Abstract
Background
We assessed the efficacy of the licensed mepolizumab dose (100 mg subcutaneously [SC]) in patients with severe eosinophilic asthma according to body weight/body mass index (BMI).
Methods
This was a post hoc individual patient-level meta-analysis of data from the Phase 3 studies MENSA (MEA115588/NCT01691521) and MUSCA (200862/NCT02281318). Patients aged ≥12 years with severe eosinophilic asthma and a history of exacerbations were randomised to 4-weekly placebo, mepolizumab 75 mg intravenously (IV) or 100 mg SC (MENSA) or placebo or mepolizumab 100 mg SC (MUSCA) for 32 (MENSA) or 24 (MUSCA) weeks. The primary endpoint was the annual rate of clinically significant exacerbations; other outcomes included the proportion of patients with no exacerbations, lung function, St George’s Respiratory Questionnaire (SGRQ) and Asthma Control Questionnaire-5 (ACQ-5) scores and blood eosinophil counts. Analyses were performed by baseline body weight and BMI (≤60, > 60–75, > 75–90, > 90, < 100, ≥100 kg; ≤25, > 25–30, > 30, < 36, ≥36 kg/m2).
Results
Overall, 936 patients received placebo or mepolizumab 100 mg SC. Across all body weight/BMI categories, mepolizumab reduced the rate of clinically significant exacerbations by 49–70% versus placebo. Improvements with mepolizumab versus placebo were also seen in lung function in all body weight/BMI categories except > 90 kg; improvements in SGRQ and ACQ-5 scores were seen across all categories.
Conclusions
Mepolizumab 100 mg SC has consistent clinical benefits in patients with severe eosinophilic asthma across a range of body weights and BMIs. Data show that the fixed-dose regimen of mepolizumab is suitable, without the need for weight-based dosing.
Trial registration
This manuscript is a post hoc meta-analysis of data from the Phase 3 studies MENSA and MUSCA. ClinicalTrials.gov, NCT01691521 (MEA115588; MENSA). Registered September 24, 2012. ClinicalTrials.gov, NCT02281318 (200862; MUSCA). Registered November 3, 2014.
Electronic supplementary material
The online version of this article (10.1186/s12931-019-1134-7) contains supplementary material, which is available to authorized users.
Keywords: Asthma, Asthma pharmacology, Body mass index, Body weight, Mepolizumab
Background
Asthma affects an estimated 339 million people worldwide [1], with 5–10% of this population having severe asthma, characterised by frequent, persistent respiratory symptoms, despite the regular use of maintenance therapies and additional controllers [2]. Severe asthma is a heterogeneous condition, with a number of clinical phenotypic expressions including severe eosinophilic asthma [2, 3]. Patients with severe eosinophilic asthma often develop disease in adult life, experience recurrent exacerbations and characteristically show eosinophilic inflammation despite appropriate treatment [2, 3], highlighting a need for more targeted therapy.
Mepolizumab is a monoclonal antibody (mAb) that selectively targets interleukin (IL)-5 and inhibits eosinophilic inflammation [4, 5]. In Phase 3 clinical studies, mepolizumab treatment was associated with reduced rates of exacerbations, decreased oral glucocorticoid dependence and improved lung function, asthma control and health-related quality of life (HRQoL), compared with placebo [6–8]. Mepolizumab is approved in the US and Europe for use as an add-on treatment for patients with severe eosinophilic asthma, and the licensed dose for adults and adolescents, administered subcutaneously (SC), is fixed at 100 mg, regardless of body weight [4, 5]. A fixed-dose regimen is preferred since it reduces the likelihood of dosing errors and drug wastage compared with a treatment regimen in which the dose is determined according to body weight [9]. However, overweight and obese patients may display reduced responses to some treatments as a result of altered drug bioavailability [10, 11]. As such, it is important to explore the treatment response of fixed-dosed regimens across a wide spectrum of body compositions.
The aim of this post hoc meta-analysis of data from two Phase 3 clinical trials, MENSA (MEA115588/NCT01691521) and MUSCA (200862/NCT02281318) [7, 8], was to assess the efficacy of the licensed dose of mepolizumab (100 mg SC) versus placebo in patients with severe eosinophilic asthma according to body weight and body mass index (BMI).
Methods
Study design
This was a post hoc individual patient-level meta-analysis of data from two Phase 3, placebo-controlled, randomised, double-blind, parallel-group, multicentre studies, MENSA and MUSCA [7, 8], which assessed the licensed dose of mepolizumab (100 mg SC) in patients with severe eosinophilic asthma. Results of these studies have been reported previously [7, 8]. In brief, patients enrolled in MENSA were randomised (1:1:1) to receive mepolizumab 75 mg intravenously (IV), mepolizumab 100 mg SC or placebo, plus standard of care (high-dose inhaled corticosteroids [ICS] and another controller), every 4 weeks for 32 weeks. Patients enrolled in MUSCA were randomised (1:1) to receive mepolizumab 100 mg SC or placebo, plus standard of care, every 4 weeks for 24 weeks. This post hoc analysis reports data from patients who received placebo or mepolizumab 100 mg SC only. MENSA and MUSCA were conducted in accordance with the ethical principles of the Declaration of Helsinki, International Conference on Harmonisation Good Clinical Practice Guidelines, and applicable country-specific regulatory requirements.
Patients
MENSA and MUSCA enrolled patients aged ≥12 years with severe eosinophilic asthma (blood eosinophil count: ≥300 cells/μL in the previous year; or ≥ 150 cells/μL at screening) who had a history of ≥2 exacerbations (requiring systemic corticosteroids) in the 12 months prior to screening despite regular treatment with high-dose ICS during the same period, plus additional controller medication(s) with or without oral corticosteroids (OCS) for ≥3 months. Neither study included specific body weight or BMI inclusion criteria. Data from patients who received ≥1 dose of either placebo or mepolizumab were included in this meta-analysis; this was the modified intent-to-treat population.
