Abstract
Transgender and gender non-conforming (TGNC) populations, including those who do not identify with gender binary constructs (man or woman) are increasingly recognized in health care settings. Research on the health of TGNC people is growing, and disparities are often noted. In this review, we examine 77 studies published between January 1, 1997 and March 22, 2017 which reported mental health outcomes in TGNC populations to (a) characterize what is known about mental health outcomes and (b) describe what gaps persist in this literature. In general, depressive symptoms, suicidality, interpersonal trauma exposure, substance use disorders, anxiety, and general distress have been consistently elevated among TGNC adults. We also used the minority stress model as a framework for summarizing existing literature. While no studies included all elements of the Minority Stress Model, this summary gives an overview of which studies have looked at each element. Findings suggest that TGNC people are exposed to a variety of social stressors, including stigma, discrimination, and bias events that contribute to mental health problems. Social support, community connectedness, and effective coping strategies appear beneficial. We argue that routine collection of gender identity data could advance our understanding mental health risk and resilience factors among TGNC populations.
Keywords: Transgender, non-conforming, gender, mental health, substance use, social stress
Context of the current review
There has been increasing interest and attention paid to the needs of transgender and gender nonconforming (TGNC) people in the United States (U.S.). In addition to increased awareness of transgender men (assigned female birth sex) and transgender women (assigned male birth sex), gender nonconforming people have also become increasingly visible, including those who identify as neither a man nor woman, as both man and woman, or as fluid between genders. Gender nonconforming identities came to the attention of mainstream media in a Time Magazine cover story entitled “Beyond ‘He’ or ‘She’” (Steinmetz, 2017). Media attention on the TGNC population has also included reality television programs centered on transgender women such as “I am Cait” (2016) – which put the former Olympian Caitlyn (formerly Bruce) Jenner at the center of the show, and Transparent (2016) about the effect of transitioning on family dynamics, to “I am Jazz” (2015) about a young girl and her struggles with identity as she grows through her teen years. Moreover, the ongoing discussions by the Department of Defense regarding policies about open service of transgender active duty military personnel have been of interest to the public and health professionals alike. Professional organizations have begun to recognize TGNC people, such as the American Psychological Association (2015), American Medical Association (AMA, 2017), the American Psychiatric Association, the American Academy of Family Physician, all of which have issued statements about the importance of transgender medicine. It is widely accepted that an interdisciplinary approach to the health and well-being of TGNC people is indicated (e.g., Shipherd et al., 2016), but reliable study of how to best assist TGNC people with their mental health needs has only begun. Indeed, training for providers interested in mental health needs of transgender people is noted to be lacking (Cochran & Robohm, 2015). Thus, a comprehensive review of mental health in TGNC could be beneficial to guide professionals seeking information about how to best assist TGNC clients and for researchers to be aware of what gaps still exist in this literature.
Identification of transgender gender and nonconforming persons in research studies
It can be difficult to identify transgender and gender nonconforming persons in research, because data on gender identity is not routinely collected in population health surveys (e.g., US Census), in medical record systems, or in routine demographic for research. For the purposes of this review, we elected to include both studies that recruited persons based upon their self-identified gender identity and studies that included medical record review or transgender-related diagnostic codes such as Gender Dysphoria (American Psychiatric Association, 2013). Each type of sample offers a unique set of information, with medical diagnoses likely including those TGNC people who are more interested in medical interventions in support of their gender identity such as hormones, mental health counseling, and/or surgical interventions. As such, medical chart identified samples are more likely to focus on people with binary identities such as transgender women or transgender men. In contrast, non-binary identified people (i.e., people who identify as a gender identity other than man or woman) may be more likely identified through survey research. Although both binary and non-binary identified individuals could be included in either type of sample.
Conceptualization of mental health risk and resilience
While it can be helpful to be aware of the types of mental health concerns that are elevated among TGNC people, it is also important to acknowledge the context of these conditions, including pathways of resilience to mental health concerns. As such, utilization of a conceptual model to interpret findings is essential. Meyer’s (2003) Minority Stress Model is used in this systematic review as a framework to group and discuss results. Recent research has shown that this Minority Stress Model—originally developed as conceptual framework to explain prejudice, social stress, and mental health among lesbian, gay, and bisexual populations—can be applied to understand these same relations among transgender and gender-nonconforming populations (Bockting, Miner, Swinburne Romine, Hamilton, & Coleman, 2013; Hendricks & Testa, 2012; Testa, Habarth, Peta, Balsam, & Bockting, 2015). Model adaptation to transgender and gender-nonconforming populations has been well-described by Hendricks and Testa (2012). In this adaptation, the authors apply the concepts original designed to interpret stress and discrimination sexual minority people experience to the experiences of TGNC peoples (see Method for more details on the application of this framework).
Objectives
This study aimed to synthesize the relevant literature, and to use Minority Stress Model (Meyer, 2003; Hendricks & Testa, 2012) to systematically classify mental health outcomes, and associated risk and resilience factors for transgender and gender non-conforming populations. Further, this review aims to assist researchers by providing an extensive overview of critical gaps in the literature, including key methodological issues. This review may also be useful to practitioners seeking guidance on key constructs noted among TGNC youth and adults as well as culturally competent mental health assessment and treatment.
Method
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Guidelines (Shamseer et al., 2015), a review protocol was designed and data extraction forms were developed. Therefore, the rationale and objectives, methods of systematic search, and the data analyses have been specified and documented below.
Search strategy
Systematic searches were conducted for in three databases: PsychINFO, PubMED, and Cochrane Database of Systematic Reviews. Article references, relevant reviews, book chapters, and Google Scholar were further searched for additional relevant publications. The search strategy was based on synonyms of the primary search terms: “transgender,” “transsexual,” “gender nonconforming,” “gender identity disorder,” “gender dysphoria,” “gender minority,” “mental health,” “psychosocial,” and “comorbidities.” We restricted our search criteria to publications from the last 20 years by entering the following date range: January 1, 1997 to March 22, 2017. We included studies that were in press [i.e.., with full text available online] at the time the search was conducted. An additional 11 studies were identified through hand searches of reference sections to assure maximal inclusion of studies.
Eligibility criteria
Studies included in the final analysis met the following criteria: (1) peer-reviewed and published between January 1, 1997 and March 22, 2017, (2) contained assessment of mental health or psychosocial constructs, (3) sample was comprised of TGNC individuals in the U.S., and (4) full-text available in English. We excluded studies based on the following criteria: (1) absence of measures of mental health or psychosocial constructs; (2) lack of direct measurement of mental health variables for transgender participants (e.g., lesbian, gay, or bisexual individuals only, providers only, parents only); (3) LGBT samples, when transgender results were not reported separately; (4) full text unavailable in English; (5) lack of quantitative data analysis (i.e., purely theoretical, editorial, or commentary OR exclusively qualitative studies [without any sample characteristics regarding mental health or psychosocial problems]); (6) non-peer reviewed (legal proceeding, chapters, dissertations, conference proceedings, etc.); (7) abstract only; (9) case studies; (10) studies that measured exposure to violence and discrimination, but did not report mental health or psychosocial correlates of these experiences; (11) non-U.S. sample.
Study selection
The database (and other source) searches yielded 1,523 after duplicates were removed. Study selection was carried out in iterative stages. After the full database search, authors independently screened 100 abstracts to develop, adapt, and standardize eligibility assessment plan. Second, abstracts were divided into two groups and screened independently be each author. Articles with questionable eligibility were discussed in weekly meetings, and exclusion criteria were refined as need. For each additional eligibility criteria that was added to the protocol, previously reviewed articles were re-screened with the new criteria. A total of 1401 records were excluded in the early stage of study selection. The remaining 132 articles were reviewed in full text, and authors continued to meet weekly to discuss exclusion of additional articles. At this stage, an additional 56 articles were excluded, yielding a final 77 articles. See Figure 1 for flow diagram representing study identification, screening, eligibility, and inclusion process.
Fig. 1.
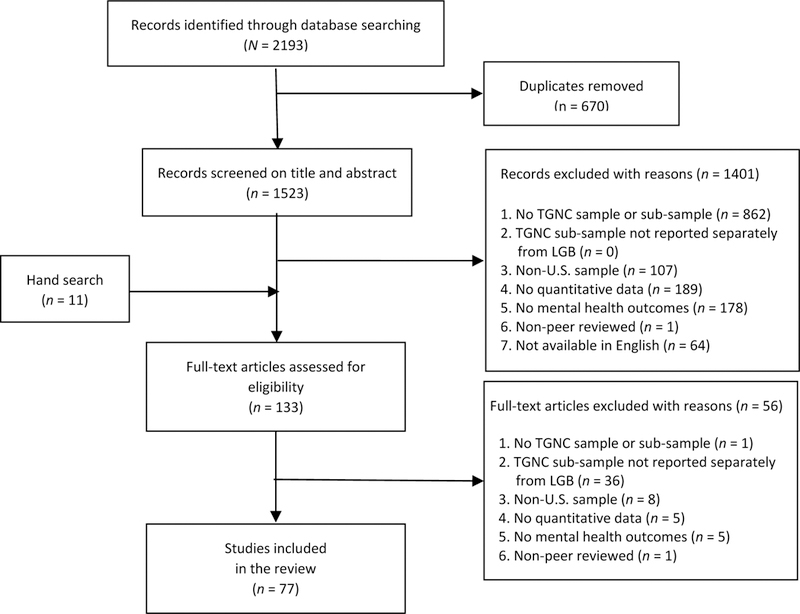
Flow Diagram
Data extraction
Each author independently extracted data from approximately half of the final 77 studies using a data extraction sheet that was developed based on PRISMA guidelines. Authors then cross-checked the extracted information for accuracy.
Data analysis
All included studies used survey or interview method to gather relevant information on mental health and psychosocial constructs. Sample selection criteria varied widely, ranging from various assessments of self-identified gender identity to ICD codes for gender dysphoria (and conceptually related ICD codes). We have provided detailed description of study samples in Table 1 to help frame the discussion, as these samples likely represent largely different populations. In Tables 2 and 3, we report most frequently assessed mental health or psychosocial problems, and most frequently reported risk or resilience factors associated with mental health outcomes in sexual and gender minority populations.
Table 1.
