Abstract
Background
Ensuring universal access to malaria diagnosis and treatment is a key component of Pillar 1 of the World Health Organization Global Technical Strategy for Malaria 2016–2030. To achieve this goal it is essential to know the types of facilities where the population seeks care as well as the malaria service readiness of these facilities in endemic countries.
Methods
To investigate the utilization and provision of malaria services, data on the sources of advice or treatment in children under 5 years with fever from the household-based Demographic and Health Surveys (DHS) and on the components of malaria service readiness from the facility-based Service Provision Assessment (SPA) surveys were examined in Malawi, Senegal and Tanzania. Facilities categorized as malaria-service ready were those with: (1) personnel trained in either malaria rapid diagnostic testing (RDT), microscopy or case management/treatment of malaria in children; (2) national guidelines for the diagnosis and treatment of malaria; (3) diagnostic capacity (available RDT tests or microscopy equipment as well as staff trained in its use); and, (4) unexpired artemisinin-based combination therapy (ACT) available on the day of the survey.
Results
In all three countries primary-level facilities (health centre/health post/health clinic) were the type of facility most used for care of febrile children. However, only 69% of these facilities in Senegal, 32% in Malawi and 19% in Tanzania were classified as malaria-service ready. Of the four components of malaria-service readiness in the facilities most frequented by febrile children, diagnostic capacity was the weakest area in all three countries, followed by trained personnel. All three countries performed well in the availability of ACT.
Conclusions
This analysis highlights the need to improve the malaria-service readiness of facilities in all three countries. More effort should be focused on facilities that are commonly used for care of fever, especially in the areas of malaria diagnostic capacity and provider training. It is essential for policymakers to consider the malaria-service readiness of primary healthcare facilities when allocating resources. This is particularly important in limited-resource settings to ensure that the facilities most visited for care are properly equipped to provide diagnosis and treatment for malaria.
Keywords: Malaria, Care seeking, Malaria-service readiness, Fever, Malawi, Tanzania, Senegal
Background
Ensuring universal access to malaria diagnosis and treatment is a key component of Pillar 1 of the World Health Organization (WHO) Global Technical Strategy for Malaria 2016–2030. To achieve universal access to malaria diagnosis and treatment, it is essential to ensure that malaria services are available and accessible to the population at risk. This requires an understanding of care-seeking practices by the at-risk population, as well as information about the conditions of the health facilities and the quality of services offered by health providers.
Prior research has shown that the affordability, acceptability and availability of services are strong determinants of a population’s care-seeking behaviour and, therefore, of service utilization [1–4]. While in many countries the national policy is to provide free treatment for children under 5 years of age, affordability remains a problem; financial constraints can be a major barrier for seeking care, although it is hard to quantify the indirect costs of seeking care, such as transport to the health facility or losing a day’s work to attend the facility [3, 5, 6]. Regarding acceptability of services, both health facility determinants and individual sociocultural factors affect a child’s caregiver’s decision to seek treatment. In some settings the characteristics of health services have been identified as barriers to care-seeking, including long waiting times, poor communication between providers and patients, and patient’s perceptions of effectiveness of treatment [7–10]. Individual factors include caregiver’s limited understanding of disease causation, symptomatology and severity of illness [11–14]. Availability of services at a facility can also affect the use of malaria services. Availability, or physical access, refers to whether health services and providers are supplied within reasonable reach of the individuals who need them, and whether the services meet people’s needs. Key influences on availability and access include facility hours of operation, drug shortages, geographic proximity, and ease of attending the facility [1, 3, 8, 15, 16].
The readiness of a facility to provide malaria services has multiple determinants. Managing authority of health facility (public or private) and the level of the health facility (primary, secondary) have been shown to affect malaria service readiness [17]. When comparing the malaria-service readiness of public versus private facilities, some studies have highlighted inadequacies of the formal public health sector to guarantee appropriate levels of drugs, as well as to provide training and guidelines to service providers [3, 18–21]. Private facilities face such challenges as inadequate oversite and monitoring, prescription of treatments that do not conform to the national policy, and less malaria rapid diagnostic test (RDT) availability compared with public facilities [22–26]. Malaria-service readiness is also associated with the level of the health facility. Historically, lower-level facilities (such as health posts) have not had sufficient diagnostic capacity because of lack of microscopes or specialized staff trained in microscopy [27]. However, the introduction of RDTs has removed a barrier for service readiness for lower-level health facilities, because these tests make parasitological diagnosis feasible at lower levels and lead to improved targeting of malaria treatment [28]. In addition, it has been widely shown that lower-level care providers, such as community health workers, when appropriately trained and supervised, are capable of delivering high-quality care for uncomplicated malaria cases with RDTs to diagnose cases [29] and administration of artemisinin-based combination therapy (ACT) medicines [30, 31].
This study investigates the utilization and provision of malaria services by examining data on the source of advice or treatment in children age under 5 years with fever from the household-based Demographic and Health Surveys (DHS) surveys and data on provision of care from the facility-based Service Provision Assessment (SPA) surveys from Malawi, Senegal and Tanzania. The results will allow for better prioritization of interventions that can improve service readiness in the facilities where most care seeking for malaria occurs.
Study setting
Malawi
In Malawi, primary-level care is delivered at health posts, dispensaries, maternity facilities, health centres, and community or rural hospitals, where primary and preventive care services are provided primarily by community health workers. Secondary-level care is provided at district hospitals, which serve as referral facilities that provide inpatient and outpatient services. Central hospitals that provide tertiary-level services serve as referral hospitals for the district hospitals. With the policy of decentralization, the health system gave authority to the district health management teams to deliver secondary and primary health services at the district level [32].
Malawi’s private-sector facilities include not-for-profit and for-profit facilities. Private not-for-profit facilities include independent church-affiliated facilities that belong to the Christian Health Association of Malawi (CHAM) and are primarily located in rural areas. These facilities charge user fees for care other than basic preventive and curative care services for which they are contracted by district health officers to provide free of charge. The private for-profit sector also operates health facilities and health programmes. The public sector supports private-sector facilities and faith-based organizations (FBOs) by providing staff training, public sector staffing for facilities, supervision, medicines, and vaccines [32].
Senegal
The operations of Senegal’s health system are implemented at district level. Each of the 76 health districts has at least one health centre, which is a secondary health facility with a medical team that provides direct care and oversees the district’s prevention efforts. Health centres are attached to the district’s health posts, staffed by nurse or midwife, and generally serve as the first level of contact with the population. Health posts are responsible for a number of health huts, which have trained community health workers and the necessary structure and equipment for providing basic services that include the diagnosis and treatment of uncomplicated malaria. Since 2008, community case management of malaria can be provided by home care providers, who are lower-level community health workers who work from their own homes rather than in a health facility [33].
Tertiary facilities include hospital centres that provide specialized care. These hospitals, which are found at the regional, departmental or communal level, typically provide care coverage for approximately 150,000 residents. There are also seven national hospital centres in Dakar. The health system has a network of regional pharmacies that supply the facilities and care providers of the corresponding regions. These regional pharmacies receive supplies from the national pharmacy. In addition to public sector facilities, there are also a number of private clinics and health posts throughout the country [33].
