Abstract
A 79-year-old man presented with unilateral unexplained sudden onset visual loss in the setting of central retinal vein occlusion (CRVO). Non ischemic CRVO in the right eye (RE) was confirmed on fluorescein angiography. Spectral domain optical coherence tomography (SD-OCT) showed absence of macular edema and hyperreflective band-like lesions in the middle retinal layers of the RE suggesting a diagnosis of paracentral acute middle maculopathy (PAMM). Patient was observed and after 3 months, best-corrected visual acuity in the RE spontaneously improved from 38 to 56 ETDRS letters. SD-OCT scans showed thinning of the inner nuclear layer of the RE. OCT angiography in the RE revealed a mild attenuation of the vascular flow signal in the superficial capillary plexus and patchy areas of vascular flow void in the deep capillary plexus, as compared to the fellow eye.
The present case outlines the importance of recognising PAMM as a cause of unexplained visual loss. In the setting of a CRVO with sudden vision loss and absence of macular edema, clinicians should pay attention to any hyperreflectivity and/or to thinning of the middle retinal layers on SD-OCT.
Keywords: Paracentral acute middle maculopathy, Central retinal vein occlusion, spectral domain optical coherence tomography, Deep capillary ischemia, Optical coherence tomography angiography
Introduction
Paracentral acute middle maculopathy (PAMM) is a spectral domain optical coherence tomography (SD-OCT) manifestation presenting with hyper-reflective band-like lesions involving the outer plexiform layer/inner nuclear layer (OPL/INL) junction resulting in permanent INL thinning.1
PAMM was first reported as a cause of unexplained vision loss in otherwise healthy subjects by Sarraf and associates.1 Patients typically presented with paracentral scotoma which persisted over the course of the condition.1 Currently PAMM is considered a manifestation of focal ischemia of the deep deep retinal circulation that may herald the presence of a secondary underlying condition.2 Several systemic conditions and retinal vascular disorders have been associated with PAMM.[2], [3] In the first and largest case series on PAMM and central retinal vein occlusion (CRVO), PAMM was reported to occur in 5.2% of the patients presenting with CRVO.4 All of these patients presented with non ischemic CRVO and only 20% of these patients had coexisting macular edema at presentation.4 However since retinal hemorrhages or edema might have limited the ability to detect PAMM, the actual presence of PAMM in CRVO might be much higher than they reported.4
Because of the relatively small number of patients reported in the current literature, little is known about the natural course of PAMM in CRVO.
Optical coherence tomography angiography (OCTA) is a recently introduced imaging technique which non-invasively provides detailed assessment of the retinal and choroidal vasculature by detecting motions of erythrocytes and visualising blood flow using serial OCT B-scans. We herein describe natural course and multimodal retinal imaging, including OCTA, of a case of PAMM secondary to non ischemic CRVO with spontaneous improvement of the vision during follow-up.
