Abstract
Background:
Cardiopulmonary resuscitation (CPR) is initiated in hospitalized children with bradycardia and poor perfusion. However, their rate of progression to pulseless cardiac arrest despite CPR, and differences in survival compared with initially pulseless arrest are unknown. We examined the prevalence and predictors of survival of children who progress from bradycardia to pulseless in-hospital cardiac arrest despite CPR.
Methods:
Pediatric patients, aged >30 days and <18 years, who received CPR at hospitals participating in Get With The Guidelines-Resuscitation during 2000-2016 were included. Each CPR event was classified as bradycardia with pulse, bradycardia with subsequent pulselessness, and initial pulseless cardiac arrest. We assessed for risk-adjusted rates of survival to hospital discharge using multilevel Poisson regression models.
Results:
Overall, 5592 pediatric patients were treated with CPR, of whom 2799 (50.1%) received CPR for bradycardia with poor perfusion and 2793 (49.9%) for initial pulseless cardiac arrest. Among those with bradycardia, 869 (31.0%, or 15.5% of cohort) became pulseless after a median of 3 minutes of CPR (IQR 1, 9). Rates of survival to discharge were 70.0% (1351/1930) for bradycardia with pulse, 30.1% (262/869) for bradycardia progressing to pulselessness, and 37.5% (1046/2793) for initial pulseless cardiac arrest (P for difference across groups <.001). Children who became pulseless despite CPR for bradycardia had a 19% lower likelihood (RR 0.81 [95% CI: 0.70, 0.93]; P=0.004) of surviving to hospital discharge than those initially pulseless. Among children who progressed to pulselessness despite CPR for bradycardia, a longer interval between CPR and pulselessness was a predictor of lower survival (reference: <2 minutes, for 2-5 minutes: RR 0.54 [95% CI: 0.41, 0.70]; for >5 minutes: RR 0.41 [95% CI: 0.32, 0.53]).
Conclusions:
Among hospitalized children in whom CPR is initiated, half have bradycardia with poor perfusion at the initiation of chest compressions, and nearly one-third of these progress to pulseless in-hospital cardiac arrest despite CPR. Survival was significantly lower for children who progress to pulselessness despite CPR, compared to those who were initially pulseless. These findings suggest that pediatric patients who lose their pulse despite resuscitation attempts are at particularly high-risk and require a renewed focus on post-resuscitation care.
Keywords: PALS, pediatric critical care, bradycardia, resuscitation
Introduction
Nearly 6,000 children suffer an in-hospital cardiac arrest in the United States each year.1–3 Cardiac arrest in children is distinct from adult cardiac arrest.4 It more frequently occurs in the setting of respiratory insufficiency and is associated with higher survival.4–6
Bradycardia with poor perfusion in children often heralds imminent cardiovascular collapse and in some instances precedes a pulseless cardiac arrest event.5 Consequently, current pediatric resuscitation guidelines recommend initiation of cardiopulmonary resuscitation (CPR) for children with bradycardia and poor perfusion as for pulseless cardiac arrest.7 Some proceed to a pulseless cardiac arrest even after initiation of CPR. Most prior studies of in-hospital cardiac arrest in children have not differentiated between patients who were initially pulseless when CPR was initiated or became pulseless after CPR initiation, assuming a similar survival likelihood for those who were initially pulseless or who became pulseless during a resuscitation effort.8–10 If this assumption is incorrect, it would have implications for current hospital benchmarking efforts on risk-standardized survival for pediatric patients with pulseless in-hospital cardiac arrest, as well as analytical models for pediatric cardiac arrest research.
Accordingly, within a large national registry for in-hospital cardiac arrest, we examined the prevalence and survival outcomes of patients who progress from bradycardia with poor perfusion to pulselessness despite initiation of CPR. Moreover, predictors of survival to hospital discharge in this patient group, including time from CPR initiation to pulselessness, remain unknown but important to understand.
Methods
Data Source
We used data from the American Heart Association’s (AHA’s) Get With The Guidelines (GWTG)-Resuscitation registry, which is a quality improvement registry for in-hospital cardiac arrest in U.S. hospitals. For hospitals caring for children, GWTG-Resuscitation also collects data on all patients receiving CPR, which includes children with bradycardia with poor perfusion, in addition to pulseless cardiac arrest. Cases are identified by hospital research staff through multiple methods, including centralized collection of cardiac arrest flow sheets, reviews of hospital paging system logs, and routine checks of code carts and pharmacy tracer drug records.11 Standardized Utstein-style definitions are used for all patient variables and outcomes to facilitate uniform reporting across hospitals.12,13 The GWTG-resuscitation data are proprietary of the AHA and can be obtained from the AHA directly. However, they cannot be shared by the authors. The analytic methods and study materials will be made available to other researchers for purposes of reproducing the results or replicating the procedure upon request.
Study Population
All children (<18 years of age) who were treated with CPR for a pulseless cardiac arrest or bradycardia with poor perfusion between 2000 and 2016 within GWTG-Resuscitation were included in the study. For patients with multiple CPR events during the hospitalization, only the index event was included and all subsequent events requiring CPR were excluded. Newborns treated with CPR in the delivery room, neonates (<30 days), children treated with CPR in the setting of trauma or as hospital visitors, or those with a preceding out-of-hospital cardiac arrest were excluded. Patients with missing information on survival to discharge – the primary outcome of the study – were also excluded.
