Abstract
Introduction
Some studies in developing countries have shown that infant mortality is highly associated with maternal education, implying that maternal education might play an important role in the reduction of infant mortality. However, other research has shown that lower levels of maternal education does not have any significant contribution to infant survival. In this systematic review, we focus on the effect of different levels of maternal education on infant mortality in Ethiopia.
Methods
MEDLINE, EMBASE, CINAHL, Scopus, and Maternity and Infant Care databases were searched between November 15, 2017 and February 20, 2018. All articles published until February 20, 2018 were included in the study. The data extraction was conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA 2009) guidelines. An I2 test was used to assess heterogeneity and a funnel plot was used to check publication bias.
Findings
We retrieved 441 records after removing duplications. During screening, 31 articles were fully accessed for data extraction. Finally, five articles were included for analysis. The overall pooled estimate indicated that attending primary education was associated with a 28% reduction in the odds of infant mortality compared to those infants born to mothers who were illiterate, OR: 0.72 (95% CI = 0.66, 0.78). Another pooled estimate indicated that attending secondary education and above was associated with a 45% reduction in the odds of infant mortality compared to those infants born to mothers who were illiterate, OR: 0.55 (95% CI = 0.47, 0.64).
Conclusion
From this study, understanding the long-term impact of maternal education may contribute to reduce infant mortality. Therefore, policy makers should give more attention in promoting the role of women through removing institutional and cultural barriers, which hinder women from access to education in order to reduce infant mortality in Ethiopia.
Introduction
The infant mortality rate is one of the most important indices for gauging the overall level of public health and the social and economic development of a country or region [1]. At the beginning of the Sustainable Development Goals (SDGs) era in 2016, maternal and child mortality remained unacceptably high, especially in sub-Saharan Africa countries [2]. In the last two decades there has been a global underinvestment in the health of newborns and infants, and as a result of this, millions of preventable deaths occur each year [3]. At the end of the Millennium Development Goals in 2015, despite the policy support provided during this period, 4.5 million infant deaths occurred globally; and most of these deaths were in developing countries [4].
Africa has the highest infant mortality rate of all the regions of the world. According to the World Health Organization report in 2015, the global infant mortality rate was 32 per 1000 live births compared to the Sub-Saharan Africa region rate of 56 per 1000 live births [1].
The infant mortality rate in Ethiopia is one of the highest in Africa [5, 6]. According to the 2016 Ethiopian Demographic and Health Survey report, infant mortality was 48 per 1000 live births [5, 6]. Nevertheless, the infant mortality rate in Ethiopia has shown a 50% reduction in the last 16 years [6]. Several studies in developing countries have shown that infant mortality is highly associated with maternal education [7–9]. According to social science researchers, maternal education is one of the most important determinants of infant mortality [10–12]. Education is proposed to increase a mother’s knowledge of health care practices related to contraceptive utilization, nutrition, hygiene and disease prevention [13]. Education is also an important determinant of social and economic development and is strongly associated with various socioeconomic measures such as lifestyle, income, and fertility for both individuals and society [6, 13].
In Ethiopia, 51% of females age six and over have ever attended school and primary school is the highest level of education completed or attended for the majority of women [6]. In the 2016 Ethiopian Demographic and Health Survey report, only 4% of women completed secondary school or went beyond secondary school [6].
Educated mothers have been found to use information in a more effective way when caring for children and tend to seek appropriate health care more effectively than mothers who are not educated [14]. Research conducted in Nigeria showed that education has also been found to enable mothers to be more autonomous, to resist harmful traditional influences and practices, and to make economic decisions to spend more on caring for children [15]. Another research conducted in in India and Pakistan indicated that eeducated mothers are also more likely to change traditional practices such as feeding and childcare practices, and make changes in fertility preferences [16]. Furthermore, maternal education increases women’s involvement in family decisions and increases demand for health services such as antenatal care utilization and institutional delivery [17]. Educated mothers are also likely to carry out key components of newborn care such as weighing the infant at birth and not giving a prelacteal feed [18]. Maternal education is also more likely to generate income for the family and increase total family resources [19]. This may be through employment, as educated women are more likely to have paid work than uneducated women [20].