Endpoints and assessments
The primary endpoint was the annual rate of clinically significant exacerbations (defined as a worsening of asthma that required the use of systemic corticosteroids and/or hospitalisation/emergency department visit). Secondary endpoints included the proportion of patients with no clinically significant exacerbations over the course of the study, change from baseline in pre-bronchodilator forced expiratory volume in 1 s (FEV1) at study end, change from baseline in St George’s Respiratory Questionnaire (SGRQ) total score at study end, the proportion of responders achieving a ≥ 4-point reduction (minimal clinically important difference [MCID] [12]) from baseline in SGRQ total score at study end, change from baseline in Asthma Control Questionnaire (ACQ-5) score at study end, the proportion of responders achieving a ≥ 0.5-point reduction (MCID [13]) from baseline in ACQ-5 score at study end, and the change from baseline in blood eosinophil count at study end.
Sample size and statistical analysis
Analyses were stratified by body weight (categories: ≤60, > 60–75, > 75–90 and > 90 kg [all endpoints]; thresholds: < 100 and ≥ 100 kg [primary endpoint only]) and BMI (categories: ≤25, > 25–30 and > 30 kg/m2 [all endpoints]; thresholds: < 36 and ≥ 36 kg/m2 [primary endpoint only]). Body weight categories were selected based on cut-offs used in analyses of previous mepolizumab studies. BMI categories were selected based on those generally used in clinical practice to define normal weight, overweight and obese.
The rate of exacerbations was analysed separately for each subgroup in each study using a negative binomial model, including the log of time on treatment as an offset variable. Continuous endpoints, including changes from baseline in pre-bronchodilator FEV1, SGRQ total score (scale 0–100, with higher scores indicating worse HRQoL), ACQ-5 score, and blood eosinophil count, were analysed using a mixed model repeated measures analysis. The proportion of patients with no clinically significant exacerbations and the proportions of SGRQ total score and ACQ-5 score responders were analysed using a logistic regression model. All model-based analyses were adjusted for treatment, number of exacerbations in the previous year (2, 3, ≥4), baseline maintenance OCS use, baseline pre-bronchodilator percent predicted FEV1 (except analysis of FEV1), geographical region, and baseline value of the analysis variable (where applicable). End-of-study treatment differences between mepolizumab 100 mg SC and placebo for each subgroup were combined across studies using an inverse variance weighted fixed-effects meta-analysis. The protocol for the meta-analysis is available on the GSK Clinical Studies Register (Study ID 208115) [14].
Results
Patient population
In total, 1136 patients who participated in the MENSA and MUSCA studies received ≥1 dose of study treatment and were included in the analysis. Of these, 936 were randomised to receive either placebo (n = 468) or mepolizumab 100 mg SC (n = 468). Patient demographics and baseline characteristics by body weight and BMI categories and thresholds are shown in Table 1. At baseline, patients had a mean weight of 78.1 kg and BMI of 28.0 kg/m2. In general, mean age was similar across body weight and BMI subgroups. Patients in the higher BMI and weight categories generally had worse SGRQ scores compared with those in the lower categories. Across subgroups, around one-quarter of patients were receiving OCS maintenance therapy at baseline.
Table 1.
Summary of patient demographics and baseline characteristics by body weight and BMI
| Body weight | BMI | Total population (N = 936) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Categories | Thresholds | Categories | Thresholds | |||||||||
| ≤60 kg (N = 144) | > 60–75 kg (N = 319) | > 75–90 kg (N = 288) | > 90 kg (N = 185) | < 100 kg (N = 819) | ≥100 kg (N = 117) | ≤25 kg/m2 (N = 323) | > 25–30 kg/m2 (N = 330) | > 30 kg/m2 (N = 283) | < 36 kg/m2 (N = 844) | ≥36 kg/m2 (N = 92) | ||
