Abstract
The common peroneal nerve is the most commonly injured nerve in the lower extremity. Peroneal nerve pathology results in loss of dorsiflexion at the tibiotalar joint, loss of eversion at the subtalar joint, and loss of extension of toes resulting in foot drop. The varied etiology of the problem is discussed. The various treatment modalities like conservative management, steroid therapy, nerve decompression, nerve repair, or reconstruction are described, but due to uncertain outcomes after primary nerve procedures, secondary procedures like tendon transfers often end up as definitive treatment. The rationale and technique of tibialis posterior transfer is discussed in detail.
Keywords: foot drop, tibialis posterior transfer, tendon transfer for foot drop
Common peroneal nerve is the most commonly injured nerve in the lower limb 1 and commonly manifests with foot drop. Peroneal nerve pathology results in loss of dorsiflexion at the tibiotalar joint, loss of ankle eversion at the subtalar joint, and loss of extension of toes which is much more complicated than what the term “foot drop” conveys.
During normal walking, heel strike and swing phase are two important phases. When the heel strikes the ground, the ankle is kept in either neutral position or in minimal extension. Then, during swing phase the toes must clear the ground, which requires active extension of the toes and the ankle to be held in neutral position. In patients with peroneal nerve palsy, these motors are absent and the patient slaps the foot on ground in heel strike and drags the toe along the ground in swing phase. To avoid this, the patient flexes the hip more than normal to lift the entire foot and toe off the ground as if he is walking up the stairs (high stepping gait). 2
The Anatomical Basis
The common peroneal nerve winds around the neck of the fibula and divides into superficial and deep branches ( Fig. 1 ). The superficial peroneal nerve supplies the peroneus longus and brevis muscles and continues as sensory branch. Hence, it is also called as the musculocutaneous nerve. The deep branch supplies the tibialis anterior, extensor digitorum, extensor hallucis, and peroneus tertius muscles. Consequently, in lesions of the common peroneal nerve there is also loss of eversion of foot. In long-standing cases, especially in leprosy, we can see callosity and ulceration developing on the lateral aspect of the foot as inversion is maintained by the tibialis posterior muscle. In partial lesions, the superficial branch is commonly spared and hence eversion of the foot is preserved. The decision to perform tendon transfer depends on whether only the anterior group is involved or if both the anterior and lateral groups are involved.
Fig. 1.
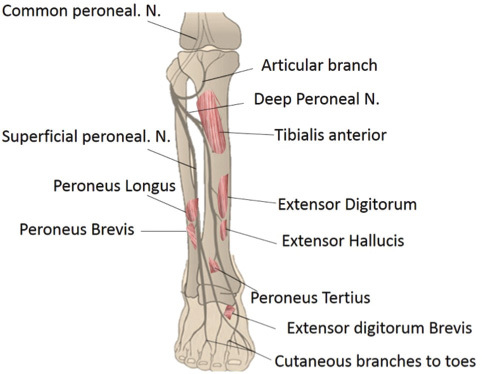
Common peroneal nerve course and muscles supplied.
Etiological Factors
Both neurological and muscular involvement can produce foot drop. Among the neurological factors, common peroneal nerve neuropathy (of idiopathic etiology), diabetic neuropathy, compression at the level of the neck of the fibula, lumbar disc prolapse, and nerve injury form the bulk of neurologic etiologies. In leprosy, the nerve gets compressed at the site where it winds around the fibular neck. At this place the nerve is also susceptible to injury as it lies comparatively superficially. Tumors of the nerve or fibula, cerebral palsy, poliomyelitis, multiple sclerosis, Charcot–Marie–Tooth disease, stroke, and spinal cord lesions are some of the other causes. Muscle injury, rupture of the tibialis anterior tendon, compartment syndrome, muscular dystrophy, and amyotrophic lateral sclerosis are some of the muscular causes. In a multi centric study done in Italy, the aetiology and predisposing factors of common peroneal nerve mono-neuropathy were studied. It was found that in 16% of patients, the cause of peroneal mono-neuropathy was idiopathic, 20.3% patients had developed neuropathy after surgery around the knee and trauma was the cause in 11.6% patients, surprisingly weight loss contributed to peroneal mono-neuropathy in 14.5% in their series. 3 In 1959 working in Polambakkam leprosy center in India, Hemerijckx 4 reported an incidence of 3 bilateral and 59 unilateral foot drop deformity in 2,337 leprosy patients with overall incidence of 2.5% in the 8 associated leprosy centers covered by the Belgian leprosy center in India.
