Nosocomial deep wound infections are serious complications after orthopedic surgery. Extended postoperative antibiotic treatment leads to a statistically significant and clinically meaningful reduction of surgical site infection [1]. However, antibiotics such as carbapenems, cephalosporins, and fluoroquinolones can disturb gastrointestinal microbiota, which may lead to reduced resistance to pathogens such as Clostridioides difficile (Clostridium difficile) [2]. We had carried out postoperative prophylactic antibiotic treatment mainly with antibiotic-resistant enterococcal probiotics (R-EP). However, we recently found in a case-control study that combination probiotics may reduce C. difficile infection (CDI) in hip surgery patients [3]. Since then, antibiotic prophylaxis after orthopedic surgery has been performed with combination probiotics including Enterococcus faecium 2×108 CFU/day, Bacillus mesentericus 1×107 CFU/day, and Clostridium butyricum 5×107 CFU/day. Thus, we compared CDI incidence in hip surgery patients aged over 75 years between before and after the introduction of combination probiotics. The diagnosis of CDI was confirmed by an enzyme-linked immunosorbent assay for glutamate dehydrogenase and C. difficile toxins A and B using frozen stool specimens for patients with antibiotic-associated diarrhea. The CDI incidence before the introduction of combination probiotics was 4.2 cases per 10 ,000 patient bed-days, which is as many as in EUCLID (the European, multicentre, prospective biannual point prevalence study of CDI in hospitalized patients with diarrhoea), which reported 7.0 cases per 10, 000 patient bed-days [4]. Surprisingly, the CDI incidence after the introduction of combination probiotics markedly decreased to 0.35 cases per 10 ,000 patient bed-days, while annual consumption of cefmetazole sodium, the main antibiotic agent for prophylaxis usage at our hospital, and the number of hip surgery patients aged over 75 years did not change when compared between before and after the initiation of combination probiotics (Fig. 1).
Fig. 1.
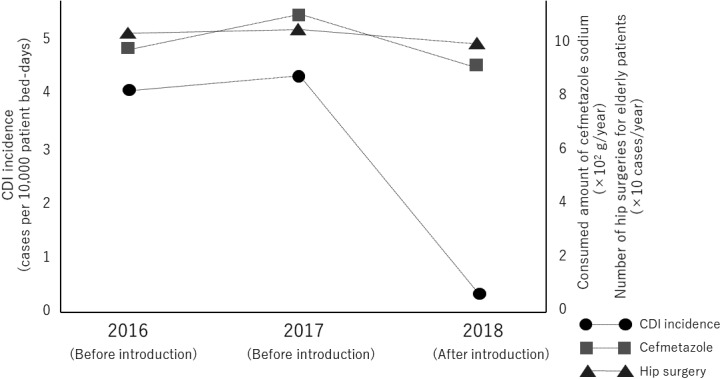
Annual CDI incidence before and after the introduction of combination probiotics.
When we administerd antibiotic prophylaxis with R-EP, CDI incidence was the same as in other developed countries. However, since combination probiotics were prescribed routinely, CDI incidence markedly decreased. Even though the data were observational and without a control group, the data may suggest that primary prevention of CDI with combination probiotics is achievable. In an in vivo study, R-EP should less viability and a weeker reduction of luminal pH than conventional enterococcal probiotics (C-EP) due to different utilization of carbohydrates [5]. Moreover, the survival rate of C. butyricum in the presence of antibiotic substances is very high because of its spore-forming effect. A recent experimental study using a new nonlethal diarrheal rat CDI model indicated that C. butyricum exerted a CDI-preventive effect due to suppression of toxin production or toxin activity [6].
In conclusion, the annual CDI incidence at our hospital markedly decreased after the introduction of combination probiotics including C-EP, B. mesentericus, and C. butyricum. CDI prevention among surgical patients is of extreme importance because antibiotic prophylaxis is usually provided after operations in Japan. The efficacy of probiotics for the prevention of CDI is highly controversial [7]. A consensus regarding which probiotic strains might prevent CDI has not been reached. Additional studies of sufficient size and with rigorous designs are needed to confirm which strains and combinations would be beneficial for the prevention of CDI.
DISCLOSURE STATEMENT
The author has no conflicts of interest relevant to the content of the article.
References
- 1.Yates AJ., JrAmerican Association of Hip and Knee Surgeons Evidence-Based Medicine Committee.2018. Postoperative prophylactic antibiotics in total joint arthroplasty. Arthroplast Today 4: 130–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ohshima T, Osaki T, Yamamoto Y, Asai S, Miyachi H, Kamiya S. 2018. Evaluation of risk factors for Clostridium difficile infection based on immunochromatography testing and toxigenic culture assay. J Clin Microbiol 56: e00555-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nagamine T, Matsumoto Y, Nakamura M. 2019. Combination probiotics may prevent Clostridium difficile infection among elderly patients undergoing an orthopedic surgery. Biosci Microbiota Food Health 38: 31–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davies KA, Longshaw CM, Davis GL, Bouza E, Barbut F, Barna Z, Delmée M, Fitzpatrick F, Ivanova K, Kuijper E, Macovei IS, Mentula S, Mastrantonio P, von Müller L, Oleastro M, Petinaki E, Pituch H, Norén T, Nováková E, Nyč O, Rupnik M, Schmid D, Wilcox MH. 2014. Underdiagnosis of Clostridium difficile across Europe: the European, multicentre, prospective, biannual, point-prevalence study of Clostridium difficile infection in hospitalised patients with diarrhoea (EUCLID). Lancet Infect Dis 14: 1208–1219. [DOI] [PubMed] [Google Scholar]
- 5.Shimazaki Y, Hosoya K, Tago K, Seo G. 1993. Studies on microbiological characteristics in Enterococcus preparations. Jpn J Hosp Pharm 19: 295–302. [Google Scholar]
- 6.Oka K, Osaki T, Hanawa T, Kurata S, Sugiyama E, Takahashi M, Tanaka M, Taguchi H, Kamiya S. 2018. Establishment of an endogenous Clostridium difficile rat infection model and evaluation of the effects of Clostridium butyricum MIYAIRI 588 probiotic strain. Front Microbiol 9: 1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goldstein EJC, Johnson SJ, Maziade PJ, Evans CT, Sniffen JC, Millette M, McFarland LV. 2017. Probiotics and prevention of Clostridium difficile infection. Anaerobe 45: 114–119. [DOI] [PubMed] [Google Scholar]