| Female, n (%) | 125 (87) | 198 (62) | 149 (52) | 76 (41) | 499 (61) | 49 (42) | 188 (58) | 179 (54) | 181 (64) | 482 (57) | 66 (72) | 548 (59) |
| Mean (SD) age, years | 46.5 (18.7) | 51.5 (14.0) | 52.1 (12.0) | 50.1 (11.3) | 50.9 (14.2) | 48.9 (11.3) | 47.8 (16.4) | 53.1 (13.0) | 51.0 (11.0) | 50.9 (14.1) | 48.5 (11.7) | 50.6 (13.9) |
| Mean (SD) duration of asthma, years | 17.4 (12.1) | 20.3 (14.9) | 20.0 (14.5) | 20.0 (14.9) | 19.8 (14.4) | 18.9 (14.6) | 17.9 (13.8) | 20.1 (14.4) | 21.4 (14.9) | 19.4 (14.2) | 23.1 (15.4) | 19.7 (14.4) |
| Clinically significant exacerbations in the previous year, n (%) | ||||||||||||
| Mean (SD) | 3.4 (2.2) | 3.2 (2.7) | 3.0 (1.8) | 3.2 (2.2) | 3.2 (2.3) | 3.2 (2.2) | 3.2 (2.4) | 3.1 (2.2) | 3.2 (2.1) | 3.2 (2.3) | 3.3 (2.4) | 3.2 (2.3) |
| 2 | 72 (50) | 187 (59) | 171 (59) | 91 (49) | 464 (57) | 57 (49) | 181 (56) | 188 (57) | 152 (54) | 472 (56) | 49 (53) | 521 (56) |
| 3 | 28 (19) | 61 (19) | 52 (18) | 49 (26) | 160 (20) | 30 (26) | 60 (19) | 73 (22) | 57 (20) | 170 (20) | 20 (22) | 190 (20) |
| ≥ 4 | 44 (31) | 71 (22) | 65 (23) | 45 (24) | 195 (24) | 30 (26) | 82 (25) | 69 (21) | 74 (26) | 202 (24) | 23 (25) | 225 (24) |
| Receiving maintenance OCS therapy at baseline, n (%) | ||||||||||||
| Yes | 24 (17) | 80 (25) | 71 (25) | 52 (28) | 196 (24) | 31 (26) | 79 (24) | 74 (22) | 74 (26) | 204 (24) | 23 (25) | 227 (24) |
| No | 120 (83) | 239 (75) | 217 (75) | 133 (72) | 623 (76) | 86 (74) | 244 (76) | 256 (78) | 209 (74) | 640 (76) | 69 (75) | 709 (76) |
| Mean (SD) % predicted pre-bronchodilator FEV1 | 62.8 (16.8) | 59.4 (17.8) | 59.1 (15.8) | 57.7 (16.6) | 59.5 (16.8) | 59.4 (17.2) | 61.4 (17.7) | 58.7 (16.6) | 58.3 (16.1) | 59.7 (17.0) | 58.1 (15.7) | 59.5 (16.8) |
| Mean (SD) SGRQ total score | 45.5 (20.6) | 45.0 (18.6) | 47.7 (19.1) | 50.8 (17.5) | 46.6 (19.2) | 50.6 (17.1) | 43.9 (19.5) | 46.5 (18.5) | 51.4 (18.1) | 46.3 (19.0) | 53.7 (17.4) | 47.1 (18.9) |
| Mean (SD) ACQ-5 score | 2.2 (1.3) | 2.2 (1.1) | 2.1 (1.2) | 2.5 (1.2) | 2.2 (1.2) | 2.4 (1.1) | 2.2 (1.1) | 2.1 (1.2) | 2.4 (1.2) | 2.2 (1.2) | 2.5 (1.2) | 2.2 (1.2) |
| Geometric mean (SD of log) blood eosinophil count, cells/μL | 370 (1.13) | 320 (0.93) | 300 (0.90) | 360 (0.87) | 320 (0.96) | 360 (0.85) | 350 (0.98) | 310 (0.90) | 310 (0.96) | 320 (0.96) | 330 (0.81) | 330 (0.95) |
Percentages may not add up to 100, due to rounding
Abbreviations: ACQ Asthma Control Questionnaire, BMI Body mass index, FEV1 Forced expiratory volume in 1 s, OCS Oral corticosteroid, SD Standard deviation, SGRQ St George’s Respiratory Questionnaire
Primary endpoint
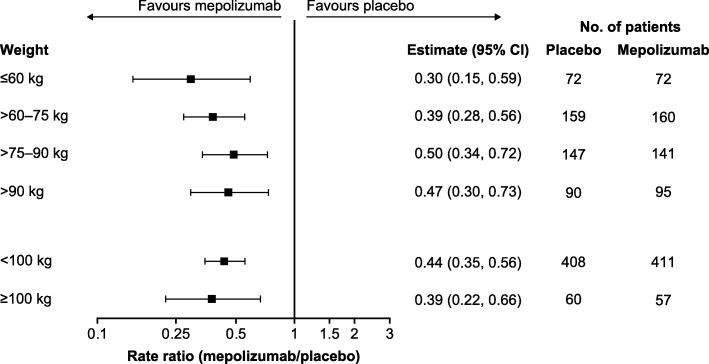
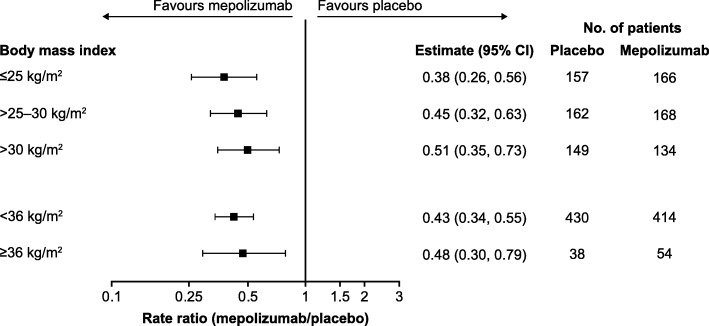
Across all body weight categories and thresholds, mepolizumab 100 mg SC treatment was associated with reductions of 50–70% in the annual rate of clinically significant exacerbations compared with placebo (Fig. 1). Reductions of 49–62% in the annual rate of clinically significant exacerbations were also seen across BMI categories and thresholds with mepolizumab versus placebo (Fig. 2).
Fig. 1.
Ratio of the annual rate of clinically significant exacerbations. Mepolizumab 100 mg SC versus placebo. CI confidence interval, SC subcutaneous
Fig. 2.
Ratio of the annual rate of clinically significant exacerbations. Mepolizumab 100 mg SC versus placebo. BMI body mass index, CI confidence interval, SC subcutaneous
Secondary endpoints
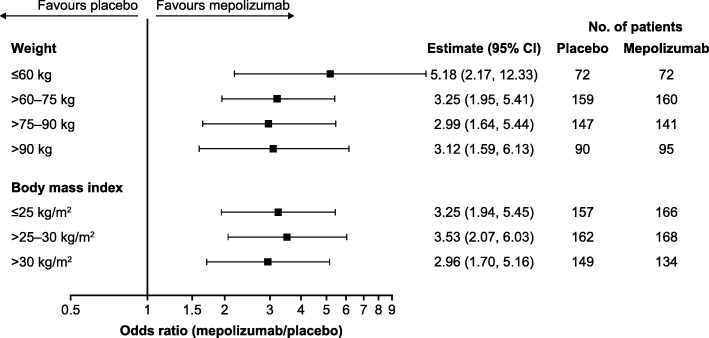
Regardless of body weight category, patients receiving mepolizumab 100 mg SC were more likely to experience no clinically significant exacerbations during the study period than those who received placebo, with odds ratios to placebo ranging between 2.99 (95% confidence interval [CI]: 1.64, 5.44) in the > 75–90 kg subgroup and 5.18 (95% CI: 2.17, 12.33) in the lowest weight subgroup of ≤60 kg (Fig. 3). Similar results were seen across BMI categories, with odds ratios to placebo ranging from 2.96 (95% CI: 1.70, 5.16) in patients in the highest BMI subgroup of BMI > 30 kg/m2 to 3.53 (95% CI: 2.07, 6.03) in those with a BMI > 25–30 kg/m2.