Case report
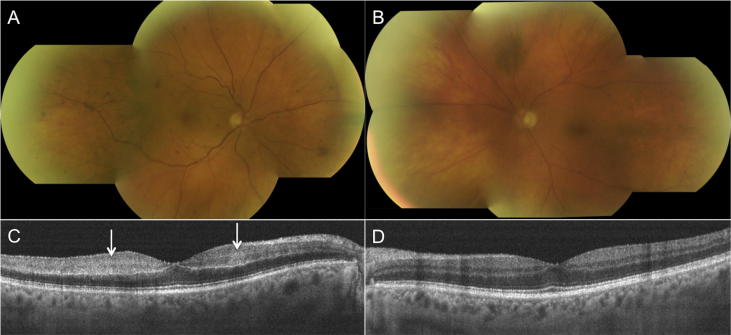
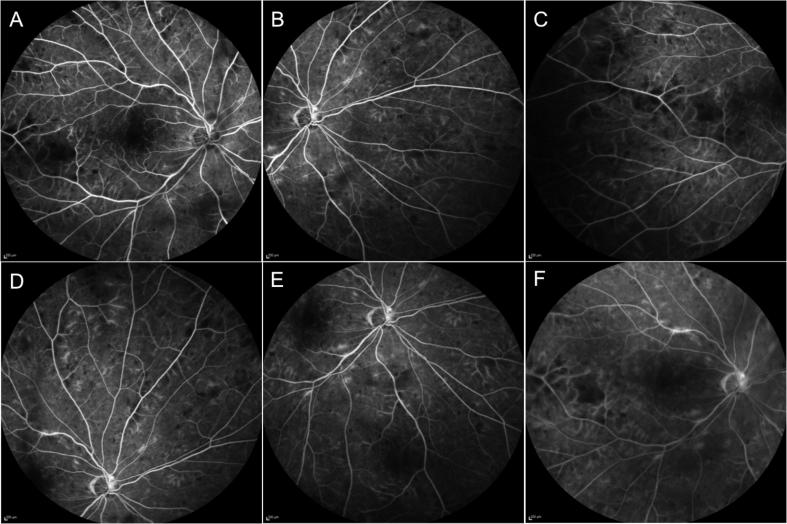
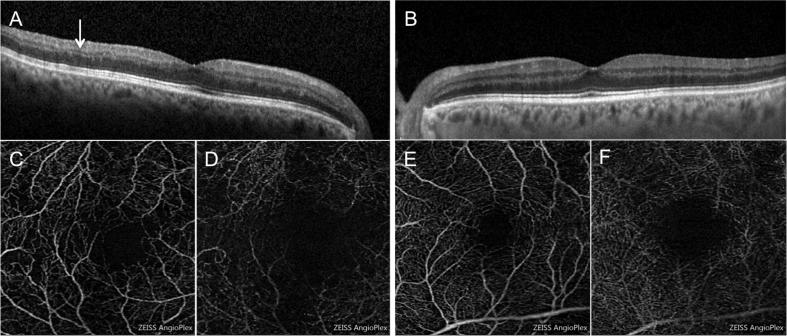
A 79-year-old man was referred for evaluation of a sudden onset loss of vision in the right eye (RE). Medical history included Type 2 diabetes for 15 years controlled by diet, hypertension on treatment, and myocardial infarction 9 years before. Ocular history of the patient was unremarkable. Best corrected visual acuity (BCVA) was 38 ETDRS letters in the RE and 81 ETDRS letters in the left eye (LE). Aside from a mild bilateral cataract, anterior segment was unremarkable in both eyes. Intraocular pressure was 19 mmHg in the RE and 12 mmHg in the LE. Dilated fundus examination of the RE revealed a mild venous engorgement and widespread peripheral retinal hemorrhages located in all 4 quadrants (Fig. 1A). The fundus of the LE was unremarkable (Fig. 1B). SD-OCT scan of the RE showed absence of macular edema and hyperreflective band-like lesions in the middle retinal layers (Fig. 1C) suggesting a diagnosis of PAMM. No abnormalities were detected on SD-OCT scans of the LE (Fig. 1D). Fluorescein angiography (FA) in the RE (Fig. 2) showed slighlty delayed venous filling and patchy areas of retinal non perfusion in the mid periphery, consistent with non ischemic central retinal vein occlusion (CRVO). After 3 months, BCVA in the RE spontaneously improved from 38 to 56 ETDRS letters and unchanged in the LE. SD-OCT scans showed thinning of the inner nuclear layer in the RE (Fig. 3A) and was unchanged in the LE (Fig. 3B). OCT angiography (Angioplex CIRRUS HD-OCT, Carl Zeiss Meditec, Inc., Dublin, USA) revealed a mild attenuation of the vascular flow signal in the superficial capillary plexus (Fig. 3C) and patchy areas of vascular flow void in the deep capillary plexus (Fig. 3D), as compared to the fellow eye (Fig. 3E,F).
Fig. 1.
Montage colour fundus photography (CFP) and spectral domain optical coherence tomography (SD-OCT) at presentation. CFP (A) of the right eye (RE) shows a mild venous engorgement and widespread peripheral retinal hemorrhages located in all 4 quadrants. CFP of the left eye (LE) (B) does not show any retinal abnormalities. SD-OCT scan of the macula of the RE (C) shows hyperreflective band-like lesions (arrows) in the middle retinal layers of the macula of the right eye and no abnormalities at the macula of the left eye (D).
