Abstract
Purpose
Corneal donation has not received adequate attention in Saudi Arabia, and donors are lacking. This study explores the underlying knowledge of, attitude regarding, and practice of corneal donation in Saudi Arabia, which will possibly help in designing healthcare policies and creating a national eye bank.
Methods
This observational cross-sectional study used a self-administered questionnaire and was administered to the residents of Saudi Arabia from August to December 2017. We surveyed 1292 random subjects who agreed to fill out the self-administered questionnaire. The sample included Saudi and non-Saudi residents across adult age groups from medical and non-medical professions.
Results
Of the 1292 respondents, only 4.3% believed that they had sufficient knowledge about corneal donation; 66.3% of the sample had not decided whether to donate their corneas after death; 40.2% stated that they would be more willing to donate if they had sufficient knowledge about corneal donation; and 46.1% of the population did not know where to apply to donate their corneas. Those who believed that they had sufficient information about corneal donation were significantly more likely to donate (p < 0.001) than those who believed they did not have enough information.
Conclusion
Increased awareness about corneal donation is required, as a higher level of awareness was associated with a higher willingness to donate corneas. Establishing healthcare policies and creating community campaigns is necessary to increase corneal donation awareness and willingness.
Keywords: Donation, Transplant, Cornea, Blindness, Eye surgery, Awareness
Introduction
The cornea, the transparent layer forming the front of the eye, covers the iris and the pupil and allows light to enter the eye.1 This transparent tissue plays a critical role in vision as it is the main refractive surface that transmits light into the retina. Multiple causes can lead to loss of function. In fact, loss of corneal transparency is one of the main causes of blindness worldwide.1 Globally, approximately 4.9 million individuals have bilateral corneal blindness, while 23 million are unilaterally blind.1 This leads to a significant health burden and reduction in quality of life.2
The burden of corneal diseases (such as keratoconus and bullous keratopathy) in Saudi Arabia is a major concern. In Asir province alone, a young population (aged 8–28 years) was found to have early-onset keratoconus with quick progression to the severe stage of the condition with estimated incident of 20 new cases per 100,000 population.3 Fortunately, corneal blindness is fully reversible with a corneal transplant.[4], [5] Corneal transplant is the most frequently performed transplant surgery worldwide [1], [4], [6], [7], [8] and the most successful human organ transplant type.[7], [8], [1]
Unfortunately, it is becoming increasingly difficult for eye banks worldwide to meet the growing demand for transplantable corneal tissue.1 Rates of corneal donation are much lower than those of solid organs are, suggesting that there is something different in the views of corneal donation.9 Corneal donation represents a rising global concern, a recent survey of eye banking and corneal transplantation worldwide indicated the presence of only 1 cornea available for every 70 needed.10
The situation of eye banking and corneal donation in the Middle East varies. In Iran, there are 68 cornea transplant units across the country.11 An eye bank there is capable of offering a transplantable graft within 2 days in emergency cases and considered a nonprofit nongovernmental organization.12 In Turkey, there is a shortage of corneal tissue since the number of recipients is higher than the number of donors.13 Moreover, in Yemen, there are no eye banks, and the waiting list of patients needing corneal grafts is long.14
When it comes to local eye banks, despite the presence of many cornea transplant centers, the possibility of accepting local donors’ corneas is almost nonexistent since the only way to get corneal grafts is through importing them from abroad. In the last 10 years around 16,800 corneas has been imported to King Khaled Eye Specialist Hospital alone, with rough estimated cost to be 179.760 million Saudi Riyals. (Unpublished data)
Understanding the underlying facts about the knowledge of, attitudes toward, and practice of corneal donation in Saudi Arabia is necessary, as it could be the first step in creating a national eye bank that accepts local grafts and acts as a base for further research. Moreover, it could help with the planning of awareness programs and serve as an educational tool.
Very few local studies have discussed this issue, however it was either narrowed to one geographic region[15], [16] or restricted to a limited group of the society.16
Hence their results cannot be generalized, therefore more representative and larger sample should be explored. This study will fill an important gap in the literature, which has local priority since majority of corneal transplants in Saudi Arabia are performed using imported corneas. The main purpose of this study is to create a reference point for use in future assessments and measure the effectiveness of health education activities in changing the behaviors. It also aims to identify the barriers and motivations for corneal donation in Saudi Arabia with the objective of increasing the number of local donors.
Materials and Methods
Participants and data collection
This observational cross-sectional study used a secondary data collection method using a self-administered questionnaire distributed to residents of Saudi Arabia. The data were collected from August to December 2017 using a simple random sampling technique. The study targeted residents of the five geographic regions of Saudi Arabia (Northern, Southern, Eastern, Western, and Central).
We surveyed 1292 random subjects who agreed to fill out the self-administered questionnaire and were able to read and understand Arabic. Participants who were unable to read Arabic were excluded. The sample included Saudi and non-Saudi residents across two age groups (i.e. 15–30 years and >30 years) in medical and non-medical professions.
