Abstract
Objectives.
Frailty Phenotype (FP) has low sensitivity towards the identification of older people who will lose one or more activities of daily living (ADL). Nevertheless, the definition of disability in terms of ADLs may not resemble the pattern of functional impairment occurring during aging. The aim of this study was to examine the discriminative capacity of the Frailty Phenotype (FP) towards the identification of patterns of disabilities in an extended list of tasks, identified among community-dwelling older people.
Design.
Longitudinal cohort study.
Setting and Participants.
We included 997 subjects of 65 years and older selected from the InCHIANTI Study population.
Measures.
Using latent class analysis, we assessed the pattern of 3-year changes in twenty-four functional tasks. Then, we calculated the discriminative capacity of the FP for each pattern of disability. Analyses were stratified by gender.
Results.
In both men and women, we recognized three classes: stable function (SFC); disability in complex tasks (CDC); global functional disability (GDC). Among women, ability of FP to identify subjects in GDC showed sensitivity=0.42, specificity=0.98, positive and negative predictive values 0.75 and 0.91; the corresponding values for prediction of CDC were 0.13, 0.98, 0.68 and 0.75. Similar results were obtained among men.
Conclusions/Implications.
Over three years, older people of the InCHIANTI population remained largely functional stable, some persons developed deficiency in complex tasks, and a minority developed global functional disability. Trying to predict these three patterns may be useful for the care of older people in order to promote individualized interventions to reduce the burden of disabilities and their consequences. To this purpose, FP showed a fairly good capacity to identify people at risk of functional decline, but further studies are needed to identify instruments with better prognostic capacity.
Keywords: frailty, disability, physical performance
Brief summary:
Frailty Phenotype has a fairly good capacity to recognize patterns of disability among community-dwelling older people, but further studies are needed to identify instruments with better prognostic ability.
Introduction
Epidemiological studies have shown that the majority of older persons are disabled in the last years of life. 1 Older adults with disabilities have worse quality of life, are at higher risk of institutionalization, hospitalization, and mortality and require greater healthcare expenditure compared to their fit counterparts. 2–4 With the progressive increase in average life expectancy, preserving functional independence of older adults and/or compressing lifetime disability into a shorter period before death have become primary goals for geriatric medicine. To this purpose, early identification of older people at risk of functional disability is essential in order to recognize potential treatable conditions and carry out timely countermeasures.
In the last twenty years, the concept of frailty has gained importance as a state of increased vulnerability to stressors and susceptibility to adverse outcomes, such as disability, institutionalization and death. 5 Among the proposed operational definitions of frailty, the Frailty Phenotype (FP) is one of the most known and frequently used and it is based on the evaluation of five criteria (exhaustion, involuntary weight loss, poor handgrip strength, slow gait speed, inactivity). 6 The FP and other frailty definitions are strongly and independently associated with incident disability in epidemiological studies 6–9, but some papers have recently shown that the ability of current frailty instruments to discriminate people who will actually become disabled is poor. 10–12 This means that, among old people identified as frail according to the FP, only a small proportion will develop disability, therefore this instrument is of limited usefulness for screening purposes.
It should be noted that in the abovementioned studies, disability has been assessed through loss of one (or more) basic activities of daily living (defined as Katz ADL Index 13) or instrumental activities of daily living (Lawton IADL Scale14). We hypothesized that the concept of frailty may be able to catch a transition from an independent status to a pattern of functional limitations rather than predicting the development of disability in a default set of ADLs. During aging, the disablement process may differ among individuals, leading to a variable loss of functional abilities, ultimately affecting the capacity of living independently. The resulting pattern of functional limitations may not necessarily be caught by the inability in performing one specific task among ADLs or IADLs.
In this study, we aimed at verifying whether a number of classes, characterized by co-occurrence of incident impairments in an extended list of functional tasks (including not only basic ADLs, but also IADLs and mobility), can be identified in a population of community dwelling older people. Then, we measured discriminative capacity of FP towards the recognition of these disability classes.
Methods
Study population
We used data from people of 65 years and older participating in the “Invecchiare in Chianti” (InCHIANTI) study, 15 a population-based study designed to investigate the factors contributing to the decline of mobility in older persons. The participants in the study were randomly selected from the populations of two town areas in the Chianti region: Greve in Chianti and Bagno a Ripoli (Tuscany, Italy). The study protocol was approved by the Italian National Institute of Research and Care on Aging ethical committee. The eligible participants were interviewed at their homes by trained study researchers using a structured questionnaire aimed at investigating their health status, physical and cognitive performance, and other factors possibly related to loss of independence in late life. The interview was followed by a physical examination at the study clinic. The first wave of the study started in 1998 and participants were followed-up with evaluations every three years.