Tanzania
A central district government structure is the basis of Mainland Tanzania’s National Health System. In this structure, the Ministry of Health, Community Development, Gender, Elderly and Children (MoHCDEC), the President’s Office of Regional Administration, and the local government share the responsibility for the delivery of public health services. The central level develops policies and guidelines, which are implemented by the regional health teams. Health facilities include dispensaries, health centres and hospitals, which operate in a hierarchical manner. The health facilities may be administered by the government, faith-based voluntary organizations, or other private organizations, and may be parastatal in nature. Dispensaries at the primary level in villages serve between 6000 and 10,000 residents, secondary-level health centres serve between 50,000 and 80,000 in a ward, and district hospitals provide tertiary-level care for more than 250,000 residents and refer cases to the regional and consultant hospitals [34]. Pharmaceutical services are provided through public-sector and FBO health facilities, private pharmacies, and accredited drug dispensing outlets (ADDOs) [34].
In Zanzibar, health services are delivered through public, private (both for-profit and non-profit), and additional government health facilities administered by military or defence forces. In the hierarchical system in Zanzibar, primary level care is provided at primary health care units (PHCUs) and primary health care cottages (PHCCs) that also provide inpatient care and X-ray services. At secondary level, the district and regional hospitals provide care. Specialized hospitals provide care at tertiary level. Under the policy of devolution, the provision of public health services, particularly preventive services, has been delegated to district health management teams in Zanzibar’s 11 districts [34].
Methods
The study examined data on use of malaria services for children under 5 years of age with fever from the household-based Demographic and Health Surveys (DHS) and data on service readiness from the facility-based Service Provision Assessment (SPA) surveys conducted in Malawi, Senegal and Tanzania. The analysis focused on these three countries because in each country the fieldwork for the DHS and the SPA was completed within 1 year of each other. Surveys analysed were the 2013–2014 Malawi SPA and 2015–2016 Malawi DHS, the 2016 Senegal Continuous SPA and 2016 Senegal Continuous DHS, and the 2014–2015 Tanzania SPA and 2015–2016 Tanzania DHS-MIS [34–39].
DHS surveys are nationally representative household surveys that provide data for a wide range of monitoring and impact evaluation indicators in the areas of population, health and nutrition. The DHS surveys have large sample sizes (usually between 5000 and 30,000 households). In malaria-endemic countries many DHS surveys include questions about malaria in both the Household Questionnaire and Woman’s Questionnaire. Responses to these questions generate data that can be used to assess progress in the core household malaria indicators that are detailed in the Roll Back Malaria Partnership to End Malaria (RBM) guidance document, Household Survey Indicators for Malaria Control [40].
This analysis uses the DHS survey indicator “proportion of children under age 5 with fever in the previous 2 weeks for whom advice or treatment was sought”. Although non-specific for malaria, fever in children is often a prompt for care seeking due to perceived risk of serious illness. In malaria-endemic countries, facilities receiving sick children should be following integrated management of childhood illness (IMCI) protocols, which include diagnosis and treatment of malaria.
SPA surveys are sample surveys of formal-sector health facilities. Typically, the SPA surveys collect data from 400 to 700 facilities selected from a comprehensive list of health facilities in a country (sampling frame), categorized by facility type, managing authority (public and non-public), and geographic region. The SPA surveys include four main questionnaires: (1) inventory questionnaire; (2) health worker or provider questionnaire; (3) observation protocols; and, (4) exit interview questionnaire. This analysis focuses on data from the inventory questionnaire and the health worker or provider questionnaire.
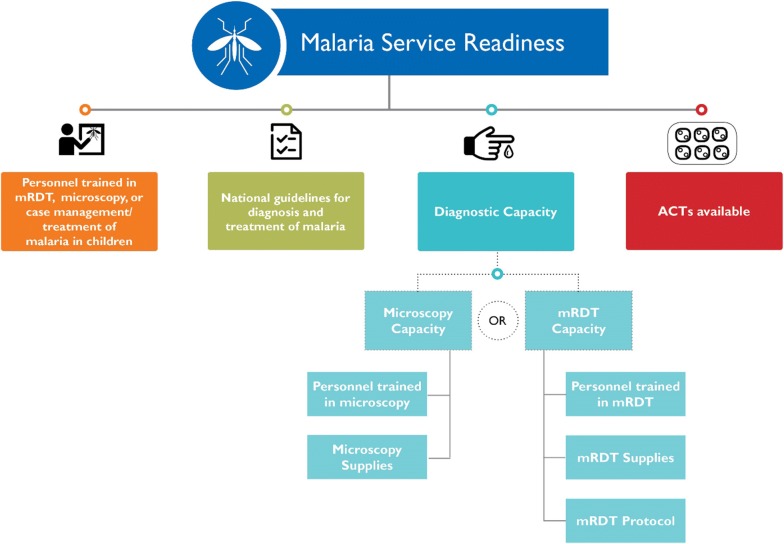
The facility-level indicator examined in this analysis is the proportion of facilities that are categorized as malaria-service ready as defined by the WHO Service Availability and Readiness Assessment (SARA) [41]. This indicator assesses the ability of a facility to provide sufficient care for the diagnosis and treatment of malaria. Facilities categorized as malaria-service ready are those with: (1) trained personnel (adequate training is defined as a facility having at least one provider of malaria services who reported having received in-service training during the 24 months before the survey in either RDT, microscopy or case management and treatment of malaria in children); (2) national guidelines for the diagnosis and treatment of malaria; (3) malaria diagnostic capacity with valid RDT tests or microscopy equipment (available equipment as well as staff trained in its use); and, (4) unexpired ACT medicine available on the day of the survey [41] (Fig. 1). As seen in Fig. 1, malaria diagnostic capacity is a composite indicator defined as a facility having microscopy diagnostic capacity or RDT diagnostic capacity. Microscopy diagnostic capacity is defined as a facility having a functioning microscope with glass slides and relevant stains, in addition to at least one health provider who received training on microscopy during the 24 months before the survey. Similarly, RDT diagnostic capacity is defined as a facility having unexpired malaria RDT kits, at least one health provider who received RDT training in the 24 months before the survey, and the facility having an instructional protocol for performing a RDT. It should be noted that the definition of malaria-service readiness is tailored towards non-severe paediatric malaria cases since it does not include the availability of pre-referral medication or severe malaria treatments (e.g., rectal artesunate or injectable anti-malarials for severe cases).
Fig. 1.
Components of malaria-service readiness
The SPA and DHS are independent of each other, meaning that there are no linkages between specific facilities listed in the SPA and DHS surveys. Without this linkage, it is not possible to know the service readiness of the exact facility where the child’s caregiver sought advice and treatment for their child with a fever. Since linkage of DHS and SPA surveys is not possible, this analysis provides an overview of the malaria service readiness (according to SPA surveys) of the specific facility categories where caregivers most frequently sought care for children under age 5 years with fever (according to the DHS surveys).