The study’s sample size was calculated using the following formula for simple random sampling (proportion formula used for prevalence if the population is >20,000):
.
where:
n = sample size
(z) is the normal distribution value (1.96) with a 95% confidence and 5% error (two-sided 95% confidence interval = 1.96)
(p) is the expected percentage for knowledge
= precision (5%)n = (Z^2*P(1 − P))/d^2 = 385
(d) is delta, the error tolerance around the estimation.
The sample size required = 385 subjects.
Data management
Study instruments
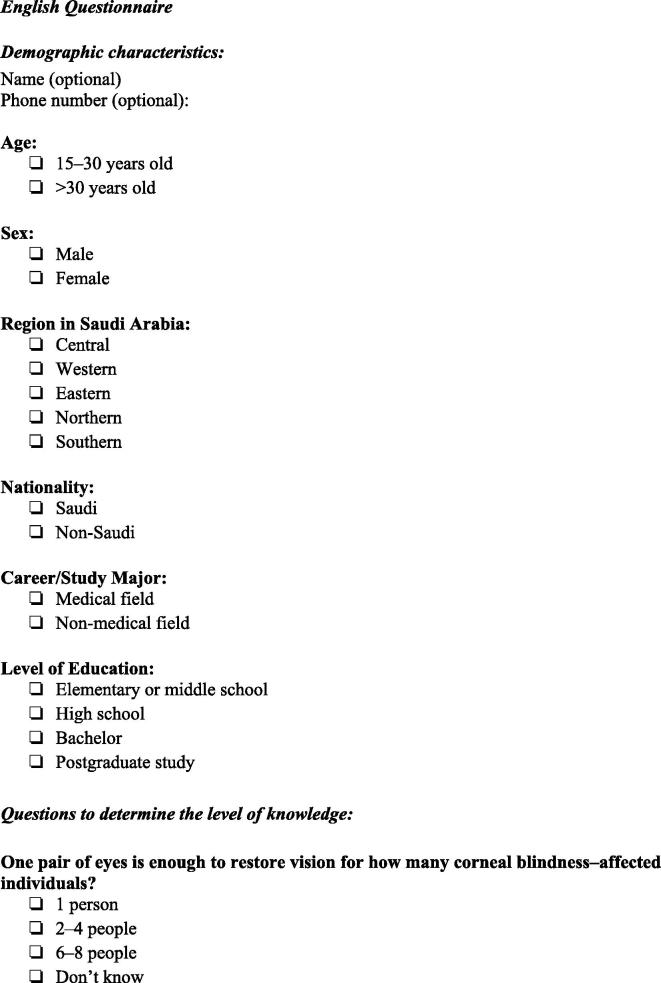
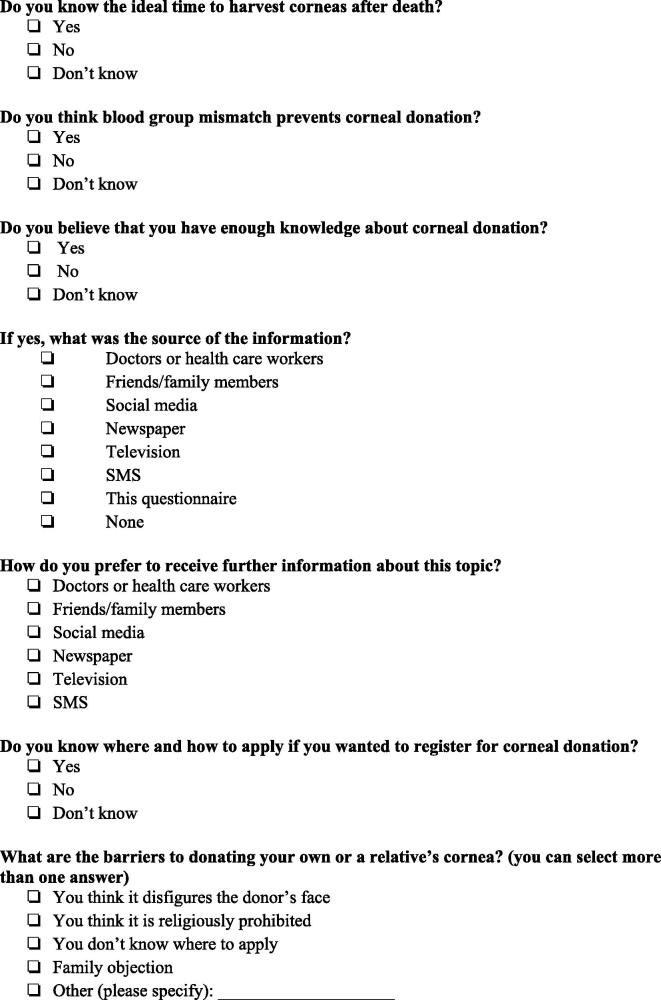
A primary questionnaire based on previous studies was created to understand the participants’ knowledge of, attitudes about, and practice of corneal donation (Appendix A). A panel of experts including ophthalmologists, optometrists, nurses, and statisticians evaluated the content validity. They were asked to assess the overall content of the study and the specific questions related to understanding attitude, beliefs, and awareness. We tested the instrument with a pilot study (N = 25) among a few people from different age groups to assess the language and perception of the questions.