Fig. 3.
Proportion of patients experiencing no clinically significant exacerbation. Mepolizumab 100 mg SC versus placebo. BMI body mass index, CI confidence interval, SC subcutaneous
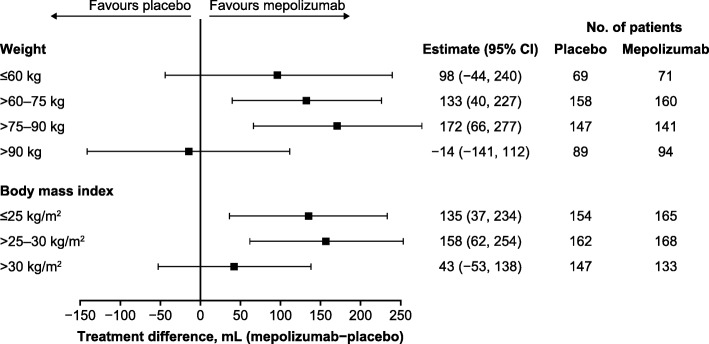
Mepolizumab treatment resulted in an increase from baseline in pre-bronchodilator FEV1 versus placebo in patients with body weight ≤ 60, > 60–75 and > 75–90 kg (treatment difference ranged from 98 to 172 mL), but not in patients with body weight > 90 kg (treatment difference: − 14 mL) (Fig. 4). Across all BMI categories, mepolizumab treatment resulted in an increase from baseline in pre-bronchodilator FEV1 versus placebo, with a smaller effect in the highest BMI category (treatment difference ranged from 43 to 158 mL) (Fig. 4).
Fig. 4.
Change from baseline in pre-bronchodilator FEV1 (mL). Mepolizumab 100 mg SC versus placebo. BMI body mass index, CI confidence interval, FEV1 forced expiratory volume in 1 s, SC subcutaneous
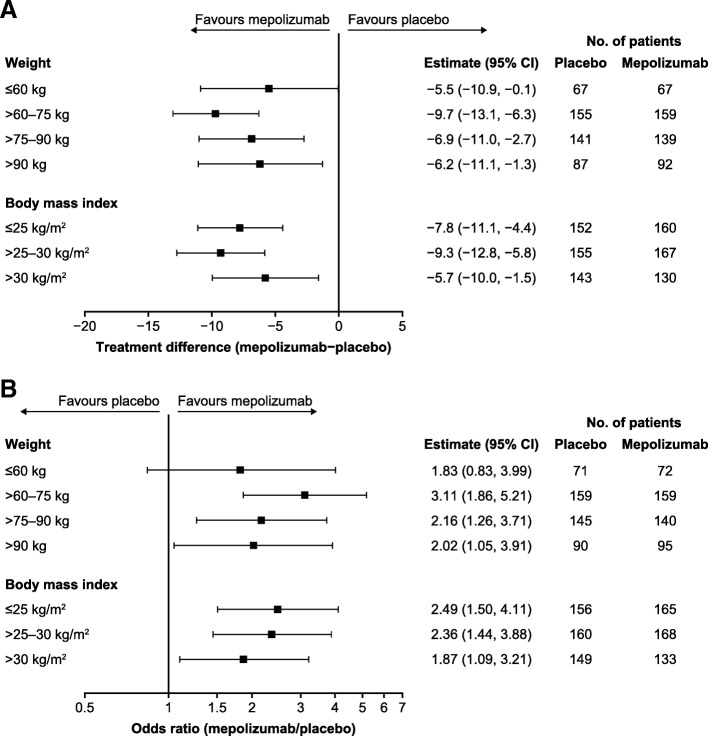
Improvements from baseline with mepolizumab versus placebo were observed in SGRQ total score at study end, irrespective of body weight or BMI category. Treatment differences ranged from − 5.5 to − 9.7 points across weight categories, and from − 5.7 to − 9.3 points across BMI categories (Fig. 5a). In addition, patients receiving mepolizumab treatment were more likely to achieve a clinically meaningful response of ≥4-point reduction (MCID) from baseline in SGRQ total score compared with patients receiving placebo, irrespective of body weight or BMI category (Fig. 5b).
Fig. 5.