In order to examine the types of facilities where individuals tend to seek care and the malaria-service readiness of those facilities, the study needed to harmonize categories of facility types between the DHS and SPA surveys, to allow for comparisons between care seeking and provision of malaria services at specific facility types. Generally, the DHS questionnaire groups health facilities by public, religious, private, and other sources, while the SPA categorizes facilities by managing authority: government, private, non-governmental organization (NGO), religious (and facility level) hospital, health centre, dispensary, clinic. The facility types were harmonized (considering managing authority and facility level) between the DHS and SPA surveys in order to examine the types of facilities where individuals seek care and the malaria service readiness of those facilities (Table 1). Efforts were made to group facilities by facility level, although this was not possible in all cases due to sample size.
Table 1.
Standardized health facilities
| Standardized name | DHS facilities | SPA facilities |
|---|---|---|
| Malawi | 2015–2016 Malawi DHS | 2013–2014 Malawi SPA |
| Government hospital | Government hospital |
Government/public: central hospital Government/public: district hospital Government/public: rural/community hospital Government/public: other hospital |
| Government health centre | Government health centre | Government/public: health centre |
| Government health post or mobile clinic |
Government health post/outreach Government mobile clinic Government HSA |
Government/public: maternity Government/public: dispensary Government/public: clinic Government/public: health post |
| Private facility |
Private hospital/clinic Private pharmacy Private doctor Private mobile clinic Private fieldworker/CHW Other private medical sector |
Private for profit: other hospital Private for profit: health centre Private for profit: maternity Private for profit: dispensary Private for profit: clinic NGO: other hospital NGO: health centre NGO: clinic Company: health centre Company: dispensary Company: clinic |
| Christian health association/mission/faith-based |
CHAM/mission hospital CHAM/mission health centre |
CHAM: rural/community hospital CHAM: other hospital CHAM: health centre CHAM: maternity CHAM: dispensary CHAM: clinic CHAM: health post Mission/faith-based (other than CHAM): Other hospital Mission/faith-based (other than CHAM): Clinic |
| Any other source |
BLM Shop Traditional practitioner Market Itinerant drug seller Youth drop-in centre Other |
No SPA equivalent |
| Senegal | 2016 Senegal Continuous DHS | 2016 Senegal Continuous SPA |
| Government hospital or health centre |
Government hospital Government health centre |
Government/public: hospital Government/public: health centre |
| Government health post or mobile clinic |
Government health post Government mobile team |
Government/public: clinic |
| Government health hut |
Other public sector Country specific public sector |
Government/public: case de santé |
| Private facility |
Private hospital/clinic Private pharmacy Private community health worker Other private medical |
NGO/private not for profit: hospital NGO/private not for profit: health center NGO/private not for profit: clinic Private for profit: hospital Private for profit: health centre Private for profit: clinic |
| Any other source |
Shop Traditional practitioner Country-specific other sector Other |
No SPA equivalent |
| Tanzania | 2015–2016 Tanzania DHS-MIS | 2014–2015 Tanzania SPA |
| Government hospital |
National/zonal referral/specialized hospital Referral regional hospital Regional hospital District hospital |
Government/public: national referral hospital Government/public: regional hospital Government/public: district hospital Government/public: district-designated hospital Government/public: other hospital Parastatal: regional hospital Parastatal: other hospital |
| Government health centre | Public health centre |
Government/public: health centre Parastatal: health center |
| Government clinic/dispensary |
Public clinic Public dispensary Public CHW |
Government/public: clinic Government/public: dispensary Parastatal: dispensary |
| Private facility |
Private hospital Private specialized hospital Private health centre Private clinic Private dispensary |
Private: other hospital Private: health centre Private: clinic Private: dispensary |
| Mission/faith-based |
Religious/voluntary referral spec. hospital religious/voluntary hospital religious/voluntary district hospital religious/voluntary health centre religious/voluntary clinic religious/voluntary dispensary |
Mission/faith-based: national referral Mission/faith-based: regional hospital Mission/faith-based: district hospital Mission/faith-based: district-designated hospital Mission/faith-based: other hospital Mission/faith-based: health centre Mission/faith-based: clinic Mission/faith-based: dispensary |
| Any other source |
Pharmacy ADDO NGO Other |
No SPA equivalent |
HSA Health Surveillance Assistants, CHAM Christian Health Association of Malawi, BLM Banja La Mtsogolo (program established by Marie Stopes International), ADDO Accredited Drug Dispensing Outlet
One limitation of the SPA survey is that it only captures the services provided by formal-sector health facilities. SPA surveys do not include some private health care providers (individual doctors operating outside sampled facilities, private pharmacies), community-based care (community health workers (CHWs) who provide integrated community case management (iCCM)), or those in the informal health care sector (traditional healers, markets, shops). Although the DHS questionnaire includes options for private healthcare providers and informal healthcare providers, it is impossible to compare data on these facilities with the data in the SPA. In this analysis, therefore, private healthcare providers and providers in the informal healthcare sectors are identified as ‘any other source’.
The study includes a country-level descriptive analysis with 95% confidence intervals of both DHS and SPA data. Estimates from both DHS and SPA surveys were adjusted for complex survey design and relevant sample weights. All analyses were conducted using Stata15 (StataCorp LP, College Station, USA).
Results
Malawi
Among facilities sampled in the 2013–2014 Malawi SPA that offered malaria diagnosis/treatment services or curative care for sick children, 25% had all the components to be considered malaria-service ready (Table 2). Individual components of malaria-service readiness ranged from 92% of facilities having ACT available to 34% having diagnostic capacity. In the Malawi 2015–2016 DHS, advice and treatment was sought for 67% of the children under 5 years old with fever in the 2 weeks before the survey. Among febrile children for whom advice or treatment was sought, the most used source for care was government health centres (39%). Malaria-service readiness in government health centres was 32%, slightly higher than the average of 25% among all facilities. Disaggregating service readiness into individual components, government health facilities were performing well in several areas: 99% had ACT available, and 71% had national guidelines for the diagnosis and treatment of malaria available at the facility. The major gap in service readiness among government health centres in Malawi was a low level of diagnostic capacity (41%). Examining the components of diagnostic capacity among government health centres reveals that 3% had microscopy diagnostic capacity and 41% had RDT diagnostic capacity. While most facilities had RDT supplies (95%) only 61% had at least one health provider who received RDT training in the 24 months before the survey (Table 3).
Table 2.