Despite the reported benefits of maternal education, some research in India and Ethiopia has shown that primary school and informal education does not have any significant contribution to the survival of infants or children [21, 22]. These findings suggest that level of education is an important factor to consider for infant and child survival, particularly since most women in Ethiopia who are educated are not educated beyond primary school level [6]. In the following systematic review, we focus on the effect of maternal education on infant mortality in Ethiopia. This systematic review is limited to Ethiopia because the categorization of education levels vary from nation to nation, which may prevent coherent results. Reviewing the effect of maternal education in one nation where infant mortality is a serious problem, namely Ethiopia, might provide important information, which can help for policy development in the nation. Therefore, the aim of this systematic review is to assess the effect of different levels of maternal education on infant mortality in Ethiopia.
Method
Search strategy
Several electronic databases were searched including MEDLINE, EMBASE, CINAHL, Scopus, and Maternity and Infant Care. The article search was started on November 15, 2017 and ended on February 20, 2018. We used a combination of multiple key terms including determinant, risk factor, child, infant, perinatal, neonatal, mortality, educational status, maternal education, education, mother, maternal, and Ethiopia. A search strategy was developed in the MEDLINE database and applied to the other electronic databases (see S1 Table). We also manually searched the reference lists of included articles.
Inclusion and exclusion criteria
Journals, describing observational studies conducted in Ethiopia (case control, cohort and analytical cross sectional studies) that assessed the relationship between maternal education and infant mortality were included. In this systematic review, infant mortality was defined as death of a child less than one year of age. All papers published until February 20, 2018 were included in this review. Death of child less than 28 days old (neonatal mortality) and death of child less than five years old (child mortality) was excluded from the study. Research conducted outside of Ethiopia was also excluded from the study.
Assessment of methodological quality
Manuscripts selected for analysis were assessed by two independent reviewers (GK, TT). For methodological validity, standardized critical appraisal instruments from the Joanna Briggs Institute Meta-Analysis of Statistics Assessment and Review Instrument (JBI-MAStARI) were used [23]. The critical appraisal checklists used in this study were for observational studies, such as analytical cross sectional studies [24], cohort [25] and case control [26] studies (see Table 1). Any disagreements that arose between reviewers were resolved through discussion. We did not exclude papers based on the methodological quality due to very few papers being eligible for the final analysis.
Table 1. List of studies included to show the effect of maternal education on infant mortality in Ethiopia.
| Authors | Study design and setting | Study population and sample size | Education category | Methodological quality |
|---|---|---|---|---|
| Asefa M et al, 2000 [8] | Community based cohort study | 8273 infants’ mothers were interviewed | No Education (no formal education) Primary education (Grade 1 to Grade 8) Secondary and above (Grade 9 and above) |
9/11 |
| Muluye S. & Wencheko E.,2005 [29] | Community based cross-sectional study | 9861 children’s mothers were interviewed | No Education Primary education Secondary and above |
7/8 |
| Dube L et al, 2013 [30] | Community based matched case control study | 254 infants’ mothers were interviewed | Illiterate Primary Secondary and above |
10/10 |
| Alemayehu et al, 2015 [31] | Population based cross-sectional study | A total of 16,267 women with 25,472 births | No Education Primary education Secondary and above |
8/8 |
| Kumar PP. and File G. 2015 [32] | Population based cross-sectional study | 14,070 children mother were interviewed | illiterate Primary Secondary & above |
6//8 |
Data extraction
The data extraction was conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA 2009) guidelines [27]. The relevance of each study was checked based on its title, objectives, and methodology. Firstly, articles were excluded based on their title. Then, abstracts were assessed and excluded if they did not match the current study objectives. For the remainder, the entire content of the articles was accessed and selected based on the exposure (maternal education) and dependent outcome (infant mortality) under review. Data extraction included specific details about the study design (cross sectional, case control and cohort), the sample size, and the number of events among exposure (the number of infant deaths among women with primary education and the number of infant deaths among women with secondary education and above) (see Table 1).