Management
Conservative Management
Conservative management is indicated for patients with foot drop secondary to leprosy of less than 12 months’ duration because 50% of these patients recover spontaneously during the first 12 months. 5 Fritschi and Brand working in the Karigiri leprosy unit have recorded that they would wait for up to a year before considering surgery. 6 In idiopathic conditions too, waiting for a year after the onset is recommended.
All patients with foot drop of more than 12 months duration will ultimately require surgery to prevent contractures and foot ulceration. 7 The aim of conservative management is to prevent development of contractures and foot ulcers while the involved nerve is allowed to spontaneously recover. Conservative management involves placing the patient under a closely supervised program of physiotherapy and splinting. The foot is splinted in a foot and ankle orthosis to prevent stretching of the paralyzed anterior group of muscles and to prevent contracture of the tendo Achilles. 7 8 Role of steroids in patients with foot drop in leprosy is still controversial. A multicenter, randomized, double-blind, placebo-controlled trial conducted in Nepal and Bangladesh did not reveal any differences between the treatment and placebo groups; however, there was reduced deterioration of nerve function in the prednisolone group. 5 The efficacy of steroid therapy seems to depend upon the duration of nerve involvement and the degree of impairment. The earlier corticosteroids were given after the onset of nerve damage, it was likelier to prevent permanent nerve function impairment. 9 10 A Cochrane Review in 2016 stated that further randomized controlled trials (RCTs) are needed to establish optimal corticosteroid regimens and to examine the efficacy and safety of adjuvant or new therapies for treating nerve damage in leprosy. 11
Nerve Surgery
Primary nerve surgery for patients with foot drop includes neurolysis or decompression, primary repair, nerve grafting, or nerve transfer. Nerve decompression aims to relieve mechanical compression due to edema secondary to neuritis. Surgical decompression is indicated in leprosy patients with obvious evidence of nerve compression, nerve abscess, nerve pain, or nerve function impairment that is refractory to medical treatment. 7 12 13 Outcomes following nerve decompression are highly varied with good outcomes reported by Chaise and Roger. 14 However, Boucher et al in a moderate size RCT stated that combined treatment with steroids and decompression showed an improvement in sensory and motor deficits but statistically significant results were observed only in patients with incomplete paralysis and patients with neuritic pain alone. 15 In patients with peroneal nerve neuropathy due to other causes, neurolysis is indicated in patients with intact nerve action potentials. Kim et al reported good outcomes in 88% of such patients. 16 As per a Japanese study, early decompression is recommended in patients with foot drop caused by lumbar degenerative disease accompanied by severe motor disturbance, especially in older patients. 17 In patients with peroneal nerve compression secondary to nerve tumors especially schwannomas, excision of tumor while preserving nerve continuity is possible with intraoperative monitoring of nerve action potentials. Kim and Kline reported 80% of patients with nerve tumors had excision of nerve tumors with complete preservation of function. 16
Nerve repair or grafting is indicated in patients in whom nerve continuity is not preserved following tumor excision or when the nerve is transected. Primary nerve repair with epineural stitches under magnification is ideal but a nerve gap of more than 3 cm will require nerve grafting. Kim and Kline analyzing 318 patients with peroneal nerve pathology of varied etiology concluded that timely surgical exploration and nerve repair or grafting achieved good results; however, in their series the wait for spontaneous recovery in trauma was only 4 months which we feel is inadequate. 16 In their series, patients who had nerve grafts less than 6 cm had better outcomes when compared with patients with longer grafts.
Nerve transfers are indicated in patients with foot drop of less than 1 year duration. This involves transfer of functional fascicles of either the superficial peroneal nerve or of the tibial nerve to the deep peroneal nerve or motor branch of tibialis anterior muscle. Nath and colleagues reported success using this technique with 11 out of 14 patients recovering grade 3+ or more muscle power. 18 19
Secondary Procedures
When direct surgical repair is not possible and conservative management or nerve surgeries have failed, then secondary procedures are required. The primary aim of the surgery is restoring active dorsiflexion of the foot and correcting the inversion deformity when the peronei are also paralyzed along with the anterior group. This is achieved using tendon transfers, and when tendon transfer is not feasible or has failed, then bony procedures like triple arthrodesis with tenodesis or ankle arthrodesis may have to be considered to achieve a stable foot. Due to uncertain outcomes after primary nerve procedures, secondary procedures like tendon transfers often end up as the definitive treatment in these patients. 7
Tendon Transfer
Preoperative Assessment : Preoperative evaluation of the involved muscles and potential donor muscles play a major role in determining the choice of procedure. The muscles of the anterior and lateral compartment are evaluated in terms of muscle power. Tibialis anterior is tested by keeping the patient in sitting position and asking the patient to dorsiflex the ankle and invert the foot without extending the toes. The extensor hallucis longus (EHL) and extensor digitorum longus (EDL) are tested by asking the patient to extend the great toe and 2nd to 5th toes, respectively, at the metatarsophalangeal joint. 20 It is essential to assess the strength of the peroneal muscles before contemplating tendon transfer. The correct way of testing the peroneus longus and brevis is to make the patient sit, place the affected limb over the opposite knee with the hip internally rotated and knee flexed, and have the patient lift the foot (evert) ( Fig. 2 ). The patient will not be able to do so if the peronei are paralyzed. If this is the case, tibialis posterior is the ideal choice as motor for the transfer. Once tibialis posterior is chosen as the motor, preoperative training of tibialis posterior is to be started by making the patient sit, place the affected foot over the opposite knee with the hip externally rotated, knee flexed, and have the patient lift the foot (invert). This is continued for few weeks and strengthening of the tibialis is achieved by suspending a sand bag over the foot while performing the same maneuver.