Source of advice or treatment for children with fever and components of malaria service readiness by facilities in Malawi, Senegal and Tanzania
| Facility type | DHS Survey Data | SPA Survey Data | ||||||
|---|---|---|---|---|---|---|---|---|
| % for whom advice or treatment was sought | Number of children under 5 years with a fever | Among facilities offering malaria diagnosis/treatment services or curative sick child care services, percentage with | ||||||
| Personnel trained in RDT, microscopy or case management treatment of malaria in children | National guidelines for diagnosis and treatment of malaria | Diagnostic capacitya | ACT available | Malaria service readiness index | Total number of facilities | |||
| Malawi | 2015–2016 Malawi DHS | 2013–2014 Malawi SPA | ||||||
| Government hospital | 7.8 [6.5–9.2] | 4774 | 83.9 [70.9–91.7] | 82.0 [68.9–90.4] | 75.9 [62.1–85.8] | 100.0 | 59.9 [45.9–72.5] | 48 |
| Government health centre | 38.6 [36.4–40.9] | 4774 | 65.4 [60.2–70.2] | 71.2 [66.2–75.7] | 41.4 [36.4–46.7] | 99.2 [97.7–99.9] | 32.0 [27.3–37.1] | 338 |
| Government health post or mobile clinic | 6.9 [5.8–8.3] | 4774 | 40.9 [29.8–53.2] | 60.4 [48.2–71.5] | 19.6 [11.7–30.9] | 80.8 [69.2–88.7] | 14.9 [8.2–25.7] | 68 |
| Private facility | 4.9 [3.8–6.2] | 4774 | 38.8 [33.6–44.2] | 50.8 [45.4–56.3] | 19.1 [15.2–23.8] | 81.5 [76.9–85.4] | 11.7 [8.6–15.7] | 330 |
| Christian health association/mission/faith-based | 3.9 [3.1–4.9] | 4774 | 57.8 [50.1–65.1] | 70.4 [63–76.9] | 43.3 [36.0–51.0] | 98.8 [95.3–99.7] | 32.5 [25.8–40.0] | 162 |
| Any other source | 5.9 [5.0–6.9] | 4774 | n/a | n/a | n/a | n/a | n/a | n/a |
| Total | 67.1 [65.1–69.0] | 4774 | 54.0 [50.8–57.1] | 63.7 [60.6–66.8] | 34.2 [31.2–37.2] | 91.8 [89.8–93.4] | 25.2 [22.5–28.0] | 947 |
| Senegal | 2016 Senegal Continuous DHS | 2016 Senegal Continuous DHS | ||||||
| Government hospital or health centre | 4.6 [3.0–7.1] | 692 | 86.2 [74.4–93.1] | 91.1 [79.8–96.4] | 81.9 [69.8–89.8] | 89.8 [78.4–95.5] | 77.0 [64.4–86.0] | 29 |
| Government health post or mobile clinic | 32.3 [27.0–38.1] | 692 | 96.2 [92.1–98.2] | 94.1 [89.8–96.7] | 73.8 [67.3–79.4] | 96.0 [92.4–97.9] | 68.8 [62.1–74.8] | 252 |
| Government health hut | 3.4 [2.0–5.7] | 692 | 84.2 [69.5–92.5] | 76.0 [60.5–86.7] | 27.6 [17.7–40.2] | 63.0 [48–75.8] | 20.9 [12.2–33.3] | 85 |
| Private facility | 8.6 [5.3–13.9] | 692 | 64.5 [51.7–75.5] | 71.9 [60–81.4] | 41.6 [30.3–53.9] | 48.5 [36.5–60.6] | 26.3 [16.9–38.5] | 70 |
| Any other source | 2.8 [1.5–4.9] | 692 | n/a | n/a | n/a | n/a | n/a | n/a |
| Total | 49.8 [45.1–54.6] | 692 | 88.1 [83.9–91.3] | 86.8 [82.4–90.2] | 60.1 [54.7–65.3] | 81.5 [76.7–85.5] | 53.2 [47.8–58.4] | 436 |
| Tanzania | 2015–2016 Tanzania DHS-MIS | 2014–2015 Tanzania SPA | ||||||
| Government hospital | 3.8 [2.6–5.3] | 1706 | 66.5 [48.9–80.5] | 47.8 [35.1–60.8] | 61.7 [45.6–75.6] | 91.0 [84.5–95.0] | 33.3 [23.7–44.4] | 24 |
| Government health centre | 5.8 [4.4–7.7] | 1706 | 73.5 [67.8–78.6] | 61.0 [54.8–66.9] | 57.4 [51.2–63.4] | 94.5 [91.2–96.6] | 35.3 [29.6–41.4] | 88 |
| Government clinic/dispensary | 18.8 [15.8–22.2] | 1706 | 46.8 [41.4–52.2] | 64.9 [59.5–70.0] | 26.5 [22.1–31.5] | 94.2 [91.0–96.2] | 18.5 [14.8–23.0] | 761 |
| Private facility | 7.7 [6.1–9.7] | 1706 | 27.5 [18.4–38.8] | 42.5 [31.0–54.9] | 20.9 [13.0–31.8] | 73.7 [61.3–83.2] | 10.9 [5.2–21.4] | 156 |
| Mission/faith-based | 3.9 [2.9–5.3] | 1706 | 47.7 [36.4–59.3] | 60.4 [48.6–71.1] | 20.5 [13.9–29.2] | 84.1 [73.1–91.2] | 12.2 [7.5–19.1] | 147 |
| Any other source | 54.3 [50.7–57.8] | 1706 | n/a | n/a | n/a | n/a | n/a | n/a |
| Total | 81.3 [78.5–83.6] | 1706 | 46.7 [42.6–50.9] | 60.7 [56.5–64.8] | 28.1 [24.7–31.7] | 90.2 [87.3–92.4] | 18.3 [15.5–21.5] | 1177 |
See Table 3 for more details on the components of diagnostic capacity
aDiagnostic capacity is defined as a facility having microscopy diagnostic capacity or RDT diagnostic capacity
Table 3.