Study Variables and Outcomes
The primary exposure was the type of CPR event, which was categorized into three mutually exclusive groups – bradycardia requiring CPR without progression to pulselessness, bradycardia requiring CPR with subsequent progression to pulselessness, and initial pulselessness at the time of CPR initiation. A bradycardia event was included in the registry if a child had a slow heart rate for their age and had poor perfusion requiring chest compressions. Those who progressed to pulselessness within 120 minutes of initiation of CPR for bradycardia defined the group with subsequent pulselessness. Initial pulseless arrests were index pulseless cardiac arrest events with pulselessness at the time of initiation of chest compressions. The primary outcome was survival to hospital discharge.
For all included children, we collected information on their demographics (age group [<1 year, 1 year to 12 years, >12 years], sex, race) and cardiac arrest characteristics, including the nature of the event (either of three exposure groups), initial pulseless rhythm if ever pulseless (ventricular fibrillation [VF], pulseless ventricular tachycardia [VT], asystole, pulseless electrical activity [PEA], or unknown), location of arrest (intensive care unit [including post-anesthesia care unit and the operating room], emergency department, floor without telemetry, floor with telemetry, and other), time of day (day [7:00AM–10:59 PM] vs night [11:00 PM–6:59 AM]) and day of week (weekday [Monday 7 AM–Friday 10:59 PM] vs weekend [Friday 11 PM–Monday 6:59 AM]), and whether the event was witnessed, among others. We also assessed markers of their baseline health, including their presenting illness (medical cardiac, medical non-cardiac, surgical cardiac, or surgical non-cardiac), comorbid conditions, and the interventions in place at the time of CPR initiation, including mechanical ventilation, continuous intravenous vasopressors, and advanced monitoring devices (presence of electrocardiography, pulse oximetry, and/or apnea monitor). We collected information on the details of the CPR event, including the need for advanced airway, device confirmation of airway positioning, and the use of vasoactive medications (atropine, epinephrine, and others). Finally, among children with bradycardia and subsequent pulselessness, we determined the time from CPR initiation to the onset of pulselessness.
Statistical analysis
We identified the proportion of all CPR events within the three groups - bradycardia without pulselessness, bradycardia with subsequent pulseless arrest, and initial pulseless arrest. Baseline differences between these 3 patient groups were assessed using chi-square tests for categorical variables and analysis of variance for continuous variables.
Next, we assessed for differences in rates of survival to hospital discharge. To determine if children who become pulseless after initiation of CPR for bradycardia have similar or different survival than patients who are initially pulseless when CPR was initiated, we constructed a multilevel Poisson regression model that explicitly accounted for clustering of patients within hospitals by modeling site as a random effect. Additionally, this model adjusted for differences in patient demographics, comorbid conditions and interventions in place at the time of the arrest, including initial pulseless cardiac arrest rhythm. An interaction between initial vs. subsequent pulselessness and initial pulseless rhythm (shockable [VF or VT] vs. non-shockable [PEA or asystole]) was also evaluated. In similar fashion, we constructed additional models to compare survival rates between patients with bradycardia without pulselessness and the 2 pulseless groups.
To better understand whether duration of time from CPR initiation to onset of pulselessness was associated with survival to discharge among children with bradycardia with subsequent pulselessness after CPR initiation, we constructed another multilevel Poisson regression model within this patient group with time to pulselessness (categorized as <2, 2 to 5, and >5 minutes) as the exposure and survival to discharge as the outcome, adjusted for demographics (age and sex), initial pulseless rhythm (PEA, asystole, VF/VT), pre-existing conditions, and interventions in place at the time of pulselessness (use of mechanical ventilation or continuous intravenous vasopressors).
All analyses were performed using SAS 9.4 (Cary, North Carolina) and were evaluated at a 2-sided significance level of 0.05. The study was approved by the Institutional Review Board at the Mid-America Heart Institute, which waived the need for informed consent as the study used de-identified data.
Results
A total of 5592 pediatric in-hospital resuscitation events were included in the study cohort (Figure 1). Of these, half (50.1%, n =2799) had an initial rhythm of bradycardia with poor perfusion at the time of CPR initiation, and the remaining half (49.9%, n = 2793) were initial pulseless in-hospital cardiac arrests. Among those with bradycardia, 869 (31.0%, or 15.5% of total cohort) progressed to pulselessness after CPR initiation after a median of 3 minutes (IQR 1 to 9).
Figure 1. Study flowsheet.
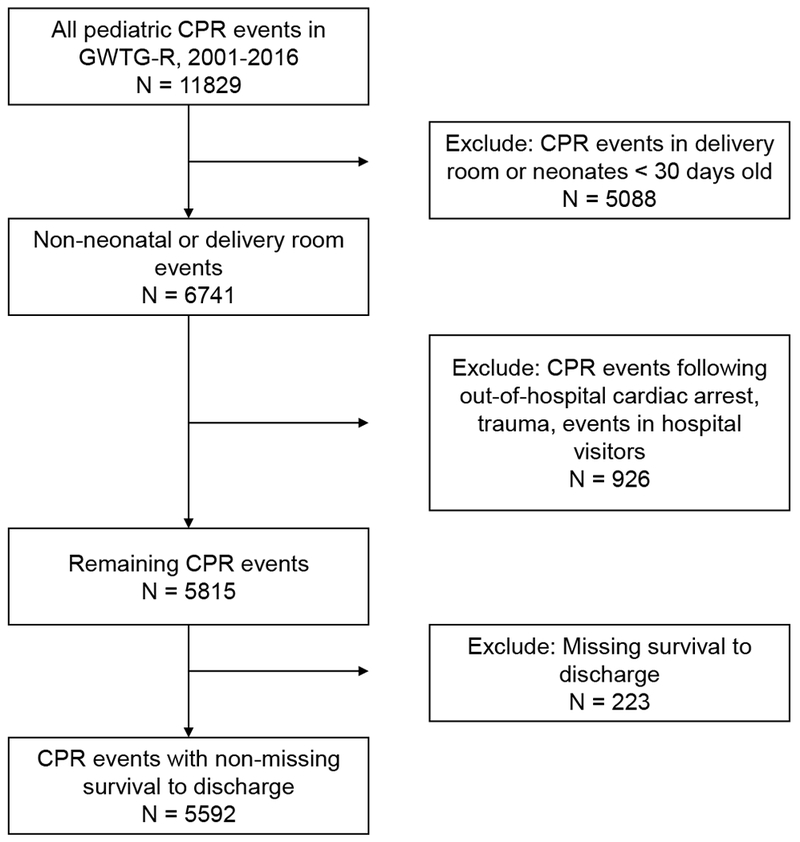
Abbreviations: CPR: cardiopulmonary resuscitation, GWTG-R: Get With The Guidelines - Resuscitation.