Change from baseline in SGRQ total score (a) and proportion of responders achieving a ≥ 4-point change from baseline in SGRQ total score (b). Mepolizumab 100 mg SC versus placebo. BMI body mass index, CI confidence interval, SC subcutaneous, SGRQ St George’s Respiratory Questionnaire
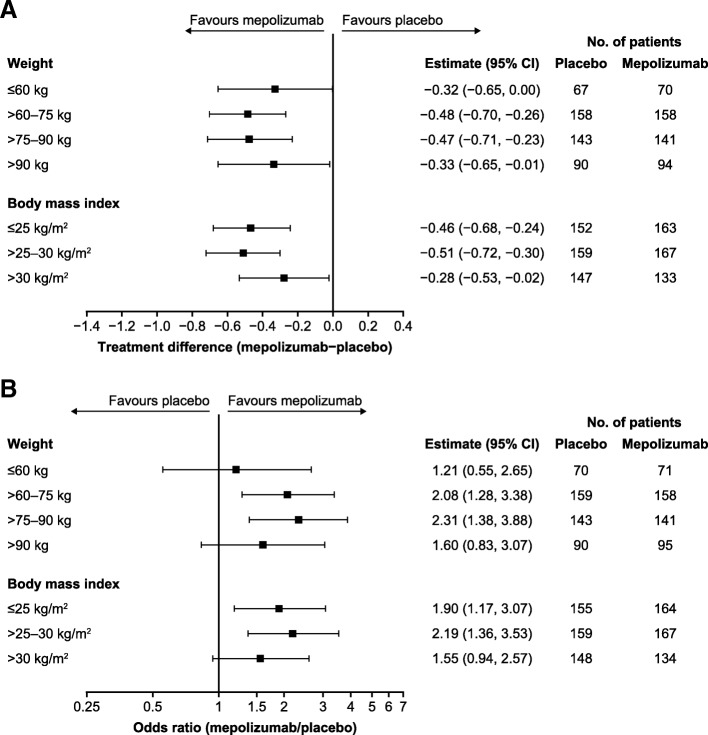
Mepolizumab was associated with improvements from baseline in ACQ-5 score at study end, compared with placebo, across all body weight categories (treatment difference ranged from − 0.32 to − 0.48 points) and all BMI categories (treatment difference ranged from − 0.28 to − 0.51) (Fig. 6a). Patients in all body weight categories were also more likely to achieve a clinically meaningful improvement of ≥0.5-point reduction from baseline in ACQ-5 score (MCID) when treated with mepolizumab versus placebo (odds ratio ranged from 1.21 to 2.31), as were patients across all BMI categories (odds ratio ranged from 1.55 to 2.19) (Fig. 6b).
Fig. 6.
Change from baseline in ACQ-5 score (a) and proportion of responders achieving a ≥ 0.5-point change from baseline in ACQ-5 score (b). Mepolizumab 100 mg SC versus placebo. ACQ-5 Asthma Control Questionnaire, BMI body mass index, CI confidence interval, SC subcutaneous
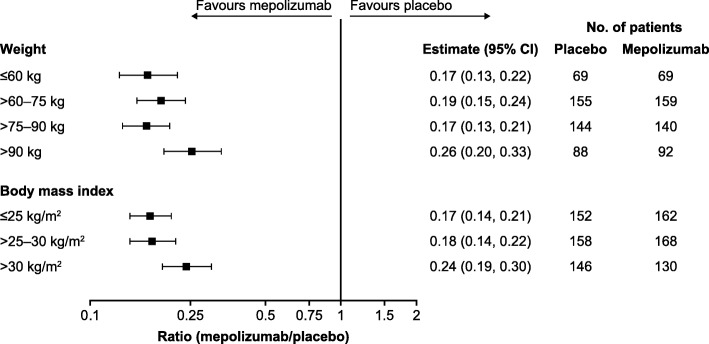
Reductions from baseline in blood eosinophil count were seen in mepolizumab- versus placebo-treated patients across all body weight categories, with reductions ranging from 83% (ratio [95% CI]: 0.17 [0.13, 0.21]) in the > 75–90 kg subgroup to 74% (0.26 [0.20, 0.33]) in the > 90 kg subgroup (Fig. 7). Across BMI categories, mepolizumab treatment resulted in greater reductions from baseline in blood eosinophil count than placebo treatment, ranging from 83% (0.17 [0.14, 0.21]) in the ≤25 kg/m2 subgroup to 76% (0.24 [0.19, 0.30]) in the > 30 kg/m2 subgroup (Fig. 7).
Fig. 7.
Ratio to baseline in blood eosinophil count. Mepolizumab 100 mg SC versus placebo. BMI body mass index, CI confidence interval, SC subcutaneous
Discussion
In this post hoc meta-analysis of the MENSA and MUSCA studies, the licensed dose of mepolizumab (100 mg SC) showed consistent improvements versus placebo in exacerbation rate, HRQoL and asthma control, independent of patients’ body weight or BMI. These data demonstrate comparable efficacy of mepolizumab in patients with either high or low body weight/BMI, and confirm that dose-weight adjustments with mepolizumab are not required, thereby addressing queries regarding the need for higher mepolizumab doses in patients with high body weight/BMI. Our findings reinforce the suitability of a simple, fixed-dose regimen across all ranges of body weight/BMI in eligible patients.
Several novel biologic treatments approved for use in patients with differing severe asthma phenotypes have demonstrated reduced efficacy in patients who are obese. For example, a recent retrospective study in patients with severe asthma (N = 340) found that obesity may reduce the effectiveness of the anti-immunoglobulin E mAb omalizumab, independent of other asthma-influencing factors [15]. In addition, a post hoc pooled analysis of the Phase 3 SIROCCO and CALIMA trials demonstrated that the effects of the anti-IL-5 receptor mAb benralizumab on the annual rate of exacerbations and lung function in patients with severe eosinophilic asthma were less robust in obese individuals than in those who were of normal weight [16]. It is important to note that the DREAM study, which was a double-blind, placebo-controlled trial assessing mepolizumab in patients with severe eosinophilic asthma, showed no dosing effect over a 10-fold dose range of mepolizumab on exacerbation rate and other outcomes [17]. For this reason it was important to further investigate whether there was any relationship between mepolizumab efficacy and body weight/BMI in patients with severe eosinophilic asthma.