Measures of frailty and disability
At baseline, frailty was defined using adapted Fried et al.’s criteria. 6 Unintentional weight loss was defined as a reduction in weight >4.5 kilograms in the previous 12 months. Exhaustion was defined as a feeling of needing an effort to do everything and was considered present if the participant reported it for more than 3 or 4 days in the last week. Reduced physical activity was defined as having performed less than 2-4 hours of light exercise per week. Walking speed was evaluated over a 15 feet course with the patient taking two walks at usual pace. The mean of the two walks was considered, and those with a walking speed below the lowest quintile as adjusted for sex and height were considered slow walkers. Finally, grip strength was measured for the dominant limb using a hand-held dynamometer. The average of two measurements was used, and those with a grip strength below the sex and BMI (quartiles) specific 20th percentile was considered to have low grip strength. Subjects were then identified as “robust” when none of the criteria was present, “pre-frail” in the case of one or two indicators, “frail” when three or more criteria were present.
At 3-year follow up, data about the capacities in an extended list of 24 functional tasks were collected through interviews. The tasks were derived from the items used to assess disability in a subanalysis of the Cardiovascular Health Study16 combined with those used in the European Longitudinal Study on Aging 17. Then, we completed the list adding the missing Katz’s ADL (urine and fecal continence) 13 and the three remaining Lawton’s IADL (doing the laundry, using public transportation, taking medications correctly).14 Disability in each task was considered present when a person was unable of doing the task or if he/she required another person’s help.
Sample selection
From the original study population we selected participants with age ≥ 65 years (N: 1155). Thereafter, we excluded participants with any missing data for the functional tasks (N: 158), leaving 997 participants available for analysis. The excluded subjects were slightly older (mean age 77.8 years vs. 75.1 years) and with a higher prevalence of women (66% vs. 55%) but with the same proportion of frail subjects (10% vs. 11%) in comparison with the selected participants.
Analytic approach
Using latent class analysis (LCA), we assessed whether incident or worsening disability in the individual 24 tasks aggregates into classes. LCA is a technique used to classify individuals into mutually exclusive types, or latent classes, based on their pattern of response on a set of categorical variables. We used this method to test our study hypothesis that the InCHIANTI population comprises a number of subpopulations (classes) characterized by co-occurrence of impairments in the examined 24 functional tasks. Considering that trajectories and burden of disabilities differ between men and women,18 we stratified the analyses by gender. We evaluated the number of latent classes needed by comparing goodness-of-fit of models with different number of classes, using Bayesian Information Criterion (BIC). Once obtained the classes, we measured discriminative capacity of the FP for each pattern of worsening disability, over a 3-year follow-up, by calculating contingency tables to obtain sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV). We also compared this discriminative capacity with that of FP for prediction of loss of at least one Katz’s ADL.
All the analyses were performed using R 3.3 for Linux (R Foundation for Statistical Computing, Vienna, Austria).
Results
The cohort included 997 subjects, 550 women (mean age 75.7 years) and 447 men (mean age 74.3 years). Baseline characteristics are summarized in Table 1. According to FP, 69 women and 40 men were frail at baseline. Women had a greater prevalence of impairment in the 24 functional tasks when compared to men, especially regarding some abilities such as walking 400 mt, doing heavy houseworks, cutting toenails, carrying a shopping bag and using public transportation. We included in the LCA 857 people who were alive and completed functional evaluation at 3-year follow-up (mean age: 73.8 years, 56% women). Both in men and women subgroups, the evaluation of BIC showed an improvement of goodness of fit with increasing number of classes up to three and only marginal improvement thereafter. Accordingly, we chose a three classes model. LCA was stratified according to sex and the three latent classes are represented in Figure 1. The first one (SFC, stable function class) was characterized by substantially preserved ability in all the examined tasks; in this class only 28% of women and 14% of men reported difficulty in cutting toenails. The second class (CDC, disability in complex activities) showed, in both genders, a prevalence of 50% and higher of some incident or worsening disabilities (difficulty in climbing stairs, walking 400mt, doing heavy housework, cutting toenails, carrying shopping bags) and, in men, a prevalence of 51% of inability in bathing. The third class (GDC, global functional disability) grouped persons with difficulties in the majority of the 24 tasks in both sexes. SFC grouped 80% of men and 62% of women, CDC included 16% of men and 26% of women, and the corresponding values for GDC were 4% and 12%. CDC and GDC comprised participants who were older and with a higher prevalence of FP, compared to people included in SFC. Table 2 summarizes the prevalence of disabilities according to each class.