Characteristics of studies included in the systematic review (N=77)
| # | Study | Location | N | Sample Descriptor | [Age range] Mean Age, SD |
% racial or ethnic minorities |
Cross-Sectional v. longitudinal v. RCT |
Approach |
|---|---|---|---|---|---|---|---|---|
| Adult Sample Populations | ||||||||
| ICD Code for Gender Dysphoria | ||||||||
| (1) | Blosnich et al. (2013) | U.S.-wide | 1326 | Veterans with ICD Code for gender identity disorder (FY00-FY11) | n.r.b | n.r. | Cross-Sectional | Chart Review |
| (2) | Blosnich et al. (2014) | U.S.-wide | 5117 | Veterans with ICD Codes for gender identity disorder, transsexualism, or transvestic fetishism (FY98-FY13) | n.r.b | n.r. | Cross-Sectional | Chart Review |
| (3) | Blosnich et al. (2016) | U.S.-wide | 1640 | Veterans with ICD Codes for gender identity disorder, transsexualism, or transvestic fetishism with 1 past-year medical visit (FY13) | [n.r.] 54.8, 13.2 | 18.8 | Cross-Sectional | Chart Review |
| (4) | Brown & Jones (2014)* | U.S.-wide | 5135 | Veterans with ICD Code for gender identity disorder (FY96-FY13) | White TG: [n.r.] 56.7,13.2 Black TG: [n.r.] 51.2,13.9 | 7.5 | Cross-Sectional | Chart Review |
| (5) | Brown & Jones (2015) | U.S.-wide | 4793 | Veterans with ICD Codes for gender identity disorder, transsexualism, or transvestic fetishism (FY00-FY13) | [n.r.] 55.5, 13.5 | 19.4 | Cross-Sectional | Chart Review |
| (6) | Brown & Jones (2016)* | U.S.-wide | 5135 | Veterans with ICD Codes for gender identity disorder, transsexualism, or transvestic fetishism (FY96-FY13) | [n.r.] 55.8, 13.5 | 19.8 | Cross-Sectional | Chart Review |
| (7) | Lindsay et al. (2016) | U.S.-wide | 332 | Veterans who served in Afghanistan with ICD Codes for gender identity disorder, transsexualism, transsexualism with asexual history; transsexual with homosexual history; transsexual with heterosexual history (FY00-FY13) | [n.r.] 33.9, 8 | 27.5 | Cross-Sectional | Chart Review |
| (8) | Reisner et al. (2014) | Boston, MA | 23 | Transmen who tested positive for sexually transmitted infection | [n.r.] 32, 7.3 | 52.2 | Cross-Sectional | Chart Review |
| Presenting for Services | ||||||||
| (9) | Keo-Meier et al. (2015) | Houston, TX | 43 | Transmen presenting for hormone treatment | [n.r.] 26.6, 8.4 | 26 | Prospective | Survey pre-post treatment |
| (10) | Leinung et al. (2013) | Albany, NY | 242(n = 192 TW, 50 TM) | Transgender clients who received hormone treatments | [n.r.] 36.3, 12.3 TW: [n.r.] 38, 12.5 TM: [n.r.] 29.9, 9.9 | n.r. | Cross-Sectional | Chart Review |
| (11) | Nemoto et al. (2005) | San Francisco, CA | 109 | Transwomen who participated in a workshop series (health, mental health, substance use, connection to services) hosted by community organization | n.r.b | n.r. | Prospective | Survey pre-post treatment |
| Presenting for Services; Self-Identified | ||||||||
| (12) | Cole et al. (1997) | n.r. | 435 | Transgender clients who presented for gender-related services | TW: [n.r.] 32, 9TM: [n.r.] 30, 8 | n.r. | Cross-Sectional | Chart review |
| Self-Identified | ||||||||
| (13) | Ainsworth & Spiegel (2010) | U.S.-wide | 247 | Transwomen who received facial feminization or genital surgeries | [n.r.] 49, n.r. | n.r. | Cross-Sectional | Web-Based Survey |
| (14) | Barr et al. (2016) | U.S.-wide | 571 | Transgender or gender non-conforming | [18–86] 31.0, 13 | 20 | Cross-Sectional | Web-Based Survey |
| (15) | Bazargan & Galvan (2012) | Los Angeles, CA | 220 | Latina Transwomen | [18+] n.r.a | 100 | Cross-Sectional | Semi-Structured Face-to-Face Interview |
| (16) | Benotsch et al. (2013) | Mid-Atlantic Richmond, VA & Washington DC areas | 155 | Transgender individuals recruited at transgender health clinics or community venues | [n.r.] 31.9, 11.6 | 62.3 | Cross-Sectional | Survey |
| (17) | Bradford et al. (2013)* | VA, 44% cities and towns represented | 350 | Transgender or gender-non conforming [Virginia Transgender Health Initiative Study] | [n.r.] 37.2, 12.7 | 38 | Cross-Sectional | Web-Based Survey; Mail-In Survey |
| (18) | Budge et al. (2013) | U.S.-wide | 351 | Transwomen or Transmen, excluding non-binary and cross-dressing | [18–78] 40, 13 | 14 | Cross-Sectional | Web-Based Survey |
| (19) | Clements-Nolle et al. (2001)* | San Francisco, CA | 515(n = 392 TW, 123 TM) | Transgender or gender-nonconforming | TW: [18–67], 34, n.r. TM: [19–61], 36, n.r. | TW: 73 TM: 33 | Cross-Sectional | Semi-Structured Face-to-Face Interview |
| (20) | Clements-Nolle et al. (2006)* | San Francisco, CA | 515(n = 392 TW, 123 TM) | Transgender or gender-nonconforming | TW: [18–67] 34, n.r. TM: [19–61] 37, n.r. | TW: 73 TM: 34 | Cross-Sectional | Semi-Structured Face-to-Face Interview |
| (21) | Colton-Meier et al. (2011) | U.S.-wide | 369 | Transmen who self-identified as “female-to-male transsexuals” | [18–68] 28, n.r. | 23 | Cross-Sectional | Web-Based Survey |
| (22) | Dowshen et al. (2016) | 15 U.S. cities | 66 | Transgender youth living with HIV | [18–24] 21.1, 2.2 | n.r. | Cross-Sectional | Computer-Based Survey (CASI) |
| (23) | DuBois (2012) | Western MA; Boston, MA; Southern VT | 65 | Transmen using testosterone | [n.r.] 31.8, 9.1 | 26 | Cross-Sectional | Semi-Structured (Clinical) Interview |
| (24) | Flentje et al. (2014) | San Francisco, CA | 199(n = 146 TW, 53 TM) | Transgender clients accessing substance abuse treatment | [n.r.] 38.3, 13.5 | TW: 62.3 TM: 45.3 | Cross-Sectional | Chart Review |
| (25) | Flentje et al. (2016) | San Francisco, CA | 49 | Transgender individuals who were homeless | n.r.b | TW: 76 TM: 44 | Cross-Sectional | Survey |
| (26) | Fredriksen-Goldsen et al. (2013)* | U.S.-wide | 174 | Transgender sub-sample from survey of LGBT older adults (50+) [Aging with Pride Project] | [n.r.] 61, 9 | 21 | Cross-Sectional | Web-Based Survey; Mail-In Survey |
| (27) | Gameral et al. (2014) | San Francisco, CA | 191 | Couples; Transwomen with cisgender male partners | [n.r.] 36, 11 | 79 | Cross-Sectional | Computer-Based Survey (CASI) |
| (28) | Glynn et al. (2016) | San Francisco, CA | 573 | Transwomen with histories of sex work | [n.r.] 35.1, 9.4 | 79 | Cross-Sectional | Survey |
| (29) | Goldblum et al. (2012)* | VA (statewide) | 290 | Transgender or gender-nonconforming [Virginia Transgender Health Initiative Study] | [18–65] 37, 13 | 34 | Cross-Sectional | Web-Based Survey; Mail-In Survey |
| (30) | Horvath et al. (2014) | U.S.-wide, split rural non-rural | 1229 | Transgender people living in rural and non-rural communities | TW: [n.r.] 38, n.r.TM: [n.r.] 26.2, n.r. | 18.5 | Cross-Sectional | Web-Based Survey |
| (31) | Hoy-Ellis et al. (2017)* | U.S.-wide | 183 | Transgender sub-sample from survey of LGBT older adults (50+) [Aging with Pride Project] | [n.r.] 60.1, n.r. | 32 | Cross-Sectional | Web-Based Survey |
| (32) | Jefferson et al. (2013) | San Francisco, CA | 98 | Transwomen of color | [n.r.] 45, 9.8 | 100 | Cross-Sectional | Semi-Structured Face-to-Face Interview |
| (33) | Kattari et al. (2016) | CO (statewide) | 417 | Transgender or gender-nonconforming[Colorado Transgender Health Survey-2014] | [n.r.] 38, n.r. | 16 | Cross-Sectional | Web-Based Survey; Mail-In Survey |
| (34) | Katz-Wise et al. (2017)* | MA | 452 | Transgender or gender-nonconforming [Project VOICE] | [n.r.] 33, 13 | 21 | Cross-Sectional | Web-Based Survey; Mail-In Survey |
| (35) | Keuroughlian et al. (2015)* | MA | 452 | Transgender or gender-nonconforming [Project VOICE] | [n.r.] 33.6, 12.8 | 20.6 | Cross-Sectional | Web-Based Survey |
| (36) | Lehavot et al. (2016) | U.S.-wide | 212(n = 186 TW, 26 TM) | Veterans who self-identified as transgender | [n.r.] 49.9, 14.9 | 10.4 | Cross-Sectional | Web-Based Survey |
| (37) | Maguen et al. (2010) | Boston, MA | 153(n = 125 TW, 28 TM) | Transgender or gender non-conforming conference attendees [2004] | [18–75] 47, 11 | 3(4 TW, 0 TM) | Cross-Sectional | Self-Report Survey |
| (38) | Mathy (2003) | U.S.-wide | 73 | Transgender sub-sample from online survey | [19–58] 37, 10 | n.r. | Cross-Sectional | Web-Based Survey |
| (39) | McDuffie & Brown(2010) | Clinic in TN | 70 | Veterans seeking treatment for gender-related concerns (FY87-FY07) | [20–70] n.r.a | 14 | Cross-Sectional | Chart Review |
| (40) | Meyer et al.(2017) | 19 U.S. states; Guam | 691 | Transgender sub-sample from a population based surveillance survey | n.r.b | n.r. | Cross-Sectional | Semi-Structured Phone Interview |
| (41) | Nemoto et al. (2015) | San Francisco & Oakland, CA | 235 | African-American Transwomen with history of sex work | [n.r.] 35.1, n.r. | 100 | Cross-Sectional | Semi-Structured Face-to-Face Interview |
| (42) | Newfield et al. (2006) | San Francisco Bay area, CA | 376 | Transmen living in the U.S. | [n.r.] 32.6, 10.8 | 11 | Cross-Sectional | Web-Based Survey |
| (43) | Nuttbrock et al. (2010) | New York, NY | 571 | Transwomen (baseline) | [19–59] 37, n.r. | 73 | Cross-Sectional | Semi-Structured Face-to-Face Interview |
| (44) | Nuttbrock et al. (2014) | New York, NY | 230 | Transwomen (baseline & follow-up) | [19–59] 34, n.r. | 65 | Prospective | Semi-Structured Face-to-Face Interview |
| (45) | Operario et al. (2011) | San Francisco Bay area, CA | 174 | Transwomen with cisgender male sexual partners | [18+] 37.8, 10.7 | 88 | Cross-Sectional | Computer-Based Survey (CASI) |
| (46) | Pflum et al. (2015) | U.S.; Canada | 865(n = 145 M, 106 W, 259 TM, 163 TW, 34 GQ-MaB, 158 GQ-FaB) | Transgender or gender-nonconforming | M: [n.r.] 31.9,11 W: [n.r.] 39.2, 16.2 TM: [n.r.] 30.9, 11.3 TW: [n.r.] 37.2, 14.9 GQ-MaB: [n.r.] 34.6, 13.9 GQ-FaB: [n.r.] 24.5, 7.1 | M: 13.8 W: 11.3 TM: 11.6 TW: 9.2 GQ-MaB: 5.9 GQ-FaB: 13.9 | Cross-Sectional | Web-Based Survey |
| (47) | Reisner et al. (2016a) | Boston, MA | Two Samples: 12, 17 | Transmen with cisgender male sexual partners | [18–29] 24.3, 2.8 | 3.5 | Prospective | Semi-Structured Face-to-Face Interview (pre-post) |
| (48) | Reisner et al. (2016b)* | MA | 452(n = 285 FTM, 167 MTF) | Transgender or gender-nonconforming [Project VOICE] | [n.r.] 33, 13 | 21 | Cross-Sectional | Web-Based Survey |
| (49) | Salzar et al. (2017) | Atlanta, GA | 92 | Transwomen with cisgender male sexual partners | [n.r.] 34, n.r. | 89 | Cross-Sectional | Semi-Structured Face-to-Face Interview |