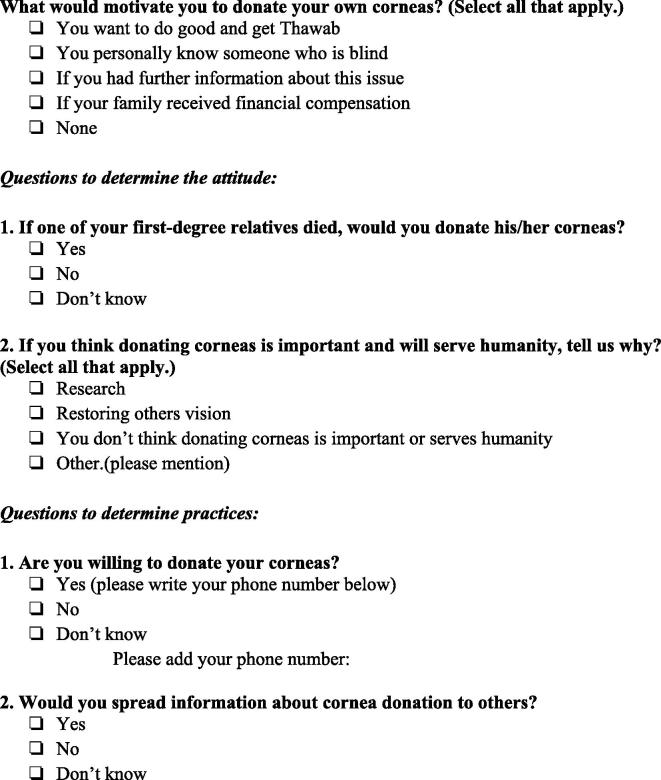
The area under the receiver operating characteristics (ROC) curve for the predicted probability of the subjects’ agreement to donate their corneas was statistically significant, AUC-ROC = 0.83, p < 0.001 (95% CI, AUC = 0.80–0.86), indicating the overall adequacy of the sensitivity and specificity of the model predictors at predicting subjects’ true corneal donation outcomes (ROC figure, Appendix B).
Statistical data analysis
Mean and standard deviation are used to describe the continuous variables, while frequencies and percentages are used to describe the categorical and binary variables. The bivariate associations between the categorical factors were measured using the chi squared (χ2) test of independence. A multiple-response dichotomy analysis was employed to describe the participants’ previously preferred sources of information, perceived barriers, and motives to donate corneas apart from their attitudes, which were measured using multiple response selections. Multivariate binary logistic regression analysis (MBLRA) was employed to assess the combined and individual associations between the participants’ demographic, corneal donation beliefs, and awareness factors and co-variates with their intents to donate their corneas when these factors and co-variates are regressed simultaneously against their odds of donating their corneas.
Ethics
The study protocol was approved by the Research Center of Medical College of King Saud University and its Ethical Committee, and all participants provided informed consent.
Results
Demographics
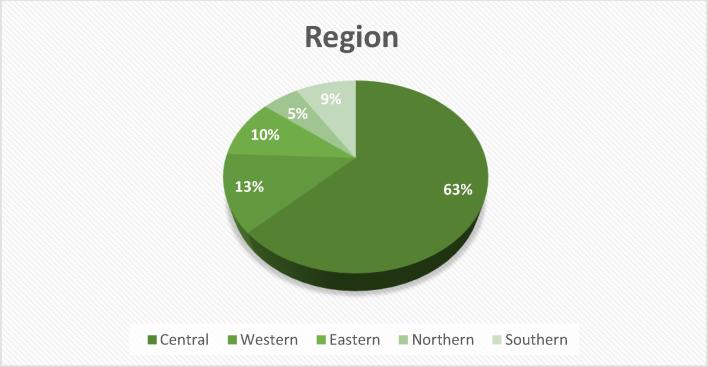
From the various regions, 1292 subjects responded to the survey. The majority of the respondents were female (80.3%). The subjects were classified into two groups based on age: 15–30 years (67.6%) and >30 years (32.4%). Detailed social demographic characteristics are shown in Table 1. A visual representation of the spread of the participants across the five regions in Saudi Arabia is shown in Fig. 1 and the bottom part of Table 1. Most of the respondents (63.9%) came from the central region, another 12.5% came from the Western region, fewer (9.8%) came from the Eastern provinces, and the rest of them came from Northern (5.3%) and Southern (8.4%) regions.
Table 1.