Table 1.
Baseline characteristics of the entire cohort according to sex.
| Women | Men | |
|---|---|---|
| N | 550 | 447 |
| Age, mean (SD) | 75.7 (7.8) | 74.3 (7) |
| Frail (FP), % | 12.6 | 9 |
| Indoor mobility, % | 5.6 | 4.7 |
| Outdoor mobility, % | 11.5 | 6.7 |
| Using stairs, % | 10.7 | 6.9 |
| Walking 400mt, % | 14.6 | 8.5 |
| Daily shopping, % | 16.9 | 10.6 |
| Washing face and arms, % | 5.1 | 3.6 |
| Bathing, % | 16.2 | 12.3 |
| Dressing, % | 8.7 | 7.6 |
| Eating, % | 3.3 | 3.1 |
| Cooking a simple meal, % | 10.7 | 9.5 |
| Using the toilet, % | 6.2 | 5.1 |
| Getting in and out of bed, % | 6.2 | 6 |
| Doing light housework, % | 10.9 | 11.3 |
| Doing heavy housework, % | 24.5 | 15.2 |
| Cutting toenails, % | 28.2 | 15.9 |
| Raising arms up over head, % | 3.5 | 3.4 |
| Using fingers to grasp or handle, % | 9.6 | 4.9 |
| Carrying a shopping bag, % | 22.4 | 10.7 |
| Urine and fecal continence, % | 7.3 | 4 |
| Using the telephone, % | 9.1 | 6.7 |
| Doing the laundry, % | 13.7 | 11.8 |
| Using public transportation, % | 25.5 | 12.9 |
| Taking medications correctly, % | 9.3 | 7.6 |
| Managing home finances, % | 16.9 | 12 |
Figure 1.
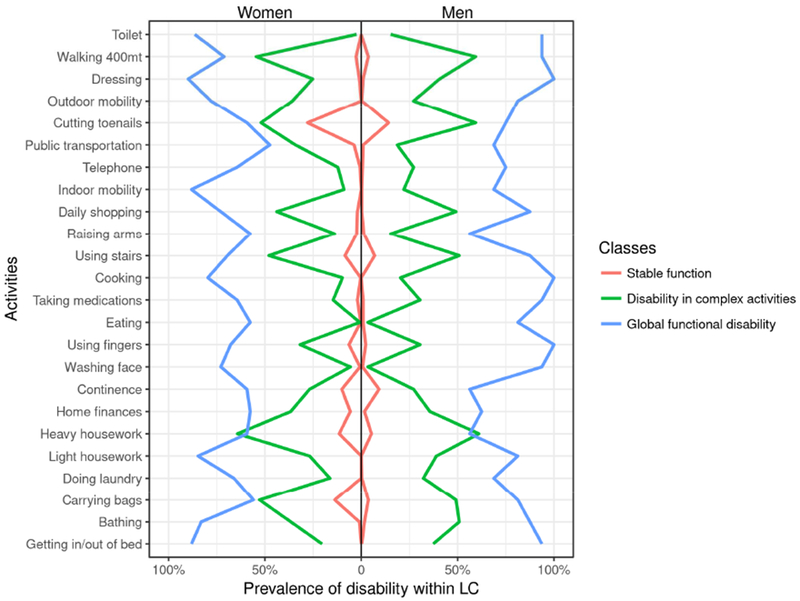
Proportion of disability in each functional task, in women and men, according to the classes obtained by latent class analysis.
The lines represent the proportion of people developing individual disabilities within each latent class. LC: latent class
Table 2.
