Abstract
The term “physician engagement” is used quite frequently, yet it remains poorly defined and measured. The aim of this study is to clarify the term “physician engagement.” This study used an eight step-method for conducting concept analyses created by Walker and Avant. MEDLINE, EMBASE, and the Cochrane Central Register of Controlled Trials were searched on February 14, 2019. No limitations were put on the searches with regard to year or language. Results identify that the term “physician engagement” is regular participation of physicians in (1) deciding how their work is done, (2) making suggestions for improvement, (3) goal setting, (4) planning, and (5) monitoring of their performance in activities targeted at the micro (patient), meso (organization), and/or macro (health system) levels. The antecedents of “physician engagement” include accountability, communication, incentives, interpersonal relations, and opportunity. The results include improved outcomes such as data quality, efficiency, innovation, job satisfaction, patient satisfaction, and performance. Defining physician engagement enables physicians and health care administrators to better appreciate and more accurately measure engagement and understand how to better engage physicians.
Keywords: physician, medical, engagement, concept analysis
Introduction
Physician engagement is often identified as being crucial to high-performing health care organizations1,2 with improved patient care outcomes and cost reduction.1,3,4 However, due to the wide use of the term, it remains a quite nebulous concept5,6 resulting in little consensus on appropriate measurement and minimal empirical evidence demonstrating the association between the engagement of physicians and improved outcomes. Although far less prominent in the literature are the terms “medical engagement” and “doctor engagement,” with the latter most prominent in Europe. Regardless, all terms refer to physicians/medical doctors.
Traditionally, physicians worked independently and were not considered hospital employees, with a focus on patient care and clinical decision-making.7 Physicians have long emphasized their critical role as patient advocates and held themselves accountable for effective care. To be effective patient advocates, doctors believed that it was important for them to have clinical self-government to determine the best care required, while the focus of health care executives and administrators was financial management.7
More recent demands on health service organizations to reform and improve their performance around patient experiences and cost-of-care reductions have led to a recognition that physicians can contribute in an important way in addressing these demands.8
It is essential to align physicians with organizational and system aims and activities, engaging physicians in both setting the course for system change and ensuring optimal execution of the desired system changes. (p. 2)8
New expectations have physicians taking on additional roles and activities perceived as “organizational imperatives” rather than “direct patient care”, creating a strong dichotomy between hospital leadership and frontline physicians, or an “us versus them” environment.8
Thus, abundant of time and resources are spent discussing and trying to “engage” physicians.5 Non engagement of clinicians has been a long-standing, international, and complex problem.9 A literature review on health care professional views on engagement in quality improvement identified that health care professionals are reluctant to engage, mainly because they perceive that initiatives will be ineffective, will be a waste of scarce personal and organizational resources, and are concerned about harmful effects that may result from quality initiatives.9
Although some scholars in the field may have a clear understanding of the term “physician engagement,” it has become evident from discussions with Canadian health care administrators and physician leaders and review of the literature, this concept is still poorly understood and measured. This conceptual “fuzziness” likely contributes to the lack of evidence in this area, making comparisons across settings challenging. Previous work in this area examining the evidence on physician engagement suggests that most of the articles published on this topic are non evidence-based and considered opinion pieces.10
Methods
Walker and Avant’s (2011) eight step-method for conducting concept analyses see Table 1, is used to examine the term “physician engagement.” This method is used quite often in health care when little is known about a topic11–13 and to help clarify ambiguous concepts,14 thus enabling researchers to conduct more thorough systematic and meta-analyses. Concept analyses help to explain the meaning of the concepts in current use in order to further develop the concept.15 Conceptual analyses use literature reviews as instruments, whereas literature reviews can simply be used as a review.15
Table 1.
Walker and Avant’s steps for conducting a concept analysis
| Steps | Description |
|---|---|
| 1 | Select a concept |
| 2 | Determine purpose of analysis |
| 3 | Identify all uses of the concept |
| 4 | Determine defining attributes |
| 5 | Construct a model case |
| 6 | Construct a borderline and contrary case |
| 7 | Identify antecedents and consequences |
| 8 | Define empirical referents |
Step 1: selecting a concept
A concept is an abstract idea that denotes elements of human phenomena.16 This study selected “physician engagement” as a concept. Despite the fact that physician engagement is beneficial to organizations, there appears to be widespread and ambiguous use of the term.6 The lack of conceptual clarity around the term “physician engagement” makes it challenging to measure and improve. This lack of conceptual and definitional clarity impedes progress in enhancing physician involvement in shared decision-making; commitment to the achievement of strategic goals; quality improvement initiatives; implementation of change programs; use of resources; and the development and utilization of evidence-based guidelines.5
Step 2: determining the purpose of analysis
This analysis seeks to explore how the term “physician engagement” is used in the literature, and theoretically define its components. It will help extricate the defining attributes and improve modeling of the concept while developing a “physician engagement” construct. This will hopefully help to clarify a universal construct such that the same understanding is given to the concept and develop an operational definition.14
Step 3: identifying uses of the concept
Data sources and search
EMBASE, the Cochrane Central Register of Controlled Trials, and, MEDLINE were searched on February 14, 2019. The search terms used were “physician engagement,” “medical engagement,” and “doctor engagement.” No limitations were put on the searches with regard to year or language. Targeted searches were also conducted to identify relevant articles (eg, after identifying an author doing extensive work in this area). Dictionaries and thesauri were also searched in addition to grey literature. Websites reviewed included Agency for Healthcare Research and Quality, the National Institutes of Health, the Canadian Medical Association, Institute for Healthcare Improvement National Institutes of Health, the Canadian Medical Association, and GreyNet International.
Data items and abstraction process
An Excel form was created containing all author names and article titles. The PI (TP) selected the first 20 cases identified in the Excel form. Two reviewers of the research team (LP and LN) independently performed a practice test on the 20 selected articles. Reviewers screened for the terms “physician engagement,” “medical engagement,” and/or “doctor engagement.” The same reviewers independently extracted the following data: definitions, instruments, how the term was being used. Discrepancies were discussed, and a resolution agreed upon. Differences were resolved by discussion. Data were entered in an Excel form. Data were reviewed to ensure there were no discrepancies. The remaining full-text articles (n=155) were screened independently by the two reviewers. Four members of the team reviewed the final data for all 175 articles and agreed upon themes.
Part of the data abstraction involved identifying whether any study authors offered a clear definition of the term “engagement.” Narrative synthesis was completed.17 A table was first created in excel. Data were extracted on definitions provided, context, antecedents and outcomes of engagement, and, finally, instruments identified for measuring engagement. The table was then examined to identify themes or groupings. Finally, concepts were mapped to identify patterns. Since this is neither a meta-analysis nor systematic review, study quality is not evaluated.18
Results
Study selection process
There were 439 records identified in total. After removing duplicates and articles unrelated to engagement, there were 175 articles remaining for analysis.
Defining engagement
The term “engagement” is defined by Merriam-Webster Collegiate Dictionary as follows:
(i) an arrangement to meet or be present at a specified time and place, or a job or period of employment especially as a performer; (ii) something that engages; (iii) the act of engaging (the state of being engaged), or emotional involvement or commitment, or betrothal (formal engagement to be married); (iv) the state of being in gear; and (v) a hostile encounter between military forces.19
In the political context, engagement describes a process of trying to influence others to a certain view.20 Skillman et al (2017) define engagement as active support for a project.21
Given that “physician engagement” is a psychological concept, one might expect that work to date has drawn on the rich research history of the related concept of “work engagement” developed in the organizational behavior and work psychology literature.6 This, however, is not the case. “Work engagement” is a positive, fulfilling work-related state of mind, encompassing vigor, dedication, and absorption. Individuals engaged in their work demonstrate high energy levels, perseverance, pride, enthusiasm, and full engrossment in their work.22
The term “physician engagement” is often not defined at all. Instead, it is used commonly as an action verb, to participate in an activity.20 McLeod and Clarke, acknowledging a universal definition does not exist, propose that engagement is measurable; however, they recognize that the lack of a consensus on a single tool accounts for some of the variability in the concept.23 Of the 175, only 18 articles provided definitions of “engagement.”1,2,5,6,10,20,21,24–34 There does not appear to be a single, widely accepted definition, see Table 2.
Table 2.