Fig. 2.

Testing the peroneus longus and brevis.
Before proceeding with tendon transfer surgery, it must be ascertained that there is no contracture of tendo Achilles. If contracture is present, it needs to be stretched or released before the actual transfer is performed. Tendo Achilles release and tendon transfer can be performed in the same sitting. In leprosy, ulcers in foot are common and they must be healed before taking up for transfers.
Disorganization of the tarsal bones is often seen in patients with foot drop secondary to leprosy and in diabetes as involvement of the tibial nerve is also present in most of the patients leading to neuropathic bone disintegration. 7 Radiological imaging of the foot is required to determine whether there are any disorganization of the tarsal bones. Radiological evidence of disorganization is a relative contraindication for tendon transfer. When the disorganization is significant to the extent that the passive range of movement of the ankle is less than 10 degrees or with the presence of instability, it may be worthwhile to opt for bony procedures rather than tendon transfer. X-rays of the foot, with the foot in full forced varus and valgus will help determine whether the instability is principally in the subtalar or ankle joint. If the instability is in the ankle joint, or if the tibialis posterior muscle is not acting, then the patient will be required to undergo ankle arthrodesis or pantalar fusion. 7
We can analyze the tendon transfer procedures under various components, viz. choice of motor, the route it takes to reach its site of insert, and various insertions.
Motor
As discussed earlier when both the anterior and lateral groups of muscle are involved, the choice of motor is the tibialis posterior muscle. This not only removes the unopposed inversion force but also helps to restore dorsiflexion when it is inserted on to the dorsum of the foot. Tibialis posterior transfer for foot drop in leprosy is credited to Paul Brand who worked in CMC Vellore in the year 1955. 21 Other choices for motor are flexor digitorum longus (FDL) used along with the tibialis posterior to power the extensor digitorum and hallucis tendons as a double transfer. 22 Leclère et al reported anterior transposition of the lateral gastrocnemius muscle along with neurotization of the peroneal nerve. 23
In patients with isolated deep peroneal nerve involvement, where the peroneus longus and brevis are spared then it is better not to transfer the tibialis posterior. 24 Removal of the tibialis posterior will eliminate the balancing inversion force against the peroneal evertors of the foot which are not paralyzed. Rerouting the peroneus longus is a better procedure in such conditions.
Route
Since the peroneus longus lies adjacent to the anterior group of muscles separated only by a septum, it can be shifted anteriorly without difficulty from the lateral side. Tibialis posterior on the other hand lies posterior to the bones and interosseous membrane, and requires taking a different route to reach the anterior compartment.
The two commonly followed routes are the interosseous route and circumtibial route ( Fig. 3 ). As reported by Watkins et al, 25 Codivilla 26 and Putti 27 are considered the pioneers of the anterior transposition of the tibialis posterior tendon to the dorsum of the foot through the interosseous membrane. Gunn and Molesworth 28 reported 56 cases of drop foot (54 of them caused by leprosy) in which the tibialis posterior tendon was inserted into the tarsus after being brought forward through the interosseous membrane of the leg.
Fig. 3.
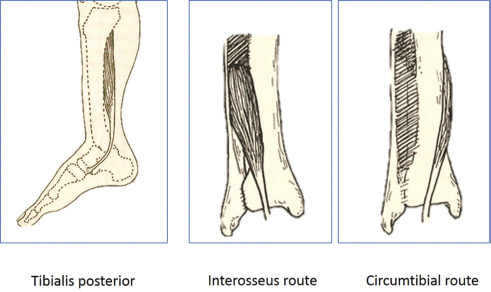
Tibialis posterior transfer—routes of tendon transfer (Courtesy: Srinivasan H. Atlas of corrective surgical procedures commonly used in leprosy).
