Abstract
Background:
Given the proximity of the medial patellofemoral ligament (MPFL) femoral insertion to the distal femoral physis in skeletally immature patients, multiple techniques for femoral graft fixation have been described.
Purpose:
To systematically review the literature and evaluate outcomes and complications following MPFL reconstruction in skeletally immature patients.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A comprehensive literature search was performed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines through use of the PubMed, Embase, and Cochrane Central databases. All original, English-language studies reporting outcomes or complications following MPFL reconstruction in skeletally immature patients were included. Skeletally mature patients were excluded. Data regarding demographics, surgical technique, graft type, outcomes, and complications were recorded. Study quality was assessed by use of the modified Coleman methodology score. Statistical analysis was performed through use of chi-square and weighted mean pooled cohort statistics, where appropriate, with significance set at P < .05.
Results:
7 studies that entailed 132 MPFL reconstructions (126 patients) met the inclusion criteria. Females comprised 57.9% of the cohort (73 females), and the mean age was 13.2 years (range, 6-17 years). Mean postoperative follow-up was 4.8 years (range, 1.4-10 years). All of the grafts used were autograft, with gracilis tendon (n = 80; 60.6%) being the most common. Methods of femoral fixation included interference screw (n = 52; 39.4%), suture anchor (n = 51; 38.6%), and soft tissue pulley around the medial collateral ligament or adductor tendon (n = 29; 21.9%). Pooled Kujala scores improved from 59.1 to 84.6 after MPFL reconstruction. The total reported complication rate was 25.0% (n = 33) and included 5 redislocations (3.8%) and 15 subluxation events (11.4%). No cases of premature physeal closure were noted, and there were 3 reports of donor site pain (2.3%). Neither autograft choice (P > .804) nor method of femoral fixation (P > .416) influenced recurrent instability or overall complication rates.
Conclusion:
These findings suggest that MPFL reconstruction in skeletally immature patients is a viable treatment option, with significant improvement in patient-reported outcomes and redislocation event rates of less than 5% at nearly 5-year follow-up. Further high-quality research is needed to determine optimal graft options and surgical technique while considering recurrent instability, donor site morbidity, and potential injury to the adjacent physis.
Keywords: medial patellofemoral ligament, patellar instability, skeletally immature, patellofemoral
Lateral patellar dislocation is the most frequently recognized acute knee injury in children.9 Traditionally, first-time patellar dislocations without loose osteochondral fragments have been treated nonoperatively with activity modification, patellar bracing, and physical therapy focused on quadriceps and hip abductor strengthening.18 However, recurrent patellar instability is often considered an indication for surgical intervention, particularly in the young patient. The risk of subsequent dislocation increases significantly with each instability event, with further concern that recurrent dislocation may lead to the development of osteoarthritis8 and diminished knee function.2,15
A variety of anatomic factors have been shown to contribute to recurrent patellar instability.9,18,25 Similarly, a plethora of surgical procedures have been described to improve biomechanics and correct or bypass typical anatomic abnormalities. In skeletally immature patients, many osseous procedures are not routinely performed because of the risk of physeal injury. Because the medial patellofemoral ligament (MPFL) is often injured after lateral patellar dislocation28 and is considered the primary static restraint to lateral translation, MPFL reconstruction has been used to reduce the rate of recurrent dislocation.4,22,25 To avoid distal femoral physeal injury in the skeletally immature population, anatomic MPFL reconstruction has been conducted via multiple fixation techniques in the patella and femur.
Although multiple surgical techniques for MPFL reconstruction have been described, no consensus is available regarding the optimal graft type or surgical technique in the skeletally immature patient. The purpose of this systematic review was to evaluate the efficacy of MPFL reconstruction in skeletally immature patients and determine whether graft choice and fixation technique influence complications and recurrent instability.
Methods
A comprehensive literature search was performed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines using PubMed, Embase, and Cochrane Central databases.17 All original English-language studies that reported outcomes or complications following isolated MPFL reconstruction in skeletally immature patients with a minimum follow-up period of 12 months were included. Furthermore, inclusion required reporting of clinical outcomes with granular data to allow stratification by graft type and fixation technique. Exclusion criteria were non–English language studies, technique guides, basic science studies, case series with fewer than 3 participants, studies reporting MPFL repair and/or MPFL reconstruction with specifically detailed concomitant procedures, data that were not stratified by graft type or fixation, and studies in which skeletal immaturity was not explicitly stated or categorized. Studies were not excluded based on graft choice.