Respondents’ Demographic Characteristics (N = 1292).
| Frequency | Percentage | |
|---|---|---|
| Sex | ||
| Male | 255 | 19.7 |
| Female | 1037 | 80.3 |
| Age | ||
| Below 25 Years | 873 | 67.6 |
| > 25 Years | 419 | 32.4 |
| Career | ||
| Medical Professional | 338 | 26.2 |
| Non-medical professional | 954 | 73.8 |
| Educational Level | ||
| Elementary to Middle | 12 | 0.9 |
| High School Level | 308 | 23.8 |
| University Degree | 907 | 70.2 |
| Higher Studies | 65 | 5 |
| Nationality | ||
| Saudi | 1223 | 94.7 |
| Non-Saudi | 69 | 5.3 |
| Saudi Region | ||
| Central | 826 | 63.9 |
| Western | 162 | 12.5 |
| Eastern | 127 | 9.8 |
| Northern | 68 | 5.3 |
| Southern | 109 | 8.4 |
Fig. 1.
A visual representation of the spread of the participants across the five regions in Saudi Arabia.
Knowledge
“Good knowledge” is defined as one’s ability to answer most of knowledge questions correctly. “Poor knowledge” is defined as giving false answers to most of the knowledge questions. The participants were asked to answer several multiple-choice questions to measure their awareness and knowledge of corneal donation in addition to their attitudes and factors that prevent or motivate them to donate. The results from the analysis are shown in Table 2.
Table 2.
Respondents’ General Awareness of and Attitudes Toward Corneal Donation (N = 1292).
| Frequency | Percentage (%) | |
|---|---|---|
| One pair of eyes is enough to restore vision for how many corneal blindness affected individuals? | ||
| One person | 236 | 18.3 |
| Two to four people | 281 | 21.7 |
| Six to eight people | 30 | 2.3 |
| Don’t Know | 745 | 57.7 |
| Do you know the ideal time to pledge the corneas after death? | ||
| Yes | 156 | 12.1 |
| No | 1136 | 87.9 |
| Do you think blood group mismatch prevents corneal donation? | ||
| Yes | 443 | 34.3 |
| No | 849 | 65.7 |
| Do you believe that you have enough knowledge on cornea donation? | ||
| Yes | 56 | 4.3 |
| No | 1236 | 95.7 |
| Do you know where and how to apply if you wanted to register for corneal donation? | ||
| Yes | 136 | 10.5 |
| No | 1156 | 89.5 |
| Perceived barriers to donate corneas | ||
| Lack of knowledge of where to Donate/Register | 737 | 57.1 |
| Family objection | 393 | 30.4 |
| Corneal Donation disfigures the donor’s face. | 374 | 29 |
| It is religiously unlawful | 98 | 7.6 |
| Perceived motives to donate corneas | ||
| Getting Thawab (Doing Good Acts) in the hereafter for donating. | 855 | 66.2 |
| If informed more about donation, I would donate | 520 | 40.2 |
| No motive in particular. | 202 | 15.9 |
| I Have loved one who is blind. | 170 | 13.2 |
| If family received financial compensation for donating. | 63 | 4.9 |
| Attitudes toward donating Corneas: | ||
| Corneal Donation helps restoring other people's sight | 1233 | 95.4 |
| Corneal Donation helps with medical research | 449 | 34.8 |
| Donating corneas is neither important nor human. | 48 | 3.7 |
| If one of your first-degree relatives died would you donate his/her corneas? | ||
| Yes | 258 | 20 |
| No | 278 | 21.5 |
| Uncertain | 756 | 58.5 |
| Would you contribute to spreading the information about cornea donation to others? | ||
| Yes | 1056 | 81.7 |
| No | 236 | 18.3 |
| Will you donate your corneas /Register as a donor this time? | ||
| Yes | 209 | 16.2 |
| No | 226 | 17.5 |
| Uncertain | 857 | 66.3 |
When asked if they had sufficient information about corneal donation, 95.7% of respondents said no. More importantly, 89% did not know how or where to apply to register as a corneal donor. There was a statistically significant correlation between the participants’ knowledge and their willingness to donate. In other words, those who correctly answered were significantly more willing to donate (p = 0.031). In addition, a significant correlation between willingness to donate and the incorrect belief that a blood group mismatch was a preventive factor, as individuals with that belief were significantly less likely to donate their corneas (p = 0.044), suggesting that those with better knowledge (i.e. those who correctly answered that a matching blood type was unnecessary) were significantly more motivated to donate their corneas. Also, there was a statistically significant difference between those who would like to donate and those who would not based on their knowledge of how many persons’ sight a pair of donated corneas would restore (p = 0.031). Moreover, those who believed they had sufficient information about corneal donation were significantly more likely to donate (p < 0.001) than those who believed that they did not have enough information. In general, after using MBLRA and accounting for all of the other variables in the model, we found that those who reported lacking knowledge about corneal donation were significantly less inclined to donate their corneas than those who reported prior knowledge corneal donation (p = 0.002).