Data analysis
Information extracted from each original study was analyzed using RevMan5 software (include citation information here as per journal guidelines). A Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) checklist was used to report the results of the study [28]. A Funnel plot asymmetry in the random effects model was used to check for publication bias. The summary effect measure used was an odds ratio. We used the I2 and chi squared test to examine the heterogeneity of studies. The assumption of heterogeneity is there is no difference among studies, and if the value of I2 is greater than 70%, it indicates that there is a substantial variability among the studies.
Results
Search result
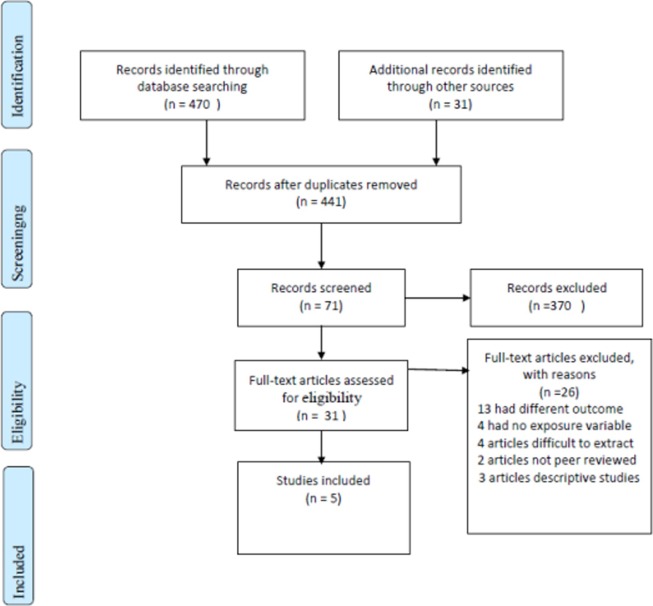
We retrieved 470 records from the database search and 31 records using hand searches from the reference lists of all previous articles. After removal of duplicate articles, 441 records remained. From these, 370 records were excluded in the initial screening because their title was not related to this systematic review. For the remaining 71 articles, abstracts were accessed and screened. From these, 40 articles were excluded due to the irrelevance of the exposure and outcome. From these remaining 31 articles, thirteen were excluded due to the outcome variable being different, such as under-five mortality and neonatal mortality. Four articles were excluded due to the exposure not being according to inclusion criteria. Another four articles were also excluded as the authors reported only the odds ratio, making it impossible to extract the data necessary for this analysis. We tried to communicate the authors through their email address to access the data, with no response. Five articles were also excluded due to not being peer reviewed and for reporting descriptive statistics only. Finally, five articles were included for analysis (Fig 1).
Fig 1. PRISMA flow diagram showing the procedure of selecting studies for meta-analysis in Ethiopia.
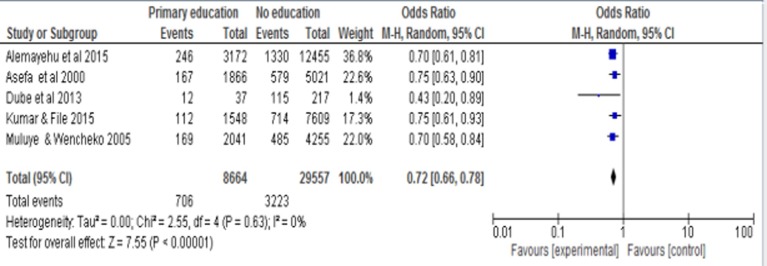
Effect of primary education on infant mortality
The overall pooled odds ratio estimate was 0.72 (95% CI = 0.66, 0.78). This pooled estimate indicated that attending primary education was associated with a 28% reduction in the odds of infant mortality compared to those infants born to mothers who were illiterate (Fig 2).