Prevalence of baseline frailty (according to Frailty Phenotype) and 3-year-follow-up inability in doing activities of daily living according to the three classes obtained by the latent class analysis.
| SFC | CDC | GDC | ||||
|---|---|---|---|---|---|---|
| Women | Men | Women | Men | Women | Men | |
| N | 297 | 303 | 123 | 59 | 59 | 16 |
| Age at baseline, mean, SD | 72.1 (5.5) | 71.9 (5.4) | 75.7 (6.7) | 76.6 (7.2) | 82.7 (6.5) | 80.2 (7) |
| Frailty (FP) at baseline, N (%) | 6(2) | 3(1) | 17(14) | 12(20) | 25(42) | 7(46) |
| At least one ADL lost at baseline, N (%) | 17 (5.7) | 6(2) | 2(2.3) | 8(13.5) | 12(20.3) | 4(25) |
| Indoor mobility, N (%) | 0 | 0 | 11(9) | 13(22) | 51(88) | 11(69) |
| Outdoor mobility, N (%) | 0 | 0 | 44(36) | 16(27) | 46(78) | 13(81) |
| Using stairs, N (%) | 23(8) | 21(7) | 59(48) | 30(51) | 41(69) | 14(88) |
| Walking 400mt, N (%) | 9(3) | 12(4) | 66(54) | 35(59) | 42(71) | 15(94) |
| Daily shopping, N (%) | 6(2) | 0 | 54(44) | 29(49) | 43(73) | 14(88) |
| Washing face and arms, N (%) | 3(1) | 3(1) | 7(6) | 2(3) | 43(73) | 15(94) |
| Bathing, N (%) | 3(1) | 6(2) | 45(37) | 30(51) | 49(83) | 14(88) |
| Dressing, N (%) | 3(1) | 3(1) | 30(25) | 24(41) | 53(90) | 16(100) |
| Eating, N (%) | 0 | 3(1) | 1(1) | 2(3) | 34(58) | 13(81) |
| Cooking, N (%) | 0 | 0 | 12(10) | 12(20) | 47(80) | 16(100) |
| Using the toilet, N (%) | 0 | 0 | 2(2) | 8(15) | 51(86) | 15(94) |
| Getting in and out of bed, N (%) | 0 | 0 | 25(20) | 22(37) | 52(88) | 15(94) |
| Doing light housework, N (%) | 0 | 0 | 33(27) | 23(39) | 50(85) | 13(81) |
| Doing heavy housework, N (%) | 32(11) | 15(5) | 79(64) | 36(61) | 35(59) | 9(56) |
| Cutting toenails, N (%) | 83(28) | 42(14) | 64(52) | 35(59) | 35(59) | 12(75) |
| Raising arms over head, N (%) | 6(2) | 3(1) | 17(14) | 8(15) | 34(58) | 9(56) |
| Using fingers to handle, N (%) | 17(6) | 6(2) | 39(32) | 18(31) | 40(68) | 16(100) |
| Carrying shopping bags, N (%) | 41(14) | 12(4) | 65(53) | 29(49) | 33(56) | 13(81) |
| Urine and fecal continence, N (%) | 30(10) | 27(9) | 33(27) | 16(27) | 35(59) | 9(56) |
| Using the telephone, N (%) | 3(1) | 3(1) | 15(12) | 16(27) | 38(64) | 12(75) |
| Doing the laundry, N (%) | 0 | 0 | 19(16) | 19(32) | 39(66) | 11(69) |
| Using public transportation, N (%) | 12(4) | 3(1) | 42(34) | 11(19) | 28(47) | 11(69) |
| Taking medications, N (%) | 6(2) | 3(1) | 18(15) | 18(31) | 38(64) | 15(94) |
| Managing home finances, N (%) | 18(6) | 6(2) | 45(37) | 21(36) | 34(58) | 10(62) |
SFC: stable function; CDC: disability in complex activities; GDC: global functional disability; FP: Frailty Phenotype (frailty is defined as the presence of at least three of five criteria); ADL: activities of daily living
The interplay among FP, disability classes and death is shown in Table 3. Of the robust women, 78.3% were included in SFC, 15.3% in CDC, 3.2% in GDC and 3.2% died. Only 25% of frail women at baseline were included in GDC and 34.2% died before the 3-year follow-up. Similar results were obtained among men (Table 3).
Table 3.