Patient and event characteristics
Of all events, the median age of children requiring resuscitation was 1 year (IQR, 4 months to 7 years) with 44.7% of children under 1 years of age, 41.3% between 1 to 12 years, and 14.0% over 12 years of age. More than half (54.9%) of those requiring resuscitation were female, and 53.5% and 25.3% were of white and black race, respectively (Table 1). There were notable differences in the age of children by CPR group, with a median age of 7 months among those with bradycardia without pulselessness, 1.1 years among those with bradycardia and subsequent pulselessness and 2.3 years for primary pulseless events (P<0.001). There were no sex or race differences by CPR group. Most of these events either occurred in patients who were undergoing cardiac monitoring or were witnessed by a healthcare provider (Table 2). Bradycardia events, both those with and without subsequent pulselessness, more frequently occurred in the ICU and in patients with mechanical ventilation as compared with patients with initial pulseless events. The first pulseless rhythm was either PEA or asystole in 85.6% of children and these rhythms were more common among those with bradycardia and subsequent pulselessness as compared with initial pulseless events (89.5% vs 84.5%, P <0.001) (see Table 2).
Table 1.
Characteristics of patients. Unless otherwise specified, values represent numbers with percentage in parentheses.
| Initially pulseless | Bradycardia with pulselessness | Bradycardia without pulselessness | Total | P-Value | |
|---|---|---|---|---|---|
| n = 2793 | n = 869 | n = 1930 | n = 5592 | ||
| Patient characteristics | |||||
| Median age (IQR), years | 2.3 (0.6, 11.0) | 1.1 (0.4, 6.0) | 0.6 (0.3, 2.0) | 1.0 (0.3, 7.0) | <0.001 |
| Age groups | <0.001 | ||||
| <1 year | 959 (34.3%) | 381 (43.8%) | 1160 (60.1%) | 2500 (44.7%) | |
| 1-12 years | 1272 (45.5%) | 382 (44.0%) | 655 (33.9%) | 2309 (41.3%) | |
| >12 years | 562 (20.1%) | 106 (12.2%) | 115 (6.0%) | 783 (14.0%) | |
| Female | 1249 (44.7%) | 403 (46.4%) | 871 (45.1%) | 2523 (45.1%) | 0.69 |
| Race | 0.08 | ||||
| White | 1522 (54.5%) | 448 (51.6%) | 1024 (53.1%) | 2994 (53.5%) | |
| Black | 706 (25.3%) | 215 (24.7%) | 491 (25.4%) | 1412 (25.3%) | |
| Other | 267 (9.6%) | 86 (9.9%) | 164 (8.5%) | 517 (9.2%) | |
| Unknown | 298 (10.7%) | 120 (13.8%) | 251 (13.0%) | 669 (12.0%) | |
| Illness category | <0.001 | ||||
| Medical, cardiac | 557 (20.0%) | 169 (19.5%) | 319 (16.5%) | 1045 (18.7%) | |
| Medical, non-cardiac | 1462 (52.4%) | 461 (53.1%) | 996 (51.6%) | 2919 (52.2%) | |
| Surgical, cardiac | 492 (17.6%) | 148 (17.1%) | 344 (17.8%) | 984 (17.6%) | |
| Surgical, noncardiac | 253 (9.1%) | 76 (8.8%) | 239 (12.4%) | 568 (10.2%) | |
| Other/missing | 29 (1.0%) | 15 (1.6%) | 32 (1.6%) | 76 (1.3%) | |
| Pre-existing conditions | |||||
| Heart failure prior to admission | 301 (10.8%) | 91 (10.5%) | 161 (8.3%) | 553 (9.9%) | 0.02 |
| Hypotension | 883 (31.6%) | 271 (31.2%) | 399 (20.7%) | 1553 (27.8%) | <0.001 |
| Respiratory insufficiency | 1580 (56.6%) | 548 (63.1%) | 1303 (67.5%) | 3431 (61.4%) | <0.001 |
| Renal insufficiency | 329 (11.8%) | 102 (11.7%) | 143 (7.4%) | 574 (10.3%) | <0.001 |
| Hepatic insufficiency | 141 (5.0%) | 52 (6.0%) | 93 (4.8%) | 286 (5.1%) | 0.42 |
| Metabolic or electrolyte abnormality | 480 (17.2%) | 150 (17.3%) | 200 (10.4%) | 830 (14.8%) | <0.001 |
| Diabetes mellitus | 54 (1.9%) | 14 (1.6%) | 9 (0.5%) | 77 (1.4%) | <0.001 |
| Baseline depression in CNS function | 492 (17.6%) | 135 (15.5%) | 277 (14.4%) | 904 (16.2%) | 0.009 |
| Pneumonia | 284 (10.2%) | 106 (12.2%) | 219 (11.3%) | 609 (10.9%) | 0.18 |
| Septicemia | 442 (15.8%) | 175 (20.1%) | 253 (13.1%) | 870 (15.6%) | <0.001 |
| Metastatic or hematologic malignancy | 218 (7.8%) | 64 (7.4%) | 61 (3.2%) | 343 (6.1%) | <0.001 |
| Interventions in place at time of arrest | |||||
| Mechanical ventilation* | 1575 (56.4%) | 546 (62.8%) | 1221 (63.3%) | 3342 (59.8%) | <0.001 |
| Vasopressor | 891 (31.9%) | 305 (35.1%) | 434 (22.5%) | 1630 (29.1%) | <0.001 |
| Cardiac monitoring | 2340 (83.8%) | 808 (93.0%) | 1775 (92.0%) | 4923 (88.0%) | <0.001 |
| Pulse oximetry | 2363 (84.6%) | 806 (92.8%) | 1799 (93.2%) | 4968 (88.8%) | <0.001 |
| Dialysis | 97 (3.5%) | 35 (4.0%) | 37 (1.9%) | 169 (3.0%) | 0.001 |
P-value is a global chi-squared goodness-of-fit test for categorical comparisons or the Kruskal Wallis test for the continuous variables. A P-value below 0.05 indicates that the distribution of a given variable was significantly different across the three groups.
