Abstract
Introduction: Telemedicine represents an emerging model for the assessment and management of various neurological disorders.
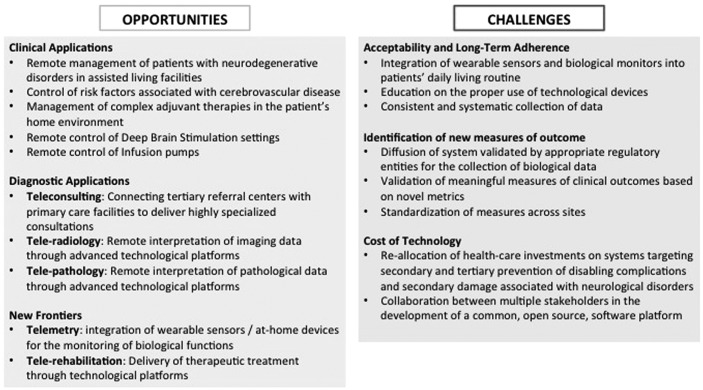
Methods: We sought to discuss opportunities and challenges for the integration of telemedicine in the management of common and uncommon neurological disorders by reviewing and appraising studies that evaluate telemedicine as a means to facilitate the access to care, deliver highly specialized visits, diagnostic consultations, rehabilitation, and remote monitoring of neurological disorders.
Results: Opportunities for telemedicine in neurological disorders include the replacement of or complement to in-office evaluations, decreased time between follow-up visits, reduction in disparities in access to healthcare, and promotion of education and training through interactions between primary care physicians and tertiary referral centers. Critical challenges include the integration of the systems for data monitoring with an easy-to-use, secure, and cost-effective platform that is both widely adopted by patients and healthcare systems and embraced by international scientific societies.
Conclusions: Multiple applications may spawn from a model based on digitalized healthcare services. Integrated efforts from multiple stakeholders will be required to develop an interoperable software platform capable of providing not only a holistic approach to care but also one that reduces disparities in the access to care.
Keywords: telemedicine, technology, telegenetics, telepathology, telerehabilitation
Introduction
As videoconferencing has become ubiquitous across the private and public sectors, telemedicine has also arisen at the forefront of clinical care. This technology has the potential to augment in-office evaluations, minimize disparities in access to healthcare, and decrease the amount of time between follow-up visits.1 These benefits ultimately stand to redesign the clinical workflow, which may streamline the management of complex medical conditions between tertiary referral centers and primary care physicians.2
Methods
We sought to critically assess opportunities and challenges for telemedicine in neurological disorders. Telemedicine was defined as an interface in a virtual patient–physician relationship to provide primary and secondary care in neurodegenerative, cerebrovascular, neuro-oncological, and neuroinflammatory disorders; assist the remote management of deep brain stimulation (DBS), transcranial direct current stimulation (tDCS), and infusion pumps; deliver highly specialized visits (telegenetics), diagnostic consultations (teleradiology and telepathology), or rehabilitative programs (telerehabilitation); and monitor motor and nonmotor functions in an ecologically valid environment (telemetry). Attention was devoted to the challenges associated with the integration of telemedicine into innovative models of care.
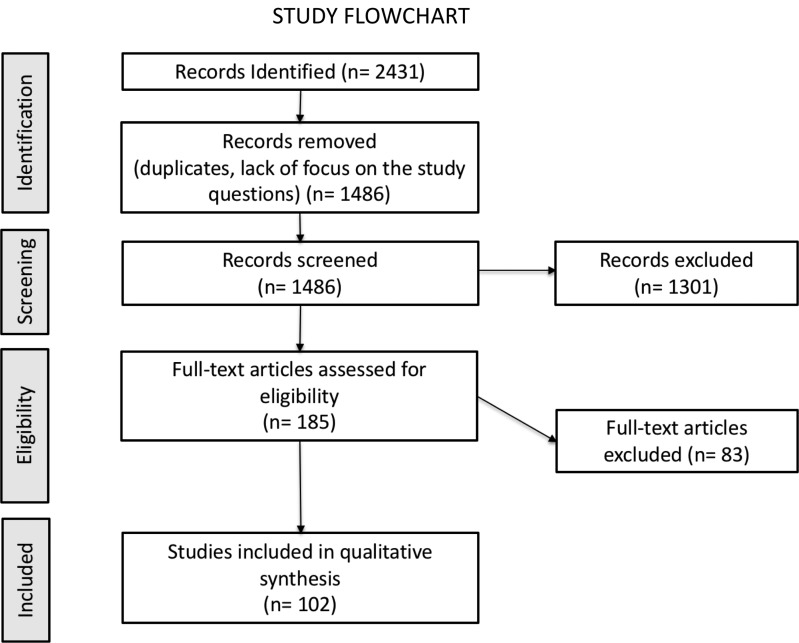
We considered articles involving human subjects published in English and indexed in PubMed between January 2000 and January 2018. Our MESH search terms included “telemedicine,” “telehealth,” “aging disorders,” “cerebrovascular diseases,” “stroke,” “hypertension,” “diabetes,” “oncology,” “neurooncology,” “multiple sclerosis,” “Parkinson's disease,” “deep brain stimulation,” “infusion systems,” “transcranial stimulation,” “genetics,” “diagnosis,” “EEG,” “telemetry,” and “rehabilitation.” No restrictions were applied to gender, age, ethnicity, disease duration, or disease severity. The reference lists were additionally screened for pertinent studies not included in the original searching strategy. Abstracts were independently reviewed for eligibility criteria by one author and validated by at least one additional author. Relevant articles (Fig. 1 and Table 1) were analyzed according to the following themes: “Opportunities” and “Challenges” (Fig. 2).
Fig. 1.
Flowchart summarizing the results of the searching strategy.
Table 1.