To date, the effect of mepolizumab 100 mg SC in patients with high body weight/BMI has not been extensively investigated. However, a post hoc analysis of the DREAM study suggested that mepolizumab remains efficacious in these individuals [18, 19]. In this analysis responder subgroups were identified using cluster analysis; the cluster demonstrating greatest response to mepolizumab was an obese, eosinophilic group with airway reversibility [19]. Moreover, a post hoc analysis of the MENSA and DREAM studies showed that treatment with mepolizumab (doses of 75, 250 or 750 mg IV or 100 mg SC) resulted in similar exacerbation rate reductions across weight categories of ≤60 kg, > 60–≤75 kg, > 75–≤90 kg and > 90 kg, with no discernible trend noted in exacerbation reductions with the 250 mg and 750 mg IV doses of mepolizumab, even at the higher weight categories (Additional file 1: Table S1) [20]. In the current analysis, mepolizumab treatment was associated with reduced exacerbation rates across all body weight and BMI categories, versus placebo. In addition, mepolizumab induced an increase from baseline in pre-bronchodilator FEV1 versus placebo in all body weight categories except > 90 kg. A similar trend was observed in the BMI categories. This is consistent with results from post hoc analyses of data from Phase 3 trials of benralizumab [16, 21]. For example, it has been shown that the increase in pre-bronchodilator FEV1 following benralizumab treatment was lower in patients with extremely high body weight (≥115 kg) compared with those with a body weight < 115 kg [21]. It is possible that mechanical factors causing airway restriction may be responsible for a reduced treatment response in obese patients [15], although it should also be noted that low patient numbers in the highest body weight category may have contributed to this observation in our analysis.
Consistent improvements in both SGRQ total score and ACQ-5 score were also seen with mepolizumab versus placebo across all body weight and BMI categories, including patients with body weight > 90 kg. Although the effects of mepolizumab on measures of HRQoL and asthma control have been reported several times previously in populations with severe eosinophilic asthma [7, 8], this is the first analysis to demonstrate a consistent effect on these parameters across all body weight and BMI categories. Given the particularly poor QoL and reduced asthma control in patients with asthma and comorbid obesity [22], this is a clinically important finding.
Also of clinical relevance is the consistent and sustained reduction in blood eosinophil count with mepolizumab versus placebo shown in this study, regardless of body weight/BMI. This finding builds upon a substantial body of evidence demonstrating mepolizumab-induced reductions in blood eosinophil levels and a correlation between reduced blood eosinophils and improvements in clinical parameters such as exacerbations and lung function [7, 8]. Of particular importance in this analysis, obesity was previously thought to be associated with a non-eosinophilic asthma phenotype that is typically unresponsive to steroids and therefore not considered to be eligible for treatment with mepolizumab [18]. However, more recently, elevated sputum IL-5 and submucosal and sputum eosinophils have been reported in obese patients with asthma [18, 23, 24]. The baseline patient characteristics in the current study are in line with this finding, with no obvious trend for lower blood eosinophil counts in patients with higher body weight or BMI, albeit in a population of patients who satisfied inclusion criteria pertaining to eosinophilic asthma. Together, these data suggest that patients with high body weight/BMI can have raised blood eosinophil levels and therefore be eligible for mepolizumab treatment, and further, that mepolizumab 100 mg SC can be efficacious in this population. One important consideration is the evidence that inflammatory biomarkers, including blood eosinophils, may be less predictive of airway eosinophilia in obese patients [25]. Nonetheless, the current analysis has demonstrated improvements in a range of clinical parameters in a population of patients with severe eosinophilic asthma across body weight and BMI categories.
Body weight typically influences the exposure of biologics [26]. However, whether this exposure difference translates into a meaningful efficacy difference also depends on the drug-to-target ratio. For omalizumab to adequately neutralise immunoglobulin E levels, a weight-based dosing strategy was deemed necessary [27]. By contrast, neutralisation of IL-5 levels with a fixed-dose regimen of mepolizumab 100 mg SC was found to be efficacious and sufficient over the expected body weight/BMI range in adults and adolescents. A previously reported analysis showed that the efficacy dose–response was consistent with that of the well-defined pharmacological dose–response, in which the half-maximal effect was estimated at 11 mg SC [28], which is well below the licensed dose of 100 mg SC. Unlike mepolizumab, the clinical development programme for reslizumab only investigated a mg/kg dosing regimen and reslizumab is therefore dosed according to body weight [29].
Combining data from two large randomised, controlled trials in the current analysis provided a large sample in which to determine the effect of mepolizumab across a range of body compositions. However, there are several limitations that should be considered. First, the post hoc nature of the analysis should be considered when interpreting the findings. In addition, the number of patients varied substantially between subgroups, with smaller patient numbers in the highest body weight and BMI subgroups. We also did not investigate whether there were any differences in safety findings between the subgroups, although previous studies have demonstrated that mepolizumab is well tolerated with minimal immunogenic potential [6–8]. Despite these limitations, our findings provide valuable insights into the use of mepolizumab in patients with severe eosinophilic asthma.
Conclusions
In summary, results from this post hoc analysis of the MENSA and MUSCA studies demonstrate that mepolizumab 100 mg SC is associated with improvements in exacerbation rate, HRQoL and asthma control in patients with severe eosinophilic asthma, across a range of patient body weights and BMI categories. The reason for a lower improvement in FEV1 in the highest body weight category remains to be investigated. Nonetheless, our findings support the use of a simple, fixed-dose regimen of mepolizumab 100 mg SC for treating patients with severe eosinophilic asthma.
Additional file
Table S1. Rate ratio of clinically significant exacerbations by body weight in the MENSA and DREAM studies (intent-to-treat population). (PDF 590 kb)
Acknowledgements
This post hoc meta-analysis (GSK ID: 208115) and the parent studies (MENSA, MEA115588/NCT01691521; MUSCA, 200862/NCT02281318) were funded by GlaxoSmithKline (GSK). Editorial support (in the form of writing assistance, including development of the initial draft from the study report, assembling tables and figures, collating author comments, grammatical editing and referencing) was provided by Laura Pearce, PhD, and Roisin McCorkell, MSc, of Fishawack Indicia Ltd., UK, and was funded by GSK.