Percentage distribution of the three latent classes and death according to Frailty Phenotype and sex.
| ROBUST | PRE-FRAIL | FRAIL | ||||
|---|---|---|---|---|---|---|
| Women % | Men % | Women % | Men % | Women % | Men % | |
| SFC | 78.3 | 90 | 50 | 56.3 | 15.8 | 20.3 |
| CDC | 15.3 | 5.2 | 28.3 | 22.6 | 25 | 20.3 |
| GDC | 3.2 | 0.9 | 10.6 | 3.5 | 25 | 12.1 |
| Death | 3.2 | 3.9 | 11.1 | 17.6 | 34.2 | 47.3 |
SFC: stable function class; CDC: disability in complex activities; GDC: global functional disability
Then, we analyzed the discriminative capacity of the FP with respect to identification of longitudinal changes in disability. In women, FP showed sensitivity=0.13, specificity=0.98, PPV=0.68, NPV=0.75 to identify CDC. Similarly, concerning the capacity to predict GDC, FP had sensitivity=0.42, specificity=0.98, PPV=0.75, NPV=0.91. The corresponding values for the prediction of loss of at least one Katz’s ADL were sensitivity=0.44, specificity=0.94, PPV=0.44, NPV=0.94. We found similar results among men (Table 4).
Table 4.
Predictive capacity of frailty for the identification of classes of disability in complex activities (CDC) and global functional disability (GDC) and for loss of at least one Katz’s activities of daily living (ADL) at three-year follow-up.
| Sensitivity | Specificity | PPV | NPV | |
|---|---|---|---|---|
| Women | ||||
| CDC | 0.13 | 0.98 | 0.68 | 0.75 |
| GDC | 0.42 | 0.98 | 0.75 | 0.91 |
| Loss of one Katz’s ADL | 0.44 | 0.94 | 0.44 | 0.94 |
| Men | ||||
| CDC | 0.20 | 0.99 | 0.73 | 0.87 |
| GDC | 0.46 | 0.99 | 0.60 | 0.98 |
| Loss of one Katz’s ADL | 0.28 | 0.95 | 0.33 | 0.95 |
Frailty was defined as the presence of at least three criteria of the Frailty Phenotype CDC: disability in complex activities; GDC: global functional disability; PPV: positive predictive value; NPV: negative predictive value.
Discussion
According to the results of our study, community dwelling older persons participating in the InCHIANTI Study showed three patterns of functional decline after a three-year follow-up: most subjects remained functionally stable (SFC), some persons developed deficiency in more complex tasks (CDC), and a minority developed global functional disability (GDC). The ability of FP to predict development of CDC and GDC showed high specificity and NPV, as expected, but also a fairly good PPV, especially when compared to the prediction of loss of at least one Katz’s ADL.
Despite many differences concerning population sampling, definition of disability and methodological aspects, our data resemble those reported by Yu and colleagues 19 who identified three distinct ADL and IADL disability trajectories among 3186 older adults in Taiwan based on a 11-year follow-up survey: maintained function, progressive disability and consistent disability. Differently from these authors, our aim was not analyzing the trajectories of individual disabilities or synergy scores over a timeframe but verifying if the FP was able to predict the pattern of functional loss defined by LCA. The fact that we described three patterns of disabilities similar to those identified by Yu and colleagues reinforces our findings and makes them generalizable. Prediction of these three patterns may help promoting individualized interventions to reduce the burden of disabilities and their consequences. For example, in subjects belonging to SFC, fostering the involvement in physical and social activities may help maintaining a good performance status as long as possible; for older people in the GDC, the use of assistive devices can be an important strategy to preserve residual independence and prevent further deterioration; for older adults belonging to CDC, early interventions and management of chronic diseases may prevent the entrance in a spiral of rapid functional decline.
At 3-year follow-up, prevalence of CDC and GDC was higher among women than men. This finding is in line with that previously reported in several population-based studies, which found that women had a higher incidence of ADL disability compared to men. 20–23 In the Framingham Heart Study, women reported greater functional limitation and physical disability than men on each of three different self-report measures of physical functioning. 24 Nevertheless, recent data reported that, when adjusting for socioeconomic, health, and social relations indicators, incidence of functional disability was similar between genders. 25,26 Moreover, gender differences in disability trajectories may be explained in part by higher initial levels of disability among older women,27 as observed also in our cohort (Table 1).