In circumtibial route described by Ober, 29 the posterior tibial tendon is brought around the medial aspect of the tibia. The difference in functional outcome between the two routes is negligible with marginal increase in range of movement of ankle in the circumtibial route 30 but there is also a likelihood of more inversion deformity than in the interosseous route. 31
The Insert
Fixation of tendon can be done to bone, periosteum or tendons on the dorsum of foot.
Barr originally inserted the tendon to the intermediate or lateral cuneiform bone or base of the second or third metatarsal bone bringing the tendon through the interosseous route. 32 Modification of Barr's procedure, fixing the tendon to the cuboid bone, according to Salihagić et al produced much better result than the classic Barr's procedure. 33 Ober fixed the tendon to the base of the third metatarsal bringing it circumtibially. 29 Stable fixation to the bone requires pull-out wire sutures, staples, or bone anchor. Many of us feel that fixing the transferred tendon to the tendons on the dorsum of the foot is easy and the balancing of forces can be achieved to correct both inversion and plantar flexion deformity. Combining a bony anchorage with tendon suturing was suggested by Vigasio et al. 22 The tibialis anterior tendon was divided proximally and the distal tendon was rerouted tunneling through the cuneiform bones and sutured to the tibialis posterior tendon brought through the interosseous route, along with FDL tendon motorizing the EHL and EDL tendons. Classical Bridle insert 34 is to the tendons of the tibialis anterior and peroneus longus balancing the inversion and eversion of the foot. In 1966, Thangaraj reported over 50 operations in which the tibialis posterior tendon, brought anteriorly through the interosseous membrane, was inserted into the tendons of the EDL and EHL in the anterior compartment of the leg. 30 Srinivasan et al described his two-tail procedure of tibialis posterior transfer which is being followed by many treating leprosy patients worldwide. He inserts the split tibialis posterior tendon brought circumtibially and sutures one slip to the EHL and the other to the EDL and peroneus tertius tendons. 35 In his series of 39 cases, 34 cases had 90 degrees or more of dorsiflexion. Out of these 34 patients, 30 had range of movement of more than 15 degrees. 35 We prefer to include the tibialis anterior along with the EHL in one slip and the other to the EDL. Insertion into the EHL, EDL, and peroneus tertius balances the foot well and produces good range of movement.
Procedure
Tibialis Posterior Transfer
The two-tail tibialis posterior procedure is given below. 36
Either general anesthesia or spinal/epidural anesthesia is given. A pneumatic tourniquet is applied. The tendon of the tibialis posterior at its insertion is identified through an oblique incision made over the tuberosity of the navicular bone along one of the creases ( Figs. 4 5 6 ). A suture is applied to the tendon close to its insertion and left long. This suture steadies the tendon and helps to retrieve it back if it gets stuck while delivering it into the leg. The tendon is then detached from its insertion and its synovial attachments are divided. Sometimes if the end looks bulbus it must be trimmed ( Fig. 7 ). A 5-cm curvilinear incision is made in the lower part of the leg close to the medial border of the tibia, about 10 cm above the medial malleolus. The tendon of the tibialis posterior is identified and pulled out ( Fig. 8 ). The lowest muscle fibers inserting into the tibialis posterior tendon may have to be shaved off from the tendon if it comes in the way of smooth gliding. The tendon is split into two tails up to where it will cross the tibia proximally ( Fig. 9 ). By keeping the split tendon over the skin circumtibially, we can assess where exactly the tendons will reach ultimately when tunneled. At this place, two transverse incisions are made on the dorsum of the foot, one over the EHL tendon and the other over the tendons of the EDL ( Figs. 10 11 ). Through these incisions, the tendons of the EHL and the EDL and peroneus tertius are identified and isolated. A tendon tunneler is passed from each of these wounds in the dorsum of the foot to the wound in the leg making two separate tunnels for each slip. The tunnels are made subcutaneously ( Fig. 12 ). The motor slips are pulled through. The recipient tendon of the EHL is lifted with a hook and pulled proximally to keep it taut. A slit is made in it and the slip of the tibialis posterior tendon is passed through it. Another slit is made distally in another plane and again it is passed through it ( Figs. 13 14 15 ). The tendon is fixed with three or four 2/0 nonabsorbable suture material. The next slip is passed similarly through the EDL and peroneus tertius keeping the tension to balance the foot in neutral position without inversion or eversion. During this stage, the knee is held in flexion of approximately 30 degrees and the ankle in dorsiflexion beyond 90 degrees to the maximum possible extent ( Fig. 16 ). We can use a tension adjustment splint as shown or held in place by placing towels as shown ( Fig. 17 ). The motor tendons are kept in moderate tension. The final position is as shown in Fig. 18 .