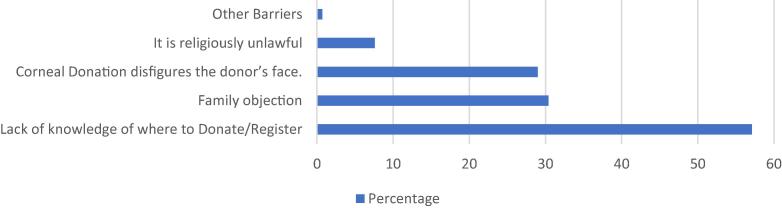
Willingness
The respondents were asked to select all barriers they believed prevented them from donating their corneas. A multiple-response dichotomy analysis was used to analyze their combined selections (Fig. 2). The largest perceived barrier was the lack of information on where to donate/register themselves as donors.
Fig. 2.
Descending percentages of respondents perceived barriers to Corneal Donation.
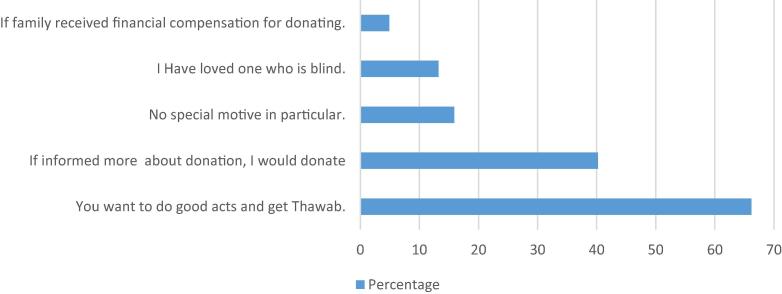
The respondents were also asked to select all motivators that they believed would encourage them to donate their corneas (Fig. 3). The top motive was the religious belief of doing good and being charitable with their body organs, while 40.2% of the respondents stated that they would be more willing to donate their corneas if they were provided with more information. Few of the respondents (4.9%) indicated that they would donate if their family received financial compensation if they would donate their corneas.
Fig. 3.
Respondents perceived motives to Donate Corneas in descending percentages. N = 1292.
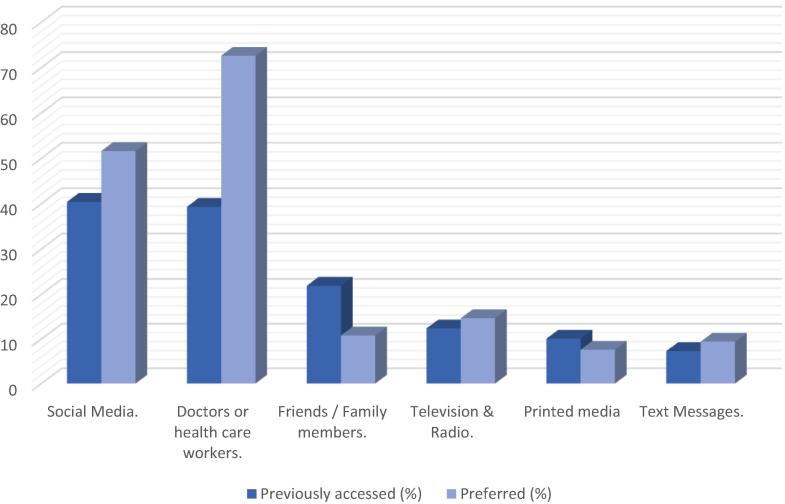
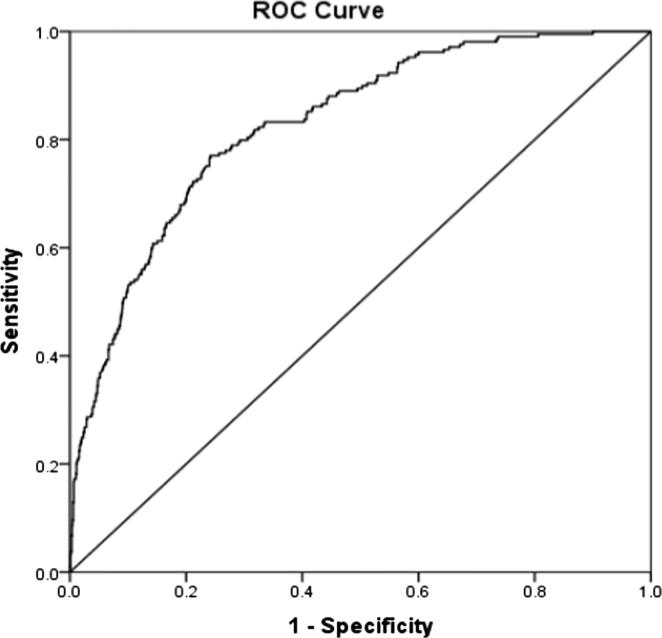
Additionally, the respondents were asked to select as many resources they had previously accessed for information about corneal donation from a list provided. Similarly, participants were asked to select the manner through which they would prefer to receive information about corneal donation. The results are shown in Fig. 4.