Overview of the Main Evidences Supporting the “Opportunities” for Telemedicine
| FIELD OF APPLICATION | EVIDENCE |
|---|---|
| Parkinson disease | Videoconferencing may provide access to multidisciplinary medical care, reducing travel time, distance, and wait time in patients with PD living in unserved areas4 |
| Feasibility, acceptance, and effectiveness of a virtual exercise coach to promote daily walking in community-dwelling persons with PD91 | |
| Feasibility of remote physical assessment of PD patients undergoing rehabilitation92 | |
| Feasibility of remote evaluation and treatment of speech disorders in patients with PD88–90 | |
| Chronic diseases and depression | Telehealth nursing conducted by daily telemonitoring and remote sessions of problem-solving treatment for depression improve symptoms and reduce the number of emergency department visits compared to in-home nursing in elderly with chronic diseases and depression5 |
| Prevention of cerebrovascular diseases | Home blood pressure monitoring in patients with hypertension is associated with better morbidity and mortality when compared to standard office visits,8–13 although significantly more expensive.14 |
| Telemedicine may improve glycemic control and promote a healthy lifestyle in patients with types I and II diabetes mellitus15–17 | |
| Pediatric neuro-oncology | Videoconferencing and e-mail communications are available twinning tools between institutions in industrialized and developing countries. Twinning facilitates the implementation of multidisciplinary neuro-oncology programs in low-income countries35–38 |
| Multiple sclerosis | Telephone counseling and web-based home telehealth monitoring improves DMT adherence in patients living with MS39 |
| Telephone-based, teleconference or web-based interventions are effective means to increase physical activity and improve fatigue in MS41–44 | |
| Remote diagnosis and management of cognitive difficulties and depression in patients with MS45,47,48 | |
| Smartphone-based telerehabilitation has favorable effects on fatigue in MS40 | |
| The use of virtual reality to effectively administer physiotherapy and rehabilitation to individuals living with MS50,51 | |
| Advanced therapies (Deep brain stimulation, infusion systems, and transcranial direct current stimulation) | Feasibility of using telemedicine for DBS in patients with PD living in unserved areas55,56 |
| Feasibility of using telemedicine for LCIG initiation in patients with PD living in unserved areas57 | |
| Feasibility of remotely supervised tDCS in the treatment of MS-associated depression58 | |
| Stroke | Combination of video consultation, teleradiology, and high stroke tele-expertise on a on a 365/24/7 basis67,68 |
| Standard of care therapies for acute stroke are facilitated by telestroke, not only by increasing intravenous thrombolysis rates and prompt decisions on endovascular therapy but also with early triage and management of transient ischemic attacks and minor strokes68,69 | |
| Epilepsy | Tele-EEG (remote EEG consultation) allows for better access to specialized medical care, reduces the costs and the total time associated with testing70 |
| Feasibility of tele-EEG for obtaining clinician second opinions and off-line reviews of prerecorded data.72 | |
| Tele-EEG is an achievable, safe, timely and effective method of providing EEG services to hospitals in which neurophysiological services are not available.70,73 |
PD, Parkinson Disease; DMT, disease-modifying therapies; MS, multiple sclerosis; DBS, deep brain stimulation; LCIG, levodopa–carbidopa intestinal gel; tDCS, transcranial direct current stimulation; EEG, electroencephalogram.
Fig. 2.
Opportunities and challenges for telemedicine in neurological diseases.
Opportunities
Management of Diseases with High Social Impact
Aging disorders
Life expectancy is projected to increase dramatically in the ensuing decades demanding careful reallocation of healthcare resources.3 Telemedicine may offer a model by which to defray these expenditures for diseases related to aging, including dementia and other neurodegenerative disorders.2 Specifically, video-based telehealth visits may mitigate burdensome and costly transportation needs and also reduce waiting times for all stakeholders. The latter benefit may then aid in longitudinal, continuous monitoring, while potentially increasing the ecological validity of the clinical picture.4
In a randomized controlled trial (RCT) of elderly homebound individuals,5 a telehealthcare model delivered by trained nurses was compared with the standard-of-care of in-home nursing care. The telehealth model included daily acquisition of symptoms, body weight, sessions of problem-solving treatment for comorbid depression, and consultations with primary care physicians for changes in the treatment plan for chronic diseases. This study demonstrated that integrated telehealth service improved symptoms and reduced the number of emergency department visits in elderly patients with chronic diseases and depression.5
Cerebrovascular disorders
Cerebrovascular disorders require periodic evaluations to check efficacy, dose, and side effects of medications. Mobile- and web-based platforms have been leveraged in the secondary and tertiary prevention of these conditions with the goal of encouraging self-monitoring of hypertension, body weight, waist circumference, blood lipid profile, smoking, and glycemia.6,7 Randomized controlled studies suggest that home blood pressure monitoring may result in lower morbidity and mortality when compared with standard office visits.8–14 Moreover, a meta-analysis showed that home blood pressure telemonitoring improves hypertension and associated healthcare outcomes, although more expensive than the usual standard-of-care.14
A few trials utilized telemedicine to improve glycemic control in patients with types I and II diabetes mellitus.15–17 In these cases, telemedicine was delivered through video conferencing, web-based educational sessions, and remote contact with healthcare professionals, as well as frequent monitoring of blood glucose levels, body weight, and blood pressure.18
Neuro-oncological disorders
Teleoncology, an emerging model for the remote management of oncological disorders, has already been used in high-income countries with vast territories, such as the United States,19,20 Canada,21 and Australia.22 Teleoncology may serve multiple needs. First, to create virtual tumor boards between physicians operating in underserved areas and tertiary referral centers.19,23 Second, to guarantee access to genetic counseling, which is becoming the foundation of “precision-medicine”-based therapeutic approaches.24 Third, to improve the primary and secondary prevention of cancer. Fourth, to offer the possibility to patients living in rural areas to be enrolled in RCT.19 Fifth, to limit the impact of follow-up visits in the increasing population of cancer survivors. Traditional models require patients to travel from their homes to cancer centers for face-to-face evaluations. Innovative models suggest that routine follow-up visits can be conducted via telemedicine without undermining the patient satisfaction or compromising the clinical outcomes.25–27 And sixth, teleoncology addresses one of the critical unmet needs for the management of advanced-stage cancer, namely the feeling of abandonment associated with the transition from an active phase of cancer-fighting treatment to a passive phase of in-hospice palliative care.28 Moreover, teleoncology has the potential to address social and geographical disparities associated with uneven wealth and healthcare distribution in the era of globalization. While cancer mortality rates are decreasing in developed countries,29 significant differences persist within select areas of the world.30 The incorrect risk stratification and the scarcity of standardized treatment protocols contribute to the different survival rates observed.31
Of note, a study of pediatric brain tumors in India showed that over 25% of patients abandoned neuro-oncological treatments due to late diagnosis, complex multidisciplinary treatments, and lack of consistency in the management between different oncology centers.32
Within this context, telemedicine might facilitate communication between advanced oncological centers and local primary care facilities, as demonstrated by successful initiatives in children with cancer and other catastrophic diseases conducted in low-middle income countries.33,34 Strategic investments in innovative model of care could significantly improve different fields of oncology and neuro-oncology.35–38 To date, studies on teleneuro-oncology are mostly limited to the pediatric population.35–38 The success in this particular age group, however, brings the promise to improve the management of primary and secondary cerebral tumors in the entire population of patients with oncological disorders.