Components of diagnostic capacity by facilities in Malawi, Senegal and Tanzania
| Facility type | Among facilities offering malaria diagnosis/treatment services or curative sick child care services, percentage with | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Components of microscopy diagnostic capacity | Components of RDT diagnostic capacity | RDT diagnostic capacityb | Malaria diagnostic capacityc | Total number of facilities | |||||
| Personnel trained in microscopy | Microscopy supplies | Microscopy diagnostic capacitya | Personnel trained in RDT | RDT supplies | RDT protocol | ||||
| Malawi | 2013–2014 Malawi SPA | ||||||||
| Government hospital | 71.9 [57.9–82.6] | 60.1 [46.0–72.6] | 39.9 [27.4–54] | 81.9 [68.7–90.3] | 98 [87.1–99.7] | 88 [75.8–94.5] | 71.9 [57.9–82.6] | 75.9 [62.1–85.8] | 48 |
| Government health centre | 48.1 [42.9–53.4] | 4.6 [2.8–7.4] | 2.9 [1.5–5.3] | 60.5 [55.2–65.5] | 94.8 [91.9–96.7] | 68.9 [63.8–73.5] | 40.9 [35.8–46.1] | 41.4 [36.4–46.7] | 338 |
| Government health post or mobile clinic | 25.7 [16.6–37.6] | 3.0 [0.7–11.1] | 1.4 [0.2–9.5] | 36.1 [25.4–48.3] | 79.6 [68–87.8] | 52.8 [40.8–64.6] | 19.6 [11.7–30.9] | 19.6 [11.7–30.9] | 68 |
| Private facility | 28.3 [23.6–33.5] | 12.6 [9.4–16.7] | 4.0 [2.3–6.8] | 34.4 [29.4–39.8] | 75.6 [70.6–80] | 45.6 [40.3–51.1] | 17.6 [13.8–22.2] | 19.1 [15.2–23.8] | 330 |
| Christian health association/mission/ faith-based | 43.9 [36.5–51.5] | 24.7 [18.7–31.8] | 15.0 [10.3–21.3] | 55.3 [47.7–62.7] | 97.5 [93.6–99.1] | 68.1 [60.6–74.7] | 38.5 [31.4–46.1] | 43.3 [36.0–51.0] | 162 |
| Total | 40.1 [37–43.2] | 13.5 [11.5–15.9] | 7.1 [5.7–8.9] | 49.8 [46.7–53] | 87.6 [85.3–89.6] | 60.5 [57.3–63.5] | 32.4 [29.5–35.4] | 34.2 [31.2–37.2] | 947 |
| Senegal | 2016 Senegal Continuous DHS | ||||||||
| Government hospital or health centre | 86.2 [74.4–93.1] | 80.7 [68.4–88.9] | 74.3 [61.6–83.9] | 62.0 [48.9–73.5] | 98.4 [89.2–99.8] | 92.6 [81.4–97.3] | 60.3 [47.3–72.1] | 81.9 [69.8–89.8] | 29 |
| Government health post or mobile clinic | 96.2 [92.1–98.2] | 1.2 [0.4–4] | 1.2 [0.4–4] | 80.5 [74.4–85.4] | 98.5 [95.3–99.5] | 90.9 [86.1–94.2] | 73.3 [66.8–79] | 73.8 [67.3–79.4] | 252 |
| Government health hut | 84.2 [69.5–92.5] | 0.0 [0.0–0.0] | 0.0 [0.0–0.0] | 41.7 [29.2–55.4] | 74.5 [57.7–86.2] | 60.6 [45.9–73.6] | 27.6 [17.7–40.2] | 27.6 [17.7–40.2] | 85 |
| Private facility | 64.5 [51.7–75.5] | 26.8 [17.4–39] | 20.2 [12.1–31.8] | 36.3 [25.7–48.6] | 74.9 [62.5–84.2] | 68.6 [56.0–78.9] | 27.9 [18.7–39.5] | 41.6 [30.3–53.9] | 70 |
| Total | 88.1 [83.9–91.3] | 10.4 [8–13.4] | 8.9 [6.8–11.6] | 64.6 [59.2–69.6] | 90 [85.4–93.3] | 81.5 [76.6–85.6] | 56.2 [50.9–61.5] | 60.1 [54.7–65.3] | 436 |
| Tanzania | 2014–15 Tanzania SPA | ||||||||
| Government hospital | 61.7 [45.5–75.6] | 55.4 [41.0–69.0] | 43.0 [31.4–55.5] | 56.0 [41.4–69.7] | 93.8 [88.2–96.9] | 88.9 [81.9–93.4] | 50.5 [37.2–63.8] | 61.7 [45.6–75.6] | 24 |
| Government health centre | 65.7 [59.7–71.3] | 44.7 [38.7–50.9] | 33.1 [27.5–39.1] | 65.9 [59.9–71.5] | 92.5 [88.5–95.2] | 79.7 [74.3–84.2] | 49.7 [43.6–55.8] | 57.4 [51.2–63.4] | 88 |
| Government clinic/dispensary | 33.5 [28.6–38.7] | 4.9 [2.9–7.9] | 0.9 [0.3–2.5] | 40.8 [35.6–46.2] | 83.8 [79.4–87.5] | 64.7 [59.3–69.7] | 26.4 [21.9–31.3] | 26.5 [22.1–31.5] | 761 |
| Private facility | 24.7 [16.0–36.1] | 38.5 [27.4–50.9] | 7.6 [4–14] | 25.7 [16.9–37.1] | 63.1 [50.6–74] | 54.8 [42.5–66.5] | 18.2 [10.7–29.2] | 20.9 [13.0–31.8] | 156 |
| Mission/faith-based | 38.1 [27.9–49.5] | 37.9 [27.5–49.6] | 12.6 [7.7–19.8] | 35.7 [25.9–46.9] | 72.4 [60.4–81.9] | 54.1 [42.4–65.4] | 16.9 [10.9–25.2] | 20.5 [13.9–29.2] | 147 |
| Total | 35.9 [32.1–39.9] | 17.5 [14.7–20.7] | 6.6 [5.4–8] | 40.4 [36.4–44.5] | 80.5 [76.9–83.7] | 63.7 [59.5–67.7] | 26.4 [23–30] | 28.1 [24.7–31.7] | 1177 |
aMicroscopy diagnostic capacity is defined as a facility having a functioning microscope with glass slides and relevant stains, in addition to at least one health provider who has received training on microscopy during the 24 months before the survey
bRDT diagnostic capacity is defined as a facility having unexpired malaria RDT kits, at least one health provider who received RDT training in the 24 months before the survey, and the facility having an instructional protocol for performing a RDT
cDiagnostic capacity is defined as a facility having microscopy diagnostic capacity or RDT diagnostic capacity
Senegal
Overall, 53% of facilities in Senegal sampled in the 2016 SPA that offered malaria diagnosis/treatment services or curative care for sick children had all the components to be considered malaria-service ready. Among the individual components of malaria-service readiness, Senegal performed highest in having personnel trained in malaria diagnosis (88%) and posted guidelines in the facility (87%). Senegal’s facilities performed less well with diagnostic capacity (60%), however. The corresponding 2016 Senegal DHS survey showed that advice or treatment was sought for 50% of the children with fever in the 2 weeks before the survey. The most commonly used source of advice or treatment for children with fever was primary-level facilities (government health post or mobile clinic), at 32%. Among government health posts or mobile clinics in Senegal, 69% met the criteria to be considered malaria-service ready, substantially higher than the 53% average among all facilities. Among the primary-level facilities, 96% had ACT medicines available and personnel trained in malaria diagnosis or treatment, and 94% had national guidelines for diagnosis and treatment of malaria, while 74% had diagnostic capacity (Table 2). Most government health posts or mobile clinics had RDT diagnostic capacity (73%) and 99% of government health posts or mobile clinics had RDT supplies. Very few government health posts or mobile clinics had microscopy diagnostic capacity (1%) (Table 3).
Tanzania
On average, facilities in Tanzania were least ready to provide malaria services; only 18% of facilities sampled in the 2014–2015 SPA had all four service readiness components, highest for the component on availability of ACT (90%). Tanzanian facilities performed poorly in diagnostic capacity (28%). In the Tanzania 2015–2016 DHS-MIS survey, advice or treatment was sought for 81% of children under 5 years old with fever in the 2 weeks before the survey. What differentiates Tanzania from other two countries studied is that for 54% of febrile children for whom advice or treatment was sought, it was from a source not sampled in the SPA survey. For Tanzania this included ADDOs and other pharmacies. However, among the sources sampled in the SPA survey the highest proportion (19%) of febrile children were taken to a government clinic/dispensary. Among government clinics/dispensaries, only 19% were malaria-service ready, much lower than among health centres and hospitals. Among government clinics/dispensaries, 94% had ACT medicines available, 65% had national guidelines for diagnosis and treatment of malaria, and 47% had personnel trained in malaria diagnosis or treatment. The major barrier to service readiness for government clinics/dispensaries, as for sampled facilities overall in Tanzania, was low diagnostic capacity (27%) (Table 2). Twenty-seven per cent of government clinics/dispensaries had RDT diagnostic capacity and 1% had microscopy diagnostic capacity. In examining the components of RDT capacity in government clinics/dispensaries, 41% had at least one health provider who received RDT training in the 24 months before the survey and 65% had a RDT protocol posted in the facility. Availability of RDTs do not appear to be a limiting factor in that 84% of facilities had RDT supplies available on the day of the survey (Table 3).