| (50) | Sanchez & Vilain(2009) | AZ, CA | 53 | Transwomen who attended a transgender conference | [21–77] 51, 11.6 | 14 | Cross-Sectional | Survey |
| (51) | Shipherd et al. (2010) | Boston, MA | 130 | Transgender or gender non-conforming conference attendees [2008] | [22–79] 49.2, 11 | 8 | Cross-Sectional | Survey |
| (52) | Shipherd et al. (2011) | Boston, MA | 97 (n=43 MTD, 54 LTD) | Transwomen conference attendees [2005] | [20–72] 47.5, 10.8 | 6–3.1 | Cross-Sectional | Survey |
| (53) | Shipherd et al. (2012) | Boston, MA | 141(n=43 veterans) | Transwomen conference attendees [2008] | [26–79] 51.6, 10.9 | 3.6 | Cross-Sectional | Survey |
| (54) | Stanton et al. (2017) | U.S.-wide | 376(n = 105 TW, 78 TM, 131 TO) | Transgender sub-sample from online survey [U.S. Social Justice Sexuality Survey] | [18–50+] n.r.a | 77 | Cross-Sectional | Web-Based Survey |
| (55) | Warren et al. (2016) | U.S.-wide | 208(n = 82 TW, 126 TM) | Transgender sub-sample from online survey of LGBT adults | TW: [18–65] 35, n.r.TM: [18–65] 27, n.r. | TW: 24 TM: 22 | Cross-Sectional | Web-Based Survey |
| (56) | White Hughto et al. (2017)* | MA | 412 | Transgender or gender-nonconforming [Project VOICE] | [18–75] 33, 13 | 21 | Cross-Sectional | Web-Based Survey |
| (57) | Wilson et al. (2014) | San Francisco, CA | 314 | Transwomen | n.r.b | n.r. | Cross-Sectional | Web-Based Survey |
| (58) | Bockting et al. (2013) | U.S.-wide, 57% rural | 1093 | Transgender and gender-nonconforming, including cross-dressing | [n.r.] 33, 12 | 21 | Cross-Sectional | Web-Based Survey |
| (59) | Yang et al. (2015) | San Francisco Bay area, CA | 191 | Transwomen with cisgender male sexual partners | [18 −50+] 38, 12 | 84 | Cross-Sectional | Computer-Based Survey (CASI) |
| Child/Adolescent/Young Adult Sample Populations | ||||||||
| ICD Code for Gender Dysphoria | ||||||||
| (60) | Peterson et al. (2016) | Cincinnati, OH | 96(n = 54 TM, 31 TW, 15 TO) | Transgender adolescents with gender dysphoria who presented to a transgender health clinic | [12–22] 17.1, 2.3 | n.r. | Cross-Sectional | Computer-Based Survey (CASI); Chart Review |
| (61) | Spack et al. (2012) | Boston, MA area | 97 | Youth with diagnosis of gender identity disorder (1998–2010) referred to a pediatric clinic, with parental support and letter from mental health provider | [4–20] 12.8, 3.4 | n.r. | Cross-Sectional | Semi-Structured (Clinical) Interview |
| (62) | Reisner et al. (2015a)* | Boston, MA area | 180(n = 105 FTM, 72 MTF) | Transgender youth receiving services at community health center | [12–29] 19.6, 3 | 53 | Cross-Sectional | Chart Review |
| (63) | Reisner et al. (2015b)* | Boston, MA area | 180(n = 105 FTM, 72 MTF) | Transgender youth receiving services at community health center | [12–29] 19.6, 3 | 53 | Cross-Sectional | Chart Review |
| Presenting for Services | ||||||||
| (64) | Chen et al. (2016) | Indianapolis, IN | 38 | Pediatric patients that received referral related to gender dysphoria | [n.r.] 14.4, 3.2 | 21.1 | Cross-Sectional | Chart Review |
| (65) | Simons et al. (2013) | Los Angeles, CA | 66 | Transgender youth presenting for care at a gender clinic | [12–24] 19, 3 | 48 | Cross-Sectional | Survey; Computer-Based Survey (CASI) |
| Self-Identified | ||||||||
| (66) | Brennan et al. (2012) | Chicago, IL; Los Angeles, CA | 151 | Transwomen living with HIV | [15–24] 21, 2.5 | 95 | Cross-Sectional | Semi-Structured Face-to-Face Interview |
| (67) | Durwood et al. (2017) | 23 U.S. states; 1 Canadian province | Two samples: 63, 116 | Children who identified as a gender differing from their natal sex in everyday life by using pronouns associated with their asserted gender | [9–14] 10.8, 1.3 | 41 | Cross-Sectional | Semi-Structured Face-to-Face Interview |
| (68) | Garofalo et al. (2006) | Chicago,` IL | 51 | Racial and ethnic minority transwomen | [16–25] 22, n.r. | 100 | Cross-Sectional | Survey |
| (69) | Le et al. (2016) | San Francisco, CA | 301 | Transwomen | [16–24] n.r.a | 63 | Cross-Sectional | Survey |
| (70) | Olson et al. (2015) | Los Angeles, CA | 96 | Transgender or gender-nonconforming, gender dysphoria, desire to receive cross-sex hormones, and naivety to hormone treatment | [12–24] 19.2, 2.9 | 48 | Cross-Sectional | Survey; Chart Review; Computer-Based Survey (CASI) |
| (71) | Olson et al. (2015) | 23 U.S. states; 1 Canadian province | 73 | Matched Controls; Children who identified as a gender differing from their natal sex in everyday life by using pronouns associated with their asserted gender | [3–12] 7.7, 2.2 | 30 | Cross-Sectional | Survey; Semi-Structured Face-to-Face Interview |
| (72) | Reisner, Biello et al. (2016) | Chicago, IL; Boston, MA | 298 | Sexually active transwomen with cisgender male sexual partners [Project LifeSkills] | [16–29] 23, 3.5 | 74 | Cross-Sectional | Semi-Structured Face-to-Face Interview |
| (73) | Reisner, Katz-Wise et al. (2016) | US-wide | 26 | Transgender sub-sample from online survey [Growing up Today Study 1] | [23–28] 25, n.r. | 25 | Cross-Sectional | Survey |
| (74) | Rowe et al. (2015)* | San Francisco, CA area | 292 | Transwomen, HIV-negative [The SHINE Study] | [16–24] 21, 2 | 63 | Cross-Sectional | Web-Based Survey |
| (75) | Russell et al. (2011) | San Francisco, CA area | 21 | Transgender sub-sample of LGBT youth survey [The Family Acceptance Project] | [21–25] 22.8, 1.4 | 53 | Cross-Sectional | Survey; Computer-Based Survey (CASI) |
| (76) | Sterzing et al. (2017) | US-wide | 310 | Transgender and genderqueer sub-sample of online survey for LGBT youth | [14–19] 16.4, 0.03 | 38 | Cross-Sectional | Survey; Web-Based Survey |
| (77) | Wilson et al. (2016)* | San Francisco, CA area | 216 | Transwomen, HIV-negative [The SHINE Study] | [16–24] n.r.a | 66 | Cross-Sectional | Survey |
= both mean age and SD not reported
= age range, mean age, and SD not reported
Studies 4 and 6 were from the same sample; Studies 17 and 29 were from same sample, the Virginia Transgender Health Initiative Study; Studies 19 and 20 were from same sample; Studies 26 and 31 were from same sample, the Aging with Pride Project; Studies 74 and 77 were from the same sample, The SHINE Study; Studies 34, 35, 56, and 48 were from the same sample, Project VOICE; Studies 62 and 63 were from the same sample.
NOTE: Italicized heading indicate how the TGNC sample was defined.
PTSD = post-traumatic stress disorder; TG = transgender; TW = transwomen; TM = transmen; TO = other transgender (non-binary/gender-fluid); FTM = female to male; MTF = male to female; GQ = genderqueer; W = women; M = men; MaB = male at birth; FaB = female at birth; MTD = more time dressed as women; LTD = less time dressed as women; AZ = Arizona; CA = California; CO = Colorado; GA = Georgia; IL = Illinois; IN = Indianapolis; MA = Massachusetts; NY = New York; OH = Ohio; TN = Tennessee; TX = Texas; VA = Virginia; VT = Vermont
Table 2.
Key mental health variables assessed (N=77)
| # | Key Mental Health Variables | na | Study ID Numbers |
|---|---|---|---|
| [1] | Depressive Symptoms | 50 | 3, 4, 5, 6, 7, 8, 9, 10, 11, 15, 16, 18, 19, 20, 21, 22, 26, 27, 28, 30, 32, 33, 34, 35, 39, 41, 43, 44, 45, 46, 47, 48, 49, 52, 56, 57, 58, 59, 61, 62, 63, 64, 65, 68, 70, 71, 73, 75, 76, 77 |
| [2] | Suicidality [ideation, attempts, or self-harm] | 33 | 1, 2, 3, 4, 5, 6, 8, 12, 15, 19, 20, 21, 22, 28, 29, 30, 33, 34, 36, 37, 38, 39, 43, 44, 47, 49, 57, 60, 61, 62, 64, 71, 75 |
| [3] | Alcohol or Substance Use | 31 | 3, 4, 5, 6, 7, 8, 10, 12, 17, 20, 21, 22, 24, 25, 26, 30, 35, 36, 37, 38, 39, 40, 45, 47, 48, 57, 59, 63, 66, 68, 72, 74, 75 |
| [4] | Psychological Distress [general] | 26 | 4, 5, 6, 7, 8, 9, 10, 12, 16, 21, 25, 31, 34, 35, 40, 47, 50, 55, 57, 58, 60, 68, 69, 72, 74, 77 |
| [5] | Anxiety | 20 | 4, 8, 16, 18, 21, 30, 33, 39, 46, 47, 50, 57, 58, 59, 61, 62, 63, 70, 71, 73 |
| [6] | Quality of Life [physical and mental health status] | 16 | 4, 13, 14, 21, 24, 25, 26, 40, 42, 49, 54, 51, 52, 65, 68, 75 |
| [7] | Posttraumatic Stress Symptoms | 15 | 3, 4, 5, 6, 7, 25, 35, 36, 39, 48,7, 48, 50, 57, 58, 59, 61, 62, 63, 70, 71, 73 |
| [8] | HIV Sexual Risk/IV Drug Risk/Transactional Sex | 14 | 15, 66, 22, 68, 35, 69, 45, 72, 63, 8, 75, 49, 57, 59 |
| [9] | Mental Health or Substance Use Service Utilization | 13 | 4, 12, 19, 20, 24, 35, 37, 38, 39, 51, 60, 62, 64 |
| [10] | Disability Status [physical and mental disability] | 6 | 4, 5, 6, 10, 26, 40 |
| [11] | Child/Developmental [autism/ADHD] | 2 | 61, 64 |
| [12] | Child/Internalizing and Externalizing | 2 | 67, 71 |
Number of studies reporting key mental health variable.
NOTE: Study ID Numbers correspond with articles detailed in Table 1.
Table 3.
Key minority stress variables assessed (N=77)
| # | Key Minority Stress Variables | na | Study ID Numbers |
|---|---|---|---|
| Minority Stress (Distal or External) | |||
| [1] | Discrimination [Transgender Identity] | 30 | 5, 6, 15, 16, 17, 20, 25, 26, 27, 29, 32, 33, 35, 36, 37, 41, 42, 45, 48, 49, 56, 58, 59, 60, 66, 72, 74, 75, 76, 77 |
| [2] | Violence | 17 | 4, 5, 7, 15, 17, 20, 25, 29, 37, 43, , 44, 48, 49, 52, 56, 66, 75 |
| [3] | Discrimination [Race, Ethnicity] | 4 | 4, 32, 48, 49 |
| Minority Stress Processes [Interactive Proximal] | |||
| [4] | Expectations of Rejection | 8 | 11, 26, 27, 31, 36, 50, 53, 75 |
| [5] | Identity Concealment | 4 | 23, 26, 36, 58 |
| Minority Stress Processes [Internalized Proximal] | |||
| [6] | Internalized stigma [transphobia] | 12 | 11, 14, 15, 16, 30, 31, 32, 61, 66, 67, 68, 75 |
| Characteristics of Minority Identity | |||
| [7] | Prominence, Valence, Integration | 6 | 14, 29, 32, 47, 58, 61 |
| Other Minority Stress Variables (resilience) | |||
| [8] | Social Support [individual, family] | 20 | 17, 18, 21, 24, 26, 28, 36, 41, 46, 49, 54, 56, 58, 65, 68, 69, 74, 75, 76, 77 |
| [9] | Social Support [TGNC community, belongingness] | 8 | 11, 14, 17, 41, 46, 50, 58, 72 |
| [10] | Coping Strategies | 5 | 18, 23, 26, 32, 56 |
| [11] | Social Support [LGBT community, belongingness] | 4 | 26, 36, 41, 54 |
Number of studies reporting key minority stress variable.