Multiple sclerosis
The successful management of patients with multiple sclerosis (MS) requires adherence to disease-modifying therapies (DMTs), individualized approach for patient-reported symptoms, and adequate control of disease comorbidities such as fatigue, depression, and cognitive impairment. Telemedicine has the potential to improve adherence to DMTs39 and management of debilitating symptoms such as fatigue. An open-label study combining telemonitoring and remote coaching detected favorable effects on fatigue in MS.40 A small RCT showed the feasibility and effectiveness of telephone-based, teleconference, or web-based interventions in increasing physical activity and reducing MS-related fatigue.41–44
Settle et al. reported the feasibility of automated neuropsychological assessments using internet-based application from the home environment of patients with MS,45 Mohr et al. administered telephone-based cognitive behavioral therapy for the treatment of MS-related depression,46,47 and Charvet et al. used a web-based, remotely supervised adaptive cognitive remediation intervention in MS.48,49 Virtual reality has been also used to administer physiotherapy and in-home rehabilitation with results comparable to in-person physical therapy.50,51
Remote Management of Neurological Disorders from High-Specialized Centers
DBS, infusion systems, and tDCS
While cost-effectiveness of DBS has been widely demonstrated,52–54 the clinical and surgical expertise required for this advanced neurosurgical technique remains a significant limit to its application in large urban centers. Telemedicine has the potential to curtail the need for in-person follow-up visits. Two recent studies from Canada55 and China56 confirmed the feasibility of using telemedicine for DBS in patients with Parkinson's Disease (PD). The number of video-guided visits directly correlated to the distance between home and the DBS referral center,55 allowing a significant reduction in the logistical burden associated with travel time and costs. Both patients and physicians reported a high degree of satisfaction with this interaction.56 In all cases, technical problems associated with video connections were negligible and resolved without complications.
A recent study from Sweden showed that telemedicine using a video communication system allows other advanced therapeutic options, such as Levodopa–carbidopa intestinal gel (LCIG) infusion, at home. This approach was found to be resource-efficient, technically feasible, well accepted, and satisfactory to patients, neurologists, and nurses alike.57 Similarly, the remote application of tDCS showed beneficial effects in the treatment of MS-associated depression. Kasschau et al. demonstrated the feasibility, safety, and reliability of remotely supervised tDCS and reported a high adherence rate that exceeded rates of adherence of clinic-based tDCS.58
Telegenetics
The management of rare genetic disorders includes three levels of care: (a) prediagnostic phase, (b) communication of the diagnosis accompanied by appropriate genetic counseling for patients and family members, and (c) multidisciplinary approach to deliver proper therapies and address potential complications associated with disease progression.59 Teleconsultation is a promising tool to provide counseling, diagnosis, monitoring, and rehabilitation of genetic disorders to satisfy these levels of care.
Telegenetics has the potential of limiting time and costs associated with traveling to ultra-specialized tertiary referral centers and facilitate a multidisciplinary approach via roundtable videoconference visits at which multiple specialists can take part.60–62 Several studies showed the potential of telegenetics as a modality to reach populations living in areas with limited access to information, treatment, and psychosocial support offered by genetic services.63–65
Telediagnosis
The application of telemedicine to radiology has had a relatively long track record of benefits, including cost-effectiveness, with pronounced concordance between conventional radiology and teleradiology regarding diagnostic accuracy and reliability.66
Telestroke is one of the most rapidly expanding applications of telemedicine that combines video consultation, teleradiology, and high stroke tele-expertise to provide continuous service to hospitals and patients.67,68 Telestroke not only increases the rate of intravenous thrombolysis and decisions on endovascular therapy but also provides early triage and management of transient ischemic attacks and minor strokes.68,69
Tele-EEG, which consists in remote EEG consultation, is another application for telediagnosis in neurological disorders.70 A Canadian study showed the feasibility of telephone-based EEG-data transmission.71 A more recent study proved the feasibility of tele-EEG for obtaining clinician's second opinions and off-line reviews of prerecorded data.72 Tele-EEG has shown to be a safe, timely, and effective method for providing EEG services to underserved hospitals.70,73
Telepathology consists of the practice of pathology by interpreting transmitted digital histologic images by pathologists at a long distance.74 In this process, the diagnosing pathologist has remote but direct control over the selection and magnification of histopathology glass slides.75,76 A recent study reported promising results from a nationwide telepathology consultation in China, built to solve problems of shortage of pathologists and subspecialty pathologists at underserved sites, and to improve pathology quality control.77
New Frontiers and Innovative Applications
Telemetry
Telemedicine is not merely remote communication via telephone or videoconferencing but also encompasses higher order transmission of data germane to a patient's health. Telemetry, defined as the “transmission of the readings of instruments to a remote location using wires, radio waves, or other means,” can be used to monitor patients using wearable sensors and mobile applications.78
Regarding the management of advanced therapies for PD, such as LCIG infusion and DBS, telemetry offers a powerful tool for increasing accessibility and effectiveness of these treatments. The possibility to remotely access important information such as battery consumption, electrode impedance, and stimulation parameters could be useful and timely, in particular, when patients report sudden and inexplicable clinical worsening, possibly due to battery exhaustion.79 Moreover, the implementation of telemetry with objective clinical measurements through wearable sensors and self-reported electronic questionnaires will increase the possibility of monitoring the health status of patients, ameliorating neurological symptoms.80 The next step in the path to telemedicine and telemetry integration consists of remote intervention on DBS and infusion systems programming. Jitkritsadakul et al.55 recently analyzed the possibility of an “indirect” intervention on DBS parameters, supervised by an expert physician through video-conferencing, and physically enacted directly by the patient or caregiver or, in a minority of cases, by a local physician or nurse.