Discussion
The percentage of facilities classified as malaria-service ready ranged from 18% in Tanzania and 25% in Malawi to 53% in Senegal. In all three countries, primary healthcare facilities (health centre/health post/health clinic) were the most used type of facility for care seeking for febrile children. Among these primary healthcare facilities, only 69% in Senegal, 32% in Malawi and 19% in Tanzania were considered as malaria-service ready, with all four required components of malaria-service readiness, although they performed better in individual components. Among the four components of malaria-service readiness in the facilities most visited by febrile children, diagnostic capacity (comprising supplies and trained personnel) was the weakest component in all three countries, due to the low availability of trained personnel. The next weakest component was personnel trained in RDT, microscopy or case management/treatment of malaria in children for Tanzania and Malawi, and national guidelines posted for diagnosis and treatment of malaria in Senegal. These results are similar to Lee et al. who examined malaria-service readiness in relationship to malaria endemicity in Kenya, Namibia and Senegal [17] and to Dolan et al. who examined malaria-service readiness as it pertains to health aid projects in Malawi [42]. Both studies also identified a lack of malaria guidelines and adequately trained staff as reasons for lower malaria service readiness in facilities.
More emphasis on training personnel would achieve the greatest improvements in malaria-service readiness of facilities most frequented by febrile children in the studied countries. Having trained personnel is not only one of the four components of malaria-service readiness but also a sub-component of diagnostic capacity. Ongoing training for service providers can ensure that providers continue to learn about the most recent developments in malaria care. In the SPA, adequate training is defined as a facility having at least one provider of malaria services who reported receiving in-service training during the 24 months before the survey. The training must include structured sessions and does not include individual instruction a provider might have received during routine supervision. Although personnel might have received training in the past (more than 24 months before to the survey) malaria policies are continually changing. There can be repercussions on the quality of diagnosis and treatment in facilities that do not have at least one provider trained in updated policies.
To improve malaria-service readiness, governments should focus on in-service training, training updates, or refresher training on the performance of malaria microscopy or RDTs, as well as correct case management procedures. This would improve not only the trained provider component of malaria-service readiness but also diagnostic capacity. While previous studies have shown mixed conclusions around the impact of large-scale investments in in-service training [43–46], it is important to offer in-service training not just once but on a regular basis and updated based on changing policies. Additionally, training that targets smaller groups, focus on a single topic and incorporate principles of adult learning have been shown to produce better results in improving performance among health workers [47].
All three countries reported high levels of availability of ACT medicine in the facilities most used by children with fever. The universal and continuous availability of anti-malarial drugs is a critical component in the delivery of malaria treatment in health facilities. Unexpired ACT medicine was available in 99% of facilities most frequented by febrile children in Malawi, 96% of facilities in Senegal and 94% of facilities in Tanzania. This finding is encouraging, because children who are positive for malaria can be treated with ACT within the facility where treatment is sought. However, this successful component of malaria-service readiness must be maintained in the future.
One important limitation of this study is the lack of linkages (SPA and DHS are independent surveys fielded at different times) between specific facilities in the DHS and SPA surveys. Without this linkage, the service readiness of the exact facilities where the children’s caregivers sought advice and treatment for children with a fever is unknown. In this analysis the SPA surveys provided information on the malaria-service readiness of facilities, while the DHS surveys provided information on population-level utilization of malaria services in children under 5 years old with fever. Linking these two types of data sources can be challenging, because the SPA and DHS are independent surveys and not designed to be linked. In addition, publicly available geolocations of DHS clusters are displaced to protect confidentiality of the participants.
Another limitation is that, because the SPA covers only formal health facilities, the analysis does not include the service readiness of informal health services or private healthcare providers who operate outside a formal facility. There is evidence that use of private healthcare providers and informal healthcare providers, such as pharmacies for the disbursement of anti-malarial drugs, could be more widespread than use of formal facilities. In the 2015–2016 Tanzania DHS-MIS, for example, 54% of children who sought advice or treatment for fever were taken to a location categorized as an ‘other source’. The primary reason that smaller private providers, informal healthcare providers, or CHWs who provide iCCM are not included in a SPA survey is the absence of an accurate sampling frame for these providers. Since many of these providers are not well documented or do not have the proper accreditation, the country’s Ministry of Health may not have a complete listing that could serve as the basis for a sampling frame. Further research is needed on the readiness and quality of services provided by informal providers in settings where the informal sector is widely used for malaria diagnosis and treatment.
The definition of malaria-service readiness is also problematic in that it is very hard to achieve, especially for lower-level health facilities. The malaria-service readiness index has many components and may not always accurately measure true readiness. For example, if a facility has all the components of RDT diagnostic capacity but do not have RDT protocol (training manual, poster or job aid for using RDT) observed in the facility, the facility does not have RDT diagnostic capacity and in turn is not considered to be malaria-service ready. Additionally, the definition of in-service training for malaria-service readiness is very specific in stating that the training must include structured sessions and does not include individual instruction a provider might have received during routine supervision. Over time many organizations are choosing to support training of frontline health workers through supervision, not through classroom training. If a facility has been supported by an organization that funds training through routine supervision instead of structured classroom settings, this facility is no longer classified as malaria-service ready since there will be no provider in the facility trained in structured sessions. These are limitations that should be considered in the future for the WHO definition of malaria service readiness.
It should also be noted that the malaria-service readiness definition used here is based on guidelines for the treatment of malaria rather than integrated treatment protocols for sick children (it does not include availability of antibiotics, for example), which may limit the interpretation of these findings.
Lastly, in harmonizing facility types between the DHS and SPA surveys, several types of health facilities had to be grouped together to provide a large enough sample size for stratification. In Senegal, for example, due to low numbers of individuals seeking care for fever at government hospitals, government hospitals and health centres were combined to generate an adequate sample size for analysis. An assumption was made that the level of service readiness is the same among the combined facilities, which is not necessarily the case.
Conclusions
This study investigated the utilization and provision of malaria services by examining data on the source of advice or treatment in children under 5 years old with fever from the household-based DHS surveys and data on provision of care from the facility-based SPA surveys from Malawi, Senegal and Tanzania. The analysis highlights the need for improving the malaria-service readiness of facilities in all three countries. More effort should be focused on facilities that are commonly used for care and treatment of fever, especially in the areas of malaria diagnostic capacity and provider training. It is essential for policymakers to consider the malaria-service readiness of primary-level healthcare facilities when allocating resources and training, particularly in limited-resource settings, to ensure that the points of care that are most used are properly equipped to provide diagnosis and treatment for malaria.