NOTE: Study ID Numbers correspond with articles detailed in Table 1
Minority Stress Model as theoretical framework
The Minority Stress Model asserts that mental health distress is often the result of a hostile or stressful social environment, thus, observed disparities in mental health in this population are socially produced (Meyer, 2003). The model describes three processes by which sexual and gender minorities are subjected to minority stress. These include (1) distal or external stressors that are environmental, including other external stressors such as exposure to discrimination and violence; these are observable and verifiable, (2) interactive proximal stressors include anticipation or expectations that external stressors will occur, and vigilance that a person must maintain to protect oneself from these external stressors; and (3) internalized proximal stressor that reflect a person’s internalization of negative attitudes and prejudice from society. Conversely, interactive and internalized proximal resilience is also possible, with internalization of positive self-image, use of adaptive coping strategies, help seeking and community attachments. Interactive and internalized proximal stressors and resiliencies are not usually directly observable, but are frequently described by sexual and gender minority individuals as distressing. The cumulative burden of distal and proximal stressors can serve to overwhelm one’s ability to cope, thus leading to poor mental health outcomes in the absence of resilience factors.
Initial adaptations of the Minority Stress Model for transgender and gender-nonconforming populations name specific distal and proximal minority stress processes, and emphasize the central importance of a social and community support network (information & formal) that affirms one’s gender identity (Hendricks & Testa, 2012). Relevant distal stressors include experiences of discrimination and violence, and relevant interactive and internalized proximal stressors include expectations of rejection, identity concealment, and internalized transphobia. The model also describes factors associated with resilience including characteristics of minority identity, such the prominence, valence, and integration of one’s minority identity. In the same way that negative-valance within-group identity may inhibit one’s ability to access adequate social and community supports, positive-valence within-group identity allows individuals to access the buffering effect of affirming supports and to learn effective coping strategies. Thus, resilience is understood as both intrapersonal and interpersonal processes. As this review aims to provide the reader with an appropriate context for understanding common mental health problems in this population, we have made the Minority Stress Model central to our organization of results, and we discuss gaps in the current literature in capturing both risk and resilience in this vulnerable population. In this way, we hope to offer the first examination of the minority stress model as it applies to TGNC people based on findings from the extant literature.
Results
Detailed information regarding study design and sample characteristics of all 77 studies included in this review can be found in in Table 1. In Table 1, studies were sorted at three levels: 1) age range (adult vs. child/adolescent studies); 2) sample selection process (e.g., medical chart identification/transgender-related diagnoses, self-identification on survey or interview); and then, 3) alphabetically by last name of first author. Study identification (ID) numbers generated in Table 1 were then used in Table 2 and Table 3 to provide the reader with a list of studies that assessed a specific outcome variable of interest. Table 2 includes a list of studies that assessed mental health, substance use, and quality of life variables. Table 3 includes a list of studies that assessed aspects of the Minority Stress Model.
Study design characteristics
Overall, 77 papers were included in the systematic review. In total, 73 (94.81%) studies used cross-sectional, whereas only 4 (5.19%) used prospective study designs. Most studies (n = 68, 88.31%) relied on self-report data collection procedures, including the use of in-person surveys (n = 20, 29.41%), semi-structured face-to-face interviews (n = 15, 22.05%), computer-assisted self-interviews (n = 8, 11.76%), and structured telephone interviews (n = 1, 1.47%). Web-based surveys were used in 24 (31.17%) studies. Only three of four prospective studies reported on pre- and post-intervention survey data on mental health variables. Medical chart reviews were used in 17 (22.08%) of the included studies.
Sample characteristics.
Sample sizes ranged from 12 to 5,135 TGNC participants, with a median sample size of 212. Most studies (n = 62, 80.52%) used self-identified gender identity to select their sample. Twelve studies used transgender-related ICD codes or diagnosis in medical chart to identify their study sample. Seven studies recruited from clinical settings where clients were accessing gender-related services. Samples varied widely across studies, and included transmen only, transwomen only, any TGNC identity, veterans with transgender-related diagnoses, transwomen at risk for HIV, treatment-seeking TGNC clients, racial and ethnic minority transwomen.
Location of studies.
Inclusion in the current review required a study to be peer-reviewed and published after January 1, 1997. All studies included in the review examined a sample population in the United States, with urban and rural designations defined according to the U.S. Census Bureau (2010). Most (n = 43, 55.84%) studies focused on samples in urban locations. National samples were examined in 22 (28.57%) of the studies. Six (7.79%) studies used state-wide samples, examining populations across the states of Massachusetts (n = 3, 3.90%), Virginia (n = 2, 2.60%), and Colorado (n = 1, 1.30%). No studies explicitly focused on recruiting rural samples.
Age, race, and gender.
Across samples, mean age ranged from 7.7 to 61 years. The majority (n = 59, 76.62%) of studies examined samples of adults at least 18 years of age. Eighteen (23.38%) studies examined “child/adolescent samples” (inclusive of “young adult”); of which three (16.67%) examined children under 12 years of age; eleven (61.11%) examined individuals between the ages of 12 and 25, and four (22.22%) examined individuals up to the age of 29. Young adult samples were sorted in this category based on the author’s description of developmental similarities with adolescent (rather than adult) samples.
Racial and ethnic minority participants comprised anywhere from 3 to 100% of the study sample, yet 12 studies did not reported data on race or ethnicity. In 39 (50.65%) of the included studies, racial and ethnic minority participants represented less than 50% of the sample, most of which (n = 24, 61.54%) examined samples where racial and ethnic minority participants comprised less than 25%. In 23 studies (29.87%) racial and ethnic minority participants represented at least 50% of the sample. Four studies examined samples solely comprised of racial and ethnic minority participants.
Transgender identity was assessed through self-identification (n = 62, 80.52%), ICD code for Gender Dysphoria (n = 12, 15.58%), or presenting for services (n = 6, 7.79%). Five of the included studies further differentiated between participants identified as transwomen and transmen within their respective samples, allowing for assessment of racial and ethnic characteristics of participants within gender identity subsamples. In these studies, racial and ethnic minority representation was greater within subsamples of transwomen compared to subsamples of transmen.
Mental health, alcohol or substance use, and behavioral health risk outcomes
See Table 2. Studies reported on a variety of mental health-related variables.
Mental health.
Over half of the studies (n = 50, 64.49%) reported on depressive symptoms, 33 studies assessed suicidality (42.86%), 26 studies assessed for general psychological distress (33.77%), 20 assessed for anxiety (25.97%), and 15 assessed for posttraumatic stress symptoms (19.48%). Additionally, studies on child or adolescent mental health examined autism spectrum disorders and ADHD (n = 2, 2.60%), and internalizing and externalizing symptoms more broadly (n = 2, 2.60%).
Alcohol or substance use.
Alcohol or substance use variables were assessed in 31 (40.2%) studies. Definitions of problematic use and assessments varied widely.
Alcohol use definitions included alcohol intoxication or binge drinking within the past one to six months. One study defined regular heavy alcohol use based on the number of daily or weekly drinks. Studies addressed problematic drinking using a range of timeframes, from number of drinks within 1 month to substance use behavior throughout lifetime. Studies assessed self-reported substance use (yes/no), diagnosis of substance use disorder, self-report of problematic use, or self-reported history of drug or alcohol treatment. In some cases, authors asked about drug or alcohol use within the same item, thus making it difficult to delineate specific substances of reference.
Self-reported substance use.
Overall, 18 studies reported on self-reported use of “drugs” or “illicit substances” (n = 6), marijuana (n = 10), cocaine or crack (n = 8), heroin (n = 7), IDU (unspecified; n = 5), tobacco (n = 6), methamphetamine (n = 5), or other drugs (i.e., GHB, ketamine, amyl nitrate, LSD; n = 7). Six studies created a composite variable of polysubstance use (based on use of same substances listed above), however studies varied on the number as well as type of substances that were included while creating this variable. Polysubstance use was defined as use of 3+ substances (inclusive of alcohol; n = 3), use of 2+ substances (exclusive of nicotine; n =1), use of 2+ substances (exclusive of nicotine and alcohol; n =1), or use of 2+ “light drug” / use of 2+ “heavy drug” (n = 1).
Substance use disorder or diagnosis.
In total, eight studies reported substance use disorder or diagnosis, that was assessed through clinical interview, self-report (yes/no), or through diagnosis in the medical record. Of these studies, four reported on “any substance use disorder” (inclusive of alcohol), 1 reported on “any substance use disorder” (exclusive of alcohol), one study reported on dependence diagnosis in the medical record for cannabis, cocaine, opioid, and “other drug.” Four studies reported on diagnosis of nicotine dependence.
Self-reported problematic substance use.
Seven studies reported on problematic use, based on assessment through survey total scores or self-reported history (yes/no). Three studies reported on self-reported “history of substance use problem” but did not define substances; likewise, two studies reported on self-reported “history of alcohol or substance use problems.” One study reported on problematic use that required drug or alcohol treatment.
Service utilization.
Thirteen studies (16.88%) assessed mental health or substance use service utilization; most (n = 12, 92.31%) of which assessed for self-reported history of psychiatric treatment or counseling, one involved retrospective chart review.
Behavioral health risks.
Behavioral health risks were inclusive of HIV sexual risk, risk for intravenous (IV) drug use, and past or current transactional sex. In 14 (18.18%) of the studies included in this review, at least one behavioral health risk indicator was assessed. Of these, 12 (85.71%) assessed HIV sexual risk, 6 (42.86%) measured IV drug use risk, and 3 (21.43%) measured history of transactional sex. However, it should be noted that studies where behavioral health risks and/or physical health outcomes (e.g., HIV status) were the sole focus of the study, papers were excluded. Thus, the studies summarized also included other mental health variables.
Other indicators of well-being.
Indicators of general well-being belonged to two different categories: quality of life measures and disability status. The quality of life indicator encompassed measures of mental and physical health as well as life satisfaction and psychological well-being. Of the included studies, 16 (21.78%) investigated at least one quality of life measure. Six studies (7.79%) assessed disability status, of which, three studies measured as a single dichotomous item.
Risk and resilience factors
Studies assessed a range of risk and resilience factors consistent with Minority Stress Model, for detail see Table 3. For these analyses, minority stress variables were differentiated into distal minority stressors (discrimination due to transgender identity or race/ethnicity, exposure to violence), interactive and internal proximal minority stress processes (expectations of rejection, identity concealment, internalized stigma), characteristics of minority resilience including positive self-identity, coping, and social support.
Distal Minority Stressors: Discrimination and violence.
Across studies, discrimination was assessed using a variety of self-report measures. In total, 30 (38.96%) studies focused specifically on discrimination due to transgender identity. Of these, 13 (43.33%) studies investigated institutional discrimination in housing, healthcare, or employment due to gender identity. Discrimination due to race or ethnicity was only investigated in four (5.19%) studies, despite the fact that racial and ethnic minorities represented at least 50% of the sample population in 23 (29.87%) of the included studies. Seventeen (22.08%) studies assessed some form of interpersonal violence; of which nine (11.69%) focused on sexual violence, seven (9.09%) include verbal/psychological violence, and one assessed in-school gender-based violence.
Proximal minority stressors: Expectations of rejection, identity concealment, and internalized stigma (transphobia). Interactive and internalized proximal minority stress processes, defined as expectations of rejection, identity concealment, internalized stigma, were assessed in 24 studies (31.17%). Of these, twelve (50.00%) focused on internalized stigma, eight (33.33%) focused on expectations of rejection, and four (16.67%) focused on identity concealment. This category also included measures of self-worth (n=1, 1.30%) and self-esteem (n=9, 11.69%).