An additional 358 patients had invasive airway without being reported as being on mechanical ventilation
Table 2.
Characteristics of events and their management. Unless otherwise specified, values represent numbers with percentage in parentheses.
| Initially pulseless | Bradycardia with pulselessness | Bradycardia without pulselessness | Total | P-Value | |
|---|---|---|---|---|---|
| n = 2793 | n = 869 | n = 1930 | n = 5592 | ||
| Rhythm in pulseless phase | <0.001 | ||||
| Asystole | 1092 (39.2%) | 387 (48.5%) | NA | 1479 (41.3%) | |
| Pulseless electrical activity | 1263 (45.3%) | 327 (41.0%) | NA | 1590 (44.4%) | |
| Ventricular fibrillation | 225 (8.1%) | 61 (7.6%) | NA | 286 (8.0%) | |
| Ventricular tachycardia | 207 (7.4%) | 23 (2.9%) | NA | 230 (6.4%) | |
| Missing/unknown | 6 | 71 | NA | 78 | |
| Location | <0.001 | ||||
| ICU | 1706 (62.8%) | 599 (73.3%) | 1244 (71.6%) | 3549 (67.4%) | |
| Monitored, non-ICU | 94 (3.5%) | 13 (1.6%) | 36 (2.1%) | 143 (2.7%) | |
| Non-Monitored, non-ICU | 203 (7.5%) | 36 (4.4%) | 111 (6.4%) | 350 (6.6%) | |
| ER | 415 (15.3%) | 83 (10.2%) | 88 (5.1%) | 586 (11.1%) | |
| Other | 297 (10.9%) | 86 (10.5%) | 258 (14.9%) | 641 (12.2%) | |
| Missing | 78 | 52 | 193 | 323 | |
| Arrest day/time | 0.66 | ||||
| Day | 1203 (50.8%) | 383 (52.3%) | 803 (52.3%) | 2389 (51.6%) | |
| Night | 377 (15.9%) | 110 (15.0%) | 226 (14.7%) | 713 (15.4%) | |
| Weekend | 786 (33.2%) | 240 (32.7%) | 506 (33.0%) | 1532 (33.1%) | |
| Arrest Management | |||||
| Monitored or Witnessed arrest | 2645 (94.7%) | 864 (99.4%) | 1912 (99.1%) | 5421 (96.9%) | <0.001 |
| AED used | 285 (10.2%) | 74 (8.5%) | 52 (2.7%) | 411 (7.4%) | <0.001 |
| Mechanical ventilation* | 2373 (85.0%) | 771 (88.7%) | 1412 (73.2%) | 4556 (81.5%) | <0.001 |
| Medications | |||||
| Atropine | 882 (31.6%) | 335 (38.6%) | 519 (26.9%) | 1736 (31.1%) | <0.001 |
| Epinephrine bolus | 2382 (87.3%) | 814 (95.2%) | 1153 (65.5%) | 4349 (81.4%) | <0.001 |
| Epinephrine, continuous | 185 (28.2%) | 87 (29.7%) | 96 (14.2%) | 368 (22.7%) | <0.001 |
| Vasopressin bolus | 130 (5.9%) | 49 (7.5%) | 16 (1.1%) | 195 (4.5%) | <0.001 |
| Vasopressin, continuous | 34 (6.0%) | 12 (4.6%) | 12 (2.0%) | 58 (4.1%) | 0.002 |
| Time to epinephrine, minutes (median, IQR) | 1.0 (0.0, 4.0) | 1.0 (0.0, 4.0) | 1.0 (0.0, 2.0) | 1.0 (0.0, 3.0) | <0.001 |
| Invasive airway established | 779/1044 (74.6%) | 214/254 (84.3%) | 325/592 (55.0%) | 1318/1890 (69.7%) | <0.001 |
| Time to establishing airway, minutes (median, IQR) | 6.0 (3.0, 11.0) | 6.0 (4.0, 10.5) | 7.0 (3.0, 13.0) | 6.0 (3.0, 11.0) | 0.08 |
| Duration of CPR | 13.0 (5.0, 31.0) | 20.0 (9.0, 41.0) | 4.0 (2.0, 13.0) | 14.0 (5.0, 33.0) | 0.22 |
P-value is a global chi-squared goodness-of-fit test for categorical comparisons or the Kruskal Wallis test for the continuous variables. A P-value below 0.05 indicates that the distribution of a given variable was significantly different across the three groups.