Examples of varying definitions of physician engagement
| Description | Reference |
|---|---|
| Appropriate and effective use of hospital services | 5 |
| Active support for a project | 21 |
| The association and partnership physicians feel toward a health care organization | 10 |
| Doctors displaying active interest or a positive role of involvement within the program | 32 |
| The extent to which the physician actively participates in and facilitates the work of the team | 121 |
| Degree to which an employee is satisfied in their work, motivated to perform well, able to suggest and implement ideas for improvement, and their willingness to act as an advocate for their organization by recommending it as a place to work | 24 |
| Physicians who reflect on the importance of reducing health disparities in their practices and have developed specific strategies to achieve this | 26 |
| Doctors act within their normal roles to maintain and enhance the performance of the organization which itself recognizes this commitment in supporting and encouraging high-quality care | 29 |
| The experience physicians have as being actively interested in the quality of their workplace, and motivation to take an active leadership role in helping to improve that workplace | 56 |
| Elements of engagement include alignment, action and accountability | 82 |
| An energetic state of involvement with activities that are personally fulfilling and enhance one’s sense of professional efficacy | 154 |
| It is more than just an intellectual property, but is about establishing relationships that nurture a sense of meaning and purpose | 155 |
| Two-way involvement at a level which influences decision making - involvement at the beginning and as an integral part of the decision-making process, rather than as an add-on or afterthought once the decisions are in place | 59 |
The term “physician engagement“ is most commonly used in North America. In Europe, however, the term “medical engagement” appears to be more predominant. Spurgeon et al (2011) define “medical engagement” as the positive and active contribution of physicians for sustaining and improving their organization’s performance.20 Spurgeon describes engagement as a commitment to high-quality care. This proposition by Spurgeon that there is a commitment to high-quality care supports work by Perreira, Berta, Ginsburg, Barnsley, and Herbert that commitment is targeted and can extend beyond simply commitment to the organization itself.35 For example, one may not be committed to their organization; however, they may be committed to their patients, their co workers or even their supervisor.
The concept of medical engagement is complex.32 Spurgeon describes engagement as intra individual, a commitment level, or motivational state that can be applied to a diverse group of activities or contexts.34 Spurgeon describes engagement as intra individual, a commitment level, or motivational state that can be applied to a diverse group of activities or contexts.34 Spurgeon states that medical engagement is closely associated to unidirectional concepts such as work engagement, burnout, and job satisfaction.36 Spurgeon suggests that medical engagement is more about reciprocity and how physicians respond to actions by the organization.36
A quick review of Table 2 will show that many of the definitions used to describe engagement use these pre existing, well-established constructs (see Table 3). From a research perspective, for accurate measurement, it is critical to clearly distinguish between constructs that have been proven to be distinct, well-validated, reliable instruments such as satisfaction, organizational support, empowerment, work engagement, perceptions of performance, and organizational citizenship behaviors (see Table 3). The relationships amongst these constructs have been shown in health care to be far more complex than unidirectional.35,37–39
Table 3.
Examples of pre existing well-established constructs
| Construct | Definition |
|---|---|
| Perceived organizational support | The degree to which an organization values employee contributions and cares about their well-being156 |
| Organizational commitment | The positive affect and affiliation that workers develop for their organizations157 |
| Job satisfaction | A worker’s positive feelings toward their job158 |
| Work engagement | Positive, fulfilling work-related state of mind that is characterized by vigor, dedication, and absorption22 |
| Psychological empowerment | Feeling capable of shaping one’s work context and work role; comprised of meaning associated with work tasks, feelings of competence and belief in one’s abilities to perform work activities, self-determination concerning control and choice over work behaviors, and observable positive impacts of one’s work behaviors159 |
| Individual work performance | Individual work performance includes effectiveness and productivity160 |
| Organizational citizenship behaviors | Extra-role behaviors that can be directed toward individuals or the organization; can include organizational praise, helping colleagues, or making suggestions to improve performance that may disrupt social relationships by challenging the status quo161 |
Step 4: determining the defining attributes of “physician engagement”
Characteristics often associated with a concept are referred to as defining attributes present in both theoretical and operational definitions. Based on the data abstracted in this review, the main defining attribute of physician engagement appears to be physician “involvement” in an activity. A few examples include the use of a physician portal/online platform,40 time spent looking at technology rather than the patient,41 reflecting on actions,42 learning activities,43,44 or communicating with patients and other providers.45
However, involvement is more than simply partaking in an activity (ie, showing up for an activity or performing a task), but rather being “involved” which is defined as “regular participation of employees in (1) deciding how their work is done, (2) making suggestions for improvement, (3) goal setting, (4) planning, and (5) monitoring of their performance.”46 The underlying assumption is that those who are involved in the process best understand it and are inspired to make improvements.46
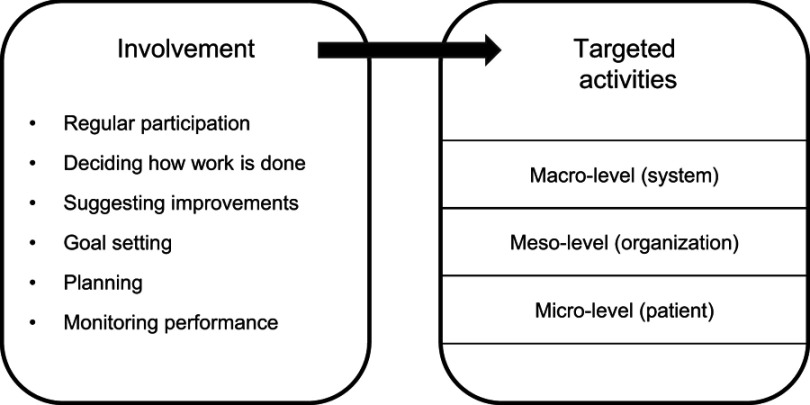
Furthermore, the literature suggests that involvement in activities appears to be targeted at one of the three levels: micro (patient), meso (organization), and/or macro (health system). See Figure 1. This distinction can help determine the most effective motivators to improve desired outcomes at each level.
Figure 1.
Attributes of physician engagement.
Micro (physician–patient) level
Physician engagement at the micro level refers to involvement in activities at the individual, physician–patient level, initiatives that impact day-to-day, direct patient care. This involves work with the patient as well as with other allied health care professionals. Examples include direct patient care and patient safety,3,47–49 huddles,50 interprofessional collaboration,51 and teamwork.3,48 This can also involve communication and interaction with patients and families52–54 as well as involvement of patients and families in decision-making.55
Meso (organization) level
Physician engagement at the meso level refers to involvement in activities at an organizational level, activities that impact organizational processes. Examples include active interest and involvement of physicians in enhancing, sustaining, supporting, and encouraging high-quality care and organizational performance,10,20 taking on active leadership roles, helping to improve the workplace10,56 involvement in strategic planning,57 participation in decision-making,10,58,59 and involvement in resource allocation and controlling costs.60,61
Macro (systemic) level
Physician engagement at the macro level refers to involvement in activities at the health system level, activities that extend beyond a single organization. Examples include improved population health and lower costs62 and health system efficiency as a whole,62–65 acting as a facilitator of system transformation58 and health advocacy66,67 such as woman’s health system change,68 their role in community issues such as gun violence prevention,69 and decision-making on tobacco treatments whether for tobacco70 or prostate cancer screening.71
Steps 5 and 6: what “physician engagement” is and what it is not
The following two sections, steps 5 and 6, help to further illustrate what physician engagement is, and what it is not.
Step 5: constructing a model case
A model case is described to help illustrate all the defining attributes of a concept.
Model case
Physician engagement, as discussed in the literature, is really about involvement in activities targeted at one of the three levels: micro (patient), meso (organization), and/or macro (health system). Let us use a commonly described example, physician engagement in leadership at the organizational (meso) level. An engaged physician would be one that regularly participates in leadership activities and attends leadership meetings as well as (1) decides by what means work is completed, (2) suggests improvements, (3) assisting is setting goals, (4) planning, and (5) performance monitoring.46
Step 6: constructing borderline and contrary cases
Borderline cases contain most, but not all of the defining attributes of a concept, whereas, contrary cases have none of the defining attributes of a concept.14 In this section, it is important to understand what “physician engagement” is not. The concepts identified in Table 3 have been used interchangeably to define “physician engagement.” However, these constructs have been established to be distinct, well-defined, validated, reliable concepts. As such, it is important to clearly articulate the desired measure. For example, if interested in a physician’s positive psychological state characterized by their dedication, how absorbed they are in their work, and how excited they are to come to work, then one should measure “work engagement.” The same should be done for other concepts such as psychological empowerment, job satisfaction, organizational support, and commitment.