Fig. 4.
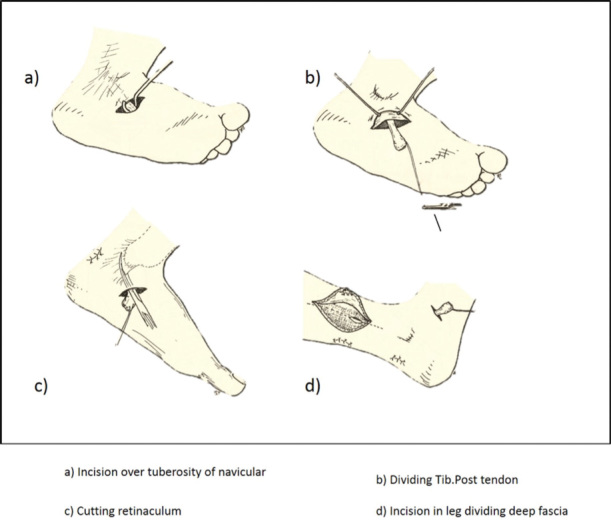
Tibialis posterior transfer: exposure and division of the tibialis posterior in the foot (Courtesy: Srinivasan H. Atlas of corrective surgical procedures commonly used in leprosy).
Fig. 5.

Incision over the tuberosity of navicular to expose the tibialis posterior tendon insertion.
Fig. 6.

Identification and isolating the tibialis posterior tendon.
Fig. 7.

Division of the tibialis posterior tendon and synovium (note the bulbous distal end of the tendon).
Fig. 8.

Retrieval of the tibialis posterior tendon into the leg wound.
Fig. 9.
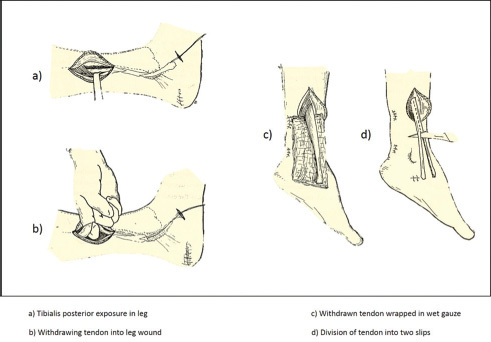
Tibialis posterior transfer—exposure in leg, retrieval of the tendon, and division into two slips (Courtesy: Srinivasan H. Atlas of corrective surgical procedures commonly used in leprosy).
Fig. 10.
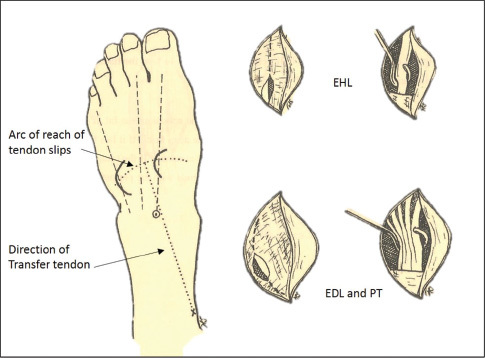
Tibialis posterior transfer—incision in foot and exposure of the recipient tendons (Courtesy: Srinivasan H. Atlas of corrective surgical procedures commonly used in leprosy).
Fig. 11.

Division of the tibialis posterior tendon into two slips, which is placed over the lower 3rd of the leg to assess their reach. It is also used to determine the orientation of the subcutaneous tunnels.
Fig. 12.
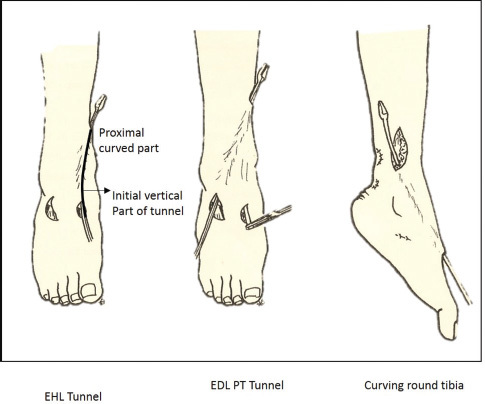
Tibialis posterior transfer—tunneling of tendon slips (Courtesy: Srinivasan H. Atlas of corrective surgical procedures commonly used in leprosy).