Search terms and strategies were created to optimize the individual function of each database. After removal of duplicates, potential articles were reviewed independently by 2 authors (A.G.S. and M.A.D.), and any inconsistencies were reviewed and rectified by the senior author (R.W.W.). Data independently extracted by the 2 authors included demographic data; surgical technique, including method of femoral and patellar fixation; graft type; recurrence of patellar instability; and surgical outcome data. Within the included articles, the most consistently reported outcome measure was recurrent instability, defined as recurrent dislocation or subluxation events reported by the patient, and the most commonly used patient-reported measure was the Kujala score.10 The recurrent dislocation or subluxation rate was chosen as the primary outcome measure, with the Kujala questionnaire results and the combined rate of instability- and non–instability related postoperative complications serving as secondary outcomes. The quality of included studies was assessed by 2 reviewers (A.G.S., M.A.D.) according to the modified Coleman methodology score (MCMS).5
Data Analysis
To account for differences in follow-up length, the redislocation rate per 100 person-years was calculated by use of the mean follow-up and was transformed via the Freeman-Tukey double-arcsine method. Inverse-variance weighted random-effects models were used to evaluate the difference in pooled complication rates between graft types and femoral fixation techniques. A forest plot was generated to display the rate of recurrent instability and 95% confidence interval for each study as well as the overall, random-effects pooled estimate for each group and its confidence interval. Analyses were completed with R version 3.1.1 (Metafor Meta-Analysis Package for R; R Foundation for Statistical Computing), with significance defined as P < .05.
Results
Literature Search
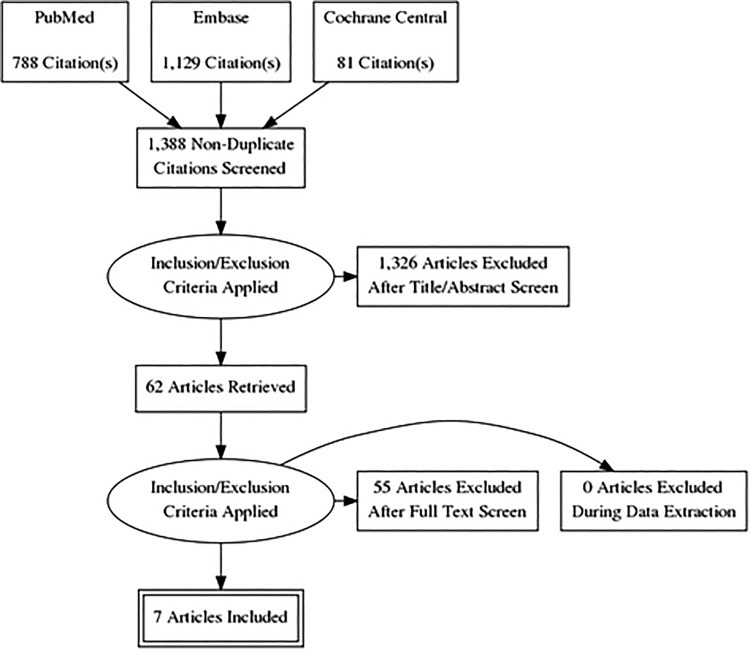
The literature search identified 1388 studies meeting the criteria for initial review. After application of the inclusion and exclusion criteria, 7 original studies1,6,11–13,20,21 were included for analysis (Figure 1). These studies included 132 MPFL reconstructions in 126 skeletally immature patients, with a mean follow-up of 4.8 years (range, 1.4-10 years) (Table 1). Of the 126 patients, 73 (57.9%) were female, with a mean age of 13.2 years (range, 6-17 years).
Figure 1.
Flow diagram detailing literature search results.
TABLE 1.