Step 7: identifying antecedents and consequences
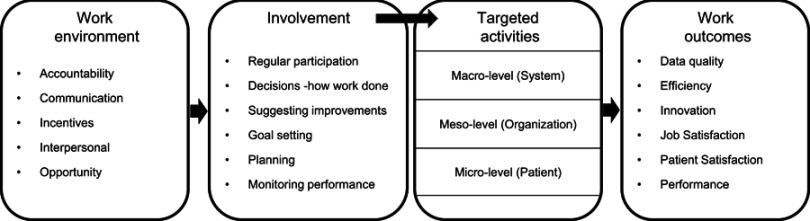
“Work psychology” involves the study of human behaviors in the workplace.72 The theoretical foundation for work in this is the Theory of Reasoned Action (TRA).73 TRA suggests that work outcomes are directly related to behavioral intentions, which are preceded by work attitudes, which in turn are impacted by one’s observations of their work environment74 and interactions with leadership and coworkers.72 A simplified version of this is presented in Figure 2. Thus, “antecedents” would be characteristics in the work environment that impact physician engagement, which in turn impacts work outcomes, in other words, the consequences of physician engagement.
Figure 2.
Relationships between work environment, behaviors, and outcomes.
Antecedents
The major overarching antecedent of physician engagement appears to be organizational culture. Organizational culture is defined as follows:
the values and behaviours that contribute the unique social and psychological environment of an organization. This includes an organization’s expectations, experiences, philosophy, and values that hold it together. It is based on shared attitudes, beliefs, customs, written and unwritten rules that have been developed over time. It is shown in
The way the organization conducts its business, treats its employee, customers, and the wider community
The extent to which freedom is allowed in decision making, developing new ideas, and personal expression,
How power and information flow through its hierarchy, and
How committed employees are toward collective objectives.75
From a leadership perspective, it is important to understand physician culture,76 workforce diversity, and cultural challenges,77 norms,78 and values.25 The four key cultural attributes that act as antecedents to physician engagement are accountability, communication, incentives, opportunity, and interpersonal skills.
Accountability
Accountability has appeared repeatedly in the literature as an antecedent of physician engagement.5,71,79–83 Examples include responsibility for clinical and health outcomes,62 patient outcomes, service utilization and system performance,64 quality, cost and care,60 clinical improvement projects,84 and government and institutional policies to involve doctors in clinical leadership roles.30
Communication
Communication is another antecedent that has appeared repeatedly in the literature.3,5,10,57,61,67,71,81–83,85–100 Specifically, two-way communication between physicians and administration,24,58 as well as amongst physicians.45 Part of communication includes transparency101 and feedback.2,82 Feedback should be non judgmental and objective.102 This includes sharing of data99 that is valid and reliable.2,57,61,79,103,104 Feedback should be provided on performance,85,95,105,106 care processes86, and outcomes.107 Specific examples identified in the literature include feedback on screening rates, outcome data, and patient experience data.91,108 Data feedback can be used to support changes in behavior109 to improve outcomes and decrease mortality rates.110 Aggregate and individual performance data can also be used to reduce clinical costs.106
Incentives
Incentives are other antecedents discussed in the literature to encourage physician engagement.60 Regardless of whether incentives are financial21,79,111 or non financial,112 they need to be made known.113 Financial incentives may include compensation for time2,93 or structured incentives, whereby funding is linked to quality and performance goals and shift the basis of payment from volume to value.114 Incentives can also be tied to patient satisfaction.108 Shared savings are also identified as a good incentive as it helps to align goals.62 Type of payment model can also act as an incentive. Salaries or stipends are linked with increased alignment; however, capitation research (payment by the number of patients treated) suggests that the effect is disrupted when monetary incentives stress individual productivity.78 Pride, competitiveness, and status are considered non financial, implicit incentives. Call-list participation and admitting privileges are examples of explicit incentives or penalties.106 Using technology to make work easier can also act as an incentive, ie, mobile health technology strategy.115
Interpersonal relationships
Good working relations are required between physicians and administrations, with the alignment of goals24,52,116,117 values,4,30,82,117,118 and beliefs.119 There needs to be trust3,10,30,98,119 and respect, whereby opinions, ideas, and beliefs are valued,4,81,83 taken into account21 and physicians feel supported.71,120 There needs to be team leadership,86 team building94, and teamwork.3,4,27,48,89,121 It is important to identify champions,21,67,84,89,93,97,103,109,119,122–124 build relationships,53,125 and develop strategic partnerships,126 whether intergroup90 or peer.125
Opportunity
Opportunity appears to be a key antecedent to physician engagement, ensuring there is an opportunity to partake and be involved in decision-making10,53,59,67,70,71,81,83,84,127 and opportunities to assess and suggest possible improvements,86 improvement projects128, and leadership.57,83,125,129 Repeated often in the literature are opportunities for education, training, and support.56,61,67,79,81,97,102,103,107,120,123,124,128,130–135 This includes training on how to use data effectively.136 In addition to providing opportunity, organizations need to allot protected time2,101,105,129,137,138 and consideration to the time of day the opportunities are offered67 were also deemed important as was opportunities to participate in vocational training of junior doctors27 and involvement in the goals of interprofessional education139 and determining the status of physicians within the system.30
Findings in this review appear to align with work by the Institute for Healthcare Improvement (IHI). The IHI developed a framework to engage physicians in a shared quality agenda. This framework consisted of six elements: (1) discovering common purpose – link hospital quality agenda to physician quality agenda; (2) reframing values and beliefs – make the system a responsibility; (3) segment engagement plan – identify roles and plan to prepare physicians for that role; (4) use “engaging” improvement methods – identified by physicians themselves; (5) provide courage – provide backup and follow through; and (6) adopt an engaging style.140 This framework was based on work from Virginia Mason Medical Center, McLeod Regional Medical Center, Hackensack University Medical Center, Immanuel St. Joseph’s – Mayo Health System, and Tallahassee Memorial Hospital, in addition to several other multispecialty group practices, independent medical staffs, and the British National Health Service.140
Consequences
Considering the lack of empirical research in this area and the wide range of the use of the term, it is not surprising that the actual outcomes described in the literature are sparse with little detail. Outcomes of physician engagement tend to fall under one of the six broad categories. First, the improvement of data quality.136 Second health system efficiency21,63,141 that leads to cost reduction,1,3,57,78,82,91,106,109,129,135,141,142 and improved service provision.28 Third is innovation23 and fourth is job satisfaction. There is a debate in the literature regarding whether job satisfaction increases the likelihood of physician engagement3,97,143 or whether physician engagement drives job satisfaction.81,83,115,120 Once again suggesting this construct may not be unidirectional. Fifth is improved patient satisfaction and experience.91,98 Finally, physician engagement is associated with improved performance, both organizational1 and system performance,30,64,117,144 specifically decreased error,131,145 improved quality,3,28,49,76,146–148 better care,52,82,98,149 improved adverse medical reporting,113 improved access to specialists (ie, decreased wait times),150 health outcomes,40,62 clinical and decision outcomes,55,85,151 use of guidelines,54,71,134 screening,104,152 enrollment of patients,153 and implementation of protocols.124
A proposed definition and model of physician engagement
To date, not a single health system has determined how to define, measure, and improve medical engagement.31
The definition of physician engagement is regular participation of physicians in (1) deciding how their work is done, (2) making suggestions for improvement, (3) goal setting, (4) planning, and (5) monitoring of their own performance in activities targeted at the micro (patient), meso (organization), and/or macro (health system) levels.
The proposed physician engagement conceptual model is depicted in Figure 3. This figure suggests that a work environment that includes a culture of accountability, communication, incentives, good interpersonal relationships, and opportunity would enhance “physician engagement” and result in improved outcomes.
Figure 3.
“Physician engagement” conceptual model.