Acknowledgements
The authors are grateful to Sarah Yang for creating graphics and DHS Program survey managers Michelle Winner and Jean de Dieu Bizimana for their valuable assistance in providing country-specific context. Additional thanks goes to Bryant Robey for editorial review.
Abbreviations
- ACT
artemisinin-based combination therapy
- ADDO
accredited drug dispensing outlet
- CHAM
Christian Health Association of Malawi
- CHW
Community Health Worker
- DHS
Demographic and Health Survey
- FBOs
Faith-based Organizations
- iCCM
integrated community case management
- IMCI
integrated management of childhood illness
- RDT
malaria rapid diagnostic test
- MoHCDEC
Ministry of Health, Community Development, Gender, Elderly and Children
- MIS
Malaria Indicator Survey
- NGO
Non-Governmental Organization
- PHCCs
primary health care cottages
- PHCUs
primary health care units
- RBM
roll back malaria
- SPA
Service Provision Assessment
- WHO
World Health Organization
Authors’ contributions
CT, AL and WW conceived the study. CT managed the datasets and analysed the data. CT and AL drafted the paper with revisions from WW, LF and HM. All authors read and approved the final manuscript.
Funding
This study was conducted with support provided by the US Agency for International Development (USAID) through The DHS Program (#AID-OAA-C-13-00095). The views expressed are those of the authors and do not necessarily reflect the views of USAID or the US Government. The findings and conclusions presented in this manuscript are those of the authors and do not necessarily reflect the official position of the PMI, USAID, or the US Government.
Availability of data and materials
The datasets analysed during the current study are available from The DHS Program web site, http://www.dhsprogram.com.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chuma J, Okungu V, Molyneux C. Barriers to prompt and effective malaria treatment among the poorest population in Kenya. Malar J. 2010;9:144. doi: 10.1186/1475-2875-9-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bennett A, Eisele T, Keating J, Yukich J. Global trends in care seeking and access to diagnosis and treatment of childhood illnesses. In: DHS Working Papers No 116. Rockville, Maryland, USA: ICF International; 2015.
- 3.Russell S. The economic burden of illness for households in developing countries: a review of studies focusing on malaria, tuberculosis, and human immunodeficiency virus/acquired immunodeficiency syndrome. Am J Trop Med Hyg. 2004;71:147–155. doi: 10.4269/ajtmh.2004.71.147. [DOI] [PubMed] [Google Scholar]
- 4.McIntyre DI, Thiede M, Birch S. Access as a policy-relevant concept in low- and middle-income countries. Health Econ Policy Law. 2009;4:179–193. doi: 10.1017/S1744133109004836. [DOI] [PubMed] [Google Scholar]
- 5.Romay-Barja M, Cano J, Ncogo P, Nseng G, Santana-Morales MA, Valladares B, et al. Determinants of delay in malaria care-seeking behaviour for children 15 years and under in Bata district, Equatorial Guinea. Malar J. 2016;15:187. doi: 10.1186/s12936-016-1239-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dhillon RS, Bonds MH, Fraden M, Ndahiro D, Ruxin J. The impact of reducing financial barriers on utilisation of a primary health care facility in Rwanda. Glob Public Health. 2012;7:71–86. doi: 10.1080/17441692.2011.593536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Altaras R, Nuwa A, Agaba B, Streat E, Tibenderana JK, Martin S, et al. How do patients and health workers interact around malaria rapid diagnostic testing, and how are the tests experienced by patients in practice? A qualitative study in Western Uganda. PLoS ONE. 2016;11:e0159525. doi: 10.1371/journal.pone.0159525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kizito J, Kayendeke M, Nabirye C, Staedke SG, Chandler CI. Improving access to health care for malaria in Africa: a review of literature on what attracts patients. Malar J. 2012;11:55. doi: 10.1186/1475-2875-11-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ansah EK, Reynolds J, Akanpigbiam S, Whitty CJ, Chandler CI. “Even if the test result is negative, they should be able to tell us what is wrong with us”: a qualitative study of patient expectations of rapid diagnostic tests for malaria. Malar J. 2013;12:258. doi: 10.1186/1475-2875-12-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klein EY, Lewis IA, Jung C, Llinás M, Levin SA. Relationship between treatment-seeking behaviour and artemisinin drug quality in Ghana. Malar J. 2012;11:110. doi: 10.1186/1475-2875-11-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dillip A, Hetzel MW, Gosoniu D, Kessy F, Lengeler C, Mayumana I, et al. Socio-cultural factors explaining timely and appropriate use of health facilities for degedege in south-eastern Tanzania. Malar J. 2009;8:144. doi: 10.1186/1475-2875-8-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Birhanu Z, Yihdego YY-E, Yewhalaw D. Caretakers’ understanding of malaria, use of insecticide treated net and care seeking-behavior for febrile illness of their children in Ethiopia. BMC Infect Dis. 2017;17:629. doi: 10.1186/s12879-017-2731-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Do M, Babalola S, Awantang G, Toso M, Lewicky N, Tompsett A. Associations between malaria-related ideational factors and care-seeking behavior for fever among children under five in Mali, Nigeria, and Madagascar. PLoS ONE. 2018;13:e0191079. doi: 10.1371/journal.pone.0191079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adedokun ST, Adekanmbi VT, Uthman OA, Lilford RJ. Contextual factors associated with health care service utilization for children with acute childhood illnesses in Nigeria. PLoS ONE. 2017;12:e0173578. doi: 10.1371/journal.pone.0173578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gulliford M, Figueroa-Munoz J, Morgan M, Hughes D, Gibson B, Beech R, et al. What does ‘access to health care’ mean? J Health Serv Res Policy. 2002;7:186–188. doi: 10.1258/135581902760082517. [DOI] [PubMed] [Google Scholar]
- 16.Onwujekwe O, Uzochukwu B, Eze S, Obikeze E, Okoli C, Ochonma O. Improving equity in malaria treatment: relationship of socio-economic status with health seeking as well as with perceptions of ease of using the services of different providers for the treatment of malaria in Nigeria. Malar J. 2008;7:5. doi: 10.1186/1475-2875-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee EH, Olsen CH, Koehlmoos T, Masuoka P, Stewart A, Bennett JW, et al. A cross-sectional study of malaria endemicity and health system readiness to deliver services in Kenya, Namibia and Senegal. Health Policy Plan. 2017;32:75–87. doi: 10.1093/heapol/czx114. [DOI] [PubMed] [Google Scholar]