DBS stimulation parameters and infusion systems parameters could also be modified directly from a remote location via a Bluetooth-based programming system installed at the patient's home.56,57,81
Telemetry also has applications in patients requiring intensive care, such as in the case of neoplastic diseases, wherein pharmacological treatments require continuous monitoring of adverse events (e.g., vomiting, dehydration, and so on) and vital signs (e.g., blood pressure, blood glucose levels, pulse rate, and so on).82,83
Regarding cerebrovascular diseases, safe administration of intravenous tissue-type plasminogen activator (tPA) in acute ischemic stroke requires adherence to thrombolysis protocols that could be improved through “telestroke” networks.67 These networks assist in the interpretation of neuroimaging findings84 to assure timely selection of tPA candidates.85,86
Telerehabilitation
Telerehabilitation, intended as a discipline involving remote delivery of different rehabilitation services, namely speech therapy and physiotherapy, has been widely examined in neurological disorders.87 Constantinescu et al.88 evaluated the level of agreement between online and face-to-face assessment of voice disorder in patients with PD, showing that the online assessment was as valid as in-person evaluations. The same authors89 as well as a different group90 found that treatment for speech disorder is feasible and potentially applicable to innovative rehabilitation techniques, such as the Lee Silverman Voice Treatment.
Telerehabilitation of motor functions has also been applied to PD. In a phase 1 nonrandomized clinical trial, Ellis et al.91 described the feasibility, acceptance, and effectiveness of a virtual exercise coach to promote daily walking in community-dwelling PD patients. The study found an improvement on walking speed, with good adherence to the virtual rehabilitation protocol. Russell et al.92 validated remote telemedicine system for the physical assessment of PD patients undergoing rehabilitation.
Telerehabilitation may improve the level of care in patients with cancer.93,94 Recent studies demonstrated the effectiveness of internet-based tailored exercise program for cancer survivors, which may improve functional capacity and cognition,95 as well as enhance strength and quality of life reducing pain and fatigue.96
Home-based telerehabilitation has also been introduced in stroke survivors, proving to be as effective as traditional rehabilitation techniques.97 Several studies showed promising results in clinical,98 kinematic,99 and neuroimaging endpoints97 in patients living away from healthcare facilities with a better cost-effectiveness profile.
Challenges
What should be Measured?
New possibilities in the field of telemedicine are offered by the development of wireless sensors, which may be combined with videoconferencing platforms. This innovative integrated technology bears the promise to dramatically change the physical assessment of patients with neurological and non-neurological disorders. For example, in PD the interactive nature of clinical scales conventionally used for quantification and rating of clinical symptoms (e.g., Movement Disorder Society Unified Parkinson's Disease Rating Scale)100 may create a challenge to implement via telemedicine.
Recent advances in wearable motion sensors allowed doctors to assess some of the most disabling physical symptoms of PD via videoconferencing platforms.46 While sensors may also assist the remote monitoring of PD and eliminate physicians' subjectivity in motor symptom evaluation,80,101 their implementation into PD patients' home environment remains to be explored. In this regard, an innovative platform for continuous effective assessment and monitoring of motor status in PD and other neurodegenerative diseases has been recently developed to assess symptoms such as bradykinesia, hypokinesia, resting tremor, rigidity, and postural instability along with information provided by patients such as diet and adherence to medications.102
The ultimate goal is to provide a holistic view of the patient status that might assist in the monitoring of disease progression and the appropriate management of treatments.
In MS, the expanded disability status scale (EDSS) is the primary clinical tool currently used to assess disability. The scale is time-consuming and requires a dedicated neurological examination, but also provides valuable information about disease progression. Researchers attempted to remotely perform the EDSS neurological examination using a webcam-based approach with the patient in their home environment. The ability to detect cerebellar and brainstem and sensory abnormalities was inferior to hands-on EDSS.39,40 A modification of the scale to focus on visual observations of the functions of the brainstem, the cerebellum, and the sensory system will be needed to obtain comprehensive information about the patient level of disability.
Acceptability and Long-Term Adherence
Regarding body-worn sensors, patient acceptability is a critical aspect. Without both physician's and patient's cooperation, these systems will not be able to provide the holistic view needed to increase patient monitoring. Many studies examined the accuracy of these sensor systems without addressing aspects related to the comfort and acceptance of these systems. Fisher et al.103 focused on the patient feedback found a negative correlation between prolonged wearing and comfort. Still, patients wore the sensors as requested for the majority of their active day.
Although promising, there remains a limited number of studies evaluating the application of wearable sensors in the patients' home environment for continuous monitoring.18 More studies are needed to examine the long-term effect of wearable systems on patients' quality of life, as well as the cost-benefit ratio of hardware and software platforms for implementation of telemedicine as a standard of care.1 Finally, the increasing ability to deliver care remotely could undermine one of the most cardinal principle of medicine, namely the therapeutic alliance between patients and physicians.104
Cost of Technologies and their Integration into Difficult Environments
Another challenge for the widespread diffusion of telemedicine is the cost of technologies, and the difficulty of integrating them into challenging environments such as in the home of elderly patients, communities with low educational status, low-middle income countries, and rural areas with incomplete or absent technology penetration.105 However, given the significant advantages associated with the use of telehealth, further studies and applications have been advocated by international societies.106
Conclusions
Integration of telemedicine and telemetry into clinical practice represents one of the main challenges of modern medicine. While widespread access to the internet and portable technologies offer the opportunity for managing complications associated with chronic conditions in a home-based, patient-centered model of care, combined efforts from multiple stakeholders are required to develop an interoperable software platform capable of providing not only a holistic approach to care but also one that reduces disparities in the access to care in an easy-to-use, secure, and cost-effective ecosystem. The limitation of this review consists of its narrative architecture; hence, further systematic studies are requested to better clarify the application of telemedicine to neurology.