Step 8: defining empirical referents
Empirical referents are used to further develop an instrument. It uses evidence to help determine how a concept potentially could be measured.14 In other words, categories that by their presence, demonstrate the occurrence of the concept of physician engagement.
Alexander developed a measure of physician engagement, specifically to address racial and ethnic health care disparities based on the Awareness, Reflection, Empowerment and Action model.42 In other words, physicians being (1) aware of an issue; (2) reflecting on one’s role in solving it; (3) empowerment, recognizing that one has the power to make change; and lastly (4) action taken to solve the problem.
Spurgeon created the Medical Engagement Survey, which is broken down into (1) a collaborative workplace culture with learning opportunity and excellent interpersonal relationships; (2) clear direction and purpose, alignment of appraisal and rewards, participation in decision-making; and (3) empowerment and feeling valued, growth opportunity and job satisfaction.20 This example once again highlights the intertwining of the term engagement with other well-established distinct, constructs such as empowerment and satisfaction, perhaps contributing to the ambiguity of the term.
Based on what has been revealed by this review, the following could be used to develop an instrument. First, two things need to be established:
What activity/task is being measured?
What is considered “regular” for this specific activity/task, as this may vary depending on the activity/task.
Then, for the specific activity/task, determine if the physician is involved in the following:
deciding how their work is done
making suggestions for improvement
goal setting
planning
monitoring of their performance
Implications
This paper helps to shed light upon the diverse use of the term “physician engagement,” while delineating the concept from other well-established constructs. One cannot assume that discussions about physician engagement are premised upon a consistent and well-understood definition. With this lack of clarity about the term, it is not surprising that the IHI identified few health care institutions have improved physician engagement.140 Based on recent discussions with health care administrators and physician leaders across Canada,6 and the literature reviewed to date, clearly defining physician engagement, measuring it, and identifying areas for improvement continue to be a struggle for many health care organizations.
The first step is more of an educational initiative; however, it is a critical one. In short, everyone needs to have a similar baseline understanding to ensure that “physician engagement” as a concept has the same meaning for all. Secondly, a standardized tool needs to be developed to quantify the concept. Key indicators of physician engagement, although preliminary, are identified in this paper. Researchers and administrators and physician leadership can use this as a starting point to collect baseline data on the level of physician engagement.
As more rigorous empirical research is conducted, the most cost-effective strategies to enhance physician engagement can be identified and shared amongst sites. This would also allow for the linking of physician engagement to specific work outcomes.
Linking physician engagement to work performance measures will help to better comprehend how organizations may enhance engagement and is critical for hospital administrators and physician leadership in developing and utilizing the suitable skills to improve engagement levels.34 This paper is intended to initiate a broader dialogue within hospitals and beyond. To improve health care overall, it is critical to have physician engagement at all three levels: the patient, organization, and system.
Limitations
This is neither a meta-analysis nor systematic review, hence study quality is not evaluated.
Conclusion
Evaluation and synthesis of the literature on physician engagement has led to a clear definition and model of physician engagement, which can be used to develop an instrument to quantify this concept and accurately assess and compare the level of physician engagement across sites and health systems. This concept analysis is the first step in further advancing science in this area. Improving our comprehension of key antecedents of engagement may help health care administrators determine where best to focus resources.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Milliken AD. Physician engagement: a necessary but reciprocal process. Can Med Assoc J. 2014;186:244–245. doi: 10.1503/cmaj.131178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taitz JM, Lee TH, Sequist TD. A framework for engaging physicians in quality and safety. BMJ Qual Saf. 2012;21:722–728. doi: 10.1136/bmjqs-2011-000167 [DOI] [PubMed] [Google Scholar]
- 3.Jarousse L. Physician engagement (getting your docs on board!). Hosp Health Net. 2014;88:41–47. [PubMed] [Google Scholar]
- 4.Scott CG, Theriault A, McGuire S, Samson A, Clement C, Worthington JR. Developing a physician engagement agreement at The Ottawa Hospital: a collaborative approach. Healthc Q. 2012;15:50–53. [DOI] [PubMed] [Google Scholar]
- 5.Spaulding A, Gamm L, Menser T. Physician engagement: strategic considerations among leaders at a major health system. Hosp Top. 2014;92:66–73. doi: 10.1080/00185868.2014.937970 [DOI] [PubMed] [Google Scholar]
- 6.Perreira TA, Perrier L, Prokopy M. Hospital physician engagement. Med Care. 2018;56:969–975. doi: 10.1097/MLR.0000000000000983 [DOI] [PubMed] [Google Scholar]
- 7.Baker GR, Denis J-L. Medical leadership in health care systems: from professional authority to organizational leadership. Public Money Manage. 2011;31:355–362. [Google Scholar]
- 8.Denis J-L. Exploring the Dynamics of Physician Engagement and Leadership for Health System Improvement Prospects for Canadian. Toronto: Institute of Health Policy, Management and Evaluation, University of Toronto; 2013. [Google Scholar]
- 9.Davies H, Powell A, Rushmer R. Healthcare professionals’ views on clinician engagement in quality improvement. Lit Rev. 2007;1:4. [Google Scholar]
- 10.Kaissi A. Enhancing physician engagement: an international perspective. Int J Healthc Serv. 2014;44:567–592. doi: 10.2190/HS.44.3.h [DOI] [PubMed] [Google Scholar]
- 11.Thanakwang K, Isaramalai S. Productive engagement in older adults: a concept analysis. Nurs Health Sci. 2013;15:124–130. doi: 10.1111/nhs.12015 [DOI] [PubMed] [Google Scholar]
- 12.Coetzee SK, Klopper HC. Compassion fatigue within nursing practice: a concept analysis. Nurs Health Sci. 2010;12:235–243. doi: 10.1111/j.1442-2018.2010.00526.x [DOI] [PubMed] [Google Scholar]
- 13.Axley L. Competency: A Concept Analysis. Nursing Forum. Wiley Online Library; Malden, USA: Blackwell Publishing Inc. 2008;43(4):214–222. [DOI] [PubMed] [Google Scholar]
- 14.Walker LO, Avant KC. Strategies for Theory Construction in Nursing. Boston: Prentice Hall; 2011. [Google Scholar]
- 15.Chinn PL, Kramer MK. Theory and Nursing: a systematic approach. American Journal of Nursing 1983;83(10):1504. [Google Scholar]
- 16.Chinn PL, Kramer MK. Integrated Theory & Knowledge Development in Nursing-E-Book. 7th edn. Mosby, St Louis, MI: Elsevier Health Sciences; 2013. [Google Scholar]
- 17.Rodgers M, Sowden A, Petticrew M, et al. Testing methodological guidance on the conduct of narrative synthesis in systematic reviews: effectiveness of interventions to promote smoke alarm ownership and function. Evaluation. 2009;15:49–73. doi: 10.1177/1356389008097871 [DOI] [Google Scholar]
- 18.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 19.(n.d.) In Merriam-Webster’s collegiate dictionary. Available from: https://www.merriam-webster.com/dictionary/engagement. Accessed July3, 2019