Fig. 4.
Comparison between people's preferred and previously accessed sources of corneal donation information.
Attitudes
Attitude is defined as the fixed feeling or way of thinking about corneal donation. Respondents’ attitudes toward donating corneas were measured using a multiple-choice question, and the respondents were allowed to select any combination of these reasons that applied to them and a multiple-response dichotomy analysis was used to analyze the results.
The majority of the respondents (95.4%) selected that restoring blind people’s sight would be their main reason to donate. Another 34.8% selected helping with medical research as an important reason to donate. However, few (3.7%) believed that corneal donation is not important at all. Nevertheless, 66.3% of the respondents were uncertain about whether they would themselves donate their corneas; only (16.2%) agreed they would do so, while 17.6% of them disagreed.
Awareness/Preferred source of information
Respondents were asked to select as many previously accessed corneal donation information resources as they believed was applicable to them from a list; each was allowed to choose all applicable answers. In the same manner, subjects were asked to select the sources of information they preferred to receive corneal donation information through. The yielded results are shown in Fig. 4. Notably, the top preferred resource of corneal information to them was found to be the physicians and Health Care Workers (HCW). Additionally, using the MBLRA, we depicted the mean predicted probability of donating corneas produced from the logistic regression model against people reported previously accessed resources. Clearly, those who received information from physicians and HCW were predicted to be the most likely to donate.
Correlations
The binary logistic regression analysis showed that females were statistically significantly less inclined to report willingness to donate corneas than males when considering the other predictor variables as accounted for (p = 0.051). Females are in fact (1 − OR) × 100 = (1–0.647) × 100 = 35.3% less likely to report willingness to donate their corneas than males when considered jointly with the other predictor independent variables.
By accounting for all the other variables in the model, those who reported lacking knowledge about corneal donation were significantly less inclined to donate their corneas than those who reported prior knowledge about corneal donation (p = 0.002). Those who did not know what corneal donation was were found to be (1 − 0.320) × 100 = 68% less likely to donate their corneas than those who had prior knowledge about the corneal donation process.
The association between subjects’ origins (i.e. regions) and their intent to donate was analyzed using the chi-squared test, which showed no statistically significant difference (p = 0.081). The results showed a statistically significant association between the subjects’ careers and their likelihood to donate (p = 0.014). Medical professionals were significantly more inclined to donate their corneas than those in other professions. However, there was no significant association between gender, age, educational level, or nationality and the likelihood to donate. In addition, people who believed corneal donation after death may lead to a disfigured face of the corpse were significantly less inclined to report willingness to donate corneas than those who do not have such a pre-occupation (p < 0.001). In fact, those occupied with such thoughts of disfigurement were (1 − 0.18) × 100 = 82% less likely to donate than those who were not concerned about facial disfigurement after corneal donation. Furthermore, those who believed in the religious forbiddance of corneal donation were predicted to be (1 − 0.181) × 100 = 81% less willing to donate their corneas than those who believed the corneal donation was not prohibited by Islamic law (p = 0.026). Markedly, those who necessitated the need for financial compensation to their families after donating their corneas were significantly less likely to donate their corneas (p = 0.021). In fact, they were 74% less likely to donate than those who did not have such motives.
Discussion
Despite the limitations of the present study, its findings are valuable in light of the growing demand for corneal transplant in Saudi Arabia. Keratoconus was reported to be the leading indication for corneal transplant in Riyadh as well as the Eastern province of the kingdom.[14], [15] due to the high prevalence in the region, indicating the need for more local corneal grafts.
To meet the demand, health awareness programs targeting the community at large are needed, and such studies are necessary to assess their effectiveness.
The findings of this study showed that higher awareness of and knowledge about corneal donation is associated with a positive attitude toward donation; subjects who believed they had sufficient information about corneal donation were significantly more likely to donate (p < 0.001) than those who did not believe that they have sufficient information, which is consistent with several previous studies.[4], [20] Additionally, Gupta et al. found that people who correctly answered the questions related to their knowledge were more likely to donate their corneas than those who answered inaccurately.1 Furthermore, Paraz et al.4 and Wang et al.20 indicated that insufficient information about corneal donation plays a major role in refusal for donation. In fact, the most common reason for registering as an eye donor was lack of awareness about eye donation in multiple studies among different countries.10
Moreover, in the current study, 40.2% of the respondents stated that they would be more willing to donate their corneas if they were provided with more information. These multiple well-established findings highlight the importance of spreading awareness among the community to increase the number of local donors.