Interactive proximal resilience: Coping abilities.
Coping abilities, processes for dealing with internal or external life demands perceived to be threatening or overwhelming (Gerrig & Zimbardo, 2002), were investigated in 5 (6.49%) of the included studies. Four (80.00%) of these studies defined coping abilities through assessment of life situations as being stressful and perceived ability to effectively handle life challenges; one study (20.00%) further defined coping abilities in relation to specific stressful events and the methods used to manage these stressful events. Coping abilities were measured using standardized tools such as the Coping Self Efficacy scale (CSE; Chesney et al., 2006), Cohen’s Perceived Stress scale (PSS; Cohen et al., 1983), and the revised Ways of Coping scale (WC-R; Folkman & Lazarus, 1985). Two studies adapted the Ways of Coping scale; one used just the subscale scores for facilitative coping and avoidant coping, the other administered only the escape-avoidance subscale.
Interactive proximal resilience: Social support from peers and family.
Social support from peers and family was investigated in a total of 20 (25.97%) of the included studies. A variety of measures, both widely used and purposefully adapted to address support about gender identity, were used across the included studies to assess individual and family social support. In studies of children and adolescents, parental support was assessed using the Multidimensional Scale of Perceived Support (MSPSS) (Zimget et al., 1990), Parental Closeness (Wilson et al., 2016), Parental Acceptance and Level of Parental Acceptance scales (Ryan et al., 2010).
Interactive proximal resilience: Social support from sexual and gender minority communities. Few studies (n = 4, 5.19%) investigated social support for transgender individuals from the LGBT community. These studies mainly assessed connectedness to and engagement with the LGBT community, as well as rating the level of positive feelings about the LGBT community. Eight (10.39%) studies investigated social support specifically from the transgender/gender-nonconforming community. Support from the transgender/gender-nonconforming community was measured with a variety of measures, mainly (n = 6, 75.00%) using the Collective Self-Esteem Scale (CSES; Luhtanen & Crocker, 1992) or the Transgender Community Connectedness scale (TCC; Doolin & Budge, 2015).
Internalized proximal resilience.
Prominence, valence, and integration of sexual minority identity were collectively defined as characteristics of minority identity. In total, these characteristics were investigated in six (7.79%) of the included studies.
Discussion
This is the first study to systematically review the literature on mental health problems among TGNC samples while also applying Minority Stress Model as a conceptual framework for critically reviewing this rapidly growing body of literature. All 77 studies included in this review were conducted in the U.S. within the past 20 years. Our analysis of all extracted mental health and minority stress variables revealed a broad spectrum of mental health outcomes, as well as key hypothesized risk and resilience factors. The discussion will focus on several methodological limitations of the existing literature that prevent us from drawing firm conclusions about the association between TGNC identity and mental health outcomes.
Methodological review
The reviewed articles are difficult to compare due to the varied methodologies that researchers applied when selecting their sample. For example, some studies (n=59) relied on standard two-step survey method for identifying their sample, by first asking for assigned sex at birth, then asking for self-identified gender identity, whereas other studies (n=18) relied on medical chart documentation of transgender-related diagnosis (e.g., GID, gender dysphoria) or services and failed to ask about self-identified gender identity. Still further, some researchers limited their samples to individuals who identified as transgender men (n=7) or transgender women (n=22), and were not inclusive of gender non-binary individuals who may also fall within the more inclusive TGNC population. As such, samples summarized here likely represent different transgender and gender-nonconforming populations and some important subgroup differences may be masked. For example, no studies to date have compared transgender men, transgender women, and non-binary identified sub-groups which might reveal important differences in treatment needs and resiliencies among these groups. Moreover, individuals seeking gender confirming services represent only a small sub-set of TGNC individuals, and potentially a population that suffers from comorbid conditions and/or more severe distress about their gender. Thus, over-reliance on data from treatment-seeking TGNC individuals prohibits generalization of findings to all TGNC individuals. Further, TGNC individuals residing in rural areas (U.S. Census Bureau, 2010) are largely unrepresented, with only 22 studies including national sampling, and no studies focusing exclusively on mental health among rural TGNC individuals. Indeed, the majority of sampling occurred in urban settings located either on the eastern (e.g., Massachusetts) or western (e.g., California) coast of the US. Differences in sample selection are not inherently problematic as they can highlight important findings among certain TGNC sample. However, we advise researchers to be explicit regarding the population that their sample purports to represent, and to refrain from generalizing findings to other populations.
Our review highlights numerous problems with measurement of mental health and risk and resilience factors in TGNC individuals. The Minority Stress Model presumes a temporal sequence by which experiences of societal and institutional discrimination (distal stressors) overlay on direct experiences of discrimination due to transgender identity within families and peers and internalized transphobia (interactive and internal proximal stressors), which predate onset of mental health outcomes. Further, resilience factors such as coping and social support from family, peers, and the TGNC community serve as buffers between distal and proximal stressors and reduce risk for mental health outcomes. However, none of the studies in this review examined prospective relationship, nor did they assess pathways associated with poor mental health. New measures such as the Gender Minority Stress and Resilience scale (Testa et al., 2015) may be useful to the field going forward, as it can assist both researchers and clinicians in identifying both risk and resilience factors present for TGNC individuals. The measure taps nine constructs of gender-related discrimination, gender-related rejection, gender-related victimization, non-affirmation of gender identity, internalized transphobia, negative expectations for future events, nondisclosure, community connectedness, and pride.
Notably, intersectionality of multiple minority identities was largely unaddressed in the studies reviewed. Although four studies examined the intersectionality between transgender identity-related discrimination and race and ethnicity-related discrimination, this is an area of research that requires further exploration. And, the context of multiple minorities identities should be further assessed in clients presenting with mental health symptoms (Bazargan & Galvan, 2012; Garofalo et al., 2006; Jefferson et al., 2013; Nemoto et al., 2015). For example, one study (Brown & Jones, 2014) highlighted the differences between white and black veterans with transgender-related diagnoses in their chart. In the context of Minority Stress Model, these analyses are particularly interesting since the white sample represents dual minority group (veterans and TGNC) as compared with those who were triple minorities (also racial/ethnic minority). Of note, odds of having a diagnosis of alcohol abuse, tobacco use, serious mental illness, incarceration and homelessness were all elevated among transgender people of color. However, resilience was also noted with lower odds of depression. Other studies have highlighted the importance of intersectionality, by limiting samples to TGNC people of color, or TGNC veterans, though extensive study of contributions of the intersection of different elements of minority identities have not been undertaken. In effect, it is not clear if the findings of some studies (e.g., those of veterans, and/or transgender people of color) generalize more broadly to the TGNC community.
Few studies (n=13, 17.11%) applied gold standard structured clinical interviews to assess for mental health or substance abuse diagnoses. Most notably, no structured clinical interview for gender dysphoria which replaced gender identity disorder in the DSM-5 (American Psychiatric Association, 2013) currently exists making rigorous assessment difficult to document across studies. Moreover, gender dysphoria is often not the primary mental health concern in this population, and is reflective of the controversy transgender-related diagnoses both in the US and internationally (Coleman et al., 2017). For example, many TGNC researchers and advocates compare the presence of gender dysphoria as a mental health condition akin to the presence of homosexuality at a mental health condition in previous versions of the DSM (removed in 1973). These assertions suggest that transgender-related diagnoses exist only within the context of the larger social context and institutionalized discrimination (James et al., 2016), and the future of the diagnosis as a stand-alone mental health condition remains uncertain. Despite controversy around transgender-related diagnoses, standard assessment may help researchers to build evidence to refute the need for this disorder in additional to mental health conditions that are common in the general population (mood, anxiety, trauma-related disorders).
Conversely, some studies relied on assessment tools that are not appropriate for assessing gender dysphoria or mental health in this population. For example, previous studies have found that The Minnesota Multiphasic Personality Inventory (MMPI; Hathaway & McKinley, 1943) has poor psychometrics and is often invalid for TGNC populations (Cole et al., 1997; Keo-Meier et al., 2015). Further, studies rarely linked exposure to discrimination or violence to posttraumatic stress symptoms, thus, rendering most assessments of posttraumatic stress symptoms (3 out of 14 studies, 21.43%) insufficient in determining probable posttraumatic stress disorder (PTSD) diagnoses. These findings highlight the importance of rigorous assessment as well as the need for prospective data, or cross-sectional designs that allow for preliminary pathway analyses.
Few studies in this systematic review included TGNC individuals as stakeholders in at every stage of the research process. TGNC individuals are largely unrepresented among medical and mental health providers and academics alike. Thus, inclusion of TGNC individuals in directing research questions, development and validation of assessment tools for this population, collection of data as trained interviewers and outreach workers, and involvement in the interpretation and presentation of findings is key. We commend studies that employed community-based participatory research strategies such as these (Garofalo et al., 2006; Reisner et al., 2016; Reisner et al., 2016; Jefferson et al., 2013; Robinson & Ross, 2013), and recommend that other researcher learn from these lessons. Simultaneously, educational institutions should extend diversity initiatives to include gender minority students, who can then increase the representation of TGNC individuals in the healthcare workforce.
Mental health outcomes
There are many studies that discussed bivariate associations between TGNC identity and a range of mental health problems, including depression, anxiety, substance use, and suicidality—so more of this work is not what is most needed in the field. Although the existing literature has measured how mental health problems correlate with some aspects of the Minority Stress Model, our results suggest the need for more comprehensive studies that draw from the Minority Stress Model and rigorously test pathways to poor mental health outcomes. The context of minority stress is of utmost importance, because this model helps to understand risk and resilience pathways in relation to health outcomes. The Minority Stress Model also suggests that individual-level interventions that help individuals (a) gain healthy coping skills, (b) access social supports, and (c) reduce symptomatology are necessary, but not sufficient in addressing the socially-produced drivers of mental health disparities in gender minority populations.
Focusing too narrowly on mental health outcomes may serve to over-pathologize a vulnerable population who may be experiencing a normative response to pervasive discrimination, violence, and exclusion. Thus, assessment of mental health symptoms should include assessment of contextual factors that produced the vulnerability for these conditions. Full diagnostic assessment for TGNC individuals should include assessment of mental health diagnoses and minority stress variables highlighted in this review, including depression, anxiety disorders, PTSD, suicidality, discrimination and violence exposure, and the client’s appraisal of whether identity is contributory to exposures or presenting problems.
Risk and resilience factors
We were pleased to find that more than half of the studies assessed some aspect of resilience among TGNC individuals that is consistent with Minority Stress Model. This included assessment of social supports, identity integration and self-esteem, and positively-valenced gender identity. These studies provide cross-sectional evidence of the association between resilience factors and lower mental health symptomatology. Moreover, there are promising findings from studies of children and adolescents with affirming parents and providers, that may point to the important buffering and, perhaps, preventative effect of affirmative early environments on the development of mental health problems. In two studies that utilized matched controls, researchers found that TGNC children and adolescents did not differ in terms of mental health outcomes compared to their siblings, and age and gender-matched controls.
Promising prevention efforts and interventions
Addressing mental health problems in TGNC populations calls for multi-level interventions that address institutional discrimination as well as individual-level symptomatology and general psychosocial functioning. Recent studies on suicidality and mental health among TGNC veterans across the US found that veterans living in states with employment protections reported lower suicidality and mental health distress compared to veterans living in states that did not have such protections (Blosnich et al. 2017). This study is just one example of how policy makers can affect TGNC population health, and call for provider to assume an advocacy role within the systems they work. To address socially produced distress, providers are charged with gaining training and knowledge necessary to help TGNC clients feel safe and welcome in clinical settings. One study in this review found that TGNC clients who reported having a transgender-inclusive provider were less likely to report symptoms of depression (38% v. 54%), anxiety (51% v. 57%), and suicidality (29% v. 48%) in the past year compared to TGNC clients who did not report having a transgender-inclusive provider (Kattari et al. 2016). Stanton and colleagues (Stanton et al., 2017) also found that provider comfort in working with TGNC client was positively associated with psychological well-being in the client. These data suggest that gender affirmation by providers is essential to addressing mental health symptoms among TGNC clients. An affirmative stance needs to be reflected across the healthcare system, including welcoming images, intake forms and established processed for preferred name and pronoun use. Our review also suggests that providers may need to engage community supports, parents, caregivers, families, and schools to emphasize the importance of gender-affirmation (through behavior and institutional policies).