- 20.Spurgeon P, Mazelan PM, Barwell F. Medical engagement: a crucial underpinning to organizational performance. Health Serv Manage Res. 2011;24:114–120. doi: 10.1258/hsmr.2011.011006 [DOI] [PubMed] [Google Scholar]
- 21.Skillman M, Cross-Barnet C, Singer RF, et al. Physician engagement strategies in care coordination: findings from the Centers for Medicare & Medicaid Services’ Health Care Innovation Awards Program. Health Serv Res. 2017;52:291–312. doi: 10.1111/1475-6773.12622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schaufeli WB, Salanova M, González-Romá V, Bakker AB. The measurement of engagement and burnout: a two sample confirmatory factor analytic approach. J Happiness Stud. 2002;3:71–92. doi: 10.1023/A:1015630930326 [DOI] [Google Scholar]
- 23.MacLeod D, Clarke N. Engaging for success: enhancing performance through employee engagement, a report to government. Richmond Surrey: Office of Public Sector Information. 2011. Available from: http://www.allthingsic.com/wp-content/uploads/2011/10/TheMacleodReport.pdf [Google Scholar]
- 24.Rinne ST, Rinne TJ, Olsen K, et al. Hospital administrators’ perspectives on physician engagement: a qualitative study. J Hosp Med. 2017. doi: 10.12788/jhm.2880 [DOI] [PubMed] [Google Scholar]
- 25.Shanafelt TD, Noseworthy JH. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92:129–146. doi: 10.1016/j.mayocp.2016.10.004 [DOI] [PubMed] [Google Scholar]
- 26.Vanderbilt SK, Wynia MK, Gadon M, Alexander GC. A qualitative study of physicians’ engagement in reducing healthcare disparities. J Natl Med Assoc. 2007;99:1315–1322. [PMC free article] [PubMed] [Google Scholar]
- 27.Ahnfeldt-Mollerup P, dePont Christensen R, Halling A, et al. Medical engagement and organizational characteristics in general practice. Fam Pract. 2015;33:69–74. doi: 10.1093/fampra/cmv085 [DOI] [PubMed] [Google Scholar]
- 28.Ahnfeldt-Mollerup P, Søndergaard J, Barwell F, Mazelan PM, Spurgeon P, Kristensen T. The relationships between use of quality-of-care feedback reports on chronic diseases and medical engagement in general practice. Qual Manag Health Care. 2018;27:191. doi: 10.1097/QMH.0000000000000188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clark J. Medical leadership and engagement: no longer an optional extra. J Health Organ Manag. 2012;26:437–443. doi: 10.1108/14777261211251517 [DOI] [PubMed] [Google Scholar]
- 30.Denis J-L, van Gestel N. Medical doctors in healthcare leadership: theoretical and practical challenges. BMC Health Serv Res. 2016;16:158. doi: 10.1186/s12913-016-1392-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dickinson H, Bismark M, Phelps G, Loh E. Future of medical engagement. Aust Health Rev. 2016;40:443–446. doi: 10.1071/AH14204 [DOI] [PubMed] [Google Scholar]
- 32.Parand A, Burnett S, Benn J, Iskander S, Pinto A, Vincent C. Medical engagement in organisation-wide safety and quality-improvement programmes: experience in the UK safer patients initiative. Qual Saf Health Care. 2010;19:e44. [DOI] [PubMed] [Google Scholar]
- 33.Ross P, Hubert J, Wong WL. Reducing the blame culture through clinical audit in nuclear medicine: a mixed methods study. JRSM Open. 2017;8:2054270416681433. doi: 10.1177/2054270416681433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spurgeon P, Long P, Clark J, Daly F. Do we need medical leadership or medical engagement? Leadersh Health Serv. 2015;28:173–184. doi: 10.1108/LHS-03-2014-0029 [DOI] [PubMed] [Google Scholar]
- 35.Perreira T, Berta W, Ginsburg L, Barnsley J, Herbert M. Insights into nurses’ work: exploring relationships among work attitudes and work-related behaviors. Health Care Manage Rev. 2018;43:315–327. doi: 10.1097/HMR.0000000000000151 [DOI] [PubMed] [Google Scholar]
- 36.Spurgeon P, Barwell F, Mazelan P. Developing a medical engagement scale (MES). Int J Clin Leadersh. 2008;16(4):213–223. [Google Scholar]
- 37.Perreira TA, Perrier L, Prokopy M. Hospital Physician Engagement. Medical care 2018;56(12):969–75. [DOI] [PubMed] [Google Scholar]
- 38.Perreira TA, Berta W, Hebert M. The employee retention triad in healthcare: exploring relationships among organizational justice, affective commitment and turnover intention. J Clin Nurs. 2018;27:e1451–e1461. doi: 10.1111/jocn.2018.27.issue-7pt8 [DOI] [PubMed] [Google Scholar]
- 39.Perreira TA, Berta W, Laporte A, et al. Shining a light: examining similarities and differences in the work psychology of health support workers employed in long-term care and home and community care settings. J Appl Gerontol. 2017. doi: 10.1177/0733464817737622. [DOI] [PubMed] [Google Scholar]
- 40.Agboola S, Palacholla RS, Centi A, Kvedar J, Jethwani K. A multimodal mhealth intervention (FeatForward) to improve physical activity behavior in patients with high cardiometabolic risk factors: rationale and protocol for a randomized controlled trial. JMIR Res Protoc. 2016;5:e84. doi: 10.2196/resprot.5489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Margalit RS, Roter D, Dunevant MA, Larson S, Reis S. Electronic medical record use and physician-patient communication: an observational study of Israeli primary care encounters. Patient Educ Couns. 2006;61:134–141. doi: 10.1016/j.pec.2005.03.004 [DOI] [PubMed] [Google Scholar]
- 42.Alexander GC, Lin S, Sayla MA, Wynia MK. Development of a measure of physician engagement in addressing racial and ethnic health care disparities. Health Serv Res. 2008;43:773–784. doi: 10.1111/j.1475-6773.2007.00780.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chelimsky TC, Fischer RL, Levin JB, Cheren MI, Marsh SK, Janata JW. The primary practice physician program for chronic pain (© 4PCP): outcomes of a primary physician-pain specialist collaboration for community-based training and support. Clin J Pain. 2013;29:1036–1043. doi: 10.1097/AJP.0b013e3182851584 [DOI] [PubMed] [Google Scholar]
- 44.Crenshaw K, Curry W, Salanitro AH, et al. Is physician engagement with Web-based CME associated with patients’ baseline hemoglobin A1c levels? The rural diabetes online care study. Acad Med. 2010;85:1511–1517. doi: 10.1097/ACM.0b013e3181eac036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mazurenko O, Hearld LR. Environmental factors associated with physician’s engagement in communication activities. Health Care Manage Rev. 2015;40:79–89. doi: 10.1097/HMR.0000000000000003 [DOI] [PubMed] [Google Scholar]
- 46.Involvement. Business Dictionary. Available from: http://www.businessdictionary.com/definition/employee-involvement.html. Accessed April 1, 2019.
- 47.Skarda D, Barnhart D. Quality, patient safety, and professional values. Semin Pediatr Surg. 2015;24:288–290. doi: 10.1053/j.sempedsurg.2015.08.006 [DOI] [PubMed] [Google Scholar]
- 48.Swensen S, Kabcenell A, Shanafelt T. Physician-organization collaboration reduces physician burnout and promotes engagement: the Mayo clinic experience. J Healthc Manag. 2016;61:105–127. [PubMed] [Google Scholar]
- 49.Dickinson H, Snelling I, Ham C, Spurgeon PC. Are we nearly there yet? A study of the English National Health Service as professional bureaucracies. J Health Organ Manag. 2017;31:430–444. doi: 10.1108/JHOM-01-2017-0023 [DOI] [PubMed] [Google Scholar]
- 50.Guo M, Tardif G, Bayley M. Medical safety huddles in rehabilitation: a novel patient safety strategy. Arch Phys Med Rehab. 2018;99(6):1217–1219. [DOI] [PubMed] [Google Scholar]
- 51.Jeffs L, Abramovich IA, Hayes C, et al. Implementing an interprofessional patient safety learning initiative: insights from participants, project leads and steering committee members. BMJ Qual Saf. 2013;22:923–930. doi: 10.1136/bmjqs-2012-001720 [DOI] [PubMed] [Google Scholar]
- 52.Bunkers B, Koch M, McDonough B, Whited B. Aligning physician compensation with strategic goals. Healthc Financ Manage. 2014;68:38–45. [PubMed] [Google Scholar]