Demographic Information, Graft Type, and Kujala Scores for the Included Studiesa
| Study | Year | Graft Type | Cases/Patients, n | Sex, Male, n (%) | Age, Mean (range), y | Follow-up, Mean (range), y | Preoperative Kujala, Mean (SD; range) | Postoperative Kujala, Mean (SD; range) |
|---|---|---|---|---|---|---|---|---|
| Lind et al12 | 2016 | Gra | 24/20 | 9 (45.0) | 12.5 (8-16) | 3.3 (1.4-6) | 61 (13; NR) | 71 (15; NR) |
| Machado et al13 | 2017 | Gra | 35/35 | 11 (31.4) | 15.9 (14-17) | 9.7 (NR) | 54 (11; NR) | 78 (3; NR) |
| Nelitz et al20 | 2013 | Gra | 21/21 | 15 (71.4) | 12.2 (10.3-13.9) | 2.8 (2.0-3.6) | 72.9 (NR; 37-87) | 92.8 (NR; 74-100) |
| Abouelsoud et al1 | 2015 | Quad | 16/16 | 5 (31.3) | 11.5 (8-15) | 2.4 (2-2.8) | 56 (4.72; 49-61) | 94 (2.73; 90-99) |
| Nelitz et al21 | 2018 | Quad | 25/25 | 9 (36.0) | 12.8 (9.5-14.7) | 2.6 (2.0-3.4) | 63 (NR; 44-81) | 89 (NR; 77-100) |
| Deie et al6 | 2003 | SemiT | 6/4 | 2 (50.0) | 8.5 (6-10) | 7.4 (4.8-10) | NR | 96.3 (NR; 89-100) |
| Kumahashi et al11 | 2012 | SemiT | 5/5 | 2 (40.0) | 13.6 (11-15) | 2.3 (2-3) | 67.4 (12.6; NR) | 95.4 (3.2; NR) |
aGra, gracilis; NR, not recorded; Quad, quadriceps; SemiT, semitendinosus.
Graft Choice
All grafts were autografts, including gracilis tendon (n = 80; 60.6%),12,13,20 quadriceps tendon (n = 41; 31.1%),1,21 and semitendinosus tendon (n = 11; 8.3%).11
Femoral Fixation
Modes of femoral fixation included soft tissue pulley around the medial collateral ligament (MCL) (n = 11) or the adductor magnus (n = 24) tendon (n = 35; 26.5%),6,11,12 suture anchors (n = 51; 38.6%),1,13 and interference screw fixation (n = 46; 34.8%).20,21 The mean ages of the soft tissue pulley and interference screw groups were similar, 12.1 years and 12.5 years, respectively, whereas the suture anchor fixation group was older, with a mean age of 14.5 years. All femoral tunnels for interference screws were placed distal to the physis.
Patellar Fixation
Methods of patellar fixation included a blind bone tunnel with an interference screw (n = 5; 3.8%),11 a single bone tunnel in which the graft was looped (n = 45; 34.1%),12,20 suture anchor fixation (n = 41; 31.1%),6,13 and no osseous fixation, with the quadriceps tendon reflected from its intact insertion on the patella (n = 41; 31.1%).1,21
Outcomes and Complications
Pooled Kujala scores improved from 59.1 to 84.6 following MPFL reconstruction. The overall complication rate was 25.0% (n = 33). The total rate of recurrent instability following MPFL reconstruction was 15.2%, including 5 redislocations (3.8%) and 15 subluxation events (11.4%) (Table 2).
TABLE 2.
Recurrent Instability and Non–Stability Related Complicationsa
| Study | Year | Graft Type | Femoral Fixation | Patellar Fixation | Redislocation, n (%) | Resubluxation, n (%) | Other Complications |
|---|---|---|---|---|---|---|---|
| Lind et al12 | 2016 | Gra | Pulley | Bone tunnel | 4 (3.0) | 5 (3.8) | None |
| Machado et al13 | 2017 | Gra | Suture | Suture | 1 (0.8) | 3 (2.3) | 5 residual knee pain, 3 donor site pain, 2 hematoma, 1 superficial infection |
| Nelitz et al20 | 2013 | Gra | Screw | Bone tunnel | 0 | 0 | 1 knee stiffness |
| Abouelsoud et al1 | 2015 | Quad | Suture | None | 0 | 5 (3.8) | None |
| Nelitz et al21 | 2018 | Quad | Screw | None | 0 | 0 | 1 knee swelling |
| Deie et al6 | 2003 | SemiT | Pulley | Suture | 0 | 2 (1.5) | None |
| Kumahashi et al11 | 2012 | SemiT | Pulley | Screw | 0 | 0 | None |
aGra, gracilis; Pulley, soft tissue pulley; Quad, quadriceps; Screw, interference screw; SemiT, semitendinosus; Suture, suture anchor.