The biggest barrier perceived by the study population was the lack of knowledge where to donate/register themselves as donors, which is similar to the Singaporean Youth Study in 2016, wherein insufficient information was reported as the main reason for indecision about corneal donation.4
The most common motive for donation in the current study was the religious belief of doing good and being charitable with their body organs, which is in contrast with multiple other studies in which it was observed that negative attitudes concerning corneal donation is the highest in individuals who are very religious.17 In fact, in different areas of the world, religion was the main reason for one’s unwillingness to donate; this was seen in Toronto, Hyderaba,18 and an African country.1 This might be due to different religions across these parts of the world. Bearing this fact in mind, according to the current results, local religion -Islam- appears to be the only religion to play an encouraging role in donating corneas, which is consistent with Bugis et al study 15 which showed that majority of their population are aware that religion is not against organ donation. Therefore, such results show the effectiveness of previous awareness programs in improving organ donation locally and the role of religious guiders on this matter worldwide. However, no study has investigated this aspect thoroughly until now.
Another motive was financial compensation: A few subjects (4.9%) indicated that if their families were financially compensated, they would donate their corneas. This is very different from the Singaporean Adult study 22 in which 50.8% indicated that they would be more willing to donate if their family were to receive the benefits. These diverse findings might be due to the different economic status among individuals in Singapore and Saudi Arabia. The current results showed no significant association between gender and willingness to donate. Previous data on this are controversial; some found that females were significantly more willing to donate than males were.[1], [9] Multiple other studies observed that negative attitudes concerning corneal donation are more pronounced in females.[2], [14] However, another study reported that gender does not play a role in the willingness to donate,[8], [18] and gender is not associated with level of awareness.15
which is consistent with the present study’s findings. There was no significant association between age and the propensity to donate. This finding is in contrast to previous findings in which old age was positively correlated with a willingness to donate, while negative attitudes concerning postmortem corneal donation were most pronounced in the young age group.[2], [14] However, the findings of another study suggest that age does not strongly influence the willingness to pledge corneas for donation,8 which is similar to the current results.
There was no significant association between the level of education and the willingness to donate. Previous findings were inconclusive; for example, Australian data showed that willingness to donate corneas significantly decreased with higher education.10 However, other studies found that a higher level of education was a significant predictor of good knowledge about eye donation.[8], [1] Similarly, research suggested that awareness and willingness were both strongly associated with higher educational status among Singaporeans.10 In a Turkish study, a low education level was the essential factor contributing to negative attitudes toward tissue donation.14 In the current population, awareness itself was not significantly associated with education level.
Creating effective policies can be beneficial to addressing the organ shortage. Many developing countries such as Argentina,19 Chile,23 and Colombia 24 have adopted the “opt-out” policy, whereby all people >18 years of age are considered organ donors unless they document their refusal. In developed world, about 24 countries have adopted a policy of presumed consent (opt-out) system, prominently in USA,21 Spain, Austria, and Belgium, resulting in higher donor rates in these countries.17
This study shares the limitations associated with questionnaire-based studies. Mostly differences in understanding and interpretation of questions. The other limitation of the current study is the predominance of female gender. In conclusion, further awareness is needed to increase the number of local donors. Physicians and HCW were the most preferred source of information; people who have good knowledge are more likely to register as donors. These findings indicate the need for policies and resources to increase awareness among the general population. We recommend creating effective policies to address the shortage of corneal grafts. We also highly recommend encouraging physicians and HCW to spread awareness throughout the community.
Conflict of interest
The authors declared that there is no conflict of interest.
Acknowledgments
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations
Our preliminary results were presented at the Red Sea Ophthalmology Symposium, Jeddah (2017), and Saudi Ophthalmology Symposium, Riyadh (2018).
Acknowledgements
The authors extend their sincere appreciation to King Khaled Eye Specialist Hospital for their indispensable cooperation to this research project.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
Contributor Information
Latifa F. Alanazi, Email: Latifafahad.a@gmail.com.
Abdullah M. Alfawaz, Email: idrfawaz@KSU.EDU.SA.
Appendix A.
Appendix B.