Fig 2. Forest plot of five studies to show the effect of primary maternal education on infant mortality in Ethiopia.
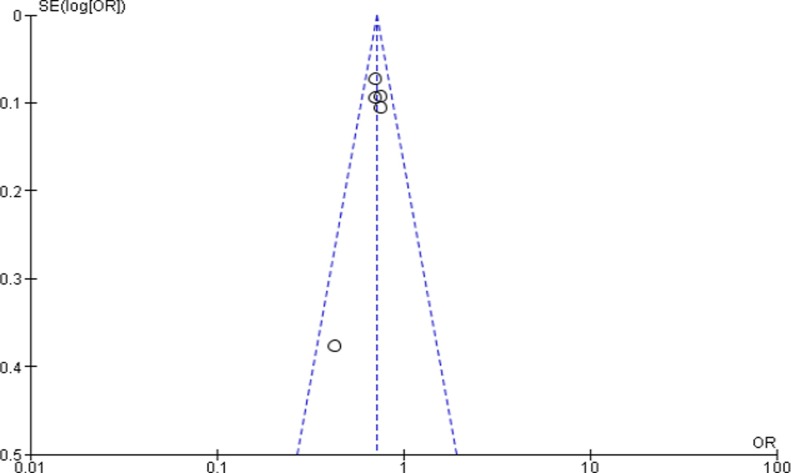
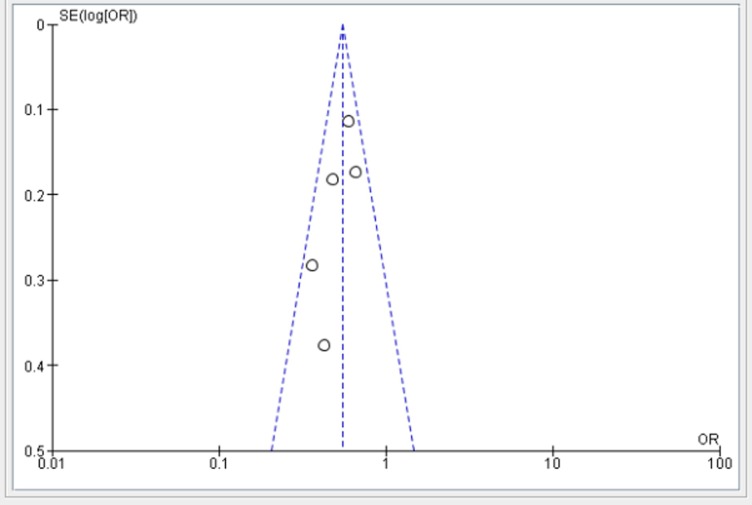
The funnel plot showed that there is no evidence of publication bias (Fig 3). Regarding heterogeneity, there was no significant difference among the five studies (p = 0.63) indicating that there is no significant variability among the studies.
Fig 3. Funnel plot of five studies to show the effect of primary maternal education on infant mortality in Ethiopia.
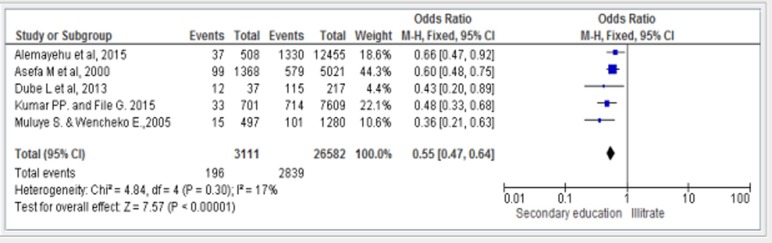
Effect of secondary education and above on infant mortality
The overall pooled odds ratio for the effect of secondary education was 0.55 (95% CI = 0.47, 0.64). This pooled estimate indicates that attending secondary education and above was associated with a reduction in the odds of infant mortality by 45% compared to those infants born to mothers who were illiterate (Fig 4).