- 53.Cox ED, Nackers KA, Young HN, Moreno MA, Levy JF, Mangione-Smith RM. Influence of race and socioeconomic status on engagement in pediatric primary care. Patient Educ Couns. 2012;87:319–326. doi: 10.1016/j.pec.2011.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Van Voorhees BW, Fogel J, Pomper BE, et al. Adolescent dose and ratings of an internet-based depression prevention program: a randomized trial of primary care physician brief advice versus a motivational interview. J Cogn Behav Psychother. 2009;9:1–19. [PMC free article] [PubMed] [Google Scholar]
- 55.Lipstein EA, Lovell DJ, Denson LA, et al. High levels of decisional conflict and decision regret when making decisions about biologics. J Pediatr Gastroenterol Nutr. 2016;63:e176–e81. doi: 10.1097/MPG.0000000000001425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Snell AJ, Briscoe D, Dickson G. From the inside out: the engagement of physicians as leaders in health care settings. Qual Health Res. 2011;21:952–967. doi: 10.1177/1049732311399780 [DOI] [PubMed] [Google Scholar]
- 57.Buell JM. Achieving financial success through improved physician engagement: revenue enhancements can be realized with stronger relationships. Healthc Exec. 2009;24:22–24. [PubMed] [Google Scholar]
- 58.Larson BK, Van Citters AD, Kreindler SA, et al. Insights from transformations under way at four Brookings-Dartmouth accountable care organization pilot sites. Health Aff. 2012;31:2395–2406. doi: 10.1377/hlthaff.2011.1219 [DOI] [PubMed] [Google Scholar]
- 59.Alliance N. Engaging Clinicians in the New NHS. London: NHS Alliance; 2003. [Google Scholar]
- 60.Akosa AN. Physician engagement is critical to the success of any accountable care organization. J Manag Care Med. 2013;16:67–76. [Google Scholar]
- 61.Daly R. Putting physicians in the lead for cost containment. Healthc Financ Manage. 2013;67:52–59. [PubMed] [Google Scholar]
- 62.Behm CR. ACOs in real life: a reflection on the medicare shared savings program. J Med Pract Manage. 2015;30:312–315. [PubMed] [Google Scholar]
- 63.Allin S, Guilcher S, Riley D, Zhang YJ. Improving health system efficiency: perspectives of decision-makers. Healthc Q. 2017;20:10–13. [DOI] [PubMed] [Google Scholar]
- 64.Bergevin Y, Habib B, Elicksen-Jensen K, et al. Transforming regions into high-performing health systems toward the triple aim of better health, better care and better value for Canadians. Healthcarepapers. 2016;16:34–52. [DOI] [PubMed] [Google Scholar]
- 65.Riney RG. Physician engagement. Partnering for collaboration. Hosp Health Net. 2012;86:63. [PubMed] [Google Scholar]
- 66.Kelly CM. Physician engagement: everybody wants you. Iowa Med. 2013;103:14–15. [PubMed] [Google Scholar]
- 67.Pariser P, Pus L, Stanaitis I, et al. Improving system integration: the art and science of engaging small community practices in health system innovation. Int J Family Med Print. 2016;2016:5926303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Saleeby E, Holschneider CH, Singhal R. Paradigm shifts: using a participatory leadership process to redesign health systems. Curr Opin Obstet Gynecol. 2014;26:516–522. doi: 10.1097/GCO.0000000000000122 [DOI] [PubMed] [Google Scholar]
- 69.Frattaroli S, Webster DW, Wintemute GJ. Implementing a public health approach to gun violence prevention: the importance of physician engagement. Ann Intern Med. 2013;158:697–698. doi: 10.7326/0003-4819-158-9-201305070-00597 [DOI] [PubMed] [Google Scholar]
- 70.Leone FT, Evers-Casey S, Graden S, Schnoll R. Behavioral economic insights into physician tobacco treatment decision-making. Ann Am Thorac Soc. 2015;12:364–369. doi: 10.1513/AnnalsATS.201410-467BC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lepore SJ, Nair RG, Davis SN, et al. Patient and physician factors associated with undisclosed prostate cancer screening in a sample of predominantly immigrant Black Men. J Immigr Minor Health. 2017;19:1343–1350. doi: 10.1007/s10903-016-0468-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kurtessis JN, Eisenberger R, Ford MT, Buffardi LC, Stewart KA, Adis CS. Perceived organizational support: a meta-analytic evaluation of organizational support theory. J Manage. 2017;43:1854–1884. doi: 10.1177/0149206315575554 [DOI] [Google Scholar]
- 73.Fishbein M, Jaccard J, Davidson AR, Ajzen I, Loken B. Predicting and Understanding Family Planning Behaviors. Understanding Attitudes and Predicting Social Behavior. Englewood Cliffs, NJ: Prentice Hall; 1980. [Google Scholar]
- 74.Sirgy MJ, Efraty D, Siegel P, Lee D-J. A new measure of quality of work life (QWL) based on need satisfaction and spillover theories. Soc Indic Res. 2001;55:241–302. doi: 10.1023/A:1010986923468 [DOI] [Google Scholar]
- 75.Culture. Business Disctionary. Available from: http://www.businessdictionary.com/definition/culture.html. Accessed April 1, 2019.
- 76.Byrnes J. Great physician engagement is key to great quality. Physician Leadersh J. 2015;2:40–42. [PubMed] [Google Scholar]
- 77.Harrison BA, Johnson AB. A generation of difference. Physician engagement in diversity and cultural competency integration. Healthc Exec. 2008;23:76. [PubMed] [Google Scholar]
- 78.O’Hare D, Kudrle V. Increasing physician engagement. Using norms of physician culture to improve relationships with medical staff. Physician Exec. 2007;33:38–45. [PubMed] [Google Scholar]
- 79.Calayag J. Physician engagement: strengthening the culture of quality and safety. Healthc Exec. 2014;29:28–30. [PubMed] [Google Scholar]
- 80.Erlandson E, Ludeman K. Physician engagement and shared accountability. Buzzwords, dilemma or choice? Mich Health Hosp. 2003;39:28–29. [PubMed] [Google Scholar]
- 81.Stark R. Increasing physician engagement: start with what’s important to physicians. J Med Pract Manage. 2014;30:171–175. [PubMed] [Google Scholar]
- 82.Studer Q, Hagins M Jr., Cochrane BS. The power of engagement: creating the culture that gets your staff aligned and invested. Healthc Manage Forum. 2014;27:S79–S97. doi: 10.1016/j.hcmf.2014.01.008 [DOI] [PubMed] [Google Scholar]
- 83.Whitlock DJ, Stark R. Understanding physician engagement - and how to increase it. Physician Leadersh J. 2014;1:8–12. [PubMed] [Google Scholar]
- 84.Patty B, Svendsen CA. A proven approach to physician engagement. Physician Exec. 2011;37:92–93. [PubMed] [Google Scholar]
- 85.Garvin D, Worthington J, McGuire S, et al. Physician performance feedback in a Canadian academic center. Leadersh Health Serv. 2017;30:457–474. doi: 10.1108/LHS-08-2016-0037 [DOI] [PubMed] [Google Scholar]
- 86.George AE, Frush K, Michener JL. Developing physicians as catalysts for change. Acad Med. 2013;88:1603–1605. doi: 10.1097/ACM.0b013e3182a7f785 [DOI] [PubMed] [Google Scholar]
- 87.Grace SM, Rich J, Chin W, Rodriguez HP. Flexible implementation and integration of new team members to support patient-centered care. Healthcare. 2014;2:145–151. doi: 10.1016/j.hjdsi.2014.02.003 [DOI] [PubMed] [Google Scholar]
- 88.Kim Y, Winner M, Page A, et al. Patient perceptions regarding the likelihood of cure after surgical resection of lung and colorectal cancer. Cancer. 2015;121:3564–3573. doi: 10.1002/cncr.29530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Friedman EL, Chawla N, Morris PT, et al. Assessing the development of multidisciplinary care: experience of the National Cancer Institute Community Cancer Centers Program. J Oncol Pract. 2015;11:e36–e43. doi: 10.1200/JOP.2014.001535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kreindler SA, Larson BK, Wu FM, et al. The rules of engagement: physician engagement strategies in intergroup contexts. J Health Organ Manag. 2014;28:41–61. doi: 10.1108/JHOM-02-2013-0024 [DOI] [PubMed] [Google Scholar]