Our study shed light on the capacity of FP to predict the pattern of worsening disability. When looking at the percentage distribution of robust, pre-frail and frail people across the three latent classes (Table 2), the FP identifies well people belonging to the SFC (78.3% of fit women and 90% of fit men are included in SFC), but frail persons have the same probability to be included in the three classes. When analyzing the predictive ability of the FP for the identification of CDC and GDC, we obtained a high NPV (range of values from .75 to .98) and a modestly good PPV (range of values from .60 to .75). Our findings strengthen the previously reported data about the high specificity and NPV of FP towards loss of ADLs. 10,11,28,29 Nevertheless, the PPV we found for the prediction of CDC and GDC is rather better than the corresponding value for the loss of one Katz’s ADL (PPV=.44 among women, .33 among men). Therefore, when considering as an outcome the pattern of disability in an extended list of tasks, the FP showed a quite good capacity to discriminate among people who remained functionally stable and those who developed dependency. More studies are needed to confirm these data and to further improve the discriminative capacity of frailty assessment instruments.
Our cohort is representative of the real world of old outpatients, since it derives from an over 65 community-dwelling Italian population. Moreover, we used an innovative approach to detect disability, including not only Katz’s ADL index, that has high floor and ceiling effects and therefore may show difficulty in identifying milder or earlier onset of disability.30
Despite these strengths, this study has some limitations. First, although the entire cohort is relatively large, the stratification of analyses according to gender and the low prevalence of frailty contributed to shrink the population at risk of developing the outcome, introducing a potential bias in our results. Second, since we studied only the FP, our results cannot be extended to other frailty indicators, despite the evidence from literature that predictive ability for ADL disability is similar for other current assessment instruments. 31 Third, we used self-reported measures of disability. Previous studies have noted discrepancies in ratings between self-reported and performance based functional measures. 32 However, the use of self-reported data is a common practice when investigating disabilities in older adults, since they are strongly associated with performance-based functional scores and more accurately reflect personal abilities for interacting with the real world. 33 Moreover, concerning discrepancy among men and women, two studies comparing self-reported function with observed performance found no gender differences in the reporting of disability. 34,35 Fourth, in our analysis we cannot exclude that functional decline is the result of major events (e.g. falls) rather than progressive aging. However, we can assume that as in other population-based studies, in our cohort FP was associated with functional deterioration irrespective of intercurrent events. Finally, since we analyzed data from a community in central Italy, our findings regarding disability patterns may not be translated to other communities. It should be noted, though, that the prevalence of baseline frailty was similar to the one reported in other large European and US population studies36,37.
Conclusions/Relevance
When considering as an outcome the pattern of disability in an extended list of tasks, instead of loss of one or more Katz’s ADL, the ability of the FP to identify people at risk of functional decline modestly improves. This study highlights the fact that the prognostic capacity of frailty assessment instruments depends also on the definition of the outcome. More research is encouraged in order to identify the best instrument for the prediction of future disability and to implement relative countermeasures.
Acknowledgments
The authors are particularly grateful to the InCHIANTI study members who contributed to data collection.
Sponsor’s role. “The InCHIANTI study was supported as a “targeted project” by the Italian Ministry of Health (ICS-110.1/RS97.71) and in part by the US National Institute on Aging (contracts N01-AG-919413 and N01-AG-821336; grants R01 AG027012 and R01 AG029148).
Funding sources: The InCHIANTI study baseline (1998 and 2000) was supported as a “targeted project” (ICS110.1/RF97.71) by the Italian Ministry of Health, and in part by the National Institute on Aging (Contracts: 263 MD 9164 and 263 MD 821336). The Follow-up 1 (2001 and 2003) was funded by the U.S. National Institute on Aging (Contracts: N.1AG-1-1 and N.1-AG-1-2111); the Follow-up 2 and 3 studies (2004 and 2010) were financed by the U.S. National Institute on Aging (Contract: N01-AG-5-0002). The study was also supported in part by the Intramural Research Program of the National Institute on Aging, National Institutes of Health, Baltimore, Maryland.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest.
Authors have no personal or financial conflicts of interest to declare.