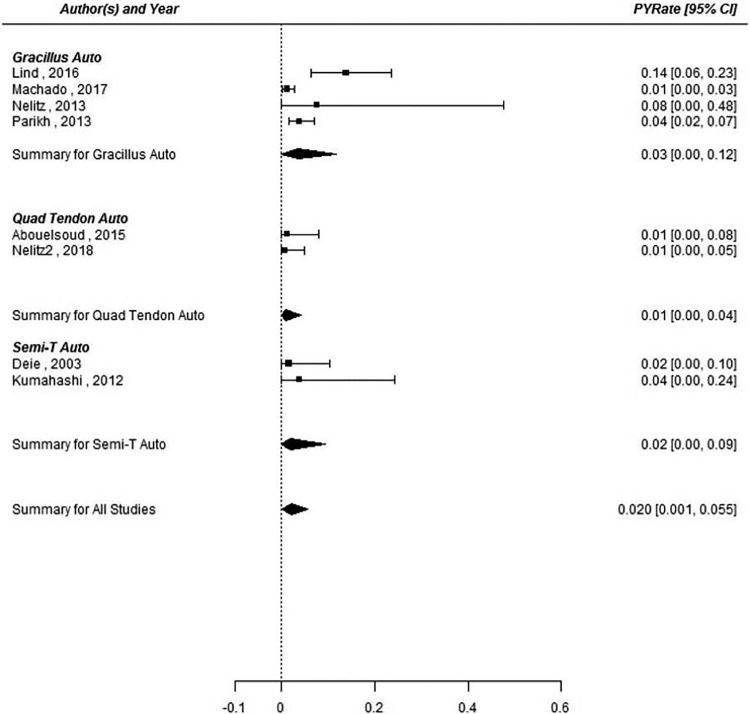
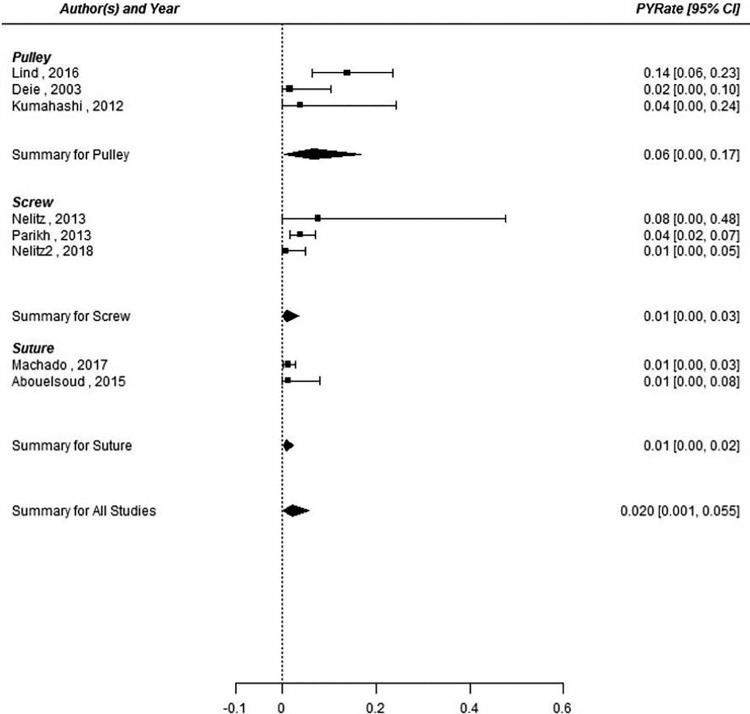
The most common postoperative, non–instability related complication was residual knee pain (n = 5; 3.8%). No cases of premature physeal closure or growth disturbance were reported, whereas 3 cases of donor site pain were described (2.3%). Neither autograft choice (P > .804) nor method of femoral fixation (P > .416) influenced recurrent instability or overall complication rates (Figures 2 and 3).
