JY, Kang HT. High-risk drinking is associated with a higher risk of diabetes mellitus in Korean men, based on the 2010–2012 KNHANES. Alcohol (Fayetteville, NY). 2015;49(3):275–281. doi: 10.1016/j.alcohol.2015.02.004 [DOI] [PubMed] [Google Scholar]
- 51.Dill PL, Wells-Parker E, Cross GW, et al. The relationship between depressed mood, self-efficacy and affective states during the drinking driving sequence. Addict Behav. 2007;32(8):1714–1718. doi: 10.1016/j.addbeh.2006.11.011 [DOI] [PubMed] [Google Scholar]
- 52.Chomsri P, Likhitsathian S, Aramrattana A, Siviroj P. Self-efficacy, sensation seeking, right attitude, and readiness to change among alcohol drinkers in a Thai vocational school. Addict Behav Rep. 2018;8:107–112. doi: 10.1016/j.abrep.2018.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Smarandescu L, Walker D, Wansink B. Mindless drinking: how gender and BMI relate to the consumption of alcohol. Int J Drug Policy. 2014;25(6):1131–1134. doi: 10.1016/j.drugpo.2014.08.018 [DOI] [PubMed] [Google Scholar]
- 54.Rathmann W, Kuss O, Anderson D, et al. Increased depression symptom score in newly diagnosed type 2 diabetes patients. Psychiatry Res. 2018;261:259–263. doi: 10.1016/j.psychres.2017.12.091 [DOI] [PubMed] [Google Scholar]
- 55.Vu HTT, Nguyen TX, Nguyen HTT, et al. Depressive symptoms among elderly diabetic patients in Vietnam. Diabetes Metab Syndr Obes. 2018;11:659–665. doi: 10.2147/DMSO.S179071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang M, Sun H, Zhang J, Ruan J. Prevalence and associated factors of elder abuse in family caregivers of older people with dementia in central China cross-sectional study. Int J Geriatr Psychiatry. 2019;34(2):299–307. doi: 10.1002/gps.5020 [DOI] [PubMed] [Google Scholar]
- 57.Zhou H, Zhu J, Liu L, et al. Diabetes-related distress and its associated factors among patients with type 2 diabetes mellitus in China. Psychiatry Res. 2017;252:45–50. doi: 10.1016/j.psychres.2017.02.049 [DOI] [PubMed] [Google Scholar]
- 58.Palmer C, Farhan B, Nguyen N, et al. Are electronic and paper questionnaires equivalent to assess patients with overactive bladder? J Urol. 2018;200(2):369–374. doi: 10.1016/j.juro.2018.03.117 [DOI] [PubMed] [Google Scholar]
- 59.Tambalis KD, Panagiotakos DB, Psarra G, Sidossis LS. Insufficient sleep duration is associated with dietary habits, screen time, and obesity in children. J Clin Sleep Med. 2018;14(10):1689–1696. doi: 10.5664/jcsm.7374 [DOI] [PMC free article] [PubMed] [Google Scholar]