Fig. 2.
Fluorescein angiography frames of the right eye at presentation show minimal patchy areas of non perfusion at the posterior pole (A) and in the mid periphery (B–E) with absence of macular edema in the late phase of the angiogram (F).
Fig. 3.
After 3 months, spectral domain optical coherence tomography (SD-OCT) scan of the right eye (A) reveals thinning of the inner nuclear layer (arrow); no abnormalities were detected in the left eye (B). OCT angiography with a scanning area of 3 × 3 mm shows mild attenuation of the vascular flow signal in the superficial capillary plexus (SCP) (C) and patchy areas of vascular flow void in the deep capillary plexus (DCP) (D) of the right eye, and normal flow in the SCP (E) and DCP (F) of the left eye.
Discussion
The retina is provided with a multilayered capillary network composed of the superficial capillary plexus (SCP) located at the level of the ganglion cell layer and the intermediate and deep capillary plexus (DCP) located at the level of the inner nuclear layer (INL).5
In 2014 Yu et al.6 identified abnormal bands of hyperreflectivity on SD-OCT as markers of deep retinal ischemia. It was observed that when the hyperreflectivity involved the SCP it corresponded to a cotton wool spot on fundus examination and a related hypoperfusion was visible on fluorescein angiography (FA). By contrast, in eyes with hyperreflective bands in the middle retinal layers, there was no FA correlate and variable degree of macular whitening on fundus examination was observed.6 In the same year, Sarraf and associates described similar abnormal bands of hyperreflectivity at the level of the outer plexiform/inner nuclear layers junction of the OCT scan with no FA correlate and these were referred to as paracentral acute middle maculopathy (PAMM).1
While PAMM was initially considered as a variant of acute macular neuroretinopathy (AMN),1 in a recent editorial,2 it was clarified that AMN and PAMM should be regarded as two distinct and different entities. Unlike PAMM, AMN typically presents with flat, reddish, wedge or teardrop-shaped intraretinal lesions usually pointing toward the fovea which are best seen using infrared reflectance imaging.7 Moreover AMN presents on OCT with hyperreflective bands located deeper (at the level of the outer plexiform/outer nuclear layers junction) than those observed in PAMM with resulting thinning of the outer retinal layer and attenuation of the ellipsoid zone and external limiting membrane bands in the post acute phase of the disease.7
Evidence of INL thinning during the natural course of PAMM suggested focal ischemia of the intermediate and DCP as the causative mechanism of PAMM manifestations.
While FA has been the gold standard for the assessment of retinal ischemia for decades, it is not able to detect the flow in the DCP. OCTA is able to noninvasively assess not only the SCP traditionally seen on FA but also the DCP5; thus OCTA offers an unique opportunity for the understanding of PAMM pathophysiology. Recent case series[8], [9] have imaged PAMM with OCTA. Sridhar et al.8 reported OCTA features of PAMM and CRVO in 5 patients. In all patients with PAMM and CRVO and in the vast majority of patients with PAMM related to other conditions, OCTA showed normal flow in the DCP in the acute phase and invariable vascular flow void of the DCP in the post acute phase.[8], [9] These findings support the hypothesis that pathogenesis of PAMM may be related to a transient hypoperfusion of the DCP with immediate restoration of microcirculation and absence of acute sctructural changes on OCTA; reperfusion injury may account for the subsequent legacy of atrophy of the INL associated with loss of the DCP visible on OCTA in the chronic phase.[8], [9]
In the present case, in spite of the INL thinning, a spontaneous improvement in the vision was noted. The reason of this improvement is unclear. From the current literature little is known about the natural course of PAMM in CRVO and spontaneous improvement in the visual acuity of these patients has been reported only in a few cases.3 In a recent case series,10 it has been showed that the natural course of visual acuity in patients with PAMM secondary to CRVO may vary and that the extent of the DCP dropout on OCTA may reflect the extent of visual acuity impairment in the post acute phase of this condition. Therefore it is possible that the extent and the time to reperfusion following the acute phase of this condition may affect the natural visual acuity outcomes of these patients.