Figure 2.
Forest plot for recurrent instability among graft type (gracilis, quadriceps, and semitendinosus) groups. Auto, autograft; PYRate, person-year rate; Quad, quadriceps; Semi-T, semitendinosus.
Figure 3.
Forest plot for recurrent instability among femur fixation (soft tissue pulley, interference screw, and suture anchor) groups. Pulley, soft tissue pulley; PYRate, person-year rate; Screw, interference screw; Suture, suture anchor.
Quality Assessment
The mean (±SD) MCMS was 62.4 ± 5.9 (range, 54-71). The majority of studies were retrospective reviews (n = 5; 71.4%) of a small number of cases (range, 6-35). All studies were level 3 (n = 1, 14.3%) or level 4 (n = 6, 85.7%) evidence.16
Discussion
In this systematic review evaluating outcomes of MPFL reconstruction in skeletally immature patients, we found that all graft types and fixation methods resulted in low recurrent instability rates with few complications and good clinical outcomes, and no statistical differences were found between groups. However, few high-quality studies were identified, and substantial heterogeneity was observed between studies. In contrast, literature examining MPFL reconstruction in adults is more expansive, including multiple randomized controlled trials.3,14,19 Overall, the quality of studies in the present literature evaluating outcomes after MPFL reconstruction in skeletally immature patients is limited and of generally low quality despite the relatively high rate of patellar dislocation in this age group.26 Based on this review, further investigation of the skeletally immature population is warranted given the high incidence of patellar instability in these patients and the high rate of persistent postoperative instability (15%).
Anatomic MPFL femoral fixation in skeletally immature patients may place the physis at risk, and technical modifications to avoid the physis have raised concerns about subsequent postoperative instability. The primary outcome measure seen in this review was recurrent instability, defined as recurrent dislocation or subluxation events. We noted 5 reported dislocations and 15 subluxation events following MPFL reconstruction, for a pooled recurrent instability rate of 15.2%. No cases of premature physeal growth arrest were reported.
The reported recurrent instability rate in this study is slightly higher than the rate in the adult MPFL reconstruction literature, where recurrent instability is consistently reported to be lower than 10%.7 Rates of reported recurrent instability following MPFL reconstruction in the pediatric literature range from 0% to 37.5%.1,11,12 Shah et al30 described various risk factors for postoperative redislocation, including limb malalignment, lateral tibial tuberosity, trochlear dysplasia, patella alta, and poor surgical technique. Lind et al12 reported 4 cases of patellar redislocation at 1-year follow-up, which were universally revised with semitendinosus tendon autograft via an adult reconstruction technique. Machado et al13 described 1 recurrent dislocation in their series of 35 pediatric MPFL reconstructions, although it is unclear whether a revision surgical procedure was performed. In a series of 179 MPFL reconstructions of both pediatric and adult patients, Parikh et al27 reported 8 redislocations (4.5%). Only 6 of these patients with recurrent instability were treated surgically (5 revision MPFL reconstructions and 1 lateral retinacular release), whereas 2 were managed conservatively with physical therapy and bracing. Of note, the authors found malpositioning of the femoral tunnel in 7 of these cases, which may have contributed to graft failure.
In the current series, patients with recurrent subluxation events without frank dislocation and those with positive clinical apprehension tests were exclusively managed nonoperatively. Additionally, no reports of premature physeal closure were found in the included studies. In a case report, Seitlinger et al29 described an MPFL reconstruction in a 14 year-old girl with gracilis tendon autograft and interference screw fixation that was complicated by physeal breach with a bone tunnel, ultimately leading to partial posterior physeal growth arrest and flexion deformity. Of note, serial long-leg radiographs assessing angular deformity were not obtained in any of the included studies, and this is an area that warrants further study. Pooled mean Kujala scores in our study improved from 59.1 to 84.6 following MPFL reconstruction, with only 1 study not reporting preoperative scores. Kujala scores consistently improved after MPFL reconstruction, supporting the efficacy of this procedure in skeletally immature patients.