There is notable gap in clinical trials addressing mental health symptoms among TGNC clients. All 3 described interventions were educational programs focused narrowly on HIV health promotion, rather than mental health interventions, per se. (Nemoto et al., 2015; Nemoto et al., 2005; Reisner et al., 2016). Some interesting conceptual work on treatment for TGNC people has been published, including the application of a Dialectical Behavior Therapy-based approach to the conceptualization and treatment of gender dysphoria (Sloan & Berke, 2018; Sloan, Berke, & Shipherd, 2017). Although, rigorous testing of this treatment approach has yet to be undertaken.
Medical interventions such as cross-sex hormones and gender confirming surgeries are important as part of interdisciplinary treatment. Existing research on the relationship between mental health symptoms and medical interventions consistently suggests the benefit and safety of these interventions (Murad et al., 2010). In this review, we identified studies suggesting clinical improvements in transmen receiving testosterone (Keo-Meier et al., 2015), lower suicidality and substance use among transwomen who had received hormones or gender confirming care compared to transwomen who did not utilize transition-related medical care (Wilson et al., 2015), and lower levels of depression, anxiety, and stress, and higher levels of social support among transmen who were using testosterone compared to transmen who were not receiving testosterone (Colton-Meier et al., 2011). Despite the promise of medical intervention in alleviating mental health distress, access to gender confirming services remains a significant problem across the U.S. For example, in the largest online sample of self-identified transgender people in the U.S., 25% endorsed problems accessing care because they were transgender, with surgical care access being denied among 55% of the sample. Moreover, 33% reported discrimination (including verbal and physical harassment) in health care settings (James et al., 2016). In our review, one study found that 29% of pediatric clients referred for gender dysphoria and their caregivers experienced difficulties finding a professional to do the required mental health evaluation for cross-sex hormones (Chen et al., 2016).
Strengths and limitations
This review extends our knowledge of the range of variables that are likely associated with mental health outcomes observed in TGNC individuals. The existing literature has captured relevant risk and resilience factors that must be appreciated when understanding the treatment needs of TGNC individuals. Together, these studies suggest a range of interventions that dually address socially produced distress as well as psychopathology, including interventions at the individual, support system, and institutional level. For example, studies consistently reported that social support was central to protecting against mental health distress, and that absence of social supports and adequate coping skills were associated with poor outcomes. We discussed our findings with attention to clinical implications and offered suggestions for policy-makers and future research. However, several limitations need to be considered. As with any systematic review, our search may not have been exhaustive. This is a rapidly growing area of research, and thus there are likely additional ongoing studies that may provide valuable insight in the near future. To demonstrate, 23 (32%) of the studies in this review were published within the last year, and 58 (80.5%) were published within the last 5 years. TGNC individuals living outside of major cities such as Boston, San Francisco, and Chicago are largely unrepresented, and studies that utilized US samples did not yield nationally representative samples. For this reason, our findings may not represent the diversity of the TGNC population, and TGNC individuals in urban settings and who had engaged in transgender-related care are overrepresented. As noted, assessments of gender identity, mental health variables, and resilience factors were not standardized across studies, thus, our categorization into specific related constructs may not have captured the experiences within each category. For example, depression (in Table 2), was assessed through structured clinical interview, inventories of depressive symptoms, diagnosis in medical records, or self-reported “history of depression.” These varied assessments prohibited us from drawing firm comparisons across studies, and we may be missing important variability in functioning in this domain as some studies examine lifetime diagnoses whereas other studies looked at current functioning. Additionally, posttraumatic stress symptoms were rarely linked to Criterion A events for PTSD, and, thus, PTSD prevalence is not adequately represented in the extant literature. An exception to this trend asked participants about trauma exposure and linked PTSD symptom assessment to the event that was troubling them the most at the time of assessment (Shipherd et al., 2011). Given that it is well established that TGNC people have higher rates of exposure to interpersonal violence (Valentine et al., 2017), we were surprised that so few studies rigorously assessed sequelae of these experiences. Finally, given that gender identity is not routinely and consistently assessed across federal or state-based surveys, nor is it consistently assessed in all medical records, it impossible to define the populations of TGNC people in the US. As such, the studies included here relied upon samples of convenience and/or subsets of the TGNC community (e.g., those with a diagnosis). As such, it is premature to discuss prevalence rates of any of the conditions evaluated in this review.
Conclusions and future directions
Research should be guided by theoretical models. The Minority Stress Model attempts to conceptualize pathways to poor mental health as well as pathways to resilience for TGNC individuals. We assert that this model should be used as a basis for future research, and that studies systematically test pathways to risk and recovery for this highly vulnerable population. We also suggest the use of standardized assessments, where possible, for mental health symptoms, and the deployment of population-based random sampling strategies to provide prevalence data. In particular, systematic and routine collection of gender identity information as a part of population health, medical record systems, as well as independent research could further expand our understanding of TGNC people. The Minority Stress Model may need further adaptation to best suit the experiences of TGNC individuals, and we strongly suggest the application of community-based participatory research strategies to inform adaptations as well as formal testing of this model.
In the absence of strong clinical trials for mental health symptoms in this population, we recommend that use of existing evidence-based treatments for depression, anxiety, and posttraumatic stress symptoms. When applying these evidence-based treatments, however, the provider must fully assess contextual factors (such as discrimination, internalized transphobia) and conceptualize how these factors are related (or are not related) the mental health symptoms targeted in treatment. Mental health clinicians are in the unique position to ameliorate some aspects of social stress by stepping into the role of the advocate for TGNC clients. This requires providers to work within their healthcare settings to create safe and welcoming environment, to be knowledgeable about hospital policies that affect TGNC clients, and to be knowledgeable of local community resources for TGNC individuals.
Acknowledgements
We would like to express our gratitude to our research assistants, Andrew Curreri and Michelle Coughlin, for their support in preparing this manuscript.
Abbreviations:
- TGNC
Transgender and gender non-conforming
References
- Ainsworth TA, & Spiegel JH (2010). Quality of life of individuals with and without facial feminization surgery or gender reassignment surgery. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 19(7), 1019–1024. doi: 10.1007/s11136-010-9668-7 [DOI] [PubMed] [Google Scholar]
- Alim TN, Graves E, Mellman TA, Aigbogun N, Gray E, Lawson W, & Charney DS (2006). Trauma exposure, posttraumatic stress disorder and depression in an african-american primary care population. Journal of the National Medical Association, 98(10), 1630–1636. [PMC free article] [PubMed] [Google Scholar]
- I am Cait. (2016). Retrieved from http://www.eonline.com/shows/i_am_cait
- I am Jazz. (2015). Retrieved from https://www.tlc.com/tv-shows/i-am-jazz/
- American Medical Association. Access to basic human services for transgender individuals H-65.964, Health Policies U.S.C; (2017). [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- American Psychological Association. (2015). Guidelines for psychological practice with transgender and gender nonconforming people. American Psychologist, 70(9), 832–864. doi: 10.1037/a0039906 [DOI] [PubMed] [Google Scholar]
- Barr SM, Budge SL, & Adelson JL (2016). Transgender community belongingness as a mediator between strength of transgender identity and well-being. Journal of Counseling Psychology, 63(1), 87–97. doi: 10.1037/cou0000127 [DOI] [PubMed] [Google Scholar]
- Bazargan M, & Galvan F (2012). Perceived discrimination and depression among low-income Latina male-to-female transgender women. BMC Public Health, 12, 663. doi: 10.1186/1471-2458-12-663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benotsch EG, Zimmerman R, Cathers L, McNulty S, Pierce J, Heck T, … Snipes D (2013). Non-medical use of prescription drugs, polysubstance use, and mental health in transgender adults. Drug and Alcohol Dependence, 132(1–2), 391–394. doi: 10.1016/j.drugalcdep.2013.02.027 [DOI] [PubMed] [Google Scholar]
- Blosnich JR, Brown GR, Shipherd Phd JC, Kauth M, Piegari RI, & Bossarte RM (2013). Prevalence of gender identity disorder and suicide risk among transgender veterans utilizing Veterans Health Administration care. American Journal of Public Health, 103(10), e27–32. doi: 10.2105/AJPH.2013.301507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blosnich JR, Brown GR, Wojcio S, Jones KT, & Bossarte RM (2014). Mortality among veterans with transgender-related diagnoses in the Veterans Health Administration, FY2000–2009. LGBT Health, 1(4), 269–276. doi: 10.1089/lgbt.2014.0050 [DOI] [PubMed] [Google Scholar]
- Blosnich JR, Marsiglio MC, Gao S, Gordon AJ, Shipherd JC, Kauth M, … Fine MJ. (2016). Mental health of transgender Veterans in US states with and without discrimination and hate crime legal protection. American Journal of Public Health, 106(3), 534–540. doi: 10.2105/AJPH.2015.302981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blosnich JR, Marsiglio MC, Dichter M, Gao S, Gordon AJ, Shipherd JC, Kauth M, Brown GR, & Fine MJ (2017). Impact of social determinants of health on medical conditions among transgender veterans. American Journal of Preventive Medicine, 52(4), 491–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bockting WO, Miner MH, Swinburne Romine RE, Hamilton A, & Coleman E (2013). Stigma, mental health, and resilience in an online sample of the US transgender population. American Journal of Public Health, 103(5), 943–951. doi: 10.2105/AJPH.2013.301241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradford J, Reisner SL, Honnold JA, & Xavier J (2013). Experiences of transgender-related discrimination and implications for health: Results from the Virginia Transgender Health Initiative Study. American Journal of Public Health, 103(10), 1820–1829. doi: 10.2105/AJPH.2012.300796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan J, Kuhns LM, Johnson AK, Belzer M, Wilson EC, Garofalo R, & Adolescent Medicine Trials Network for HIV. (2012). Syndemic theory and HIV-related risk among young transgender women: The role of multiple, co-occurring health problems and social marginalization. American Journal of Public Health, 102(9), 1751–1757. doi: 10.2105/AJPH.2011.300433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown GR, & Jones KT (2014). Racial health disparities in a cohort of 5,135 transgender veterans. Journal of Racial and Ethnic Health Disparities, 1(4), 257–266. doi: 10.1007/s40615-014-0032-4 [DOI] [Google Scholar]