Abbreviations: AED, Automated external defibrillator; CPR. Cardiopulmonary resuscitation; CNS. Central nervous system; ICU, Intensive care unit; IQR, inter-quartile range
An additional 358 patients had invasive airway without being reported as being on mechanical ventilation
Care characteristics and patient survival
The treatment of these events varied substantially (Table 2). A majority of children (59.8%) were already on mechanical ventilation at the time of CPR initiation (Table 1). Of those without an invasive airway at the time of the arrest 69.8% were intubated within a median of 6 minutes (IQR, 3, 11), without significant differences in time to establishing an airway across the three groups (P = 0.08). There were no differences in rates of intravascular access at the time of the arrest across the two groups with bradycardia, regardless of subsequent pulselessness (91%), but this rate was modestly lower for those with initially pulseless arrest (87%, P<0.001). Medications received during resuscitation varied between groups - patients with bradycardia events that did not progress to pulselessness were less frequently treated with atropine than those progressing to pulselessness and primary pulseless arrests. Further, epinephrine was used in two thirds of bradycardia events that did not progress to pulselessness and nearly 90% of arrests with initial or subsequent pulselessness. The bradycardia group had a shorter time to the first epinephrine dose than both bradycardia and subsequent pulselessness as well initial pulseless arrests (Table 2).
Children with bradycardia without pulselessness had the highest unadjusted rate of survival to discharge (70.0%), which was approximately 2-fold higher than either pulseless group (30.2% for those with bradycardia progressing to pulselessness and 37.5% for initial pulseless in-hospital cardiac arrests, P<0.001) (Table 3). In adjusted models after accounting for differences in patient characteristics between CPR events, patients with bradycardia and subsequent pulselessness despite initiation of CPR were 19% less likely to survive to hospital discharge than those pulseless at the time of start of CPR (risk ratio [RR] 0.81; 95% CI: 0.70, 0.93; P = 0.004).
Table 3.
Survival to discharge, overall and by rhythm type. Values represents numbers with percentage in parentheses.
| Initial pulseless | Bradycardia with pulselessness | Bradycardia without pulselessness | |||||
|---|---|---|---|---|---|---|---|
| Total N | Survival, n (%) | Total N | Survival, n (%) | Total N | Survival, n (%) | P-value | |
| Overall | 2793 | 1046 (37.5%) | 869 | 262 (30.1%) | 1930 | 1351 (70.0) | <0.001 |
| PEA/asystole | 2355 | 849 (36.1%) | 714 | 224 (31.4%) | - | - | 0.02 |
| VF/VT | 432 | 195 (45.1%) | 84 | 17 (20.2%) | - | - | <0.001 |
Abbreviations: PEA, pulseless electrical activity; VF, ventricular fibrillation; VT, ventricular tachycardia
There were substantial differences based on initial pulseless rhythm. Patients with bradycardia and subsequent pulselessness due to PEA or asystole were 16% less likely to survive to discharge as compared with patients with an initial pulseless arrest due to these non-shockable rhythms (subsequent pulselessness, 31.4%; initially pulseless 36.1%; RR of 0.84; 95% CI 0.72, 0.98; P = 0.03). A similar pattern was observed for shockable rhythms of VF or VT (subsequent pulselessness, 20.2%; initially pulseless 45.1%; RR of 0.47; 95% CI 0.31, 0.71; P <0.001). Notably, for bradycardia events progressing to pulselessness, compared with initially pulseless cardiac arrest, differences in survival were larger for shockable vs non-shockable cardiac arrests (interaction P value of 0.008 in risk-adjusted analyses).
Comparing survival rates relative to patients without pulselessness, patients with bradycardia and subsequent pulselessness had a 57% lower risk-adjusted survival to discharge as compared with bradycardia events which never became pulseless (RR 0.43; 95% CI: 0.38, 0.50; P<0.001). Similarly, patients with initial pulseless cardiac arrest had a 47% lower risk-adjusted rate of survival to discharge compared with patients with bradycardia without pulselessness (RR: 0.53; 95% CI; 0.51, 0.56; P<0.001).
Time to pulselessness and survival
Among bradycardic events that transitioned to pulselessness despite resuscitation, there was a wide variation in the time interval between initiation of CPR and pulselessness (Supplemental Figure 1). Overall, among children who became pulseless following bradycardia with poor perfusion and initiation of CPR, 37.1% became pulseless within 2 minutes, 31.6% between 2 and 5 minutes, and 31.3% after 5 minutes of CPR initiation. This period of transition had prognostic implications, as a longer time from initiation of CPR to pulselessness was associated with a lower likelihood of survival to discharge. Nearly half of the children (47.0%) who became pulseless within 2 minutes from the onset of bradycardia and CPR initiation survived to discharge, compared with 25.2% (adjusted RR 0.53; 95% CI 0.40, 0.69; P<0.001) for those who became pulseless between 2 to 5 minutes of CPR initiation and 17.7% (adjusted RR 0.41; 95% CI 0.31, 0.53; P<0.001) for those who became pulseless after 5 minutes of CPR initiation (Table 4 and Figure 2). A similar relationship was observed for both PEA and asystole as first pulseless rhythms, with a progressive decrease in survival if pulselessness occurred beyond 2 minutes from initiation of CPR for bradycardia. For arrests with VF/VT as the first pulseless rhythm, the sample size was small, precluding a rhythm-specific assessment on risk-adjusted survival outcomes.