Fig. 13.
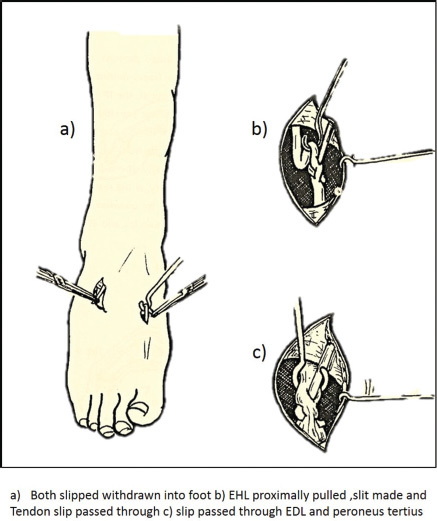
Tibialis posterior transfer—suturing of slips (Courtesy: Srinivasan H. Atlas of corrective surgical procedures commonly used in leprosy).
Fig. 14.

Passing and suturing of the slip of the tibialis posterior tendon through slits made in the extensor hallucis longus tendon.
Fig. 15.

Passing and suturing of the slip of the tibialis posterior tendon through slits made in the extensor digitorum longus tendon and peroneus tertius tendons.
Fig. 16.

The position to be maintained during tenorrhaphy, knee in flexion and the ankle in maximum dorsiflexion (beyond 90 degrees).
Fig. 17.
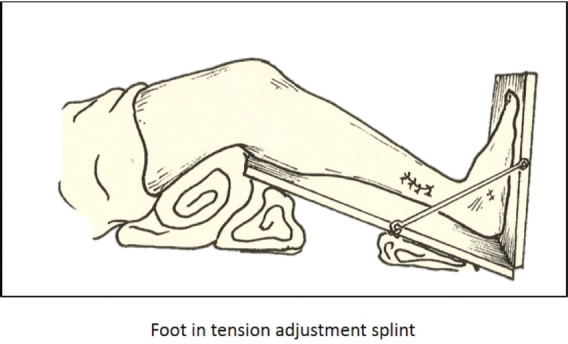
Tibialis posterior transfer—tension adjustment splint (Courtesy: Srinivasan H. Atlas of corrective surgical procedures commonly used in leprosy).
Fig. 18.

The final resting tension after completion of the transfer.
Peroneus Longus Transfer
An oblique incision is made over the lateral aspect of the foot from base of the fifth metatarsal to approximately 1 cm below the lateral malleolus to expose the insertion of the peroneus longus and brevis. Srinivasan divides the brevis tendon distally and longus more distally and sutures the proximal brevis tendon to the distal longus tendon making the brevis act as a longus. Many do not use this step. The longus which is divided distally is delivered in the leg through a 5-cm-long incision made anterolaterally approximately 5 cm above the lateral malleolus. The tendon is then split as in tibialis posterior transfer. Like the tibialis posterior procedure, tunnels are made and suturing done as before. The only difference being the tendon slips reach the foot from the lateral side instead of the medial side in the tibialis posterior transfer.
Postoperative Period
A below-knee plaster is applied. The plaster is bi-valved after 3 weeks. Physiotherapy is started with reeducation as discussed earlier. Initially after 3 weeks, training is done to contract the tibialis muscle. After 4 week, the patient is made to stand with support. Between periods of exercise, the leg and foot are kept in the plaster slab. After 6 weeks, the patient is allowed to walk between parallel bars with minimal weight bearing. From 8 weeks onwards, full weight bearing is allowed.
Complications
The reported complications following tendon transfers of the foot and ankle include persistent deformity, pain and rigidity, wound infections and abscesses, tarsal tunnel syndrome, sural nerve injuries, and other causes of paresthesias, and neuropathic pain. 37 Postoperative surgical site infections are rare. Adhesions giving rise to reduced range of movements are noticed especially in interosseous route transfers which can be avoided if the window in the interosseous membrane is large enough. Insufficient tension gives rise to reduced dorsiflexion or persistent equinus deformity. In circumtibial transfers excessive inversion may be noticed. This can be avoided by tunneling first vertically from the EHL site proximally and then curving it around the tibia facilitating vertical pull. Interosseous route transfers do not produce this. Similarly, eversion can occur if excess tension is given while the EDL slip is tightened more. Rarely in leprosy the tibialis posterior may become paralyzed later and may not work. Dehiscence is rare.