References
- 1.Guralnik JM, LaCroix AZ, Branch LG, Kasl SV, Wallace RB. Morbidity and disability in older persons in the years prior to death. Am J Public Health. 1991;81:443–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luppa M, Luck T, Weyerer S, König H-H, Brähler E, Riedel-Heller SG. Prediction of institutionalization in the elderly. A systematic review. Age Ageing. 2010;39:31–8. [DOI] [PubMed] [Google Scholar]
- 3.Millán-Calenti JC, Tubío J, Pita-Fernández S, González-Abraldes I, Lorenzo T, Fernández-Arruty T, et al. Prevalence of functional disability in activities of daily living (ADL), instrumental activities of daily living (IADL) and associated factors, as predictors of morbidity and mortality. Arch Gerontol Geriatr. 2010;50:306–10. [DOI] [PubMed] [Google Scholar]
- 4.Fried TR, Bradley EH, Williams CS, Tinetti ME. Functional disability and health care expenditures for older persons. Arch Intern Med. 2001;161:2602–7. [DOI] [PubMed] [Google Scholar]
- 5.Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381:752–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–156. [DOI] [PubMed] [Google Scholar]
- 7.Ensrud KE, Ewing SK, Taylor BC, Fink HA, Cawthon PM, Stone KL, et al. Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Arch Intern Med. 2008;168:382–9. [DOI] [PubMed] [Google Scholar]
- 8.Bandeen-Roche K, Xue Q-L, Ferrucci L, Walston J, Guralnik JM, Chaves P, et al. Phenotype of frailty: characterization in the women’s health and aging studies. J Gerontol A Biol Sci Med Sci. 2006;61:262–6. [DOI] [PubMed] [Google Scholar]
- 9.Rockwood K, Howlett SE, MacKnight C, Beattie BL, Bergman H, Hébert R, et al. Prevalence, attributes, and outcomes of fitness and frailty in community-dwelling older adults: report from the Canadian study of health and aging. J Gerontol A Biol Sci Med Sci. 2004;59:1310–7. [DOI] [PubMed] [Google Scholar]
- 10.Pijpers E, Ferreira I, Stehouwer CDA, Nieuwenhuijzen Kruseman AC. The frailty dilemma. Review of the predictive accuracy of major frailty scores. Eur J Intern Med. 2012;23:118–23. [DOI] [PubMed] [Google Scholar]
- 11.Pedone C, Costanzo L, Cesari M, Bandinelli S, Ferrucci L, Antonelli Incalzi R. Are Performance Measures Necessary to Predict Loss of Independence in Elderly People? J Gerontol A Biol Sci Med Sci. 2016;71:84–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Costanzo L, Pedone C, Cesari M, Ferrucci L, Bandinelli S, Antonelli Incalzi R. Clusters of functional domains to identify older persons at risk of disability. Geriatr Gerontol Int. In Press; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. STUDIES OF ILLNESS IN THE AGED. THE INDEX OF ADL: A STANDARDIZED MEASURE OF BIOLOGICAL AND PSYCHOSOCIAL FUNCTION. JAMA. 1963;185:914–9. [DOI] [PubMed] [Google Scholar]
- 14.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–86. [PubMed] [Google Scholar]
- 15.Ferrucci L, Bandinelli S, Benvenuti E, Di Iorio A, Macchi C, Harris TB, et al. Subsystems contributing to the decline in ability to walk: bridging the gap between epidemiology and geriatric practice in the InCHIANTI study. J Am Geriatr Soc. 2000;48:1618–25. [DOI] [PubMed] [Google Scholar]
- 16.Fried LP, Ettinger WH, Lind B, Newman AB, Gardin J. Physical disability in older adults: a physiological approach. Cardiovascular Health Study Research Group. J Clin Epidemiol. 1994;47:747–60. [DOI] [PubMed] [Google Scholar]
- 17.Ferrucci L, Guralnik JM, Cecchi F, Marchionni N, Salani B, Kasper J, et al. Constant hierarchic patterns of physical functioning across seven populations in five countries. Gerontologist. 1998;38:286–94. [DOI] [PubMed] [Google Scholar]
- 18.Newman AB, Brach JS. Gender gap in longevity and disability in older persons. Epidemiol Rev. 2001;23:343–50. [DOI] [PubMed] [Google Scholar]
- 19.Yu H-W, Chen D-R, Chiang T-L, Tu Y-K, Chen Y-M. Disability trajectories and associated disablement process factors among older adults in Taiwan. Arch Gerontol Geriatr. 2015;60:272–80. [DOI] [PubMed] [Google Scholar]
- 20.Crimmins EM, Saito Y, Reynolds SL. Further evidence on recent trends in the prevalence and incidence of disability among older Americans from two sources: the LSOA and the NHIS. J Gerontol B Psychol Sci Soc Sci. 1997;52:S59–71. [DOI] [PubMed] [Google Scholar]