Fig 4. Forest plot of five studies to show the effect of secondary and above maternal education on infant mortality in Ethiopia.
The funnel plot showed that there is no evidence of publication bias (Fig 5). Regarding heterogeneity, there is no significant difference among the five studies (P = 0.30) and I2 of 17% indicating that there was no significant variability among studies.
Fig 5. Funnel plot of five studies to show the effect of secondary and above maternal education on infant mortality in Ethiopia.
Discussion
The overall pooled estimate from the meta analysis showed that there is a strong association between maternal education and infant mortality. The pooled odds ratio for primary education was 0.72 (95% CI = 0.66, 0.78) and the pooled odds ratio for the effect of secondary education on infant mortality was 0.55 (95% CI = 0.47, 0.64).
In Ethiopia, mortality has been found to be higher for infants born to mothers who were illiterate than those whose educational status was secondary and above [33]. The risk of infant death was 3.8 and 3 times higher among mothers who had no education and attended primary education respectively compared to illiterate mothers [29]. In a cross sectional survey from two rounds of nationally representative data among 45,952 live births, it was shown that a mother who completed high school was 31% less likely to experience the death of an infant than a mother with no education [31]. In a study in Addis Ababa from a population and housing census, researchers also reported that child survival is greater among educated mothers and the impact of maternal education was generally more important in the step from primary to secondary schooling than from the illiterate to the literate group [34]. In addition, researchers in Ethiopia found that children whose mothers have attended secondary or higher education were 42% less likely to die as compared with infants whose mothers have no education [35]. In a longitudinal population-based surveillance in Ethiopia researchers also found that infants had a 56% lower risk of death if they were born to mothers who attained secondary school and above compared to those infants whose mothers did not attend formal education [21]. In the 2016 Ethiopian Health Survey report, the rate of infant mortality declined by 29 deaths per 1,000 live births (from 64 deaths per 1000 livebirths to 35 deaths per 1000 live births as maternal education increased to secondary school) [6].
The association between education and infant health can be explained a number of different ways [36, 37]. An educated mother might be more able to use health care information and therefore understand the importance of child immunization, early child health seeking and appropriate caring for children practice better than illiterate mothers [36]. An educated mother can also seek appropriate health care, can be autonomous, could refuse harmful traditional practices and could make economic decisions to spend more on caring for children [15]. Educated mothers can modify the traditional child feeding and care practices, changing fertility preference such as giving more focus to the quality of children’s lives rather than quantity, and increase their involvement in family decisions [19, 38]. Education is an important social indicator, which can determine the status of a household [39]. The household’s socio-economic status, such as access to improved water, income and access to improved latrine facilities were associated with maternal education. The household’s socio-economic status can further explain the relationship between education and infant mortality [40].
The effect of maternal education on infant survival can be explained in different dimensions (economic, social demographic, environmental and biomedical) [36]. For example, maternal education can create awareness and can promote appropriate infant feeding and care [41]. Alternatively, participation in higher education enables a woman to acquire a better occupation and hence a higher income/wealth level [37].
Maternal education can also influence the attitudes of mothers towards traditional norms and beliefs including traditional infant caring practices, knowledge about illness and disease prevention practices, which have an impact on the infant and child survival [40]. An educated mother is more likely to use modern health care facilities and more aware about hygienic practices [42, 43]. Educated mothers are also give their own care during pregnancy and the care of her child through the most vulnerable stages of its life than non-educated mothers [40, 44].
Educational level can also affect infant survival by influencing the reproductive behaviour and increasing mother’s skills in health care practices related to contraception use, nutrition, hygiene, preventive care and disease treatment [45]. It may also increase chance of marrying a man in a higher occupation group and/or with a higher income, which may increase the opportunity or greater capability to provide a variety of goods, services and assets at the household level, which in turn enhances child health and survival [45]. Maternal education also increases the opportunity of a household to provide children with a sufficient amount of food, and also improves the capacity to pay health service during maternity care and childbirth [46, 47].