Abbreviations
- ACQ-5
Asthma Control Questionnaire-5
- BMI
Body mass index
- FEV1
Forced expiratory volume in 1 s
- HRQoL
Health-related quality of life
- ICS
Inhaled corticosteroids
- IL
Interleukin
- IV
Intravenously
- mAb
monoclonal antibody
- OCS
Oral corticosteroids
- SC
Subcutaneously
- SGRQ
St George’s Respiratory Questionnaire
Authors’ contributions
DJB and FCA contributed to the conception and design of the analysis. CT was involved in the acquisition of the data during the primary studies. All authors contributed to the analysis and interpretation of the data, development of the manuscript and approval of the final draft to be published.
Funding
This post hoc meta-analysis (GSK ID: 208115) and the parent studies (MENSA, MEA115588/NCT01691521; MUSCA, 200862/NCT02281318) were funded by GSK. Editorial support (in the form of writing assistance, including development of the initial draft based on author direction, assembling tables and figures, collating authors’ comments, grammatical editing and referencing) was funded by GSK. All authors had roles in the conception, design and interpretation of the analysis. All authors participated in the development of the manuscript and had access to the data from the studies. The decision to submit for publication was that of the authors alone. The sponsor did not place any restrictions on access to the data or on the statements made in the manuscript. The corresponding author had final responsibility for the decision to submit for publication.
Availability of data and materials
Anonymised individual participant data from the studies listed within this publication and their associated documents can be requested for further research from www.clinicalstudydatarequest.com.
Ethics approval and consent to participate
All patients provided written informed consent for MENSA and MUSCA. The original MENSA and MUSCA study protocols (on which this analysis was based) were approved by local or national research ethics committees. Both MENSA and MUSCA were conducted in accordance with the ethical principles of the Declaration of Helsinki, the International Conference on Harmonisation Good Clinical Practice guidelines, and the applicable country-specific regulatory requirements.
Consent for publication
Not applicable.
Competing interests
DJB, ESB, SWY and NK are employees of GSK and hold stocks/shares in GSK. FCA was an employee of GSK at the time of this analysis and holds stocks/shares in GSK. AP has received grants, personal fees and non-financial support and other from AstraZeneca, Teva, Mundipharma, GSK, Chiesi and Boehringer Ingelheim; has received personal fees and non-financial support from Novartis, Menarini and Zambon; and has received grants from Sanofi. CT has received fees from GSK, AstraZeneca, Novartis, Teva, Sanofi, Genzyme and Roche (consultancy, advisory boards) and was an investigator in trials involving GSK, AstraZeneca, Novartis, Sanofi, Roche and Boehringer Ingelheim.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Global asthma report. http://globalasthmareport.org/. Accessed 16 Oct 2018.
- 2.Chung KF, Wenzel SE, Brozek JL, Bush A, Castro M, Sterk PJ, Adcock IM, Bateman ED, Bel EH, Bleecker ER, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43:343–373. doi: 10.1183/09031936.00202013. [DOI] [PubMed] [Google Scholar]
- 3.Wenzel S. Severe asthma: from characteristics to phenotypes to endotypes. Clin Exp Allergy. 2012;42:650–658. doi: 10.1111/j.1365-2222.2011.03929.x. [DOI] [PubMed] [Google Scholar]
- 4.Mepolizumab (NUCALA) US prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/125526Orig1s000Lbl.pdf. Accessed 4 Dec 2018.
- 5.Mepolizumab (NUCALA) EU summary of product characteristics. https://www.ema.europa.eu/documents/product-information/nucala-epar-product-information_en.pdf. Accessed 4 Dec 2018.
- 6.Bel EH, Wenzel SE, Thompson PJ, Prazma CM, Keene ON, Yancey SW, Ortega HG, Pavord ID, Investigators S. Oral glucocorticoid-sparing effect of mepolizumab in eosinophilic asthma. N Engl J Med. 2014;371:1189–1197. doi: 10.1056/NEJMoa1403291. [DOI] [PubMed] [Google Scholar]
- 7.Chupp GL, Bradford ES, Albers FC, Bratton DJ, Wang-Jairaj J, Nelsen LM, Trevor JL, Magnan A, Ten Brinke A. Efficacy of mepolizumab add-on therapy on health-related quality of life and markers of asthma control in severe eosinophilic asthma (MUSCA): a randomised, double-blind, placebo-controlled, parallel-group, multicentre, phase 3b trial. Lancet Respir Med. 2017;5:390–400. doi: 10.1016/S2213-2600(17)30125-X. [DOI] [PubMed] [Google Scholar]
- 8.Ortega HG, Liu MC, Pavord ID, Brusselle GG, FitzGerald JM, Chetta A, Humbert M, Katz LE, Keene ON, Yancey SW, et al. Mepolizumab treatment in patients with severe eosinophilic asthma. N Engl J Med. 2014;371:1198–1207. doi: 10.1056/NEJMoa1403290. [DOI] [PubMed] [Google Scholar]
- 9.Hendrikx J, Haanen J, Voest EE, Schellens JHM, Huitema ADR, Beijnen JH. Fixed dosing of monoclonal antibodies in oncology. Oncologist. 2017;22:1212–1221. doi: 10.1634/theoncologist.2017-0167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garcia-Rio F, Alvarez-Puebla MJ, De Esteban I, Barranco P, Olaguibel JM. Obesity and asthma. Key clinical questions. J Investig Allergol Clin Immunol. 2018;29. 10.18176/jiaci.0316. [DOI] [PubMed]
- 11.Smit C, De Hoogd S, Bruggemann RJM, Knibbe CAJ. Obesity and drug pharmacology: a review of the influence of obesity on pharmacokinetic and pharmacodynamic parameters. Expert Opin Drug Metab Toxicol. 2018;14:275–285. doi: 10.1080/17425255.2018.1440287. [DOI] [PubMed] [Google Scholar]
- 12.Jones PW. Interpreting thresholds for a clinically significant change in health status in asthma and COPD. Eur Respir J. 2002;19:398–404. doi: 10.1183/09031936.02.00063702. [DOI] [PubMed] [Google Scholar]
- 13.Cloutier MM, Schatz M, Castro M, Clark N, Kelly HW, Mangione-Smith R, Sheller J, Sorkness C, Stoloff S, Gergen P. Asthma outcomes: composite scores of asthma control. J Allergy Clin Immunol. 2012;129:S24–S33. doi: 10.1016/j.jaci.2011.12.980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.GSK Clinical Studies Register. https://www.gsk-studyregister.com/study/6079. Accessed 19 July 2019.