Table 4.
Survival to discharge in patients with bradycardia with subsequent pulselessness, by time to pulselessness. Values represents numbers with percentage in parentheses*
| <2 minutes | 2 to 5 minutes | >5 minutes | |||||
|---|---|---|---|---|---|---|---|
| Total N | Survival, n (%) | Total N | Survival, n (%) | Total N | Survival, n (%) | P-trend | |
| Overall | 262 | 123 (47.0%) | 242 | 61 (25.2%) | 265 | 47 (17.7%) | <0.001 |
| PEA/asystole | 233 | 114 (48.9%) | 199 | 48 (24.1%) | 197 | 33 (16.8%) | <0.001 |
| VF/VT | 10 | 1 (10.0%) | 22 | 5 (22.7%) | 40 | 10 (25.0%) | 0.36 |
Abbreviations: PEA, pulseless electrical activity; VF, ventricular fibrillation; VT, ventricular tachycardia
A total of 97 patients did not have time to pulselessness – 38 PEA, 47 asystole, 12 VF/VT
Figure 2. Time to pulselessness and survival to discharge.
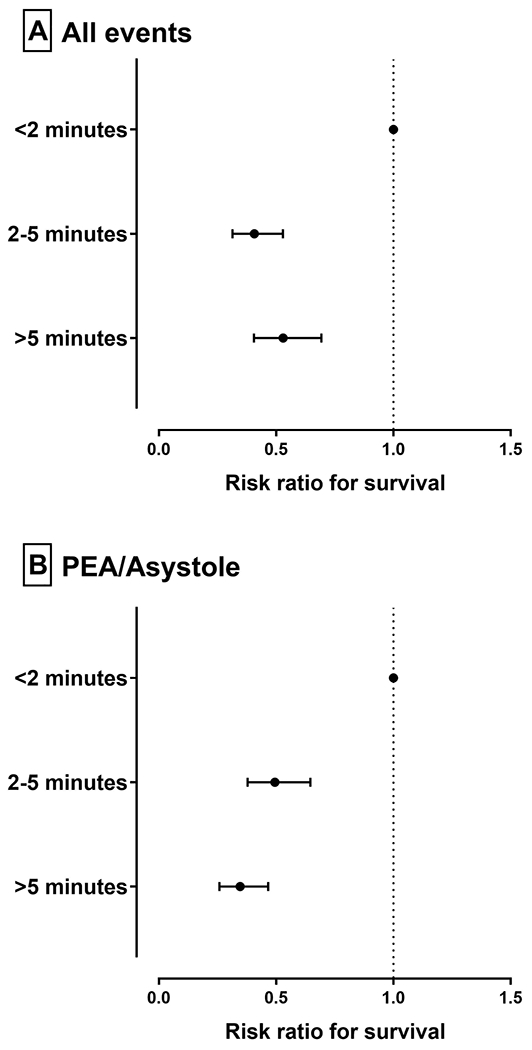
In bradycardia with subsequent pulselessness, risk-adjusted rates for survival to discharge were lower among those with time between cardiopulmonary resuscitation (CPR) imitation to pulselessness >2 minutes, for (A) all events, and for (B) events with subsequent non-shockable pulseless rhythms of pulseless electrical activity (PEA) and/or asystole.
Discussion
In a national registry of in-hospital cardiac arrest, nearly half of all pediatric resuscitation events were for bradycardia with poor perfusion, a third of which subsequently became pulseless despite CPR. Although children with pulseless events with antecedent bradycardia had generally similar patient and cardiac arrest characteristics as compared with those who were initially pulseless at the time of CPR initiation, they had a much lower likelihood of surviving to hospital discharge. Among children treated with CPR for bradycardia who then progress to pulselessness, the longer the time from initiation of CPR to pulselessness, the lower the likelihood of survival. Collectively, these findings provide novel insights about the epidemiology of children who are treated with CPR during in-hospital resuscitation, especially with regards to the prognosis of patients with bradycardia who subsequently become pulseless after initiation of CPR.
The present study adds to the literature on pediatric resuscitation in several important ways. Pediatric resuscitation guidelines recommend initiation of CPR, including chest compressions and vasoactive medications, for bradycardia with poor perfusion in children.7 Consequently, bradycardia and pulseless arrests are frequently studied together in pediatric cardiac arrest research, including the study of its epidemiology, treatment, and outcomes.8–10 In this study, we found that CPR initiated for bradycardia with poor perfusion and for pulselessness on initial presentation have significantly different survival outcomes, similar to a prior study.14 However, we also found that patients with bradycardia who progress to pulselessness had a lower likelihood of survival than initially pulseless patients, regardless of whether the initial pulseless rhythm was non-shockable (PEA and asystole) or shockable (VF/VT). Notably, the absolute magnitude of the survival difference was larger if the pulseless rhythm was shockable, consistent with data from adult cardiac arrest literature cardiac arrests due to VF and VT have higher survival.6, 15
Differential survival rates between the initially and subsequently pulseless groups have important implications for research studies on pediatric in-hospital cardiac arrest. It suggests that analyses should account for whether pediatric in-hospital cardiac arrest events were initially or subsequently pulseless with an indicator variable,16 and include an interaction term between this indicator variable and whether the pulseless rhythm was shockable or non-shockable. Moreover, ongoing efforts to recognize pediatric hospitals on survival outcomes for in-hospital cardiac arrest in quality improvement registries such as GWTG-Resuscitation may need to account for these factors in their calculations of risk-standardized survival rates for hospital benchmarking.