In summary, the present case outlines the importance of recognising PAMM as a cause of unexplained visual loss. In the setting of a CRVO with sudden vision loss and absence of macular edema, clinicians should pay attention to any hyperreflectivity and/or to thinning of the middle retinal layers on OCT. While the hyperreflective bands in the middle retina are a typical feature of PAMM on OCT at presentation, inner nuclear thinning and hypoperfusion of the DCP on OCTA, are suggestive of PAMM in the post acute phase. While currently there is no treatment for PAMM, management of patients should be targeted toward the identification and treatment of related vasculopathic and systemic risk factors, when present.2
Conflict of interest
The authors declared that there is no conflict of interest.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.Sarraf D., Rahimy E., Fawzi A.A. Paracentral acute middle maculopathy: a new variant of acute macular neuroretinopathy associated with retinal capillary ischemia. JAMA Ophthalmol. 2013;131:1275–1287. doi: 10.1001/jamaophthalmol.2013.4056. [DOI] [PubMed] [Google Scholar]
- 2.Rahimy E., Kuehlewein L., Sadda S.R., Sarraf D. Paracentral acute middle maculopathy: what we knew then and what we know now. Retina. 2015;35:1921–1930. doi: 10.1097/IAE.0000000000000785. [DOI] [PubMed] [Google Scholar]
- 3.Chen X., Rahimy E., Sergott R.C. Spectrum of retinal vascular diseases associated with paracentral acute middle maculopathy. Am J Ophthalmol. 2015;160:26–34. doi: 10.1016/j.ajo.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Rahimy E., Sarraf D., Dollin M.L., Pitcher J.D., Ho A.C. Paracentral acute middle maculopathy in non ischemic central retinal vein occlusion. Am J Ophthalmol. 2014;158:372–380. doi: 10.1016/j.ajo.2014.04.024. [DOI] [PubMed] [Google Scholar]
- 5.Spaide R.F., Klancnik J.M., Cooney M.J. Retinal vascular layers imaged by fluorescein angiography and optical coherence tomography angiography. JAMA Ophthalmol. 2015;133:45–50. doi: 10.1001/jamaophthalmol.2014.3616. [DOI] [PubMed] [Google Scholar]
- 6.Yu S., Wang F., Pang C.E., Yannuzzi L.A., Freund K.B. Multimodal imaging findings in retinal deep capillary ischemia. Retina. 2014;34:636–646. doi: 10.1097/IAE.0000000000000048. [DOI] [PubMed] [Google Scholar]
- 7.Fawzi A.A., Pappuru R.R., Sarraf D. Acute macular neuroretinopathy: long- term insights revealed by multimodal imaging. Retina. 2012;32:1500–1513. doi: 10.1097/IAE.0b013e318263d0c3. [DOI] [PubMed] [Google Scholar]
- 8.Sridhar J., Shahlaee A., Rahimy E. Optical coherence tomography angiography and en face optical coherence tomography features of paracentral acute middle maculopathy. Am J Ophthalmol. 2015;160:1259–1268. doi: 10.1016/j.ajo.2015.09.016. [DOI] [PubMed] [Google Scholar]
- 9.Nemiroff J., Kuehlewein L., Rahimy E. Assessing deep retinal capillary ischemia in paracentral acute middle maculopathy by optical coherence tomography angiography. Am J Ophthalmol. 2015;162:121–132. doi: 10.1016/j.ajo.2015.10.026. [DOI] [PubMed] [Google Scholar]
- 10.Casalino G., Williams M., McAvoy C., Bandello F., Chakravarthy U. Optical coherence tomography angiography in paracentral acute middle maculopathy secondary to central retinal vein occlusion. Eye (Lond) 2016;30:888–893. doi: 10.1038/eye.2016.57. [DOI] [PMC free article] [PubMed] [Google Scholar]