A variety of autografts and allografts are described in the literature for use in MPFL reconstruction, including semitendinosus, gracilis, quadriceps, adductor magnus, and tibialis anterior tendon. Furthermore, artificial grafts have been used for MPFL reconstruction in a few small series.23,24 The most commonly used grafts in our study were gracilis autograft followed by quadriceps tendon, contributing to 60.6% and 31.1% of autografts, respectively. We found no relationship between choice of autograft and recurrent instability when comparing gracilis versus quadriceps (P = .887), gracilis versus semitendinosus (P = .916), and quadriceps versus semitendinosus (P = .804) groups. This finding is consistent with reports in the literature, as considerable debate persists regarding the most effective autograft for both skeletally immature and skeletally mature patients. Of note, no studies using allograft were included, although allograft is described and used for this extra-articular reconstruction.
The MPFL graft can be fixed to the patella with suture anchors, with interference screws, or through bone tunnels. Of the included studies, the most common mode of fixation was a single patellar bone tunnel in which the MPFL graft was looped. All cases that entailed quadriceps tendon autograft left the tendon insertion on the patella intact and reflected the graft 90° to the femoral insertion. Currently, no mode of patellar fixation has demonstrated superior outcomes in the published literature.7 Theoretically, the method of patellar fixation during MPFL reconstruction should not be chosen based on skeletal immaturity because no physes are placed in jeopardy. However, the size of the patella may influence fixation techniques in some scenarios.
Similar to patellar fixation, femoral graft fixation entails a variety of techniques. Interference screws or suture anchors provide secure fixation into the anatomic footprint of the MPFL and have been shown to be effective.1,13,20,21,27 Alternatively, the MPFL graft can be looped around anatomic structures such as the MCL or adductor magnus tendon.6,11,12 Although the soft tissue pulley technique does not place open physes at risk, it does not allow for anatomic reconstruction of the MPFL. The most common modes of femoral fixation in our study were interference screw (39.4%) followed by suture anchor (38.6%). We found no relationship between choice of femoral fixation and recurrent instability when comparing soft tissue pulley versus interference screw (P = .416), soft tissue pulley versus suture anchor (P = .435), and interference screw versus suture anchor (P = .746) groups. Similar to the choice of autograft, the most effective method of femoral fixation for patients with open physes was not revealed in our study.
The pooled non-stability-related complication rate was 9.8% in our study. This finding is consistent with previous literature, which reported an overall complication rate of 16.2% in patients younger than 21 years undergoing MPFL reconstruction.27 The most common complication was knee pain postoperatively (3.8%) followed by donor site pain (2.3%), knee swelling (2.3%), and stiffness (0.8%). Overtightening of the graft is a known complication of MPFL reconstruction, leading to knee stiffness and pain postoperatively. For a successful reconstruction, it is critical to obtain physiologic tension on the graft during knee range of motion. Stephen et al31 stated that 2 N of pressure on the graft is all that is required to obtain normal patellar tracking. Fixation of the graft at various knee flexion angles has been described, and the most effective tensioning position has yet to be determined. Although not seen in our cohort, patellar fracture is a described complication of MPFL reconstruction and has been attributed to the use of large femoral bone tunnels or patellar bone tunnels used for patellar fixation.7,19,26 Parikh et al27 reported 6 patellar fractures in which patellar fixation was achieved through the use of 2 connecting perpendicular bone tunnels. Although this is a rare complication, the results may influence surgeons to use surgical techniques that do not require bone tunnels. Finally, the 3 reported cases of autograft donor site pain were described by Machado et al13 in their series of 35 skeletally immature patients treated by use of gracilis autograft for MPFL reconstruction.
The limitations of the current study include those inherent to all systematic reviews. A risk of publication bias is present because only published studies were queried. Furthermore, we were reliant on the authors of the selected articles to accurately collect and report their results. None of the included studies used full-length lower extremity radiographs to assess leg lengths and coronal angular alignment and instead relied on clinical examination or patient reports to determine growth arrest that would result in limb-length discrepancy or angular deformity. Although the relatively short follow-up period may be sufficient to assess stability, longer follow-up may be needed to reveal cases of physeal arrest or patellofemoral arthritis secondary to graft overtightening. Our review is also limited by the lack of high-quality studies included for analysis, the majority of which were retrospective case series of a small number of patients. Non–English language articles were excluded, which may have removed eligible studies from our literature search. Finally, given the low numbers of cases available in the literature, the statistical analysis is likely underpowered to detect between-group differences according to graft fixation type, and results may be subject to type II error.