- 21.Dunlop DD, Hughes SL, Manheim LM. Disability in activities of daily living: patterns of change and a hierarchy of disability. Am J Public Health. 1997;87:378–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hardy SE, Allore HG, Guo Z, Gill TM. Explaining the effect of gender on functional transitions in older persons. Gerontology. 2008;54:79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beckett LA, Brock DB, Lemke JH, Mendes de Leon CF, Guralnik JM, Fillenbaum GG, et al. Analysis of change in self-reported physical function among older persons in four population studies. Am J Epidemiol. 1996;143:766–78. [DOI] [PubMed] [Google Scholar]
- 24.Murabito JM, Pencina MJ, Zhu L, Kelly-Hayes M, Shrader P, D’Agostino RB. Temporal trends in self-reported functional limitations and physical disability among the community-dwelling elderly population: the Framingham heart study. Am J Public Health. 2008;98:1256–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Louie GH, Ward MM. Sex disparities in self-reported physical functioning: true differences, reporting bias, or incomplete adjustment for confounding? J Am Geriatr Soc. 2010;58:1117–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rodrigues MAP, Facchini LA, Thumé E, Maia F. Gender and incidence of functional disability in the elderly: a systematic review. Cad Saude Publica. 2009;25 Suppl 3:S464–476. [DOI] [PubMed] [Google Scholar]
- 27.Gill TM, Gahbauer EA, Lin H, Han L, Allore HG. Comparisons between older men and women in the trajectory and burden of disability over the course of nearly 14 years. J Am Med Dir Assoc. 2013;14:280–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.García-García FJ, Carcaillon L, Fernandez-Tresguerres J, Alfaro A, Larrion JL, Castillo C, et al. A new operational definition of frailty: the frailty trait scale. J Am Med Dir Assoc. 2014;15:371.e7–371.e13. [DOI] [PubMed] [Google Scholar]
- 29.Daniels R, van Rossum E, Beurskens A, van den Heuvel W, de Witte L. The predictive validity of three self-report screening instruments for identifying frail older people in the community. BMC Public Health. 2012;12:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wade DT. Measurement in neurological rehabilitation. Curr Opin Neurol Neurosurg. 1992;5:682–6. [PubMed] [Google Scholar]
- 31.Forti P, Rietti E, Pisacane N, Olivelli V, Maltoni B, Ravaglia G. A comparison of frailty indexes for prediction of adverse health outcomes in an elderly cohort. Arch Gerontol Geriatr. 2012;54:16–20. [DOI] [PubMed] [Google Scholar]
- 32.Smith KV, Goldman N. Measuring health status: self-, interviewer, and physician reports of overall health. J Aging Health. 2011;23:242–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van den Brink CL, Tijhuis M, Kalmijn S, Klazinga NS, Nissinen A, Giampaoli S, et al. Self-reported disability and its association with performance-based limitation in elderly men: a comparison of three European countries. J Am Geriatr Soc. 2003;51:782–8. [DOI] [PubMed] [Google Scholar]
- 34.Melzer D, Lan T-Y, Tom BDM, Deeg DJH, Guralnik JM. Variation in thresholds for reporting mobility disability between national population subgroups and studies. J Gerontol A Biol Sci Med Sci. 2004;59:1295–303. [DOI] [PubMed] [Google Scholar]
- 35.Merrill SS, Seeman TE, Kasl SV, Berkman LF. Gender differences in the comparison of self-reported disability and performance measures. J Gerontol A Biol Sci Med Sci. 1997;52:M19–26. [DOI] [PubMed] [Google Scholar]
- 36.O’Caoimh R, Galluzzo L, Rodríguez-Laso Á, Van der Heyden J, Ranhoff AH, Lamprini-Koula M, et al. Prevalence of frailty at population level in European ADVANTAGE Joint Action Member States: a systematic review and meta-analysis. Ann 1st Super Sanita. 2018;54:226–38. [DOI] [PubMed] [Google Scholar]
- 37.Bandeen-Roche K, Seplaki CL, Huang J, Buta B, Kalyani RR, Varadhan R, et al. Frailty in Older Adults: A Nationally Representative Profile in the United States. J Gerontol A Biol Sci Med Sci. 2015;70:1427–34. [DOI] [PMC free article] [PubMed] [Google Scholar]