Further, we found that even the group that became pulseless after initiation of CPR for bradycardia is heterogeneous, and potentially not directly comparable to initial pulseless events, as the survival of children in this group is inversely associated with time to pulselessness. The mechanism for this observation is not known, but likely reflects a complex interplay between underlying physiology and adequacy of resuscitation efforts to restore perfusion. First, given the similarity of resuscitation efforts for pulseless arrests and bradycardia with early pulselessness, the high survival of those with early transition to pulselessness may reflect more appropriate resuscitation efforts, including timely, rhythm specific management. It is also conceivable that resuscitation measures applied for bradycardia, especially in those that transition to pulselessness after prolonged resuscitation, may not be optimal and the ischemic injury incurred during this period may be reflected in lower survival. Finally, those progressing to pulselessness despite prolonged resuscitative efforts may simply represent failure to rescue high-risk patients, suggesting a substantially higher mortality risk.
Nevertheless, the observation has important implications. Resuscitation care for bradycardia may warrant an assessment for quality of care delivered, particularly if hospitals have systems in place that actually respond to bradycardia events appropriately. This is important to address to ensure good outcomes through appropriate monitoring for signs of pulselessness among those with bradycardia, given the decrease in survival with pulselessness, particularly with the longer time to transition to pulselessness. Perhaps more importantly, these findings suggest that the first few minutes of CPR in patients with bradycardia and poor perfusion may be especially important for good outcomes, and that the quality of CPR during those first few minutes deserve special attention.
Our study’s findings should be interpreted in light of the following limitations. The higher survival rate for bradycardia without pulselessness may be, in part, due to a low threshold of starting CPR in children with poor perfusion. Nonetheless, CPR initiation is a guideline recommendation in children with bradycardia and poor perfusion. Further, the assessment of time to pulselessness is dependent on accurate reporting in patients and across hospitals. To the extent that time is inaccurately recorded, we would expect errors to be non-differential and to bias our analyses regarding time to pulselessness toward the null. Moreover, while we accounted for potential confounding by underlying severity of disease and used hierarchical models that accounted for patient clustering within hospitals, there is the possibility for residual confounding. We are unable to account for the timeliness of certain therapies, such as atropine, or the quality of respiratory support achieved in those with mechanical ventilation, which may reflect in differences in patient outcomes. Further, the duration of resuscitation for individual cases might vary based on the goals of care for each of the families of these patients. Finally, since the study only included events from hospitals that participated in GWTG-Resuscitation, our findings may not be generalizable to non-participating hospitals. However, it is unlikely that hospitals that do not participate in a quality improvement registry would systematically have different outcomes across these 3 patient groups.
Conclusion
Among non-neonatal pediatric patients in whom CPR is initiated, half have bradycardia with poor perfusion, and nearly one-third of these progress to in-hospital cardiac arrest despite CPR. Survival was lower for pediatric patients who subsequently became pulseless despite CPR as compared to those who were initially pulseless. These findings suggest that pediatric patients who lose their pulse despite resuscitation attempts are at particularly high-risk and require a renewed focus on post-resuscitation care.
Supplementary Material
Clinical Perspective.
What is new?
Among hospitalized children in whom cardiopulmonary resuscitation (CPR) is initiated, half have bradycardia with poor perfusion at the initiation of chest compressions, and nearly one-third of these progress to pulseless in-hospital cardiac arrest despite CPR.
Survival is significantly lower for children who progress to pulselessness despite CPR, compared to those who are initially pulseless.
What are the clinical implications?
In hospitalized pediatric patients, CPR for bradycardia with poor perfusion represents a large proportion of in-hospital resuscitation events.
Pediatric patients who lose their pulse despite resuscitation attempts are at particularly high-risk and require a renewed focus on post-resuscitation care.
Acknowledgments
Hospitals participating in the registry submit clinical information regarding the medical history, hospital care, and outcomes of consecutive patients hospitalized for cardiac arrest using an online, interactive case report form and Patient Management Tool™ (IQVIA, Parsippany, New Jersey). IQVIA serves as the data collection (through their Patient Management Tool – PMT™) and coordination center for Get With The Guidelines. The University of Pennsylvania serves as the data analytic center and has an agreement to prepare the data for research purposes. Members of the Get With The Guidelines Pediatric Resuscitation Task Force: Anne-Marie Guerguerian MD PhD FRCPC; Dianne Atkins MD; Elizabeth Foglia MD MSCE; Ericka Fink MD; Javier J. Lasa MD FAAP; Joan Roberts MD; Jordan Duval-Arnould MPH DrPH; Melanie Bembea MD MPH; Michael Gaies MD MPH MSc; Monica Kleinman MD; Punkaj Gupta MBBS; Robert Sutton MD MSCE; Taylor Sawyer DO Med
Sources of Funding
Dr. Khera (UL1TR001105) is supported by the National Center for Advancing Translational Sciences of the National Institutes of Health. Dr. Chan (R01HL123980) and Dr. Girotra (K08HL122527) are supported by funding from the National Heart Lung and Blood Institute. Neither funding agency had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Disclosures
Dr. Chan has served as a consultant for the American Heart Association. None of the other authors has any conflicts of interest or financial interests to disclose.
GWTG-Resuscitation is sponsored by the American Heart Association, which had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The manuscript is reviewed and approved by the GWTG-Resuscitation research and publications committee prior to journal submission.