Conclusion
The results of this systematic review suggest that MPFL reconstruction in skeletally immature patients is a viable treatment option, with significant improvement in patient-reported outcomes and a redislocation rate of less than 5% at nearly 5-year follow-up. Further high-quality research is needed to determine optimal graft options and surgical technique while considering stability, donor site morbidity, and potential injury to the neighboring physis.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: K.R.D. has received educational support from Smith & Nephew and grants from DJO. R.W.W. has received educational support from Smith & Nephew, Arthrex, and Medical Device Business Services. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Abouelsoud MM, Abdelhady A, Elshazly O. Anatomic physeal-sparing technique for medial patellofemoral ligament reconstruction in skeletally immature patients with ligamentous laxity. Eur J Orthop Surg Traumatol. 2015;25(5):921–926. [DOI] [PubMed] [Google Scholar]
- 2. Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med. 2000;28(4):472–479. [DOI] [PubMed] [Google Scholar]
- 3. Bitar AC, D’Elia CO, Demange MK, Viegas AC, Camanho GL. Randomized prospective study on traumatic patellar dislocation: conservative treatment versus reconstruction of the medial patellofemoral ligament using the patellar tendon, with a minimum of two years of follow-up. Rev Bras Ortop. 2011;46(6):675–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Camp CL, Krych AJ, Dahm DL, Levy BA, Stuart MJ. Medial patellofemoral ligament repair for recurrent patellar dislocation. Am J Sports Med. 2010;38(11):2248–2254. [DOI] [PubMed] [Google Scholar]
- 5. Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10(1):2–11. [DOI] [PubMed] [Google Scholar]
- 6. Deie M, Ochi M, Sumen Y, Yasumoto M, Kobayashi K, Kimura H. Reconstruction of the medial patellofemoral ligament for the treatment of habitual or recurrent dislocation of the patella in children. J Bone Joint Surg Br. 2003;85(6):887–890. [PubMed] [Google Scholar]
- 7. Diduch DR, Kandil A, Burrus MT. Lateral patellar instability in the skeletally mature patient: evaluation and surgical management. J Am Acad Orthop Surg. 2018;26(12):429–439. [DOI] [PubMed] [Google Scholar]
- 8. Fithian DC, Paxton EW, Stone ML. et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(5):1114–1121. [DOI] [PubMed] [Google Scholar]
- 9. Hennrikus W, Pylawka T. Patellofemoral instability in skeletally immature athletes. J Bone Joint Surg Am. 2013;95(2):176–183. [PubMed] [Google Scholar]
- 10. Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9(2):159–163. [DOI] [PubMed] [Google Scholar]
- 11. Kumahashi N, Kuwata S, Tadenuma T, Kadowaki M, Uchio Y. A “sandwich” method of reconstruction of the medial patellofemoral ligament using a titanium interference screw for patellar instability in skeletally immature patients. Arch Orthop Trauma Surg. 2012;132(8):1077–1083. [DOI] [PubMed] [Google Scholar]
- 12. Lind M, Enderlein D, Nielsen T, Christiansen SE, Fauno P. Clinical outcome after reconstruction of the medial patellofemoral ligament in paediatric patients with recurrent patella instability. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):666–671. [DOI] [PubMed] [Google Scholar]
- 13. Machado SAF, Pinto RAP, Antunes AJAM, de Oliveira PAR. Patellofemoral instability in skeletally immature patients. Porto Biomedical Journal. 2017;2(4):120–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mackay ND, Smith NA, Parsons N, Spalding T, Thompson P, Sprowson AP. Medial patellofemoral ligament reconstruction for patellar dislocation: a systematic review. Orthop J Sports Med. 2014;2(8):2325967114544021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Maenpaa H, Lehto MU. Patellofemoral osteoarthritis after patellar dislocation. Clin Orthop Relat Res. 1997;339:156–162. [DOI] [PubMed] [Google Scholar]