References
- 1.Brunette I., Roberts C.J., Vidal Franç. Alternatives to eye bank native tissue for corneal stromal replacement. Progress Retinal Eye Res. 2017 doi: 10.1016/j.preteyeres.2017.04.002. [DOI] [PubMed] [Google Scholar]
- 2.Uhlig C.E. Attitudes toward postmortem cornea donation in germany: a multicenter survey. Graefe's Archive Clin Experiment Ophthalmol. 2014;252(12):1955–1962. doi: 10.1007/s00417-014-2796-y. [DOI] [PubMed] [Google Scholar]
- 3.Assiri A.A., Yousuf B.I., Quantock A.J. Incidence and severity of keratoconus in Asir province Saudi Arabia. British J Ophthalmol. 2005;89:1403–1406. doi: 10.1136/bjo.2005.074955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paraz Carisa Mariella Alvarez. “Knowledge and attitudes toward corneal donation among singaporean youth: a cross-sectional study”. Eye and Vision 3.1. 2016 doi: 10.1186/s40662-016-0049-3. n. pag. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bijapur Vijayamahantesh M., Vallabha K. “Knowledge, attitude and practice patterns regarding eye donation, eye banking and corneal transplant in a tertiary care hospital”. J Krishna Inst Medical Sci Univ. 2015;4(4):94–103. [Google Scholar]
- 6.Röck Daniel. “Evaluation of factors limiting corneal donation”. Annals Transplant. 2016;21:701–707. doi: 10.12659/aot.900456. [DOI] [PubMed] [Google Scholar]
- 7.Tabbara Khalid, Omar Nazri, Chacra Charbel Bou. “Outcome of corneal transplantation in a private institution in Saudi Arabia”. Clin Ophthalmol. 2013:1311. doi: 10.2147/OPTH.S43719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gupta A., Jain S., Jain T., Gupta K. Awareness and perception regarding eye donation in students of a nursing college in Bangalore. Indian J Community Med [serial online] 2009;34:122–125. doi: 10.4103/0970-0218.51235. http://www.ijcm.org.in/text.asp?2009/34/2/122/51235 Available from:[cited 2017 Jun 8] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lawlor M. Specific unwillingness to donate eyes: the impact of disfigurement, knowledge and procurement on corneal donation. Am J Transplant. 2010;10(3):657–663. doi: 10.1111/j.1600-6143.2009.02986.x. [DOI] [PubMed] [Google Scholar]
- 10.Williams A., Muir K. Awareness and attitudes toward corneal donation: challenges and opportunities. Clin Ophthalmol. 2018;12:1049–1059. doi: 10.2147/OPTH.S142702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Broumand B. Transplantation activities in Iran. Exp Clin Transplant. 2005 Jun;3(1):333–337. [PubMed] [Google Scholar]
- 12.Newsletter of IRANTOP, 2004. No. 2, page 2
- 13.Palamar M., Durusoy R., Egrilmez S., Salis O., Yagci A. Public opinion concerning corneal donation and transplant: a survey from Izmir. Turkey Exp Clin Transpl. 2011;9(2):134–138. Apr. [PubMed] [Google Scholar]
- 14.Al-Akily Saleh A., Bamashmus Mahfouth A. “Causes of blindness among adult yemenis: a hospital-based study”. Middle East African J Ophthalmol. 2008;15(1):3–6. doi: 10.4103/0974-9233.53367. PMC. Web. 26 Aug. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bugis A., Ali A., Almaghrabi A., Alharbi A., Fatani Y., Alem S., Siddiqui M. Knowledge and attitudes regarding eye donation and corneal transplants in Saudi Arabia a cross-sectional study. Int J Medical Res Profession. 2018:272–275. http://www.academia.edu/36764871/Knowledge_and_Attitudes_Regarding_Eye_Donation_and_Corneal_Transplants_In_Saudi_Arabia_A_Cross-Sectional_Study Available at: [Google Scholar]
- 16.Hameed N., Jadidy E. Knowledge and attitude regarding eye donation and corneal transplantation among medical students of Taibah University in Medina, Saudi Arabia 2015. Int. J. Academic Sci Res. 2015;3(4):18–26. http://www.ijasrjournal.org [online] Available at: [Google Scholar]
- 17.Desde hoy la donación de órganos es obligatoria [Internet]. Publimetro Colombia. 2017. Available from: <https://www.publimetro.co/co/colombia/2017/02/04/donacion-organos-obligatoria.html>.
- 18.Patil R., Gothankar J., Bhat P., Saluja J., Sane S. Eye donation: awareness and willingness among shopkeepers. Int J Community Med Public Health. 2017;4(6):2056. [Google Scholar]
- 19.BORA [Internet]. Boletinoficial.gob.ar. 2005. Available from: https://www.boletinoficial.gob.ar/#!DetalleNorma/7283011/20051222
- 20.Wang X., Jin L., Wang J. Attitudes and knowledge concerning corneal donation in a population-based sample of urban chinese adults. Cornea. 2016;35(10):1362–1367. doi: 10.1097/ICO.0000000000000943. [DOI] [PubMed] [Google Scholar]
- 21.Gormley, Michael (April 27, 2010). “New York To Be First Organ Donor Opt-Out State?”. New York. The Huffington Post. New York City. Archived from the original on April 30, 2010. Retrieved March 7, 2014.
- 22.Yew Y.-W. “Knowledge and beliefs on corneal donation in singapore adults”. Br J Ophthalmol. 2005;89(7):835–840. doi: 10.1136/bjo.2004.057372. Web. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.LEY-20413 15-ENE-2010 MINISTERIO DE SALUD, SUBSECRETARÍA DE SALUD PÚBLICA - Ley Chile - Biblioteca del Congreso Nacional [Internet]. Ley Chile - Biblioteca del Congreso Nacional. 2017. Available from: <https://www.leychile.cl/Navegar?idNorma=1010132>.
- 24.Desde hoy la donación de órganos es obligatoria [Internet]. Publimetro Colombia. 2017. Available from: <https://www.publimetro.co/co/colombia/2017/02/04/donacion-organos-obligatoria.html>.