Arthrodesis
As discussed earlier, if there is disorganization of the tarsal bones and in cases where the tibialis posterior is also involved, it may be worthwhile arthrodesing the ankle and subtalar joints.
In conclusion, when there is no recovery after primary procedures for foot drop, in leprosy and other causes of peroneal neuropathy, dynamic transfers yield very good results. There is not much difference between circumtibial and interosseous routes. Tendon fixations are much easier to perform than bony fixation and can give excellent results. In our experience, two-tail tibialis posterior procedure gives good results.
Footnotes
Conflict of Interest None
References
- 1.Huckhagel T, Nüchtern J, Regelsberger J, Gelderblom M, Lefering R. TraumaRegister DGU®. Nerve trauma of the lower extremity: evaluation of 60,422 leg injured patients from the TraumaRegister DGU® between 2002 and 2015. Scand J Trauma Resusc Emerg Med. 2018;26(01):40. doi: 10.1186/s13049-018-0502-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wiszomirska I, Błażkiewicz M, Kaczmarczyk K, Brzuszkiewicz-Kuźmicka G, Wit A. Effect of drop foot on spatiotemporal, kinematic, and kinetic parameters during gait. Appl Bionics Biomech. 2017;2017:3.595461E6. doi: 10.1155/2017/3595461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aprile I, Caliandro P, La Torre G. Multicenter study of peroneal mononeuropathy: clinical, neurophysiologic, and quality of life assessment. J Peripher Nerv Syst. 2005;10(03):259–268. doi: 10.1111/j.1085-9489.2005.10304.x. [DOI] [PubMed] [Google Scholar]
- 4.Hemerijckx F. Polambakkam, India: privately printed; 1959. Report of the Activities of the Leprosy Control Campaign (1955–58) of the Belgian Leprosy Centre, Polambakkam. [Google Scholar]
- 5.Richardus J H, Withington S G, Anderson A M. Treatment with corticosteroids of long-standing nerve function impairment in leprosy: a randomized controlled trial (TRIPOD 3) Lepr Rev. 2003;74(04):311–318. [PubMed] [Google Scholar]
- 6.Fritschi E P, Brand P W. The place of reconstructive surgery in the prevention of foot ulceration in leprosy. Int J Lepr. 1957;25(01):1–8. [PubMed] [Google Scholar]
- 7.Richard B. Kathmandu, Nepal: Ekta Books; 2004. Surgical management of neuritis. [Google Scholar]
- 8.Andersen J G. Foot drop in leprosy and its surgical correction. Acta Orthop Scand. 1963;33(01)(04):151–171. [Google Scholar]
- 9.Becx-Bleumink M, Berhe D, Mannetje W. The management of nerve damage in the leprosy control services. Lepr Rev. 1990;61(01):1–11. doi: 10.5935/0305-7518.19900001. [DOI] [PubMed] [Google Scholar]
- 10.Naafs B.Bangkok Workshop on Leprosy Research. Treatment of reactions and nerve damage Int J Lepr Other Mycobact Dis 19966404SupplS21–S28. [PubMed] [Google Scholar]
- 11.Van Veen N H, Schreuders T A, Theuvenet W J, Agrawal A, Richardus J H. Decompressive surgery for treating nerve damage in leprosy. Cochrane Database Syst Rev. 2012;12(12):CD006983. doi: 10.1002/14651858.CD006983.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malaviya G N. Shall we continue with nerve trunk decompression in leprosy? Indian J Lepr. 2004;76(04):331–342. [PubMed] [Google Scholar]
- 13.Palande D D. Preventive nerve surgery in leprosy. Lepr India. 1980;52(02):276–298. [PubMed] [Google Scholar]
- 14.Chaise F, Roger B. Neurolysis of the common peroneal nerve in leprosy. A report on 22 patients. J Bone Joint Surg Br. 1985;67(03):426–429. doi: 10.1302/0301-620X.67B3.3997954. [DOI] [PubMed] [Google Scholar]
- 15.Boucher P, Millan J, Parent M, Moulia-Pela J P. Randomized controlled trial of medical and medico-surgical treatment of Hansen's neuritis [in French] Acta Leprol. 1999;11(04):171–177. [PubMed] [Google Scholar]
- 16.Kim D H, Kline D G.Management and results of peroneal nerve lesions Neurosurgery 19963902312–319.discussion 319–320 [DOI] [PubMed] [Google Scholar]