- 91.Lee VS, Miller T, Daniels C, Paine M, Gresh B, Betz AL. Creating the exceptional patient experience in one academic health system. Acad Med. 2016;91:338–344. doi: 10.1097/ACM.0000000000001007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Manary M, Staelin R, Kosel K, Schulman KA, Glickman SW. Organizational characteristics and patient experiences with hospital care: a survey study of hospital chief patient experience officers. Am J Med Qual. 2015;30:432–440. doi: 10.1177/1062860614539994 [DOI] [PubMed] [Google Scholar]
- 93.Pantaleoni JL, Stevens LA, Mailes ES, Goad BA, Longhurst CA. Successful physician training program for large scale EMR implementation. Appl Clin Inform. 2015;6:80–95. doi: 10.4338/ACI-2014-09-CR-0076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Puri AK, Bhaloo T, Kirshin T, Mithani A. A comprehensive approach to effectively engage physicians during a hospital closure: using the physician engagement model. Healthc Manage Forum. 2006;19:34–39. doi: 10.1016/S0840-4704(10)60244-X [DOI] [PubMed] [Google Scholar]
- 95.Rangachari P. Role of social knowledge networking technology in facilitating meaningful use of electronic health record medication reconciliation. J Hosp Adm. 2016;5:98–106. doi: 10.5430/jha.v5n3p98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ricottone M. Reducing alternate level of care days at Winchester district memorial hospital. Healthc Manage Forum. 2015;28:190–194. doi: 10.1177/0840470415588668 [DOI] [PubMed] [Google Scholar]
- 97.Rosenstein AH. Strategies to Enhance Physician Engagement. J Med Pract Manage. 2015;31:113–116. [PubMed] [Google Scholar]
- 98.Sondheim SE, Patel DM, Chin N, et al. Governance practices in an era of healthcare transformation: achieving a successful turnaround. J Healthc Manag. 2017;62:316–326. doi: 10.1097/JHM-D-15-00036 [DOI] [PubMed] [Google Scholar]
- 99.Townsend CS, McNulty M, Grillo-Peck A. Implementing huddles improves care coordination in an academic health center. Prof Case Manag. 2017;22:29–35. doi: 10.1097/NCM.0000000000000200 [DOI] [PubMed] [Google Scholar]
- 100.Wei AC, Sandhu L, Devitt KS, et al. Practice patterns for the management of hepatic metastases from colorectal cancer: a mixed methods analysis. Ann Surg Oncol. 2013;20:1567–1574. doi: 10.1245/s10434-012-2698-3 [DOI] [PubMed] [Google Scholar]
- 101.Silver SA, Harel Z, McQuillan R, et al. How to begin a quality improvement project. Clin J Am Soc Nephrol. 2016;11:893–900. doi: 10.2215/CJN.11491015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hettema JE, Sorensen JL, Uy M, Jain S. Motivational enhancement therapy to increase resident physician engagement in substance abuse education. Subst Abus. 2009;30:244–247. doi: 10.1080/08897070903041210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Krein SL, Kowalski CP, Harrod M, Forman J, Saint S. Barriers to reducing urinary catheter use: a qualitative assessment of a statewide initiative. JAMA Intern Med. 2013;173:881–886. doi: 10.1001/jamainternmed.2013.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hayward K, Haaland WL, Hrachovec J, et al. Reliable pregnancy testing before intravenous cyclophosphamide: a quality improvement study. Pediatrics. 2016;138(6): e20160378- e20160378. [DOI] [PubMed] [Google Scholar]
- 105.Law TJ, Leistikow NA, Hoofring L, Krumm SK, Neufeld KJ, Needham DM. A survey of nurses’ perceptions of the intensive care delirium screening checklist. Dynamics (Pembroke, Ont). 2012;23:18–24. [PubMed] [Google Scholar]
- 106.Thompson D, Velasco F, Classen D, Raddemann RJ. Reducing clinical costs with an EHR. Healthc Financ Manage. 2010;64:106–108. [PubMed] [Google Scholar]
- 107.Hockey PM, Bates DW. Physicians’ identification of factors associated with quality in high- and low-performing hospitals. Jt Comm J Qual Patient Saf. 2010;36:217–223. doi: 10.1016/S1553-7250(10)36035-1 [DOI] [PubMed] [Google Scholar]
- 108.Rosen P, Burrows JF, Greenspan JS. Physician engagement in the transformation of the pediatric patient experience. J Pediatr. 2016;169:4–5. doi: 10.1016/j.jpeds.2015.11.023 [DOI] [PubMed] [Google Scholar]
- 109.Sears N. 5 strategies for physician engagement. Healthc Financ Manage. 2011;65:78–82. [PubMed] [Google Scholar]
- 110.Selvam A. Data, physician engagement key to decreasing mortality rate at UPHS. Mod Healthc. 2013;43:32. [PubMed] [Google Scholar]
- 111.Klugman R, Gitkind MJ, Walsh KE. The physician quality officer model: 5-year follow-up. Am J Med Qual. 2015;30:454–458. doi: 10.1177/1062860614536221 [DOI] [PubMed] [Google Scholar]
- 112.Lee TH. Financial versus non-financial incentives for improving patient experience. J Patient Exp. 2015;2:4–6. doi: 10.1177/237437431500200102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Xue Y, Yang J, Zhang J, Luo M, Zhang Z, Liang H. Motivating physicians to report adverse medical events in China: stick or carrot? J Patient Saf. 2017;1. doi: 10.1097/PTS.0000000000000371 [DOI] [PubMed] [Google Scholar]
- 114.Hebert GJ, Colasante C, Ilse RG, Forster AJ. Using structured incentives to increase value for money in an academic health sciences centre. Healthc Manage Forum. 2017;30:187–189. doi: 10.1177/0840470417698716 [DOI] [PubMed] [Google Scholar]
- 115.Martinez F. Developing a full-cycle mHealth strategy. Front Health Serv Manage. 2012;29:11–20. [PubMed] [Google Scholar]
- 116.Walsh KE, Ettinger WH, Klugman RA. Physician quality officer: a new model for engaging physicians in quality improvement. Am J Med Qual. 2009;24:295–301. doi: 10.1177/1062860609336219 [DOI] [PubMed] [Google Scholar]
- 117.Rice JA, Sagin T. New conversations for physician engagement. Five design principles to upgrade your governance model. Healthc Exec. 2010;25:66–70. [PubMed] [Google Scholar]
- 118.Weiss R. The quest for physician engagement: physician relationships are crucial in today’s changing environment. Mark Health Serv. 2011;31:29–31. [PubMed] [Google Scholar]
- 119.Gosfield AG, Reinertsen JL. Finding common cause in quality: confronting the physician engagement challenge. Physician Exec. 2008;34:26–28. [PubMed] [Google Scholar]
- 120.Marsden J, van Dijk M, Doris P, Krause C, Cochrane D. Improving care for British Columbians: the critical role of physician engagement. Healthc Q. 2012;15:51–55. [DOI] [PubMed] [Google Scholar]
- 121.Strasser DC, Burridge AB, Falconer JA, Uomoto JM, Herrin J. Toward spanning the quality chasm: an examination of team functioning measures. Arch Phys Med Rehabil. 2014;95:2220–2223. doi: 10.1016/j.apmr.2014.06.013 [DOI] [PubMed] [Google Scholar]
- 122.Nelson MF, Merriman CS, Magnusson PT, Thomassian KV, Strawn A, Martin J. Creating a physician-led quality imperative. Am J Med Qual. 2014;29:508–516. [DOI] [PubMed] [Google Scholar]
- 123.McFadyen C, Lankshear S, Divaris D, et al. Physician level reporting of surgical and pathology performance indicators: a regional study to assess feasibility and impact on quality. Can J Surg. 2015;58:31–40. doi: 10.1503/cjs.004314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Wilson KC, Merli GJ. Performance measures for improving the prevention of venous thromboembolism: achievement in clinical practice. J Thromb Thrombolysis. 2011;32:293–302. doi: 10.1007/s11239-011-0605-6 [DOI] [PubMed] [Google Scholar]
- 125.Duberman T, Hemker B, Solomon L. Innovative strategies for physician partnerships. One health system shares the steps it took to strengthen physician engagement. Healthc Exec. 2015;30:84–86. [PubMed] [Google Scholar]
- 126.Kraft S. Changes in acquisition patterns. Health systems rely on due diligence, physician engagement to ensure successful alignment. MGMA Connex/Med Group Manage Assoc. 2015;15:40–43. [PubMed] [Google Scholar]
- 127.Bremault-Phillips SC, Parmar J, Friesen S, Rogers LG, Pike A, Sluggett B. An evaluation of the decision-making capacity assessment model. Can Geriatr J. 2016;19:83–96. doi: 10.5770/cgj.19.222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Donaghy G, McKeever K, Flanagan C, et al. Helping doctors in training to STEP-UP: a leadership and quality improvement programme in the Belfast health and social care trust. Ulster Med J. 2018;87:112. [PMC free article] [PubMed] [Google Scholar]