References
- 1.Topjian AA, Berg RA and Nadkarni VM. Pediatric cardiopulmonary resuscitation: advances in science, techniques, and outcomes. Pediatrics. 2008;122:1086–1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berg MD, Nadkarni VM, Zuercher M and Berg RA. In-hospital pediatric cardiac arrest. Pediatr Clin North Am 2008;55:589–604, x. [DOI] [PubMed] [Google Scholar]
- 3.Morrison LJ, Neumar RW, Zimmerman JL, Link MS, Newby LK, McMullan PW Jr., Hoek TV, Halverson CC, Doering L, Peberdy MA, Edelson DP, American Heart Association Emergency Cardiovascular Care Committee CoCCCP, Resuscitation CoC, Stroke Nursing CoCC and Council on P. Strategies for improving survival after in-hospital cardiac arrest in the United States: 2013 consensus recommendations: a consensus statement from the American Heart Association. Circulation. 2013;127:1538–1563. [DOI] [PubMed] [Google Scholar]
- 4.Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, Mancini ME, Nichol G, Lane-Truitt T, Potts J, Omato JP, Berg RA and National Registry of Cardiopulmonary Resuscitation I. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295:50–57. [DOI] [PubMed] [Google Scholar]
- 5.de Caen AR, Berg MD, Chameides L, Gooden CK, Hickey RW, Scott HF, Sutton RM, Tijssen JA, Topjian A, van der Jagt EW, Schexnayder SM and Samson RA. Part 12: Pediatric Advanced Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132:S526–S542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Girotra S, Spertus JA, Li Y, Berg RA, Nadkarni VM, Chan PS and American Heart Association Get With the Guidelines-Resuscitation I. Survival trends in pediatric in-hospital cardiac arrests: an analysis from Get With the Guidelines-Resuscitation. Circ Cardiovasc Qual Outcomes. 2013;6:42–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kleinman ME, Chameides L, Schexnayder SM, Samson RA, Hazinski MF, Atkins DL, Berg MD, de Caen AR, Fink EL, Freid EB, Hickey RW, Marino BS, Nadkarni VM, Proctor LT, Qureshi FA, Sartorelli K, Topjian A, van der Jagt EW and Zaritsky AL. Part 14: pediatric advanced life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S876–S908. [DOI] [PubMed] [Google Scholar]
- 8.Andersen LW, Raymond TT, Berg RA, Nadkarni VM, Grossestreuer AV, Kurth T, Donnino MW and American Heart Association’s Get With The Guidelines-Resuscitation I. Association Between Tracheal Intubation During Pediatric In-Hospital Cardiac Arrest and Survival. JAMA. 2016;316:1786–1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sutton RM, Niles D, French B, Maltese MR, Leffelman J, Eilevstjonn J, Wolfe H, Nishisaki A, Meaney PA, Berg RA and Nadkarni VM. First quantitative analysis of cardiopulmonary resuscitation quality during in-hospital cardiac arrests of young children. Resuscitation. 2014;85:70–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lasa JJ, Rogers RS, Localio R, Shults J, Raymond T, Gaies M, Thiagarajan R, Laussen PC, Kilbaugh T, Berg RA, Nadkarni V and Topjian A. Extracorporeal Cardiopulmonary Resuscitation (E-CPR) During Pediatric In-Hospital Cardiopulmonary Arrest Is Associated With Improved Survival to Discharge: A Report from the American Heart Association’s Get With The Guidelines-Resuscitation (GWTG-R) Registry. Circulation. 2016;133:165–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, Berg RA, Nichol G and Lane-Trultt T. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. [DOI] [PubMed] [Google Scholar]
- 12.Cummins RO, Chamberlain D, Hazinski MF, Nadkarni V, Kloeck W, Kramer E, Becker L, Robertson C, Koster R, Zaritsky A, Bossaert L, Ornato JP, Callanan V, Allen M, Steen P, Connolly B, Sanders A, Idris A and Cobbe S. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital ‘Utstein style’. American Heart Association. Circulation. 1997;95:2213–2239. [DOI] [PubMed] [Google Scholar]
- 13.Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, Cassan P, Coovadia A, D’Este K, Finn J, Halperin H, Handley A, Herlitz J, Hickey R, Idris A, Kloeck W, Larkin GL, Mancini ME, Mason P, Mears G, Monsieurs K, Montgomery W, Morley P, Nichol G, Nolan J, Okada K, Perlman J, Shuster M, Steen PA, Sterz F, Tibballs J, Timerman S, Truitt T and Zideman D. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation. 2004;110:3385–3397. [DOI] [PubMed] [Google Scholar]
- 14.Donoghue A, Berg RA, Hazinski MF, Praestgaard AH, Roberts K, Nadkarni VM and American Heart Association National Registry of CPRI. Cardiopulmonary resuscitation for bradycardia with poor perfusion versus pulseless cardiac arrest. Pediatrics. 2009;124:1541–1548. [DOI] [PubMed] [Google Scholar]
- 15.Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS and American Heart Association Get with the Guidelines-Resuscitation I. Trends in survival after in-hospital cardiac arrest. N Engl J Med 2012;367:1912–1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jayaram N, Spertus JA, Nadkarni V, Berg RA, Tang F, Raymond T, Guerguerian AM, Chan PS and American Heart Association’s Get with the Guidelines-Resuscitation I. Hospital variation in survival after pediatric in-hospital cardiac arrest. Circ Cardiovasc Qual Outcomes. 2014;7:517–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