- 16. Marx RG, Wilson SM, Swiontkowski MF. Updating the assignment of levels of evidence. J Bone Joint Surg Am. 2015;97(1):1–2. [DOI] [PubMed] [Google Scholar]
- 17. McInnes MDF, Moher D, Thombs BD. et al. Preferred Reporting Items for a Systematic Review and Meta-Analysis of Diagnostic Test Accuracy Studies: the PRISMA-DTA Statement. JAMA. 2018;319(4):388–396. [DOI] [PubMed] [Google Scholar]
- 18. McNeilan RJ, Everhart JS, Mescher PK, Abouljoud M, Magnussen RA, Flanigan DC. Graft choice in isolated medial patellofemoral ligament reconstruction: a systematic review with meta-analysis of rates of recurrent instability and patient-reported outcomes for autograft, allograft, and synthetic options. Arthroscopy. 2018;34(4):1340–1354. [DOI] [PubMed] [Google Scholar]
- 19. Mikashima Y, Kimura M, Kobayashi Y, Miyawaki M, Tomatsu T. Clinical results of isolated reconstruction of the medial patellofemoral ligament for recurrent dislocation and subluxation of the patella. Acta Orthop Belg. 2006;72(1):65–71. [PubMed] [Google Scholar]
- 20. Nelitz M, Dreyhaupt J, Reichel H, Woelfle J, Lippacher S. Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents with open growth plates: surgical technique and clinical outcome. Am J Sports Med. 2013;41(1):58–63. [DOI] [PubMed] [Google Scholar]
- 21. Nelitz M, Dreyhaupt J, Williams SRM. Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents using a pedicled quadriceps tendon graft shows favourable results at a minimum of 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1210–1215. [DOI] [PubMed] [Google Scholar]
- 22. Nikku R, Nietosvaara Y, Aalto K, Kallio PE. Operative treatment of primary patellar dislocation does not improve medium-term outcome: a 7-year follow-up report and risk analysis of 127 randomized patients. Acta Orthop. 2005;76(5):699–704. [DOI] [PubMed] [Google Scholar]
- 23. Nomura E, Horiuchi Y, Kihara M. A mid-term follow-up of medial patellofemoral ligament reconstruction using an artificial ligament for recurrent patellar dislocation. Knee. 2000;7(4):211–215. [DOI] [PubMed] [Google Scholar]
- 24. Nomura E, Inoue M, Kobayashi S. Long-term follow-up and knee osteoarthritis change after medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2007;35(11):1851–1858. [DOI] [PubMed] [Google Scholar]
- 25. Ostermeier S, Holst M, Hurschler C, Windhagen H, Stukenborg-Colsman C. Dynamic measurement of patellofemoral kinematics and contact pressure after lateral retinacular release: an in vitro study. Knee Surg Sports Traumatol Arthrosc. 2007;15(5):547–554. [DOI] [PubMed] [Google Scholar]
- 26. Panni AS, Vasso M, Cerciello S. Acute patellar dislocation: what to do? Knee Surg Sports Traumatol Arthrosc. 2013;21(2):275–278. [DOI] [PubMed] [Google Scholar]
- 27. Parikh SN, Nathan ST, Wall EJ, Eismann EA. Complications of medial patellofemoral ligament reconstruction in young patients. Am J Sports Med. 2013;41(5):1030–1038. [DOI] [PubMed] [Google Scholar]
- 28. Sallay PI, Poggi J, Speer KP, Garrett WE. Acute dislocation of the patella: a correlative pathoanatomic study. Am J Sports Med. 1996;24(1):52–60. [DOI] [PubMed] [Google Scholar]
- 29. Seitlinger G, Moroder P, Fink C, Wierer G. Acquired femoral flexion deformity due to physeal injury during medial patellofemoral ligament reconstruction. Knee. 2017;24(3):680–685. [DOI] [PubMed] [Google Scholar]
- 30. Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40(8):1916–1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Stephen JM, Kaider D, Lumpaopong P, Deehan DJ, Amis AA. The effect of femoral tunnel position and graft tension on patellar contact mechanics and kinematics after medial patellofemoral ligament reconstruction. Am J Sports Med. 2014;42(2):364–372. [DOI] [PubMed] [Google Scholar]