Acknowledgment
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure Statement
Martina Chirra: no conflict of interest; Linsdey Wattley: no conflict of interest; Leonard Sokol: no conflict of interest; Elizabeth Keeling: no conflict of interest; Simona Maule: no conflict of interest; Gabriele Sobrero: no conflict of interest; Carlo Alberto Artusi: he has received travel grants for attending courses and congresses from Zambon and Boston Scientific; Alberto Romagnolo: grant support and speaker's honoraria from AbbVie, speaker honoraria from Chiesi Farmaceutici, and travel grants from Lusofarmaco and UCB Pharma; Maurizio Zibetti: he is speaker and has received consulting honoraria from Medtronic, Lundbeck, and AbbVie; Leonardo Lopiano: has received honoraria for advisory board, lecturing and travel grants from AbbVie, UCB, Zambon, Chiesi, Medtronic, Doc, Allergan, and Bial; Alberto J Espay: he has received grant support from the NIH, Great Lakes Neurotechnologies, and the Michael J Fox Foundation; personal compensation as a consultant/scientific advisory board member for Abbvie, TEVA, Impax, Acadia, Acorda, Cynapsus/Sunovion, Lundbeck, and USWorldMeds; publishing royalties from Lippincott Williams & Wilkins, Cambridge University Press, and Springer; and honoraria from Abbvie, UCB, USWorldMeds, Lundbeck, Acadia, the American Academy of Neurology, and the Movement Disorders Society; Luca Marsili: no conflict of interest; Ahmed Z Obeidat: he is supported by the National Multiple Sclerosis Society, Grant: #CF-1607-25342; Aristide Merola: he is supported by NIH (KL2 TR001426) and has received speaker honoraria from CSL Behring, Cynapsus Therapeutics, and AbbVie. He has received grant support from Lundbeck and Abbott.
All the coauthors listed above gave their final approval of this article version and agreed to conditions noted on the Authorship Agreement Form.
References
- 1. Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med 2017;377:1585–1592 [DOI] [PubMed] [Google Scholar]
- 2. Pedrosa F, Shaikh F, Rivera G, et al. . The impact of prospective telemedicine implementation in the management of childhood acute lymphoblastic leukemia in recife, Brazil. Telemed J E Health 2017;23:863–867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stenberg K, Hanssen O, Edejer TT, et al. . Financing transformative health systems towards achievement of the health Sustainable Development Goals: A model for projected resource needs in 67 low-income and middle-income countries. Lancet Glob Health 2017;5:e875–e887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pretzer-Aboff I, Prettyman A. Implementation of an integrative holistic healthcare model for people living with Parkinson's disease. Gerontologist 2015;55:S146–S153 [DOI] [PubMed] [Google Scholar]
- 5. Gellis ZD, Kenaley BL, Ten Have T. Integrated telehealth care for chronic illness and depression in geriatric home care patients: The Integrated Telehealth Education and Activation of Mood (I-TEAM) study. J Am Geriatr Soc 2014;62:889–895 [DOI] [PubMed] [Google Scholar]
- 6. Neubeck L, Cartledge S, Dawkes S, et al. . Is there an app for that? Mobile phones and secondary prevention of cardiovascular disease. Curr Opin Cardiol 2017;32:567–571 [DOI] [PubMed] [Google Scholar]
- 7. Rehman H, Kamal AK, Sayani S, et al. . Using mobile health (mHealth) technology in the management of diabetes mellitus, physical inactivity, and smoking. Curr Atheroscler Rep 2017;19:16. [DOI] [PubMed] [Google Scholar]
- 8. Cappuccio FP, Kerry SM, Forbes L, et al. . Blood pressure control by home monitoring: Meta-analysis of randomised trials. BMJ 2004;329:145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Glynn LG, Murphy AW, Smith SM, et al. . Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev 2010;3:CD005182. [DOI] [PubMed] [Google Scholar]
- 10. Bray EP, Holder R, Mant J, et al. . Does self-monitoring reduce blood pressure? Meta-analysis with meta-regression of randomized controlled trials. Ann Med 2010;42:371–386 [DOI] [PubMed] [Google Scholar]
- 11. Agarwal R, Bills JE, Hecht TJ, et al. . Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hyper- tension control: A systematic review and meta-analysis. Hypertension 2011;57:29–38 [DOI] [PubMed] [Google Scholar]
- 12. Ward AM, Takahashi O, Stevens R, et al. . Home measurement of blood pressure and cardiovascular disease: Systematic review and meta-analysis of prospective studies. J Hypertens 2012;30:449–456 [DOI] [PubMed] [Google Scholar]
- 13. Stergiou GS, Siontis KC, Ioannidis JP. Home blood pressure as a cardiovascular outcome predictor: It's time to take this method seriously. Hypertension 2010;55:1301–1303 [DOI] [PubMed] [Google Scholar]
- 14. Omboni S, Gazzola T, Carabelli G, et al. . Clinical usefulness and cost effectiveness of home blood pressure telemonitoring: Meta-analysis of randomized controlled studies. J Hypertens 2013;31:455–467 [DOI] [PubMed] [Google Scholar]
- 15. Lee SWH, Ooi L, Lai YK. Telemedicine for the Management of glycemic control and clinical outcomes of type 1 diabetes mellitus: A systematic review and meta-analysis of randomized controlled studies. Front Pharmacol 2017;8:330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bashshur RL, Shannon GW, Smith BR, et al. . The empirical evidence for the telemedicine intervention in diabetes management. Telemed J E Health 2015;21:321–354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Health Quality Ontario. Home telemonitoring for type 2 diabetes: An evidence-based analysis. Ont Health Technol Assess Ser 2009;9:1–38 [PMC free article] [PubMed] [Google Scholar]
- 18. Marcolino MS, Oliveira JAQ, D'Agostino M, et al. . The impact of mHealth interventions: Systematic review of systematic reviews. JMIR Mhealth Uhealth 2018;6:e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Shalowitz DI, Smith AG, Bell MC, Gibb RK. Teleoncology for gynecologic cancers. Gynecol Oncol 2015;139:172–177 [DOI] [PubMed] [Google Scholar]
- 20. Doolittle GC, Spaulding AO, Williams AR. The decreasing cost of telemedicine and telehealth. Telemed J E Health 2011;17:671–675 [DOI] [PubMed] [Google Scholar]