Limitations
This meta-analysis may have the following limitations; as this meta-analysis included few publications, the power of this pooled effect may be small. Due to the nature of meta-analysis, that used group data, other confounding factors that can affect infant mortality were not reported. In addition to this, all studies included are observational studies that the confounding factors might present in the original studies and this may affect the overall estimate. Therefore, the findings of this study are best if considered the context of both limitations of the original studies and this meta-analysis.
Conclusion
From this systematic review, we found that increased level of maternal education was significantly associated with infant mortality; when the level of maternal education was higher, the infant mortality was lower. From this study, investment in maternal education might be one of the important ways to reduce infant mortality in the long run; it is also one of the indicators of development of a country. Therefore, understanding the long-term effect of maternal education on infant mortality may contributes to the improvement of infant health in Ethiopia. In Ethiopia, only 4% of women completed secondary school or went beyond secondary school, obviously this calls the attention of policy makers to encourage women to go to school for longer period of time and for greater number of years. This can be done by changing the attitude of the communities, families and parents to keep women in school for longer number of years. In this regard, there should be an intersectoral collaboration between the Federal Ministry of Education and the Federal Ministry Health in Ethiopia. In addition, education programme and community information in Ethiopia should work in collaboration to promote awareness and understanding of the broad field of population issues with the purpose of developing responsible attitudes and behaviour toward that issue. Overall, policy makers should give more attention in promoting the role of women through removing institutional and cultural barriers, which hinder women from access to education in order to reduce infant mortality in Ethiopia.
Supporting information
(DOC)
(DOC)
(DOC)
(DOC)
(DOC)
Acknowledgments
We would like to thank to the University of Newcastle, Australia for providing a free access to the digital online library to search the electronic databases for this systematic review.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Organization, W.H. Development of indicators for monitoring progress towards health for all by the year 2000. 1981. [Google Scholar]
- 2.Organization, W.h. WHO recommendations on antenatal care for a positive pregnancy experience. 2016. [PubMed] [Google Scholar]
- 3.Unicef, Levels & Trends in Child Mortality: Report 2010: Estimates Developed by the UN Inter-Agency Group for Child Mortality Estimation. 2010: United Nations Children's Fund.
- 4.Oza S, Lawn JE, Hogan DR, Mathers C, Cousens S.Neonatal cause-of-death estimates for the early and late neonatal periods for 194 countries: 2000–2013. Bulletin of the World Health Organization, 2015. 93(1): p. 19–28. 10.2471/BLT.14.139790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.You D, Hug L, Ejdemyr S, Beise J. Levels and trends in child mortality. Estimates developed by the UN Inter-agency Group for Child Mortality Estimation (IGME). Report 2015. 2015.
- 6.CSA, I. Ethiopia demographic and health survey 2016. Addis Ababa, Ethiopia and Calverton, Maryland, USA: Central Statistical Agency and ICF International, 2017. 551. [Google Scholar]
- 7.Shamebo D, Sandström A, Muhe L, Freij L, Krantz I, Lönnberg G, et al. The Butajira project in Ethiopia: a nested case-referent study of under-five mortality and its public health determinants. Bulletin of the World Health Organization, 1993. 71(3–4): p. 389 [PMC free article] [PubMed] [Google Scholar]
- 8.Asefa M, Drewett R, Tessema F. A birth cohort study in South-West Ethiopia to identify factors associated with infant mortality that are amenable for intervention. Ethiopian Journal of Health Development, 2000. 14(2): p. 161–168. [Google Scholar]