- Brown GR, & Jones KT (2015). Health correlates of criminal justice involvement in 4,793 transgender veterans. LGBT Health, 2(4), 297–305. doi: 10.1089/lgbt.2015.0052 [DOI] [PubMed] [Google Scholar]
- Brown GR, & Jones KT (2016). Mental health and medical health disparities in 5135 transgender veterans receiving healthcare in the Veterans Health Administration: A case-control study. LGBT Health, 3(2), 122–131. doi: 10.1089/lgbt.2015.0058 [DOI] [PubMed] [Google Scholar]
- Brown LS, Pantalone D, Shipherd JC, Maguen S, Skidmore WC, & Abramovitz SM (2011). Potentially traumatic events in a transgender sample. Traumatology, 17(2), 56–67. doi: 10.1177/1534765610395614 [DOI] [Google Scholar]
- Budge SL, Adelson JL, & Howard KAS (2013). Anxiety and depression in transgender individuals: The roles of transition status, loss, social support, and coping. Journal of Consulting and Clinical Psychology, 81(3), 545–557. doi: 10.1037/a0031774 [DOI] [PubMed] [Google Scholar]
- Chen M, Fuqua J, & Eugster EA (2016). Reply to: Zucker et al., “comment on chen, fuqua, and eugster’s (2016) ‘characteristics of referrals for gender dysphoria over a 13-year period’”. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 58(6), 694. doi: 10.1016/j.jadohealth.2016.03.028 [DOI] [PubMed] [Google Scholar]
- Chesney MA, Neilands TB, Chambers DB, Taylor JM and Folkman S (2006), A validity and reliability study of the coping self-efficacy scale. British Journal of Health Psychology, 11: 421–437. doi: 10.1348/135910705X53155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clements-Nolle K, Marx R, Guzman R, & Katz M (2001). HIV prevalence, risk behaviors, health care use, and mental health status of transgender persons: Implications for public health intervention. American Journal of Public Health, 91(6), 915–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clements-Nolle K, Marx R, & Katz M (2006). Attempted suicide among transgender persons: The influence of gender-based discrimination and victimization. Journal of Homosexuality, 51(3), 53–69. doi: 10.1300/J082v51n03_04 [DOI] [PubMed] [Google Scholar]
- Cochran BN, & Robohm JS (2015). Integrating LGBT competencies into the multicultural curriculum of graduate psychology training programs: Expounding and expanding upon hope and chappell’s choice points: Commentary on “Extending training in multicultural competencies to include individuals identifying as lesbian, gay, and bisexual: Key choice points for clinical psychology training programs”. Clinical Psychology: Science and Practice, 22(2), 119–126. doi: 10.1111/cpsp.12095 [DOI] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. [PubMed] [Google Scholar]
- Cole CM, O’Boyle M, Emory LE, & Meyer WJ (1997). Comorbidity of gender dysphoria and other major psychiatric diagnoses. Archives of Sexual Behavior, 26(1), 13–26. [DOI] [PubMed] [Google Scholar]
- Coleman E, Wylie K, Coates R, Rubio-Aurioles E, Hernandez-Serrano R, Wabrek A, … Forleo R (2017). Commentary: Revising the international classification of diseases (ICD-11) and improving global sexual health: Time for an integrated approach that moves beyond the mind-body divide. International Journal of Sexual Health, 29(2), 113–114. doi: 10.1080/19317611.2017.1311126 [DOI] [Google Scholar]
- Colton Meier SL, Fitzgerald KM, Babcock J, & Pardo ST (2011). The effects of hormonal gender affirmation treatment on mental health in female-to-male transsexuals. Journal of Gay & Lesbian Mental Health, 15(3), 281–299. doi: 10.1080/19359705.2011.581195 [DOI] [Google Scholar]
- Doolin G, & Budge SL (2015). Validation of the Lesbian Community Belongingness Scale Unpublished manuscript. Madison, WI: University of Wisconsin-Madison. [Google Scholar]
- Dowshen N, Matone M, Luan X, Lee S, Belzer M, Fernandez MI, & Rubin D (2016). Behavioral and health outcomes for HIV+ young transgender women linked to and engaged in medical care. LGBT Health, 3(2), 162–167. doi: 10.1089/lgbt.2014.0062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubois LZ (2012). Associations between transition-specific stress experience, nocturnal decline in ambulatory blood pressure, and C-reactive protein levels among transgender men. American Journal of Human Biology: The Official Journal of the Human Biology Council, 24(1), 52–61. doi: 10.1002/ajhb.22203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durwood L, McLaughlin KA, & Olson KR (2017). Mental health and self-worth in socially transitioned transgender youth. Journal of the American Academy of Child and Adolescent Psychiatry, 56(2), 116–123.e2. doi: 10.1016/j.jaac.2016.10.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (1997). Structured clinical interview for DSM-IV axis I disorders (SCID-I), clinician version, User’s guide. Arlington, VA. [Google Scholar]
- Flentje A, Heck NC, & Sorensen JL (2014). Characteristics of transgender individuals entering substance abuse treatment. Addictive Behaviors, 39(5), 969–975. doi: 10.1016/j.addbeh.2014.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flentje A, Leon A, Carrico A, Zheng D, & Dilley J (2016). Mental and physical health among homeless sexual and gender minorities in a major urban US city. Journal of Urban Health: Bulletin of the New York Academy of Medicine, 93(6), 997–1009. doi: 10.1007/s11524-016-0084-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman S, & Lazarus RS (1985). If it changes it must be a process: Study of emotion and coping during three stages of a college examination. Journal of Personality and Social Psychology, 48(1), 150–170. http://dx.doi.org.ezproxy.bu.edu/10.1037/0022-3514.48.1.150 [DOI] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K, Cook-Daniels L, Kim H, Erosheva EA, Emlet CA, Hoy-Ellis C, … Muraco A (2014). Physical and mental health of transgender older adults: An at-risk and underserved population. The Gerontologist, 54(3), 488–500. doi: 10.1093/geront/gnt021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamarel KE, Reisner SL, Laurenceau J, Nemoto T, & Operario D (2014). Gender minority stress, mental health, and relationship quality: A dyadic investigation of transgender women and their cisgender male partners. Journal of Family Psychology: JFP: Journal of the Division of Family Psychology of the American Psychological Association (Division 43), 28(4), 437–447. doi: 10.1037/a0037171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R, Deleon J, Osmer E, Doll M, & Harper GW (2006). Overlooked, misunderstood and at-risk: Exploring the lives and HIV risk of ethnic minority male-to-female transgender youth. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 38(3), 230–236. doi: 10.1016/j.jadohealth.2005.03.023 [DOI] [PubMed] [Google Scholar]
- Gerrig RJ, & Zimbardo PG (2002). Psychology and life (16th ed). Boston, MA: Allyn and Bacon. [Google Scholar]
- Glynn TR, Gamarel KE, Kahler CW, Iwamoto M, Operario D, & Nemoto T (2016). The role of gender affirmation in psychological well-being among transgender women. Psychology of Sexual Orientation and Gender Diversity, 3(3), 336–344. doi: 10.1037/sgd0000171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hathaway SR, & McKinley JC. 1943. The Minnesota Multiphasic Personality Inventory (Rev. ed., 2nd printing). Minneapolis, US: University of Minnesota Press. [Google Scholar]
- Gorgens KA (2011). Structured clinical interview for DSM-IV (SCID-I/SCID-II) In Kreutzer JS, DeLuca J & Caplan B (Eds.), Encyclopedia of clinical neuropsychology (pp. 2410–2417). New York, NY: Springer New York. doi: 10.1007/978-0-387-79948-3_2011 [DOI] [Google Scholar]
- Hendricks ML, & Testa RJ (2012). A conceptual framework for clinical work with transgender and gender nonconforming clients: An adaptation of the minority stress model. Professional Psychology: Research and Practice, 43(5), 460–467. doi: 10.1037/a0029597 [DOI] [Google Scholar]
- Horvath KJ, Iantaffi A, Swinburne-Romine R, & Bockting W (2014). A comparison of mental health, substance use, and sexual risk behaviors between rural and non-rural transgender persons. Journal of Homosexuality, 61(8), 1117–1130. doi: 10.1080/00918369.2014.872502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoy-Ellis C, Shiu C, Sullivan KM, Kim H, Sturges AM, & Fredriksen-Goldsen K (2017). Prior military service, identity stigma, and mental health among transgender older adults. The Gerontologist, 57, S63–S71. doi: 10.1093/geront/gnw173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- James SE, Herman JL, Rankin S, Keisling M, Mottet L, & Anafi M (2016). The report of the 2015 U.S. transgender survey. Washington, DC: National Center for Transgender Equality. [Google Scholar]
- Jefferson K, Neilands TB, & Sevelius J (2013). Transgender women of color: Discrimination and depression symptoms. Ethnicity and Inequalities in Health and Social Care, 6(4), 121–136. doi: 10.1108/EIHSC-08-2013-0013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kattari SK, Walls NE, Speer SR, & Kattari L (2016). Exploring the relationship between transgender-inclusive providers and mental health outcomes among transgender/gender variant people. Social Work in Health Care, 55(8), 635–650. doi: 10.1080/00981389.2016.1193099 [DOI] [PubMed] [Google Scholar]
- Katz-Wise S, Reisner SL, White Hughto JM, & Budge SL (2017). Self-reported changes in attractions and social determinants of mental health in transgender adults. Archives of Sexual Behavior, 46(5), 1425–1439. doi: 10.1007/s10508-016-0812-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keo-Meier C, Herman LI, Reisner SL, Pardo ST, Sharp C, & Babcock JC (2015). Testosterone treatment and MMPI-2 improvement in transgender men: A prospective controlled study. Journal of Consulting and Clinical Psychology, 83(1), 143–156. doi: 10.1037/a0037599 [DOI] [PubMed] [Google Scholar]
- Keuroghlian AS, Reisner SL, White JM, & Weiss RD (2015). Substance use and treatment of substance use disorders in a community sample of transgender adults. Drug and Alcohol Dependence, 152, 139–146. doi: 10.1016/j.drugalcdep.2015.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le V, Arayasirikul S, Chen Y, Jin H, & Wilson EC (2016). Types of social support and parental acceptance among transfemale youth and their impact on mental health, sexual debut, history of sex work and condomless anal intercourse. Journal of the International AIDS Society, 19(3), 20781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehavot K, Simpson TL, & Shipherd JC (2016). Factors associated with suicidality among a national sample of transgender veterans. Suicide & Life-Threatening Behavior, 46(5), 507–524. doi: 10.1111/sltb.12233 [DOI] [PubMed] [Google Scholar]
- Leinung MC, Urizar MF, Patel N, & Sood SC (2013). Endocrine treatment of transsexual persons: Extensive personal experience. Endocrine Practice: Official Journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists, 19(4), 644–650. doi: 10.4158/EP12170.OR [DOI] [PubMed] [Google Scholar]
- Lindsay JA, Keo-Meier C, Hudson S, Walder A, Martin LA, & Kauth MR (2016). Mental health of transgender veterans of the iraq and afghanistan conflicts who experienced military sexual trauma. Journal of Traumatic Stress, 29(6), 563–567. doi: 10.1002/jts.22146 [DOI] [PubMed] [Google Scholar]
- Luhtanen R, & Crocker J (1992). A collective self-esteem scale: Self-evaluation of one’s social identity. Pers Soc Psychol Bull, 18(3), 302–318. doi: 10.1177/0146167292183006 [DOI] [Google Scholar]
- Maguen S, & Shipherd JC (2010). Suicide risk among transgender individuals. Psychology and Sexuality, 1(1), 34–43. 10.1080/19419891003634430 [DOI] [Google Scholar]
- Mathy RM (2003). Transgender identity and suicidality in a nonclinical sample. Journal of Psychology & Human Sexuality, 14(4), 47–65. doi: 10.1300/J056v14n04_03 [DOI] [Google Scholar]
- McDuffie E, & Brown GR (2010). 70 U.S. veterans with gender identity disturbances: A descriptive study. International Journal of Transgenderism, 12(1), 21–30. doi: 10.1080/15532731003688962 [DOI] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. doi: 10.1037/0033-2909.129.5.674 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, Brown TNT, Herman JL, Reisner SL, & Bockting WO (2017). Demographic characteristics and health status of transgender adults in select US regions: Behavioral risk factor surveillance system, 2014. American Journal of Public Health, 107(4), 582–589. doi: 10.2105/AJPH.2016.303648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murad MH, Elamin MB, Garcia MZ, Mullan RJ, Murad A, Erwin PJ, & Montori VM (2010). Hormonal therapy and sex reassignment: A systematic review and meta-analysis of quality of life and psychosocial outcomes. Clinical Endocrinology, 72(2), 214–231. doi: 10.1111/j.1365-2265.2009.03625.x [DOI] [PubMed] [Google Scholar]