- 21. Palkhivala A. Canada develops models of teleoncology. J Natl Cancer Inst 2011;103:1566–1568 [DOI] [PubMed] [Google Scholar]
- 22. Sabesan S. Specialist cancer care through telehealth models. Aust J Rural Health 2015;23:19.–23. [DOI] [PubMed] [Google Scholar]
- 23. Salami AC, Barden GM, Castillo DL, et al. . Establishment of a regional virtual tumor board program to improve the process of care for patients with hepatocellular carcinoma. J Oncol Pract 2015;11:e66–e74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. American Society of Clinical Oncology. The State of Cancer Care in America, 2016: A Report by the American Society of Clinical Oncology. J Oncol Pract 2016;12:339–383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dickinson R, Hall S, Sinclair JE, Bond C, Murchie P. Using technology to deliver cancer follow-up: A systematic review. BMC Cancer 2014;14:311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Boele FW, van Uden-Kraan CF, Hilverda K, et al. . Neuro-oncology family caregivers' view on keeping track of care issues using eHealth systems: It's a question of time. J Neurooncol 2017;134:157–167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Boele FW, Klein M, Verdonck-de Leeuw IM, et al. . Internet-based guided self-help for glioma patients with depressive symptoms: A randomized controlled trial. J Neurooncol 2018;137:191–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Worster B, Swartz K. Telemedicine and palliative care: An increasing role in supportive oncology. Curr Oncol Rep 2017;19:37. [DOI] [PubMed] [Google Scholar]
- 29. Hashim D, Boffetta P, La Vecchia C, et al. . The global decrease in cancer mortality: Trends and disparities. Ann Oncol 2016;27:926–933 [DOI] [PubMed] [Google Scholar]
- 30. Vrdoljak E, Bodoky G, Jassem J, et al. . Cancer Control in Central and Eastern Europe: Current situation and recommendations for improvement. Oncologist 2016;21:1183–1190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rajagopal R, Abd-Ghafar S, Ganesan D, et al. . Challenges of Treating Childhood Medulloblastoma in a Country With Limited Resources: 20 Years of Experience at a Single Tertiary Center in Malaysia. J Glob Oncol 2016;3:143–156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Suresh SG, Srinivasan A, Scott JX, et al. . Profile and outcome of pediatric brain tumors—experience from a tertiary care pediatric oncology Unit in South India. J Pediatr Neurosci 2017;12:237–244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ribeiro RC. Improving survival of children with cancer worldwide: The St. Jude International Outreach Program approach. Stud Health Technol Inform 2012;172:9–13 [PubMed] [Google Scholar]
- 34. Adler E, Alexis C, Ali Z, et al. . Bridging the Distance in the Caribbean: Telemedicine as a means to build capacity for care in paediatric cancer and blood disorders. Stud Health Technol Inform 2015;209:1–8 [PubMed] [Google Scholar]
- 35. Qaddoumi I, Mansour A, Musharbash A, et al. . Impact of telemedicine on pediatric neuro-oncology in a developing country: The Jordanian-Canadian experience. Pediatr Blood Cancer 2007;48:39–43 [DOI] [PubMed] [Google Scholar]
- 36. Qaddoumi I, Musharbash A, Elayyan M, et al. . Closing the survival gap: Implementation of medulloblastoma protocols in a low-income country through a twinning program. Int J Cancer 2008;122:1203–1206 [DOI] [PubMed] [Google Scholar]
- 37. Qaddoumi I, Bouffet E. Supplementation of a successful pediatric neuro-oncology telemedicine-based twinning program by e-mails. Telemed J E Health 2009;15:975–982 [DOI] [PubMed] [Google Scholar]
- 38. Al-Qudimat MR, Day S, Almomani T, Odeh D, Qaddoumi I. Clinical nurse coordinators: A new generation of highly specialized oncology nursing in Jordan. J Pediatr Hematol Oncol 2009;31:38–41 [DOI] [PubMed] [Google Scholar]
- 39. Turner AP, Sloan AP, Kivlahan DR, et al. . Telephone counseling and home telehealth monitoring to improve medication adherence: Results of a pilot trial among individuals with multiple sclerosis. Rehabil Psychol 2014;59:136–146 [DOI] [PubMed] [Google Scholar]
- 40. D'hooghe M, Van Gassen G, Kos D, et al. . Improving fatigue in multiple sclerosis by smartphone-supported energy management: The MS TeleCoach feasibility study. Mult Scler Relat Disord 2018;22:90–96 [DOI] [PubMed] [Google Scholar]
- 41. Turner AP, Hartoonian N, Sloan AP, et al. . Improving fatigue and depression in individuals with multiple sclerosis using telephone-administered physical activity counseling. J Consult Clin Psychol 2016;84:297. [DOI] [PubMed] [Google Scholar]
- 42. Finlayson M, Preissner K, Cho C, et al. . Randomized trial of a teleconference-delivered fatigue management program for people with multiple sclerosis. Mult Scler J 2011;17:1130–1140 [DOI] [PubMed] [Google Scholar]
- 43. Moss-Morris R, McCrone P, Yardley L, et al. . A pilot randomised controlled trial of an Internet-based cognitive behavioural therapy self-management programme (MS Invigor8) for multiple sclerosis fatigue. Behav Res Ther 2012;50:415–421 [DOI] [PubMed] [Google Scholar]
- 44. Dlugonski D, Motl RW, Mohr DC, et al. . Internet-delivered behavioral intervention to increase physical activity in persons with multiple sclerosis: Sustainability and secondary outcomes. Psychol Health Med 2012;17:636–651 [DOI] [PubMed] [Google Scholar]
- 45. Settle JR, Robinson SA, Kane R, et al. . Remote cognitive assessments for patients with multiple sclerosis: A feasibility study. Mult Scler J 2015;21:1072–1079 [DOI] [PubMed] [Google Scholar]
- 46. Mohr DC, Hart SL, Julian L, et al. . Telephone-administered psychotherapy for depression. Arch Gener Psychiatry 2005;62:1007–1014 [DOI] [PubMed] [Google Scholar]
- 47. Mohr DC, Hart S, Vella L. Reduction in disability in a randomized controlled trial of telephone-administered cognitive-behavioral therapy. Health Psychol 2007;26:554. [DOI] [PubMed] [Google Scholar]