- 9.Cochrane SH, OHara DJ, Leslie J. The effects of education on health. 1980. [Google Scholar]
- 10.Abuqamar M, Coomans D, Louckx F. The impact of parental education on infant mortality in Gaza strip, Palestine. Journal of Public Health and Epidemiology, 2011. 3(1): p. 28–33. [Google Scholar]
- 11.Mosley WH, Chen LC. An analytical framework for the study of child survival in developing countries. Population and development review, 1984. 10: p. 25–45. [PMC free article] [PubMed] [Google Scholar]
- 12.Desai S, Alva S. Maternal education and child health: Is there a strong causal relationship? Demography, 1998. 35(1): p. 71–81. [PubMed] [Google Scholar]
- 13.Mosley WH, Chen LC. Child survival: strategies for research, in Child survival: strategies for research. 1984, Cambridge University Press; Population & Development Review; supplement to volume 10. [Google Scholar]
- 14.Glewwe P. Why does mother's schooling raise child health in developing countries? Evidence from Morocco. Journal of human resources, 1999: p. 124–159. [Google Scholar]
- 15.Caldwell J.C. Education as a factor in mortality decline an examination of Nigerian data. Population studies, 1979: p. 395–413. [Google Scholar]
- 16.Jejeebhoy SJ, Sathar ZA. Sathar, Women's autonomy in India and Pakistan: the influence of religion and region. Population and development review, 2001. 27(4): p. 687–712. [Google Scholar]
- 17.Acharya DR, Bell JS, Simkhada P, Van Teijlingen ER, Regmi PR.Women's autonomy in household decision-making: a demographic study in Nepal. Reproductive health, 2010. 7(1): p. 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mehta SR, Parmar GB, Gamit CL, Mansuri BM, Patel PB, Patel SS. Does maternal education affect maternal and child health care utilization? A community based study in a urban slum area of western India. Int J Interdiscip Multidiscip Stud, 2014. 1(10): p. 80–7. [Google Scholar]
- 19.Schultz T.P. Studying the impact of household economic and community variables on child mortality. population and Development Review, 1984. 10: p. 215–235. [Google Scholar]
- 20.Shahraki M, Agheli L, Arani AA, Sadeghi H. The effect of mothers’ education and employment on children’s health. Jentashapir Journal of Health Research, 2016. 7(4). [Google Scholar]
- 21.Weldearegawi B, Melaku YA, Abera SF, Ashebir Y, Haile F, Mulugeta A., et al. Infant mortality and causes of infant deaths in rural Ethiopia: a population-based cohort of 3684 births. BMC public health, 2015. 15(1): p. 770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kusneniwar GN, Mishra AK, Balasubramanian K, Reddy PS. Determinants of infant mortality in a developing region in rural Andhra Pradesh. National journal of integrated research in medicine, 2013. 4(4): p. 20 [PMC free article] [PubMed] [Google Scholar]
- 23.Institute, J.B. Meta-analysis of statistics: assessment and review instrument (JBI mastari). Adelaide: Joanna Briggs Institute, 2006. [Google Scholar]
- 24.Institute, J.B. The Joanna Briggs Institute Critical Appraisal Tools for Use in JBI Systematic Reviews Checklist for Analytical Cross Sectional Studies. The Joanna Briggs Institute: North Adelaide, Australia, 2017. [Google Scholar]
- 25.The Joanna Briggs Institute. JBI Critical Appraisal Checklist for Cohort Studies Joanna Briggs Institute Reviewers' Manual. 2016 ed. 2016, Australia: The Joanna Briggs Institute. [Google Scholar]
- 26.The Joanna Briggs Institute. JBI Critical Appraisal Checklist for Case Control Studies Joanna Briggs Institute Reviewers' Manual. 2016 ed. 2016, Australia: The Joanna Briggs Institute. [Google Scholar]
- 27.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP., et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS medicine, 2009. 6(7): p. e1000100 10.1371/journal.pmed.1000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of internal medicine, 2009. 151(4): p. 264–269. 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- 29.Muluye S. and Wencheko E. Determinants of infant mortality in Ethiopia: A study based on the 2005 EDHS data. Ethiopian Journal of Health Development, 2012. 26(2): p. 72–77. [Google Scholar]