- 129.Engelman D, Benjamin EM. Physician engagement: the “Secret sauce” to success in Bundled health care. Am J Med Qual. 2018;33(1):100–102. doi: 10.1177/1062860617703730. [DOI] [PubMed] [Google Scholar]
- 130.Patterson CJ. Best practices in specialty pharmacy management. J Manag Care Spec Pharm. 2013;19:42–48. doi: 10.18553/jmcp.2013.19.1.42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Gray D, Nussle R, Cruz A, et al. Effects of a catheter-associated urinary tract infection prevention campaign on infection rate, catheter utilization, and health care workers’ perspective at a community safety net hospital. Am J Infect Control. 2016;44:115–116. doi: 10.1016/j.ajic.2015.08.011 [DOI] [PubMed] [Google Scholar]
- 132.Tuttle JC. Cutting CAUTIs in critical care. J Clin Outcomes Manag. 2017;24:267–272. [Google Scholar]
- 133.Wynn JD, Draffin E, Jones A, Reida L. The Vidant health quality transformation. Jt Comm J Qual Patient Saf. 2014;40:212–218. doi: 10.1016/S1553-7250(14)40028-X [DOI] [PubMed] [Google Scholar]
- 134.Nordstrom BR, Saunders EC, McLeman B, et al. Using a learning collaborative strategy with office-based practices to increase access and improve quality of care for patients with opioid use disorders. J Addict Med. 2016;10:117–123. doi: 10.1097/ADM.0000000000000200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Sears NJ. Managing margins through physician engagement. Healthc Financ Manage. 2012;66:44–47. [PubMed] [Google Scholar]
- 136.Croft G. Engaging clinicians in improving data quality in the NHS. Institute of Health Record & Information Management. 2006;47(5-6):32. [PubMed] [Google Scholar]
- 137.Greysen SR, Detsky AS. Solving the puzzle of posthospital recovery: what is the role of the individual physician? J Hosp Med. 2015;10:697–700. doi: 10.1002/jhm.2421 [DOI] [PubMed] [Google Scholar]
- 138.Uy V, May SG, Tietbohl C, Frosch DL. Barriers and facilitators to routine distribution of patient decision support interventions: a preliminary study in community-based primary care settings. Health Expect. 2014;17:353–364. doi: 10.1111/j.1369-7625.2011.00760.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Whitehead C. The doctor dilemma in interprofessional education and care: how and why will physicians collaborate? Med Educ. 2007;41:1010–1016. doi: 10.1111/j.1365-2923.2007.02893.x [DOI] [PubMed] [Google Scholar]
- 140.Reinertsen JL, Gosfield AG, Rupp W, Whittington JW. Engaging Physicians in a Shared Quality Agenda. IHI Innovation Series White Paper. Cambridge, MA: Institute for Healthcare Improvement; 2007:1–48. [Google Scholar]
- 141.Harvey LFB, Smith KA, Curlin H. Physician engagement in improving operative supply chain efficiency through review of surgeon preference cards. J Minim Invasive Gynecol. 2017;24:1116–1120. doi: 10.1016/j.jmig.2017.06.018 [DOI] [PubMed] [Google Scholar]
- 142.Dawkins KD, Gershlick T, de Belder M, et al. Percutaneous coronary intervention: recommendations for good practice and training. Heart. 2005;91:1–27. doi: 10.1136/hrt.2004.042515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Lindgren A, Baathe F, Dellve L. Why risk professional fulfilment: a grounded theory of physician engagement in healthcare development. Int J Health Plann Manage. 2013;28:e138–57. doi: 10.1002/hpm.2142 [DOI] [PubMed] [Google Scholar]
- 144.Sandy LG, Rattray MC, Thomas JW. Episode-based physician profiling: a guide to the perplexing. J Gen Intern Med. 2008;23:1521–1524. doi: 10.1007/s11606-008-0684-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Pillai A, Medford ARL. Greater physician involvement improves coding outcomes in endobronchial ultrasound-guided transbronchial needle aspiration procedures. Respiration. 2013;85:417–421. doi: 10.1159/000346574 [DOI] [PubMed] [Google Scholar]
- 146.Caverzagie KJ, Bernabeo EC, Reddy SG, Holmboe ES. The role of physician engagement on the impact of the hospital-based practice improvement module (PIM). J Hosp Med. 2009;4:466–470. doi: 10.1002/jhm.495 [DOI] [PubMed] [Google Scholar]
- 147.Gosfield AG. Improving quality through physician engagement. Trustee. 2010;63:30–31. [PubMed] [Google Scholar]
- 148.Agarwal S, Kerwin M, Meindertsma J, Wolf A A novel decision aid to encourage smoking cessation among patients with low health literacy. Netherlands: 40th Annual Meeting of the Society of General Internal Medicine, SGIM 2017; 2017; United States 32 (2 Supplement 1) (pp S729); Springer New York LLC. [Google Scholar]
- 149.Baathe F, Ahlborg G Jr., Edgren L, Lagstrom A, Nilsson K. Uncovering paradoxes from physicians’ experiences of patient-centered ward-round. Leadersh Health Serv. 2016;29:168–184. doi: 10.1108/LHS-08-2015-0025 [DOI] [PubMed] [Google Scholar]
- 150.Schachter ME, Romann A, Djurdev O, Levin A, Beaulieu M. The British Columbia Nephrologists’ Access Study (BCNAS) - A prospective, health services interventional study to develop waiting time benchmarks and reduce wait times for out-patient nephrology consultations. BMC Nephrol. 2013;14 Arte Number: 182. ate of Pubaton: 2013. doi: 10.1186/1471-2369-14-182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Totten MK, Combes JR. Achieving stronger physician engagement. Steps CEOs and boards should take to understand and improve engagement. Healthc Exec. 2013;28:64–66. [PubMed] [Google Scholar]
- 152.Massie J, Ioannou L, Delatycki M. Prenatal and preconception population carrier screening for cystic fibrosis in Australia: where are we up to? Aust N Z J Obstet Gynaecol. 2014;54:503–509. doi: 10.1111/ajo.12255 [DOI] [PubMed] [Google Scholar]
- 153.Overman MJ, Morris V, Kee B, et al. Utility of a molecular prescreening program in advanced colorectal cancer for enrollment on biomarker-selected clinical trials. Ann Oncol. 2016;27:1068–1074. doi: 10.1093/annonc/mdw073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Maslach C, Leiter MP. Early predictors of job burnout and engagement. J Appl Psychol. 2008;93:498. doi: 10.1037/0021-9010.93.3.498 [DOI] [PubMed] [Google Scholar]
- 155.Mohapel P, Dickson G. Physician Engagement: Principles to Maximize Physician Participation in the Health Care System. Victoria, BC: Centre of Health Leadership and Research; 2007. [Google Scholar]
- 156.Rhoades L, Eisenberger R. Perceived organizational support: a review of the literature. J Appl Psychol. 2002;87:698. doi: 10.1037/0021-9010.87.4.698 [DOI] [PubMed] [Google Scholar]
- 157.Meyer JP, Stanley DJ, Herscovitch L, Topolnytsky L. Affective, continuance, and normative commitment to the organization: a meta-analysis of antecedents, correlates, and consequences. J Vocat Behav. 2002;61:20–52. doi: 10.1006/jvbe.2001.1842 [DOI] [Google Scholar]
- 158.Bowling NA, Hammond GD. A meta-analytic examination of the construct validity of the Michigan organizational assessment questionnaire job satisfaction subscale. J Vocat Behav. 2008;73:63–77. doi: 10.1016/j.jvb.2008.01.004 [DOI] [Google Scholar]
- 159.Spreitzer GM, Kizilos MA, Nason SW. A dimensional analysis of the relationship between psychological empowerment and effectiveness satisfaction, and strain. J Manage. 1997;23:679–704. [Google Scholar]
- 160.Koberg CS, Boss RW, Senjem JC, Goodman EA. Antecedents and outcomes of empowerment: empirical evidence from the health care industry. Group Organ Manage. 1999;24:71–91. doi: 10.1177/1059601199241005 [DOI] [Google Scholar]
- 161.Choi JN. Change‐oriented organizational citizenship behavior: effects of work environment characteristics and intervening psychological processes. J Occup Organ Psychol. 2007;28:467–484. doi: 10.1002/(ISSN)1099-1379 [DOI] [Google Scholar]