- Nemoto T, Cruz TM, Iwamoto M, & Sakata M (2015). A tale of two cities: Access to care and services among african-american transgender women in oakland and san francisco. LGBT Health, 2(3), 235–242. doi: 10.1089/lgbt.2014.0046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemoto T, Operario D, Keatley J, Nguyen H, & Sugano E (2005). Promoting health for transgender women: Transgender resources and neighborhood space (TRANS) program in san francisco. American Journal of Public Health, 95(3), 382–384. doi: 10.2105/AJPH.2004.040501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newfield E, Hart S, Dibble S, & Kohler L (2006). Female-to-male transgender quality of life. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 15(9), 1447–1457. doi: 10.1007/s11136-006-0002-3 [DOI] [PubMed] [Google Scholar]
- Nuttbrock L, Bockting W, Rosenblum A, Hwahng S, Mason M, Macri M, & Becker J (2014). Gender abuse and major depression among transgender women: A prospective study of vulnerability and resilience. American Journal of Public Health, 104(11), 2191–2198. doi: 10.2105/AJPH.2013.301545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuttbrock L, Hwahng S, Bockting W, Rosenblum A, Mason M, Macri M, & Becker J (2010). Psychiatric impact of gender-related abuse across the life course of male-to-female transgender persons. Journal of Sex Research, 47(1), 12–23. doi: 10.1080/00224490903062258 [DOI] [PubMed] [Google Scholar]
- Olson J, Schrager SM, Belzer M, Simons LK, & Clark LF (2015). Baseline physiologic and psychosocial characteristics of transgender youth seeking care for gender dysphoria. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 57(4), 374–380. doi: 10.1016/j.jadohealth.2015.04.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson KR, Durwood L, DeMeules M, & McLaughlin KA (2016). Mental health of transgender children who are supported in their identities. Pediatrics, 137(3), e20153223. doi: 10.1542/peds.2015-3223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Operario D, Nemoto T, Iwamoto M, & Moore T (2011). Unprotected sexual behavior and HIV risk in the context of primary partnerships for transgender women. AIDS and Behavior, 15(3), 674–682. doi: 10.1007/s10461-010-9795-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson CM, Matthews A, Copps-Smith E, & Conard LA (2017). Suicidality, self-harm, and body dissatisfaction in transgender adolescents and emerging adults with gender dysphoria. Suicide & Life-Threatening Behavior, 47(4), 475–482. doi: 10.1111/sltb.12289 [DOI] [PubMed] [Google Scholar]
- Reisner SL, Biello KB, White Hughto JM, Kuhns L, Mayer KH, Garofalo R, & Mimiaga MJ (2016). Psychiatric diagnoses and comorbidities in a diverse, multicity cohort of young transgender women: Baseline findings from project LifeSkills. JAMA Pediatrics, 170(5), 481–486. doi: 10.1001/jamapediatrics.2016.0067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Katz-Wise S, Gordon AR, Corliss HL, & Austin SB (2016). Social epidemiology of depression and anxiety by gender identity. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 59(2), 203–208. doi: 10.1016/j.jadohealth.2016.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Vetters R, Leclerc M, Zaslow S, Wolfrum S, Shumer D, & Mimiaga MJ (2015a). Mental health of transgender youth in care at an adolescent urban community health center: A matched retrospective cohort study. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 56(3), 274–279. doi: 10.1016/j.jadohealth.2014.10.264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Vetters R, White JM, Cohen EL, LeClerc M, Zaslow S, … Mimiaga MJ (2015b). Laboratory-confirmed HIV and sexually transmitted infection seropositivity and risk behavior among sexually active transgender patients at an adolescent and young adult urban community health center. AIDS Care, 27(8), 1031–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, White JM, Mayer KH, & Mimiaga MJ (2014). Sexual risk behaviors and psychosocial health concerns of female-to-male transgender men screening for STDs at an urban community health center. AIDS Care, 26(7), 857–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, White Hughto JM, Pardee DJ, Kuhns L, Garofalo R, & Mimiaga MJ (2016a). LifeSkills for men (LS4M): Pilot evaluation of a gender-affirmative HIV and STI prevention intervention for young adult transgender men who have sex with men. Journal of Urban Health: Bulletin of the New York Academy of Medicine, 93(1), 189–205. doi: 10.1007/s11524-015-0011-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, White Hughto JM, Gamarel KE, Keuroghlian AS, Mizock L, & Pachankis JE (2016b). Discriminatory experiences associated with posttraumatic stress disorder symptoms among transgender adults. Journal of Counseling Psychology, 63(5), 509–519. doi: 10.1037/cou0000143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson M, & Ross LE (2013). Gender and sexual minorities: Intersecting inequalities and health. Ethnicity and Inequalities HSC, 6(4), 91–96. doi: 10.1108/EIHSC-01-2014-0003 [DOI] [Google Scholar]
- Rowe C, Santos G, McFarland W, & Wilson EC (2015). Prevalence and correlates of substance use among trans female youth ages 16–24 years in the san francisco bay area. Drug and Alcohol Dependence, 147, 160–166. doi: 10.1016/j.drugalcdep.2014.11.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell ST, Ryan C, Toomey RB, Diaz RM, & Sanchez J (2011). Lesbian, gay, bisexual, and transgender adolescent school victimization: Implications for young adult health and adjustment. The Journal of School Health, 81(5), 223–230. doi: 10.1111/j.1746-1561.2011.00583.x [DOI] [PubMed] [Google Scholar]
- Ryan C, Russell ST, Huebner D, Diaz R, & Sanchez J (2010). Family acceptance in adolescence and the health of LGBT young adults. Journal of Child and Adolescent Psychiatric Nursing : Official Publication of the Association of Child and Adolescent Psychiatric Nurses, Inc, 23(4), 205–213. doi: 10.1111/j.1744-6171.2010.00246.x [DOI] [PubMed] [Google Scholar]
- Sánchez FJ, & Vilain E (2009). Collective self-esteem as a coping resource for male-to-female transsexuals. Journal of Counseling Psychology, 56(1), 202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar LF, Crosby RA, Jones J, Kota K, Hill B, & Masyn KE (2017). Contextual, experiential, and behavioral risk factors associated with HIV status: A descriptive analysis of transgender women residing in Atlanta, Georgia. International Journal of STD & AIDS, 28(11), 1059–1066. doi: 10.1177/0956462416686722 [DOI] [PubMed] [Google Scholar]
- Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, … Stewart LA (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration & explanation. BMJ, 349 doi: 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- Shipherd JC, Green KE, & Abramovitz S (2010). Transgender Clients: Identifying and Minimizing Barriers to Mental Health Treatment. Journal of Gay & Lesbian Mental Health, 14(2), 94–108. 10.1080/19359701003622875 [DOI] [Google Scholar]
- Shipherd JC, Maguen S, Skidmore WC, & Abramovitz SM (2011). Potentially traumatic events in a transgender sample: Frequency and associated symptoms. Traumatology, 17(2), 56–67. 10.1177/1534765610395614 [DOI] [Google Scholar]
- Shipherd JC, Mizock L, Maguen S, & Green KE (2012). Male-to-Female Transgender Veterans and VA Health Care Utilization. International Journal of Sexual Health, 24(1), 78–87. 10.1080/19317611.2011.639440 [DOI] [Google Scholar]
- Shipherd JC, Kauth MR, Firek AF, Garcia R, Mejia S, Laski S, … Byne W (2016). Interdisciplinary transgender veteran care: Development of a core curriculum for VHA providers. Transgender Health, 1(1), 54–62. doi: 10.1089/trgh.2015.0004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons L, Schrager SM, Clark LF, Belzer M, & Olson J (2013). Parental support and mental health among transgender adolescents. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 53(6), 791–793. doi: 10.1016/j.jadohealth.2013.07.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan CA, & Berke DS (2018). In Kauth MR, Shipherd JC (Eds.), Dialectical behavior therapy as a treatment option for complex cases of gender dysphoria In Adult Transgender Care: An Interdisciplinary Approach for Training Mental Health Professionals. Routledge, NY. [Google Scholar]
- Sloan CA, Berke DS, & Shipherd JC (2017). Utilizing a dialectical framework to inform conceptualization and treatment of gender dysphoria. Professional Psychology: Research and Practice. 48(5), 301–309. 10.1037/pro0000146. [DOI] [Google Scholar]
- Spack NP, Edwards-Leeper L, Feldman HA, Leibowitz S, Mandel F, Diamond DA, & Vance SR (2012). Children and adolescents with gender identity disorder referred to a pediatric medical center. Pediatrics, 129(3), 418–425. doi: 10.1542/peds.2011-0907 [DOI] [PubMed] [Google Scholar]
- Stanton MC, Ali S, & Chaudhuri S (2017). Individual, social and community-level predictors of wellbeing in a US sample of transgender and gender non-conforming individuals. Culture, Health & Sexuality, 19(1), 32–49. [DOI] [PubMed] [Google Scholar]
- Steinmetz K (2017, March 16). Beyond “he” or “she”: The changing meaning of gender and sexuality. Time. Retrieved from http://time.com/4703309/infinite-identities-gender-sexuality-young-people/
- Sterzing PR, Ratliff GA, Gartner RE, McGeough BL, & Johnson KC (2017). Social ecological correlates of polyvictimization among a national sample of transgender, genderqueer, and cisgender sexual minority adolescents. Child Abuse & Neglect, 67, 1–12. doi: 10.1016/j.chiabu.2017.02.017 [DOI] [PubMed] [Google Scholar]
- Testa RJ, Habarth J, Peta J, Balsam K, & Bockting W (2015). Development of the gender minority stress and resilience measure. . Psychology of Sexual Orientation and Gender Diversity, 2(1), 65–77. doi:doi: 10.1037/sgd0000081 [DOI] [Google Scholar]
- Transparent. (2016). Retrieved from http://www.tv.com/shows/transparent/
- U.S. Census Bureau. (2010). 2010 census urban and rural classification and urban area criteria. Retrieved from https://www.census.gov/geo/reference/ua/urban-rural-2010.html
- Valentine SE, Peitzmeier SM, King DS, O’Cleirigh C, Marquez S, Presley C, & Potter J (2017). Disparities in exposure to intimate partner violence among transgender/gender nonconforming and sexual minority primary care patients. LGBT Health, 4(4), 270–267. doi: 10.1089/lgbt.2016.0113 [DOI] [PubMed] [Google Scholar]
- Valentine SE, Woulfe J, & Shipherd JC (in press). An evidence-based approach to conceptualizing trauma responses among transgender and gender non-conforming (TGNC) adults. In Pachankis JE, & Safren SA (Eds.), Handbook of evidence-based mental health practice with LGBT clients (). New York: Oxford University Press. [Google Scholar]
- Warren JC, Smalley KB, & Barefoot KN (2016). Differences in psychosocial predictors of obesity among LGBT subgroups. LGBT Health, 3(4), 283–291. [DOI] [PubMed] [Google Scholar]
- White Hughto JM, Pachankis JE, Willie TC, & Reisner SL (2017). Victimization and depressive symptomology in transgender adults: The mediating role of avoidant coping. Journal of Counseling Psychology, 64(1), 41–51. doi: 10.1037/cou0000184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson EC, Chen Y, Arayasirikul S, Raymond HF, & McFarland W (2016). The impact of discrimination on the mental health of trans*female youth and the protective effect of parental support. AIDS and Behavior, 20(10), 2203–2211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson EC, Chen Y, Arayasirikul S, Wenzel C, & Raymond HF (2015). Connecting the dots: Examining transgender women’s utilization of transition-related medical care and associations with mental health, substance use, and HIV. Journal of Urban Health: Bulletin of the New York Academy of Medicine, 92(1), 182–192. doi: 10.1007/s11524-014-9921-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang M, Manning D, van d. B., & Operario D. (2015). Stigmatization and mental health in a diverse sample of transgender women. LGBT Health, 2(4), 306–312. doi: 10.1089/lgbt.2014.0106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. (1990). Psychometric characteristics of the multidimensional scale of perceived social support. Journal of Personality Assessment, 55(3–4), 610–7. [DOI] [PubMed] [Google Scholar]