- 30.Dube L, Taha M, Asefa H. Determinants of infant mortality in community of Gilgel Gibe Field Research Center, Southwest Ethiopia: a matched case control study. BMC Public Health, 2013. 13: p. 401 10.1186/1471-2458-13-401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alemayehu YK, Theall K, Lemma W, Hajito KW, Tushune K. The Role of Empowerment in the Association between a Woman’s Educational Status and Infant Mortality in Ethiopia: Secondary Analysis of Demographic and Health Surveys. Ethiopian journal of health sciences, 2015. 25(4): p. 353–362. 10.4314/ejhs.v25i4.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kumar PP, File G. Infant and child mortality in Ethiopia: a statistical analysis approach. Ethiopian Journal of Education and Sciences, 2010. 5(2). [Google Scholar]
- 33.Mekonnen D. Infant and Child Mortality in Ethiopia: The role of Socioeconomic, Demographic and Biological factors in the previous five years period of 2000 and 2005. Lund, Sweden: Lund University, 2011. [Google Scholar]
- 34.Kinfu Y. Maternal education and child survival in Addis Ababa. The Ethiopian Journal of Health Development (EJHD), 2017. 6(1). [Google Scholar]
- 35.Negera A, Abelti G, Bogale T, Gebreselassie T, Pearson R. An Analysis of the Trends, Differentials and Key Proximate Determinants of Infant and Under-five Mortality in Ethiopia. Journal of Applied Sciences, 2013. 1(2): p. 23–34. [Google Scholar]
- 36.Vikram K, Vanneman R, Desai S. Maternal Education and Child Mortality: Exploring the Pathways of Influence September 2010. [Google Scholar]
- 37.Aslam M, Kingdon GG. Parental education and child health—understanding the pathways of impact in Pakistan. World Development, 2012. 40(10): p. 2014–2032. [Google Scholar]
- 38.Handa S. Maternal education and child height. Economic Development and Cultural Change, 1999. 47(2): p. 421–439. [Google Scholar]
- 39.Galobardes B, Shaw M, Lawlor DA, Lynch JW, Smith GD. Indicators of socioeconomic position (part 1). Journal of Epidemiology & Community Health, 2006. 60(1): p. 7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bicego GT, Boerma JT. Maternal education and child survival: a comparative study of survey data from 17 countries. Social science & medicine, 1993. 36(9): p. 1207–1227. [DOI] [PubMed] [Google Scholar]
- 41.Guldan GS, Zeitlin MF, Beiser AS, Super CM, Gershoff SN, Datta S. Maternal education and child feeding practices in rural Bangladesh. Social Science & Medicine, 1993. 36(7): p. 925–935. [DOI] [PubMed] [Google Scholar]
- 42.Mekonnen Y, Mekonnen A. Utilization of maternal health care services in Ethiopia. 2002.
- 43.Fatema SR, Kabir MH. Maternal Education, Hygienic Practices and Children’s Health Status. EPH-International Journal of Medical and Health Science (ISSN: 2456-6063), 2017. 3(7): p. 01–13. [Google Scholar]
- 44.Ikeako LC, Onah HE, Iloabachie GC. Influence of formal maternal education on the use of maternityservices in Enugu, Nigeria. Journal of obstetrics and gynaecology, 2006. 26(1): p. 30–34. 10.1080/01443610500364004 [DOI] [PubMed] [Google Scholar]
- 45.Cleland JG, Van Ginneken JK. Maternal education and child survival in developing countries: the search for pathways of influence. Social science & medicine, 1988. 27(12): p. 1357–1368. [DOI] [PubMed] [Google Scholar]
- 46.Raj A, Saggurti N, Winter M, Labonte A, Decker MR, Balaiah D, et al. The effect of maternal child marriage on morbidity and mortality of children under 5 in India: cross sectional study of a nationally representative sample. Bmj, 2010. 340: p. b4258 10.1136/bmj.b4258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Frost MB, Forste R, Haas DW. Maternal education and child nutritional status in Bolivia: finding the links. Social science & medicine, 2005. 60(2): p. 395–407. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOC)
(DOC)
(DOC)
(DOC)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.