- 18.Zurovac D, Tibenderana JK, Nankabirwa J, Ssekitooleko J, Njogu JN, Rwakimari JB, et al. Malaria case-management under artemether–lumefantrine treatment policy in Uganda. Malar J. 2008;7:181. doi: 10.1186/1475-2875-7-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kangwana BB, Njogu J, Wasunna B, Kedenge SV, Memusi DN, Goodman CA, et al. Malaria drug shortages in Kenya: a major failure to provide access to effective treatment. Am J Trop Med Hyg. 2009;80:737–738. doi: 10.4269/ajtmh.2009.80.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Njogu J, Akhwale W, Hamer DH, Zurovac D. Health facility and health worker readiness to deliver new national treatment policy for malaria in Kenya. East Afric Med J. 2008;85:213–221. doi: 10.4314/eamj.v85i5.9615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hanson K, Goodman C, Lines J, Meek S, Bradley D, Mills A. The economics of malaria control interventions. In: Hanson K, editor. Global Forum for Health Research. Geneva: World Health Organization; 2004. [Google Scholar]
- 22.Kaula H, Buyungo P, Opigo J. Private sector role, readiness and performance for malaria case management in Uganda, 2015. Malar J. 2017;16:219. doi: 10.1186/s12936-017-1824-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mills A, Brugha R, Hanson K, McPake B. What can be done about the private health sector in low-income countries? Bull World Health Organ. 2002;80:325–330. [PMC free article] [PubMed] [Google Scholar]
- 24.Noor AM, Rage IA, Moonen B, Snow RW. Health service providers in Somalia: their readiness to provide malaria case-management. Malar J. 2009;8:100. doi: 10.1186/1475-2875-8-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Poyer S, Shewchuk T, Tougher S, Ye Y, Mann AG, Willey BA, et al. Availability and price of malaria rapid diagnostic tests in the public and private health sectors in 2011: results from 10 nationally representative cross-sectional retail surveys. Trop Med Int Health. 2015;20:744–756. doi: 10.1111/tmi.12491. [DOI] [PubMed] [Google Scholar]
- 26.Visser T, Bruxvoort K, Maloney K, Leslie T, Barat LM, Allan R, et al. Introducing malaria rapid diagnostic tests in private medicine retail outlets: a systematic literature review. PLoS ONE. 2017;12:e0173093. doi: 10.1371/journal.pone.0173093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ssempiira J, Kasirye I, Kissa J, Nambuusi BB, Mukooyo E, Opigo J, et al. Measuring health facility readiness and its effects on severe malaria outcomes in Uganda. Sci Rep. 2018;8:17928. doi: 10.1038/s41598-018-36249-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kyabayinze DJ, Asiimwe C, Nakanjako D, Nabakooza J, Counihan H, Tibenderana JK. Use of RDTs to improve malaria diagnosis and fever case management at primary health care facilities in Uganda. Malar J. 2010;9:200. doi: 10.1186/1475-2875-9-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ruizendaal E, Dierickx S, Peeters Grietens K, Schallig HD, Pagnoni F, Mens PF. Success or failure of critical steps in community case management of malaria with rapid diagnostic tests: a systematic review. Malar J. 2014;13:229. doi: 10.1186/1475-2875-13-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.WHO/UNICEF Joint Statement . Integrated Community Case Management (iCCM): An equity-focused strategy to improve access to essential treatment services for children. Geneva: World Health Organization; 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rowe SY, Kelly JM, Olewe MA, Kleinbaum DG, McGowan JE, Jr, McFarland DA, et al. Effect of multiple interventions on community health workers’ adherence to clinical guidelines in Siaya district, Kenya. Trans R Soc Trop Med Hyg. 2007;101:188–202. doi: 10.1016/j.trstmh.2006.02.023. [DOI] [PubMed] [Google Scholar]
- 32.Ministry of Health—MoH, ICF: Malawi Service Provision Assessment 2013–2014. Lilongwe: MoH/Malawi and ICF International; 2014.
- 33.Programme National de Lutte contre le Paludisme-Senegal: Plan Strategique National de Lutte contre le Paludisme au Senegal 2016–2020. Dakar; 2015.
- 34.Ministry of Health. Social WT. Ministry of HZ. National Bureau of ST. Office of Chief Government ST. International ICF . Tanzania Service Provision Assessment Survey 2014–2015. Tanzania: Dar es Salaam; 2016. [Google Scholar]
- 35.Ministry of Health, International ICF. Malawi Service Provision Assessment 2013–14. Lilongwe, Malawi; 2014.
- 36.National Statistical OM. ICF: Malawi Demographic and Health Survey 2015–16. Zomba: National Statistical Office and ICF; 2017. [Google Scholar]
- 37.Agence Nationale de la Statistique et de la Démographie AS, Ministère de la Santé et de l’Action S . ICF: Sénégal Enquête Continue sur la Prestation des Services de Soins de Santé (ECPSS) USA: ANSD/Sénégal and ICF; 2016. p. Rockville. [Google Scholar]
- 38.Agence Nationale de la Statistique et de la Démographie AS, ICF: Senegal Enquête Démographique et de Santé Continue (EDS-Continue) 2016. Dakar, Sénégal; 2017.
- 39.Ministry of Health CDGE, National Bureau of Statistics NBST, Office of Chief Government Statistician OZ, ICF. Tanzania Demographic and Health Survey and Malaria Indicator Survey 2015–2016. Dar es Salaam, Tanzania; 2016.
- 40.Roll Back Malaria Partnership to End Malaria (RBM). Household Survey Indicators for Malaria Control. Geneva; 2013.
- 41.Health Statistics and Information Systems, WHO. Service Availability and Readiness Assessment (SARA): an annual monitoring system for service delivery vol. Reference Manual, Version 2.2; 2015.
- 42.Dolan CB. Health aid projects have both expanded and constrained the capacity of health facilities to deliver malaria services to under-five children in Malawi. BMJ Global Health. 2018;3:e001051. doi: 10.1136/bmjgh-2018-001051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Blanas DA, Ndiaye Y, Nichols K, Jensen A, Siddiqui A, Hennig N. Barriers to community case management of malaria in Saraya, Senegal: training, and supply-chains. Malar J. 2013;12:95. doi: 10.1186/1475-2875-12-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wasunna B, Zurovac D, Bruce J, Jones C, Webster J, Snow RW. Health worker performance in the management of paediatric fevers following in-service training and exposure to job aids in Kenya. Malar J. 2010;9:261. doi: 10.1186/1475-2875-9-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zurovac D, Ndhlovu M, Rowe AK, Hamer DH, Thea DM, Snow RW. Treatment of paediatric malaria during a period of drug transition to artemether-lumefantrine in Zambia: cross sectional study. BMJ. 2005;331:734. doi: 10.1136/bmj.331.7519.734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rowe AK, Hamel MJ, Flanders WD, Doutizanga R, Ndoyo J, Deming MS. Predictors of correct treatment of children with fever seen at outpatient health facilities in the Central African Republic. Am J Epidemiol. 2000;151:1029–1035. doi: 10.1093/oxfordjournals.aje.a010131. [DOI] [PubMed] [Google Scholar]
- 47.Rowe AK, de Savigny D, Lanata CF, Victora CG. How can we achieve and maintain high-quality performance of health workers in low-resource settings? Lancet. 2005;366:1026–1035. doi: 10.1016/S0140-6736(05)67028-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analysed during the current study are available from The DHS Program web site, http://www.dhsprogram.com.