- 48. Charvet LE, Yang J, Shaw MT, et al. . Cognitive function in multiple sclerosis improves with telerehabilitation: Results from a randomized controlled trial. PLoS One 2017;12:e0177177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Bogosian A, Chadwick P, Windgassen S, et al. . Distress improves after mindfulness training for progressive MS: A pilot randomised trial. Mult Scler J 2015;21:1184–1194 [DOI] [PubMed] [Google Scholar]
- 50. Gutiérrez RO, Galán Del Río F, Cano de la Cuerda R, et al. . A telerehabilitation program by virtual reality-video games improves balance and postural control in multiple sclerosis patients. NeuroRehabilitation 2013;33:545–554 [DOI] [PubMed] [Google Scholar]
- 51. Paul L, Coulter EH, Miller L, et al. . Web-based physiotherapy for people moderately affected with Multiple Sclerosis; quantitative and qualitative data from a randomized, controlled pilot study. Clin Rehabil 2014;28:924–935 [DOI] [PubMed] [Google Scholar]
- 52. Hariz M. Twenty-five years of deep brain stimulation: Celebrations and apprehensions. Mov Disord 2012;27:930–933 [DOI] [PubMed] [Google Scholar]
- 53. Pietzsch JB, Garner AM, Marks WJ., Jr. Cost-Effectiveness of Deep Brain Stimulation for Advanced Parkinson's Disease in the United States. Neuromodulation 2016;19:689–697 [DOI] [PubMed] [Google Scholar]
- 54. Fundament T, Eldridge PR, Green AL, et al. . Deep Brain Stimulation for Parkinson's disease with early motor complications: A UK cost-effectiveness analysis. PLoS One 2016;11:e0159340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Jitkritsadakul O, Rajalingam R, Toenjes C, et al. . Tele-health for patients with deep brain stimulation: The experience of the Ontario Telemedicine Network. Mov Disord 2018;33:491–492 [DOI] [PubMed] [Google Scholar]
- 56. Chen Y, Hao H, Chen H, Li L. The study on a telemedicine interaction mode for Deep Brain Stimulation postoperative follow-up. Conf Proc IEEE Eng Med Biol Soc 2015;2015:186–189 [DOI] [PubMed] [Google Scholar]
- 57. Willows T, Dizdar N, Nyholm D, et al. . Initiation of Levodopa-Carbidopa Intestinal Gel Infusion Using Telemedicine (Video Communication System) Facilitates Efficient and Well-Accepted Home Titration in Patients with Advanced Parkinson's Disease. J Parkinsons Dis 2017;7:719–728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Kasschau M, Reisner J, Sherman K, et al. . Transcranial direct current stimulation is feasible for remotely supervised home delivery in multiple sclerosis. Neuromodulation 2016;19:824–831 [DOI] [PubMed] [Google Scholar]
- 59. Sokol LL, Young MJ, Jankovic J. Counseling at-risk Parkinson's disease cohorts: Integrating emerging evidence. Curr Genet Med Rep 2017;5:100–107 [Google Scholar]
- 60. Gray J, Brain K, Iredale R, et al. . A pilot study of telegenetics. J Telemed Telecare 2000;6:245–247 [DOI] [PubMed] [Google Scholar]
- 61. Mitchell JA, Demiris G. Telegenetics: The next phase in the provision of genetics services? Genet Med 2005;7:1–2 [DOI] [PubMed] [Google Scholar]
- 62. Vrečar I, Hristovski D, Peterlin B. Telegenetics: An update on availability and use of telemedicine in clinical genetics service. J Med Syst 2017;41:21. [DOI] [PubMed] [Google Scholar]
- 63. Godard B, Kääriäinen H, Kristoffersson U, et al. . Provision of genetic services in Europe: Current practices and issues. Eur J Hum Genet 2003;2:S13–S48 [DOI] [PubMed] [Google Scholar]
- 64. Lea DH. A new world view of genetics service models. Online J Issues Nurs 2000;5:5. [PubMed] [Google Scholar]
- 65. Hawkins AK, Hayden MR. A grand challenge: Providing benefits of clinical genetics to those in need. Genet Med 2011;13:197–200 [DOI] [PubMed] [Google Scholar]
- 66. Bashshur RL, Krupinski EA, Thrall JH, Bashshur N. The empirical foundations of teleradiology and related applications: A review of the evidence. Telemed J E Health 2016;22:868–898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Wechsler LR, Demaerschalk BM, Schwamm LH, et al. . Telemedicine quality and outcomes in stroke: A Scientific Statement for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2017;48:e3–e25 [DOI] [PubMed] [Google Scholar]
- 68. Dumitrascu OM, Demaerschalk BM. Telestroke. Curr Cardiol Rep 2017;19:85. [DOI] [PubMed] [Google Scholar]
- 69. Blacquiere D, Lindsay MP, Foley N, et al. . Heart and Stroke Foundation Canadian Stroke Best Practice Committees. Canadian Stroke Best Practice Recommendations: Telestroke Best Practice Guidelines Update 2017. Int J Stroke 2017;12:886–895 [DOI] [PubMed] [Google Scholar]
- 70. Campos C, Caudevilla E, Alesanco A, et al. . Setting up a telemedicine service for remote real-time video-EEG consultation in La Rioja (Spain). Int J Med Inform 2012;81:404–414 [DOI] [PubMed] [Google Scholar]
- 71. House AM. Telemedicine in Canada. Can Med Assoc J 1977;117:386–388 [PMC free article] [PubMed] [Google Scholar]
- 72. Patterson V. Teleneurology. J Telemed Telecare 2005;11:55–59 [DOI] [PubMed] [Google Scholar]
- 73. Coates S, Clarke A, Davison G, et al. . Tele-EEG in the UK: A report of over 1,000 patients. J Telemed Telecare 2012;18:243–246 [DOI] [PubMed] [Google Scholar]
- 74. Wiley CA, Murdoch G, Parwani A, et al. . Interinstitutional and interstate teleneuropathology. J Pathol Inform 2011;2:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Bashshur RL, Krupinski EA, Weinstein RS, et al. . The empirical foundations of telepathology: Evidence of feasibility and intermediate effects. Telemed J E Health 2017;23:155–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Szymas J, Wolf G, Papierz W, Jarosz B, Weinstein RS. Online Internet-based robotic telepathology in the diagnosis of neuro-oncology cases: A teleneuropathology feasibility study. Hum Pathol 2001;32:1304–1308 [DOI] [PubMed] [Google Scholar]
- 77. Chen J, Jiao Y, Lu C, et al. . A nationwide telepathology consultation and quality control program in China: Implementation and result analysis. Diagn Pathol 2014;9:S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. MeSH Descriptor Data. Telemetry. Available at https://meshb.nlm.nih.gov/record/ui?name=Telemetry/ (last accessed March31, 2018)
- 79. Artusi CA, Merola A, Espay AJ, et al. . Parkinsonism-hyperpyrexia syndrome and deep brain stimulation. J Neurol 2015;262:2780–2782 [DOI] [PubMed] [Google Scholar]