- 17.Matsui H, Kanamori M, Kawaguchi Y, Kitagawa H, Nakamura H, Tsuji H. Clinical and electrophysiologic characteristics of compressed lumbar nerve roots. Spine. 1997;22(18):2100–2105. doi: 10.1097/00007632-199709150-00007. [DOI] [PubMed] [Google Scholar]
- 18.Nath R K, Lyons A B, Paizi M. Successful management of foot drop by nerve transfers to the deep peroneal nerve. J Reconstr Microsurg. 2008;24(06):419–427. doi: 10.1055/s-0028-1082894. [DOI] [PubMed] [Google Scholar]
- 19.Nath R K, Somasundaram C. Gait improvements after peroneal or tibial nerve transfer in patients with foot drop: a retrospective study. Eplasty. 2017;17:e31. [PMC free article] [PubMed] [Google Scholar]
- 20.Kendall F P, McCreary E K, Provance P G, Rodgers M M, Romani W A. 5th ed. Baltimore: Williams & Wilkins; 2005. Muscles, Testing and Function with Posture and Pain; pp. 408–411. [Google Scholar]
- 21.Brand P W. The value of surgical and physiotherapeutic measures in leprosy. Lepr India. 1955;27:131. [Google Scholar]
- 22.Vigasio A, Marcoccio I, Patelli A, Mattiuzzo V, Prestini G. New tendon transfer for correction of drop-foot in common peroneal nerve palsy. Clin Orthop Relat Res. 2008;466(06):1454–1466. doi: 10.1007/s11999-008-0249-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leclère F M, Badur N, Mathys L, Vögelin E. Neurotized lateral gastrocnemius muscle transfer for persistent traumatic peroneal nerve palsy: surgical technique [in French] Neurochirurgie. 2015;614:292–297. doi: 10.1016/j.neuchi.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 24.Fritschi E P. Bristol: Wright; 1971. Reconstructive Surgery in Leprosy. [Google Scholar]
- 25.Watkins M B, Jones J B, Ryder C T, Jr, Brown T H., Jr Transplantation of the posterior tibial tendon. J Bone Joint Surg Am. 1954;36-A(06):1181–1189. [PubMed] [Google Scholar]
- 26.Codivilla A. On tendon transplants in orthopedic practice [in Italian] Arch Ortop. 1899;16:225–250. [Google Scholar]
- 27.Mayer L. The physiological method of tendon transplantation in the treatment of paralytic drop-foot. J Bone Joint Surg Am. 1937;19(02):389–394. [Google Scholar]
- 28.Gunn D R, Molesworth B D. The use of tibialis posterior as a dorsiflexor. J Bone Joint Surg Br. 1957;39-B(04):674–678. doi: 10.1302/0301-620X.39B4.674. [DOI] [PubMed] [Google Scholar]
- 29.Ober F R. Tendon transplantation in the lower extremity. N Engl J Med. 1933;209:52–59. [Google Scholar]
- 30.Thangaraj R H. Reconstructive surgery in the treatment and prevention of ulcers of the foot. Lepr Rev. 1966;37(01):35–37. doi: 10.5935/0305-7518.19660007. [DOI] [PubMed] [Google Scholar]
- 31.Soares D. Tibialis posterior transfer for the correction of foot drop in leprosy. Long-term outcome. J Bone Joint Surg Br. 1996;78(01):61–62. [PubMed] [Google Scholar]
- 32.Crenshaw A H. 7th ed. St. Louis: The C.V. Mosby Company; 1987. Campbell's Operative Orthopedics. [Google Scholar]
- 33.Salihagić S, Hadziahmetović Z, Fazlić A. Classic and modified Barr's technique of anterior transfer of the tibialis posterior tendon in irreparable peroneal palsies. Bosn J Basic Med Sci. 2008;8(02):156–159. doi: 10.17305/bjbms.2008.2973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Johnson J E, Paxton E S, Lippe J. Outcomes of the Bridle procedure for the treatment of foot drop. Foot Ankle Int. 2015;36(11):1287–1296. doi: 10.1177/1071100715593146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Srinivasan H, Mukherjee S M, Subramaniam R A. Two-tailed transfer of tibialis posterior for correction of drop-foot in leprosy. J Bone Joint Surg Br. 1968;50(03):623–628. [PubMed] [Google Scholar]
- 36.Srinivasan H. Chennai, India: Published by author, Janatha Printing and Publishing Co. Pvt Ltd; 2004. Atlas of Corrective Surgical Procedures Commonly Used in Leprosy; pp. 150–169. [Google Scholar]
- 37.Clanton T O, Betech A A, Bott A M. Complications after tendon transfers in the foot and ankle using bioabsorbable screws. Foot Ankle Int. 2013;34(04):486–490. doi: 10.1177/1071100713477625. [DOI] [PubMed] [Google Scholar]