- 15.Sposato B, Scalese M, Milanese M, Masieri S, Cavaliere C, Latorre M, Scichilone N, Matucci A, Vultaggio A, Ricci A, et al. Factors reducing omalizumab response in severe asthma. Eur J Intern Med. 2018;52:78–85. doi: 10.1016/j.ejim.2018.01.026. [DOI] [PubMed] [Google Scholar]
- 16.Trudo F, Hirsch I, Gopalan G, Martin U. Impact of body mass index on efficacy of benralizumab in patients with severe, uncontrolled eosinophilic asthma: pooled analysis of the SIROCCO and CALIMA trials. Am J Respir Crit Care Med. 2018;197:A2490. [Google Scholar]
- 17.Pavord ID, Korn S, Howarth P, Bleecker ER, Buhl R, Keene ON, Ortega H, Chanez P. Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo-controlled trial. Lancet. 2012;380:651–659. doi: 10.1016/S0140-6736(12)60988-X. [DOI] [PubMed] [Google Scholar]
- 18.Haldar P. Patient profiles and clinical utility of mepolizumab in severe eosinophilic asthma. Biologics. 2017;11:81–95. doi: 10.2147/BTT.S93954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ortega H, Li H, Suruki R, Albers F, Gordon D, Yancey S. Cluster analysis and characterization of response to mepolizumab. A step closer to personalized medicine for patients with severe asthma. Ann Am Thorac Soc. 2014;11:1011–1017. doi: 10.1513/AnnalsATS.201312-454OC. [DOI] [PubMed] [Google Scholar]
- 20.Ortega H., Albers F., Llanos-Ackert J., Bradford E., Price R., Pouliquen I., Castro M. P506 Impact of weight on the efficacy of mepolizumab in patients with severe eosinophilic asthma. Annals of Allergy, Asthma & Immunology. 2017;119(5):e3–e4. doi: 10.1016/j.anai.2017.09.072. [DOI] [Google Scholar]
- 21.Chia YL, Yan L, Yu B, Wang B, Barker P, Goldman M, Roskos L. Relationship between benralizumab exposure and efficacy for patients with severe eosinophilic asthma. Clin Pharmacol Ther. 2019. 10.1002/cpt.1371. [DOI] [PMC free article] [PubMed]
- 22.Novosad S, Khan S, Wolfe B, Khan A. Role of obesity in asthma control, the obesity-asthma phenotype. J Allergy (Cairo) 2013;2013:538642. doi: 10.1155/2013/538642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Desai D, Newby C, Symon FA, Haldar P, Shah S, Gupta S, Bafadhel M, Singapuri A, Siddiqui S, Woods J, et al. Elevated sputum interleukin-5 and submucosal eosinophilia in obese individuals with severe asthma. Am J Respir Crit Care Med. 2013;188:657–663. doi: 10.1164/rccm.201208-1470OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Scott HA, Gibson PG, Garg ML, Wood LG. Airway inflammation is augmented by obesity and fatty acids in asthma. Eur Respir J. 2011;38:594–602. doi: 10.1183/09031936.00139810. [DOI] [PubMed] [Google Scholar]
- 25.Lugogo N, Green CL, Agada N, Zhang S, Meghdadpour S, Zhou R, Yang S, Anstrom KJ, Israel E, Martin R, et al. Obesity's effect on asthma extends to diagnostic criteria. J Allergy Clin Immunol. 2018;141:1096–1104. doi: 10.1016/j.jaci.2017.04.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dirks NL, Meibohm B. Population pharmacokinetics of therapeutic monoclonal antibodies. Clin Pharmacokinet. 2010;49:633–659. doi: 10.2165/11535960-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 27.Lowe PJ, Georgiou P, Canvin J. Revision of omalizumab dosing table for dosing every 4 instead of 2 weeks for specific ranges of bodyweight and baseline IgE. Regul Toxicol Pharmacol. 2015;71:68–77. doi: 10.1016/j.yrtph.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 28.Pouliquen IJ, Kornmann O, Barton SV, Price JA, Ortega HG. Characterization of the relationship between dose and blood eosinophil response following subcutaneous administration of mepolizumab. Int J Clin Pharmacol Ther. 2015;53:1015–1027. doi: 10.5414/CP202446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reslizumab (CINQAIR) US prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/761033lbl.pdf. Accessed 21 Mar 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Rate ratio of clinically significant exacerbations by body weight in the MENSA and DREAM studies (intent-to-treat population). (PDF 590 kb)
Data Availability Statement
Anonymised individual participant data from the studies listed within this publication and their associated documents can be requested for further research from www.clinicalstudydatarequest.com.