- 80. Heldman D, Harris D, Felong T, et al. . Telehealth Management of Parkinson's Disease Using Wearable Sensors: An Exploratory Study. In: 69th Annual Meeting of the American Academy of Neurology, Boston, MA, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Chen Y, Hao H, Chen H, et al. . The study on a real-time remote monitoring system for Parkinson's disease patients with deep brain stimulators. Conf Proc IEEE Eng Med Biol Soc 2014;2014:1358–1361 [DOI] [PubMed] [Google Scholar]
- 82. Peterson SK, Shinn EH, Basen-Engquist K, et al. . Identifying early dehydration risk with home-based sensors during radiation treatment: A feasibility study on patients with head and neck cancer. J Natl Cancer Inst Monogr 2013;2013:162–168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Yilmaz T, Foster R, Hao Y. Detecting vital signs with wearable wireless sensors. Sensors 2010;10:10837–10862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Demaerschalk BM, Bobrow BJ, Raman R, et al. . CT interpretation in a telestroke network: Agreement among a spoke radiologist, hub vascular neurologist, and hub neuroradiologist. Stroke 2012;43:3095–3097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Meyer BC, Raman R, Hemmen T, et al. . Efficacy of site-independent telemedicine in the STRokE DOC trial: A randomised, blinded, prospective study. Lancet Neurol 2008;7:787–795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Müller-Barna P, Hubert GJ, Boy S, et al. . TeleStroke units serving as a model of care in rural areas: 10-year experience of the TeleMedical project for integrative stroke care. Stroke 2014;45:2739–2744 [DOI] [PubMed] [Google Scholar]
- 87. Agostini M, Moja L, Banzi R, et al. . Telerehabilitation and recovery of motor function: A systematic review and meta-analysis. J Telemed Telecare 2015;21:202–213 [DOI] [PubMed] [Google Scholar]
- 88. Constantinescu G, Theodoros D, Russell T, et al. . Assessing disordered speech and voice in Parkinson's disease: A telerehabilitation application. Int J Lang Commun Disord 2010;45:630–644 [DOI] [PubMed] [Google Scholar]
- 89. Constantinescu GA, Theodoros DG, Russell TG, et al. . Home-based speech treatment for Parkinson's disease delivered remotely: A case report. J Telemed Telecare 2010;16:100–104 [DOI] [PubMed] [Google Scholar]
- 90. Howell S, Tripoliti E, Pring T. Delivering the Lee Silverman Voice Treatment (LSVT) by web camera: A feasibility study. Int J Lang Commun Disord 2009;44:287–300 [DOI] [PubMed] [Google Scholar]
- 91. Ellis T, Latham NK, DeAngelis TR, et al. . Feasibility of a virtual exercise coach to promote walking in community-dwelling persons with Parkinson disease. Am J Phys Med Rehabil 2013;92:472–481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Russell TG, Hoffmann TC, Nelson M, et al. . Internet-based physical assessment of people with Parkinson disease is accurate and reliable: A pilot study. J Rehabil Res Dev 2013;50:643–650 [DOI] [PubMed] [Google Scholar]
- 93. Runowicz CD, Leach CR, Henry NL, et al. . American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline. CA Cancer J Clin 2016;66:43–73 [DOI] [PubMed] [Google Scholar]
- 94. Hailey D, Roine R, Ohinmaa A, et al. . Evidence of benefit from telerehabilitation in routine care: A systematic review. J Telemed Telecare 2011;17:281–287 [DOI] [PubMed] [Google Scholar]
- 95. Galiano-Castillo N, Arroyo-Morales M, Lozano-Lozano M, et al. . Effect of an Internet-based telehealth system on functional capacity and cognition in breast cancer survivors: A secondary analysis of a randomized controlled trial. Support Care Cancer 2017;25:3551–3559 [DOI] [PubMed] [Google Scholar]
- 96. Galiano-Castillo N, Cantarero-Villanueva I, Fernández-Lao C, et al. . Telehealth system: A randomized controlled trial evaluating the impact of an internet-based exercise intervention on quality of life, pain, muscle strength, and fatigue in breast cancer survivors. Cancer 2016;122:3166–3174 [DOI] [PubMed] [Google Scholar]
- 97. Chen J, Jin W, Dong WS, et al. . Effects of home-based telesupervising rehabilitation on physical function for stroke survivors with hemiplegia: A randomized controlled trial. Am J Phys Med Rehabil 2017;96:152–160 [DOI] [PubMed] [Google Scholar]
- 98. Chumbler NR, Quigley P, Li X, et al. . Effects of telerehabilitation on physical function and disability for stroke patients: A randomized, controlled trial. Stroke 2012;43:2168–2174 [DOI] [PubMed] [Google Scholar]
- 99. Langan J, Delave K, Phillips L, et al. . Home-based telerehabilitation shows improved upper limb function in adults with chronic stroke: A pilot study. J Rehabil Med 2013;45:217–220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Goetz CG, Tilley BC, Shaftman SR, et al. . Movement Disorder Society-sponsored revision of the Unified Parkinson's Disease Rating Scale (MDS-UPDRS): Scale presentation and clinimetric testing results. Mov Disord 2008;23:2129–2170 [DOI] [PubMed] [Google Scholar]
- 101. Heldman DA, Urrea-Mendoza E, Lovera LC, et al. . App-based bradykinesia tasks for clinic and home assessment in Parkinson's disease: Reliability and responsiveness. J Parkinsons Dis 2017;7:741–747 [DOI] [PubMed] [Google Scholar]
- 102. Cancela J, Pastorino M, Arredondo MT, et al. . A telehealth system for Parkinson's disease remote monitoring. The PERFORM approach. Conf Proc IEEE Eng Med Biol Soc 2013;2013:7492–7495 [DOI] [PubMed] [Google Scholar]
- 103. Fisher JM, Hammerla NY, Ploetz T, et al. . Unsupervised home monitoring of Parkinson's disease motor symptoms using body-worn accelerometers. Parkinsonism Relat Disord 2016;33:44–50 [DOI] [PubMed] [Google Scholar]
- 104. Aminoff MJ. The future of the neurologic examination. JAMA Neurol 2017;74:1291–1292 [DOI] [PubMed] [Google Scholar]
- 105. Sokol LL, Shapiro D, Young MJ, et al. . The Parkinson Care Advocate: Integrating care delivery. Front Neurol 2017;8:364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. World Health Organization. Report on the second global survey on eHealth - Global Observatory for eHealth series. Online Referencing Volume 2, Available at www.who.int/goe/publications/ehealth_series_vol2/en/ (last accessed on April2, 2018)